
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 29 August 2023
Sec. Cardiovascular Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1235247
Introduction: The oxidative damage suffered in cardiac surgery is associated with declining trace elements which lead to the development of multi organ dysfunction (MOD), acute kidney injury (AKI), or increased length of hospital stay (LOS). Recent evidence shows the cardioprotective role of the trace element selenium as it mitigates worsening outcomes post cardiac surgery. Hence, this meta analysis aims to investigate the role of selenium in lowering cardiac surgery related adverse outcomes.
Methods: Literature search of five electronic databases was performed from the inception of the paper till 29th July, 2023. Eligibility criteria included; (a) randomized clinical trials with Adult patients (≥18 years) undergoing cardiac surgery (b) intervention with selenium pre or/and postoperatively; (c) a control group of a placebo, normal saline, or no selenium. Outcomes of interest include postoperative mortality, LOS in the hospital and Intensive Care Unit (ICU), AKI, troponin I, and Creatinine Kinase-MB (CK-MB). The Cochrane bias assessment tool was used to evaluate the risk of bias. Outcomes were pooled with the Mantel-Haenszel Random-effects model using Review Manager.
Results: Seven RCTs with 2,521 patients and 65% of males were included in this paper. No noticable differences were observed between selenium and control groups in terms of postoperative AKI, mortality, LOS in hospital and ICU, troponin I, and CK-MB levels. All studies had a low risk of bias on quality assessment.
Discussion: Our meta analysis demonstrated no discernible effects of selenium infusion on post operative complications among patients undergoing cardiac surgery. Further large scale multi centered studies comparing the protective role of selenium with combined therapy of other bioactive agents are needed to provide convincing explanations.
Systematic Review Registration: PROSPERO Identifier: 424920.
Cardiac surgery and its outcomes are determined by various preoperative, intraoperative and postoperative factors that contribute to a higher morbidity rate as comparison to noncardiac surgeries (1). Increased oxidative stress (OS) is a significant contributor to the pathophysiology of cardiovascular disease and has been implicated in disease progression, the main culprit being reactive oxygen species (ROS) (2). This metabolic disturbance is worsened when patients undergo cardiac surgery and are subjected to the cardiopulmonary bypass (CP) pump which further increases the levels of lipid hydroperoxides and advanced oxidation protein products (3), predisposing patients to postoperative complications such as acute respiratory distress syndrome and acute kidney injury (AKI) (4).
Bioactive metabolites such as iron, copper, zinc, and selenium are important in regulating cell metabolism and their antioxidative properties may help prevent the progression of cardiovascular disease (5). The oxidative damage suffered in cardiac surgery is associated with declining trace elements which may predispose patients to develop multiple organ dysfunction (MOD) (6). Therefore, it can be postulated that supplementation with these minerals before cardiac surgery may help prevent postoperative complications leading to better outcomes for patients.
The trace element, selenium, has specifically shown a protective effect against oxidative stress (7) as it forms an essential component of our body's antioxidant defense mechanism. The inflammatory signaling pathways that modify ROS are modulated through selenium as it suppresses the nuclear factor-kappa B (NF-B) cascade, hence enhancing antioxidant capacity and reducing the generation of interleukins and tumor necrosis factor alpha (TNF-alpha) (8). A meta analysis conducted by Jenkins et al., demonstrates that adding selenium to the antioxidant mixture helps reduce the mortality rate in patients with cardiovascular disease. Moreover, removing selenium from the mixture led to a significantly increased risk of mortality, further highlighting the role of selenium in the antioxidant mix (9). Metabolic therapy with selenium was also noticed to decrease organ dysfunction (10) and myocardial damage in patients undergoing cardiac surgery (8). Recent evidence has established the role of selenium in reducing the hospital and ICU LOS in trauma patients, however, no concrete evidence exists that determines whether similar results are obtained in cardiac surgery patients (11).
Previously, pooled analyses have been conducted that explore the effects of other metabolic agents such as vitamin C in complex cardiac surgeries (12) but so far no conclusive results exist to demonstrate whether selenium depletion is the real culprit behind worsening postoperative outcomes in cardiac surgery patients. Hence, our meta-analysis aims to discover whether intervention with a bioactive agent, selenium, in patients undergoing cardiac surgery could help improve postoperative outcomes such as LOS, mortality, AKI, and troponin I and Creatinine Kinase-MB (CK-MB) levels.
