- 1Department of Cardiology and Critical Care, Asklepios Clinic St. Georg, Hamburg, Germany
- 2Asklepios ProResearch, Hamburg, Germany
- 3DZHK (German Centre for Cardiovascular Research), Partner Site Hamburg/Kiel/Luebeck, Hamburg, Germany
- 4Department of Cardiac Surgery, Asklepios Clinic St. Georg, Hamburg, Germany
- 5Department of Emergency Medicine, Asklepios Clinic St. Georg, Hamburg, Germany
- 6Department of Anaesthesiology and Critical Care, Asklepios Clinic St. Georg, Hamburg, Germany
- 7Department of Cardiology and Critical Care, Asklepios Clinic Altona, Hamburg, Germany
- 8Semmelweis-University, Budapest, Hungary
Introduction: The use of venoarterial extracorporeal membrane oxygenation (VA-ECMO) in extracorporeal cardiopulmonary resuscitation (eCPR) has emerged as a treatment option for selected patients who are experiencing refractory cardiac arrest (CA). In the light of increasing availability, the analyses of outcome-relevant predisposing characteristics are of growing importance. We evaluated the prognostic influence of gender in patients presenting with out-of-hospital cardiac arrest (OHCA) treated with eCPR.
Methods: We retrospectively analysed the data of 377 consecutive patients treated for OHCA using eCPR in our cardiac arrest centre from January 2016 to December 2022. The primary outcome was defined as the survival of patients until they were discharged from the hospital, with a favourable neurological outcome [cerebral performance category (CPC) score of ≤2]. Statistical analyses were performed using baseline comparison, survival analysis, and multivariable analyses.
Results: Out of the 377 patients included in the study, 69 (21%) were female. Female patients showed a lower prevalence rate of pre-existing coronary artery disease (48% vs. 75%, p < 0.001) and cardiomyopathy (17% vs. 34%, p = 0.01) compared with the male patients, while the mean age and prevalence rate of other cardiovascular risk factors were balanced. The primary reason for CA differed significantly (female: coronary event 45%, pulmonary embolism 23%, cardiogenic shock 17%; male: coronary event 70%, primary arrhythmia 10%, cardiogenic shock 10%; p = 0.001). The prevalence rate of witnessed collapse (97% vs. 86%; p = 0.016) and performance of bystander CPR (94% vs. 85%; p = 0.065) was higher in female patients. The mean time from collapse to the initiation of eCPR did not differ between the two groups (77 ± 39 min vs. 80 ± 37 min; p = 0.61). Overall, female patients showed a higher percentage of neurologically favourable survival (23% vs. 12%; p = 0.027) despite a higher prevalence of procedure-associated bleeding complications (33% vs. 16%, p = 0.002). The multivariable analysis identified a shorter total CPR duration (p = 0.001) and performance of bystander CPR (p = 0.03) to be associated with superior neurological outcomes. The bivariate analysis showed relevant interactions between gender and body mass index (BMI).
Conclusion: Our analysis suggests a significant survival benefit for female patients who obtain eCPR, possibly driven by a higher prevalence of witnessed collapse and bystander CPR. Interestingly, the impact of patient age and BMI on neurologically favourable outcome was higher in female patients than in male patients, warranting further investigation.
1 Introduction
Out-of-hospital cardiac arrest (OHCA) is one of the leading causes of death in Europe, with an incidence rate ranging from 67 to 170 per 100,000 person-years and persistently low rates of survival (1). Recently, extracorporeal cardiopulmonary resuscitation (eCPR) has emerged as a treatment option for refractory cardiac arrest (CA). Albeit recently published randomised controlled trials have displayed variable results, the number of cases and medical centres adopting eCPR therapy has increased rapidly, possibly driven by reports of favourable outcomes in retrospective analyses and the positive results of the ARREST trial (2–5). However, patient selection seems to be of incremental importance, given the highly invasive nature and the consecutive risk for complications, as well as the considerably high demand in personnel and resources of this treatment option (6).
Although certain factors, such as witnessed cardiac arrest, short overall resuscitation duration, and refractory ventricular fibrillation, have been identified as having a positive effect on outcome measures, the impact of gender on these measures remains unclear. Two-thirds of cardiac arrest patients are male. Nonetheless, female patients remain underrepresented in the current randomised controlled trials, with only 17% of the participants being of female gender in the ARREST and Prague OHCA studies (2, 3). Studies have suggested that women exhibit overall lower survival rates and worse neurological outcomes after conventional CPR for CA compared with men (7–9). When analysing women of reproductive age, these effects seem to be suspended, with favourable outcomes reported in this collective (10). Whether these gender differences exist in the context of eCPR remains widely unknown, with only limited data available reporting inconsistent results (11, 12). We aimed to assess the impact of gender on outcomes in a diverse group of patients treated with eCPR for OHCA at our cardiac arrest centre.
2 Methods
2.1 Patient selection
We present retrospective data obtained from a single-centre registry of patients treated with eCPR for refractory OHCA at the Cardiac Arrest Center (CAC) of the Asklepios Clinic St. Georg (Hamburg, Germany). During the period of the analysis, spanning from January 2016 to December 2022, a total of 377 patients were treated with VA-ECMO at our centre. Excluding 47 patients with a significant amount of missing data, the study focused on 330 cases of patients treated with eCPR for OHCA. The primary outcome was defined as the survival of patients until they were discharged from the hospital with a favourable neurological outcome [cerebral performance category (CPC) score of ≤2]. The secondary outcome was defined as the survival of patients until they were discharged from the hospital, regardless of the CPC scoring. The study protocol was approved by the local ethics committee (2023-300393-WF).
2.2 Statistical analyses
All cases were categorised into gender-specific subgroups depending on their biological gender. The two groups were characterised, and baseline characteristics were compared using Fisher’s exact test, Pearson's chi-squared test, and Wilcoxon rank sum test when applicable. Continuous data were summarised as means ± standard deviations or as medians (25th and 75th percentiles) as appropriate. The categorical data were presented as N (%). Overall survival and survival with good neurological outcome (CPC ≤ 2) were visualised using Kaplan–Meier plots. Regarding the survival endpoint with good neurological outcome, patients who were discharged alive but had demonstrated poor neurological status were assigned the discharge time as the event time.
