- 1The George Institute for Global Health, University of New South Wales, Sydney, NSW, Australia
- 2The George Institute for Global Health, Beijing, China
- 3Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 4China Centre for Health Development Studies, Peking University, Beijing, China
- 5School of Public Health, University of Illinois Chicago, Chicago, IL, United States
- 6Yeda Hospital of Yantai, Yantai, Shandong, China
- 7Yantaishan Hospital of Yantai, Yantai, Shandong, China
- 8Yantai Sino-French Friendship Hospital, Yantai, Shandong, China
- 9Department of Epidemiology and Biostatistics, Imperial College London, London, United Kingdom
- 10Department of Hygiene and Epidemiology, University of Ioannina School of Medicine, Ioannina, Greece
Objective: In China, a limited number of studies focus on women and examine the effect of cardiometabolic multimorbidity (defined as the presence of two or more cardiometabolic diseases) on health outcomes. This research aims to investigate the epidemiology of cardiometabolic multimorbidity and the association of cardiometabolic multimorbidity with long-term mortality.
Methods: This study used data from the China Health and Retirement Longitudinal Study between 2011 and 2018, which includes 4,832 women aged 45 years and older in China. Poisson-distributed Generalized Linear Models (GLM) were applied to examine the association of cardiometabolic multimorbidity with all-cause mortality.
Results: Overall, the prevalence of cardiometabolic multimorbidity was 33.1% among the total sample of 4,832 Chinese women, and increased with age, ranging from 28.5% (22.1%) for those aged 45–54 years to 65.3% (38.2%) for those aged ≥75 years in urban (rural) areas. Compared with the group of none and single disease, cardiometabolic multimorbidity was positively associated with all-cause death (RR = 1.509, 95% CI = 1.130, 2.017), after adjusting socio-demographic and lifestyle behavioral covariates. Stratified analyses revealed that the association between cardiometabolic multimorbidity and all-cause death was only statistically significant (RR = 1.473, 95% CI = 1.040, 2.087) in rural residents, but not significant in urban residents.
Conclusion: Cardiometabolic multimorbidity is common among women in China and has been associated with excess mortality. Targeted strategies and people-centered integrated primary care models must be considered to more effectively manage the cardiometabolic multimorbidity shift from focusing on single-disease.
1. Introduction
Metabolic disease is associated with the high risk of cardiovascular diseases (1, 2) and all-cause mortality (3–5) has been a major global challenge. In 2019, one-third of all deaths worldwide were due to cardiovascular disease and the cardiovascular diseases, especially coronary heart disease and stroke, is the leading cause of death worldwide (3). The disease burden of cardiometabolic multimorbidity (defined as the coexistence of two or more cardiometabolic diseases) is rising rapidly. In China and low-and middle income countries (LMICs), the number of people experiencing cardiometabolic multimorbidity has increased rapidly over the past few decades (6–8). In European countries and the United States, multimorbidity is associated with higher healthcare service utilization, poorer health outcomes, and mortality, challenging the single-disease framework of most healthcare configurations (9, 10).
Although several studies have been conducted in high-income countries (HICs) on the burden and effect of multimorbidity, this topic remains an emerging research area of research in LMICs (11–13). Recently, only a few studies in certain regions of China have explored this topic (14–16). For example, the Chinese Electronic Health Records Research in Yinzhou (CHERRY) study focusing on Yinzhou County, which examined the burden of cardiometabolic multimorbidity and mortality risk among 1 million subjects in China (16).
Most of previous studies investigated the relationships between some single chronic conditions alone and health outcomes. There is limited evidence on the long-term changes of health related outcomes in individuals who are suffering from cardiometabolic multimorbidity (3–5). In China, there is no study focusing on females and estimated the impact of cardiometabolic multimorbidity on long-term mortality using nationally representative data (17–21). Therefore, the objective of this research is to investigate the prevalence of cardiometabolic multimorbidity among Chinese women and the association of cardiometabolic multimorbidity with all-cause mortality, using nationally representative population-based cohort data.
2. Materials and methods
2.1. Data source
A nationally representative population-based cohort study was designed, using longitudinal data from the baseline and newest wave of China Health and Retirement Longitudinal Study (CHARLS) conducted from 2011 to 2018. The aim of CHARLS is to collect a set of high-quality micro-data representing families and individuals of middle-aged and elderly people aged 45 and above in China. The CHARLS baseline survey was launched in 2011, covering 150 counties, 450 villages/communities as primary sampling units (PSUs), and over 17,000 individuals in about 10,000 households. These samples will then be tracked every 2 to 3 years. Data were collected in a survey in which four-stage stratified cluster sampling was used to select eligible individuals. Details of the procedures involved in CHARLS and its multistage stratified sampling are described elsewhere (22). The CHARLS questionnaire includes: basic socio-demographic information, family structure and income, health status, health service utilization and expenditure, retirement and pensions, anthropometric measurements and biomarkers. Written informed consent was obtained from all participants (22).
The baseline of CHARLS collected a total of 17,708 participants, including 9,230 adult women, with the respondent rate above 80%. The fourth wave of CHARLS survey successfully re-interviewed 7,593 females in 2018. This study identified 5,538 participants with biomarker information and blood test. After deleting the individuals aged below 45 years and those respondents with missing values for the outcome variable and covariates of interest, 4,832 individuals who performed the two wave surveys were included (The sample selection flowchart was shown in Supplementary Figure 1).
2.2. Measures
We counted the number of chronic diseases for each participant, identifying those with multimorbidity (23, 24). Cardiometabolic multimorbidity was defined as the presence of two or more cardiometabolic diseases included for each participant (17, 20, 21). A total of seven cardiovascular and metabolic diseases were used to measure multimorbidity. Hypertension, diabetes, dyslipidaemia, hyperuricemia and central obesity were measured by biomarkers or blood test information. Another two non-fatal cardiometabolic diseases, including heart disease and stroke, were ascertained via self-reports of a physician or health professional diagnosis of heart disease or stroke.
