- 1Mehiläinen, Airport Health Center, Vantaa, Finland
- 2Department of Forensic Medicine, University of Helsinki, Helsinki, Finland
- 3Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa
- 4Cardiovascular Research, Wihuri Research Institute, Helsinki, Finland
Introduction
The risk of wildfires has been increasing which may well be associated with climate change (1, 2). The effects of wildfires can have serious consequences on human health. Currently, extremely destructive wildfires in Canada have generated substantial smoke within as well as beyond the borders of Canada (3). It has been estimated that toxic wildfire smoke from about 200 wildfires in Quebec alone, has affected over 100 million people in Canada and the USA (4). The severity of harm is such that residents in smoke-affected areas have been advised to use N95 masks when outdoors and, if possible, to remain indoors.
There are broad-based negative health effects caused by forest fires that will only worsen as their numbers and severity increase (5, 6). As an example, a study compared hospital visits during a wildfire in August 2015 and post-wildfire in September 2015 in the city of Calgary (7). In this study, physician visits increased by 19% among seniors, mainly related to ischemic heart disease (95% CI: 7%−33%). Wildfire smoke has also been associated with out-of-hospital cardiac arrest (8). Importantly, wildfire smoke has a significant negative impact on airway epithelial cell viability, as there is a disruption of the cellular survival processes governed by autophagy, i.e., of processes that are already dysregulated in chronic obstructive pulmonary obstructive disease (9). Moreover, even short-term exposures of pulmonary airways to PM2.5 particles cause systemic inflammation, oxidative stress, and changes in the balance of the autonomic nervous system, all of which may then jointly result in vascular thrombosis and ventricular arrhythmias (8, 10). The primary initiating pathways causing systemic oxidative stress and systemic inflammation include the migration of PM2.5 particles from the lungs to the circulation (11, 12), and as shown in a recent in vivo study, exposure to PM2.5 particles associates with features of vulnerable atherosclerotic plaques in coronary arteries (13).
It can be reasonably concluded that significant forest fires and smoke exposure are associated with a notable additional burden on healthcare services. Moreover, studies have revealed that several sectors of the population are particularly vulnerable to the effects of smoke from forest fires. As an example of social vulnerability, a study using satellite-collected data on wildfire smoke exposure at locations of exposed populations during 2011–2021 indicated that in almost 90% of the US population, large increases of exposure were especially high in communities representing ethnic minorities (14). In this article, we focus on another vulnerable group, i.e., people with cardiovascular disease.
Our intent was to perform a cursory assessment of public guidance that has been recommended for individuals with cardiovascular disease, hopefully, to prevent additional health-threatening events during exposure to wildfire smoke. The purpose is not to determine the effectiveness of current wildfire smoke health exposure guidelines (15), but simply to explore whether such guidelines contain evidence-based guidance for high-risk cardiovascular disease patients who are exposed to toxic smoke.
Wildfire smoke exposure and cardiovascular events
In general, exposure to wildfire smoke has been shown to increase cardiovascular-related health issues such as acute myocardial infarction, cardiovascular mortality, cardiovascular emergency department visits and hospitalization, cardiac arrest, as well as heart failure (16–19). Especially vulnerable are those individuals who have pre-existing cardiovascular disease who, when exposed to external factors such as wildfire smoke-generated PM2.5 particles, can severely worsen their pre-existing endothelial dysfunction (20–22). Even acute exposure to PM2.5 particle pollution is associated with increased cardiovascular morbidity and mortality (18). This observation is due to inhaled particles entering the circulation and worsening systemic endothelial dysfunction which in turn causes adverse cardiovascular effects due to oxidative stress, inflammation, cytokine release, and hypercoagulability (23, 24). Additionally, diabetics are at increased risk from PM2.5 particle exposure because of pre-existing endothelial dysfunction as well as autonomic dysfunction due to diabetic neuropathy (20). Similarly, we proposed that patients with familial hypercholesterolemia, who have pre-existing endothelial dysfunction from lifelong exposure to elevated LDL-cholesterol levels, are likely to be at increased risk if exposed to PM2.5 particles (22). Lastly, the majority of patients presenting with an acute coronary syndrome have endothelial dysfunction, and in a 6-year follow-up study, endothelial dysfunction was an independent significant positive predictive value for major adverse cardiovascular events (hazard ratio 2.04, 95% confidence interval 1.43–2.89, P < 0.001) (25).