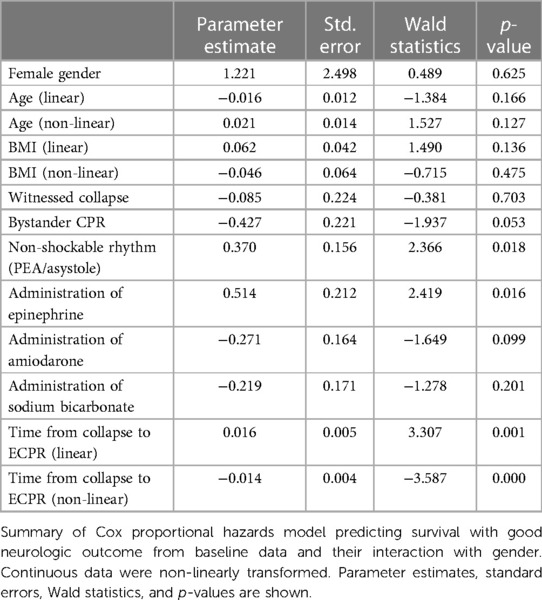
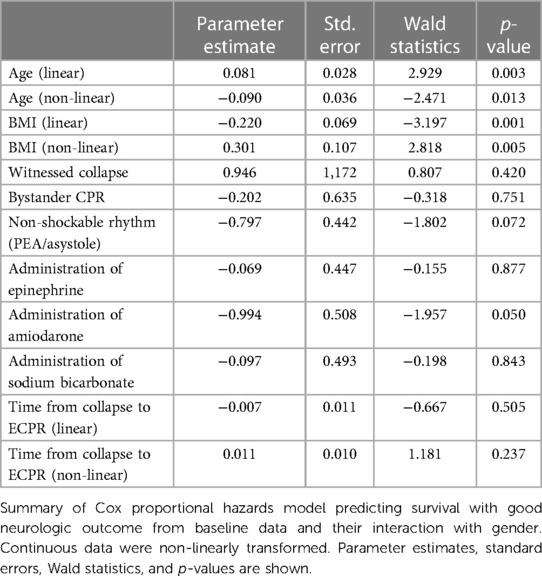
The variables considered in the Cox proportional hazards model for determining survival with good neurological outcome were age, body mass index (BMI), witnessed collapse (yes/no), bystander cardiopulmonary resuscitation (yes/no), initial ECG (VF or VT), the administration of sodium bicarbonate (yes/no), amiodarone, and epinephrine, and the duration from collapse to the initiation of eCPR. The interaction effects between each variable and gender were taken into account. Continuous variables (age, duration to eCPR, BMI) were transformed in advance using restricted cubic spline functions with three knots to consider non-linearity. All model terms were shown with parameter estimates, standard errors, Wald statistics and p-values. The effects on mortality were presented as hazard ratios and 95% confidence intervals. The interactions between gender and BMI and between gender and age were shown using log relative hazard plots and figures presenting model-based survival predictions. All p-values were two-sided, and a p-value < 0.05 was considered significant. All calculations were performed using the statistical analysis software R (R Core Team, 2023).
2.3 eCPR program
Embedded in a tertiary care hospital in the urban area of Hamburg (Germany), our CAC falls back on a long-term experience with VA-ECMO implantation and management with a focus on eCPR. We offer an around-the-clock ECMO service with a specialised intensive care unit, as well as specialised heart failure and chest pain units.
In case of OHCA patients arriving to the emergency department, the interdisciplinary cardiac arrest receiving team (CART) is alerted beforehand. The CART comprises personnel from the departments of interventional cardiology, anaesthesiology, and emergency medicine. Based on the presumed aetiology, other departments are alerted simultaneously. Treatment decision is made upon arrival at a “cardiac arrest fast assessment area” based on the current expert opinion as well as individual criteria with a focus on the avoidance of time delay. Positive indicators for eCPR initiation are witnessed collapse, performance of bystander CPR, no-flow-time of <5 min, low-flow-time of <60 min, age <75 years (y), and shockable initial rhythm. However, the final decision is left to the CART, and no strict criteria for deferral are provided. VA-ECMO implantation is performed in the cardiac catheter laboratory under fluoroscopic guidance. In the absence of contraindications, uni- or bilateral peripheral femoral access is used, and cannulation is performed via Seldinger's technique. To prevent peripheral limb ischaemia, the implantation of a distal perfusion cannula when feasible is the standard practice. Postinterventional further diagnostics include a coronary angiography and an individualised computed tomography. Intensive care management is at the discretion of the intensive care specialist, following the current guidelines for treatment of the underlying medical condition (e.g., cardiogenic shock, acute myocardial infarction, pulmonary embolism), as well as post-resuscitation care (13–15). Cerebral performance category scoring is performed routinely by trained personnel at the time of discharge from the intensive care unit or prior to transfer to a neurological rehabilitation unit.
3 Results
3.1 Patient characteristics
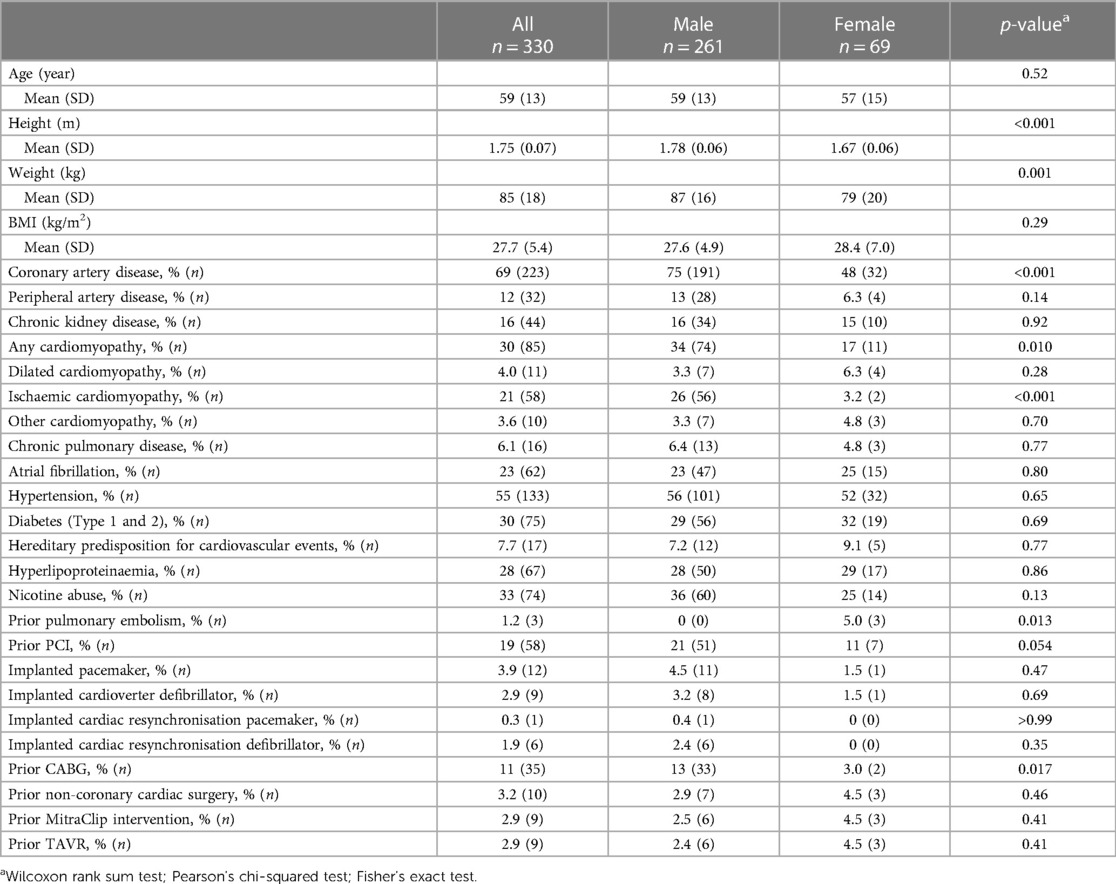
The studied collective was predominantly male (female gender n = 69, 21%). No relevant difference in age was found. Male patients were taller and heavier than female patients, without exhibiting differences in body mass index. Male patients showed a higher prevalence of pre-existing coronary artery disease (CAD) and consecutively higher rates of ischaemic cardiomyopathy (ICM), as well as prior operative myocardial revascularisation. The rates of prior percutaneous coronary interventions (PCI) were higher in male patients as well, although without reaching statistical significance. Female patients on the other hand were seen to have a higher prevalence of prior pulmonary embolism. Prevalence of known cardiovascular risk factors and comorbidities were balanced (Table 1).
