
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cardiovasc. Med. , 28 February 2024
Sec. Hypertension
Volume 11 - 2024 | https://doi.org/10.3389/fcvm.2024.1300319
This article is part of the Research Topic Exploring the Role of Exercise in Hypertension and Blood Pressure Variability View all 4 articles
 Qingyuan Zhang1,2,†
Qingyuan Zhang1,2,† Xiaogang Xu1,†
Xiaogang Xu1,† Qianyan Wu1
Qianyan Wu1 Jingwen Zhang1
Jingwen Zhang1 Shenghe Huang1
Shenghe Huang1 Lin Wu1
Lin Wu1 Minping Tian3
Minping Tian3 Delin Zhang1,4*
Delin Zhang1,4*
Background: As a therapy to prevent and treat essential hypertension (EH), traditional Chinese exercises (TCEs) were widely used in clinical practice. However, there is a lack of strictly comparison of the antihypertensive efficacy of different TCEs, which not conducive to the selection of the best and most optimal treatment. This study aimed to perform a network meta-analysis to objectively evaluate which TCE has the best effects in assisting with lowering blood pressure.
Methods: PubMed, Embase, the Cochrane Library, Chinese National Knowledge Infrastructure (CNKI), VIP, SinoMed and Wanfang Data were searched for all randomized controlled trials (RCTs) on TCEs for the treatment of EH published up to July 10, 2023. RoB2.0 tool was utilized to evaluate the quality of the RCTs. The network meta-analysis was performed by R 4.1.2 and Stata 17.0. Weighted mean difference (WMD) was calculated for continuous outcomes.
Results: A total of 29 studies, including 2,268 patients were included to analyze 6 different interventions. The network meta-analysis results presented that in comparison with control group, Tai Chi + antihypertensive medication [WMD = −10.18, 95% CI, (−14.94, −5.44)] is the most effective intervention for lowering systolic blood pressure (SBP), and Wuqinxi + antihypertensive medication [WMD = −10.36, 95% CI (−18.98, −1.66)] is the most effective intervention for lowering diastolic blood pressure (DBP).
Conclusion: TCEs combined with antihypertensive medication may be able to achieve more prominent antihypertensive effects with Tai Chi and Wuqinxi potentially being the higher-priority options. However, well-designed randomized studies are warranted to further verify currently conclusion.
Hypertension is a clinical syndrome characterized by increased systemic arterial pressure and increased peripheral arteriolar resistance. According to epidemiological investigation, the number of people aged 30–79 years with hypertension doubled from 1990 to 2019, and the number of people with hypertension is expected to reach 1.56 billion (1.54–1.58 billion) worldwide by 2025 (1, 2). As compared with healthy people, the risk of cardiovascular and cerebrovascular diseases in hypertensive patients is considerably greater (3, 4). Anti-hypertension medication still serves as a major therapy choice for treating hypertension now. However, due to medication side effects, treatment resistance as well as economic factors, an extensive number of patients still have hypertension that cannot be successfully controlled (5, 6). Therefore, it is essential to further explore a widely available, low-cost and sustainable treatment method (7).
Traditional Chinese exercises (TCEs) are an aerobic exercise therapy that focuses on regulating breathing and controlling the mind (8), which mainly includes Tai Chi (TC), Baduanjin (BDJ), Liuzijue (LZJ) and Wuqinxi (WQX). Presently, the total number of people practicing TCEs worldwide has surpassed 6.5 million across 56 countries or regions (9). Due to their ease of adoption, widespread availability, and affordability, TCEs have been utilized as an adjunct therapy in treating various cardiovascular and cerebrovascular diseases in China (10–13). Several systematic reviews and meta-analysis have evaluated the efficacy of TCEs in the treatment of hypertension (14–16). However, their conclusions are all based on a pairwise meta-analysis which is limited in the fact that they can only compare the efficacy of paired interventions. In addition, some kinds of TCEs (Liuzijue, Wuqinxi) were neglected and not included in the evaluation, which not conducive to the selection of the best and most optimal treatment. Therefore, a systematic and comprehensive study is urgently required to effectively compare and rank the antihypertensive effects of the different TCEs.
Different from the traditional meta-analysis, network meta-analysis (NMA) can efficiently compare up to three or more interventions at the same time (17), which allows the investigators to compare and rank the effectiveness of multiple interventions directly or indirectly (18, 19). This study aims to utilized Bayesian network meta-analysis method, which accounts for both direct and indirect comparisons to provide valid evidence supporting the application of TCEs for EH.
This network meta-analysis was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis 2020 (PRISMA 2020) (20), and the PRISMA checklist can be located in Supplementary Material S1. The protocol of this review was registered in International prospective register of systematic reviews (PROSPERO) under registration number CRD42023438688.
A combination of manual and computer retrieval methods was utilized and the retrieval databases include CNKI, Wanfang Data, VIP, SinoMed, PubMed, Cochrane Library, and Embase. The search was for randomized controlled trials (RCTs) of different TCEs for the treatment of EH. The last retrieval date was July 10, 2023, and all relevant retrieval strategies of the database were listed in Supplementary Material S2.
The inclusion criteria for this study was strictly adhered to the PICOS framework, and the inclusion criteria are as follows: (1) Type of study: published randomized controlled trials (RCTs) for the treatment of essential hypertension; (2) Patients: patients that were diagnosed with essential hypertension with systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg; (3) Interventions: the treatment group received TCEs combined with conventional antihypertensive medication; (4) Comparison: the control group received conventional antihypertensive medication or conventional antihypertensive medication combined with aerobic exercise; (5) Outcomes: changes in SBP and DBP after treatment (blood pressure change = prior treatment blood pressure value−post-treatment blood pressure value).
