- 1Epidemiology, Medical Faculty, University of Augsburg, Augsburg, Germany
- 2Department of Cardiology, Respiratory Medicine and Intensive Care, University Hospital Augsburg, Augsburg, Germany
- 3KORA Study Centre, University Hospital of Augsburg, Augsburg, Germany
- 4Helmholtz Zentrum München, German Research Center for Environmental Health, Institute for Epidemiology, Neuherberg, Germany
- 5Chair of Epidemiology, Institute for Medical Information Processing, Biometry and Epidemiology, Medical Faculty, Ludwig-Maximilians-Universität München, Munich, Germany
- 6German Center for Diabetes Research (DZD) Neuherberg, Neuherberg, Germany
Background: The objective of this study was to investigate the differences in presenting symptoms between patients with and without diabetes being diagnosed with an acute myocardial infarction (AMI).
Methods: A total of 5,900 patients with a first-time AMI were included into the analysis. All patients aged between 25 and 84 years were recorded by the population-based Myocardial Infarction Registry in Augsburg, Germany, between 2010 and 2017. The presence (yes/no) of 12 AMI typical symptoms during the acute event was assessed within the scope of a face-to-face interview. Multivariable adjusted logistic regression models were calculated to analyze the associations between presenting symptoms and diabetes mellitus in AMI patients.
Results: Patients with diabetes had significantly less frequent typical pain symptoms, including typical chest pain. Also, other symptoms like sweating, vomiting/nausea, dizziness/vertigo and fear of death/feeling of annihilation occurred significantly more likely in non-diabetic patients. The only exception was the symptom of shortness of breath, which was found significantly more often in patients with diabetes. In multivariable-adjusted regression models, however, the observed effects were attenuated. In patients younger than 55 years, the associations between diabetes and various symptoms were mainly missing.
Conclusions: Type 2 diabetes mellitus is a risk factor not only for the development of AMI, but is also associated with an adverse outcome after AMI. Atypical clinical presentation additionally complicates the diagnostic process. It is therefore essential for physicians to be aware of the more often atypical symptoms that diabetic AMI patients report.
1 Background
Type 2 diabetes is a rising health problem worldwide (1). Among many other health consequences, it increases the risk of coronary artery disease (CAD) with subsequent acute myocardial infarction (AMI) (2). In AMI patients, a diabetes diagnosis additionally goes along with worse outcomes and higher mortality (3, 4). Therefore, early diagnosis and timely treatment of diabetes are especially important. Prior studies indicated that AMI patients with diabetes less often report typical chest pain symptoms and some other typical AMI symptoms (5–10). Thus, diagnostics of AMI in diabetic patients would be impeded. However, there are also studies reporting conflicting results by indicating no (relevant) differences in typical AMI symptoms between patients with and without diabetes (11–15). Consequently, the current scientific knowledge is quite ambiguous and often based on smaller samples of AMI patients. So the aim of this study was to investigate the association between the presence of type 2 diabetes and the frequency of a variety of specific AMI symptoms using population-based data and calculating multivariable logistic regression models thereby taking into account various potential confounders.
2 Methods
2.1 Study population
This study uses data from the population-based Augsburg Myocardial Infarction Registry. As part of the MONICA-project (Monitoring Trends and Determinants in Cardiovascular disease) it was established in 1984 and since 1996 operated as the KORA Myocardial Infarction Registry (16). Since 2021, it is continued as Augsburg Myocardial Infarction Register at the University Hospital Augsburg. The study area includes the city of Augsburg, Germany, and the two adjacent counties (approximately 680,000 inhabitants in total). All cases of hospitalized AMI were recorded on the following conditions: the patient survived the first 24 h after hospital admission, had his/her primary residence within the study area and was between 25 and 84 years of age at time of infarction. Detailed information on case identification, diagnostic classification of events and quality control of the data can be found in a previous publication (16). All study participants gave written informed consent. Methods of data collection have been approved by the ethics committee of the Bavarian Medical Association (Bayerische Landesärztekammer) and the study was performed in accordance with the Declaration of Helsinki.
For the following statistical analysis, only patients with a first-time AMI between 2010 and 2017 were considered (n = 6,327 cases). All patients with missing information on typical chest pain symptoms or relevant covariables (n = 427) were excluded. The final study population consisted of 5,900 patients with incident AMI.
2.2 Data collection
During hospital stay the patients were interviewed by trained study nurses in a face-to-face interview at the general ward. A standardized questionnaire was used including questions about specific symptoms in the context of the acute event. The patients were asked about the presence (yes/no) of the following symptoms: typical chest pain symptoms (defined as “chest pain or a feeling of pressure or tightness behind the breastbone”), pain in the left arm/shoulder, pain in the right arm/shoulder, pain between the shoulder blades, pain in the upper abdomen, pain in the throat/jaw, sweating, vomiting/nausea, shortness of breath, dizziness/vertigo, syncope/unconsciousness and fear of death/feeling of annihilation. In addition to the interview, the patients’ medical chart was reviewed in order to collect demographic data, data on cardiovascular risk factors, medical history, comorbidities, laboratory values, in-hospital course and medication.
