- 1Sichuan Ding Cheng Judical Expertise Center, Chengdu, China
- 2Department of Pediatric Surgery and Urology-Andrology, First Moscow State Medical University named after Sechenov, Moscow, Russia
- 3Faculty of Forensic Medicine, Zhongshan School of Medicine, Sun Yat-Sen University, Guangzhou, China
Cardiac injury plays a critical role in the process of thoracic trauma-related fatal outcomes. Historically, most patients who suffer a cardiac rupture typically die at the scene of occurrence or in the hospital, despite prompt medical intervention. Delayed cardiac rupture, although rare, may occur days after the initial injury and cause sudden unexpected death. Herein, we present the clinical details of a young man who suffered a chest stab injury and recovered well initially, but died days later due to delayed cardiac rupture. The forensic autopsy confirmed delayed cardiac rupture as the cause of death. We also reviewed previous similar reports to provide suggestions in such rare cases in clinical and forensic practice.
Highlights
• We report a case of sudden death due to delayed cardiac rupture.
• Delayed cardiac rupture and tamponade post chest trauma were carefully reviewed.
• The present case and literature review could provide reference in such rare cases in forensic practice.
Introduction
Thoracic trauma is the second-leading cause of morbidity and mortality and often involves cardiac injuries that can increase the mortality rate by 15 times (1). Given the varied definitions and diagnostic criteria of cardiac injury, its exact incidence is still unknown; however, previous studies have indicated that it ranges from 3% to 71% (2–4). Specifically, the incidence of cardiac rupture in chest trauma is reported to be 0.5% and is often associated with a lethal outcome (5). In 2023, Sessa et al. reviewed the published studies focusing on penetrating cardiac injury associated with firearm from 1990 to 2022, concluded that the morality of penetrating cardiac injury was affected by the location and severity of the heart injury, the interval between injury and medical intervention, the quantity of blood lost and presence of cardiac tamponade (6).
The presence of cardiac tamponade was common in the fatal cases indicating cardiac rupture is a medical emergency. Most patients die at the scene of occurrence without prompt medical intervention. By contrast, delayed cardiac rupture is a rare phenomenon that may cause sudden unexpected death in individuals with a history of chest trauma. It poses a significant threat to individuals who recover well at first after the initial chest injury in clinical practice. This complicates the link between the primary injury and subsequent fatal outcomes in forensic practice. However, the underlying mechanisms of delayed cardiac rupture are still debatable and require further investigation.
In this study, we present the clinical details of a young man who suffered a chest stab injury and recovered well initially, but died several days later because of delayed cardiac rupture, as confirmed by forensic autopsy.
Case presentation
A 21-year-old man was stabbed in the left front chest with a folding fruit knife and was subsequently admitted to the hospital. Radiographic examination revealed left hemothorax. Closed thoracic drainage and blood-transfusion were performed, and the patient's condition stabilized. However, 5 days later, his condition suddenly deteriorated, and he died despite receiving timely medical intervention.
A forensic autopsy was performed one day later, which revealed bilateral hemothorax, and 800 ml and 500 ml blood were found in the left and right thoracic cavities, respectively. A 1.2-cm-long oblique strip with a sharp-edge wound was found on the right side of the pericardium and the middle of the right ventricular anterior wall. The pericardial cavity was filled with blood up to a volume of approximately 100 ml. A 1.0-cm-long wound with the same characteristics was found in the middle of the right ventricular anterior wall and pierced into the cardiac chamber.
Numerous multinucleated cells infiltrated the epicardium at the trauma site in the right ventricle. Thrombosis, degenerated and necrotic myocardium, and macrophage infiltration were also observed at the trauma sites. To further evaluate the time interval post-injury, Masson's trichome and Prussian blue staining were performed. Large amounts of blue collagen fibers distributed at the injury site were observed by Masson staining (Figure 1). Other organs showed anemia without any pathological changes.
