- 1Clinical Epidemiology Research Office, The First Affiliated Hospital of Hunan Normal University, Changsha, China
- 2Key Laboratory of Molecular Epidemiology, Hunan Normal University, Changsha, China
- 3Department of Epidemiology and Statistics, College of Medicine, Hunan Normal University, Changsha, China
- 4Research Department, The First Affiliated Hospital of Hunan Norma University, Changsha, China
Background: Recent studies have reported better predictive performance of triglyceride glucose (TyG) index for cardiovascular events in women, however, whether this association persists in postmenopausal women is inconclusive. We investigated the association between TyG index and H-type hypertension (HHT) in postmenopausal women.
Methods: 1,301 eligible women with hypertension were included in this cross-sectional study. Concomitant homocysteine levels >10 μmol/L were defined as H-type hypertension. The TyG index was calculated as ln [triglycerides (mg/dl) × fasting glucose (mg/dl)/2]. Multivariable logistic regression models and restricted cubic spline models were used to assess the association between TyG index and H-type hypertension in postmenopausal women, and subgroup analyses were performed for potential confounders.
Results: Of the 1,301 hypertensive patients, 634 (48.7%) participants had H-type hypertension. In each adjusted model, TyG index was significantly associated with the risk of H-type hypertension. each 1-unit increase in TyG index was associated with an increased risk of H-type hypertension in all participants (OR = 1.6; 95% CI, 1.3–2.0; P < 0.001), and there was a linear relationship between TyG index and H-type hypertension (P for linear trend < 0.001).
Conclusion: TyG index is positively associated with H-type hypertension in postmenopausal women, suggesting that TyG index may be a promising marker for H-type hypertension. By controlling lipid levels and blood glucose levels, it may help prevent H-type hypertension in postmenopausal women.
1. Introduction
As the most common cardiovascular disease, hypertension affects more than 1.278 billion people worldwide aged 30 to 79 years (1). Hypertension with homocysteine (Hcy) levels above 10 μ/L suggests H-type hypertension (2). In China, more than 70% of hypertensive patients have elevated plasma homocysteine levels (3). A cross-sectional study showed that hyperhomocysteinemia(HHcy) and hypertension are two independent, modifiable risk factors that add up to an increased risk of cardiovascular and cerebrovascular events (4). Therefore, early intervention of H-type hypertension is quite important.
Insulin resistance (IR) is a well-known predictor of many cardiovascular diseases (CVD) (5, 6). A hyperinsulin-normoglycemic clamp is the gold standard for measuring IR, but it is too expensive and complex to be used in clinical settings. Recently, triglyceride glucose (TyG) index, calculated from triglycerides (TG) and fasting glucose (FPG), has been proposed as a reliable alternative marker for IR (7). The TyG index is more sensitive and specific for the diagnosis of IR than past alternatives such as the homeostatic model insulin resistance index (HOMA-IR) and TG/HDL-C (8). The association between TyG index and hypertension has been demonstrated in relevant epidemiologic studies (9, 10).
As estrogen levels decline in postmenopausal women, cardiovascular diseases such as hypertension and hyperhomocysteinemia are more prevalent (11). H-type hypertension is more prevalent in postmenopausal women than in premenopausal women and men of the same age (12, 13). In addition, in postmenopausal women, IR is more likely to result from weight gain or abdominal obesity (14). According to previous studies, TyG index has better predictive efficacy in women than in men when it comes to major adverse cardiovascular events (15). This may be due to increased insulin resistance and decreased estrogen levels in postmenopausal women, but validation is still lacking. Thus, this cross-sectional study explores the relationship between TyG index and H-type hypertension among postmenopausal women.
2. Materials and methods
2.1. Study population
This cross-sectional study included 1,301 female patients treated at Hunan Provincial People's Hospital between January 2021 and January 2023 without missing data. Participant inclusion criteria: (1) postmenopausal women (cessation of menstruation for more than 1 year); (2) Diagnosis of essential hypertension; (3) cooperation with the survey and signing of informed consent form. Exclusion criteria: (1) participants who had used medications that could impact their blood pressure and homocysteine levels; (2) Patients who are unable to accurately describe their own state, such as mental illness, speech problems, etc.