In this study, the hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg, and/or taking antihypertensive drugs for elevated blood pressure (25). The diabetes was defined as (1) fasting blood glucose level ≥126 mg/dL (7.0 mmol/L); and/or (2) HbA1c concentration ≥6.5%; and/or (3) insulin therapy and/or medication for elevated blood glucose (26). The dyslipidemia was defined as (1) total cholesterol ≥240 mg/dL (6.22 mmol/L); and/or (2) low-density lipoprotein cholesterol ≥160 mg/dL (4.14 mmol/L); and/or (3) high-density lipoprotein cholesterol Protein cholesterol <40 mg/dL (1.04 mmol/L); and/or (4) triglycerides ≥200 mg/dL (2.26 mmol/L); and/or (5) taking anti-dyslipidemic drugs (27). The hyperuricemia is defined as a serum uric acid concentration greater than 7.0 mg/dL in men and greater than 6.0 mg/dL in women (28). The central obesity was defined as a waist circumference greater than 85 cm in female participants with a body mass index (BMI) ≥30 kg/m2 (29). The presence of heart disease and stroke, respectively, was determined by two questions in CHARLS survey: the participants were asked “Have you been diagnosed with heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems by a doctor” and “Have you been diagnosed with stroke by a doctor?”
Regarding the health related outcome variable, all-cause mortality during the period of 2011–2018 was used as the primary outcome. The death information of participants at baseline was collected in sequential surveys and the last follow-up was conducted in 2018.
2.3. Statistical analysis
Poisson-distributed Generalized Linear Models (GLM) were conducted to determine the longitudinal association of Cardiometabolic multimorbidity with all-cause mortality. Models are adjusted on age, marital status, educational level, residence place, region, and social health insurance at baseline (model 1) and other confounding factors (smoking, drinking alcohol, other non-communicable diseases (NCDs), and depression) (model 2). Depressive disorder was measured by the 10-item Center for Epidemiologic Studies Depression Scale (CES-D 10), which has been identified as a valid and reliable useful mental health assessment tool in China (30).
We performed stratified analyses to further investigate urban-rural differences of the association of cardiometabolic multimorbidity with all-cause death. In terms of the multivariable regression analyses, relative risk ratios (RR) and 95% confidence intervals (CI) were reported. We performed the sensitivity analysis on relationships between the single components of cardiometabolic syndrome and all-cause mortality. We also conducted the regression analyses by using a newer cut-off of 5.1 mg/dl for the definition of hyperuricemia for females (31). All analyses were weighted to account for the multi-stage probability-proportionate-to-size sampling (PPS) design of CHARLS, and conducted using Stata Version 16.0 (Stata Corp., College Station, TX, USA). P-values < 0.05 were deemed statistically significant.
3. Results
Our analysis included 4,832 females from the CHARLS in China. The mean age of respondents was 57.7 years at the baseline survey. Among the participants, 60.1% of the respondents were illiterate, 65.1% of individuals living in rural areas and 93.6% of individuals with social medical insurances. Among Chinese women, the proportion of current smoking and alcohol drinking was 5.9 and 12.2%, respectively. The prevalence of depression disorder was 44.3% (Table 1).
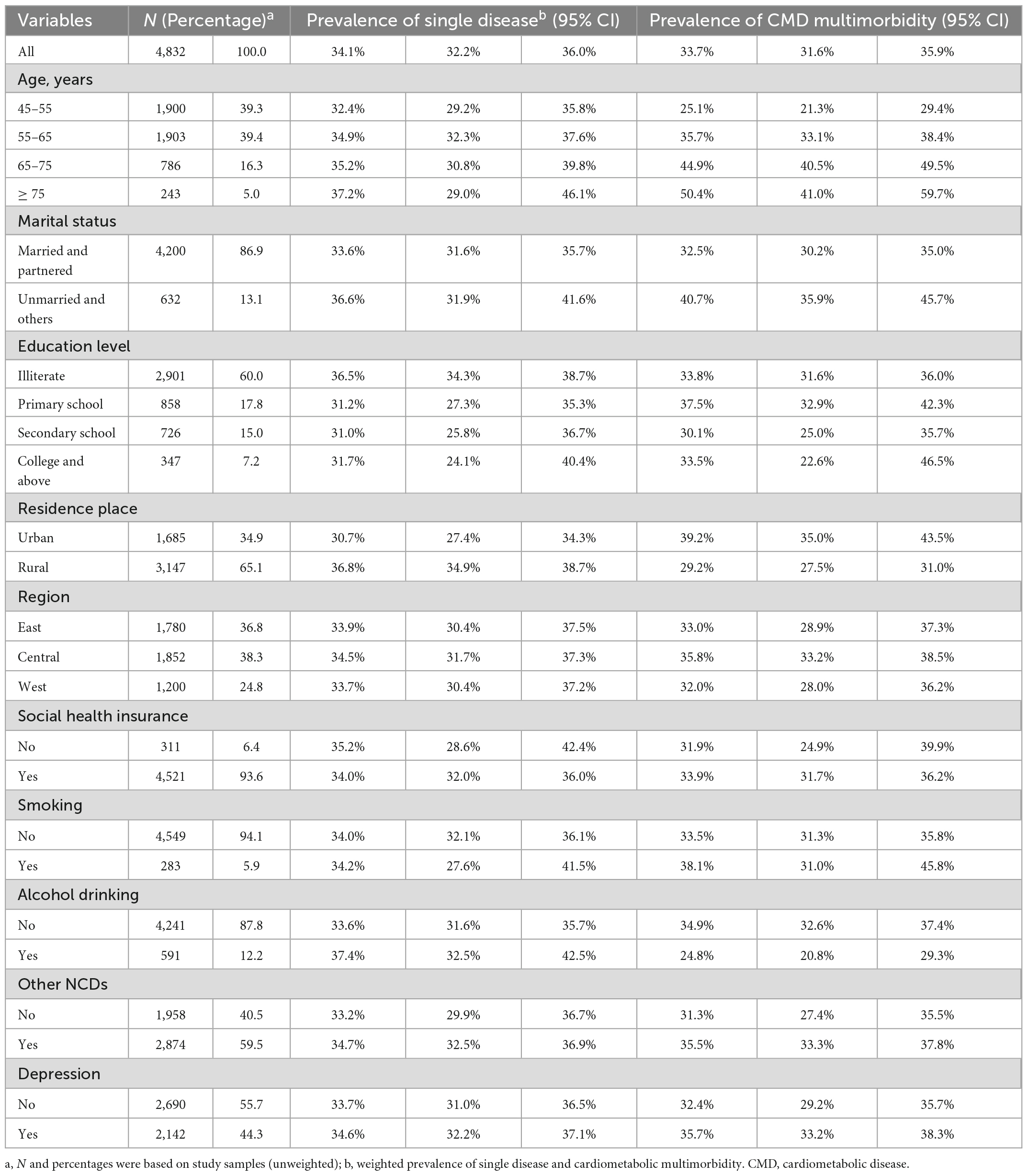
Table 1. Characteristics of participants, the prevalence of single condition and CMD multimorbidity.