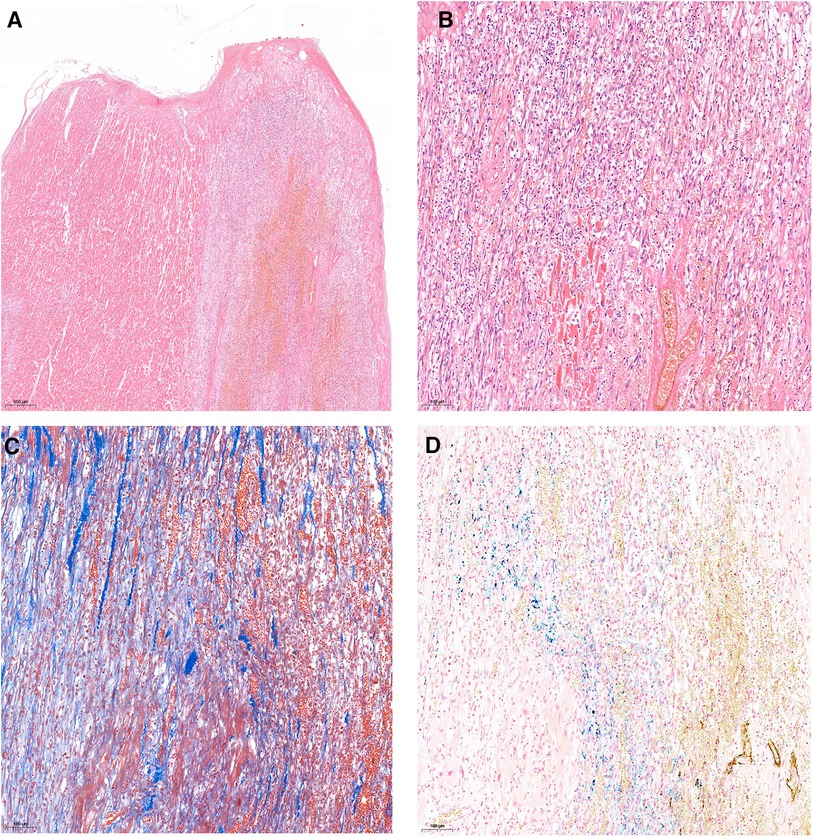
Figure 1. Histopathology examination of the trauma site on right ventricular anterior wall: thrombosis, degenerated and necrotic myocardium, and macrophages infiltration. (A) H&E staining, 20×; (B) H&E staining, 100×; (C) Masson's trichrome staining 100×, (D), Prussian blue staining, 100×.
Discussion
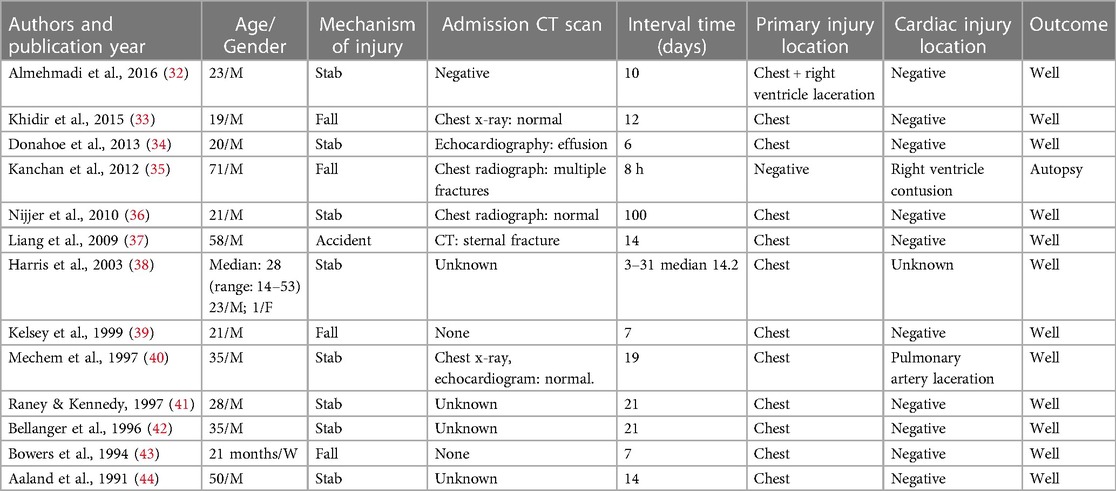
The incidence of penetrating chest trauma has increased in urban regions in the past three decades. The cause of penetrating cardiac injuries varies according to the population and culture, and stabbing is still the leading cause in China (7, 8). Penetrating cardiac trauma is associated with immediate fatal outcomes; however, delayed cardiac rupture, although rare, can occur. To better understand the characteristics of such cases, we carefully reviewed the literature on delayed cardiac rupture in PubMed, and have summarized them in Table 1 (9–28). Delayed cardiac rupture can occur as soon as several hours post-trauma or as long as after 74 days, but most of them occur within a month, with stabbing accounting for half of the reported cases.
