
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 02 November 2023
Sec. Atherosclerosis and Vascular Medicine
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1295718
This article is part of the Research Topic Case Reports in Atherosclerosis and Vascular Medicine: 2023 View all 7 articles
 Yuichi Tamura1,2*
Yuichi Tamura1,2* Sayamaa Lkhagvadorj3
Sayamaa Lkhagvadorj3 Yudai Tamura1
Yudai Tamura1 Asuka Furukawa1
Asuka Furukawa1 Shinsuke Aida4
Shinsuke Aida4 Hirotoshi Ebinuma5
Hirotoshi Ebinuma5 Takayuki Shiomi3
Takayuki Shiomi3
Background: This study investigates the pulmonary arterial histopathology in patients with idiopathic pulmonary arterial hypertension (IPAH) and acute vasoreactive phenotype, who demonstrated long-term survival (>30 years) and incidental death from causes other than PAH progression. The pathological changes observed in these patients were compared with those in patients with bone morphogenetic protein receptor type 2 (BMPR2) mutation.
Case Presentation: We present two cases of patients with pulmonary arterial hypertension (PAH) who died incidentally from causes unrelated to PAH progression. We report compares pulmonary arterial histopathology in long-term survivors of CCB-responsive PAH patient and a hereditary PAH patient with a BMPR2 mutation. Lung specimens were analyzed using the Heath and Edwards (HE) classification and percentage muscular wall thickness (%MWT) of pulmonary arterioles. A significant difference in the severity of grading (p = 0.0001) and distribution between grades 1-2, 4 (p = 0.001), and 5 (p = 0.014) was observed between both patients. These findings suggest differential vascular pathology between the two cases, with CCB responders displaying more mild illness lesions compared to BMPR2 mutant patients.
Conclusion: The study revealed that CCB responders exhibit more mild illness vascular lesions than BMPR2 mutant patients despite their long-term survival, suggesting a difference in vascular pathology between the two phenotypes.
Acute vasoreactive phenotype has a prevalence of 12.5% among patients with idiopathic pulmonary arterial hypertension (IPAH), with 6.8% of patients showing long-term improvement with calcium channel blockers (CCBs); patients who respond to CCBs are reported to have long-term survival, with an average 7-year survival rate of 97% under favorable hemodynamics and mild pathologic vascular degeneration in their pulmonary arteries (1). There has been a lack of information on vascular pathology in cases of ultra-long-term survivors of more than 30 years.
This study evaluated the pathological changes in the pulmonary arteries of patients with stable pulmonary arterial hypertension (PAH) who incidentally died from causes other than PAH progression 34 years after onset. Compared to the pulmonary histopathology of PAH patients with bone morphogenetic protein receptor type 2 (BMPR2) mutation who also survived for a long time and died incidentally, most pathological manifestations in CCB responders reported in this study were mild illness lesions, even in cases with a very long survival period.
Case 1 was a 64-year-old woman. She was diagnosed with IPAH at 30 years of age following pregnancy. Her initial hemodynamic evaluation revealed that she had presented a 35-mmHg mPAP, 3.90-L/min CO, 7.18 Wood's-Units PVR, and presented responsiveness to CCB. Therefore, she was managed with high-dose CCB monotherapy for the first 20 years. Sequential additions of an endothelin receptor antagonist and a PDE-5 inhibitor to improve PH management stabilized her hemodynamic status in the last 14 years. The last hemodynamic evaluation was performed at 64 years of age and showed a 37-mmHg mPAP, 6.08-L/min CO, 3.62 Wood's-Units PVR, and NYHA Class II. The patient subsequently died at 64 years of age due to complications of infective endocarditis and sepsis triggered by a urinary tract infection, but she had never been hospitalized for right heart failure 34 years since PAH onset.
Case 2 was a 58-year-old man who was diagnosed with hereditary PAH associated with a BMPR2 nonsense-mutation at 46 years of age. He was treated with triple combination therapy, including continuous intravenous epoprostenol. His last hemodynamic evaluation was performed at 56 years of age, with a 53-mmHg mPAP, 4.37-L/min CO, 10.5 Wood's-Units PVR, and NYHA Class III. There were no further worsening PAH events, including right heart failure, but at the age of 57 years, he was diagnosed with colorectal cancer with multiple inoperable metastases and subsequently died at 58 years of age.