The presence of diabetes mellitus was assessed by the patient's statement in the interview as well as by extracting relevant information from the medical record. The patient was assigned to the diabetes group if either he clearly stated to have a medical diagnosis of diabetes mellitus and/or there was an explicit indication of a diabetes mellitus diagnosis in the medical chart. In case neither in the interview nor in the medical chart there was an explicit indication of diabetes mellitus, the patients was assigned to the non-diabetes group. For this study, we did not distinguish between diabetes mellitus type 1 and type 2.
2.3 Statistical analysis
Categorical variables were presented as absolute frequencies with percentages and Chi-square tests were used to test for group differences. Continuous variables were presented as mean (standard deviation, SD) or as median (inter-quartiles range, IQR) and Student's t-test and Mann–Whitney U test, respectively, were applied to test differences between the groups.
For the continuous variables peak CKMB levels and prehospital time (in minutes) we conducted multiple imputation by chained equations (imputation method: “predictive mean matching” with linear regression as the regression model for the variables “peak CKMB levels” and “prehospital time”, the number of iterations: 5, number of created imputed data sets: 5). The variables were initially square-rooted due to a strong right-skewed distribution. The imputation process was performed with MICE-package (R statistic software). The subsequent regression models were calculated for each of the 5 imputed data sets and results were pooled in the end.
2.4 Logistic regression models
Logistic regression models were calculated in order to examine the association between diabetes and specific symptoms. First, unadjusted models were calculated. Next, we calculated models adjusted for sex and age. Finally, according to literature review, the multivariable adjusted logistic models were adjusted for sex, age, type of infarction (STEMI, NSTEMI, bundle branch block), renal function according to eGFR (groups: eGFR > 60 ml/min/1.73 m2, 30–60 ml/min/1.73 m2, < 30 ml/min/1.73 m2 and a group with missing information), left ventricular ejection fraction (groups: EF > 30%, EF ≤ 30%, no information on EF), prehospital time in minutes and peak CKMB levels. For the regression models, the values of continuous variables prehospital time and peak CKMB levels were used with square rooted values due to strong right-skewed distributions.