The exclusion criteria are as follows: (1) The patients were diagnosed with secondary hypertension; (2) Duplicated publications; (3) Studies that failed to reported the baseline which results in an inability to calculate changes in SBP and DBP after treatment; (4) Studies that only reported antihypertensive efficiency rate but failed to provide specific numerical values.
EndNote X9 was used to complete the selection process of the studies. Firstly, removed the duplicates. Subsequently, two reviewers (WQY and HSH) independently read through the titles, abstracts as well as full texts meticulously. At the same time, the reviewers strictly adhered to the inclusion criteria and exclusion criteria to screening the literature. If the event when a disagreement occurred between the two reviewers, we would refer to the views of the third researcher (WL).
After the screening process, the data for final inclusion in the literature were extracted by two reviewers (WL and TMP) using a pre-designed data extraction form that consists of the following: (1) Basic information of literature that includes the title, first author, corresponding author, year, intervention, comparison, as well as the methods of random sequence generation and allocation concealment; (2) Basic information of the patients which includes the gender and age; (3) Information of intervention which includes the intensity, frequency, and duration; (4) SBP and DBP values before and after treatment. Lastly, any disagreement that arose in the data extraction process shall be resolved through a team discussion.
The risk of bias for the included trials was independently evaluated by the two researchers (ZQY and XXG) using the Revised Cochrane Risk of Bias Tool (RoB 2.0) (21). The evaluation contents predominantly include (1) randomization process; (2) deviations from intended interventions; (3) missing outcome data; (4) measurement of the outcome; (5) selection of the reported result. To assess the risk of bias within each domain, one or more signaling questions were answered, which generally contain five alternative answers: (1) yes; (2) probably yes; (3) no information; (4) probably no; (5) no. Based on reviewers' responses to the signal questions, the risk of bias for each domain can be rated on three levels, respectively as low risk of bias, some concerns and high risk of bias. Subsequently, judgments within each domain contributed to an overall risk of bias assessment per study. Any discrepancy in the assessment of RoB2 would be discussed to reach a consensus.
The systolic and diastolic blood pressures are the outcomes in this study. The difference between the baseline and endpoint of systolic and diastolic blood pressures were calculated and included in the analysis in order to determine the best and most optimal treatment for hypertension more accurately and intuitively. The calculation formula is as follows (22):
The included data were presented as the weighted mean difference (WMD) with a 95% confidence interval (CI). The network evidence plots were generated utilizing Stata17.0 software. Bayesian random-effects Network Meta-Analysis (NMA) for all outcomes was performed using R4.1.2 with the gemtc package (23, 24). The initial setup included four Markov chains, a step size of 1, 20,000 pre-iterations for burn-in, and 50,000 iterations to achieve convergence. Following iterations for convergence, a PSRF nearing 1indicated satisfactory model convergence; otherwise, iterations were extended. When there was a closed loop, the node splitting method was utilized to test the local inconsistency, and it was judged that the consistency was good and favorable when P > 0.05 (25). Stata17.0 software was employed to generate surface under the cumulative ranking curve (SUCRA) plots for effective intervention ranking and comparison-adjusted funnel plots. Begg's test was conducted using R4.1.2 with the netmeta package. Subsequently, by combining funnel plots with Begg's test, we examined whether there was publication bias in the NMA. Finally, the I2 statistic assessed heterogeneity, the robustness of the results of this study were assessed by including treatment duration as a covariate to conduct a meta-regression analysis.
For each outcome, the quality of evidence across the network was assessed using the Confidence in Network Meta-Analysis (CINeMA) framework that is based on the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach (26, 27). The evaluation contents included within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. In the CINeMA framework, the confidence rating is an overall qualitative assessment that summarizes judgment across the 6 domains which assess the quality of evidence. Similarly, being identical to the GRADE framework, confidence can be classified as high, moderate, low, or very low (28).
A total of 3,676 articles were initially identified. Subsequently, through meticulous reading and screening of each respective records, 29 studies (29–57) were eventually included in the network meta-analysis, and no additional studies were identified by screening the reference lists of the relevant reviews and selected studies. The process of inclusion and exclusion was presented in Figure 1.
A total of 2,268 patients with 1,155 in the treatment group and 1,133 in the control group in the included 29 clinical studies completed the trial. The shortest course of treatment in treatment group for TCEs was 8 weeks, and the longest course of treatment was 6 months. At the same time, the most common practice frequency was 1–2 times/day, and the duration of a single practice was mostly maintained at 30–60 min. The basic characteristics of included patients and studies were listed in the Supplementary Material S3.
In terms of the randomization process, two studies (49, 56) detailed reported the methods of randomized grouping and used the sealed opaque containers to conceal the allocation. Meanwhile, there was no observed differences between intervention groups at baseline, so these studies were assessed as low risk of bias, and the remaining studies were assessed as moderate risk of bias cause they did not indicate whether allocation concealment was performed or failed to report the specific method of randomization. In terms of deviations from intended interventions, all studies presented a moderate risk of bias due to the peculiarity of the interventions made it difficult to perfectly perform blinding to patients and carers. In terms of missing outcome data, all studies were assessed as low risk of bias due to the absence of significant withdrawal as well as the adoption of appropriate data analysis methods. In terms of outcome measurement, two studies (49, 56) were assessed as low risk of bias due to the application of appropriate outcome assessment methods and blinded the outcome assessors, while the remaining studies were assessed as moderate risk of bias. As all studies were unable to attain their trial protocols, the risks for selective reporting were all assessed as moderate risks of bias. Lastly, for the overall risk of bias, all studies were assessed as moderate risk of bias. The detail of the assessment was showed in Figure 2.
A total of 29 studies (29–57) with 6 interventions were included in the network meta-analysis. The network plots were presented in Figure 3. The inconsistency test demonstrated that the deviance information criterion (DIC) difference between the consistent model and the inconsistent model was less than 5 which indicates good consistency. Therefore, the consistent model was selected for the network meta-analysis.
