
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 12 January 2024
Sec. Cardiovascular Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1316063
This article is part of the Research Topic Case Reports in Heart Surgery: 2023 View all 15 articles
Cardiac myxoma is a rare etiology of ischemic stroke, especially in young people. We report a case of multiple myxomas in left atrium and right ventricle inducing acute cerebral infarction. No significant abnormalities were detected in the patient's preoperative laboratory examination. Following emergency surgery, the patient's prognosis was satisfactory, providing valuable empirical insight for the surgical management of acute cerebral infarction in individuals diagnosed with cardiac myxoma. Our objective is to heighten awareness regarding the evaluation and treatment of patients with acute cerebral infarction subsequent to early diagnosis of cardiac myxoma.
Cardiac myxomas account for between 50% and 85% of all cardiac tumors (1). Sixty percent to 80% of cardiac myxomas occur in the left atrium, usually attached to fossa ovalis, the right atrium and ventricle and valves are relatively rare (1, 2). Controversy surrounds the treatment of neurologic symptoms caused by cardiac myxoma, focusing on whether to prioritize removing cardiac tumors or addressing cerebral infarction first.
A 25-year-old woman came to our emergency center with repeated chest tightness, palpitations, asthma, occasional hand and foot numbness, and worsening symptoms during daily activities over a 2-month period. Dizziness, headache, nausea and vomiting occurred 1 day before hospital admission. A magnetic resonance imaging (MRI) of the head revealed multiple specks and flaky signals in the left cerebral hemisphere, suggesting the possibility of multiple acute cerebral infarctions (Figure 1, arrow). Intraoperative transesophageal ultrasound demonstrated a soft mass shadow attached to the anterior lobe of the mitral valve, which collided with the left ventricle during diastole. Additionally, another mass shadow was observed at the apex of the right ventricle with minimal activity (Figure 2, arrow below). Subsequently, a dark red jelly-like mass, sized approximately 5 × 3 cm in the left atrium and 3 × 2 cm in the right ventricle, was identified and completely excised (Figure 3). The histopathological examination of a biopsy specimen confirmed the presence of cardiac myxomas (Figure 4).
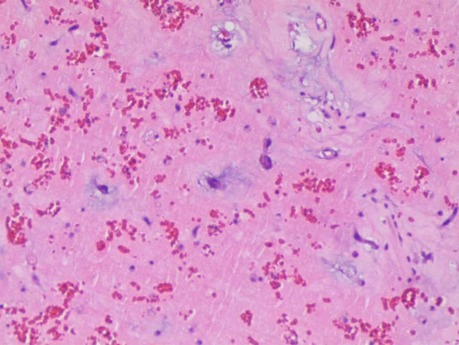
Figure 4. Sections under microscopic examination showed that the tumor cells are scattered in the myxoid matrix, star-shaped and polygonal, diffuse or intertwined into a network, and the focal area bleeds.
Ten hours after admission, the patient underwent an emergency operation in which a median sternal incision was made to gain access to the chest. Heparinization of the entire body was then carried out, followed by the establishment of cardiopulmonary bypass through the ascending aorta and superior and inferior vena cava. Subsequently, the entire body was cooled, and the superior and inferior vena cava were blocked. The left atrium was then incised and drained, with temporary omission of the left atrial tube insertion, to prevent the myxoma from dislodging. The ascending aorta was then blocked and cardioplegia was infused through the aortic root before a longitudinal incision was made in the right atrium and atrial septum following cardiac arrest. During the procedure, a dark red jelly-like mass, measuring approximately 5 × 3 cm, was identified in the left atrium and successfully removed. A left atrial retractor was then used to open the anterior lobe of the tricuspid valve, revealing a dark red jelly-like tumor measuring about 3 × 2 cm in the right ventricle. Following its removal, the tumor was meticulously rinsed multiple times with warm water to ensure no residual tumor was left in any cardiac cavity, thereby minimizing the risk of recurrence (3). The procedure lasted a total of 76 min under cardiopulmonary bypass, with 49 min being cardiac function-blocked. Post-operation, the patient was transferred to the intensive care unit with endotracheal intubation, and regained consciousness 3 h later. The endotracheal tube was successfully removed on the second day after the operation.
The patient was discharged from the hospital 10 days after surgery in good spirits and the muscle strength of the limbs was normal. Despite the successful recovery in physical strength, there was an observed temporary decrease in the patient's calculation ability. However, during the 3-month follow-up, the patient exhibited no residual dysarthria or difficulty accessing words, and there were no recurrent ischemic events. Additionally, her calculation ability had returned to normal.
As per our literature search, this is the first case report of multiple myxomas in left atrial and right ventricular inducing acute cerebral infarction in a young female patient. In this case, the patient was young and had cerebral infarction symptoms, which reminds doctors to pay attention to cardiogenic factor (4). In addition, the preoperative head magnetic resonance (MRI) of the patient showed that the areas of cerebral infarction were not confined to the same vascular area, which suggested that the stroke originated from the heart (5).
Cardiac MRI can provide unique information in the diagnosis of cardiac myxoma with robust tissue signature sequences (6). In this case, the patient suffered from acute cerebral infarction caused by cardiac myxomas. In order to prevent further aggravation of obstruction induced by cardiac myxomas, we performed emergency surgery as soon as possible to remove the risk of re-obstruction. The treatment of neurologic symptoms resulting from cardiac myxoma-induced infarction is a subject of debate, with no established guideline for stroke associated with myxoma (7). However, some scholars argue that immediate treatment of cardiac myxoma upon diagnosis is crucial for averting re-vascular obstruction, prioritizing it over the alleviation of neurological or other embolic symptoms in the brain (8).