Our meta-analysis followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines and was conducted within the framework laid out by the Cochrane collaboration (13). This systematic review and meta analysis has been registered on Prospero (ID: 424920). PRISMA checklist for this paper is provided in Supplementary Table 1.
Pubmed, Google Scholar, ScienceDirect, ClinicalTrials.gov, and Cochrane CENTRAL were searched for literature from the inception of the paper till 29th July 2023. The following Medical Subject Headings (MESH terms) were incorporated into our search string: “selenium”, “selenium compounds”, “organoselenium”, “organoselenium”, “organoselenium compounds”, “cardiac surgery”, “cardiac operation”, “heart surgery”, “cardiothoracic surgery”, “coronary artery bypass grafting”, “cardiopulmonary bypass”. The complete search strategies used in each of the databases are provided in Supplementary Table 2. While performing the literature search, no location or time restrictions were applied and unpublished literature records were thoroughly searched to ensure that no material pertinent to our study had been omitted.
The retrieved articles from the literature search were transferred to the Mendeley Desktop 1.19.8 (Mendeley Ltd., Amsterdam, Netherlands) to scan for duplicates. Once the duplicates were removed, two independent reviewers (STR, FE) screened the articles and selected them if they matched with the PICO criteria of our study. In the initial study selection process, articles were chosen after reading their abstract and later were finalized after screening their full textThe following eligibility criteria was used to select studies: (a) randomized controlled trials (RCTs); (b) adult patients (≥18 years) undergoing cardiac surgery [CABG, valvular surgery, aortic surgery, left ventricular assist device (LVAD) implantation, intra aortic balloon pump]; (c) intervention with selenium pre or/and postoperatively; (d) control group of placebo, normal saline or no selenium; (e) outcomes of interest including postoperative mortality, LOS in the hospital and Intensive Care Unit, AKI, troponin I and CK-MB. Excluded articles included observational studies, commentaries, letters, and case reports. Articles in a language other than English and articles that administered other metabolites with selenium in intervention groups such as Vitamin C, Zinc, and Calcium were also excluded to exclusively see the effects of selenium on patients undergoing cardiac surgery. Studies evaluating the effects of selenium on surgeries other than cardiac procedures were also eliminated from our paper.
Data on baseline characteristics such as study type, sample size, mean age, intervention, dosage, control, type of surgery, and primary outcomes were extracted into a Microsoft Excel sheet. Two reviewers (FE and STR) independently assessed the quality of the seven included RCTs. A third independent reviewer was consulted to resolve any discrepancies in the risk of bias assessments between the two review writers (LI). The risk of bias was assessed using the The Cochrane bias assessment tool (14) that categorized the risk of bias criteria as either low, high, or unclear on the basis of items described in the Cochrane Handbook for Systematic Reviews of Interventions (15). The RCTs were assessed on the basis of the following five categories: (i) selection bias (ii) performance bias (iii) detection bias (iv) attrition bias (v) reporting bias.
The Mantel-Haenszel Random-effects model was used to pool the results using Review Manager (Version 5.3. The Cochrane Collaboration). Continuous data in our study were presented as mean difference and 95% confidence interval (CI) and to represent dichotomous data, odds ratios (OR) with 95% CI were employed. Heterogeneity was quantified using Higgins I2 statistics; a value of I2 = 25%–50% was considered statistically mild, 50%–75% as moderate, and >75% as severe heterogeneity. A p-value <0.05 was considered significant and this was consistent across all the studies.
An initial search of 5 electronic databases and a few other sources provided 3,660 studies, out of which 3,387 records were left after removing the duplicate studies. 3,335 studies were eliminated after the title and abstract screening. After a full-text review of 52 articles which were assessed for their eligibility, 45 articles were excluded which did not meet the inclusion criteria. Consequently, 7 RCTs were finalized for this meta-analysis (16–22). A complete literature search has been highlighted in the PRISMA flowchart in Figure 1.
Study characteristics and patients' baseline characteristics have been mentioned in detail in Tables 1, 2. A total of 2,521 patients were enrolled in these 7 RCTs, out of which 1,192 patients belonged to the selenium supplemented group, 1,194 patients belonged to the control group while 135 patients did not belong to any of our groups of interest. The mean age of the patients ranged from 52.8 years to 68.2 years with an average of 60.4 years. The percentage of males ranged from 38.3% to 95%, with a mean of 65.1% of the total population.