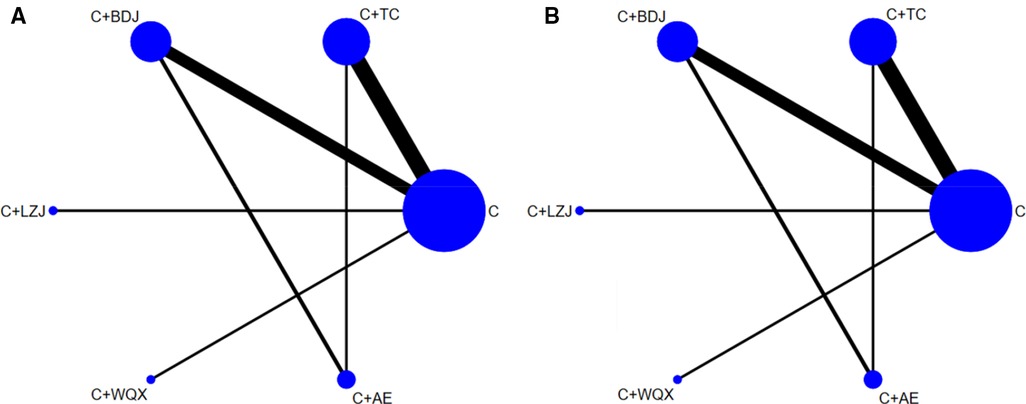
Figure 3. (A) The network plot of systolic blood pressure; (B) the network plot of diastolic blood pressure. C, conventional antihypertensive medication; TC, Tai Chi; BDJ, Baduanjin; LZJ, Liuzijue; WQX, Wuqinxi; AE, aerobic exercise.
A total of 29 studies (29–57) reported the results of the SBP. The network meta-analysis presented that conventional antihypertensive medication + Tai Chi [WMD = −10.18, 95% CI, (−14.94, −5.44)], conventional antihypertensive medication + Baduanjin [WMD = −7.61, 95% CI (−12.88, −2.31)] were significantly better as compared to use conventional antihypertensive medication alone in improving SBP. However, there was no statistical significance observed between the other interventions as presented in the Table 1, and the heterogeneity test between the studies was showed in Supplementary Material S4.
A total of 29 studies (29–57) reported the results of the DBP. The results of the network meta-analysis presented that compared to conventional antihypertensive medication, conventional antihypertensive medication + Tai Chi [WMD = −5.99, 95% CI (−9.39, −2.57)], conventional antihypertensive medication + Baduanjin [WMD = −6.93, 95% CI (−10.79, −3.04)] and conventional antihypertensive medication + Wuqinxi [WMD = −10.36, 95% CI (−18.98, −1.66)] were significantly better in lowering DBP. Lastly, there was no statistical difference observed between the other treatments as presented in the Table 2, and the heterogeneity test between the studies was showed in Supplementary Material S4.
We ranked all the interventions involved according to the results calculated by SUCRA. The therapeutic effect of different interventions in lowering SBP is in descending order as follows: C + TC > C + WQX > C + BDJ > C + LZJ > C + C + AE > C, as shown in Figure 4A. Correspondingly, the therapeutic effect of different interventions in lowering DBP is in descending order as follows: C + WQX > C + LZJ > C + BDJ > C + TC > C + AE > C, as shown in Figure 4B.
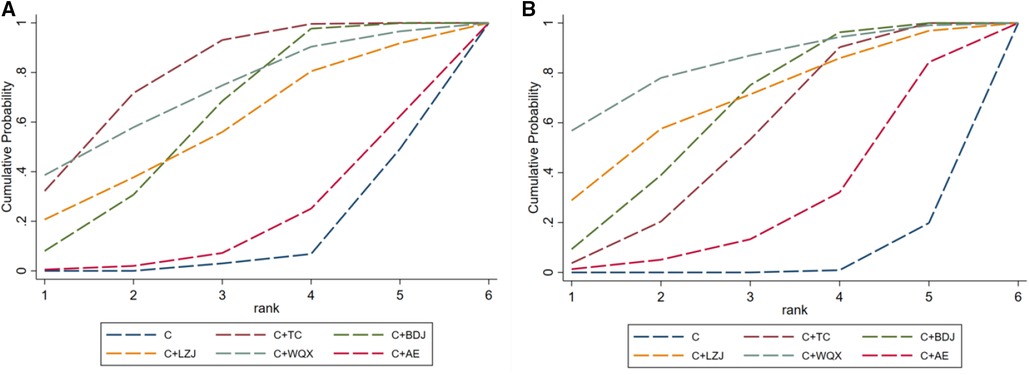
Figure 4. (A) The probability ranking of different TCEs in lowering SBP; (B) the probability ranking of different TCEs in lowering DBP. C, conventional antihypertensive medication; TC, Tai Chi; BDJ, Baduanjin; LZJ, Liuzijue; WQX, Wuqinxi; AE, aerobic exercise.
Considering the variations in the duration and frequency of exercises among the included studies, we performed a meta-regression analysis to assess their potential impact on the antihypertensive effect. The results of the meta-regression analysis indicated that beyond an 8-week period of TCEs, the duration of treatment might not be the primary factor influencing the therapeutic effect. However, the varying frequency of TCEs may affect the antihypertensive effect. The results of the meta-regression were listed in the Supplementary Material S5.
A total of 15 treatment comparisons were evaluated, the confidence ratings of the treatment comparisons were judged as rated as very low to moderate. The main reasons for downgrading including within-study bias, indirectness and heterogeneity. The details of evidence assessment were presented in the Supplementary Material S6.
After a thorough and meticulous review of the included articles, one study (32) evaluated on its safeness and it is reported to exhibit zero adverse events.