3.2 Prehospital data
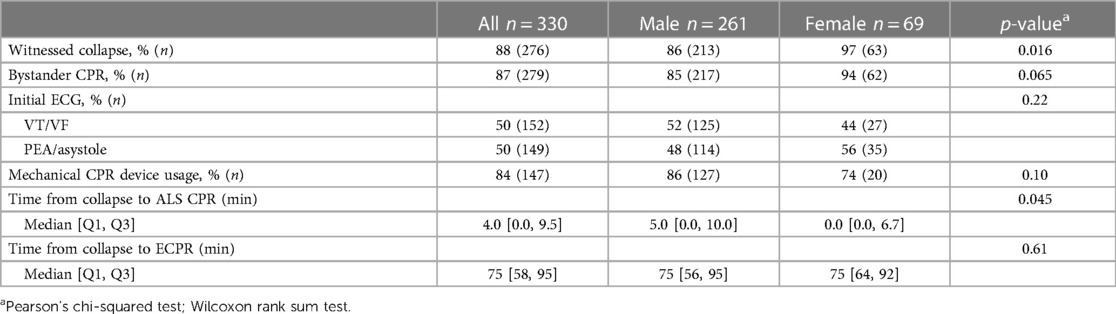
The overall prevalence of witnessed collapse and bystander CPR was high. Initial rhythm was shockable in 50% of the cases. Female patients had consistently higher rates of witnessed collapse and showed a tendency for a higher prevalence of bystander CPR. A shockable rhythm was observed more frequently in male patients, while no overall statistically significant difference was noted. Furthermore, female patients had a shorter time to initiation of advanced life support (ALS) CPR, e.g., the arrival of trained emergency medicine service (EMS) teams. Overall, the median resuscitation duration from collapse to the initiation of eCPR was 75 minutes (min) and did not differ between the gender-specific subgroups (Table 2).
3.3 Procedure data and complications
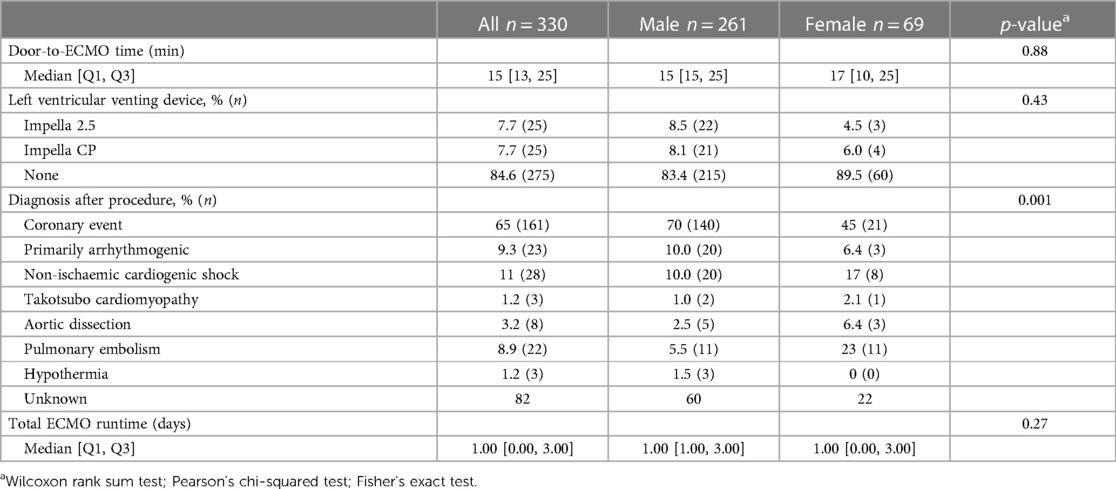
While the primary reason for cardiac arrest in the entire collective and both subgroups was an acute coronary event, this was more pronounced in male patients, with 70% of the cases presenting this presumed aetiology. The prevalence of the acute coronary event in female patients was lower (45%), while the rates of pulmonary embolism where considerably higher in female patients than that in male patients. Other relevant presumed origins of CA were cardiogenic shock and primarily arrhythmogenic. The median door-to-ECMO time was 15 min, and no gender-specific differences were apparent. ECMO implantation was followed-up with primary implantation of an active left ventricular (LV) unloading device in 15% of the cases. Overall, the median ECMO runtime was 1 day and comparable in both subgroups (Table 3).
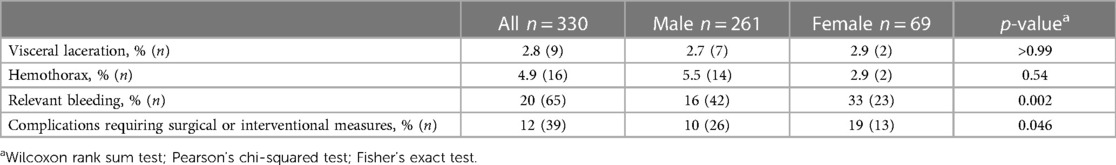
Female patients displayed higher rates of periprocedural bleeding complications compared with male patients, with consequently higher need for interventional and/or surgical measures to treat these adverse events. No difference was seen in other relevant periprocedural complications (Table 4).