The majority of the included studies reported an overall low risk of bias, enhancing the authenticity of this meta analysis. Out of the 7 included studies, 3 studies reported detection bias which was the only main factor that hindered the quality of included studies (18, 21, 22). Additionally, the trial conducted by Amini et al. reported performance bias (18). On assessment, the overall quality of all the included studies was declared high. The detailed results of the quality assessment are listed in Figures 2, 3.
The seven included RCTs (16–22) reported the role of selenium supplementation vs. control on postoperative outcomes in patients undergoing cardiac surgeries. Comprehensive forest plots with effect sizes of primary and secondary outcomes are given in Figures 4, 5.
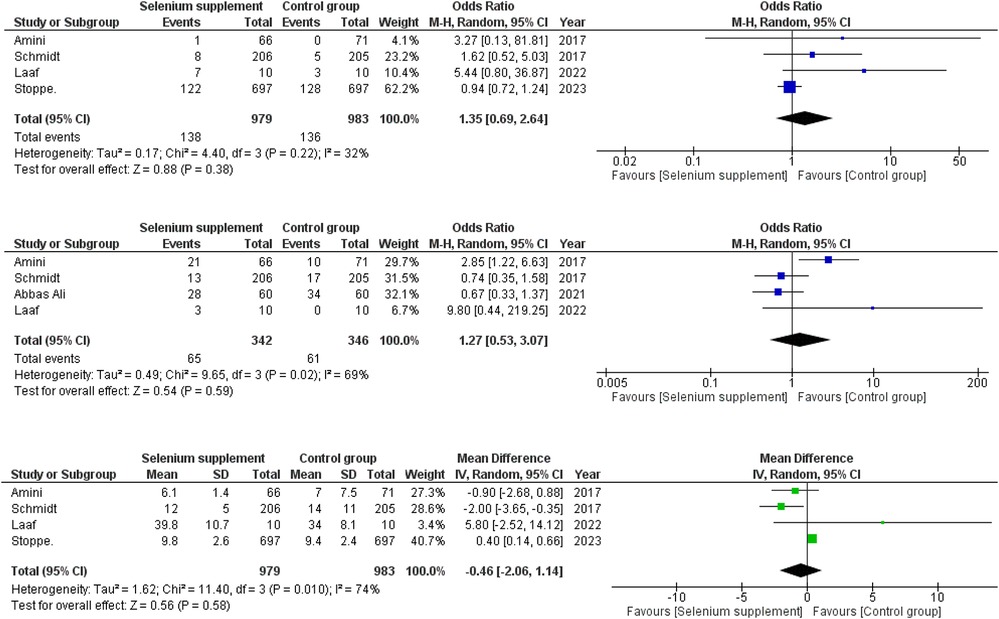
Figure 4. (A) Forest plot depicting odds ratios for mortality in selenium supplemented vs. control group patients. (B) Forest plot depicting odds ratios for AKI in selenium supplemented vs. control group patients. (C) Forest plot depicting mean differences for LOS in hospital in selenium supplemented vs. control group patients.
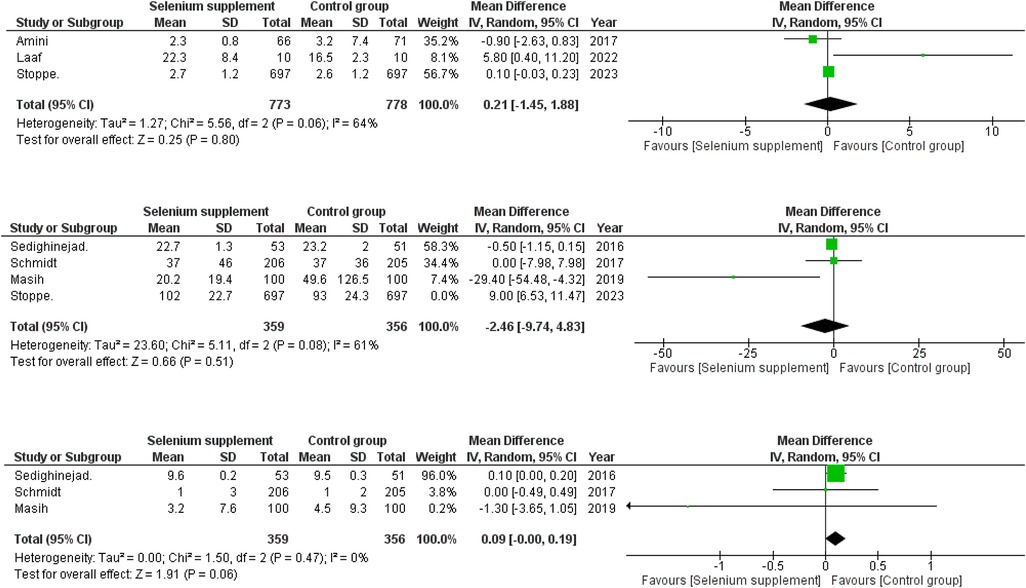
Figure 5. (A) Forest plot depicting mean differences for LOS in ICU in selenium supplemented vs. control group patients. (B) Forest plot depicting mean differences for post-operative CK-MB levels in selenium supplemented vs. control group patients after sensitivity analysis. (C) Forest plot depicting mean differences for post-operative Troponin I in selenium supplemented vs. control group patients.