Pharmacological prevention of cardiovascular events during wildfire smoke exposure
When exposed to wildfire toxic smoke, a likely preventive measure to decrease cardiac events is to lower PM2.5 particle exposure and thereby limit further endothelial dysfunction. The use of effective masks (e.g., N95 masks) during short and particularly long-lasting wildfires is one relatively inexpensive solution, but these can become uncomfortable, particularly if they need to be worn for a protracted period whilst exposed to polluting particles. Another alternative, but still an effective and practical approach, is to pharmacologically improve endothelial function to reduce the risk of cardiovascular events (26). In a recent review, Hadley and coworkers (18) stressed that an important target when preparing for the wildfire season is the prevention of cardiovascular disease. This goal can be met to some degree by the reduction of endothelial dysfunction, which can be rather rapidly achieved with pharmacological agents (27). The use of statins, which are relatively inexpensive and readily accessible, should be prioritized, as these agents acutely improve endothelial function and offer long-term stabilization of vulnerable plaques (28, 29). Several studies are showing that statin use beneficially modifies PM2.5 effects on inflammation and, as a result, most likely also improves endothelial function (30–35).
Public health guidance for heart patients to prevent cardiovascular events
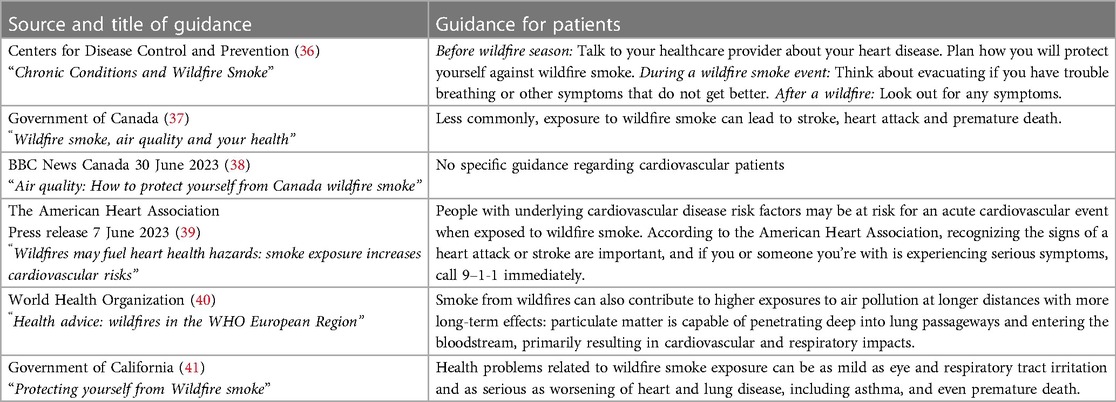
To assess whether pharmacological prevention is recommended to address the effects of wildfire smoke exposure, we analyzed several public guidance documents provided by the Centers for Disease Control and Prevention (CDC), USA (36), Government of Canada (37), BBC News (38), American Heart Association (AHA) press release (39), World Health Organization (WHO) Europe (40) and the Government of California (41) Table 1. The Government of Canada indicates that there is a rare risk of cardiovascular events, and that “wildfire smoke can worsen heart and lung disease”. The BBC news guidance does not address the challenges for heart patients during wildfires, while the AHA press release reminds cardiovascular patients of the risk—“People with underlying cardiovascular disease risk factors may be at risk for an acute cardiovascular event when exposed to wildfire smoke.” However, it does not mention the importance of effectively treating the underlying cardiovascular disease itself. The WHO only warns of the cardiovascular risk related to wildfire smoke exposure—“Particulate matter is capable of penetrating deep into lung passageways and entering the bloodstream, primarily resulting in cardiovascular and respiratory impacts”. Interestingly, only the CDC indirectly recommends pharmacological prevention before the wildfire season by stating, “Plan how you will protect yourself against wildfire smoke.” The CDC advises that “Before wildfire season: Talk to your healthcare provider about your heart disease”. This advice would seem to indicate that there is an unmet need to medically evaluate cardiovascular disease and to ensure that it is being effectively treated prior to wildfire smoke exposure.
Conclusion
Although not considered in current guidances, it can be concluded that pharmacological prevention using statins acutely improves endothelial function (28), and in the longer term may stabilize vulnerable plaques (29) and thereby reducing the risk of acute cardiovascular events. Only the CDC has included it in its guidance and arguably only indirectly. We encourage the various relevant authorities to place more emphasis on this neglected area to inform vulnerable cardiovascular patients exposed to wildfire smoke of their risk, to recommend that such patients seek appropriate medical care, and when medically relevant, that the use of lipid-lowering statins is considered.