The evidence network plots of SBP and DBP both have closed loops. Therefore, a local inconsistency test was required. The results of node splitting portrayed that there was no significant difference between the direct and indirect comparisons of the network meta-analysis for systolic and diastolic blood pressure (P > 0.05), indicating that the consistency is good. The diagnostic results of convergence showed that the model test of all network meta-analyses was 1.00 ≤ PSRF ≤ 1.05, and the analysis results were reliable. The results of inconsistency test and convergence analysis can be located in the Supplementary Material S7.
The comparison-adjusted funnel plots showed that all the studies were basically distributed on both sides of the midline, as shown in Figure 5. While Begg's test (P = 0.4531 for SBP, P = 0.5994 for DBP) indicated no observable publication bias (Supplementary Material S8). From the results, it could be considered that there was no significant publication bias.
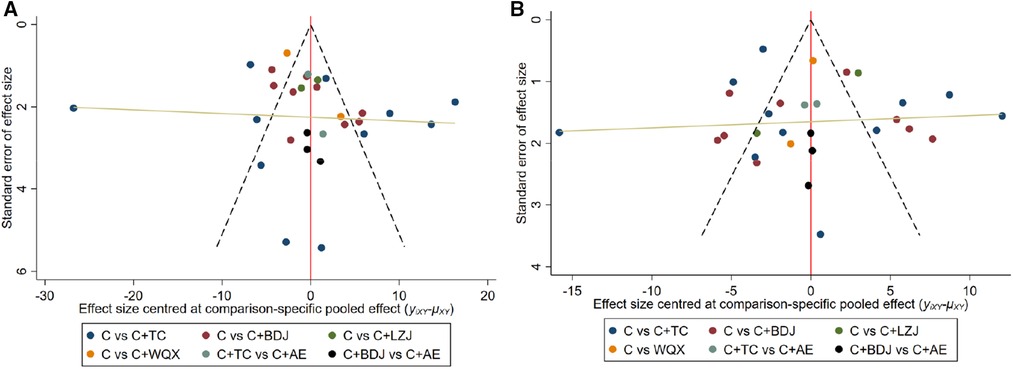
Figure 5. (A) Bias specific pooled effect for SBP; (B) bias specific pooled effect for DBP. C, conventional antihypertensive medication; TC, Tai Chi; BDJ, Baduanjin; LZJ, Liuzijue; WQX, Wuqinxi; AE, aerobic exercise.
Large-scale epidemiological studies have provided definitive evidence that high blood pressure maintains a continuous graded association with the risk of fatal and nonfatal stroke, ischemic heart disease, heart failure, and noncardiac vascular disease (58, 59). Although regular aerobic exercise can lower blood pressure, due to the high physical fitness requirements of aerobic exercise, most adults with hypertension are unwilling or unable to exercise. Therefore, many alternative therapies for aerobic exercise, such as Tai Chi, Baduanjin, Wuqinxi and Liuzijue (60–62), have been widely recommended in clinical practice and proved to be effective. The purpose of this study was to compare which TCE possesses the best effects on essential hypertension. In this network meta-analysis, we included 29 studies that involved 2,268 participants and compared the antihypertensive effects of 6 interventions. Our results showed that in lowering blood pressure, C + TC, C + WQX, C + BDJ, C + LZJ, C + AE resulted in better outcomes for patients with essential hypertension compared with the C group. Based on the probability ranking, it is clear that C + TC is the most effective intervention for improve SBP. Regarding the improvement of DBP, C + WQX is the most effective intervention.
Tai Chi is not solely aerobic; it also encompasses muscle-strengthening elements, especially for the quadriceps. Research has demonstrated that Tai Chi results in significant improvements in handgrip strength, functional capacity, postural balance, and thoracolumbar spine flexibility (63). During Tai Chi practice, subjects in a meditative state try to shift their weight slowly from side to side while concurrently concentrating and visualizing each movement sequence. This process aids in efficient muscle utilization, enhancing circulation, and regulating the autonomic control of blood pressure (64). Wuqinxi is a traditional Chinese health practice attributed to Hua Tuo, a renowned ancient Chinese physician. It involves a series of bio-mimetic techniques emulating the movements of tigers, deer, bears, apes, and birds. Similar to Tai Chi, during Wuqinxi practice, attaining a state of mind and body that is “relaxed, tranquil, natural, and harmonious internally and externally” is essential (65). These attributes potentially contribute to the effectiveness of both Tai Chi and Wuqinxi in lowering blood pressure.
In our NMA, we found high heterogeneity in some directly pairwise comparison (C VS C + TC and C VS C + BDJ), considering that the therapeutic effect of TCEs may be related to the course or frequency of treatment (66), we conducted a meta-regression analysis to explore the potential impact of these two covariates. The meta-regression results showed that while the duration of treatment might not be the primary factor influencing the therapeutic effect, the varying frequency of TCEs may affect the antihypertensive effect. Due to the limitations of the number of included articles and the quality of the study, the meta-regression results should not be interpreted excessively. Although duration of treatment might not be the primary factor influencing the therapeutic effect, we still recommend that in future clinical applications, more comprehensive consideration should be given to the duration of individual sessions and the total duration of treatment in order to avoid the situation where a favorable effect cannot be successfully attained due to a short exercise time or that the physical strength and exercise enthusiasm of patients are affected by a pro-long exercise duration. Moreover, the frequency of exercises and duration of single exercise sessions has also varied considerably in clinical design among studies. Taking all these factors into account, the certainty of evidence was rated as ranging from very low to moderate due to methodological deficiencies and imprecision among studies, but this review presents an updated overview of different TCEs for essential hypertension.