Table 2 showed the prevalence of main cardiometabolic diseases and multimorbidity across age group and residence place. Among the Chinese women, the prevalence of cardiometabolic multimorbidity was 33.1%, and raised with age, ranging from 28.5% (22.1%) for those aged 45–54 years to 65.3% (38.2%) for those aged 75 years and above in urban (rural) areas. Over 30% of Chinese women experiencing hypertension and hyperlipidemia. The prevalence of heart disease, diabetes, concentric obesity, hyperuricemia and stroke was 15.9, 14.7 5.5, 4.5, and 2.6%, respectively. The prevalence of hypertension, hyperlipidemia, diabetes as well as stroke increased with age among urban citizens and was commonly higher than those of rural residents. Figure 1 showed a higher proportions of all-cause death among individuals in rural areas compared to individuals in urban areas.
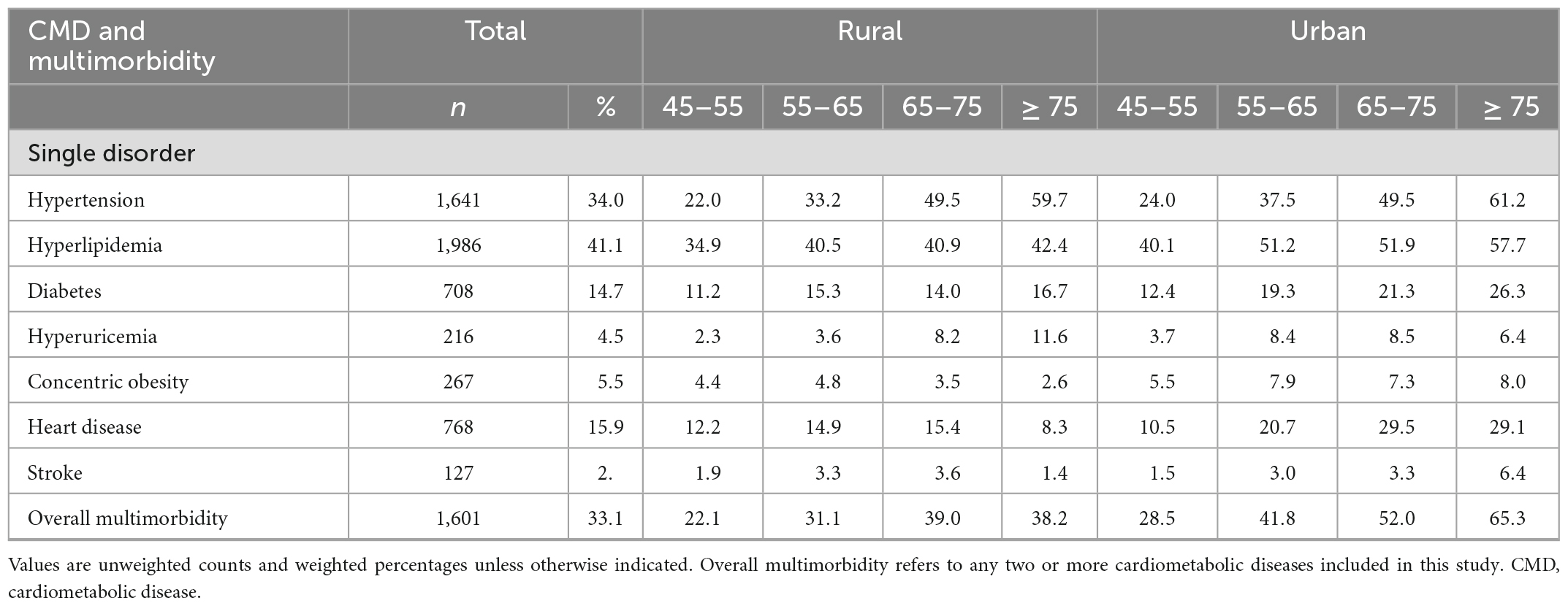
Table 2. The proportion of cardiometabolic diseases and multimorbidity among Chinese adults by age group and residence place (N = 4,832).