All study participants signed an informed consent form before taking part in the study, which was evaluated and approved by the Medical Ethics Committee of Hunan Normal University (No. 034/2017). After data collection, all participant information is kept anonymous and each participant is given a code. No names are ever published in any way.
2.2. Sample size calculation
Sample size calculations were based on the prevalence of H-type hypertension among hypertensive patients using a single population proportion sample size formula. According to the literature review, the proportion of H-type hypertension in the Chinese hypertensive population was 73% (3), and a minimum sample size of 1,250 cases was required for the study, assuming an α of 0.05, a β of 0.80 and a 95% confidence interval.
2.3. Data collection and definitions
The data collection consisted of questionnaires, physical examination and laboratory tests. The questionnaire was administered by a uniformly trained investigator by face-to-face questioning, which included basic information, smoking history, drinking history, diet and physical activity.
Educational background was categorized into four groups: primary school and below, junior school, senior school, and college and above. Single or married were the two categories for marital status. Patients' level of regular activity was assessed based on how many times they worked out each week: 0 represented no exercise, 1–3 represented irregular exercise, and >3 represented regular exercise. We defined current alcohol intake as having at least two drinks per week and current smoking as continuously or cumulatively smoking one or more cigarettes per day for six months. The definition of covariates was informed by a previous questionnaire designed by the subject group for a cross-sectional survey of H-type hypertension (16).
Measurements of height, weight, waist circumference, and blood pressure are all part of a physical examination. A trained nurse used a conventional mercury sphygmomanometer to take three blood pressure readings at baseline, following a strategy that was developed from the American Heart Association's guidelines. A systolic blood pressure (SBP) ≥ 140 mmHg and/or a diastolic blood pressure (DBP) ≥ 90 mmHg were considered to be a diagnosis of hypertension (17). Patients with H-type hypertension were those who were diagnosed with essential hypertension and had a Hcy level >10 mol/L (18).
Within 24 h of admission, we took 5 ml of fasting venous blood and sent it to the Hunan Provincial People's Hospital's Department of Laboratory Medicine's fully automated biochemical analyzer to measure triglycerides (TG), fasting blood glucose (FPG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), alanine transaminase (ALT), serum cr (Scr) and estimated glomerular filtration rate (eGFR).
2.4. Triglyceride-glucose index calculation
The values for glucose and triglycerides were converted from mmol/l to mg/dl. (multiplied by 18.020 and 88.545, respectively) (19). Triglyceride-glucose index was calculated as ln [triglycerides (mg/dl) × fasting glucose (mg/dl)/2] (20).
2.5. Statistical methods
Categorical variables were presented as numbers (n) and percentages (%), and the χ2 test was used to compare group differences. Data for normally distributed continuous variables are expressed as mean ± standard deviation (SD), and t-tests were used to compare differences between groups. Data for continuous variables with skewed distribution were expressed as median (interquartile spacing), which was examined by the Mann-Whitney test. Before applying the tests, its normality was checked with the Kolmogorov–Smirnov test, and its homoscedasticity was checked with Levene's test. We utilized multivariable logistic regression models to examine the association between Tyg quartile subgroups and risk of H-type hypertension after adjusting for known possible confounders between TyG and H-type hypertension as well as for covariates at P < 0.05 in univariate analysis. We created three models: model 1 was unadjusted; model 2 included adjustments for age, BMI, educational background, exercise, smoking and drinking history; model 3: The variables LDL, BUN, and eGFR were subsequently added to model 2. We observed no significant covariance between these variables (all VIF < 3) (Supplementary Table S1). To investigate the form of the association between the TyG index and H-type hypertension, we also used a restricted triple spline with three nodes (5th, 50th, and 90th percentiles), each truncated at the highest and lowest 0.5% of the TyG index. To determine whether relevant factors (age, body mass index, eGFR, smoking, alcohol consumption, and exercise history) influenced the association between TyG index and H-type hypertension, we performed subgroup analyses in which an interaction term was added to the logistic regression model. For different definitions of H-type hypertension (Hcy levels ≥ 15 μ/L), we further performed sensitivity analyses to explore whether the association continued to exist. All statistical analyses were performed using SPSS 25.0 and R 4.1.2, and the study was conducted using a two-sided test for p-values, with p < 0.05 considered significant.
