- 1Lemore Center for Integrated Lymphatics and Vascular Research, Lewis Katz School of Medicine at Temple University, Philadelphia, PA, United States
- 2Centers of Metabolic Disease Research and Thrombosis Research Center, Departments of Cardiovascular Sciences, Lewis Katz School of Medicine at Temple University, Philadelphia, PA, United States
- 3Center for Translational Medicine, Vascular Biology and Therapeutics Program, Department of Medicine, Thomas Jefferson University, Philadelphia, PA, United States
- 4DeWitt Daughtry Family Department of Surgery, Leonard M. Miller School of Medicine, University of Miami, Miami, FL, United States
Editorial on the Research Topic
Debates in cardiovascular pharmacology and drug discovery: 2022
Introduction
Cardiovascular diseases (CVDs) are the leading cause of death worldwide. High-throughput metabolomics analysis is a powerful tool in characterizing metabolomic reprogramming related to various diseases in biomedical fields, uncovering the underlying novel metabolic mechanisms, and identifying diagnostic biomarkers (1, 2). Yet, our understanding of the metabolite-based danger-associated molecular patterns (DAMPs) (3, 4) amplified inflammation during CVDs (5) is not fully elucidated. Our Research Topic: Debates in Cardiovascular Pharmacology and Drug Discovery: 2022 at the Frontiers in Cardiovascular Medicine highlighted five papers. Those highlights encompass original research papers and reviews and provide a comprehensive view of drugs and metabolic mechanisms associated with CVDs. In 2023, we will continue to maintain an exceptional platform that fosters the exchange of groundbreaking insights among cardiologists, translational cardiovascular researchers, and experts in cardiovascular pharmacology and drug discovery.
Metabolic reprogramming and trained immunity/inflammation constitute a significant risk factor for the development of cardiovascular diseases
CVDs, for the most part, originate from disturbances in cardiovascular metabolism (6–9). Metabolites are the dynamic feedback of metabolism in cells, tissues, or organisms. They are uniquely positioned in the ‘omics’ hierarchy, representing the terminal products of processes originating from other “upstream levels” such as the genome, epigenome, transcriptome, and proteome. Metabolomics, a cutting-edge technology, has become a valuable tool for studying CVDs by revealing changes in metabolism. Comparing metabolite variations in the presence of pathophysiological conditions offers additional insights into the metabolomic mechanisms underlying the pathogenesis of diseases (2).
The development of CVDs is closely tied to inflammation pathologies. Nevertheless, the precise mechanisms through which metabolic reprogramming promotes inflammation in the context of CVD remain elusive. Earlier publications have indicated that persistent inflammatory metabolic reprogramming of innate immune cells and their bone marrow precursors plays a pivotal role in the onset and progression of CVDs (10). This metabolic reprogramming is associated with the concept of trained immunity (also termed innate immune memory) (2, 11). To be more specific, trained immunity is achieved through metabolic alterations within innate immune cells in response to stimuli. This process involves histone modifications such as methylation and acetylation, resulting in enduring epigenetic changes in inflammation-associated gene promoters and activating four metabolic pathways, including glycolysis, acetyl coenzyme A (acetyl-CoA) generation, mevalonate-cholesterol synthesis, and glutaminolysis (5). Innate immune cells that have undergone this “training” and developed stimuli-non-specific memories exhibit more robust responses when faced with the potential for re-stimulation (12).
Nevertheless, a significant question that remains is: how do different CVDs simultaneously and uniformly reprogram all four metabolic pathways? A recent publication has revealed that during early hyperlipidemia-induced atherosclerosis, three distinct types of trained immunity coexist. Each of these trained immunity types is characterized by specific mechanisms, including acetyl-CoA-cholesterol-driven histone acetylation dependence, S-adenosylhomocysteine (SAH) hypomethylation-triggered histone demethylation dependence, and glycolysis-independent metabolic pathways (2). These concurrent forms of trained immunity collectively play a pivotal role in exacerbating inflammation (13–20) and driving the progression of atherosclerosis (2, 21). In addition, this paper clearly showed that metabolomic reprogramming exhibits pronounced specificity at the tissue and subcellular organelle levels (22, 23). It is noteworthy that a significant number of upregulated metabolites are prominently expressed within the mitochondria of the heart. This underscores the elevated energy demand (24) associated with the initial stages of atherosclerosis in the cardiac tissue (2).
