- 1School of Public Health, North China University of Science and Technology, Tangshan, China
- 2Department of Cardiology, Kailuan General Hospital, Tangshan, China
- 3Department of Neurosurgery, Affiliated Hospital of North China University of Science and Technology, Tangshan, China
Background: The association between mean arterial pressure (MAP) trajectory in young adults and risk of cardiovascular diseases (CVD) and all-cause mortality is not well-characterized. The objective of this study was to investigate the effects of different MAP trajectory on the risk of CVD and all-cause mortality among the young.
Methods: In the Kailuan cohort study, 19,171 participants aged 18–40 years were enrolled without CVD (including myocardial infarction, stroke, atrial fibrillation and heart failure). The potential hybrid model was used to fit different trajectory patterns according to longitudinal changes of MAP. Hazard ratios and 95% confidence intervals for risk of CVD and all-cause mortality were analyzed using Cox proportional hazard regression models for participants with different trajectories.
Results: Five distinct MAP trajectories were identified during 2006–2013. Each of the trajectories was labelled as low-stable, middle-stable, decreasing, increasing, or high-stable. With the low-stable trajectory group as the reference, the multivariate adjusted HR (95%CI) of CVD for the middle-stable, decreasing, increasing and high-stable groups were 2.49 (1.41–4.40), 5.18 (2.66–10.06), 5.91 (2.96–11.80) and 12.68 (6.30–25.51), respectively. The HR (95%CI) for all-cause deaths were 1.27 (0.84–1.94), 2.01 (1.14–3.55), 1.96 (1.04–4.3.72), and 3.28 (1.69–6.37), respectively.
Conclusion: In young adults, MAP trajectories were associated with the risk of CVD or all-cause mortality and increasing MAP trajectories within the currently designated “normal” range may still increase the risk for CVD.
1. Introduction
Hypertension has been universally acknowledged as a paramount risk factor for cardiovascular diseases (CVD) and stroke (1, 2), rendering it the primary cause of worldwide disability and mortality (3). On an annual basis, high blood pressure accounts for over 9 million deaths, half of which are specifically attributed to CVD and stroke (4). Recent epidemiological studies have indicated a striking 50% surge in the incidence of CVD within young populations across the globe over the past decade, with a notable prevalence of 10%–15% occurring among adults aged 18–50 years (5). Despite this concerning trend, limited research has delved into the prospective impact of blood pressure on CVD within the confines of this youthful cohort.
Research data has revealed that approximately 70% of cardiovascular diseases (CVD) can be attributed to high blood pressure (6–9). Traditionally, the assessment of cardiovascular risk has relied on two primary components derived from the pressure waveform, one of which encompasses the stable aspect represented by mean arterial pressure (MAP) (10). While prior studies have predominantly concentrated on the individual impact of systolic blood pressure (SBP), diastolic blood pressure (DBP) (11), or pulse pressure (PP) (12) as independent risk factors, the potential influence of long-term MAP on CVD outcomes or mortality has received limited attention. Notably, MAP has demonstrated a superior predictive capability compared to SBP and DBP in forecasting the risk of CVD (13). Over the past two decades, the prognostic utility of MAP in predicting cardiovascular events and mortality has been extensively acknowledged. For instance, a substantial cohort study involving a vast population (N = 69,989; aged 40–69; mean follow-up time of 9.5 years) underscored the influential role of MAP (14), determined based on brachial arterial blood pressure measurements, in determining cardiovascular mortality.
However, a single blood pressure measurement may not be sufficient to predict the risk of long-term cardiovascular events. Changes in blood pressure over time were an principal factor that should be taken into account (15). In recent years, trajectories assessment has been widely used to reflect long-term patterns of blood pressure changes (11). Several studies have shown that different blood pressure trajectories were strongly associated with the occurrence of cardiovascular events (16, 17). However, few of these studies focused on MAP trajectories and young adults, which was why national guidelines for hypertension do not specifically recommend blood pressure management in young adults. To make up for these shortcomings, this study analyzed the effects of different MAP trajectories on the risk of early onset CVD and all-cause mortality in young adults based on the Kailuan study.
2. Methods
2.1. Study design and participants
The Kailuan study began in 2006, active and retired employees of Kailuan Group were enrolled and took the physical examination by Kailuan General Hospital and its 11 affiliated hospitals. After that, the cohort was followed up every two years. Information on the use of medications was obtained through questionnaires, and relevant physical examination data were also collected. Detailed data collection methods were described in our previous studies (18, 19).
In the current analyses, a total of 19,171 participants who were younger than 40 years old and without CVD in their first survey in 2006–2009 and did not have CVD until the baseline (the third survey was defined as the baseline) were included (the flow chart of participants selection was showed in Supplementary Figure S3). The study was approved by the Ethics Committee of Kailuan General Hospital and is in accordance with the Declaration of Helsinki.