3. Results
3.1. Baseline characteristics of included hypertension patients
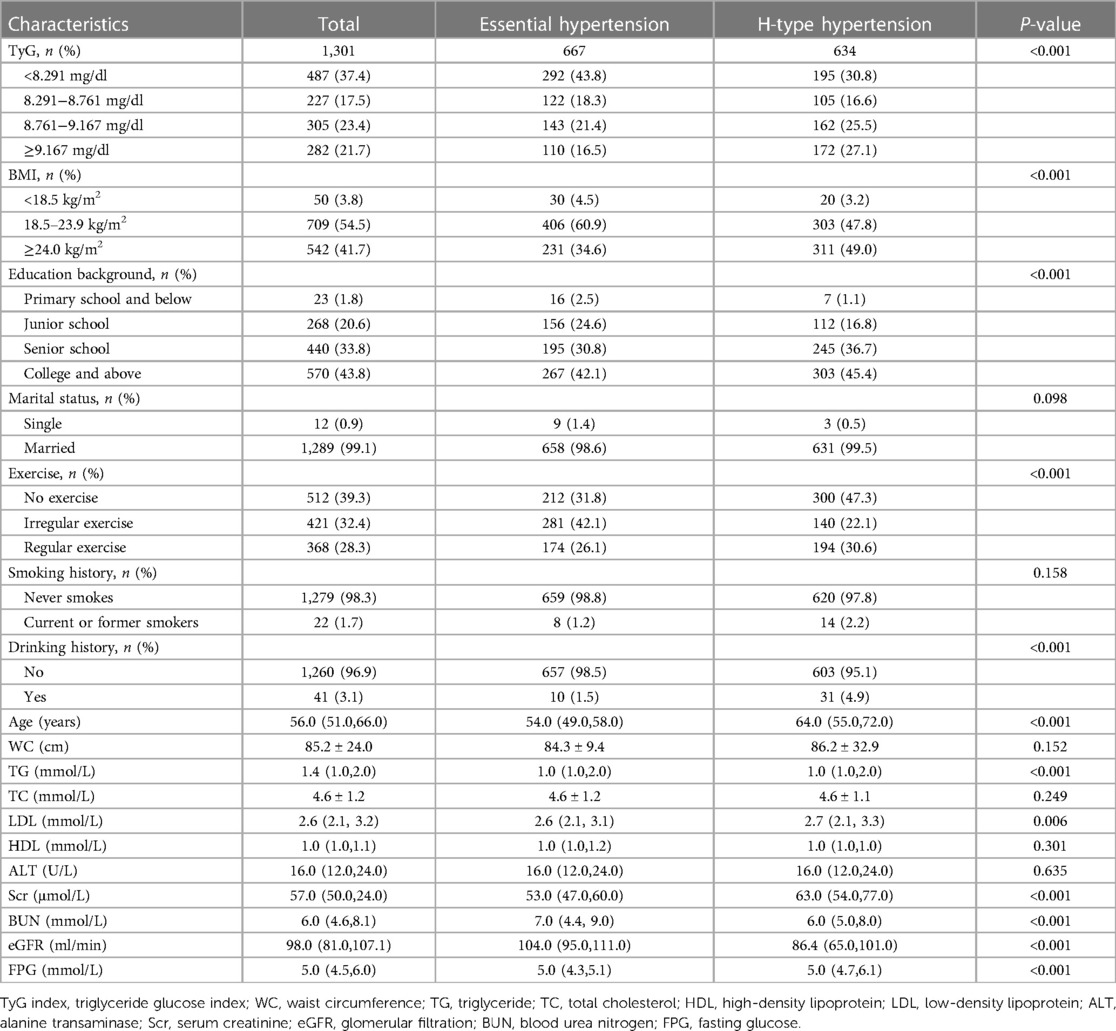
In this investigation, we examined 1,301 postmenopausal women who had essential hypertension. The individuals' median TyG index concentration was 8.761 mg/dl (interquartile range, 8.291–9.167), and their median age (interquartile range) was 56.0 (51.0–66.0) years. By hypertension status, Table 1 displays the participant baseline characteristics. This investigation revealed 634 (48.7%) patients with H-type hypertension overall, with statistically significant variations in TyG quartile subgroups. In comparison to controls, obesity, low education, insufficient physical activity, and alcohol use were all linked to an elevated risk of H-type hypertension. Additionally, individuals with H-type hypertension had significantly lower eGFR and significantly higher levels of TG, LDL, Scr, BUN and FPG (P < 0.05).