Five highlights of our research topic relate to therapeutic studies in metabolic reprograming, inflammation, and trained immunity
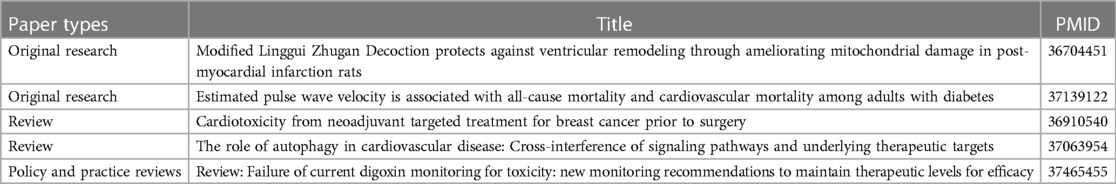
Metabolomics plays a crucial role in delineating pathophysiological responses and identifying markers for potential drug candidates. As we mentioned above, mitochondria (25) play a major role in the process of atherosclerosis, and a similar result was also reported by Xiang et al. in myocardial infarction (MI). Xiang’s group investigated a traditional Chinese medicine called Modified Linggui Zhugan Decoction (MLZD), which protects against MI by improving mitochondrial functions and reversing ventricular remodeling (26). In addition, Wu et al. examined the association of estimated pulse wave velocity with all causes and cardiovascular mortality in patients with diabetes (27). Jiang et al. comprehensively summarized the signaling pathway of cross-interference between autophagy and different types of CVDs (28). Our research topic not only emphasizes the investigation of underlying mechanisms but also provides comprehensive reviews of cardiovascular damage resulting from drug toxicities. Liu et al. conducted a review that centered on targeted drug toxicity affecting the heart in the context of breast cancer (29), whereas Gona et al. delved into the subject of cardiovascular toxicity in relation to digoxin (30).
We listed these five key highlights in Table 1, and we are confident that the articles within our research topic offer fresh perspectives on metabolomic reprogramming associated with CVDs. This reprogramming presents therapeutic targets and drug toxicities for treating a variety of disease conditions, including as metabolic CVDs, diabetes, and breast cancer. It also enables conceptual innovation of trained immunity and disease progression.
Author contributions
KX: Writing – original draft. FS: Writing – review & editing. YS: Writing – review & editing. YL: Writing – review & editing. XJ: Writing – review & editing. SW: Writing – review & editing. JS: Writing – review & editing. FS: Writing – review & editing. LM: Writing – review & editing. RV: Writing – review & editing. HW: Writing – review & editing. PY: Supervision, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Du F, Virtue A, Wang H, Yang XF. Metabolomic analyses for atherosclerosis, diabetes, and obesity. Biomark Res. (2013) 1:17. doi: 10.1186/2050-7771-1-17
2. Xu K, Saaoud F, Shao Y, Lu Y, Wu S, Zhao H, et al. Early hyperlipidemia triggers metabolomic reprogramming with increased SAH, increased acetyl-CoA-cholesterol synthesis, and decreased glycolysis. Redox Biol. (2023) 64:102771. doi: 10.1016/j.redox.2023.102771
3. Shao Y, Nanayakkara G, Cheng J, Cueto R, Yang WY, Park JY, et al. Lysophospholipids and their receptors serve as conditional DAMPs and DAMP receptors in tissue oxidative and inflammatory injury. Antioxid Redox Signaling. (2018) 28(10):973–86. doi: 10.1089/ars.2017.7069