Some scholars support the priority use of intravenous thrombolytic drugs after cerebral embolism, with recombinant tissue plasminogen activator considered safe and effective. However, postoperative pathology findings in successful thrombolysis cases revealed that the main component of the embolus was thrombosis. This finding may be attributed to the local vascular ischemic damage caused by myxoma embolus blocking cerebral blood vessels (9).
The choice of operation time window has also become a controversial topic. Wakako Fukuda et al. (10) conducted a study revealing that the occurrence of worsening brain complications decreased by 10% when surgery was performed more than 15 days after cerebral infarction. In the case reported by Yoshioka et al. (11), the patient's preoperative cranial MRI showed only multiple small infarcts in the brain without any signs of cerebral hemorrhage. After emergency surgery, right occipital lobe cerebral hemorrhage was found, notably, the patient's preoperative test results, including a platelet count of only 1 × 104/mm3 and a D-dimer level of 12.72 μg/ml, indicated severe disseminated intravascular coagulation (DIC). This case emphasizes the critical nature of preoperative coagulation function examination to avoid unforeseen complications during surgery.
In this case, after surgically removing the risk of cardiogenic obstruction, the neurological symptoms improved, and there were no new obstruction symptoms in other organs. Therefore, we believe it is crucial to promptly remove cardiac myxoma in non-DIC patients.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CT: Conceptualization, Formal Analysis, Writing – original draft. XG: Conceptualization, Writing – original draft. TC: Methodology, Writing – review & editing. JS: Investigation, Writing – review & editing. TZ: Visualization, Writing – review & editing. XZ: Formal Analysis, Investigation, Writing – review & editing. CR: Conceptualization, Funding acquisition, Writing – original draft.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Foundation of Yangzhou Science and Technology Planning (YZ2020076).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Gošev I, Paić F, Durić Z, Gošev M, Ivčević S, Jakuš FB, et al. Cardiac myxoma the great imitators: comprehensive histopathological and molecular approach. Int J Cardiol. (2013) 164(1):7–20. doi: 10.1016/j.ijcard.2011.12.052
2. Wang JG, Li YJ, Liu H, Li NN, Zhao J, Xing XM. Clinicopathologic analysis of cardiac myxomas: seven years’ experience with 61 patients. J Thorac Dis. (2012) 4(3):272–83. doi: 10.3978/j.issn.2072-1439.2012.05.07
3. Zhao S, Li H, Wu C, Pan Z, Wang G, Dai J. Surgical treatment of rare pediatric cardiac myxomas:12 years clinical experience in a single institution. BMC Cardiovasc Disord. (2023) 23(1):219. doi: 10.1186/s12872-023-03255-2
4. Lm Silva M Jr, Albuquerque TE, Melo ES. Giant atrial myxoma leading to stroke. Med J Aust. (2021) 215(6):258–e1. doi: 10.5694/mja2.51231
5. Kelley RE, Kelley BP. Heart-brain relationship in stroke. Biomedicines. (2021) 9(12):1835. doi: 10.3390/biomedicines9121835
6. Beroukhim RS, Ghelani S, Ashwath R, Balasubramanian S, Biko DM, Buddhe S, et al. Accuracy of cardiac magnetic resonance imaging in diagnosing pediatric cardiac masses: a multicenter study. JACC Cardiovasc Imaging. (2022) 15(8):1391–405. doi: 10.1016/j.jcmg.2021.07.010
7. Al-Said Y, Al-Rached H, Baeesa S, Kurdi K, Zabani I, Hassan A. Emergency excision of cardiac myxoma and endovascular coiling of intracranial aneurysm after cerebral infarction. Case Rep Neurol Med. (2013) 2013:839270. doi: 10.1155/2013/839270
8. Isogai T, Yasunaga H, Matsui H, Tanaka H, Hisagi M, Fushimi K. Factors affecting in-hospital mortality and likelihood of undergoing surgical resection in patients with primary cardiac tumors. J Cardiol. (2017) 69(1):287–92. doi: 10.1016/j.jjcc.2016.05.008
9. Acampa M, Guideri F, Tassi R, D’Andrea P, Marotta G, Lo Giudice G, et al. Thrombolytic treatment of cardiac myxoma-induced ischemic stroke: a review. Curr Drug Saf. (2014) 9(2):83–8. doi: 10.2174/1574886308666140110123705
10. Eishi K, Kawazoe K, Kuriyama Y, Kitoh Y, Kawashima Y, Omae T. Surgical management of infective endocarditis associated with cerebral complications. Multi-center retrospective study in Japan. Thorac Cardiov Sur. (1995) 110(6):1745–55. doi: 10.1016/S0022-5223(95)70038-2
Keywords: myxomas, neurologic symptoms, emergency operation, case report, cardiac tumors
Citation: Tang C, Gao X, Chen T, Shao J, Zhu T, Zheng X and Ren C (2024) Case Report: Acute cerebral infarction caused by left atrial and right ventricular myxoma received emergency operation. Front. Cardiovasc. Med. 10:1316063. doi: 10.3389/fcvm.2023.1316063
Received: 10 October 2023; Accepted: 28 December 2023;
Published: 12 January 2024.
Edited by:
Giuseppe Gatti, Azienda Sanitaria Universitaria Giuliano Isontina, ItalyReviewed by:
Francesco Patanè, Azienda Ospedaliera Ospedali Riuniti Papardo Piemonte, Italy© 2024 Tang, Gao, Chen, Shao, Zhu, Zheng and Ren. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanli Ren cmVuY2hsQDE2My5jb20=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.