2.2. Assessment of blood pressure
Face-to-face surveys were conducted by trained nurses and doctors in 2006 and during a biennial follow-up. BP in the left arm was measured using a mercury sphygmomanometer with an appropriately sized cuff, as per standard recommended procedures. The SBP is the point at which the first of two or more Korotkoff sounds are heard, and the disappearance of the Korotkoff sound is used to define the DBP. From 2014 onwards, the BP was measured using an electronic BP meter (HEM-8102A; Omron Limited, Dalian, China). After resting in a chair for at least 5 min, participants took at least two SBP and DBP readings every 5 min. BP was then measured again if the difference between the 2 measurements was ≥5 mmHg. MAP = 1/3SBP + 2/3DBP.
2.3. Follow up
MAP trajectories were determined based on the blood pressure from the first three surveys (referred as the trajectory period). Information of the third survey was defined as the baseline for the present study (Supplementary Figure S2). The outcome event was CVD or all-cause death. If the participants had multiple CVD, the first occurrence event was regarded as the outcome event. If no outcome event occurred, the follow-up ended on December 31, 2020. The physiological and biochemical indexes such as height, weight, blood glucose, and blood pressure were followed up by professionally trained doctors. Follow-up was performed every 2 years on average.
2.4. Assessment of CVD events and all-cause death
The outcome was CVD (including myocardial infarction, stroke, atrial fibrillation and heart failure). The diagnosis of CVD has been described in previous Kailuan study (20, 21). In brief, all participants were enrolled in the municipal social insurance agency and the registration form for cardiovascular discharge was universally covered among Kailuan study.
All suspected CVD events underwent medical record review by three experienced clinical referees who were blinded to the study design. According to the multi-country monitoring criteria for Trends and Determinants of CVD established by the World Health Organization (WHO), a diagnosis of occasional myocardial infarction is based on clinical symptoms, dynamic changes in myocardial enzyme or biomarker concentrations, and electrocardiogram results. Stroke diagnosis is based on symptoms and neuroimaging obtained through computed tomography (CT) or magnetic resonance imaging (MRI), with additional diagnostic reports provided in accordance with World Health Organization standards, as previously specified. The diagnosis of heart failure is based on criteria set by the European Society of Cardiology (22). Diagnostic criteria include clinical presentation and laboratory examination. All-cause death data were collected through provincial offices of Vital Statistics.
2.5. Covariates at baseline
Diabetes mellitus was defined as fasting blood glucose level ≥7.0 or <7.0 mmol/L but was taking hypoglycemic medications or with established diabetes. Hypertension is defined as having a systolic blood pressure of 140 mmHg or higher, a diastolic blood pressure of 90 mmHg or higher, a history of diagnosed hypertension, or taking medication for high blood pressure. Body mass index (BMI) = weight (kg)/height squared (m²). Smoking was defined as the consumption of at least one cigarette per day on average for a period of 1 year or more. Alcohol consumption was defined as an average daily intake of 100 ml liquor with over 50% alcohol content for a minimum duration of 1 year. Physical exercise was defined as engaging in physical activity at least three times per week. High-salt diet was defined as a daily salt intake of 10 g or more.
2.6. Statistical analyses
Statistical software SAS9.4 (SAS Institute, Cary, NC, USA) was used for data analysis. Each participant was followed up from the end of the baseline year until the date of CVD onset, death, loss of follow-up [of 1,820/19,171 (9.5%)], or end of follow-up (December 31, 2020), whichever came first.
Latent mixing modeling (PROC-TRAJ) was used to identify subgroups with similar latent MAP patterns, regardless of whether antihypertensive medications were used. Bayesian information criteria were used to evaluate model fit. We started a model with 5 trajectories, and then compared BIC's to BIC's with 4, 3, 2, and 1 trajectory, respectively. The model that identifies five trajectories was the best fit.
Cox proportional hazard regression model was used to analyze the effects of different MAP trajectories on the risk of CVD and all-cause mortality. Potential confounding factors [including age, sex, smoking status, alcohol consumption, physical activity, salt intake, use of glucose-lowering, blood pressure lowering, lipid-lowering medications, body mass index (BMI), estimated glomerular filtration rate (eGFR), triglyceride (TG) concentration, high density lipoprotein (HDL-c), low density lipoprotein (LDL-c), and high sensitivity C-reactive protein (hs-CRP)] were included for correction. The proportional-hazards assumption was satisfied. Kaplan-Meier method was used to calculate the cumulative incidence of cardiovascular events and all-cause death in groups with different MAP trajectories, and Log-rank test was used for comparison among groups. All statistical tests were 2-sided, and P < 0.05 was regarded as significant.
2.6.1. Sensitivity analysis
Because taking antihypertensive, glucose-lowering, and lipid-lowering medications might have some influence on the results, repeated Cox proportional risk regression analysis was conducted to analyze the effect of different MAP trajectories on the risk of CVD and all-cause mortality after excluded the population taking medications during the trajectory period or during the follow-up. To examine whether the potential association between MAP trajectory and the risk of CVD or all-cause mortality could be explained by either MAP status, MAP at first survey and at baseline was further corrected.