Although the mechanism of TCEs in treating hypertension is not clear, the increase in endogenous nitric oxide (NO) production and the decrease in endothelin-1 (ET-1) in plasma after TCEs therapy may be one of the main biological mechanisms of TCEs in treating essential hypertension (36). As a potent vasodilator factor, NO can induce vasodilation, improve microvascular reactivity, and increase blood perfusion. Therefore, through the intervention by TCEs, the blood flow in patients was redistributed, and the blood flow in the skeletal muscle and myocardium will be increased correspondingly, and this will lead to an increase in shear stress. Simultaneously, the increase of vascular shear stress will also stimulate the release of NO from the blood vessels and stimulate the activity of nitric oxide synthase at the same time. In this case, it will further promote the production of NO to increase, thus achieving the aim of relaxing blood vessels and lowering blood pressure (56, 67, 68). In contrast to NO, ET-1 is a powerful vasoconstrictor, it affects salt and water homeostasis by affecting the renin-angiotensin-aldosterone system and vasopressin, thereby increasing blood pressure (69). Animal study showed that appropriate physical activity will reduce the ET levels, while excessive exercise will increase plasma ET levels correspondingly (70), as a mind-body exercise, TCEs have an appropriate amount of physical activity. Therefore, after the intervention of TCEs, the hypertension of patients is controlled correspondingly under the combination of increased NO production and decreased ET-1 content. Furthermore, as TCEs belong to a type of aerobic exercise that is guided by the mind, patients will be able to effectively relieve tensions and promote aerobic metabolism of the whole body through long-term practice. By acting on the cerebral cortex and vasomotor center, TCEs will be able to regulate the body's functional state, increases the tension of the vagus nerve, decreases the excitability of the sympathetic nerve, promotes vasorelaxation, and contributes to a significant role in lowering blood pressure by reducing peripheral vascular resistance (71, 72).
Compared to previous study (73), we have the following advantages. First, we registered the protocol before our work began and we used explicit inclusion and exclusion criteria to ensure the similarity between included studies which reduced the risk of bias of this NMA. Second, we firstly provided the evidence of Liuzijue in the treatment of EH. Third, we used the CINeMA tool to evaluate the certainty of evidence and provided the level of evidence for each comparison. Finally, according to the nodal split model, it is clear that there is no significant difference between direct or indirect comparisons for each split node (P > 0.05), while the diagnostic plots for each outcome showed that the median and 97.5% values of the contraction factor converge to 1, which indicates that our findings are stable and reliable.
Our study was not without its limitations. First, all included studies had moderate bias risks. Second, the differences in sample size, baseline, frequency of practice and age of the patients inevitably contributed to existence of clinical heterogeneity. Third, since there are relatively few clinical studies that use Wuqinxi or Liuzijue as interventions, there may be a small sample size effect which may exaggerate their therapeutic effect. Finally, most of the evidence provided in this study is based on indirect comparisons, more direct comparative evidence a required in the future to verify the current conclusions.
In summary, TCEs combined with antihypertensive medication may be able to achieve more prominent antihypertensive effects with Tai Chi and Wuqinxi potentially being the higher-priority options. However, it should be highlighted that, because of the low level of evidence of most of the included studies we cannot make any strong suggestions, until more well-designed randomized studies with large sample sizes are conducted.
QZ: Methodology, Software, Writing – original draft. XX: Methodology, Writing – original draft. QW: Investigation, Writing – review & editing. JZ: Conceptualization, Writing – review & editing. SH: Investigation, Writing – review & editing. LW: Data curation, Writing – review & editing. MT: Data curation, Writing – review & editing. DZ: Conceptualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was supported by the Jiangxi University of Chinese Medicine Science and Technology Innovation Team Development Program (No. CXTD22016), State Administration of Traditional Chinese Medicine Chinese Medicine Ancient Books and Characteristic Technology Inheritance Special Project (No. GZY-KJS-2021-034), Science and Technology Research Project of Jiangxi Provincial Department of Education (No. GJJ190639).
The funder had no role in study design, data collection, analysis, decision to publish, or the preparation of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1300319/full#supplementary-material
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398(10304):957–80. doi: 10.1016/s0140-6736(21)01330-1
2. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. (2005) 365(9455):217–23. doi: 10.1016/s0140-6736(05)17741-1
3. Redon J, Tellez-Plaza M, Orozco-Beltran D, Gil-Guillen V, Pita Fernandez S, Navarro-Pérez J, et al. Impact of hypertension on mortality and cardiovascular disease burden in patients with cardiovascular risk factors from a general practice setting: the ESCARVAL-risk study. J Hypertens. (2016) 34(6):1075–83. doi: 10.1097/hjh.0000000000000930
4. Gupta AK, McGlone M, Greenway FL, Johnson WD. Prehypertension in disease-free adults: a marker for an adverse cardiometabolic risk profile. Hypertens Res. (2010) 33(9):905–10. doi: 10.1038/hr.2010.91