The lung specimens of two patients were fixed in formalin from both lungs during autopsy. Twelve tissue sections from each patient were embedded in paraffin, sectioned (each section was 3-µm thick), and stained with hematoxylin & eosin and elastin van gienson stain to determine the detailed morphologic structures. Pulmonary arterial and arteriole characteristics were examined under NanoZoomer NDP views 2 software (Hamamatsu, Tokyo, Japan) and graded from 1 to 6 according to the histologic Heath and Edwards (HE) classification (2).
The degree of pulmonary arterioles musculization was determined by measuring percentage muscular wall thickness (%MWT). The %MWT of small pulmonary arterioles between 20 and 50 µm in diameter was calculated as follows: %MWT = (2 × MWT/external diameter) ×100 (3). MWT was measured in the same direction as the external diameter on both sides of circular arterioles with a constant circumferential wall thickness, and two measurements were averaged to obtain the final value.3 Statistical analysis was performed using PASW version 21.0 (SPSS Inc., Chicago, IL, USA). Categorical variables are expressed as a frequency or percentage, the Chi-squared test was used for comparisons, and the Mann-Whitney post-hoc test was used to determine individual grade differences between patients. For continuous variables, which are expressed as mean ± standard deviation and were compared using a non-parametric Student's t-test, a p-value <0.05 was considered statistically significant.
According to the histologic HE classification, a statistically significant difference in the severity of grading (p = 0.0001; Figure 1A) and a distribution difference between grades 1-2, 4 (p = 0.001), and 5 (p = 0.014) were observed between both patients. In the CCB responder, the vessels presented mostly mild illness changes and a predominance of grade 2, showing medial hypertrophy (Figures 2A,B). However, in the BMPR 2 mutant case, an irreversible grade 4 was predominant, along with a worsening grade 5 (Figures 2C,D).
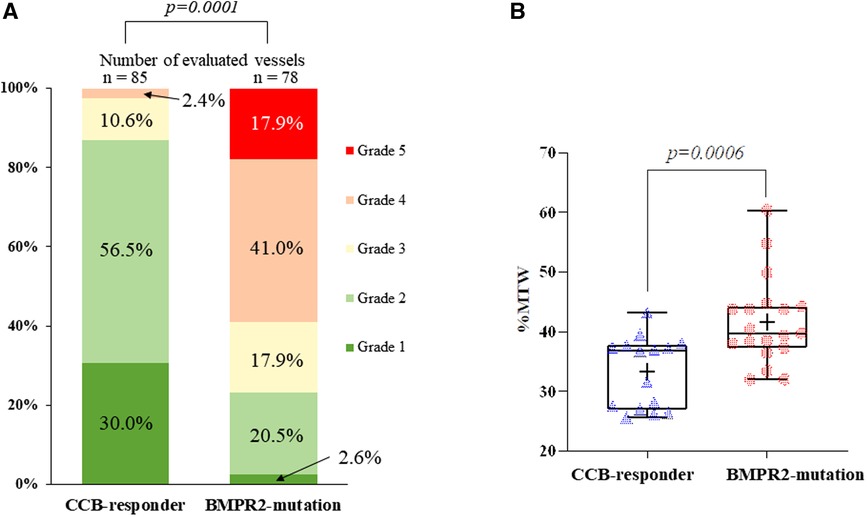
Figure 1. Comparison of histomorphological measurements. (A) According to the Heath and Edwards classification, the corresponding percentage for each grade (grades 1–6) in two cases is shown. No vascular changes were assessed as grade 6. There was a statistically significant difference in the severity and distribution of grading between cases (p = 0.0001). (B) The Box-and-Whisker diagram indicates the comparison of the percentage media wall thickness (%MWT) between case, with statistically significant differences (p = 0.0006). The box shows the interquartile range, with the median value indicated by the horizontal line; the mean value is indicated by (+); symbols indicate outliers.