3.2. Odds ratios of TyG index for H-type hypertension
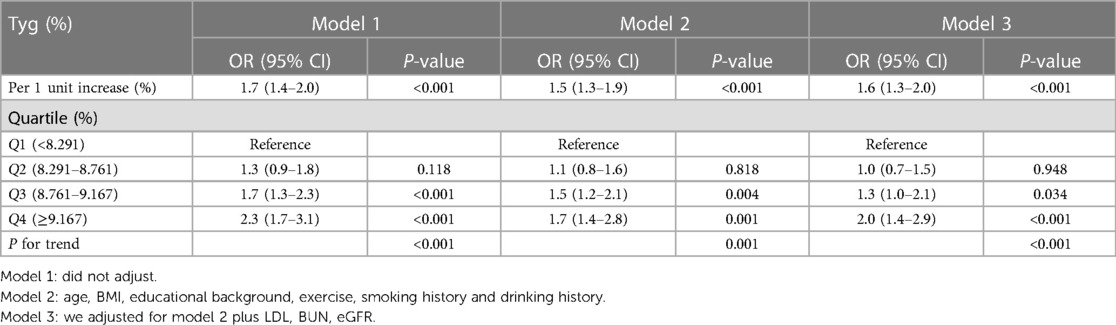
Table 2 illustrates the connection between the TyG index and H-type hypertension. When compared to the lowest quartile of the TyG index, the ORs (95% CI) for H-type hypertension were 2.3 (1.7–3.1) in univariate analysis for the highest quartile. In a logistic regression model (model 3) adjusted for a number of confounders (age, BMI, educational background, exercise, smoking history, drinking history, LDL, BUN, eGFR), higher TyG index remained significantly associated with increased risk of H-type hypertension. The fully adjusted OR (95% CI) for the risk of HHT in quartile 4 vs. quartile 1 was 2.0 (1.4–2.9; P < 0.001). The TyG index was also examined as a continuous variable. According to model 3, postmenopausal women's chance of developing H-type hypertension increased by 0.6 (95% CI: 1.3–2.0; P < 0.001) per unit increase in TyG index. The association between TyG index and H-type hypertension remained significant even after adjustment for potential confounders.
3.3. Linear relationship between TyG index and H-type hypertension
The TyG index and H-type hypertension were shown to be correlated linearly by restricted cubic spline regression models (P for linear trend < 0.001; Figure 1). The reference point is the cutoff value of the first quartile (8.291 mg/dl), and the nodes are located at the TyG index's horizontal range at the 5th, 50th, and 90th percentiles. The trend test (P < 0.001) between Tyg quartiles in the unadjusted model and the two adjusted models further illustrates the linear relationship, as shown in Table 2. The findings imply that a persistent rise in the TyG index increases the chance of postmenopausal women acquiring H-type hypertension.
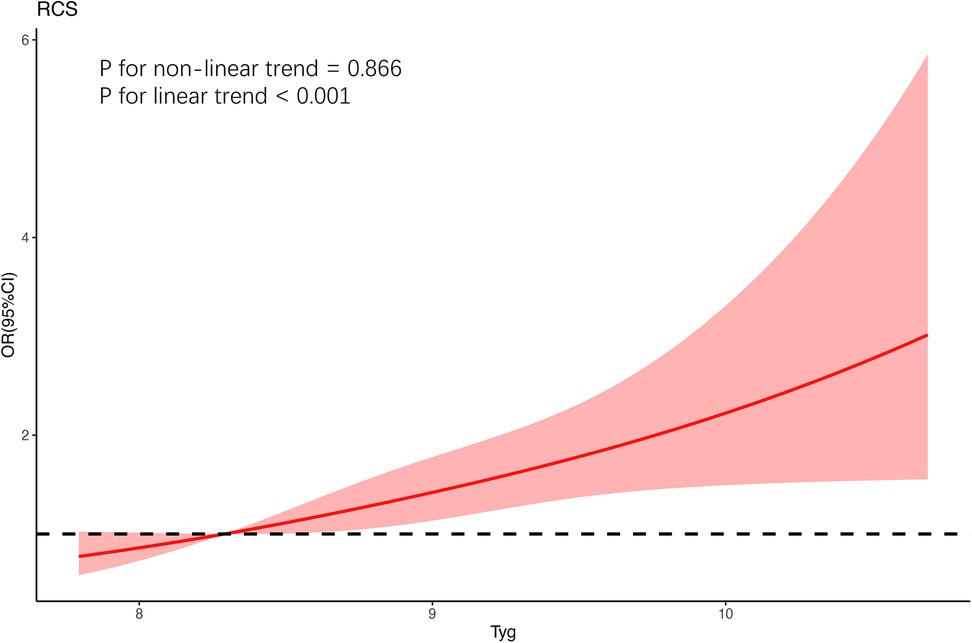
Figure 1. The restricted cubic spline for the association between postmenopausal women's TyG index and HHT. As a cut-off value for the first quartile, the reference value for TyG was established. For the model, restricted cubic spline regression was trimmed at the highest and lowest 0.5% of each TyG index, with the nodes in the three TyG indices at the 5th, 50th and 95th percentiles, and the variables for age, BMI, educational background, exercise, smoking and drinking history, LDL, BUN, and eGFR were all modified.