Table 1 shows that according to previous reports, the left ventricle is the most common site of injury with delayed cardiac rupture. However, the anatomical location of the heart causes the right ventricle to be most frequently affected by a thoracic stab injury (29). The thinner wall of the right ventricle makes it impossible to close the defect by muscle overlap and contraction. Hence, the penetrating trauma may result in copious bleeding, even with low intraventricular pressure, resulting in rapid death. By contrast, the thick muscular wall in the left ventricle may easily close a stab injury and thus seal the trauma. However, even if the persistent bleeding is slight, it may still eventually result in cardiac tamponade, even with drainage intervention. The atria are most susceptible to penetrating trauma, as they completely lack a sealing effect (30). The formed thrombosis, which adheres tightly to the wound as in Case 1 may be the origin of the delayed cardiac rupture.
The data in Table 1 indicate that non-penetrating chest trauma can cause cardiac rupture, and common blunt cardiac rupture injuries among civilians, including traffic accidents, falls, heavy impact, and even a punch, can cause fatal damage. Cardiac ruptures are not always accompanied by thoracic wall injuries or rib fractures (31). Delayed cardiac rupture is often associated with hemopericardium as bleeding into the pericardial sac. To better understand the fatal outcome of delayed chest trauma, we searched for delayed hemopericardium or cardiac tamponade in PubMed, and have summarized the literatures on negative or healed cardiac injuries in Table 2 (32–44).
The clinical manifestations of chest traumas listed in Tables 1, 2 are common in that their condition is rather stable after primary medical intervention. Moreover, other examinations such as chest radiography and computed tomography show negative findings, even with cardiac rupture and effusion. A previous study has indicated that delayed cardiac ruptures can be asymptomatic (45). The post-trauma ECG may initially be abnormal; however, ECG changes are not specific, as they can also occur in normal autopsy findings, and delayed cardiac rupture may occur even with normal ECG post-injury (46–48). This was the same as the CK-MB level and echocardiography with respect to cardiac injury. CK-MB, echocardiography, repeated ECG, and chest radiographic examinations may play a role in suspected cardiac injury cases (22, 49).
In 2023, Sessa et al. reviewed the published studies focusing on penetrating cardiac injury associated with firearm from 1990 to 2022, and identified 38 articles, 39 cases were involved (6). Among which, 33 were males, the entrance wound is located in the anterior chest in 30 cases. Based on the study, he suggested that timely transport, resuscitation, and immediate surgery were the critical management in the therapy of penetrating cardiac injury. In 2022, Berrichi et al. reported delayed cardiac herniation after a traumatic pericardial rupture in an adult male who fall from 8m high, and the patient was rescued through timely surgery (50). In the present case, the entrance wound is on left front chest, and the decedent was given immediate surgery and he was recovered well at first. However, few days later he suffered from delayed cardiac rupture and tamponade and died. The asymptomatic of his later fatal complications delayed the diagnose of his complication and eventually resulted in his tragedy.
Although rare, delayed cardiac rupture and tamponade after chest trauma is a challenge in clinical and forensic practice. Physicians should bear in mind this rare complication to provide better medical therapy. In forensic practice, the original cause of later cardiac complications and time interval after the primary injury make the real link underlying them more complicated. Forensic pathologists should carefully document the primary injury and thoroughly investigate the patient's medical history and interval time through histopathological examination and other advanced technologies.
Conclusion
Delayed cardiac rupture and tamponade after chest trauma are rare in clinical and forensic practice and may cause sudden death. The casual link between the primary injury and later complications remains to be elucidated.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The requirement of ethical approval was waived by Zhongshan School of Medicine Sun Yat Sen University for the studies involving humans. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LT: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. XG: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. HL: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. SZ: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fineschi V, Baroldi G, Silver MD. Pathology of the Heart and Sudden Death in Forensic Medicine. London: CRC (2006).