Many physicians may not be necessarily aware of the harmful cardiovascular effects caused by wildfire smoke and this needs to be brought to their attention. For example, the 2021 European Society of Cardiology (ESC) Guidelines on cardiovascular disease prevention in clinical practice mentions that “Important sources of fine particles are road traffic, power plants, and industrial and residential heating using oil, coal, and wood” (42). However, wildfire smoke is not clearly mentioned in this guideline as an acute toxic exposure that can increase the risk of having a cardiovascular event. It would be beneficial in this and other respective guidance materials to inform healthcare providers and at-risk individuals, as well as the greater population, of the substantial risk that wildfire smoke poses, and that there are preventive measures that can, and should, be taken. Further prospective controlled studies with larger sample sizes are needed to confirm the association between wildfire smoke, major adverse cardiovascular events, and the role of statins in preventing them. This is particularly because there are data to show that wildfire smoke is even more toxic than many other forms of air pollution (24).
Author contributions
AV: Writing – original draft, Writing – review & editing. BB: Writing – review & editing. FR: Writing – review & editing. PK: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
AV has received consultancy fees from Amgen and Novartis. PK has received consultancy fees, lecture honoraria, and/or travel fees from Amarin, Amgen, Novartis, Raisio Group, and Sanofi. BB none. FR has received research grants, honoraria, or consulting fees for professional input and/or lectures from Sanofi, Regeneron, Amgen, Novartis, and LIB Therapeutics.
AV declared that he is an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bowman DMJS, Kolden CA, Abatzoglou JT, Johnston FH, van der Werf GR, Flanningan M. Vegetation fires in the Anthropocene. Nat Rev Earth Environ. (2020) 1:500–15. doi: 10.1038/s43017-020-0085-3
2. Vuorio A, Kovanen PT, Budowle B, Sajantila A, Palo JU, Stoop J. Wildfire-related catastrophes: the need for a modern international safety investigation procedure. Front Clim. (2021) 3:659437. doi: 10.3389/fclim.2021.659437
3. Graham F. Daily briefing: the science behind extreme wildfires in Canada. Nature. (2023). doi: 10.1038/d41586-023-01954-6
4. Tanne JH. Canadian Wildfires create hazardous air conditions in eastern US. Br Med J. (2023) 381:1320. doi: 10.1136/bmj.p1320
5. Black C, Tesfaigzi Y, Bassein JA, Miller LA. Wildfire smoke exposure and human health: significant gaps in research for a growing public health issue. Environ Toxicol Pharmacol. (2017) 55:186–95. doi: 10.1016/j.etap.2017.08.022
6. Schwarz L, Aguilera R, Aguilar-Dodier LC, Castillo Quiñones JE, García MEA, Benmarhnia T. Wildfire smoke knows no borders: differential vulnerability to smoke effects on cardio-respiratory health in the San Diego-Tijuana region. PLOS Glob Public Health. (2023) 3:e0001886. doi: 10.1371/journal.pgph.0001886
7. Mahsin MD, Cabaj J, Saini V. Respiratory and cardiovascular condition-related physician visits associated with wildfire smoke exposure in Calgary, Canada, in 2015: a population-based study. Int J Epidemiol. (2022) 51:166–78. doi: 10.1093/ije/dyab206
8. Jones CG, Rappold AG, Vargo J, Cascio WE, Kharrazi M, McNally B. Out-of-hospital cardiac arrests and wildfire-related particulate matter during 2015−2017 California wildfires. J Am Heart Assoc. (2020) 9:e014125. doi: 10.1161/JAHA.119.014125
9. Roscioli E, Hamon R, Lester SE, Jersmann HPA, Reynolds PN, Hodge S. Airway epithelial cells exposed to wildfire smoke extract exhibit dysregulated autophagy and barrier dysfunction consistent with COPD. Respir Res. (2018) 19:234. doi: 10.1186/s12931-018-0945-2