3. Results
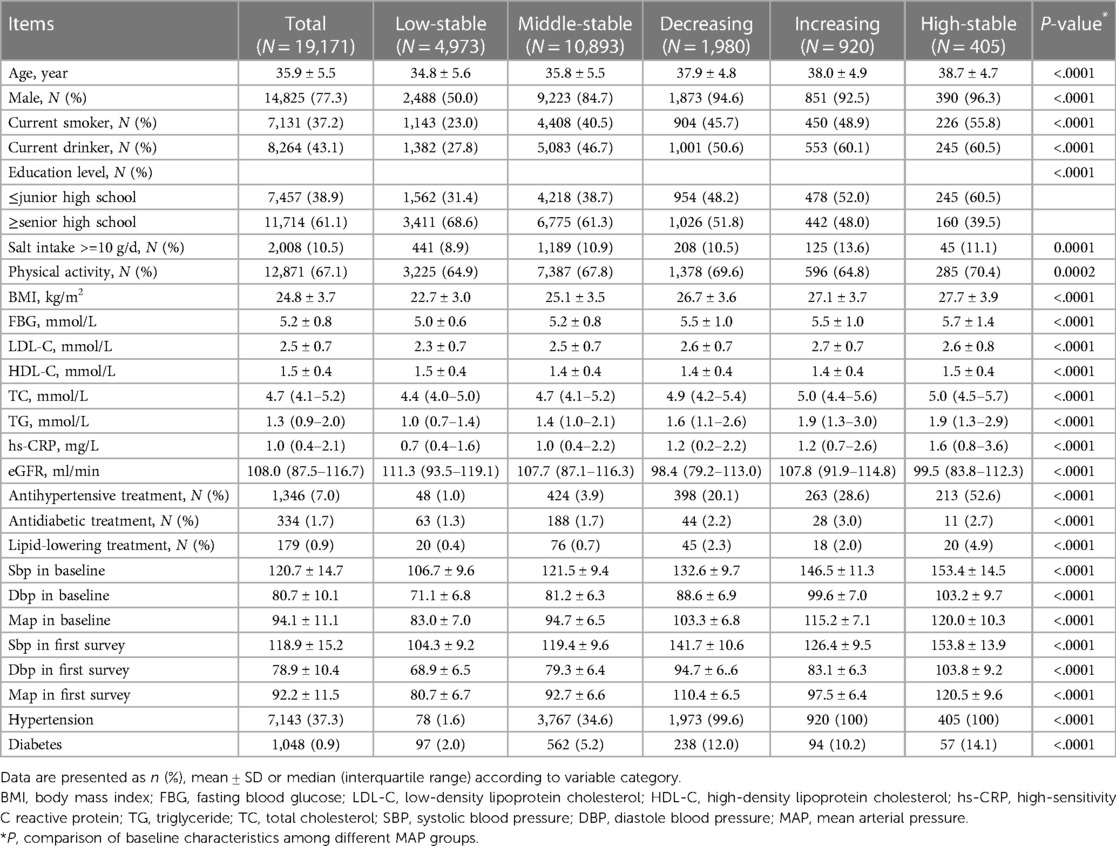
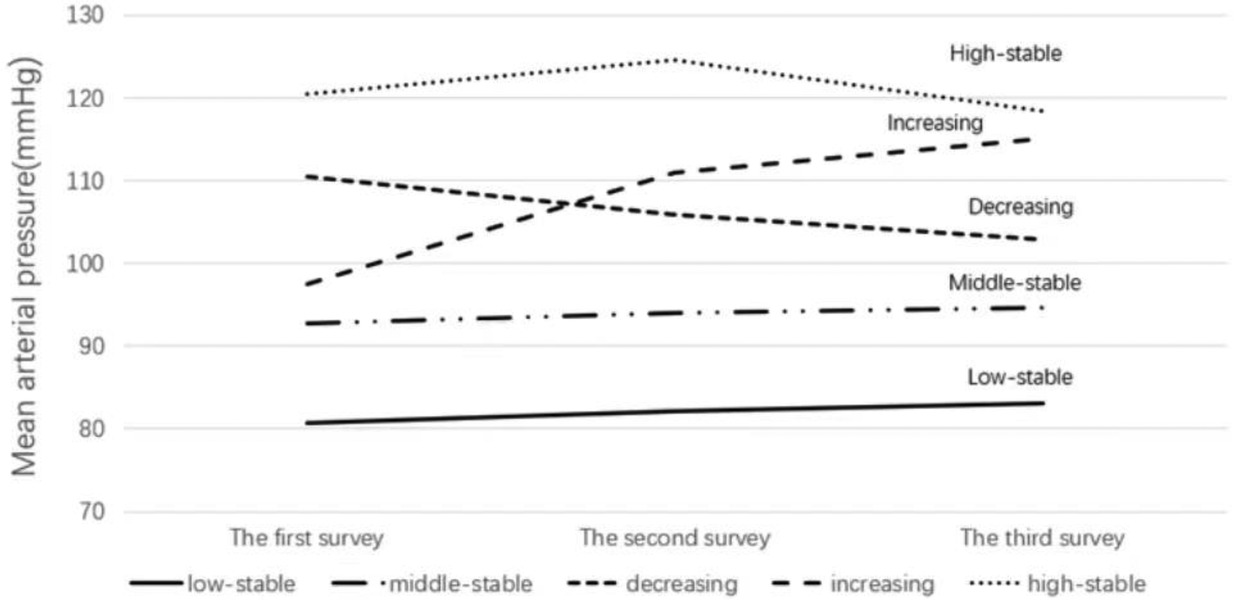
Of the 19,171 subjects in the study, 14,825 were male, accounting for 77.3% of the subjects (Table 1). The baseline mean age was (35.9 ± 5.5) years. During the trajectory period, five different trajectories were identified. MAP was consistently stable at around 120 mmHg in 2.2% (n = 405) of participants (referred as the “high stable mode”), around 90–110 mmHg in 53.7% (n = 10,893) of participants (referred as the “middle stable mode”), around 80–90 mmHg in 27.3% (n = 4,973) of participants (referred as the “low stable mode”). 5.8% (n = 920) of participants had a MAP of about 100 mmHg in the first survey, which increased to about 110 mmHg during the trajectory period (referred as the “increasing mode”); 11% (n = 1,980) of participants had an average arterial pressure of approximately 110 mmHg at their first survey and continued to decline to 100 mmHg during the trajectory period (referred to as the “decreasing mode”) (Figure 1).