Four RCTs (16–19) provided data for the effects of selenium supplementation on the mortality rate amongst the patients. A slight difference was observed between the two groups with higher chances of mortality in selenium supplementation group (OR = 1.35; 95% CI = 0.69–2.64; P = 0.38; I2= 32%) with a mild heterogeneity present amongst the RCTs (Figure 4).
Four out of seven RCTs (17–20) provided data on the incidence of postoperative AKI. A minor difference was observed when the two groups were compared (OR = 1.27; 95% CI = 0.53–3.07; P = 0.59; I2 = 69%) with mild chances of AKI in the selenium supplementation group. A moderate level of heterogeneity was observed between the RCTs (Figure 4).
Four RCTs (16–19) reported data on post-operative hospital LOS in relation to selenium supplementation. A minor difference was observed between the two groups in terms of LOS in hospital (WMD = −0.46; 95% CI = −2.06–1.14; P = 0.58; I2 = 74%) with the selenium supplemented group having a LOS some degree shorter than the control group. Only a moderate level of heterogeneity was found amongst the studies (Figure 4).
Three RCTs (16, 18, 19) published data on post-operative LOS in the ICU. A minor difference was observed amongst the two groups when their LOS in ICU were compared (WMD = 0.21; 95% CI = −1.45–1.88; P = 0.80; I2 = 64%) with the selenium supplemented group having moderately longer ICU stay as compared to the non selenium group. Moderate level heterogeneity was found among the included studies (Figure 5).
Four of seven RCTs (16, 17, 21, 22) compared data on the post-operative CK-MB levels between selenium-supplemented and control group patients. A marginal difference was found in the postoperative CK-MB levels between the two groups (WMD = 0.73; 95% CI = −6.80–8.26; P = 0.85; I2 = 95%). Considering the high level of heterogeneity, we performed sensitivity analysis by removing one study (16), (WMD = −2.46; 95% CI = −9.74–4.83; P = 0.51; I2 = 61%) that greatly reduced the heterogeneity and showed lower postoperative CK-MB levels in selenium supplemented group (Figure 5).
Out of seven RCTs, three (17, 21, 22) of them provided data on the post-operative troponin I levels between selenium-supplemented and control group patients. The pooled analysis showed a borderline difference between the two groups with mild elevation of troponin I levels in the selenium supplemented group postoperatively (WMD = 0.09; 95% CI = −0.00–0.19; P = 0.06; I2 = 0%) (Figure 5). No in study heterogeneity was found during analysis (Figure 5).
In this comprehensive meta analysis we assessed the protective role of the bioactive agent, selenium, in the postoperative outcomes of patients undergoing cardiac surgery. Data from seven RCTs consisting of a total of 2,521 patients were pooled in this meta-analysis Our findings illustrate that administering selenium to patients undergoing cardiac surgery only slightly affected mortality, acute kidney injury, and LOS in hospital and ICU. Furthermore, individuals in the selenium group were demonstrated to have a greater risk of mortality, AKI and a longer ICU LOS as compared to the control group. Moreover, there was only a marginal statistical difference in the postoperative levels of cardiac biomarkers among the two comparable groups. Even though current literature has provided promising results regarding the benefits of selenium administration in cardiac surgery patients, our study found no firm data to validate the given hypothesis.