Moreover, we performed subgroup analysis to examine differences between age groups. We stratified the sample into 4 age groups: patients <55 years of age, patients between 55 and 64, patients between 65 and 74, and patient between 75 and 84 years. For each group, we calculated the multivariable adjusted logistic regression models as described above for the total sample.
All statistical analyses were performed using R version 4.2.1.
3 Results
Overall, 5,900 cases of first-time AMI were included in the present analysis. Table 1 displays baseline characteristics, symptoms at the event, clinical parameters and information about treatment stratified for diabetes (yes/no). In total, 1,859 (31.5%) patients had a known diagnosis of diabetes mellitus at the time of the acute event. Within the diabetes group, women were slightly overrepresented: 33.6% of all patients were female in the diabetes group, while in the non-diabetes group only 29.5% were women. With a mean age of 69.0 (SD: 10.7) years, the diabetes patients were significantly older than the non-diabetes patients with 65.1 (SD: 12.2) years. The patients with diabetes also had significantly more frequently other comorbidities (hypertension, hyperlipidemia, impaired renal function, severely impaired ventricular ejection fraction). On the other hand, patients with diabetes were significantly less likely to receive PCI treatment compared to non-diabetic AMI patients.
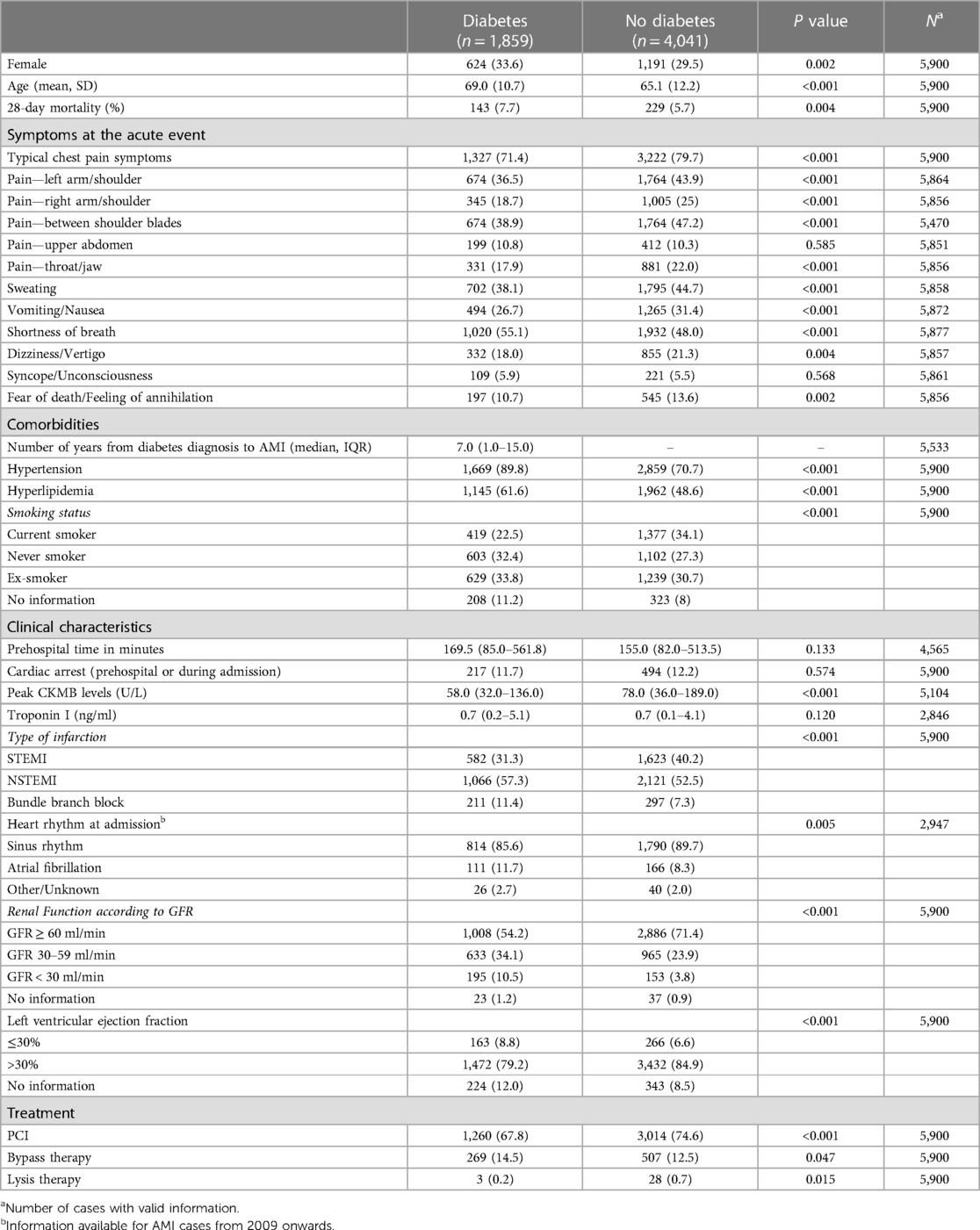
Table 1. Baseline characteristics for the total sample and stratified for diabetes (yes/no) given by total number and % or mean and SD or median and IQR.
3.1 Diabetes and symptoms at the acute event
The most frequently occurring symptom at the event was typical chest pain, which was reported by 71.4% of patients with diabetes, which is significantly less often than in the non-diabetes group (79.7%), see Table 1. The same refers to pain in other parts of the body, which occurred significantly more frequently in non-diabetes patients (except upper abdomen). Likewise, the unspecific symptoms sweating, vomiting/nausea, dizziness/vertigo and fear of death/feeling of annihilation were reported significantly less frequently by individuals with diabetes. Surprisingly, shortness of breath was the only symptom that was significantly more present in patients with diabetes (Table 1).
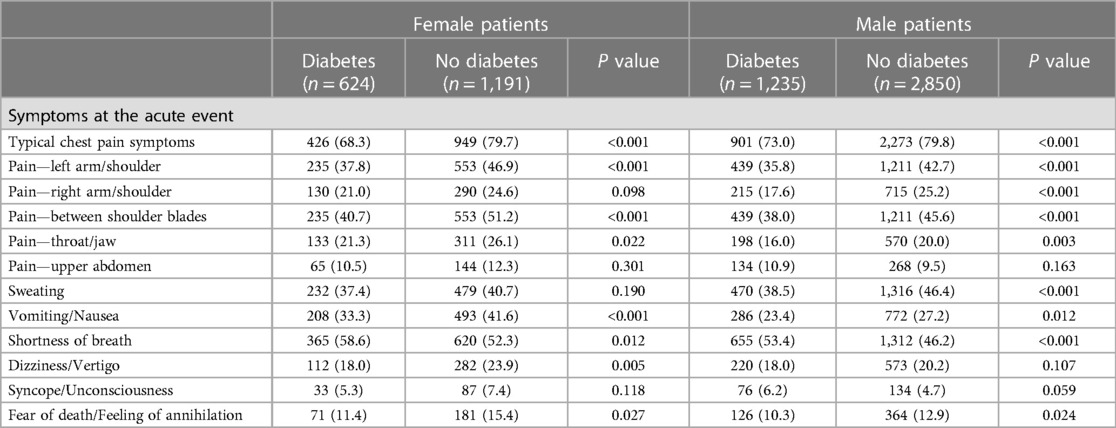
Table 2 shows the frequency of specific symptoms stratified for sex and diabetes. The figure indicates, that the associations between diabetes and various symptoms observed see Table 1 are valid for males and females alike.