During a mean follow-up period of 9.67 ± 1.44 years, 310 subjects (1.62%) had cardiovascular diseases, including 201 stroke, 49 myocardial infarction, 46 heart failure, and 25 atrial fibrillation. The mean age of occurring the cardiovascular diseases was 45.49 ± 4.88 years. The incidence density was 0.31/1,000, 1.22/1,000, 3.98/1,000, 5.16/1,000 and 11.95/1,000 person years for the low-stable, middle-stable, decreasing, increasing and high-stable groups, respectively (Table 2). There were 267 all-cause deaths, and the incidence density was 0.70/1,000, 1.22/1,000, 2.79/1,000, 2.80/1,000 and 6.12/1,000 person years for the low-stable, middle-stable, decreasing, increasing and high-stable groups, respectively (Table 3). There were statistically significant differences for the incidence of CVD or all-cause death across the different trajectory components (Log-rank test, P < 0.05, Supplementary Figure S1).
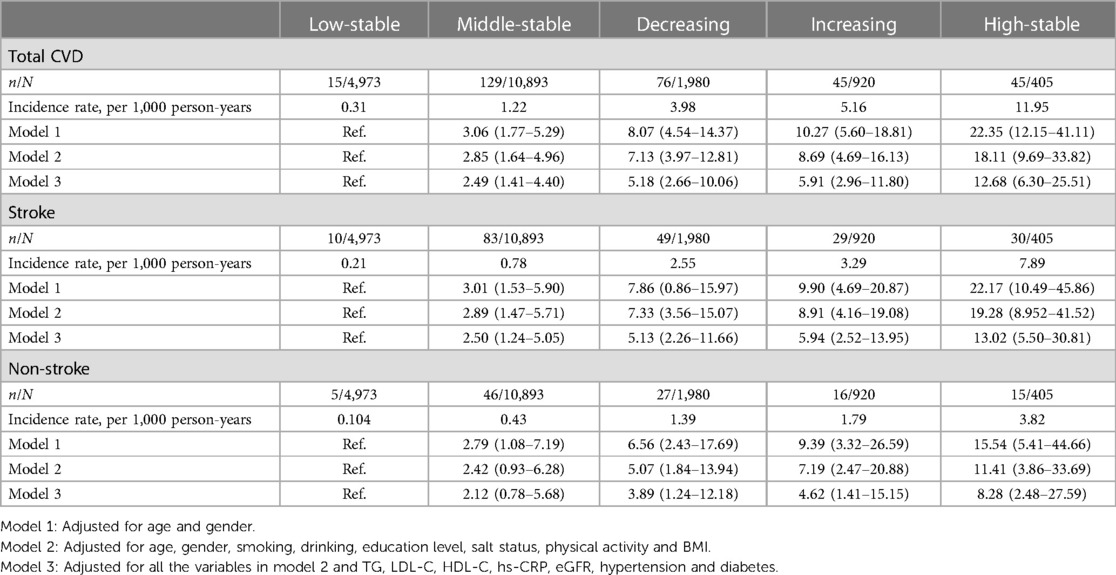
Table 2. Adjusted hazard ratios and 95% confidence intervals for risks of CVD according to MAP trajectories.