5. Reinhart M, Puil L, Salzwedel DM, Wright JM. First-line diuretics versus other classes of antihypertensive drugs for hypertension. Cochrane Database Syst Rev. (2023) 7(7):Cd008161. doi: 10.1002/14651858.CD008161.pub3
6. Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. (2007) 370(9587):591–603. doi: 10.1016/s0140-6736(07)61299-9
7. Kostova D, Spencer G, Moran AE, Cobb LK, Husain MJ, Datta BK, et al. The cost-effectiveness of hypertension management in low-income and middle-income countries: a review. BMJ Glob Health. (2020) 5(9):e002213. doi: 10.1136/bmjgh-2019-002213
8. Pölönen P, Lappi O, Tervaniemi M. Effect of meditative movement on affect and flow in qigong practitioners. Front Psychol. (2019) 10:2375. doi: 10.3389/fpsyg.2019.02375
9. Song Y, Xia X, Guo Z. Strategy of fitness qigong integrating into and promoting the development of health service industry in China. J Shanghai University Sport. (2020) 44(04):84–94. doi: 10.16099/j.sus.2020.04.010
10. Mao S, Zhang X, Chen M, Wang C, Chen Q, Guo L, et al. Beneficial effects of baduanjin exercise on left ventricular remodelling in patients after acute myocardial infarction: an exploratory clinical trial and proteomic analysis. Cardiovasc Drugs Ther. (2021) 35(1):21–32. doi: 10.1007/s10557-020-07047-0
11. Liang C, Gao C, Zhang J, Ye Q, Zhai L, Zhao F, et al. Traditional Chinese medicine training for cardiac rehabilitation: a randomized comparison with aerobic and resistance training. Coron Artery Dis. (2019) 30(5):360–6. doi: 10.1097/mca.0000000000000734
12. Salmoirago-Blotcher E, Wayne PM, Dunsiger S, Krol J, Breault C, Bock BC, et al. Tai Chi is a promising exercise option for patients with coronary heart disease declining cardiac rehabilitation. J Am Heart Assoc. (2017) 6(10):e006603. doi: 10.1161/jaha.117.006603
13. Wang J, Li G, Ding S, Yu L, Wang Y, Qiao L, et al. Liuzijue qigong versus traditional breathing training for patients with post-stroke dysarthria complicated by abnormal respiratory control: results of a single-center randomized controlled trial. Clin Rehabil. (2021) 35(7):999–1010. doi: 10.1177/0269215521992473
14. Shao BY, Zhang XT, Vernooij RWM, Lv QY, Hou YY, Bao Q, et al. The effectiveness of Baduanjin exercise for hypertension: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med Ther. (2020) 20(1):304. doi: 10.1186/s12906-020-03098-w
15. Liang H, Luo S, Chen X, Lu Y, Liu Z, Wei L. Effects of Tai Chi exercise on cardiovascular disease risk factors and quality of life in adults with essential hypertension: a meta-analysis. Heart Lung. (2020) 49(4):353–63. doi: 10.1016/j.hrtlng.2020.02.041
16. Xiong X, Wang P, Li S, Zhang Y, Li X. Effect of Baduanjin exercise for hypertension: a systematic review and meta-analysis of randomized controlled trials. Maturitas. (2015) 80(4):370–8. doi: 10.1016/j.maturitas.2015.01.002
17. Riley RD, Jackson D, Salanti G, Burke DL, Price M, Kirkham J, et al. Multivariate and network meta-analysis of multiple outcomes and multiple treatments: rationale, concepts, and examples. Br Med J. (2017) 58:j3932. doi: 10.1136/bmj.j3932
18. Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods. (2012) 3(2):80–97. doi: 10.1002/jrsm.1037
19. Mills EJ, Ioannidis JP, Thorlund K, Schünemann HJ, Puhan MA, Guyatt GH. How to use an article reporting a multiple treatment comparison meta-analysis. JAMA. (2012) 308(12):1246–53. doi: 10.1001/2012.jama.11228
20. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
21. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. doi: 10.1136/bmj.l4898
22. Zhou X, Cao Q, Orfila C, Zhao J, Zhang L. Systematic review and meta-analysis on the effects of astaxanthin on human skin ageing. Nutrients. (2021) 13(9):2917. doi: 10.3390/nu13092917
23. Madden LV, Piepho HP, Paul PA. Statistical models and methods for network meta-analysis. Phytopathology. (2016) 106(8):792–806. doi: 10.1094/phyto-12-15-0342-rvw
24. Neupane B, Richer D, Bonner AJ, Kibret T, Beyene J. Network meta-analysis using R: a review of currently available automated packages. PLoS One. (2014) 9(12):e115065. doi: 10.1371/journal.pone.0115065
25. van Valkenhoef G, Dias S, Ades AE, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. (2016) 7(1):80–93. doi: 10.1002/jrsm.1167
26. Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. (2020) 17(4):e1003082. doi: 10.1371/journal.pmed.1003082
27. Chaimani A, Salanti G. Using network meta-analysis to evaluate the existence of small-study effects in a network of interventions. Res Synth Methods. (2012) 3(2):161–76. doi: 10.1002/jrsm.57
28. Gupta AK, Venkataraman M, Talukder M, Bamimore MA. Relative efficacy of minoxidil and the 5-α reductase inhibitors in androgenetic alopecia treatment of male patients: a network meta-analysis. JAMA Dermatol. (2022) 158(3):266–74. doi: 10.1001/jamadermatol.2021.5743
29. Xu H. Effect of 24-type simplified Tai Ji on blood pressure and quality of life in patients with hypertension. Hubei J Tradit Chin Med. (2016) 38(07):38–9.
30. Wang XB, Ye LP. Effect of 24-type simplified Tai Ji on primary hypertension with mild anxiety in the elderly. Fujian J Tradit Chin Med. (2019) 50(04):73–5. doi: 10.13260/j.cnki.jfjtcm.011881
31. Jiang YH, Fu GL, Wang QP, Bao XP, Liu XX. Effect of Baduanjin on aged patients with hypertension and anxiety of liver yang hyperactivity syndrome. J Qilu Nur. (2019) 25(19):104–6. doi: 10.3969/j.issn.1006-7256.2019.19.037
32. Zheng LW, Fan WY, Zhou LY, Chen F, Rao YL, Fang XH. Effect of Baduanjin in elderly hypertensive patients with frailty. J Nur Sci. (2021) 36(24):90–93+97.
33. Wang F, Wang H. A random controlled trial of Baduanjin combined with antihypertensive drugs in the treatment of I-grade hyperactivity of liver yang in hypertension. Spec Health. (2021) 35:103–4.