3.4. Subgroup analysis
With regard to age, BMI, smoking history, drinking history, exercise, eGFR, subgroup analysis revealed that TyG index was positively associated with H-type hypertension. Futhermore there were no significant interactions between TyG index and these potential risk factors of interest for H-type hypertension (P > 0.05 for all interactions) (Figure 2).
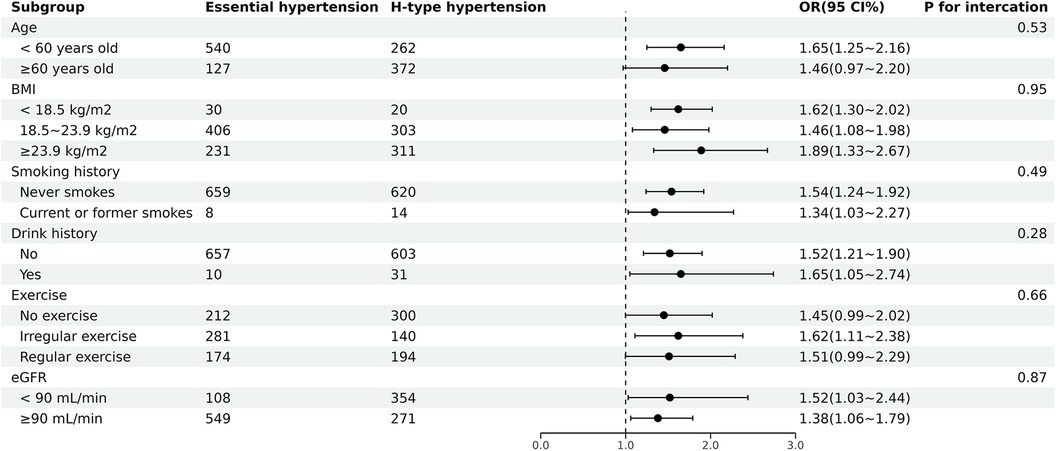
Figure 2. Subgroup analyses of the association between TyG index and H-type hypertension. ORs were adjusted for age, BMI, educational background, exercise, smoking history and drinking history, LDL, BUN, eGFR.
3.5. Sensitivity analysis
As shown in Table 3, the results were stabilized (OR = 1.4; 95% CI, 1.1–1.9; P = 0.008) by sensitivity analyses for different definitions of H-type hypertension (Hcy levels ≥ 15μ/L).
4. Discussion
In this cross-sectional study based on essential hypertension in postmenopausal women, we found that a higher TyG index was associated with the development of H-type hypertension in postmenopausal women. a positive dose-dependent association of TyG index with the risk of prevalence was obtained, after adjusting for possible confounders. Similar results were seen in subgroup analysis, highlighting the strength of these correlations even more.