2. Sybrandy KC, Cramer MJ, Burgersdijk C. Diagnosing cardiac contusion: old wisdom and new insights. Heart. (2003) 89:485–9. doi: 10.1136/heart.89.5.485
3. McGillicuddy D, Rosen P. Diagnostic dilemmas and current controversies in blunt chest trauma. Emerg Med Clin North Am. (2007) 25:695–711. doi: 10.1016/j.emc.2007.06.004
4. Holanda MS, Domínguez MJ, López-Espadas F, López M, Díaz-Regañón J, Rodríguez-Borregán JC. Cardiac contusion following blunt chest trauma. Eur J Emerg Med. (2006) 13:373–6. doi: 10.1097/MEJ.0b013e32801112f6
5. Darok M, Beham-Schmid C, Gatternig R, Roll P. Sudden death from myocardial contusion following an isolated blunt force trauma to the chest. Int J Legal Med. (2001) 115:85–9. doi: 10.1007/s004140100230
6. Sessa F, Cocimano G, Esposito M, Zuccarello P, Scoto E, Mazzeo P, et al. Systematic review of penetrating cardiac injury by a firearm: forensic implications. Healthcare (Basel). (2023) 11:265. doi: 10.3390/healthcare11020265
7. Kang N, Hsee L, Rizoli S, Alison P. Penetrating cardiac injury: overcoming the limits set by nature. Injury. (2009) 40:919–27. doi: 10.1016/j.injury.2008.12.008
8. Rendon F, Danes LHG, Castro M. Delayed cardiac tamponade after penetrating thoracic trauma. Asian Cardiovasc Thorac Ann. (2004) 12:139–42. doi: 10.1177/021849230401200212
9. Ochi A, Hardikar AA. Delayed presentation of cardiac injury four weeks after stabbing. Asian Cardiovasc Thorac Ann. (2020) 28:62–4. doi: 10.1177/0218492319874271
10. Dokoupil M, Marecová K, Uvíra M, Joukal M, Mrázková E, Chmelová J, et al. Fatal delayed hemopericardium and hemothorax following blunt chest trauma. Forensic Sci Med Pathol. (2019) 15:272–5. doi: 10.1007/s12024-018-0069-5
11. Pooniya S, Behera C, Mridha AR, Swain R. Cardiac rupture delayed for a week in an asymptomatic child following blunt trauma. Med Sci Law. (2016) 56:217–20. doi: 10.1177/0025802414562500
12. Greene CL, Boyd JH. Successful operative repair of delayed left ventricle rupture from blunt trauma. Ann Thorac Surg. (2016) 102:e101–3. doi: 10.1016/j.athoracsur.2016.01.031
13. Esfahanizadeh J, Abbasi Tashnizi M, Moeinipour AA, Sepehri Shamloo A. Undetected aorto-RV fistula with aortic valve injury and delayed cardiac tamponade following a chest stab wound: a case report. Trauma Mon. (2013) 18:95–7. doi: 10.5812/traumamon.11607
14. Bartoloni G, Trio F, Bartoloni A, Giorlandino A, Pucci A. A fatal stab wound causing selective injury to the left anterior descending coronary artery, myocardial infarction and delayed cardiac tamponade. Forensic Sci Int. (2013) 229:e16–8. doi: 10.1016/j.forsciint.2013.03.023
15. Ueda S, Ito Y, Konnai T, Suzuki S, Isogami K. Delayed cardiac rupture occurring two months after blunt chest trauma. Gen Thorac Cardiovasc Surg. (2011) 59:45–7. doi: 10.1007/s11748-010-0625-8
16. Hermens JA, Wajon EM, Grandjean JG, Haalebos MM, von Birgelen C. Delayed cardiac tamponade in a patient with previous minor blunt chest trauma. Int J Cardiol. (2009) 131:e124–6. doi: 10.1016/j.ijcard.2007.07.080
17. Babin-Ebell J, Roth P. Delayed pericardial tamponade, mitral insufficiency and VSD after stab wound to the heart. Thorac Cardiovasc Surg. (2008) 56:113–4. doi: 10.1055/s-2007-965710