34. Bai Y, Li XY, Xu WJ, Wei QY. Efficacy of Baduanjin combined with diltiazem hydrochloride sustained-release capsule in the treatment of grade Ⅰ-Ⅱ primary hypertension. Chin J Convalescent Med. (2020) 29(01):46–7. doi: 10.13517/j.cnki.ccm.2020.01.018
35. Fan WY, Zheng LW, Chen F, Zhou LY, Rao YL, Fang XH. Effect of Baduanjin exercise on anxiety and depression in 38 elderly patients with essential hypertension. Fujian J Tradit Chin Med. (2021) 52(02):11–3. doi: 10.13260/j.cnki.jfjtcm.012171
36. Zheng LW, Chen QY, Chen F, Mei LJ, Zheng JX. The influence of Baduanjin exercise on vascular endothelium function in old patients with hypertension grade 1. Chin J Rehabil Med. (2014) 29(03):223–7. doi: 10.3969/j.issn.1001-1242.2014.03.006
37. Chen LH. Application of Baduanjin in rehabilitation nursing of elderly patients with hypertension. J Front Med. (2016) 6(22):340–1.
38. Tang QH. Effects of traditional sports on the clinical symptom of aged intellectual patients with essential hypertension. J Beijing Sport University. (2009) 32(02):67–9. doi: 10.19582/j.cnki.11-3785/g8.2009.02.017
39. Lin Q, Yan XH. Promoting effect of body-building Baduanjin on rehabilitation of elderly patients with hypertension. Chin J Gerontol. (2017) 37(12):3024–6. doi: 10.3969/j.issn.1005-9202.2017.12.075
40. Dong DG, Yu ZD, Yu ZS. Effects of fitness Qigong Baduanjin on phlegm-dampness hypertension. Chin J Appl Physiol. (2020) 36(02):157–60. doi: 10.12047/j.cjap.5924.2020.035
41. Yang G. Effect of health Qigong·six-character formula on essential hypertension for liver-fire hyperactivity syndrome. (Dissertation/master’s thesis) Henan University of Chinese Medicine, Henan (2017).
42. Liu J. Study on intervention of essential hypertension group by Tai Chi combined with health management. Guiding J Tradit Chin Med Pharmacy. (2017) 23(05):64–6. doi: 10.13862/j.cnki.cn43-1446/r.2017.05.021
43. Luo H. Clinical study on primary hypertension treated with Tai Ji combined with medication. Chin Med Herald. (2006) 33:43–4. doi: 10.3969/j.issn.1673-7210.2006.33.019
44. Liu T, Huang QD, Liu WZ. Effect of Tai Ji on blood pressure, hemorheology and long-term quality of life in elderly patients with hypertension. Chin J Gerontol. (2018) 38(06):1396–8. doi: 10.3969/j.issn.1005-9202.2018.06.050
45. Feng LJ, Guan L, Zhang DL, Lin ZC, Li MX, Jin RJ. Clinical effect of 24-simpilified Taijiquan exercise on the antihypertensive effect of elderly patients with essential hypertension and on their blood lipid level. Chin J Convalescent Med. (2018) 27(10):1009–13. doi: 10.13517/j.cnki.ccm.2018.10.001
46. Yang H, Zhao YN, Li JM. Effect of Baduanjin exercise on autonomic nerve reaction in patients with hypertension. Chin J Coal Industry Med. (2014) 17(07):1143–6. doi: 10.11723/mtgyyx.1007-9564.201407038
47. Chen H, Zhou YN. Effect of Baduanjin on blood pressure and serum high-sensitivity C-reactive protein in patients with essential hypertension. Chin J Rehabil Med. (2012) 27(02):178–9. doi: 10.3969/j.issn.1001-1242.2012.02.023
48. Liang YH, Liao SQ, Han CL, Wang H, Peng Y. Effect of Baduanjin exercise intervention on blood pressure and blood lipid in patients with essential hypertension. Henan Tradit Chin Med. (2014) 34(12):2380–1. doi: 10.16367/j.issn.1003-5028.2014.12.102
49. Yang XW. The effect of tai chi on sleep quality in elderly patients with essential hypertension. (Dissertation/master’s thesis). Chengdu University of Traditional Chinese Medicine, Chengdu (2018).
50. Zhang XD, Deng B, Peng ZJ. Clinical observation on liuzjue adjusting breath method in the treatment of hypertension complicated with anxiety and depression. Chin Med Modern Distance Educ Chin. (2022) 20(23):37–40. doi: 10.3969/j.issn.1672-2779.2022.23.015
51. Chen FZ, Lv QB. Effect of Tai Ji Chuan on blood pressure in patients with hypertension. Modern Nur. (2013) 4:18–9.
52. Lin H, Huang JS. Promoting effect of fitness Qigong Wuqinxi on rehabilitation of elderly patients with hypertension. Chin J Gerontol. (2013) 33(07):1645–7. doi: 10.3969/j.issn.1005-9202.2013.07.073
53. Tan LH, Jiang P, Ye L. Clinical study on eight-section brocade in adjuvant treatment of essential hypertension complicated with insomnia in senile patients. New Chin Med. (2022) 54(16):175–8. doi: 10.13457/j.cnki.jncm.2022.16.038