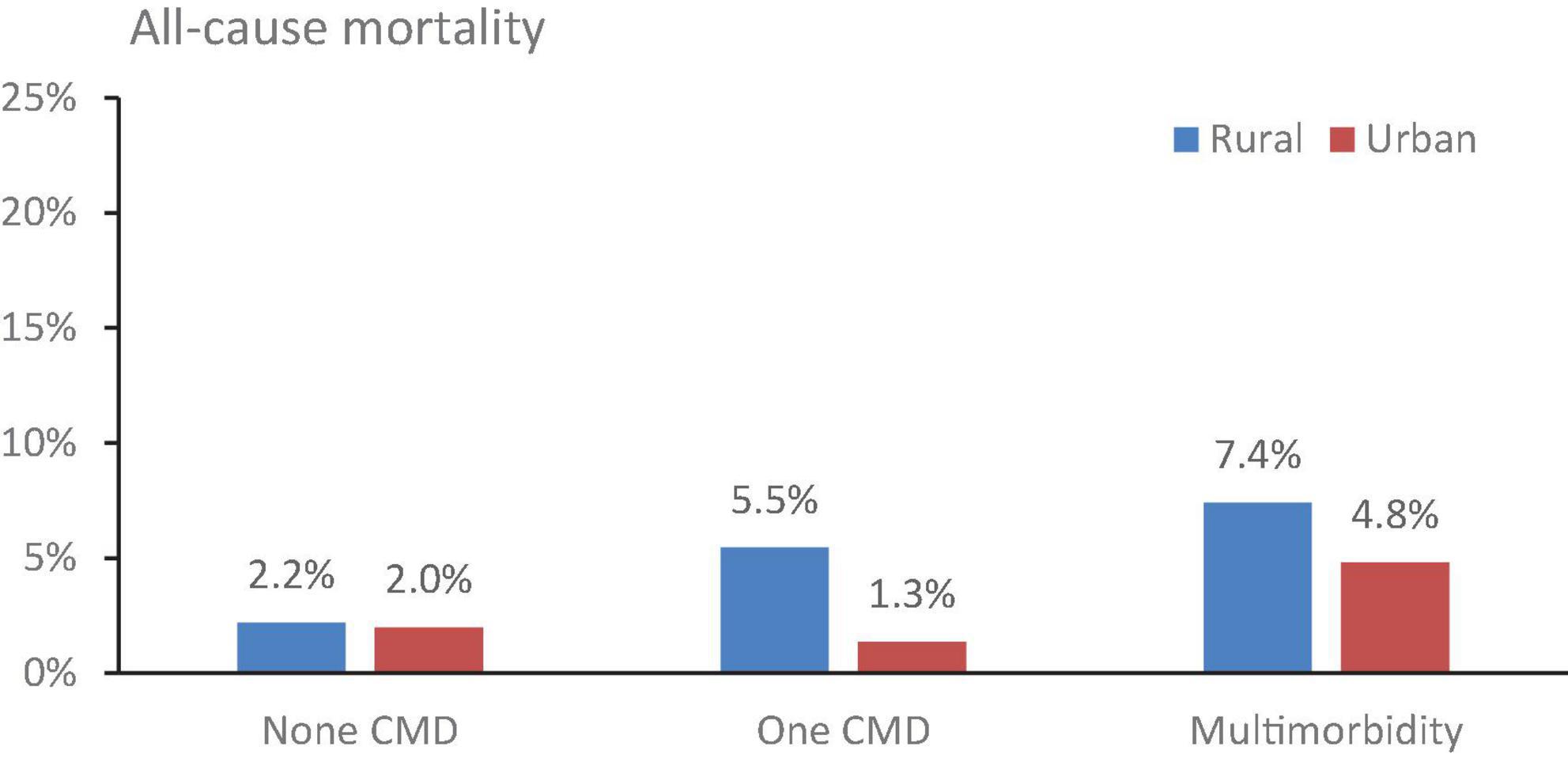
Figure 1. The all-cause mortality from 2011 to 2018 by the number of disease and residence place. CMD, cardiometabolic disease.
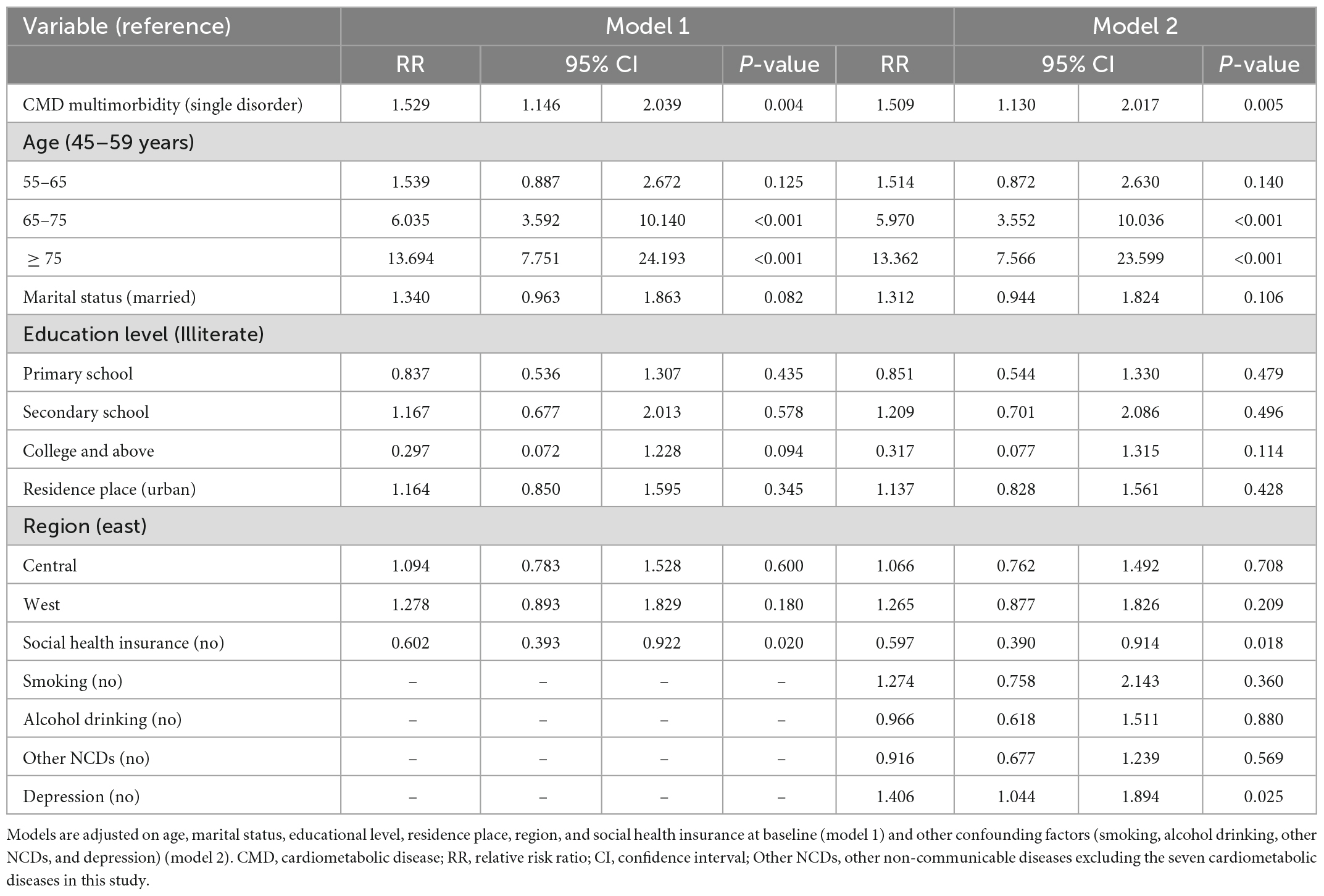
Table 3 revealed the relationship between cardiometabolic multimorbidity and health-related outcomes. Cardiometabolic multimorbidity was positively associated with all-cause death (RR = 1.509, 95% CI = 1.130, 2.017), after adjusting socio-demographic and lifestyle behavioral covariates. In women with ages above 65 years, depression and those without social health insurance were more likely to have the risk of death (Table 3). The stratified analysis showed that he