At present, there are several potential explanations that justify the benefits of selenium supplementation among patients undergoing cardiac surgery. A steep increase in OS, markedly reduced antioxidant (AOX) capacity, as well as postoperative inflammation has been observed among patients undergoing surgery (23). These factors not only lead to the development of organ failure but also increase mortality among such patients (24). According to evidence provided by current studies, selenium has been established as an essential element for improving heart functions and ameliorating heart injury (24). Selenium being a vital cofactor of various antioxidant enzymes could decrease the stress oxidative process and prevent postoperative complications after cardiac surgery (21, 25). Selenium in addition to other metals such as zinc and copper is vital for the functioning of the endogenous antioxidant system responsible for the degradation of free radicals produced as a result of various metabolic processes, thus maintaining a balance between oxidative stress and antioxidants available (9). Furthermore, it has been speculated that diminished selenium intake among patients with coronary heart disease and sepsis is a significant risk factor for an elevated post surgery mortality rate (26).
A wide variety of cohort and observational studies have evaluated the difference in the plasma levels of selenium pre and post cardiac surgery (7, 10, 17, 27). In a prospective observational trial of one hundred four cardiac surgical patients, a significant postoperative decline in circulating selenium levels was observed despite high-dose sodium-selenite administration prior to surgery (10). These cohort studies not only provided evidence regarding the drop in selenium levels post cardiac surgery but also demonstrated that low selenium levels are associated with severe complications post surgery (7, 10). It has been observed that the majority of the patients enrolled for cardiac surgery already have low selenium levels, implicating the pivotal role of this bioactive agent among these patients (6, 28). In a prospective observational clinical study, circulating selenium levels after completion of surgery were independently associated with the development of multi organ failure, peri operative inflammation and ICU length of stay (6). Additionally, Stevanovic et al. elucidated the importance of low postoperative selenium levels in predicting the likelihood of postoperative complications including organ dysfunction (29).
However, our meta analysis provided contrary findings regarding the protective role of selenium on post cardiac surgery complications. Several prospective studies in the past have illustrated that selenium supplementation was safe among cardiac surgery patients, but did not have any positive impact on post surgery clinical outcomes such as systemic inflammatory response and organ dysfunction (23, 30). This inconsistency in the findings between available data could be because of variable dosages of selenium supplementation among the different studies (10). Moreover, the limited sample size and the single-centered approach in the respective studies could also hinder the authenticity of the findings which should be interpreted with caution (23, 30). Further large scale multi centered studies are needed to provide a legitimate explanation for such ambiguity among findings of the protective role of selenium among patients undergoing cardiac surgery.
Vitamin C, another prominent antioxidant with distinctive organ-protective properties has also been evaluated for its cardioprotective effects. A meta analysis conducted to evaluate the correlation between peri operative vitamin C administration and overall outcomes after cardiac surgery revealed no significant effect on mortality (31). Furthermore, several meta analyses have assessed the protective role of iron supplementation on patients undergoing cardiac surgery (32–34). Yang et al. in their systematic review and meta analysis demonstrated no effect of iron supplementation on improved recovery of patients post cardiac surgery (31). Such corroboration with the results of previous meta analyses not only enhances the authenticity of our analysis but also highlights the ambiguity regarding the role of bioactive agents in postoperative outcomes of patients undergoing cardiac surgery, Furthermore, several studies (27, 35) have demonstrated the protective role of combined bioactive infusion rather than giving supplements separately. For example, a single centered trial aimed to investigate the impact of combined micronutrients supplementation (consisting of selenium, zinc, vitamin C, and vitamin B1), on clinical outcomes in ICU patients with conditions characterized by oxidative stress, revealed significant reductions in inflammatory response among the intervention group (35). Another similar study investigated the potency of peri operative metabolic therapy (consisting of coenzyme Q10, magnesium orotate, lipoic acid, omega-3 fatty acids, and selenium) among cardiac surgery patients (27). This study illustrated that such metabolic therapy is not only associated with enhanced redox status but is also linked with diminished myocardial damage and shortened length of hospital stay (27). Such consistency among the available studies could be employed to elucidate the protective role of a combined bioactive therapy rather than administering the bioactive agents separately.