4. Wang X, Li YF, Nanayakkara G, Shao Y, Liang B, Cole L, et al. Lysophospholipid receptors, as novel conditional danger receptors and homeostatic receptors modulate inflammation-novel paradigm and therapeutic potential. J Cardiovasc Transl Res. (2016) 9:343–59. doi: 10.1007/s12265-016-9700-6
5. Ct D, Saaoud F, Shao Y, Sun Y, Xu K, Lu Y, et al. Trained immunity and reactivity of macrophages and endothelial cells. Arterioscler Thromb Vasc Biol. (2021) 41:1032–46. doi: 10.1161/ATVBAHA.120.315452
6. McGarrah RW, Crown SB, Zhang GF, Shah SH, Newgard CB. Cardiovascular metabolomics. Circ Res. (2018) 122:1238–58. doi: 10.1161/CIRCRESAHA.117.311002
7. Griffin JL, Atherton H, Shockcor J, Atzori L. Metabolomics as a tool for cardiac research. Nat Rev Cardiol. (2011) 8:630–43. doi: 10.1038/nrcardio.2011.138
8. Lim RMH, Koh AS. Cardiovascular aging and physical activity: insights from metabolomics. Front Cardiovasc Med. (2021) 8:728228. doi: 10.3389/fcvm.2021.728228
9. Iliou A, Mikros E, Karaman I, Elliott F, Griffin JL, Tzoulaki I, et al. Metabolic phenotyping and cardiovascular disease: an overview of evidence from epidemiological settings. Heart. (2021) 107:1123–9. doi: 10.1136/heartjnl-2019-315615
10. Bahrar H, Bekkering S, Stienstra R, Netea MG, Riksen NP. Innate immune memory in cardiometabolic disease. Cardiovasc Res. (2023):cvad030. doi: 10.1093/cvr/cvad030 [Epub ahead of print].36795085
11. Netea MG, Dominguez-Andres J, Barreiro LB, Chavakis T, Divangahi M, Fuchs E, et al. Defining trained immunity and its role in health and disease. Nat Rev Immunol. (2020) 20:375–88. doi: 10.1038/s41577-020-0285-6
12. Xu K, Zhang Y, Saaoud F, Shao Y, Lu Y, Jiang X, et al. Editorial: insights in cardiovascular therapeutics 2022-cardiovascular innate immunity. Front Cardiovasc Med. (2023) 10:1184030. doi: 10.3389/fcvm.2023.1184030
13. Li X, Fang P, Sun Y, Shao Y, Yang WY, Jiang X, et al. Anti-inflammatory cytokines IL-35 and IL-10 block atherogenic lysophosphatidylcholine-induced, mitochondrial ROS-mediated innate immune activation, but spare innate immune memory signature in endothelial cells. Redox Biol. (2020) 28:101373. doi: 10.1016/j.redox.2019.101373
14. Lu Y, Sun Y, Ct D, Nanayakkara GK, Shao Y, Saaoud F, et al. Increased acetylation of H3K14 in the genomic regions that encode trained immunity enzymes in lysophosphatidylcholine-activated human aortic endothelial cells – novel qualification markers for chronic disease risk factors and conditional DAMPs. Redox Biol. (2019) 24:101221. doi: 10.1016/j.redox.2019.101221
15. Lu Y, Sun Y, Saaoud F, Shao Y, Xu K, Jiang X, et al. ER Stress mediates angiotensin II-augmented innate immunity memory and facilitates distinct susceptibilities of thoracic from abdominal aorta to aneurysm development. Front Immunol. (2023) 14:1268916. doi: 10.3389/fimmu.2023.1268916
16. Lu Y, Sun Y, Xu K, Saaoud F, Shao Y, Ct D, et al. Aorta in pathologies may function as an immune organ by upregulating secretomes for immune and vascular cell activation, differentiation and trans-differentiation-early secretomes may serve as drivers for trained immunity. Front Immunol. (2022) 13:858256. doi: 10.3389/fimmu.2022.858256