association of cardiometabolic multimorbidity with all-cause death was only statistically significant (RR = 1.473, 95% CI = 1.040, 2.087) in rural residents, but not significant in urban residents (Table 4). The sensitivity analyses suggested consistent results (Supplementary Tables 1, 2). For the single disorders, stroke, heart disease and diabetes showed a statistically significant association with all-cause mortality, after adjusting socio-demographic and lifestyle behavioral covariates (Supplementary Table 3).
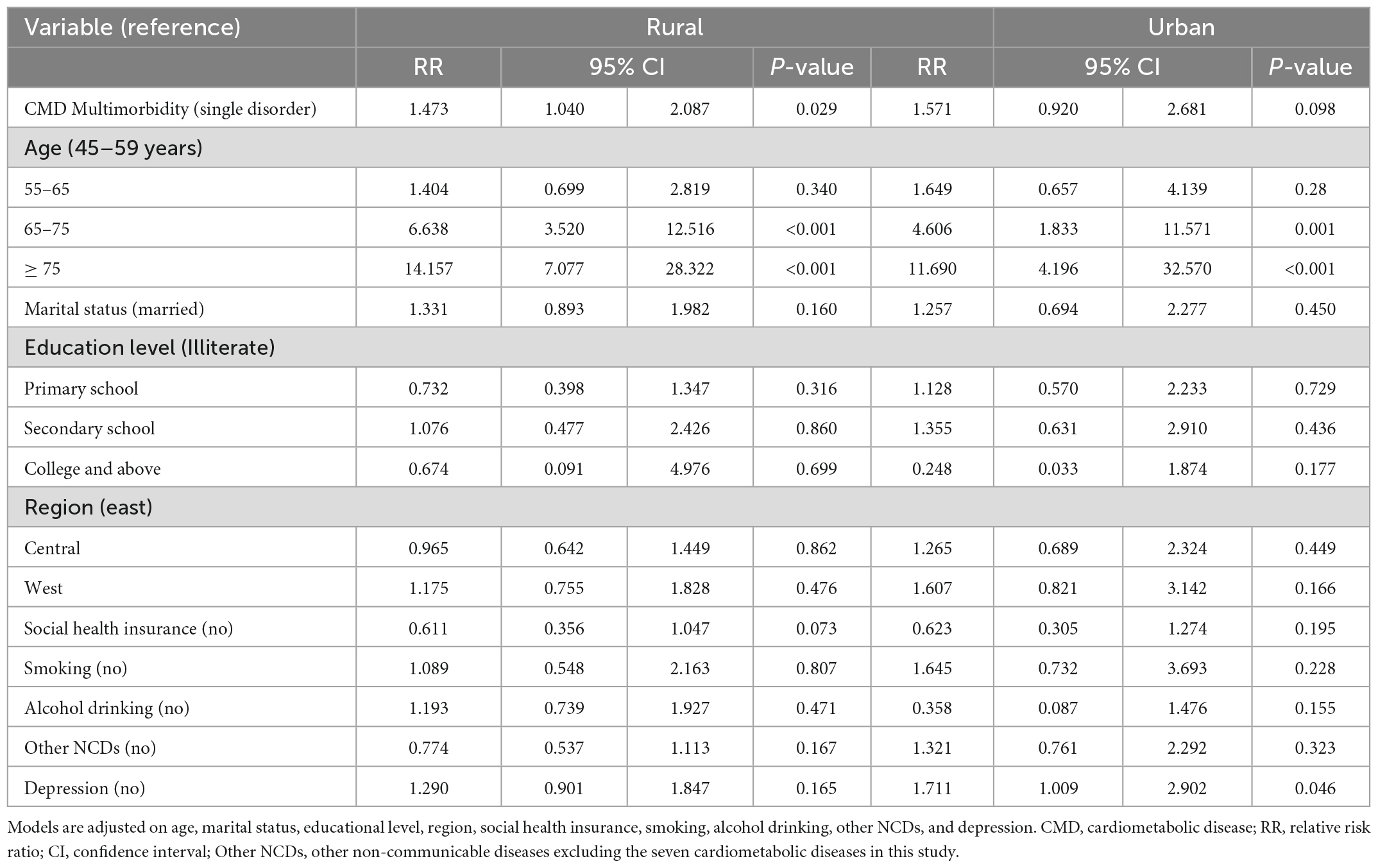
Table 4. Association of CMD multimorbidity with all-cause death among participants living the rural and urban area.