Figure 1 shows the percentages of different symptoms in the diabetes group and the non-diabetes group. The figure suggests, that the older age group does not differ very much from the total sample. But the figure also shows, that patients with diabetes in the age group 55 years and younger were more likely to have some specific symptoms compared to their non-diabetic controls indicating a different associations for this age group.
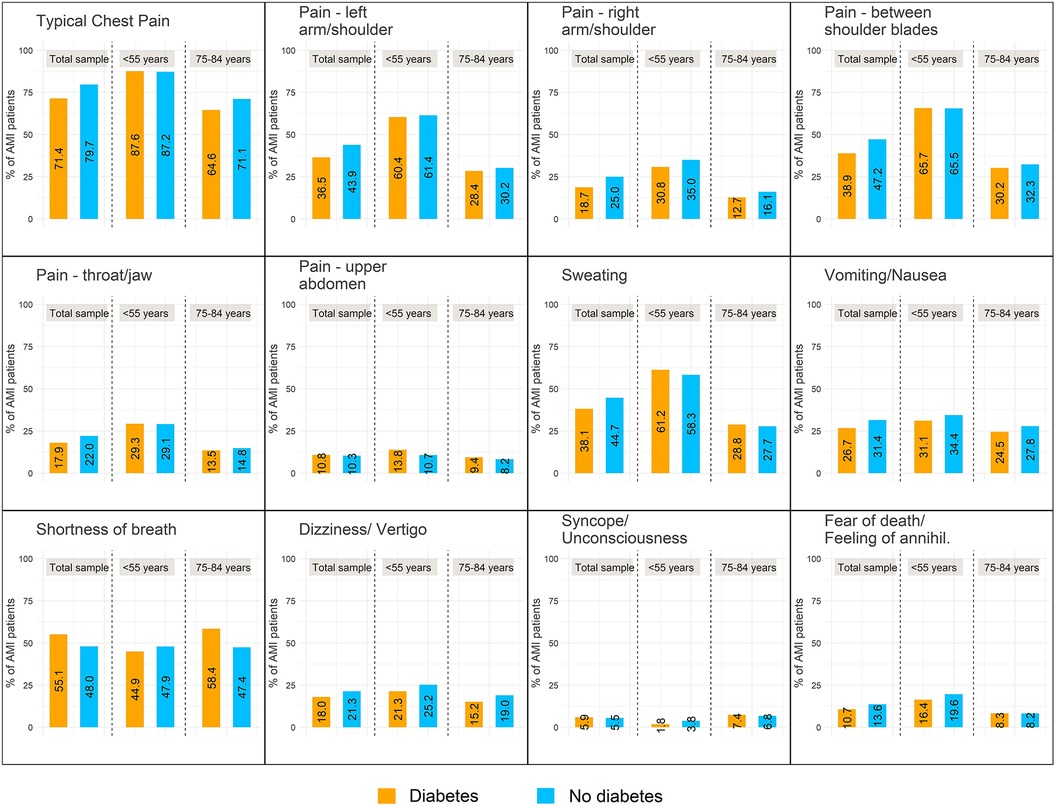
Figure 1. Relative frequencies of reported symptoms at AMI stratified for diabetes. On the left hand side of each plot the percentages for the total sample are plotted; in the middle the respective frequencies for young patients (<55 years) and on the right hand side the frequencies for older patients (age group 75–84 years) are displayed.
Table 3 displays the results of different logistic regression models analyzing the associations between diabetes (exposure) and specific symptoms (outcome). The unadjusted models and the models adjusted for sex and age actually provide comparable results in line with the relative frequencies shown in Table 1: while diabetes showed significant negative associations with several pain symptoms (including typical chest pain) and other symptoms, shortness of breath showed a strong positive association with diabetes. While the latter association between shortness of breath and diabetes was confirmed by the multivariable adjusted model, the association of diabetes with most other symptoms appeared strongly attenuated in the multivariable adjusted model (only typical chest pain symptoms and pain in the right arm/shoulder remained significant).
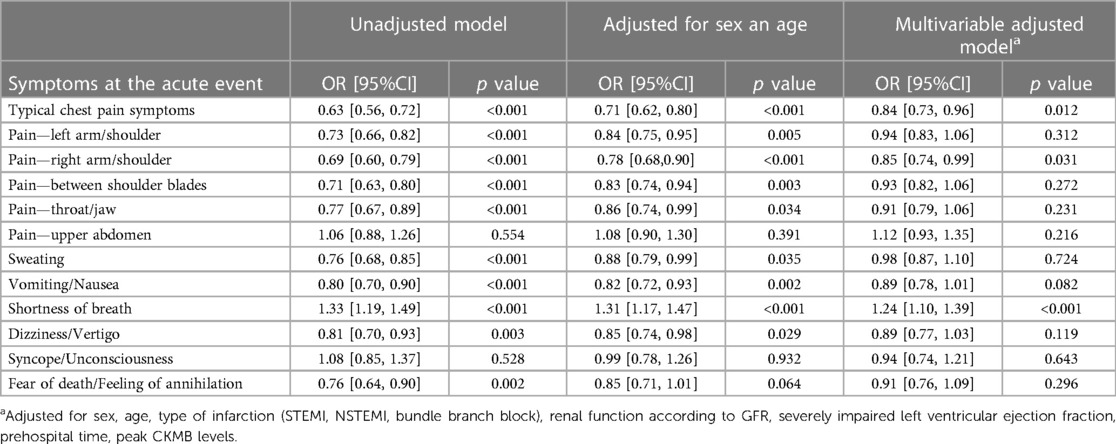
Table 3. Association between diabetes and specific symptoms at the acute event analyzed by different logistic regression models: unadjusted model (left), model adjusted for sex and age (middle) and multivariable adjusted model.