18. Eisenman A, Vasan A, Joseph L, Aravot D. Unusual delayed manifestation of a penetrating chest trauma. Eur J Trauma. (2006) 32:396–8. doi: 10.1007/s00068-006-5073-x
19. Moore FO, Berne JD, Fulda GJ, Fox AD, Tinkoff GH, Davies AL, et al. Atriocaval laceration presenting as delayed pericardial tamponade. J Thorac Cardiovasc Surg. (2006) 132:194–5. doi: 10.1016/j.jtcvs.2006.03.022
20. Murai N, Saito M, Chiba T, Okada S, Imazeki T. Delayed blow-out type rupture of the right ventricle following blunt chest trauma. Jpn J Thorac Cardiovasc Surg. (2003) 51:696–8. doi: 10.1007/s11748-003-0015-6
21. Murillo CA, Owens-Stovall SK, Kim S, Thomas RP, Chung DH. Delayed cardiac tamponade after blunt chest trauma in a child. J Trauma. (2002) 52:573–5. doi: 10.1097/00005373-200203000-00029
22. Lassus J, Tulikoura I, Konttinen YT, Santavirta S. Myocardial contusion as a cause of delayed cardiac rupture. A case report. Injury. (2001) 32:789–93. doi: 10.1016/S0020-1383(01)00105-X
23. Klinkenberg TJ, Kaan GL, Lacquet LK. Delayed squealee of penetrating chest trauma: a plea for early sternotomy. J Cardiovasc Surg. (1994) 35:173–5.
24. Pollak S, Stellwag-Carion C. Delayed cardiac rupture due to blunt chest trauma. Am J Forensic Med Pathol. (1991) 12:153–6. doi: 10.1097/00000433-199106000-00012
25. Martin R, Mitchell A, Dhalla N. Late pericardial tamponade and coronary arteriovenous fistula after trauma. Br Heart J. (1986) 55:216–8. doi: 10.1136/hrt.55.2.216
26. Lempinem M, Silvonen E. Sydantamponaatio yhdeksan vuorokautta rintakehan pistohaavab jalkeen. Jatetty Toimitukselle. (1972) 8:49–51.
27. Pastor BH, Betts RH. Late symptoms due to traumatic hemopericardium. N Engl J Med. (1961) 265:1139–43. doi: 10.1056/NEJM196112072652304
28. Cosman B, Byerly WG, Wichern WA. Penetrating wound of the heart with delayed recurrent hemothorax; case report. Ann Surg. (1958) 147:87–92. doi: 10.1097/00000658-195801000-00015
29. Leite L, Gonçalves L, Nuno Vieira D. Cardiac injuries caused by trauma: review and case reports. J Forensic Leg Med. (2017) 52:30–4. doi: 10.1016/j.jflm.2017.08.013
30. Karmy-Jones R, van Wijngaarden MH, Talwar MK, Lovoulos C. Penetrating cardiac injuries. Injury. (1997) 28:57–61. doi: 10.1016/S0020-1383(96)00141-6
31. Durak D. Cardiac rupture following blunt trauma. J Forensic Sci. (2001) 46:171–2. doi: 10.1520/JFS14931J
32. Almehmadi F, Chandy M, Connelly KA, Edwards J. Delayed tamponade after traumatic wound with left ventricular compression. Case Rep Cardiol. (2016) 2016:2154748. doi: 10.1155/2016/2154748
33. Khidir HH, Bloom JP, Hawkins AT. Delayed recurrent pericarditis complicated by pericardial effusion and cardiac tamponade in a blunt trauma patient. J Emerg Trauma Shock. (2015) 8:49–51. doi: 10.4103/0974-2700.150398
34. Donahoe L, Ouzounian M, MacDonald S, Field S. Delayed pericardial effusion and cardiac tamponade following penetrating chest trauma. CJEM. (2013) 15:186–9. doi: 10.2310/8000.2012.120729
35. Kanchan T, Menezes RG, Acharya PB, Monteiro FN. Blunt trauma to the chest–a case of delayed cardiac rupture. J Forensic Leg Med. (2012) 19:46–7. doi: 10.1016/j.jflm.2011.07.012
36. Nijjer SS, Dubrey SW, Dreyfus GD, Grocott-Mason R. Delayed pericardial effusions: life-threatening complication presenting up to 100 days after chest trauma. Clin Med (Lond). (2010) 10:88–90. doi: 10.7861/clinmedicine.10-1-88