There are two possible mechanisms by which excessive TyG leads to an increased risk of developing H-type hypertension. First, IR causes a decrease in the efficiency of glucose uptake and utilization by insulin in the body, resulting in compensatory secretion of excess insulin by the body. Excess insulin increases sympathetic nervous system activity and promotes the body to secrete more epinephrine and norepinephrine, which ultimately increases cardiac output and peripheral vascular resistance, and thickens vascular smooth muscle (20). In addition, IR has been shown to induce inappropriate activation of the renin-angiotensin-aldosterone system and the sympathetic nervous system (21), which may have a negative impact on renal function and, in turn, cause elevated Hcy levels. At the same time, elevated Hcy levels can cause increased secretion of various inflammatory factors, leading to abnormalities in the function of adipose tissue, promoting the production and secretion of resistin, which in turn promotes the occurrence of inflammatory reactions and insulin resistance (22, 23). Second, as two components of TyG, both TG and FPG are closely associated with the development of H-type hypertension. Hcy can increase oxidized LDL levels through oxidative modifications, prompting macrophages to take up large amounts of lipids to transform into foam cells and accelerate the deposition of cholesterol and TG on the vascular wall, while causing a large depletion of HDL, thus diminishing its ability to reverse cholesterol transport. This ultimately leads to the development of cardiovascular events, suggesting an association between HHcy and high TG (24). At the same time, a large number of epidemiological studies have shown that most hypertensive patients have dyslipidemia (25) and it has been demonstrated that lipid accumulation index (LAP) levels are higher in patients with H-type hypertension than in patients with non-H-type hypertension (26). Clinical observations have shown that hypertensive patients with elevated Hcy levels are positively associated with insulin resistance and diabetes mellitus (27–29), suggesting an association between FPG and H-type hypertension.
Previous studies have found gender differences in the relationship between TyG index and cardiovascular disease (15). As women age, ovarian function declines, estrogen decreases, and the body experiences a range of menopause-related symptoms (30). At the same time, as the protective effect of estrogen gradually decreases, the cardiovascular system of postmenopausal women undergoes significant changes, especially the risk of developing hypertension is significantly increased (31), and Hcy is also significantly higher in postmenopausal women (32). Epidemiological studies have demonstrated that menopause has become an independent risk factor for increased cardiovascular disease morbidity and mortality in women (33). Gender differences in the association between traditional cardiovascular risk factors can be explained by increased insulin resistance and lower estrogen levels in menopausal women, leading to an increased risk of cardiovascular disease (34). Our investigation reported similar findings suggesting that insulin resistance (high TyG index) is a risk factor for H-type hypertension in postmenopausal women. It is suggested that the development of H-type hypertension can be reduced by controlling FPG and TG and thus lowering the TyG index.
Despite these benefits and possible clinical applications, numerous study limitations must be taken into account when analyzing the findings. Firstly, in our cross-sectional survey, the possibility of residual confounding factors cannot be completely ruled out, this limits our ability to establish a causal relationship between TyG index and H-type hypertension in hypertensive patients. Therefore, to confirm the current findings, larger prospective investigations are required in the future. Finally, because we only examined postmenopausal women, it is not possible to extrapolate our findings to other populations.
5. Conclusions