It is imperative to note that the numerous benefits associated with selenium intake depend on its concentration and chemical structure. It has been highlighted by several studies that inorganic selenium and the daily ingestion of selenium exceeding 1 mg per 1 kg of body can be toxic to an average person (36). The recommended intake of selenium by the World Health Organization (WHO) was 30–40 mg per day for adult men and women (36). The main organic forms of selenium are selenomethionine (Semet) and selenocysteine (Secys), an essential component of selenoprotein which play a key role in numerous body functions including antioxidation (37). There has been increasing evidence regarding the risk of developing hyperglycemia and hence type 2 diabetes mellitus (T2DM) in addition to developing dyslipidemia among individuals with high selenium levels (11). Nevertheless, some studies have also illustrated the neutral or positive effect of selenium on T2DM. Therefore, further research is needed to clarify the potential benefits and adverse outcomes associated with different compositions of selenium in order to maximize its benefits among critical patients.
Until yet, no meta analysis has evaluated the protective role of the bioactive agent, selenium, on the post operative outcomes of patients undergoing cardiac surgery. Our meta analysis is the first pooled result of comparative trials of selenium vs. no selenium or placebo group in improving postoperative outcomes of cardiac surgery. The in-depth search approach employed in this study yielded only those studies that exclusively evaluated the protective role of selenium alone rather than infusing it in combination with other bioactive agents. The randomized, double or single-blinded, and placebo-controlled approach as well as the low risk of bias of the studies included in this comprehensive meta analysis further strengthens the credibility of our pooled analysis. However, a few limitations have hindered the authenticity and the acceptability of the results of this study. First, the comparatively moderate sample size and heterogeneity of the included population may not only limit the statistical power of the paper but may also prevent the results from being extrapolated in the general population. Another major limitation of this study was the variation in the dosages of selenium supplementation in the different RCTs included in our review and hence an absence of dose response analysis which could hinder the authenticity of the findings.
In conclusion, our meta analysis demonstrated no discernible effect of selenium infusion on post operative complications among patients undergoing cardiac surgery. Considering the crucial role of bioactive agents in post operative recovery of cardiac surgery patients, it has become vital to shift the focus of research towards bioactive metabolites such as selenium in reducing post operative mortality and morbidity. Further large scale multi centered studies comparing the protective role of selenium with combined therapy of bioactive agents are needed to provide an authentic explanation for the effectiveness of selenium that could be extrapolated in the general population.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
SR and HH conceived the idea; LI, FE, and MA did write up of the manuscript; and finally, MA, and SR reviewed the manuscript for intellectual content critically. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1235247/full#supplementary-material
1. Chaney MA, Il C. Outcome after cardiac surgery: the devil is in the details. J Cardiothorac Vasc Anesth. (2022) 36(1):91–2. doi: 10.1053/j.jvca.2021.10.025
2. Hutcheson R, Rocic P. The metabolic syndrome, oxidative stress, environment, and cardiovascular disease: the great exploration. Exp Diabetes Res. (2012) 2012:271028. doi: 10.1155/2012/271028
3. Vukicevic P, Klisic A, Neskovic V, Babic L, Mikic A, Bogavac-Stanojevic N, et al. Oxidative stress in patients before and after on-pump and off-pump coronary artery bypass grafting: relationship with syntax score. Oxid Med Cell Longev. (2021) 2021:3315951. doi: 10.1155/2021/3315951