3.4 Outcome
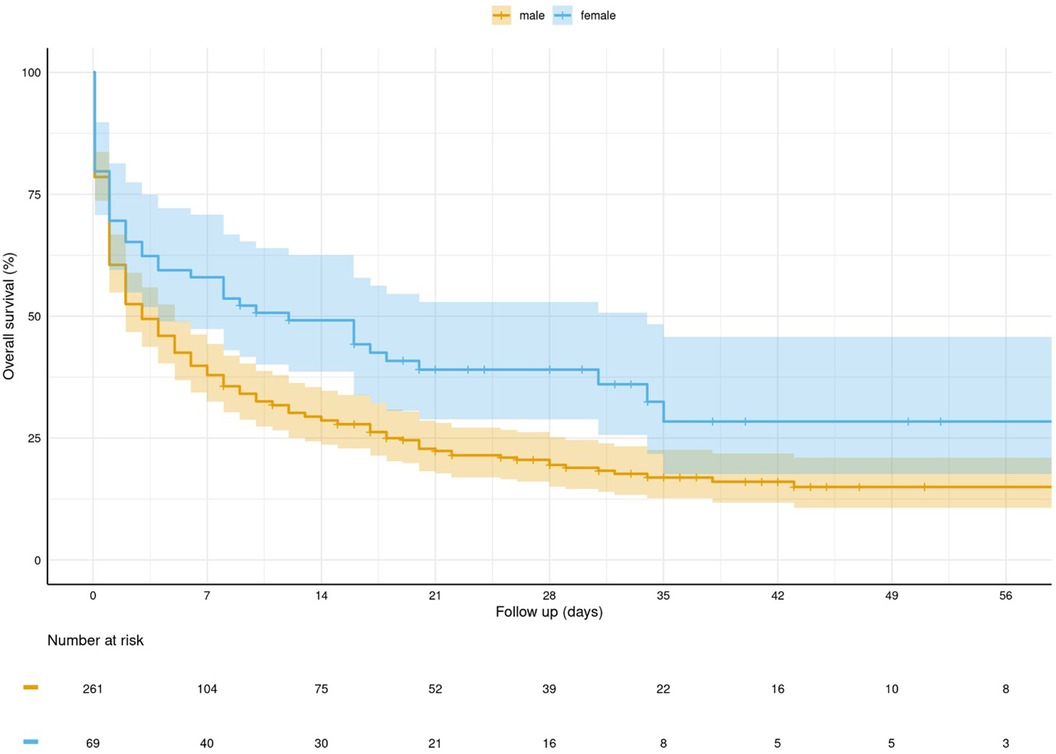
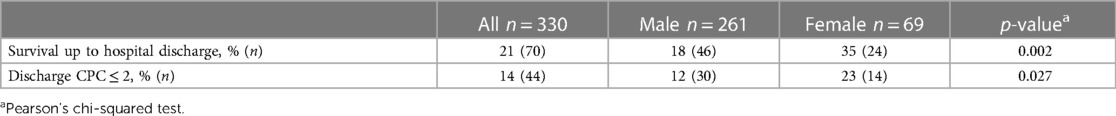
Out of the 330 studied patients, 70 survived up to hospital discharge (21%), and 44 (14%) patients showed favourable neurological outcomes, defined as a CPC score of ≤2. Female patients had significantly higher rates of survival (Figure 1), as well as higher rates of neurologically favourable outcomes at the time of discharge (Table 5, Figure 2).
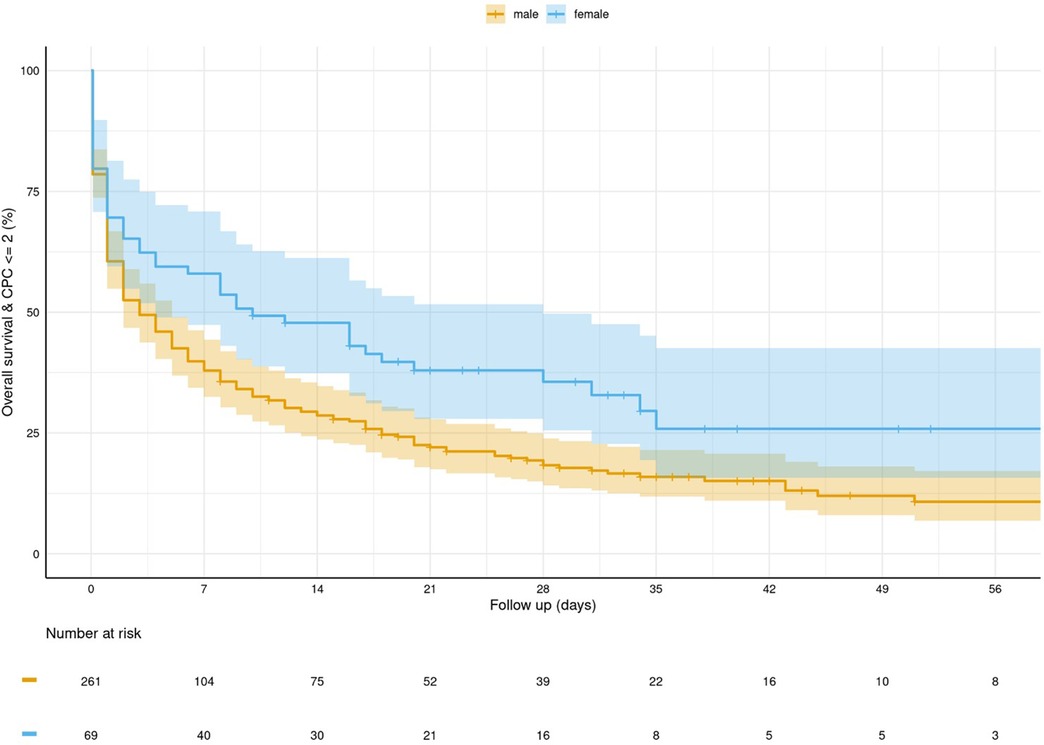
Figure 2. Kaplan–Meier curve for survival and favourable neurological outcome (CPC ≤ 2) stratified by gender.
3.5 Multivariable survival model
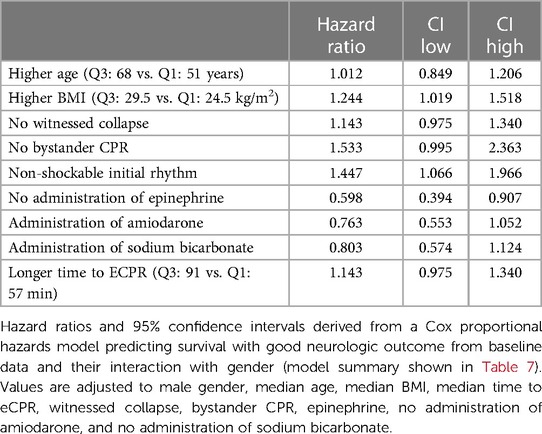
The aggravating influence on adverse outcome was highest for an initially non-shockable rhythm and a higher BMI. Unwitnessed collapse, no performance of bystander CPR, and a longer time from collapse to eCPR initiation showed a tendency for being associated with worse neurological outcomes, without reaching statistical significance. Patients, in whom no epinephrine was administered, were more likely to survive with favourable neurological outcomes (Table 6).