In the present cross-sectional study, we found that the TyG index was independently associated with the development of H-type hypertension in postmenopausal women, and this simple index may be useful in identifying those at risk for H-type hypertension. We recommend that postmenopausal women control their lipid levels (TG) and blood glucose levels (FPG) levels, which may help prevent H-type hypertension.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Hunan Normal University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZD: conceptualization, methodology, formal analysis, and writing – original draft. SD: conceptualization, supervision, and writing – review and editing. YY: conceptualization and writing – review and editing. YT: methodology and writing – review and editing. XH: resources, supervision, writing – review and editing, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the National Natural Science Foundation of China (8177120863), Hunan Provincial Science and Technology Department (2020JJ4047) and Science and Technology Bureau, Changsha (kq1801096).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1224296/full#supplementary-material
References
1. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet (London, England). (2021) 398:957–80. doi: 10.1016/S0140-6736(21)01330-1
2. Li J, Jiang S, Zhang Y, Tang G, Wang Y, Mao G, et al. H-type hypertension and risk of stroke in Chinese adults: a prospective, nested case-control study. J Transl Int Med. (2015) 3:171–8. doi: 10.1515/jtim-2015-0027
3. Liang Z, Fan FF, Zhang Y, Qin XH, Li JP, Huo Y. Rate and characteristics of H-type hypertension in Chinese hypertensive population and comparison with American population. Beijing Da Xue Xue Bao Yi Xue Ban. (2022) 54:1028–37. doi: 10.19723/j.issn.1671-167X.2022.05.033
4. Wang W, Ji P, Wang Y, Guo H, Bian R, Xu J, et al. Prevalence of hyperhomocysteinemia and its associated factors in patients with primary hypertension in Chinese urban communities: a cross-sectional study from Nanjing. Clin Exp Hypertens. (2018) 40:495–500. doi: 10.1080/10641963.2017.1403621
5. Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. (2018) 17:122. doi: 10.1186/s12933-018-0762-4
6. Laakso M. Is insulin resistance a feature of or a primary risk factor for cardiovascular disease? Curr Diab Rep. (2015) 15:105. doi: 10.1007/s11892-015-0684-4
7. Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. (2010) 95:3347–51. doi: 10.1210/jc.2010-0288
8. Khan SH, Sobia F, Niazi NK, Manzoor SM, Fazal N, Ahmad F. Metabolic clustering of risk factors: evaluation of triglyceride-glucose index (TyG index) for evaluation of insulin resistance. Diabetol Metab Syndr. (2018) 10:74. doi: 10.1186/s13098-018-0376-8
9. Deng D, Chen C, Wang J, Luo S, Feng Y. Association between triglyceride glucose-body mass index and hypertension in Chinese adults: a cross-sectional study. J Clin Hypertens (Greenwich). (2023) 25(4):370–9. doi: 10.1111/jch.14652
10. Zheng R, Mao Y. Triglyceride and glucose (TyG) index as a predictor of incident hypertension: a 9-year longitudinal population-based study. Lipids Health Dis. (2017) 16:175. doi: 10.1186/s12944-017-0562-y
11. Yeasmin N, Akhter QS, Mahmuda S, Banu N, Yeasmin S, Akhter S, Nahar S. Association of hypertension with serum estrogen level in postmenopausal women. Mymensingh Med J. (2017) 26(3):635–41. 28919621
12. Zhu Z, Jiang S, Li C, Liu J, Tao M. Relationship between serum homocysteine and different menopausal stage. Climacteric. (2020) 23:59–64. doi: 10.1080/13697137.2019.1634045
13. Hodis HN, Mack WJ, Henderson VW, Shoupe D, Budoff MJ, Hwang-Levine J, et al. Vascular effects of early versus late postmenopausal treatment with estradiol. N Engl J Med. (2016) 374:1221–31. doi: 10.1056/NEJMoa1505241
14. Chedraui P, Pérez-López FR, Escobar GS, Palla G, Montt-Guevara M, Cecchi E, et al. Research group for the Omega women’s health project. Circulating leptin, resistin, adiponectin, visfatin, adipsin and ghrelin levels and insulin resistance in postmenopausal women with and without the metabolic syndrome. Maturitas. (2014) 79:86–90. doi: 10.1016/j.maturitas.2014.06.008
15. Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, et al. Triglyceride–glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the kailuan cohort. Cardiovasc Diabetol. (2021) 20:19. doi: 10.1186/s12933-020-01210-5
16. Du S, Hong X, Yang Y, Ding Z, Yu T. Association between body fat percentage and H-type hypertension in postmenopausal women. Front Public Health. (2022) 10:950805. doi: 10.3389/fpubh.2022.950805
17. European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European society of hypertension-European society of cardiology guidelines for the management of arterial hypertension. J Hypertens. (2003) 21:1011–53. doi: 10.1097/00004872-200306000-00001