4. Zakkar M, Guida G, Suleiman MS, Angelini GD. Cardiopulmonary bypass and oxidative stress. Oxid Med Cell Longev. (2015) 2015:189863. doi: 10.1155/2015/189863
5. Mohammadifard N, Humphries KH, Gotay C, Mena-Sánchez G, Salas-Salvadó J, Esmaillzadeh A, et al. Trace minerals intake: risks and benefits for cardiovascular health. Crit Rev Food Sci Nutr. (2019) 59(8):1334–46. doi: 10.1080/10408398.2017.1406332
6. Stoppe C, Schälte G, Rossaint R, Coburn M, Graf B, Spillner J, et al. The intraoperative decrease of selenium is associated with the postoperative development of multiorgan dysfunction in cardiac surgical patients. Crit Care Med. (2011) 39(8):1879–85. doi: 10.1097/CCM.0b013e3182190d48
7. Eslami G, Salehi R, Samaee H, Habibi V, Shokrzadeh M, Moradimajd P. Relationship between selenium trace and patient outcome after open-heart surgery. Anesth Pain Med. (2020) 10(4):e105895. doi: 10.5812/aapm.105895
8. Benstoem C, Goetzenich A, Kraemer S, Borosch S, Manzanares W, Hardy G, et al. Selenium and its supplementation in cardiovascular disease–what do we know? Nutrients. (2015) 7(5):3094–118. doi: 10.3390/nu7053094
9. Jenkins DJA, Kitts D, Giovannucci EL, Sahye-Pudaruth S, Paquette M, Blanco Mejia S, et al. Selenium, antioxidants, cardiovascular disease, and all-cause mortality: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. (2020) 112(6):1642–52. doi: 10.1093/ajcn/nqaa245
10. Stoppe C, Spillner J, Rossaint R, Coburn M, Schälte G, Wildenhues A, et al. Selenium blood concentrations in patients undergoing elective cardiac surgery and receiving perioperative sodium selenite. Nutrition. (2013) 29(1):158–65. doi: 10.1016/j.nut.2012.05.013
11. Huang JF, Hsu CP, Ouyang CH, Cheng CT, Wang CC, Liao CH, et al. The impact of selenium supplementation on trauma patients-systematic review and meta-analysis. Nutrients. (2022) 14(2):342. doi: 10.3390/nu14020342
12. Hill A, Clasen KC, Wendt S, Majoros ÁG, Stoppe C, Adhikari NKJ, et al. Effects of vitamin C on organ function in cardiac surgery patients: a systematic review and meta-analysis. Nutrients. (2019) 11(9):2103. doi: 10.3390/nu11092103
13. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
14. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
15. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Chichester (UK): Cochrane (2022). Available at: www.training.cochrane.org/handbook
16. Stoppe C, McDonald B, Meybohm P, Christopher KB, Fremes S, Whitlock R, et al. Effect of high-dose selenium on postoperative organ dysfunction and mortality in cardiac surgery patients: the SUSTAIN CSX randomized clinical trial. JAMA Surg. (2023) 37:1172–80. doi: 10.1001/jamasurg.2022.6855
17. Schmidt T, Pargger H, Seeberger E, Eckhart F, von Felten S, Haberthür C. Effect of high-dose sodium selenite in cardiac surgery patients: a randomized controlled bi-center trial. Clin Nutr. (2018) 37(4):1172–80. doi: 10.1016/j.clnu.2017.04.019
18. Amini S, Robabi HN, Tashnizi MA, Selenium VV. Vitamin C and N-acetylcysteine do not reduce the risk of acute kidney injury after off-pump CABG: a randomized clinical trial. Braz J Cardiovasc Surg. (2018) 33:129–34. doi: 10.21470/1678-9741-2017-0071
19. Laaf E, Benstoem C, Rossaint R, Wendt S, Fitzner C, Moza A, et al. High-dose supplementation of selenium in left ventricular assist device implant surgery: a double-blinded, randomized controlled pilot trial. J Parenter Enteral Nutr. (2022) 46(6):1412–9. doi: 10.1002/jpen.2309
20. Zeraati AA, Amini S, Samadi M, Mortazi H, Zeraati T, Samadi K. Evaluation of the preventive effect of selenium on acute kidney injury following on-pump cardiac surgery. Hypertension. (2021) 25(52):0–99. 10.32592/ircmj.2021.23.9.377
21. Sedighinejad A, Imantalab V, Mirmansouri A, Mohammadzadeh JA, Nassiri SN, Naderi NB, et al. Effect of selenium on ischemia-reperfusion injury in the coronary artery bypass graft surgery: a clinical trial study. Iran. Red. Crescent. Med. J. (2019) 21 doi: 10.5812/ircmj.42562
22. Shafa M, Azemati S, Abasi M, Hemati R. Effect of selenium added to the cardioplegic solution on cardiac protection in coronary artery bypass grafting surgeries: a randomized, double-blinded, clinical trial study. Iran Red Crescent Med J. (2019) 21(10). doi: 10.5812/ircmj.92737