54. Zhou HH. Effect of wuqinxi on patients with essential hypertension. Med Diet Health. (2022) 20(11):186–188+192.
55. Luo F. Intervention effect and mechanism analysis of Baduanjin on elderly patients with type 2 diabetes mellitus complicated with hypertension. Chin J Geriatric Care. (2021) 19(05):13–6. doi: 10.3969/j.issn.1672-2671.2021.05.005
56. Zheng LW, Chen ZS, Chen F, Liu J, Ge L. Mechanism of Baduanjin exercise on essential hypertension based on L-Arg/NOS/NO pathway. Fujian J Tradit Chin Med. (2021) 52(01):8–12. doi: 10.13260/j.cnki.jfjtcm.012151
57. Chen XX, Lv HQ. Effects of taijiquan exercise on hypertension Patients”NO consistency in plasma,the activity of RBC Na -K+.ATPase and Ca+-Mg+ATPase. J Beijing Sport University. (2006) 10:1359–61. doi: 10.19582/j.cnki.11-3785/g8.2006.10.023
58. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. (2002) 360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-11918
59. Lawes CM, Rodgers A, Bennett DA, Parag V, Suh I, Ueshima H, et al. Blood pressure and cardiovascular disease in the Asia pacific region. J Hypertens. (2003) 21(4):707–16. doi: 10.1097/00004872-200304000-00013
60. Tao S, Li Z. Effects of qigong exercise on cardiovascular risk factors in patients with metabolic syndrome: a systematic review and meta-analysis. Front Physiol. (2023) 14:1092480. doi: 10.3389/fphys.2023.1092480
61. Steadman Breit JP, Kelley GA. Response variation as a result of tai chi on resting blood pressure in hypertensive adults: an aggregate data meta-analysis. Complement Ther Clin Pract. (2022) 49:101641. doi: 10.1016/j.ctcp.2022.101641
62. Ma Z, Lei H, Tian K, Liu Z, Chen Y, Yang H, et al. Baduanjin exercise in the treatment of hypertension: a systematic review and meta-analysis. Front Cardiovasc Med. (2022) 9:936018. doi: 10.3389/fcvm.2022.936018
63. Wehner C, Blank C, Arvandi M, Wehner C, Schobersberger W. Effect of Tai Chi on muscle strength, physical endurance, postural balance and flexibility: a systematic review and meta-analysis. BMJ Open Sport Exerc Med. (2021) 7(1):e000817. doi: 10.1136/bmjsem-2020-000817
64. Alsubiheen A, Petrofsky J, Yu W, Lee H. Effect of Tai Chi combined with mental imagery on cutaneous microcirculatory function and blood pressure in a diabetic and elderly population. Healthcare. (2020) 8(3):342. doi: 10.3390/healthcare8030342
65. Shen AM, Wei Y, Hua JJ. Study of Wuqinxi exercise reducing absolute risk of ischemic cardiovascular disease. Sports Sci Res. (2015) 19(06):38–40. doi: 10.19715/j.tiyukexueyanjiu.2015.06.008
66. Song Y, Li J, István B, Xuan R, Wei S, Zhong G, et al. Current evidence on traditional Chinese exercises for quality of life in patients with essential hypertension: a systematic review and meta-analysis. Front Cardiovasc Med. (2020) 7:627518. doi: 10.3389/fcvm.2020.627518
67. Lin B, Jin Q, Liu C, Zhao W, Ji R. Effect and mechanism of tai chi on blood pressure of patients with essential hypertension: a randomized controlled study. J Sports Med Phys Fitness. (2022) 62(9):1272–7. doi: 10.23736/s0022-4707.21.13394-11398
68. Pan X, Zhang Y, Tao S. Effects of Tai Chi exercise on blood pressure and plasma levels of nitric oxide, carbon monoxide and hydrogen sulfide in real-world patients with essential hypertension. Clin Exp Hypertens. (2015) 37(1):8–14. doi: 10.3109/10641963.2014.881838
69. Van Guilder GP, Westby CM, Greiner JJ, Stauffer BL, DeSouza CA. Endothelin-1 vasoconstrictor tone increases with age in healthy men but can be reduced by regular aerobic exercise. Hypertension. (2007) 50(2):403–9. doi: 10.1161/hypertensionaha.107.088294
70. Jin QG, Li NC, Sun XR, Huang SH. Effect of taurine on endocrine function of endothelial cells after strenuous training in rats. Chin Sport Sci. (1999) 19(6):90–3. doi: 10.3969/j.issn.1000-677X.1999.06.022
71. Field T. Tai Chi research review. Complement Ther Clin Pract. (2011) 17(3):141–6. doi: 10.1016/j.ctcp.2010.10.002
72. Zeng F, Luo J, Ye J, Huang H, Xi W. Postoperative curative effect of cardiac surgery diagnosed by compressed sensing algorithm-based E-health CT image information and effect of Baduanjin exercise on cardiac autonomic nerve function of patients. Comput Math Methods Med. (2022) 2022:4670003. doi: 10.1155/2022/4670003
Keywords: essential hypertension, traditional Chinese exercise, Tai Chi, Baduanjin, systematic review, network meta-analysis
Citation: Zhang Q, Xu X, Wu Q, Zhang J, Huang S, Wu L, Tian M and Zhang D (2024) Effects of different traditional Chinese exercise in the treatment of essential hypertension: a systematic review and network meta-analysis. Front. Cardiovasc. Med. 11:1300319. doi: 10.3389/fcvm.2024.1300319
Received: 23 September 2023; Accepted: 19 February 2024;
Published: 28 February 2024.
Edited by:
Giuseppe Caminiti, Università telematica San Raffaele, ItalyReviewed by:
Jilin Li, Second Affiliated Hospital of Shantou University Medical College, China© 2024 Zhang, Xu, Wu, Zhang, Huang, Wu, Tian and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Delin Zhang ZGVsaW41MTg2QDE2My5jb20=
†These authors have contributed equally to this work
Abbreviations TCEs, traditional Chinese exercises; NMA, network meta-analysis; TC, Tai Chi; BDJ, Baduanjin; WQX, Wuqinxi; LZJ, Liuziju; SBP, systolic blood pressure; DBP, diastolic blood pressure; RCTs, randomized controlled trials; WMD, weighted mean difference; CI, confidence interval; CINeMA, confidence in network meta-analysis; GRADE, grading of recommendations assessment, development, and evaluation; NO, nitric oxide; ET-1, endothelin-1.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.