37. Liang HM, Chen QL, Zhang EY, Hu J. Sternal fractures and delayed cardiac tamponade due to a severe blunt chest trauma. Am J Emerg Med. (2016) 34:758. doi: 10.1016/j.ajem.2015.07.075
38. Harris DG, Janson JT, Van Wyk J, Pretorius J, Rossouw GJ. Delayed pericardial effusion following stab wounds to the chest. Eur J Cardiothorac Surg. (2003) 23:473–6. doi: 10.1016/S1010-7940(03)00006-X
39. Kelsey JH, Henderson SO, Newton K. Bedside ultrasound in delayed traumatic pericardial effusion. Am J Emerg Med. (1999) 17:313–4. doi: 10.1016/S0735-6757(99)90136-5
40. Mechem CC, Alam GA. Delayed cardiac tamponade in a patient with penetrating chest trauma. J Emerg Med. (1997) 15:31–3. doi: 10.1016/S0736-4679(96)00240-5
41. Raney JL, Kennedy ES. Delayed cardiac tamponade following a stab wound: a case report. J Ark Med Soc. (1997) 93:589–91.9154744
42. Bellanger D, Nikas DJ, Freeman JE, Izenberg S. Delayed posttraumatic tamponade. South Med J. (1996) 89:1197–9. doi: 10.1097/00007611-199612000-00013
43. Bowers P, Harris P, Truesdell S, Stewart S. Delayed hemopericardium and cardiac tamponade after unrecognized chest trauma. Pediatr Emerg Care. (1994) 10:222–4. doi: 10.1097/00006565-199408000-00010
44. Aaland MO, Sherman RT. Delayed pericardial tamponade in penetrating chest trauma: case report. J Trauma. (1991) 31:1563–65. doi: 10.1097/00005373-199111000-00022
45. Hirschl DA, Jain VR, Spindola-Franco H, Gross JN, Haramati LB. Prevalence and characterization of asymptomatic pacemaker and ICD lead perforation on CT. Pacing Clin Electrophysiol. (2007) 30:28–32. doi: 10.1111/j.1540-8159.2007.00575.x
46. Potkin RT, Werner JA, Trobaugh GB, Chestnut CH 3rd, Carrico CJ, Hallstrom A, et al. Evaluation of noninvasive tests of cardiac damage in suspected cardiac contusion. Circulation. (1982) 66:627–31. doi: 10.1161/01.CIR.66.3.627
47. Blair E, Topuzlu C, Davis JH. Delayed or missed diagnosis in blunt chest trauma. J Trauma. (1971) 11:129–45. doi: 10.1097/00005373-197102000-00005
48. Hiatt JR, Yeatman LA Jr, Child JS. The value of echocardiography in blunt chest trauma. J Trauma. (1988) 28:914–22. doi: 10.1097/00005373-198807000-00003
49. Karalis DG, Victor MF, Davis GA, McAllister MP, Covalesky VA, Ross JJ Jr, et al. The role of echocardiography in blunt chest trauma: a transthoracic and transesophageal echocardiographic study. J Trauma. (1994) 36:53–8. doi: 10.1097/00005373-199401000-00008
Keywords: pathology, autopsy, delayed cardiac rupture, cardiac tamponade, case report
Citation: Tinzin L, Gao X, Li H and Zhao S (2024) Sudden death associated with delayed cardiac rupture: case report and literature review. Front. Cardiovasc. Med. 11:1355818. doi: 10.3389/fcvm.2024.1355818
Received: 14 December 2023; Accepted: 3 April 2024;
Published: 12 April 2024.
Edited by:
Junjie Xiao, Shanghai University, ChinaReviewed by:
Francesco Patanè, Azienda Ospedaliera Ospedali Riuniti Papardo Piemonte, ItalyFrancesco Sessa, University of Catania, Italy
© 2024 Tinzin, Gao, Li and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuquan Zhao emhhb3NocTI3QG1haWwuc3lzdS5lZHUuY24=
†These authors have contributed equally to this work
 Lopsong Tinzin1†
Lopsong Tinzin1† Shuquan Zhao
Shuquan Zhao