The subgroup analysis for different age groups (see Table 4) revealed that the above reported associations are largely not seen in patients below age 55 [no significant associations were found for this age group and the obtained results (point estimators/odds ratio) pointed in the opposite direction for some symptoms like shortness of breath]. In terms of a sensitivity analysis, we did the same calculations with only three age groups (<65 years, 65–79 years and ≥80 years), see Supplementary Table S1. It shows, that indeed only the very young patients <55 years differ substantially from the other age groups, since the results for the group <65 years are quite comparable to the age group 65–79 years.
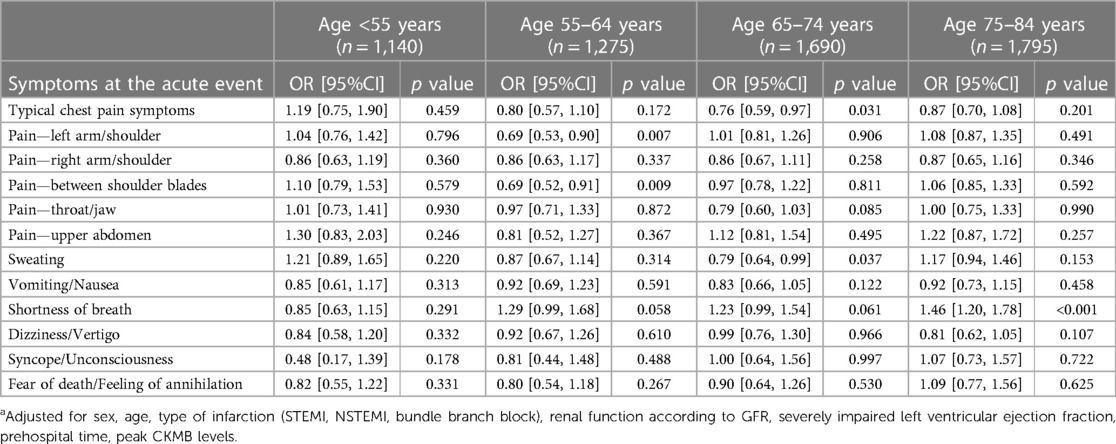
Table 4. Association between diabetes and specific symptoms at the acute event analyzed by multivariable adjusted logistic regression modelsa and stratified for different age groups.
4 Discussion
The present study shows that AMI patients with diabetes experience less often typical AMI symptoms, including the most characteristic symptom, i.e., chest pain. Only shortness of breath was reported more frequently by diabetic patients. Nevertheless, adjusting for several potential confounders the overall associations appeared to be attenuated, but remained significant for chest pain (more often in patients without diabetes) and shortness of breath (more often in patients with diabetes). Further analyses revealed, that the observed associations did not apply to younger AMI patients (age 54 and younger) with no significant associations between diabetes and specific symptoms at all.
Also prior studies have reported that diabetes goes along with less AMI symptoms including typical chest pain as well (5–10). A current review/meta-analysis specifically analyzing chest pain symptoms and diabetes came to the same conclusion (17). However, there were also studies finding no significant differences in reported AMI symptoms between patients with and without diabetes or even some atypical symptoms more frequently reported by diabetic patients (11–15). In particular, a study from Sweden (Northern Sweden MONICA Study) analyzed 4,028 patients with first myocardial infarction aged 25–74 years (14). They found no difference regarding typical symptoms between patients with and without diabetes, and diabetes was not identified as a predictor of atypical symptoms. So, this large study based on a myocardial infarction registry data came to differing results compared to the results in the present analysis. It can be speculated though, whether the different time frames of patient recruitment (between 2000 and 2006 for the Swedish study and 2010–2017 for the present study) had any influence on the results (e.g., the wide-spread use of high-sensitive troponin diagnostics led to the diagnosis of more smaller infarctions with higher frequencies of atypical symptoms).
Most studies reporting on this specific topic have not applied multivariable-adjusted regression models. So, their findings cannot be interpreted in the way that diabetes is independently associated with less or atypical AMI symptoms. And indeed, the results of the present study suggested that even though some associations remain significant, the estimated effects were considerably attenuated by the multivariable adjustment. In a sensitivity analysis we calculated a variety of different logistic regression models with varying adjusting variables. It was found, that in particular the inclusion of the variables eGFR group (representing renal function) and left ventricular ejection fraction into the regression models affected the results [attenuation of the point estimators (Odds ratio) for diabetes]. These observations are confirmed by a study from Korea which identified renal dysfunction as a major risk factor for painless AMI (18). The authors concluded, that particularly the joint occurrence of reduced GFR and diabetes mellitus went along with an increased appearance of painless AMI.