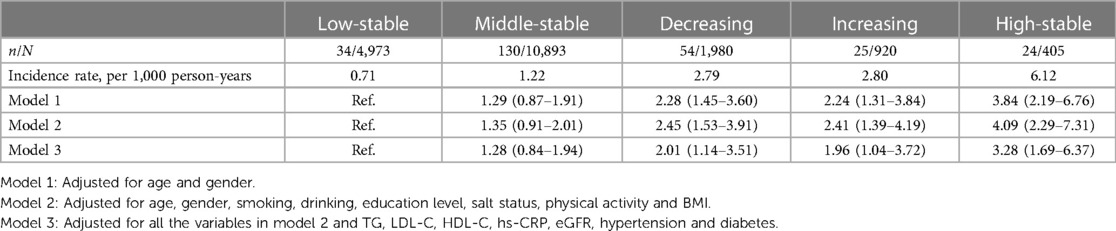
Table 3. Adjusted hazard ratios and 95% confidence intervals for risks of all-cause deaths according to MAP trajectories.
Different MAP trajectories were grouped as independent variables, and the occurrence of CVD or all-cause deaths as dependent variables, respectively. Cox proportional hazard regression results showed that compared with participants in the low-stability group, The HR (95%CI) of total CVD were 2.48 (1.40–4.40), 5.18 (2.66–10.06), 5.91 (2.96–11.80) and 12.68 (6.30–25.51) for participants in the middle-stable, decreasing, increasing and high-stable groups, respectively (Table 2). The HR (95%CI) for all-cause deaths were 1.27 (0.83–1.94), 2.01 (1.14–3.55), 1.96 (1.04–3.72), and 3.28 (1.69–6.37), respectively (Table 3). After classifying CVD into stroke and non-stroke (including myocardial infarction, atrial fibrillation and heart failure), similar results were observed for participants with decreasing, increasing or high-stable MAP trajectories. However, for participants with middle-stable MAP trajectory, the association was observed only for stroke, not for non-stroke (Table 2).
To eliminate the impact of medication intake on the outcomes, the Cox proportional hazard regression model was repeated after excluding the patients who took antihypertensive, hypoglycemic, or lipid lowering medications during the trajectory or follow-up period (Supplementary Table S1). The results were consistent with the main analysis. Further adjustment for baseline MAP and first survey MAP generated similar results (Table 4).
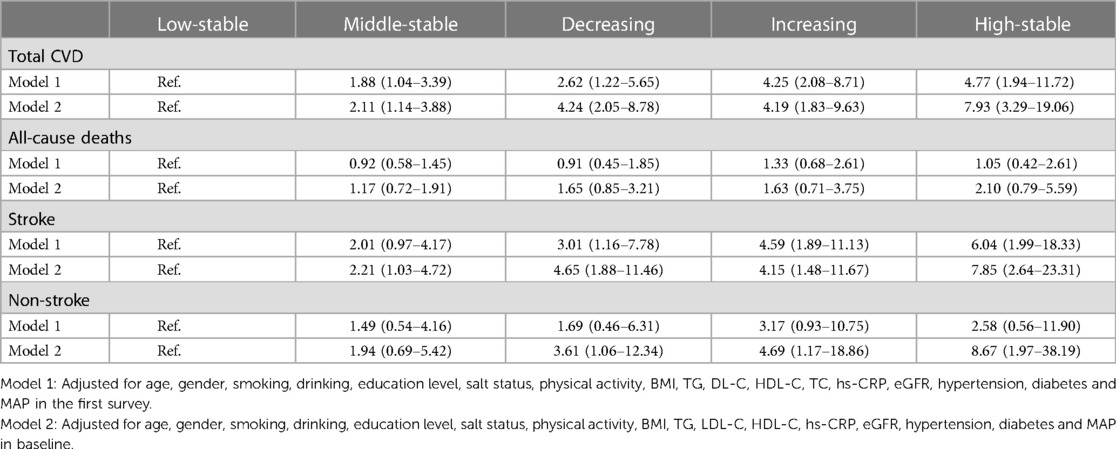
Table 4. Association between risks of diseases and MAP trajectories after adjusted MAP in the first survey or in baseline.
4. Discussion
In the present study, we followed 19,171 young participants (less than 40 years) for about 9 years and observed that the MAP trajectories were associated with the risk of CVD and all-cause death in young adults. Compared to participants with low stable MAP trajectory, the CVD risk was 2.49–12.68 folds higher for those with middle-stable, decreasing, increasing or high-stable MAP trajectories, and the all-cause death risk was 2.01–3.28 folds higher for those with decreasing, increasing or high-stable MAP trajectories. There was a lack of specific studies on MAP changes and disease risk in previous studies. However, some studies showed that the single blood pressure value was associated with the cardiovascular disease risk, which was similar to our results (13, 23). The findings of our study suggested that monitoring blood pressure trajectory should be helpful in identifying individuals with high risk of CVD or death, and preventing the occurrence of CVD and death in young population.
The trajectory approach takes into account mean, variability and direction of variation, so it was better in understanding and illustrating the evolution of disease risk (24). In the present study, the participants with increasing trajectory had higher risk of CVD or all-cause death, despite their MAP at the first survey was lower than those with decreasing trajectory. The results confirmed that using a single blood pressure value to predict cardiovascular risk might misclassify the population at risk, whereas long-term blood pressure changes can predict disease risk more effectively.