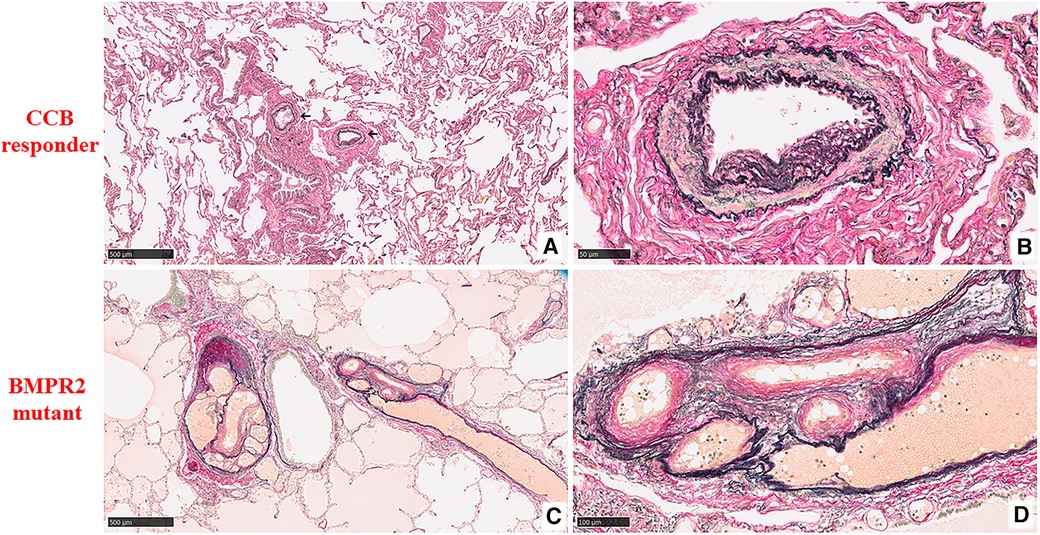
Figure 2. Histopathological findings of pulmonary arteries and arterioles by the heath and edwards classification (elastin van gienson stain). (A) At low magnification, two muscular arteries surrounding the bronchial tree are seen (marked with a black arrow) in the CCB responder. The remaining lung parenchyma is unremarkable (5×). (B) At high magnification, those pulmonary muscular arteries show medial hypertrophy with intimal cellular proliferation, which is classified as grade 2 (40×). (C) At low magnification, two muscular arteries on the right and left of the bronchiole are dilated and form an angiomatoid lesion in the BMPR2 mutant (5×). (D) At higher magnification, an oblique section of these formations is composed of several thin blood vascular structures having a wall of simple elastic tissue and medial and intimal fibroses, which are classified as grade 5 (20×).
Small arterioles (20–50 μm in diameter) were measured, with an average vessel number of 17 ± 2. The mean external diameter was 39.6 ± 8.07 and 32.7 ± 7.5 µm in patients 1 and 2, respectively, and mean medial wall thickness was 6.5 ± 1.7 and 6.7 ± 1.8 µm. %MWT in the BMPR2 mutant (41.6% ± 7.3%) was significantly higher (p = 0.0006) than in the CCB responder (33.3% ± 5.9%) (Figure 1B).
From the contrastive analysis of these two cases, we demonstrated that most pulmonary arteries in CCB responders with IPAH remain mild illness lesions with an HE classification of grade ≤3, regardless of whether the duration of IPAH is more than 30 years. In contrast, patients with BMPR2-positive IPAH show more irreversible lesions with an HE classification of grade 4–5, despite not reaching the end-stage of PH.
Hemins et al. have shown that the pathophysiology of CCB responders is related to Wnt/β-catenin signaling and intercellular adhesion based on their examination of RNA expression patterns (4). This suggests that pathophysiological differences exist between responder and nonresponder IPAH, which is characterized by BMP signaling abnormalities, resulting in vascular endothelial cell damage and vascular smooth muscle proliferation (5).