23. Mirmansouri A, Imantalab V, Mohammadzadeh Jouryabi A, Kanani G, Naderi Nabi B, Farzi F, et al. Effect of selenium on stress response in coronary artery bypass graft surgery: a clinical trial. Anesth Pain Med. (2017) 7(1):e43864. doi: 10.5812/aapm.43864
24. Hardy G, Hardy I, Manzanares W. Selenium supplementation in the critically ill. Nutr Clin Pract. (2012) 27(1):21–33. doi: 10.1177/0884533611434116
25. Bleys J, Navas-Acien A, Guallar E. Serum selenium levels and all-cause, cancer, and cardiovascular mortality among US adults. Arch Intern Med. (2008) 168(4):404–10. doi: 10.1001/archinternmed.2007.74
26. Angstwurm MW, Engelmann L, Zimmermann T, Lehmann C, Spes CH, Abel P, et al. Selenium in intensive care (SIC): results of a prospective randomized, placebo-controlled, multiple-center study in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Crit Care Med. (2007) 35(1):118–26. doi: 10.1097/01.CCM.0000251124.83436.0E
27. Leong JY, van der Merwe J, Pepe S, Bailey M, Perkins A, Lymbury R, et al. Perioperative metabolic therapy improves redox status and outcomes in cardiac surgery patients: a randomised trial. Heart Lung Circ. (2010) 19(10):584–91. doi: 10.1016/j.hlc.2010.06.659
28. Rayman MP. The importance of selenium to human health. Lancet. (2000) 356(9225):233–41. doi: 10.1016/S0140-6736(00)02490-9
29. Stevanovic A, Coburn M, Menon A, Rossaint R, Heyland D, Schälte G, et al. The importance of intraoperative selenium blood levels on organ dysfunction in patients undergoing off-pump cardiac surgery: a randomised controlled trial. PLoS One. (2014) 9(8):e104222. doi: 10.1371/journal.pone.0104222
30. Sedighinejad A, Imantalab V, Mirmansouri A, Mohammadzadeh Jouryabi A, Kanani G, Nassiri Sheikhani N, et al. Effects of low-dose selenium on the inflammatory response in coronary artery bypass graft surgery: a clinical trial. Iran Red Crescent Med J. (2016) 18(8):e37918. doi: 10.5812/ircmj.37918
31. Koszta G, Kacska Z, Szatmári K, Szerafin T, Fülesdi B. Lower whole blood selenium level is associated with higher operative risk and mortality following cardiac surgery. J Anesth. (2012) 26(6):812–21. doi: 10.1007/s00540-012-1454-y
32. Yang SS, Al Kharusi L, Gosselin A, Chirico A, Baradari PG, Cameron MJ. Iron supplementation for patients undergoing cardiac surgery: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth. (2022) 69(1):129–39. doi: 10.1007/s12630-021-02113-z
33. Gupta S, Panchal P, Gilotra K, Wilfred AM, Hou W, Siegal D, et al. Intravenous iron therapy for patients with preoperative iron deficiency or anaemia undergoing cardiac surgery reduces blood transfusions: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. (2020) 31(2):141–51. doi: 10.1093/icvts/ivaa094
34. Zhao L, Yang X, Zhang S, Zhou X. Iron metabolism-related indicators as predictors of the incidence of acute kidney injury after cardiac surgery: a meta-analysis. Ren Fail. (2023) 45(1):2201362. doi: 10.1080/0886022X.2023.2201362
35. Berger MM, Soguel L, Shenkin A, Revelly JP, Pinget C, Baines M, et al. Influence of early antioxidant supplements on clinical evolution and organ function in critically ill cardiac surgery, major trauma, and subarachnoid hemorrhage patients. Crit Care. (2008) 12(4):R101. doi: 10.1186/cc6981
36. Lee SH, Kwon SW, Lee Y, Nam SH. Fast and simple selenium speciation by solid phase extraction and laser-induced breakdown spectroscopy. J Anal Sci Technol. (2020) 11(1):1–8. doi: 10.1186/s40543-019-0200-6
Keywords: AKI, cardiac surgery, meta analysis, oxidative damage, selenium
Citation: Rehan ST, Hussain Hu, Imran L, Eqbal F and Asghar MS (2023) Perioperative selenium administration in cardiac surgery patients, a way out to reduce post surgical adversities? A meta analysis. Front. Cardiovasc. Med. 10:1235247. doi: 10.3389/fcvm.2023.1235247
Received: 6 June 2023; Accepted: 15 August 2023;
Published: 29 August 2023.
Edited by:
Giuseppe Gatti, Azienda Sanitaria Universitaria Giuliano Isontina, ItalyReviewed by:
Miha Antonic, Maribor University Medical Centre, Slovenia© 2023 Rehan, Hussain, Imran, Eqbal and Asghar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muhammad Sohaib Asghar c29oYWliX2FzZ2hhcjEyM0B5YWhvby5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.