Our findings revealed that individuals with consistently elevated mean arterial pressure (MAP) falling within the range of 90–100 mmHg, which is considered within the normal MAP range, exhibited a significantly higher risk of cardiovascular disease (CVD) compared to those with a consistently lower MAP below 90 mmHg. These results align with Sesso's study (13), which demonstrated an increased risk of CVD in individuals younger than 60 years old with a MAP exceeding 88 mmHg. Consequently, implementing more rigorous blood pressure control strategies may prove to be more effective in preventing CVD among young adults. However, determining the optimal blood pressure target for preventing cardiovascular events in the young population remains unclear. The SPRINT trial compared the occurrence of CVD in a non-diabetic cohort following either an enhanced blood pressure control strategy or a standard blood pressure control strategy. The study found that the enhanced blood pressure control strategy resulted in a lower incidence of major cardiovascular events and overall mortality (25). These findings, along with our study results, collectively underscore the importance of strengthening blood pressure control measures to reduce the risk of CVD in the young population.
Our study further analyzed the association of MAP trajectory and baseline MAP with CVD. The results showed that the influence of baseline MAP on CVD risk disappeared after the MAP trajectory was brought into the same model, but the MAP trajectory was still associated with CVD. It suggested that the association between MAP trajectory and CVD was stronger than baseline MAP. Although there was no previous study to compare the strength of the association between MAP trajectory or baseline MAP and CVD, Portegies et al. found a stronger correlation between blood pressure trajectory and stroke than blood pressure at baseline level (17), which supported our results to some extent. It was also found that the association between MAP trajectory and CVD was independent of blood pressure at the first survey, which strongly supports the necessity of long-term blood pressure monitoring to reduce the risk of CVD. However, the results were not similar for all-cause death in our study. Baseline MAP seems to have a greater impact on the risk of death than MAP trajectories, which was consistent with other studies (23).
We also observed that the risks of CVD or death in participants with early and remained elevated blood pressure (HR (95%CI) were 12.68 (6.30–25.51) for CVD and 3.28 (1.69–6.37) for all-cause death) were higher than that in participants with late elevated blood pressure (HR (95%CI) were 5.91 (2.96–11.80) for CVD and 1.96 (1.04–3.72) for all-cause death). It suggested that the risks of CVD and all-cause mortality in people with persistently high levels of MAP were higher than those in people with MAP rising to high levels in a short period. This was consistent with the conclusions of a study based on data from the Atherosclerosis Risk in Communities Study (26), which found that subjects whose SBP remained above 140 mmHg had a higher CVD death risk than subjects whose SBP rose sharply from pre-hypertensive levels to more than 140 mmHg. Our results showed that for those with early elevated MAP, although lowering MAP might decrease the risk of CVD or all-cause death, the risks were still higher even their elevated MAP decreased to normal range (HR (95%CI) were 5.18 (2.66–10.06) for CVD and 2.01 (1.14–3.55) for all-cause death). On the one hand, the results demonstrated the importance of lowing blood pressure as early as possible. On the other hand, the results emphasized the importance of primary prevention in disease controlling, that was, early prevent the occurrence of diseases.
Previous studies have shown that longitudinal changes in blood pressure were negatively correlated with ankle-brachial index and positively correlated with pulse wave velocity, and suggested a relationship between changes in blood pressure and impaired vascular function (27). Long-term exposure to higher blood pressure may lead to endothelial cell damage, which may alter the interaction between blood cells and endothelial cells, eventually leading to local thrombosis and ischemic lesions, leading to cardiovascular and cerebrovascular diseases (28, 29). Fibrous necrosis is considered a potential risk factor for CVD, resulting in lacunar infarction through focal stenosis and occlusion. Degenerative changes in endothelial cells and smooth muscle cells may lead to aneurysm formation and cerebral hemorrhage. High blood pressure also speeds up the atherogenic process, increasing the likelihood of brain damage associated with narrowing and embolization caused by large extracranial blood vessels (30). In addition, some known risk factors for CVD, such as left ventricular hypertrophy, are also associated with long-term elevated blood pressure. Therefore, a longer pattern of blood pressure monitoring may better reflect these pathophysiological changes. MAP acts as a major driving force for vital organ perfusion is associated with CVD and all-cause mortality (31). More detailed studies are needed to elucidate the role of MAP longitudinal changes in the development of mortality and CVD and the related mechanisms to help refine our understanding and guidance on optimal blood pressure management in young adults.
We found that the MAP trajectory pattern was associated with the risk of CVD or all-cause death in young adults and was independent of baseline MAP. Therefore, early controlling of blood pressure and long-term monitoring of blood pressure can effectively reduce the risk of CVD or all-cause death, thereby reducing the financial burden of CVD on patients’ quality of life and on families and society. In addition, young individuals with CVD might lose their ability to work prematurely. Blood pressure control should be strengthened to reduce the occurrence of CVD or death in young people. In all, our results had important clinical and public health implications in disease controlling for young population.