It has long been expected that the main lesions in CCB responder patients are localized in the smooth muscle cell layer of pre-capillaries since the administration of vasodilating agents rapidly decreases pulmonary vascular resistance. Pathological reports in young CCB responder patients have also shown only the medial hypertrophy of pulmonary arteries (6). Additionally, the only systematic pathology report suggested that CCB-responding PAH is characterized by a decreased number of vascular endothelial degenerations compared to non-CCB responding PAH (7). The present report illustrates the different long-term pathological characteristics of CCB responders, suggesting that different background mechanisms prevent irreversible degeneration of pulmonary vessels over a long period of time (≥30 years). Therefore, it can be expected that CCB responder patients can avoid irreversible changes in pulmonary arteries for a long period of time through continued appropriate treatment by not activating the remodeling signal.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by institutional Ethics Committee at the International University of Health and Welfare. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
YT: Conceptualization, Funding acquisition, Methodology, Resources, Writing – original draft. SL: Data curation, Investigation, Writing – original draft. YT: Resources, Writing – original draft. AF: Investigation, Writing – original draft. SA: Investigation, Writing – review & editing. HE: Conceptualization, Resources, Writing – review & editing. TS: Conceptualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was funded by the Japan Agency for Medical Research and Development (AMED) under Grant no. JP21ek0109567.
The authors wish to acknowledge Rika Takeyasu and Hiromi Takada who helped coordinate the clinical care and data collection during transitions. And the authors appreciated the participated patient in our study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
PAH, pulmonary arterial hypertension; IPAH, idiopathic pulmonary arterial hypertension; CCB, calcium channel blockers; BMPR2, bone morphogenetic protein receptor type 2; HE classification, Heath-Edwards classification.
1. Sitbon O, Humbert M, Jaïs X, Ioos V, Hamid AM, Provencher S, et al. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation. (2005) 111:3105–11. doi: 10.1161/CIRCULATIONAHA.104.488486
2. Heath D, Edwards JE. The pathology of hypertensive pulmonary vascular disease; a description of six grades of structural changes in the pulmonary arteries with special reference to congenital cardiac septal defects. Circulation. (1958) 18:533–47. doi: 10.1161/01.CIR.18.4.533
3. Davey M, Shegu S, Danzer E, Ruchelli E, Adzick S, Flake A, et al. Pulmonary arteriole muscularization in lambs with diaphragmatic hernia after combined tracheal occlusion/glucocorticoid therapy. Am J Obstet Gynecol. (2007) 197(381):e1–381.e7. doi: 10.1016/j.ajog.2007.06.061
4. Hemnes AR, Zhao M, West J, Newman JH, Rich S, Archer SL, et al. Critical genomic networks and vasoreactive variants in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med. (2016) 194:464–75. doi: 10.1164/rccm.201508-1678OC
5. Guignabert C, Humbert M. Targeting transforming growth factor-β receptors in pulmonary hypertension. Eur Respir J. (2021) 57:2002341. doi: 10.1183/13993003.02341-2020
6. Satyanarayana Rao BN, Moller JH, Edwards JE. Primary pulmonary hypertension in a child. Response to pharmacologic agents. Circulation. (1969) 40(4):583–7. doi: 10.1161/01.CIR.40.4.583
Keywords: pulmonary arterial hypertension, calcium channel blockers, long term survivor, pathophysiology, pathology
Citation: Tamura Y, Lkhagvadorj S, Tamura Y, Furukawa A, Aida S, Ebinuma H and Shiomi T (2023) Case report: Pathological differences in pulmonary arterial hypertension in long-term responders to calcium channel blockers. Front. Cardiovasc. Med. 10:1295718. doi: 10.3389/fcvm.2023.1295718
Received: 17 September 2023; Accepted: 16 October 2023;
Published: 2 November 2023.
Edited by:
Nobuhiro Tahara, School of Medicine, Kurume University, Japan© 2023 Tamura, Lkhagvadorj, Tamura, Furukawa, Aida, Ebinuma and Shiomi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuichi Tamura dGFtdXJhLnUxQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.