In the present study, there was a positive association between shortness of breath at acute MI and diabetes, which was the only significant positive association we found. This association remained significant in the multivariable adjusted logistic regression model for the total sample, but could not be detected in the youngest age group however. Prior studies have also indicated that patients with diabetes experience more frequently some form of shortness of breath or hyperventilation (6, 7, 11).
One major pathophysiological mechanisms underlying the observed phenomenon might be the impact of diabetic polyneuropathy as a complication of long-standing diabetes. Polyneuropathy is a micro-damage of the peripheral nerve system and caused by (chronic) hyperglycemia and altered insulin signaling (19). With up to 50% of all diabetic patients it is a very common complication and the prevalence rises with disease duration (19). Especially in diabetic patients with confirmed coronary artery disease the prevalence seems to be particularly high with a majority of those patients suffering from a polyneuropathy (19). Diabetic polyneuropathy quite frequently goes along with a decreased pain perception (19), which may be responsible for the reduced (pain) symptoms in diabetic AMI patients. However, in most cases it takes years or decades for a relevant diabetic polyneuropathy to develop. So, the diabetes diseases must preexist the acute event for quite a long time period. In fact, this would fit well into the picture that emerged when analyzing the different age groups: we found no reduced frequency of (pain) symptoms in young diabetes patients. These patients simple may be too young to have developed major complications like polyneuropathy. It may become a major issue in older age for which we found reduced frequencies of major (pain) symptoms.
We cannot explain why diabetes was strongly positively associated with shortness of breath; but again not in young patients however. Shortness of breath is a pretty unspecific symptom that cannot only occur in AMI patients as part of the typical angina pectoris symptom, but is also frequent in many other diseases like pulmonary embolism or pneumonia. It often also accompanies exceptional psychological situation like panic attacks and severe states of anxiety. With all this said, shortness of breath might also, at least in some sense, represent the patient’s current cardiovascular condition, e.g., in terms of acute heart failure with dyspnea as the leading symptom (20). Actually it has been reported that the presence of shortness of breath is associated with higher mortality after AMI (21). So it could be speculated if this particular symptom might be somehow an expression of more severe events, worse cardiovascular status and an overall worse prognosis; a condition for which diabetes is a well-known (causal) risk factor.
The results of this analysis underline the importance of thorough diagnostics in AMI-suspected patients with diabetes even without typical chest pain symptoms, which means an ECG within 10 min to rule out STEMI and serial high-sensitive Troponin testing to detect NSTEMI (22). Especially in older patients with diabetes, AMIs might be hidden under rather unspecific symptoms, like shortness of breath. The absence of typical AMI symptoms, in particular chest pain, goes along with an increased risk of delayed diagnosis and treatment (23–25), which can lead to an elevated mortality and overall worse outcomes (10, 21, 23–26). Accordingly, AMI patients with diabetes indeed have longer pre-hospital delays (13, 15, 27) and a higher mortality after the event (3, 4). Awareness of this particularity in clinical presentation is key to a fast diagnosis and subsequent treatment, which is especially important in patients with the additional risk factor diabetes mellitus.
4.1 Strengths and limitations
The present study is characterized by some major strengths. The data analyzed was collected by a population-based registry, avoiding any selection bias as best as possible. The relatively high number of patients included into this analysis provides solid statistical power. Symptoms at the acute event were assessed by a standardized questionnaire in a face-to-face interview only days after the infarction. For each patients, a variety of different information and data was collected that allowed to perform multivariable adjusted logistic regression models.
There are also some limitations. First, we have no patients older than 85 years included into this study. Likewise, no information on ethnicity was available, so the results might not be generalized to all ethnicities and age groups. Patients that were unable or unwilling to complete the interview and report their symptoms could not be considered for this study and their absence in the analyses might have affected the overall results. The interview with the AMI patients was conducted several days after admission, so fading memory might have affected the reporting of symptoms in some cases. Since there is an unneglectable number of AMI patients with undiagnosed diabetes (28), we might have misclassified some patients as non-diabetes patients. Finally, since some potentially important information (for instance on pulmonary pathologies) were missing, we might have not have considered all relevant confounders in the multivariable adjusted models.
5 Conclusion
AMI patients with diabetes have less symptoms at the acute event compared to patients without diabetes. One major exception is shortness of breath, which is significantly more often present in diabetic patients. However, the results obtained for the total sample could not be reproduced in patients younger than 55 years.
This studies demonstrates that patients with diabetes often report less symptoms at the acute event despite an overall worse prognosis. Especially the absence of typical chest pain and the presence of shortness of breath might be typical for diabetes in AMI patients aged 55+. Consequently, fast diagnostics and quick treatment appears to be essential particularly in these patients.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics committee of the Bavarian Medical Association (Bayerische Landesärztekammer). The studies were conducted in accordance with the local legislation and institutional requirements. All study participants gave written informed consent.