4.1. Limitations
This study is subject to certain limitations that should be considered. Firstly, all participants included in our study were employed by Kailuan Study in Tangshan, China. Therefore, the identified trajectories may not be generalized to other populations. However, the homogeneity of our cohort can help reduce confounding factors such as racial and healthcare differences, thereby enhancing content validity. Secondly, our cohort had a relatively small representation of women, and we did not perform gender stratification to assess potential differences between blood pressure trajectory and CVD risk. This limits our ability to fully understand gender-specific associations. Lastly, it is important to note that the study population consisted of young individuals who are generally at lower risk for CVD. Consequently, the number of CVD events observed was relatively small, which may impact the level of certainty in our findings.
5. Conclusion
Our study showed that MAP trajectories were associated with the risk of CVD or all-cause mortality and increasing MAP trajectories within the currently designated “normal” range may still increase the risk for CVD. Monitoring blood pressure trajectory can provide an important way to identify people at high risk and decrease the occurrence of CVD or all-cause death in young population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Requests to access these datasets should be directed to Yun Li,bGl5dW44MDIyQDE2My5jb20=.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Kailuan General Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SW, SC, and YL: designed the study, reviewed and revised the manuscript. ZS, ZW, and PY: coded and analyzed the data. ZS, HZ, YT, and ZW: wrote the manuscript. ZW and WZ: collected data. YW and SC: helped interpret the data. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Natural Science Foundation of Hebei Province. (H2021209018).
Acknowledgments
The authors thank all the survey teams of the Kailuan study group for their contribution and the study participants who contributed their information.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1222995/full#supplementary-material
References
1. Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. (1993) 153(5):598–615. doi: 10.1001/archinte.153.5.598
2. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA. (1996) 275(20):1571–6.8622248
3. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Collaboration PS. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. (2002) 360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-8
4. Aune D, Huang W, Nie J, Wang Y. Hypertension and the risk of all-cause and cause-specific mortality: an outcome-wide association study of 67 causes of death in the national health interview survey. BioMed Res Int. (2021) 2021:9376134. doi: 10.1155/2021/9376134
5. Collaborators GRF. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388(10053):1659–724. doi: 10.1016/s0140-6736(16)31679-8
6. Singam A, Ytterberg C, Tham K, von Koch L. Participation in complex and social everyday activities 6 years after stroke: predictors for return to pre-stroke level. PloS one. (2015) 10(12):e0144344. doi: 10.1371/journal.pone.0144344
7. Lattanzi S, Brigo F, Silvestrini M. Blood pressure and stroke: from incidence to outcome. J Clin Hypertens. (2019) 21(5):605–7. doi: 10.1111/jch.13525
8. Turin TC, Okamura T, Afzal AR, Rumana N, Watanabe M, Higashiyama A, et al. Hypertension and lifetime risk of stroke. J Hypertens. (2016) 34(1):116–22. doi: 10.1097/hjh.0000000000000753
9. Guzik A, Bushnell C. Stroke epidemiology and risk factor management. Continuum (Minneapolis, Minn). (2017) 23(1, Cerebrovascular Disease):15–39. doi: 10.1212/con.0000000000000416
10. Darne B, Girerd X, Safar M, Cambien F, Guize L. Pulsatile vs. steady component of blood pressure: a cross-sectional analysis and a prospective analysis on cardiovascular mortality. Hypertension. (1989) 13(4):392–400. doi: 10.1161/01.hyp.13.4.392
11. Allen NB, Siddique J, Wilkins JT, Shay C, Lewis CE, Goff DC, et al. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. (2014) 311(5):490–7. doi: 10.1001/jama.2013.285122
12. Liu D, Qin P, Liu L, Liu Y, Sun X, Li H, et al. Association of pulse pressure with all-cause and cause-specific mortality. J Hum Hypertens. (2021) 35(3):274–9. doi: 10.1038/s41371-020-0333-5
13. Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Gaziano JM, Manson JE, et al. Systolic and diastolic blood pressure, pulse pressure, and mean arterial pressure as predictors of cardiovascular disease risk in men. Hypertension. (2000) 36(5):801–7. doi: 10.1161/01.hyp.36.5.801
14. Thomas F, Blacher J, Benetos A, Safar ME, Pannier B. Cardiovascular risk as defined in the 2003 European blood pressure classification: the assessment of an additional predictive value of pulse pressure on mortality. J Hypertens. (2008) 26(6):1072–7. doi: 10.1097/HJH.0b013e3282fcc22b