The multivariable analysis revealed time from collapse to eCPR initiation, non-shockable initial rhythm, and administration of epinephrine to be independently associated with outcome, while the effect of age and BMI seemed to be gender dependent (Tables 7, 8).
3.6 Relevant interactions
Relevant interactions between gender and suspected risk factor for an adverse neurological outcome were observed in the case of age and BMI. Female patients exhibited an almost linear increase of risk for adverse neurological outcome with increasing age up to an age of 60 years. In male patients the aforementioned risk was higher at a younger age and decreased slightly with increasing age. Above 60 years of age, the adverse impact of age decreased in female patients and slightly increased in male patients (Figure 3). Hence, the model-based estimates for neurologically favourable survival rates according to age differed between female and male patients (Figure 4).
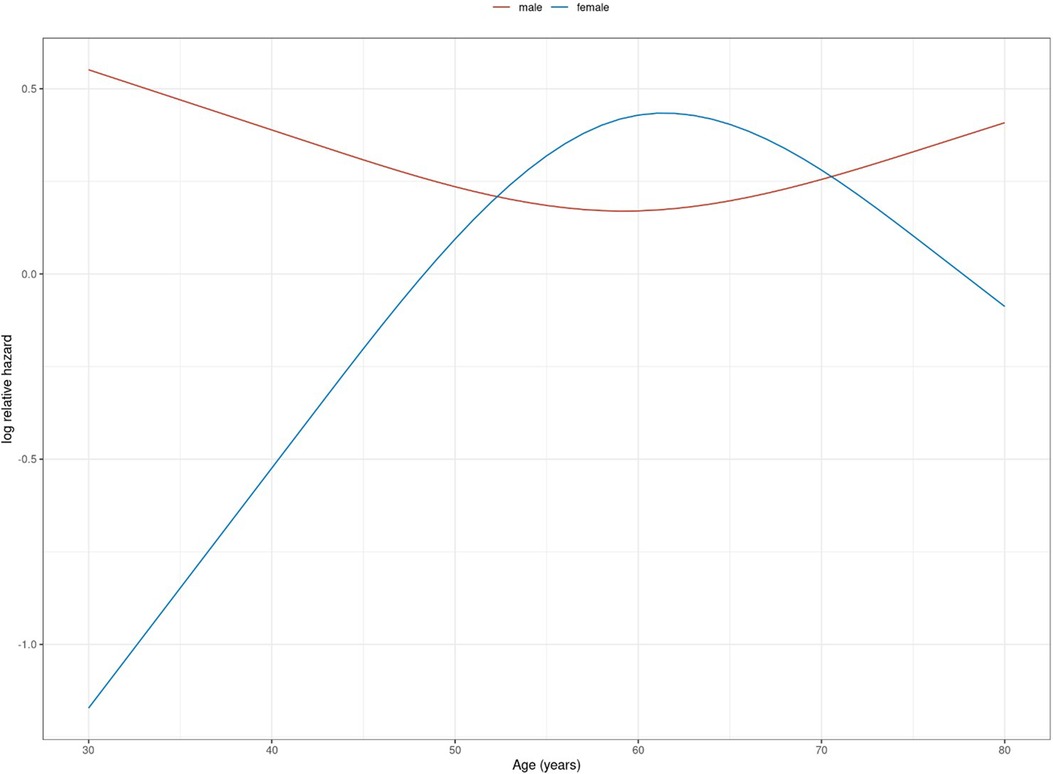
Figure 3. Logarithmic relative hazard for age (in years) on adverse neurological outcome (death or survival with CPC > 2) stratified by gender.
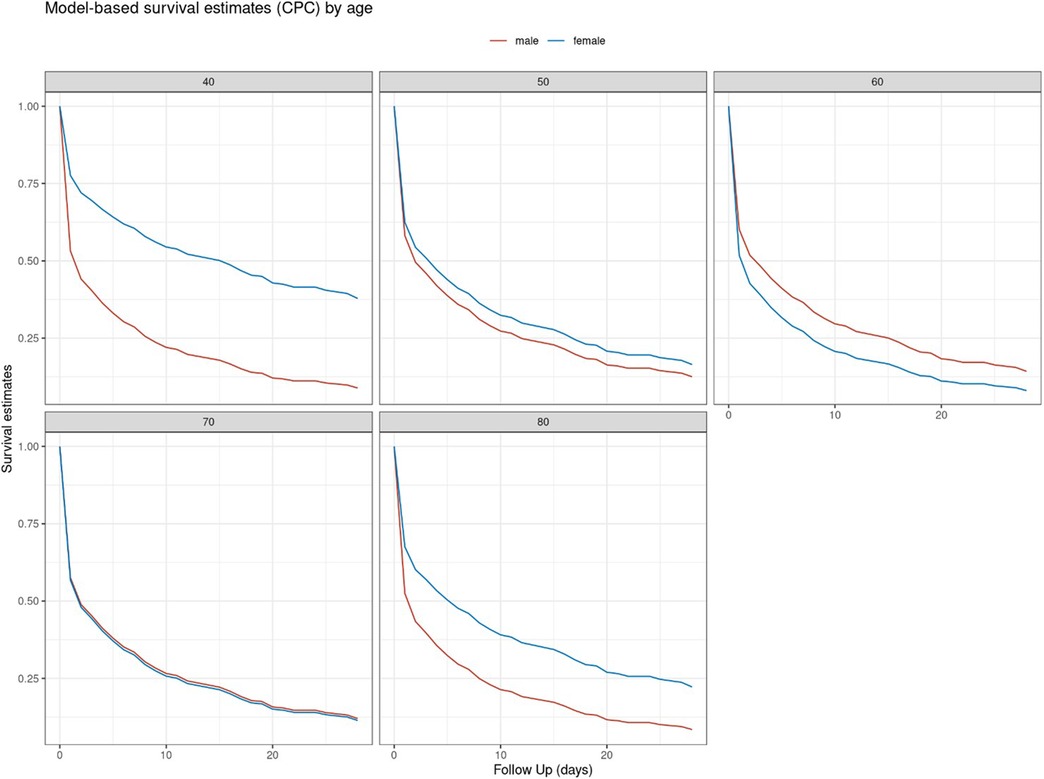
Figure 4. Model-based based estimate for neurologically favourable survival rates (CPC ≤ 2) for selected age values (in years) stratified by gender.
In male patients, the increasing BMI values were associated with an almost linear increase of risk for death or neurologically unfavourable outcomes. In female patients on the other hand, low and high BMI values were equally associated with a higher risk for adverse outcomes, with relevant relative risk reduction in the range of 25–33 kg/m2. Overall, female patients seemed to suffer a higher impact of BMI on adverse outcome than male patients did (Figure 5). The model-based estimates for neurologically favourable survival rates by BMI differed accordingly (Figure 6).