Author contributions
TS: Conceptualization, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft. BW: Supervision, Validation, Writing – review & editing. PR: Supervision, Validation, Writing – review & editing. MH: Data curation, Funding acquisition, Resources, Supervision, Validation, Writing – review & editing. AP: Funding acquisition, Resources, Supervision, Validation, Writing – review & editing. JL: Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing. CM: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the Helmholtz Zentrum München, German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education, Science, Research and Technology and by the State of Bavaria and the German Federal Ministry of Health. This research also received support from the Faculty of Medicine, University of Augsburg, and the University Hospital of Augsburg, Germany. Since the year 2000, the collection of MI data has been co-financed by the German Federal Ministry of Health to provide population-based MI morbidity data for the official German Health Report (see www.gbe-bund.de).
Acknowledgments
We would like to thank all members of the Helmholtz Zentrum München, Institute of Epidemiology, and the Chair of Epidemiology at the University Hospital of Augsburg, who were involved in the planning and conduct of the study. Steering partners of the Augsburg MI Registry include the Chair of Epidemiology at the University Hospital of Augsburg and the Department of Internal Medicine I, Cardiology, University Hospital of Augsburg. Many thanks for their support go to the local health departments, the office-based physicians and the clinicians of the hospitals within the study area. Finally, we express our appreciation to all study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1324451/full#supplementary-material
References
1. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
2. Cui J, Liu Y, Li Y, Xu F, Liu Y. Type 2 diabetes and myocardial infarction: recent clinical evidence and perspective. Front Cardiovasc Med. (2021) 8:644189. doi: 10.3389/fcvm.2021.644189
3. Meisinger C, Heier M, Scheidt W von, Kirchberger I, Hörmann A, Kuch B. Gender-specific short and long-term mortality in diabetic versus nondiabetic patients with incident acute myocardial infarction in the reperfusion era (the MONICA/KORA myocardial infarction registry). Am J Cardiol. (2010) 106:1680–4. doi: 10.1016/j.amjcard.2010.08.009
4. Milazzo V, Cosentino N, Genovese S, Campodonico J, Mazza M, Metrio M de, et al. Diabetes mellitus and acute myocardial infarction: impact on short and long-term mortality. Adv Exp Med Biol. (2021) 1307:153–69. doi: 10.1007/5584_2020_481
5. Berman N, Jones MM, de Coster DA. ‘Just like a normal pain’, what do people with diabetes mellitus experience when having a myocardial infarction: a qualitative study recruited from UK hospitals. BMJ open. (2017) 7:e015736. doi: 10.1136/bmjopen-2016-015736
6. DeVon HA, Penckofer S, Larimer K. The association of diabetes and older age with the absence of chest pain during acute coronary syndromes. West J Nurs Res. (2008) 30:130–44. doi: 10.1177/0193945907310241
7. DeVon HA, Penckofer SM, Zerwic JJ. Symptoms of unstable angina in patients with and without diabetes. Res Nurs Health. (2005) 28:136–43. doi: 10.1002/nur.20067
8. Culić V, Eterović D, Mirić D, Silić N. Symptom presentation of acute myocardial infarction: influence of sex, age, and risk factors. Am Heart J. (2002) 144:1012–7. doi: 10.1067/mhj.2002.125625
9. Manistamara H, Sella YO, Apriliawan S, Lukitasari M, Rohman MS. Chest pain symptoms differences between diabetes mellitus and non-diabetes mellitus patients with acute coronary syndrome: a pilot study. J Public Health Res. (2021) 10(2):2186. doi: 10.4081/jphr.2021.2186
10. Pong JZ, Ho AF, Tan TX, Zheng H, Pek PP, Sia C-H, et al. ST-segment elevation myocardial infarction with non-chest pain presentation at the emergency department: insights from the Singapore myocardial infarction registry. Intern Emerg Med. (2019) 14:989–97. doi: 10.1007/s11739-019-02122-3
11. Kentsch M, Rodemerk U, Gitt AK, Schiele R, Wienbergen H, Schubert J, et al. Angina intensity is not different in diabetic and non-diabetic patients with acute myocardial infarction. Z Kardiol. (2003) 92:817–24. doi: 10.1007/s00392-003-0965-9
12. Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Symptoms and type of symptom onset in acute coronary syndrome in relation to ST elevation, sex, age, and a history of diabetes. Am Heart J. (2005) 150:234–42. doi: 10.1016/j.ahj.2004.08.035