17. Fagenson AM, Xu K, Saaoud F, Nanayakkara G, Jhala NC, Liu L, et al. Liver ischemia reperfusion injury, enhanced by trained immunity, is attenuated in caspase 1/caspase 11 double gene knockout mice. Pathogens. (2020) 9(11):879. doi: 10.3390/pathogens9110879
18. Drummer CIV, Saaoud F, Sun Y, Atar D, Xu K, Lu Y, et al. Hyperlipidemia may synergize with hypomethylation in establishing trained immunity and promoting inflammation in NASH and NAFLD. J Immunol Res. (2021) 2021:3928323. doi: 10.1155/2021/3928323
19. Shao Y, Saaoud F, Cornwell W, Xu K, Kirchhoff A, Lu Y, et al. Cigarette smoke and morphine promote treg plasticity to Th17 via enhancing trained immunity. Cells. (2022) 11(18):2810. doi: 10.3390/cells11182810
20. Yang Q, Zhang R, Tang P, Sun Y, Johnson C, Saredy J, et al. Ultrasound may suppress tumor growth, inhibit inflammation, and establish tolerogenesis by remodeling innatome via pathways of ROS, immune checkpoints, cytokines, and trained immunity/tolerance. J Immunol Res. (2021) 2021:6664453. doi: 10.1155/2021/6664453
21. Zhong C, Yang X, Feng Y, Yu J. Trained immunity: an underlying driver of inflammatory atherosclerosis. Front Immunol. (2020) 11:284. doi: 10.3389/fimmu.2020.00284
22. Yang Q, Nanayakkara GK, Drummer C, Sun Y, Johnson C, Cueto R, et al. Low-Intensity ultrasound-induced anti-inflammatory effects are mediated by several new mechanisms including gene induction, immunosuppressor cell promotion, and enhancement of exosome biogenesis and docking. Front Physiol. (2017) 8:818. doi: 10.3389/fphys.2017.00818
23. Liu M, Wu N, Xu K, Saaoud F, Vasilopoulos E, Shao Y, et al. Organelle crosstalk regulators are regulated in diseases, tumors, and regulatory T cells: novel classification of organelle crosstalk regulators. Front Cardiovasc Med. (2021) 8:713170. doi: 10.3389/fcvm.2021.713170
24. Ct D, Saaoud F, Jhala NC, Cueto R, Sun Y, Xu K, et al. Caspase-11 promotes high-fat diet-induced NAFLD by increasing glycolysis, OXPHOS, and pyroptosis in macrophages. Front Immunol. (2023) 14:1113883. doi: 10.3389/fimmu.2023.1113883
Keywords: metabolomics, cardiovascular diseases, cardiovascular injuries, inflammation, trained immunity
Citation: Xu K, Saaoud F, Shao Y, Lu Y, Jiang X, Wu S, Sun J, Fernades Conti F, Martinez L, Vazquez-Padron R, Wang H and Yang X (2023) Editorial: Debates in cardiovascular pharmacology and drug discovery: 2022. Front. Cardiovasc. Med. 10:1304680. doi: 10.3389/fcvm.2023.1304680
Received: 29 September 2023; Accepted: 9 October 2023;
Published: 18 October 2023.
Edited and Reviewed by: Masanori Aikawa, Harvard Medical School, United States
© 2023 Xu, Saaoud, Shao, Lu, Jiang, Wu, Sun, Fernades Conti, Martinez, Vazquez-Pedron, Wang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaofeng Yang xfyang@temple.edu
 Keman Xu
Keman Xu Fatma Saaoud
Fatma Saaoud Ying Shao
Ying Shao Yifan Lu
Yifan Lu Xiaohua Jiang1,2
Xiaohua Jiang1,2 Sheng Wu
Sheng Wu Jianxin Sun
Jianxin Sun Filipe Fernades Conti
Filipe Fernades Conti Laisel Martinez
Laisel Martinez Roberto Vazquez-Padron
Roberto Vazquez-Padron Hong Wang
Hong Wang Xiaofeng Yang
Xiaofeng Yang