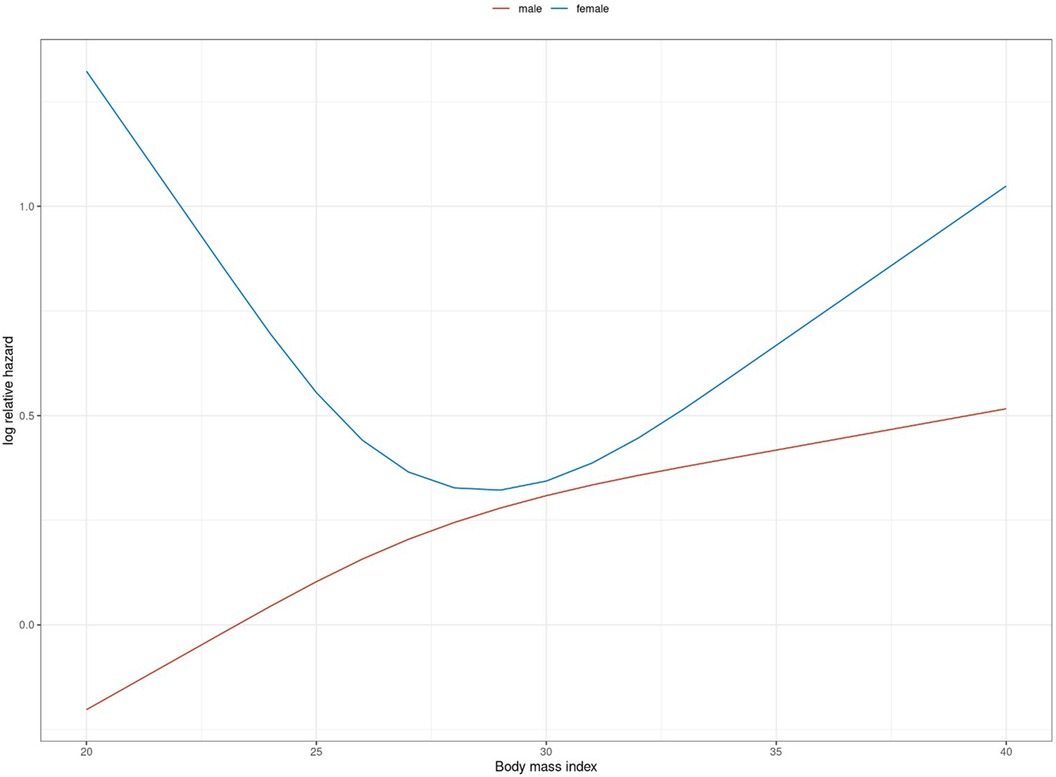
Figure 5. Logarithmic relative hazard for BMI (in kg/m2) on adverse neurological outcome (death or survival with CPC > 2) stratified by gender.
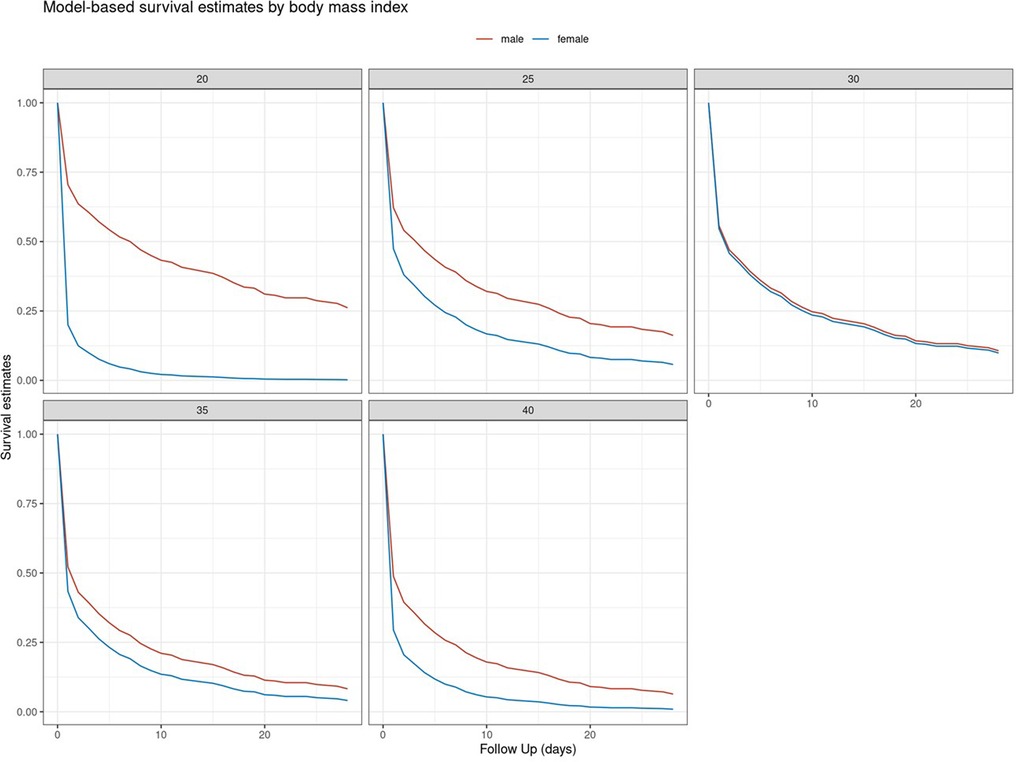
Figure 6. Model-based based estimate for neurologically favourable survival rates (CPC ≤ 2) for selected BMI values (in kg/m2) stratified by gender.
4 Discussion
In our study of a large all-comers collective of patients undergoing eCPR for OHCA, female patients had significantly higher rates of overall, as well as neurologically favourable, survival. Gender-independent survival was 21%; 14% of patients were discharged with favourable neurological outcomes. The suspected aetiology of cardiac arrest differed between the gender-specific subgroups, with female patients presenting lower rates of acute coronary events than male patients and exhibiting more cases of pulmonary embolism. Bleeding complications were observed more frequently in female patients.
The multivariable analysis revealed that the time from collapse to eCPR was independently associated with outcome, and the effect of age and BMI was ascertained to be gender dependent. A significant influence on adverse outcome was observed for higher age, higher BMI, and non-shockable initial rhythm.
The stated survival rates and percentage of patients discharged with a favourable neurological outcome is consistent with the current literature (4, 16), although the data should be evaluated under the constraint that we describe an all-comers collective recorded over a long time interval with an inherent learning curve. The discrepancy to the higher survival rates in current RCTs (2, 3) could arguably be due to the lower rates of shockable primary rhythm and longer time from collapse to eCPR initiation in our collective. A possible explanation of the longer overall resuscitation duration seen in our collective might be the limited availability of mechanical CPR (mCPR) devices in the studied region until December 2020. Prior to this date, these devices had to be requested from the EMS provided by the German army and separately transported to the resuscitation location. This might account for a possible time delay in transport and consecutively longer resuscitation duration until eCPR was established.