13. Ahmed S, Khan A, Ali SI, Saad M, Jawaid H, Islam M, et al. Differences in symptoms and presentation delay times in myocardial infarction patients with and without diabetes: a cross-sectional study in Pakistan. Indian Heart J. (2018) 70:241–5. doi: 10.1016/j.ihj.2017.07.013
14. Angerud KH, Brulin C, Näslund U, Eliasson M. Patients with diabetes are not more likely to have atypical symptoms when seeking care of a first myocardial infarction. An analysis of 4028 patients in the Northern Sweden MONICA study. Diabet Med. (2012) 29:e82–7. doi: 10.1111/j.1464-5491.2011.03561.x
15. Ängerud KH, Thylén I, Sederholm Lawesson S, Eliasson M, Näslund U, Brulin C. Symptoms and delay times during myocardial infarction in 694 patients with and without diabetes; an explorative cross-sectional study. BMC Cardiovasc Disord. (2016) 16:108. doi: 10.1186/s12872-016-0282-7
16. Löwel H, Meisinger C, Heier M, Hörmann A. The population-based acute myocardial infarction (AMI) registry of the MONICA/KORA study region of Augsburg. Gesundheitswesen. (2005) 67(Suppl 1):S31–7. doi: 10.1055/s-2005-858241
17. Kumar A, Sanghera A, Sanghera B, Mohamed T, Midgen A, Pattison S, et al. Chest pain symptoms during myocardial infarction in patients with and without diabetes: a systematic review and meta-analysis. Heart (British Cardiac Society). (2023) 109(20):1516–24. doi: 10.1136/heartjnl-2022-322289
18. Choi JS, Kim CS, Park JW, Bae EH, Ma SK, Jeong MH, et al. Renal dysfunction as a risk factor for painless myocardial infarction: results from Korea acute myocardial infarction registry. Clin Res Cardiol. (2012) 101:795–803. doi: 10.1007/s00392-012-0461-1
19. Feldman EL, Callaghan BC, Pop-Busui R, Zochodne DW, Wright DE, Bennett DL, et al. Diabetic neuropathy. Nat Rev Dis Primers. (2019) 5:42. doi: 10.1038/s41572-019-0092-1
20. Martindale JL, Wakai A, Collins SP, Levy PD, Diercks D, Hiestand BC, et al. Diagnosing acute heart failure in the emergency department: a systematic review and meta-analysis. Acad Emerg Med. (2016) 23:223–42. doi: 10.1111/acem.12878
21. Kirchberger I, Heier M, Kuch B, Scheidt Wv, Meisinger C. Presenting symptoms of myocardial infarction predict short- and long-term mortality: the MONICA/KORA myocardial infarction registry. Am Heart J. (2012) 164:856–61. doi: 10.1016/j.ahj.2012.06.026
22. Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. (2023) 44:3720–826. doi: 10.1093/eurheartj/ehad191
23. Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. (2000) 283:3223–9. doi: 10.1001/jama.283.24.3223
24. Brieger D, Eagle KA, Goodman SG, Steg PG, Budaj A, White K, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the global registry of acute coronary events. Chest. (2004) 126:461–9. doi: 10.1378/chest.126.2.461
25. Song C-X, Fu R, Yang J-G, Xu H-Y, Gao X-J, Wang C-Y, et al. Angiographic characteristics and in-hospital mortality among patients with ST-segment elevation myocardial infarction presenting without typical chest pain: an analysis of China acute myocardial infarction registry. Chin Med J. (2019) 132:2286–91. doi: 10.1097/CM9.0000000000000432
26. Fujino M, Ishihara M, Ogawa H, Nakao K, Yasuda S, Noguchi T, et al. Impact of symptom presentation on in-hospital outcomes in patients with acute myocardial infarction. J Cardiol. (2017) 70:29–34. doi: 10.1016/j.jjcc.2016.10.002
27. Ängerud KH, Brulin C, Näslund U, Eliasson M. Longer pre-hospital delay in first myocardial infarction among patients with diabetes: an analysis of 4266 patients in the Northern Sweden MONICA study. BMC Cardiovasc Disord. (2013) 13:6. doi: 10.1186/1471-2261-13-6
Keywords: myocardial infarction, acute symptoms, diabetes mellitus, atypical presentation, chest pain, shortness of breath
Citation: Schmitz T, Wein B, Raake P, Heier M, Peters A, Linseisen J and Meisinger C (2024) Do patients with diabetes with new onset acute myocardial infarction present with different symptoms than non-diabetic patients?. Front. Cardiovasc. Med. 11:1324451. doi: 10.3389/fcvm.2024.1324451
Received: 19 October 2023; Accepted: 3 January 2024;
Published: 15 January 2024.
Edited by:
Neftali Eduardo Antonio-Villa, National Institute of Cardiology Ignacio Chavez, MexicoReviewed by:
Alexandru Scafa Udriste, Carol Davila University of Medicine and Pharmacy, RomaniaDejan Orlic, University of Belgrade, Serbia
© 2024 Schmitz, Wein, Raake, Heier, Peters, Linseisen and Meisinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Timo Schmitz dGltby5zY2htaXR6QG1lZC51bmktYXVnc2J1cmcuZGU=
 Timo Schmitz
Timo Schmitz Bastian Wein2
Bastian Wein2 Jakob Linseisen
Jakob Linseisen Christa Meisinger
Christa Meisinger