15. Brickman AM, Reitz C, Luchsinger JA, Manly JJ, Schupf N, Muraskin J, et al. Long-term blood pressure fluctuation and cerebrovascular disease in an elderly cohort. Arch Neurol. (2010) 67(5):564–9. doi: 10.1001/archneurol.2010.70
16. Tielemans SMAJ, Geleijnse JM, Menotti A, Boshuizen HC, Soedamah-Muthu SS, Jacobs DR, et al. Ten-year blood pressure trajectories, cardiovascular mortality, and life years lost in 2 extinction cohorts: the Minnesota business and professional men study and the Zutphen study. J Am Heart Assoc. (2015) 4(3):e001378. doi: 10.1161/jaha.114.001378
17. Portegies MLP, Mirza SS, Verlinden VJA, Hofman A, Koudstaal PJ, Swanson SA, et al. Mid- to late-life trajectories of blood pressure and the risk of stroke: the rotterdam study. Hypertension. (2016) 67(6):1126–32. doi: 10.1161/hypertensionaha.116.07098
18. Zhao M, Song L, Sun L, Wang M, Wang C, Yao S, et al. Associations of type 2 diabetes onset age with cardiovascular disease and mortality: the Kailuan study. Diabetes Care. (2021) 44(6):1426–32. doi: 10.2337/dc20-2375
19. Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, et al. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the kailuan cohort. Cardiovasc Diabetol. (2021) 20(1):19. doi: 10.1186/s12933-020-01210-5
20. Wu Z, Jin C, Vaidya A, Jin W, Huang Z, Wu S, et al. Longitudinal patterns of blood pressure, incident cardiovascular events, and all-cause mortality in normotensive diabetic people. Hypertension. (2016) 68(1):71–7. doi: 10.1161/hypertensionaha.116.07381
21. Wu Z, Huang Z, Jin W, Rimm EB, Lichtenstein AH, Kris-Etherton PM, et al. Peripheral inflammatory biomarkers for myocardial infarction risk: a prospective community-based study. Clin Chem. (2017) 63(3):663–72. doi: 10.1373/clinchem.2016.260828
22. Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the task force for the diagnosis and treatment of chronic heart failure of the European society of cardiology. Eur Heart J. (2005) 26(11):1115–40. doi: 10.1093/eurheartj/ehi204
23. Sun S, Lo K, Liu L, Huang J, Feng YQ, Zhou Y-L, et al. Association of mean arterial pressure with all-cause and cardiovascular mortality in young adults. Postgrad Med J. (2020) 96(1138):455–60. doi: 10.1136/postgradmedj-2019-137354
24. Jones BL, Nagin DS. Advances in group-based trajectory modeling and an sas procedure for estimating them. Sociol Methods Res. (2007) 35(4):542–71. doi: 10.1177/0049124106292364
25. Group SR, Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. (2015) 373(22):2103–16. doi: 10.1056/NEJMoa1511939
26. Petruski-Ivleva N, Viera AJ, Shimbo D, Muntner P, Avery CL, Schneider ALC, et al. Longitudinal patterns of change in systolic blood pressure and incidence of cardiovascular disease: the atherosclerosis risk in communities study. Hypertension. (2016) 67(6):1150–6. doi: 10.1161/hypertensionaha.115.06769
27. Okada H, Fukui M, Tanaka M, Inada S, Mineoka Y, Nakanishi N, et al. Visit-to-visit variability in systolic blood pressure is correlated with diabetic nephropathy and atherosclerosis in patients with type 2 diabetes. Atherosclerosis. (2012) 220(1):155–9. doi: 10.1016/j.atherosclerosis.2011.10.033
28. Brandes RP. Endothelial dysfunction and hypertension. Hypertension. (2014) 64(5):924–8. doi: 10.1161/hypertensionaha.114.03575
29. Dharmashankar K, Widlansky ME. Vascular endothelial function and hypertension: insights and directions. Curr Hypertens Rep. (2010) 12(6):448–55. doi: 10.1007/s11906-010-0150-2
30. Johansson BB. Hypertension mechanisms causing stroke. Clin Exp Pharmacol Physiol. (1999) 26(7):563–5. doi: 10.1046/j.1440-1681.1999.03081.x
Keywords: blood pressure pattern, trajectory, cardiovascular diseases, all-cause mortality, young people
Citation: Song Z, Zhao H, Wei Z, Zhao W, Tan Y, Yang P, Chen S, Wu Y, Li Y and Wu S (2023) Mean arterial pressure trajectory with premature cardiovascular disease and all-cause mortality in young adults: the Kailuan prospective cohort study. Front. Cardiovasc. Med. 10:1222995. doi: 10.3389/fcvm.2023.1222995
Received: 15 May 2023; Accepted: 4 September 2023;
Published: 13 September 2023.
Edited by:
Sebhat Erqou, Brown University, United StatesReviewed by:
Arnaud Kaze, Sovah health, United StatesMingzhi Zhang, Soochow University, China
Jianxin Li, Chinese Academy of Medical Sciences and Peking Union Medical College, China
© 2023 Song, Zhao, Wei, Zhao, Tan, Yang, Chen, Wu, Li and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Li bGl5dW44MDIyQDE2My5jb20= Shouling Wu ZHJ3dXNsQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Zongshuang Song
Zongshuang Song Haiyan Zhao2,†
Haiyan Zhao2,† Zhihao Wei
Zhihao Wei Wenliu Zhao
Wenliu Zhao Shuohua Chen
Shuohua Chen YunTao Wu
YunTao Wu Yun Li
Yun Li Shouling Wu
Shouling Wu