10. Cascio WE. Proposed pathophysiologic framework to explain some excess cardiovascular death associated with ambient air particle pollution: insights for public health translation. Biochim Biophys Acta. (2016) 1860:2869–79. doi: 10.1016/j.bbagen.2016.07.016
11. Münzel T, Gori T, Al-Kindi S, Deanfield J, Lelieveld J, Daiber A, et al. Effects of gaseous and solid constituents of air pollution on endothelial function. Eur Heart J. (2018) 39:3543–50. doi: 10.1093/eurheartj/ehy481
12. Gangwar RS, Bevan GH, Palanivel R, Das L, Rajagopalan S. Oxidative stress pathways of air pollution mediated toxicity: recent insights. Redox Biol. (2020) 34:101545. doi: 10.1016/j.redox.2020.101545
13. Montone RA, Camilli M, Russo M, Termite C, La Vecchia G, Innaccone G, et al. Air pollution and coronary plaque vulnerability and instability: an optical coherence tomography study. JACC Cardiovasc Imaging. (2022) 15:325–42. doi: 10.1016/j.jcmg.2021.09.008
14. Vargo J, Lappe B, Mirabelli MC, Conlon KC. Social vulnerability in US communities affected by wildfire smoke, 2011 to 2021. Am J Public Health. (2023) 113:759–67. doi: 10.2105/AJPH.2023.307286
15. LaRocca R, Yost J, Dobbins M, Ciliska D, Butt M. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health. (2012) 12:751. doi: 10.1186/1471-2458-12-751
16. Wettstein ZS, Hoshiko S, Fahimi J, Harrison RJ, Cascio WE, Rappold AG. Cardiovascular and cerebrovascular emergency department visits associated with wildfire smoke exposure in California in 2015. J Am Heart Assoc. (2018) 7:e007492. doi: 10.1161/JAHA.117.007492
17. Hahn MB, Kuiper G, O'Dell K, Fischer EV, Magzamen S. Wildfire smokeis associated with an increased risk of cardiorespiratory emergency department visits in Alaska. Geohealth. (2021) 5:e2020GH000349. doi: 10.1029/2020GH000349
18. Hadley MB, Henderson SB, Brauer M, Vedanthan R. Protecting cardiovascular health from Wildfire smoke. Circulation. (2022) 146:788–801. doi: 10.1161/CIRCULATIONAHA.121.058058
19. Doubleday A, Sheppard L, Austin E, Busch Isaksen T. Wildfire smoke exposure and emergency department visits in Washington State. Environ Res Health. (2023) 1:025006. doi: 10.1088/2752-5309/acd3a1
20. O'Neill MS, Veves A, Zanobetti A, Sarnat JA, Gold DR, Economides PA, et al. Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation. (2005) 111:2913–20. doi: 10.1161/CIRCULATIONAHA.104.517110
21. Al-Kindi SG, Brook RD, Biswal S, Rajagopalan S. Environmental determinants of cardiovascular disease: lessons learned from air pollution. Nat Rev Cardiol. (2020) 17:656–72. doi: 10.1038/s41569-020-0371-2
22. Vuorio A, Budowle B, Kovanen PT. Airborne particles and cardiovascular morbidity in severe inherited hypercholesterolemia: vulnerable endothelium under multiple attacks. Bioessays. (2022) 44:e2100273. doi: 10.1002/bies.202100273
23. Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliot CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. (2016) 124:1334–43. doi: 10.1289/ehp.1409277
24. Chen H, Samet JM, Bromberg PA, Tong H. Cardiovascular health impacts of wildfire smoke exposure. Part Fibre Toxicol. (2021) 18:2. doi: 10.1186/s12989-020-00394-8
25. Yoshii T, Matsuzawa Y, Kato S, Sato R, Hanajima Y, Kikuchi S, et al. Endothelial dysfunction predicts bleeding and cardiovascular death in acute coronary syndrome. Int J Cardiol. (2023) 376:11–7. doi: 10.1016/j.ijcard.2023.01.079
26. Vuorio A, Kovanen PT. Statins for coronary patients exposed to wildfire-related air pollution: an opportunity to reduce the increased risk of coronary events. Can J Cardiol. (2023). doi: 10.1016/j.cjca.2023.06.014
27. van Nieuw Amerongen GP, Vermeer MA, Nègre-Aminou P, Lankelma J, Emeis JJ, van Hinsbergh VW. Simvastatin improves disturbed endothelial barrier function. Circulation. (2000) 102:2803–9. doi: 10.1161/01.cir.102.23.2803
28. Liu C, Shen M, Tan WLW, Chen YI, Liu Y, Yu X, et al. Statins improve endothelial function via suppression of epigenetic-driven EndMT. Nat Cardiovasc Res. (2023) 2:467–85. doi: 10.1038/s44161-023-00267-1