We hypothesise that the driving factors in outcome superiority in female patients were the significantly higher rates of witnessed collapse, tendency to more frequent performance of bystander CPR, and overall shorter time to initiation of ALS CPR. Opposing our results, the recent meta-analyses of CA collectives without focusing on eCPR do not support a survival benefit for female patients. This could be due to overall lower rates of witnessed collapse and bystander CPR and higher rates of non-shockable rhythm compared with our collective (9, 17), although the overall comparability is impaired due to the selected eCPR cohort we describe. Interestingly, small sample studies on patients undergoing eCPR for OHCA with similar baseline characteristics as the present analysis support our results suggesting favourable outcomes for female patients, particularly of younger age, speculating that higher blood levels of oestrogen might have a beneficial impact on cardiac regeneration and inflammation after CA (11, 18, 19).
Hormonal influences on beneficial outcome could explain the apparent gender dependence of age in our studied collective, with female patients of reproductive age displaying increased rates of neurologically favourable outcome compared with male patients of the same age category.
Large-scale data regarding gender differences in outcome in the context of eCPR, as well as in-depth analyses of possible hormonal effects, remain to be provided.
In our collective, female patients showed significantly lower rates of pre-existing CAD and ICM, which was also reflected in a lower percentage of acute coronary events as the suspected cause of cardiac arrest. Taking into account the higher rates of pulmonary embolism in female gender, this finding suggests that there might be considerable gender-specific differences in the events causing OHCA, calling for an individualised approach. These findings are consistent with the data from recent meta-analyses stating lower rates of acute coronary events as CA aetiology in female patients (9, 17), as well as observational studies showing an overall lower prevalence and delayed incidence of cardiovascular atherosclerotic disease in female patients (20, 21). Considering the higher rates of beneficial outcome in female patients, our data provide a reason to consider VA-ECMO as a therapy option for pulmonary embolism deteriorating to CA, supporting the present findings suggesting that this might be a feasible therapeutic strategy (22).
The reason for the higher rates of bleeding complications in female patients remains unclear. A potential explanation could be the higher rates of pulmonary embolism in female patients and therefore possible administration of thrombolytic therapy prior to eCPR initiation, accounting for higher rates of periprocedural bleeding due to the invasive nature of VA-ECMO implantation. Furthermore, these findings might derive from gender-specific anatomical differences. Female patients are known to have significantly smaller iliofemoral arterial diameters potentially complicating vascular access (23). This might also justify the gender-specific differences in the impact of BMI on adverse outcomes. Regarding coronary interventions, data suggest an increased risk for periinterventional all-cause mortality for underweight to normoweight female patients (24). Our data suggest that these findings might be transferable to the context of eCPR.
Specifically shockable initial rhythm, witnessed collapse, and performance of bystander CPR are the known predictors for a favourable outcome and are therefore found in the current inclusion criteria for eCPR (25). The results from our multivariable analysis support the impact of these factors.
4.1 Limitations
The present analysis is based on retrospective data from a single centre and thus might not be applicable to the general population. Accounting for 21% (n = 69) of the study population, the percentage of female patients in our study was higher compared with that of present RCTs, but it was still below the percentage of female patients suffering OHCA described in the current registry data (34%) (26). Furthermore, our results are limited by the long study timespan, portraying an inherent learning curve, not only regarding the management of eCPR patients, but also the identification and selection of patients susceptible to this therapy. We report comparatively high rates of non-shockable initial rhythm impeding comparison with current RCTs. While the decision to implement eCPR remains an individualised decision, the trend has shifted to limit this therapy to patients presenting with shockable initial rhythm. The apparent selection bias, as to whom is deemed suitable for this highly invasive and resource-demanding therapeutic option, has to be reported as a major constraint, not only in the present study, but in all investigations in the field of eCPR. In addition, the earlier-described limited availability of mCPR devices during the study period might have considerably affected resuscitation durations and therefore potentially outcome parameters.
5 Conclusion
Gender differences are relevant for favourable outcomes in patients undergoing eCPR for OHCA. Along with the underrepresentation of female gender in the present studies, this calls for further in-depth investigation and potentially consecutive individualisation of therapy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Commission of the Medical Chamber Hamburg. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
AS: Conceptualisation, Data curation, Investigation, Writing – original draft, Writing – review & editing. AD: Writing – review & editing, Investigation. JR: Investigation, Writing – review & editing. LK: Investigation, Writing – review & editing. EB: Investigation, Writing – review & editing. HS: Investigation, Writing – review & editing. PW: Data curation, Formal Analysis, Investigation, Visualisation, Writing – review & editing, Methodology. NG: Investigation, Writing – review & editing, Resources. KH: Investigation, Writing – review & editing. JW: Investigation, Writing – review & editing. BB: Investigation, Resources, Writing – review & editing. TS: Data curation, Writing – review & editing. SW: Resources, Supervision, Writing – review & editing, Investigation. SH: Investigation, Supervision, Writing – review & editing. ET: Conceptualisation, Data curation, Investigation, Project administration, Writing – original draft, Methodology, Supervision.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gräsner JT, Herlitz J, Tjelmeland IBM, Wnent J, Masterson S, Lilja G, et al. European Resuscitation Council guidelines 2021: epidemiology of cardiac arrest in Europe. Resuscitation. (2021) 161:61–79. PMID: 33773833. doi: 10.1016/J.RESUSCITATION.2021.02.007
2. Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. (2022) 327(8):737–47. PMID: 35191923; PMCID: 8864504. doi: 10.1001/JAMA.2022.1025
3. Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet (London, England). (2020) 396(10265):1807–16. PMID: 33197396; PMCID: 7856571. doi: 10.1016/S0140-6736(20)32338-2
4. Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV, et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med. (2023) 388(4):299–309. PMID: 36720132. doi: 10.1056/NEJMOA2204511/SUPPL_FILE/NEJMOA2204511_DATA-SHARING.PDF
5. Inoue A, Hifumi T, Sakamoto T, Kuroda Y. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest in adult patients. J Am Heart Assoc. (2020) 9(7):e015291. doi: 10.1161/JAHA.119.015291
6. Mentzelopoulos SD, Couper K, Voorde PV, Druwé P, Blom M, Perkins GD, et al. European Resuscitation Council guidelines 2021: ethics of resuscitation and end of life decisions. Resuscitation. (2021) 161:408–32. PMID: 33773832. doi: 10.1016/j.resuscitation.2021.02.017
7. Mody P, Pandey A, Slutsky AS, Segar MW, Kiss A, Dorian P, et al. Gender-based differences in outcomes among resuscitated patients with out-of-hospital cardiac arrest. Circulation. (2021) 143(7):641–9. doi: 10.1161/CIRCULATIONAHA.120.050427
8. Morrison LJ, Schmicker RH, Weisfeldt ML, Bigham BL, Berg RA, Topjian AA, et al. Effect of gender on outcome of out of hospital cardiac arrest in the resuscitation outcomes consortium. Resuscitation. (2016) 100:76–81. PMID: 26705971; PMCID: 4761304. doi: 10.1016/J.RESUSCITATION.2015.12.002
9. Lei H, Hu J, Liu L, Xu D. Sex differences in survival after out-of-hospital cardiac arrest: a meta-analysis. Crit Care. (2020) 24(1):1–13. doi: 10.1186/S13054-020-03331-5/TABLES/3
10. Choi HZ, Chang H, Ko SH, Kim MC. Gender effect in survival after out-of-hospital cardiac arrest: a nationwide, population-based, case-control propensity score matched study based Korean national cardiac arrest registry. PLoS One. (2022) 17(5):e0258673. doi: 10.1371/JOURNAL.PONE.0258673
11. Gaisendrees C, Djordjevic I, Sabashnikov A, Adler C, Eghbalzadeh K, Ivanov B, et al. Gender-related differences in treatment and outcome of extracorporeal cardiopulmonary resuscitation-patients. Artif Organs. (2021) 45(5):488–94. PMID: 33052614. doi: 10.1111/AOR.13844
12. Goto Y, Funada A, Maeda T, Okada H, Goto Y. Sex-specific differences in survival after out-of-hospital cardiac arrest: a nationwide, population-based observational study. Crit Care. (2019) 23(1):1–10. doi: 10.1186/S13054-019-2547-X/FIGURES/5
13. Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med. (2021) 47(4):369–421. PMID: 33765189; PMCID: 7993077. doi: 10.1007/s00134-021-06368-4
14. Lorusso R, Shekar K, MacLaren G, Schmidt M, Pellegrino V, Meyns B, et al. ELSO interim guidelines for venoarterial extracorporeal membrane oxygenation in adult cardiac patients. ASAIO J. (2021) 67(8):827–44. doi: 10.1097/MAT.0000000000001510. Erratum in: ASAIO J. (2022) 68(7):e133. PMID: 34339398.34339398
15. ELSO General Guidelines Extracorporeal Life Support Organization (ELSO) general guidelines for all ECLS cases. (2017). Available at: www.elso.org (Accessed November 24, 2020).
16. Downing J, Al Falasi R, Cardona S, Fairchild M, Lowie B, Chan C, et al. How effective is extracorporeal cardiopulmonary resuscitation (ECPR) for out-of-hospital cardiac arrest? A systematic review and meta-analysis. Am J Emerg Med. (2022) 51:127–38. PMID: 34735971. doi: 10.1016/J.AJEM.2021.08.072
17. Lakbar I, Ippolito M, Nassiri A, Delamarre L, Tadger P, Leone M, et al. Sex and out-of-hospital cardiac arrest survival: a systematic review. Ann Intensive Care. (2022) 12(1):1–16. PMID: 36534195; PMCID: 9763524. doi: 10.1186/S13613-022-01091-9/TABLES/3
18. Hasan OF, Al Suwaidi J, Omer AA, Ghadban W, Alkilani H, Gehani A, et al. The influence of female gender on cardiac arrest outcomes: a systematic review of the literature. Curr Med Res Opin. (2014) 30(11):2169–78. PMID: 2494082619. doi: 10.1185/03007995.2014.936552
19. Bray JE, Stub D, Bernard S, Smith K. Exploring gender differences and the “oestrogen effect” in an Australian out-of-hospital cardiac arrest population. Resuscitation. (2013) 84(7):957–63. doi: 10.1016/J.RESUSCITATION.2012.12.004
20. Maas AHEM, Appelman YEA. Gender differences in coronary heart disease. Netherlands Hear J. (2010) 18(12):598. doi: 10.1007/S12471-010-0841-Y
21. Gao Z, Chen Z, Sun A, Deng X. Gender differences in cardiovascular disease. Med Nov Technol Devices. (2019) 4:100025. doi: 10.1016/J.MEDNTD.2019.100025
22. Hobohm L, Sagoschen I, Habertheuer A, Barco S, Valerio L, Wild J, et al. Clinical use and outcome of extracorporeal membrane oxygenation in patients with pulmonary embolism. Resuscitation. (2022) 170:285–92. PMID: 3465355023. doi: 10.1016/J.RESUSCITATION.2021.10.007
23. Tran K, Dorsey C, Lee JT, Chandra V. Gender-Related differences in iliofemoral arterial anatomy among abdominal aortic aneurysm patients. Ann Vasc Surg. (2017) 44:171–8. doi: 10.1016/J.AVSG.2017.01.025
24. Faggioni M, Baber U, Afshar AE, Giustino G, Sartori S, Sorrentino S, et al. Effects of body mass index on clinical outcomes in female patients undergoing percutaneous coronary intervention with drug-eluting stents: results from a patient-level pooled analysis of randomized controlled trials. JACC Cardiovasc Interv. (2018) 11(1):68–76. PMID: 29248412. doi: 10.1016/J.JCIN.2017.06.060
25. Schmitzberger FF, Haas NL, Coute RA, Bartos J, Hackmann A, Haft JW, et al. ECPR2: expert consensus on PeRcutaneous cannulation for extracorporeal CardioPulmonary resuscitation. Resuscitation. (2022) 179:214–20. PMID: 35817270. doi: 10.1016/J.RESUSCITATION.2022.07.003
26. Fischer M, Wnent J, Gräsner J-T, Seewald S, Brenner S, Bein B, et al. Öffentlicher Jahresbericht 2021 Des Deutschen Reanimationsregisters: Außerklinische Reanimation 2021. (2022). Available at: www.reanimationsregister.de/berichte.html
Keywords: eCPR, VA-ECMO, OHCA, gender, CPR
Citation: Springer A, Dreher A, Reimers J, Kaiser L, Bahlmann E, van der Schalk H, Wohlmuth P, Gessler N, Hassan K, Wietz J, Bein B, Spangenberg T, Willems S, Hakmi S and Tigges E (2024) Gender disparities in patients undergoing extracorporeal cardiopulmonary resuscitation. Front. Cardiovasc. Med. 10:1265978. doi: 10.3389/fcvm.2023.1265978
Received: 25 July 2023; Accepted: 30 November 2023;
Published: 16 January 2024.
Edited by:
Helle Soeholm, University of Copenhagen, DenmarkReviewed by:
Sebastian Schnaubelt, Medical University of Vienna, AustriaVedant Arun Gupta, University of Kentucky, United States
© 2024 Springer, Dreher, Reimers, Kaiser, Bahlmann, van der Schalk, Wohlmuth, Gessler, Hassan, Wietz, Bein, Spangenberg, Willems, Hakmi and Tigges. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: E. Tigges ZS50aWdnZXNAYXNrbGVwaW9zLmNvbQ==
 A. Springer
A. Springer A. Dreher1
A. Dreher1 K. Hassan
K. Hassan B. Bein
B. Bein S. Hakmi
S. Hakmi