4. Discussion
This research analyzed nationally representative longitudinal data from the CHARLS to examine the prevalence of cardiometabolic multimorbidity and its association of cardiometabolic multimorbidity with all-cause death among middle-aged and elderly Chinese females. This study revealed that cardiometabolic multimorbidity is common among Chinese women, especially among the elderly and urban citizens. We found that cardiometabolic multimorbidity was associated with excess mortality. Furthermore, the association between cardiometabolic multimorbidity and all-cause death was only statistically significant in rural residents, but not significant in urban residents.
The cardiometabolic multimorbidity prevalence estimated by this study was 33.1% among middle-aged and older Chinese women in 2011. For general adults in China, there were studies showing a lower prevalence of metabolic disorder (16.5% in 2000 and 23.3% in 2009) (7). A meta-analysis in the basis of studies from mainland China also showed that the pooled prevalence of metabolic syndrome was 24.5% (32). Those evidence suggested that China is experiencing an emerging cardiometabolic disease epidemic, which may be related to the accelerated changes in dietary patterns and lifestyle behaviors due to demographic and socioeconomic transitions during the past decades (33). Moreover, there are many studies revealing a high prevalence of cardiometabolic syndromes in western developed countries and other regions in Asia, such as the United States (35%), Iran (37%), and Turkey (44%) (34–36). Variations in cardiometabolic syndrome prevalence between LMICs and HICs could be because of real differences across countries, and might also be due to potentially different definitions and sampling methods (36, 37).
The results from this research also suggested that cardiometabolic multimorbidity increased with the individual’s age and the people living in urban areas had a higher proportion of cardiometabolic multimorbidity than those rural persons in China. In line with previous findings, the burden of cardiometabolic disease increases with age due to the declining trends in cardiometabolic function (34, 38). Urban residents experiences a higher proportion of cardiometabolic multimorbidity than rural residents (32, 39), which could be attributed to physical inactivity, sedentary, unhealthy diet (such as excessive intake of high-calorie food, fat and salt) during the process of urbanization and economic development (39–41).
A few of studies have suggested that multiple chronic diseases have a significant impact on health related outcomes and mortality (10, 16–18). These findings are consistent with our previous studies in China (16, 19–21), United States (10, 42, 43), Japan (44), and Europe (45), where multimorbidity presented in health-related outcomes and deaths (10, 16). Cardiovascular and metabolic diseases have been revealed by several studies to play a dominant role in multiple multimorbidity patterns (41). The association between single cardiometabolic disease and negative health outcomes and mortality has also been documented (46). This research further provides new evidence that significant relationship between cardiometabolic multimorbidity and long-term mortality among adult women in China. We also performed the regression analyses by using a recently lower cut-off of 5.1 mg/dl for the definition of hyperuricemia for females (31), which also suggested consistent results.
Stratified analyses of this study revealed a significant association between cardiometabolic multimorbidity and all-cause death in rural residents, but there was not a significant association in urban residents while they had a high prevalence of cardiometabolic multimorbidity. Previous studies from China have documented disparities in the healthcare access and service utilization between residents living in rural and urban areas (47). Patients in rural areas have less geographic access to health-care than those patients living in urban areas. Rural areas in China could be more prone to healthcare provider shortages and lack of medical resources (48, 49). Rural residents usually face greater financial barriers and relatively low-quality health care (50). Thus, early screening of high-risk groups of cardiometabolic multimorbidity should be strengthened, and targeted preventive measures should be taken further. A strong people-centered primary care system needs to be oriented toward cardiometabolic diseases and multimorbidity, which has been shown to be the most cost-effective way to manage chronic diseases (51–54).
Establishing a multidisciplinary team composed of clinical physicals, geriatricians, pharmacists, nurses, nutritionists, rehabilitation physiotherapists, social workers, patients and their families is a potential model for dealing with multimorbidity issues, following the “people-centered principle” of managing multimorbidity. In the process of achieving the “Healthy China 2030” strategic goals (55) and Sustainable Development Goals, considering the increasing burden of multimorbidity populations and its long-term impact in future, it need more attention from clinicians, researchers and health policy makers from China as well as other countries with economies in transition.
To our best knowledge, this is the first nationally representative cohort study that focused on adult women and investigated associations of cardiometabolic multimorbidity with long-term mortality in China that examined the rural-urban differences in the relationships, by using longitudinal data with cardiometabolic biomarkers for the disease diagnosis. This study also has some limitations. First, while we identify several cardiometabolic diseases on the basis of biomarkers, the partial use of self-reported measures of heart disease and stroke could underestimate the prevalence of these chronic diseases. Second, we estimated the prevalence of cardiometabolic multimorbidity and its association with health outcomes by simply counting the number of chronic conditions, hence the accuracy of findings may be affected by the types of cardiometabolic multimorbidity. CHARLS only collected the data for calculating all-cause mortality and we could not further analyze the association between multimorbidity and mortality due to stroke or cardiovascular diseases. Third, there was only a 7-year follow-up period of CHARLS data and long-term impacts on health-related outcomes due to multimorbidity should be examined further. Finally, this study only analyzed the middle-aged and older Chinese women due to the CHARLS data collection, which may affect the generalizability of the findings from this study. The prevalence of cardiometabolic multimorbidity and its relationships with more health related outcomes among younger populations should be considered for future studies.