29. Biccirè FG, Gatto L, La Porta Y, Pignatelli P, Prati F, Pastori D. Effects of lipid lowering therapies on vulnerable plaque features: an updated narrative review of the literature. J Cardiovasc Dev Dis. (2023) 10:260. doi: 10.3390/jcdd10060260
30. Schwartz J, Park SK, O'Neill MS, Vokonas PS, Sparrow D, Weiss S, et al. Glutathione-S-transferase M1, obesity, statins, and autonomic effects of particles: gene-by-drug-by-environment interaction. Am J Respir Crit Care Med. (2005) 172:1529–33. doi: 10.1164/rccm.200412-1698OC
31. O'Neill MS, Veves A, Sarnat JA, Zanobetti A, Gold DR, Economides PA, et al. Air pollution and inflammation in type 2 diabetes: a mechanism for susceptibility. Occup Environ Med. (2007) 64:373–9. doi: 10.1136/oem.2006.030023
32. Delfino RJ, Staimer N, Tjoa T, Polidori A, Arhami M, Gillen DL, et al. Circulating biomarkers of inflammation, antioxidant activity, and platelet activation are associated with primary combustion aerosols in subjects with coronary artery disease. Environ Health Perspect. (2008) 116:898–906. doi: 10.1289/ehp.11189
33. Alexeeff SE, Coull BA, Gryparis A, Suh H, Sparrow D, Vokonas PS, et al. Medium-term exposure to traffic-related air pollution and markers of inflammation and endothelial function. Environ Health Perspect. (2011) 119:481–6. doi: 10.1289/ehp.1002560
34. Ostro B, Malig B, Broadwin R, Basu R, Gold EB, Bromberger JT, et al. Chronic PM2.5 exposure and inflammation: determining sensitive subgroups in mid-life women. Environ Res. (2014) 132:168–75. doi: 10.1016/j.envres.2014.03.042
35. Busenkell E, Collins CM, Moy ML, Hart JE, Grady ST, Coull BA, et al. Modification of associations between indoor particulate matter and systemic inflammation in individuals with COPD. Environ Res. (2022) 209:112802. doi: 10.1016/j.envres.2022.112802
36. Centers for Disease Control and Prevention 2023. Chronic Conditions and Wildfire Smoke. Available at: https://www.cdc.gov/air/wildfire-smoke/chronic-conditions.htm#heartdisease (Accessed July 10, 2023).
37. Government of Canada 2023. Wildfire smoke, air quality and your health. Available at: https://www.canada.ca/en/environment-climate-change/services/air-quality-health-index/wildfire-smoke.html#toc3 (Accessed July 10, 2023).
38. BBC News Canada 30 June 2023. Air quality: How to protect yourself from Canada wildfire smoke. Available at: https://www.bbc.com/news/world-us-canada-6584348530 (Accessed July 10, 2023).
39. The American Heart Association Press Release 7 June 2023. Wildfires may fuel heart health hazards: smoke exposure increases cardiovascular risks. Available at: https://newsroom.heart.org/news/wildfires-may-fuel-heart-health-hazards-smoke-exposure-increases-cardiovascular-risks (Accessed July 15, 2023).
40. World Health Organization 2023. Health advice: wildfires in the WHO European Region. Available at: https://www.who.int/europe/news/item/12-08-2021-health-advice-wildfires-in-the-who-european-region (Accessed July 10, 2023).
41. Government of California 2023. Protecting yourself from wildfire smoke. Available at: https://ww2.arb.ca.gov/protecting-yourself-wildfire-smoke (Accessed July 10, 2023).
Keywords: wildfire smoke, endothelial dysfunction, acute myocardial infarction, cardiovascular disease, prevention, PM2.5
Citation: Vuorio A, Budowle B, Raal F and Kovanen PT (2023) Wildfire smoke exposure and cardiovascular disease—should statins be recommended to prevent cardiovascular events?. Front. Cardiovasc. Med. 10:1259162. doi: 10.3389/fcvm.2023.1259162
Received: 17 July 2023; Accepted: 28 August 2023;
Published: 14 September 2023.
Edited by:
Amit K. Dey, National Institutes of Health (NIH), United StatesReviewed by:
Kumar Ashish, CarolinaEast Medical Center, United States© 2023 Vuorio, Budowle, Raal and Kovanen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alpo Vuorio YWxwby52dW9yaW9AZ21haWwuY29t
 Alpo Vuorio
Alpo Vuorio Bruce Budowle
Bruce Budowle Frederick Raal
Frederick Raal Petri T. Kovanen
Petri T. Kovanen