18. Qin X, Huo Y. H-Type hypertension, stroke and diabetes in China: opportunities for primary prevention. J Diabetes. (2016) 8:38–40. doi: 10.1111/1753-0407.12333
19. Miao M, Zhou G, Bao A, Sun Y, Du H, Song L, et al. Triglyceride-glucose index and common carotid artery intima-media thickness in patients with ischemic stroke. Cardiovasc Diabetol. (2022) 21:43. doi: 10.1186/s12933-022-01472-1
20. Ma X, Dong L, Shao Q, Cheng Y, Lv S, Sun Y, et al. Triglyceride glucose index for predicting cardiovascular outcomes after percutaneous coronary intervention in patients with type 2 diabetes mellitus and acute coronary syndrome. Cardiovasc Diabetol. (2020) 19:31. doi: 10.1186/s12933-020-01006-7
21. Tack CJ, Smits P, Willemsen JJ, Lenders JW, Thien T, Lutterman JA. Effects of insulin on vascular tone and sympathetic nervous system in NIDDM. Diabetes. (1996) 45:15–22. doi: 10.2337/diab.45.1.15
22. Zhou M-S, Schulman IH, Zeng Q. Link between the renin-angiotensin system and insulin resistance: implications for cardiovascular disease. Vasc Med. (2012) 17:330–41. doi: 10.1177/1358863X12450094
23. Yang N, Yao Z, Miao L, Liu J, Gao X, Fan H, et al. Novel clinical evidence of an association between homocysteine and insulin resistance in patients with hypothyroidism or subclinical hypothyroidism. PLoS One. (2015) 10:e0125922. doi: 10.1371/journal.pone.0125922
24. Schaffer A, Verdoia M, Cassetti E, Marino P, Suryapranata H, De Luca G, et al. Relationship between homocysteine and coronary artery disease. Results from a large prospective cohort study. Thromb Res. (2014) 134:288–93. doi: 10.1016/j.thromres.2014.05.025
25. Deng X, Hou H, Wang X, Li Q, Li X, Yang Z, et al. Development and validation of a nomogram to better predict hypertension based on a 10-year retrospective cohort study in China. Elife. (2021) 10:e66419. doi: 10.7554/eLife.66419
26. Yuan W, Shao Y, Zhao D, Zhang B. Correlation analysis of lipid accumulation index, triglyceride-glucose index and H-type hypertension and coronary artery disease. PeerJ. (2023) 11:e16069. doi: 10.7717/peerj.16069
27. Catena C, Colussi G, Nait F, Capobianco F, Sechi LA. Elevated homocysteine levels are associated with the metabolic syndrome and cardiovascular events in hypertensive patients. Am J Hypertens. (2015) 28:943–50. doi: 10.1093/ajh/hpu248
28. Pang H, Han B, Fu Q, Zong Z. Association of high homocysteine levels with the risk stratification in hypertensive patients at risk of stroke. Clin Ther. (2016) 38:1184–92. doi: 10.1016/j.clinthera.2016.03.007
29. Wang C, Wu Q, Zhang L, Hao Y, Fan R, Peng X, et al. Elevated total plasma homocysteine levels are associated with type 2 diabetes in women with hypertension. Asia Pac J Clin Nutr. (2015) 24:683–91. doi: 10.6133/apjcn.2015.24.4.09
30. Armeni A, Anagnostis P, Armeni E, Mili N, Goulis D, Lambrinoudaki I. Vasomotor symptoms and risk of cardiovascular disease in peri- and postmenopausal women: a systematic review and meta-analysis. Maturitas. (2023) 171:13–20. doi: 10.1016/j.maturitas.2023.02.004
31. El Khoudary SR. Age at menopause onset and risk of cardiovascular disease around the world. Maturitas. (2020) 141:33–8. doi: 10.1016/j.maturitas.2020.06.007
32. Wang Y, Zhao L, Gao L, Pan A, Xue H. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. (2021) 9:446–61. doi: 10.1016/S2213-8587(21)00118-2
33. Chou C-C, Chien L-Y, Lin M-F, Wang C-J. Cognitive function and associated factors among postmenopausal women with hypertension and natural menopause in Taiwan. Geriatr Nurs. (2021) 42:110–6. doi: 10.1016/j.gerinurse.2020.12.007
Keywords: H-type hypertension, triglyceride glucose index, insulin resistance, postmenopausal women, cross-sectional study
Citation: Ding Z, Du S, Yang Y, Yu T and Hong X (2023) Association between triglyceride glucose index and H-type hypertension in postmenopausal women. Front. Cardiovasc. Med. 10:1224296. doi: 10.3389/fcvm.2023.1224296
Received: 17 May 2023; Accepted: 18 October 2023;
Published: 1 November 2023.
Edited by:
Belen Ponte, Hôpitaux universitaires de Genève (HUG), SwitzerlandReviewed by:
Fangfang Fan, Peking University, ChinaXiang Ma, First Affiliated Hospital of Xinjiang Medical University, China
© 2023 Ding, Du, Yang, Yu and Hong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuqin Hong eGl1cWluaG9uZzA1MjhAaHVubnUuZWR1LmNu
 Zihao Ding
Zihao Ding Shihong Du
Shihong Du Yi Yang1,2
Yi Yang1,2 Xiuqin Hong
Xiuqin Hong