5. Conclusion
Cardiometabolic multimorbidity is common among women in China and has been associated with excess mortality. Health-care delivery models need to shift from focusing on single-disease to effectively managing cardiometabolic multimorbidity. Targeted strategies and people-centered integrated primary care models must be considered to more effectively manage the cardiometabolic multimorbidity shift from focusing on single-disease. Medical resources need to be prioritized to screen, prevent and treat cardiometabolic diseases as well as multimorbidity, especially in rural areas.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The Biomedical Ethics Review Committee of Peking University approved the CHARLS study (approval number: IRB00001052–11015), and all interviewees were required to provide informed consent. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YZ conceived and designed the study and did the initial analysis. LS supervised data analysis. YZ and SZ wrote the first draft of the manuscript. HZ, XL, AD, QW, LS, and IT critically revised the first draft. All authors reviewed, edited and commented on multiple versions of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.922932/full#supplementary-material
References
1. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. (2009) 120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644
2. Meigs JB. Invited commentary: insulin resistance syndrome? Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol. (2000) 152:908–11. doi: 10.1093/aje/152.10.908
3. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
4. Rutter MK, Meigs JB, Wilson PW. Cardiovascular risk and the metabolic syndrome. Metab Syndr Relat Disord. (2006) 4:252–60. doi: 10.1089/met.2006.4.252
5. Kivimaki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. (2017) 6:e277–85. doi: 10.1016/S2468-2667(17)30074-9
6. Gu D, Reynolds K, Wu X, Chen J, Duan X, Reynolds RF, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. (2005) 365:1398–405. doi: 10.1016/S0140-6736(05)66375-1
7. Xi B, He D, Hu Y, Zhou D. Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: the China Health and Nutrition Survey in 2009. Prev Med. (2013) 57:867–71. doi: 10.1016/j.ypmed.2013.09.023
8. Boyd CM, Fortin M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Rev. (2010) 32:451–74. doi: 10.1007/BF03391611
9. Palladino R, Lee JT, Millett C. Associationbetween multimorbidity and healthcareutilisation and health outcomesamong elderly people in Europe. Eur J Public Health. (2014) 24:49. doi: 10.1093/eurpub/cku151.118
10. Angelantonio ED, Kaptoge S, Wormser D, Willeit P, Butterworth AS, Bansal N, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. (2015) 314:52–60.
11. Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Family Pract. (2011) 28:516–23. doi: 10.1093/fampra/cmr013
12. Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, et al. Health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. (2011) 68:387–420. doi: 10.1177/1077558711399580
13. Lee JT, Hamid F, Pati S, Atun R, Millett C. Impact of noncommunicable disease multimorbidity on health care utilisation and out-of-pocket expenditures in middle-income countries: cross sectional analysis. PLoS One. (2015) 10:e0127199. doi: 10.1371/journal.pone.0127199
14. Chen H, Cheng M, Zhuang Y, Broad JB. Multimorbidity among middle-aged and older persons in urban China: prevalence, characteristics and health service utilization. Geriatr Gerontol Int. (2018) 18:1447–52. doi: 10.1111/ggi.13510
15. Chen H, Chen Y, Cui B. The association of multimorbidity with health care expenditure among the elderly patients in Beijing, China. Arch Gerontol Geriat. (2018) 79:32–8. doi: 10.1016/j.archger.2018.07.008
16. Zhang D, Tang X, Shen P, Si Y, Liu X, Xu Z, et al. Multimorbidity of cardiometabolic diseases: prevalence and risk for mortality from one million Chinese adults in a longitudinal cohort study. BMJ Open. (2019) 9:e024476. doi: 10.1136/bmjopen-2018-024476
17. Archana SM, Aurore F, Séverine S, Tabak A, Shipley M, Dugravot A, et al. Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: a cohort study. PLoS Med. (2018) 15:e1002571. doi: 10.1371/journal.pmed.1002571
18. Arokiasamy P, Uttamacharya U, Jain K, Biritwum RB, Yawson AE, Wu F, et al. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal? BMC Med. (2015) 13:178. doi: 10.1186/s12916-015-0402-8
19. Zhao Y, He L, Han C, Oldenburg B, Sum G, Haregu TN, et al. Urban-rural differences in the impacts of multiple chronic disease on functional limitations and work productivity among Chinese adults. Glob Health Action. (2021) 14:1975921. doi: 10.1080/16549716.2021.1975921
20. Zhao Y, Zhang P, Lee JT, Oldenburg B, van Heusden A, Haregu TN, et al. The prevalence of metabolic disease multimorbidity and its associations with spending and health outcomes in middle-aged and elderly Chinese adults. Front Public Health. (2021) 9:658706. doi: 10.3389/fpubh.2021.658706
21. Emerging Risk Factors Collaboration, Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. (2015) 314:52–60. doi: 10.1001/jama.2015.7008
22. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
23. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. doi: 10.1016/S0140-6736(12)60240-2
24. Zhao Y, Atun R, Oldenburg B, McPake B, Tang S, Mercer SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. (2020) 8:e840-9. doi: 10.1016/S2214-109X(20)30127-3
25. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. National heart, lung, and blood institute joint national committee on prevention, detection, evaluation, and treatment of high blood pressure; national high blood pressure education program coordinating committee: the seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. (2003) 289:2560–72. doi: 10.1001/jama.289.19.2560
26. Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. (2013) 310:948–59. doi: 10.1001/jama.2013.168118
27. Zhang M, Deng Q, Wang L, Huang Z, Zhou M, Li Y, et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: a nationally representative survey of 163,641 adults. Int J Cardiol. (2018) 260:196–203. doi: 10.1016/j.ijcard.2017.12.069
28. Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. (2008) 359:1811–21. doi: 10.1016/S1471-4892(02)00143-1
29. Association CDSoM. Guideline to the prevention and treatment of type 2 diabetes in China (2013 Edition). Chin J Endocrinol Metab. (2014) 10:893–942. doi: 10.3760/cma.j.issn.1000-6699.2014.10.02031
30. Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. (1999) 14:608–17. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z
31. Maloberti A, Giannattasio C, Bombelli M, Desideri G, Cicero AFG, Muiesan ML, et al. Hyperuricemia and risk of cardiovascular outcomes: the experience of the URRAH (Uric Acid Right for Heart Health) project. High Blood Press Cardiovasc Prev. (2020) 27:121–8. doi: 10.1007/s40292-020-00368-z
32. Li R, Li W, Lun Z, Zhang H, Sun Z, Kanu JS, et al. Prevalence of metabolic syndrome in mainland china: a meta-analysis of published studies. BMC Public Health. (2016) 16:296. doi: 10.1186/s12889-016-2870-y
33. Lao XQ, Ma WJ, Sobko T, Zhang YH, Xu YJ, Xu XJ, et al. Dramatic escalation in metabolic syndrome and cardiovascular risk in a Chinese population experiencing rapid economic development. BMC Public Health. (2014) 14:983. doi: 10.1186/1471-2458-14-983
34. Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA. (2015) 313:1973–4. doi: 10.1001/jama.2015.4260
35. Gundogan K, Bayram F, Gedik V, Kaya A, Karaman A, Demir O, et al. Metabolic syndrome prevalence according to ATP III and IDF criteria and related factors in Turkish adults. Arch Med Sci. (2013) 9:243–53. doi: 10.5114/aoms.2013.34560
36. Amirkalali B, Fakhrzadeh H, Sharifi F, Kelishadi R, Zamani F, Asayesh H, et al. Prevalence of metabolic syndrome and its components in the iranian adult population: a systematic review and meta-analysis. Iran Red Crescent Med J. (2015) 17:e24723. doi: 10.5812/ircmj.24723
37. Santos A, Barros H. Impact of metabolic syndrome definitions on prevalence estimates: a study in a Portuguese community. Diabetes Vasc Dis Res. (2007) 4:320–7. doi: 10.3132/dvdr.2007.059
38. Agborsangaya CB, Lau D, Lahtinen M, Cooke Tim, Johnson JA. Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC Public Health. (2012) 12:201. doi: 10.1186/1471-2458-12-201
39. Lu J, Wang L, Li M, Xu Y, Jiang Y, Wang W, et al. Metabolic syndrome among adults in China - The 2010 China noncommunicable disease surveillance. J Clin Endocrinol Metab. (2016) 102:507–15. doi: 10.1210/jc.2016-2477
40. Wikstrom K, Lindstrom J, Harald K, Peltonen M, Laatikainen T. Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982-2012. Eur J Intern Med. (2015) 26:211–6. doi: 10.1016/j.ejim.2015.02.012
41. Noe G, Ai K, Somnath C, Tyrovolas S, Olaya B, Leonardi M, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol. (2016) 71:205–14. doi: 10.1093/gerona/glv128
42. Bowling CB, Deng L, Sakhuja S, Morey MC, Jaeger BC, Muntner P. Prevalence of activity limitations and association with multimorbidity among US adults 50 to 64 years old. J Gen Intern Med. (2019) 34:2390–6.
43. Jindai K, Nielson CM, Vorderstrasse BA, Quiñones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005-2012. Prev Chronic Dis. (2016) 13:E151–151. doi: 10.5888/pcd13.160174
44. Jiao D, Watanabe K, Sawada Y, Tanaka E, Watanabe T, Tomisaki E, et al. Multimorbidity and functional limitation: the role of social relationships. Arch Gerontol Geriatr. (2021) 92:104249–104249. doi: 10.1016/j.archger.2020.104249
45. Singer L, Green M, Rowe F, Ben-Shlomo Y, Kulu H, Morrissey K. Trends in multimorbidity, complex multimorbidity and multiple functional limitations in the ageing population of England, 2002–2015. J Comorb. (2019) 9:2235042X19872030. doi: 10.1177/2235042X19872030
46. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. (2010) 56:1113–32. doi: 10.1016/j.jacc.2010.05.034
47. Chen Y, Yin Z, Xie Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int J Equity Health. (2014) 13:34. doi: 10.1186/1475-9276-13-34
48. Wu RX, Cai Y, Lan L, Fan ZW, Xue M. Trend analysis on the allocation of primary health care resources between urban and rural areas in China from 2008 to 2015. Chin Health Resour. (2017) 3:20–3.
49. Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv Res. (2011) 11:20. doi: 10.1186/s12913-017-1983-z
50. Yongjian X, Jie M, Na W, Fan X, Zhang T, Zhou Z, et al. Catastrophic health expenditure in households with chronic disease patients: a pre-post comparison of the New Health Care Reform in Shaanxi Province, China. PLoS One. (2018) 13:e0194539. doi: 10.1371/journal.pone.0194539
51. Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. (2012) 345:809–e5205. doi: 10.1136/bmj.e5205
52. Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. (2008) 14(Suppl 1):28–32. doi: 10.1080/13814780802436093
53. Smith SM, Wallace E, O’Dowd T, Fortin M, Smith SM. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. (2016) 2017(9):CD006560.
54. Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM. Managing patients with multimorbidity in primary care. BMJ. (2015) 350:h176.
Keywords: cardiometabolic disease, multimorbidity, health outcomes, women, Chinese adults
Citation: Zhao Y, Zhang H, Liu X, Desloge A, Wang Q, Zhao S, Song L and Tzoulaki I (2023) The prevalence of cardiometabolic multimorbidity and its associations with health outcomes among women in China. Front. Cardiovasc. Med. 10:922932. doi: 10.3389/fcvm.2023.922932
Received: 18 April 2022; Accepted: 20 January 2023;
Published: 09 February 2023.
Edited by:
Elsayed Z. Soliman, Wake Forest University, United StatesReviewed by:
Raman Kutty, Amala Cancer Research Centre, IndiaAlessandro Maloberti, University of Milano-Bicocca, Italy
Copyright © 2023 Zhao, Zhang, Liu, Desloge, Wang, Zhao, Song and Tzoulaki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lili Song,  bHNvbmdAZ2VvcmdlaW5zdGl0dXRlLm9yZy5jbg==
bHNvbmdAZ2VvcmdlaW5zdGl0dXRlLm9yZy5jbg==
 Yang Zhao
Yang Zhao Huan Zhang3
Huan Zhang3 Lili Song
Lili Song Ioanna Tzoulaki
Ioanna Tzoulaki