
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 03 August 2023
Sec. Coronary Artery Disease
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1217069
This article is part of the Research TopicComputational Morphofunctional Assessment of Coronary Artery DiseaseView all 5 articles
 Ke Xu1,†
Ke Xu1,† Yue Jiang1,†
Yue Jiang1,† Wentao Yang1
Wentao Yang1 Weifeng Zhang1
Weifeng Zhang1 Dong Wang1
Dong Wang1 Yu Zhao1
Yu Zhao1 Shunwen Zheng1
Shunwen Zheng1 Ziyong Hao1
Ziyong Hao1 Lan Shen1
Lan Shen1 Lisheng Jiang1
Lisheng Jiang1 Xingbiao Qiu1
Xingbiao Qiu1 Javier Escaned2
Javier Escaned2 Shengxian Tu3
Shengxian Tu3 Linghong Shen1*
Linghong Shen1* Ben He1*
Ben He1*
Introduction: In coronary bifurcation lesions treated with percutaneous coronary intervention (PCI) using a 1-stent strategy, the occurrence of side branch (SB) compromise may lead to long-term myocardial ischemia in the SB territory. Murray law–based quantitative flow ratio (μQFR) is a novel angiography-based approach estimating fractional flow reserve from a single angiographic view, and thus is more feasible to assess SB compromise in routine practice. However, its association with long-term SB coronary blood flow remains unknown.
Methods: A total of 146 patients with 313 non-left main bifurcation lesions receiving 1-stent strategy with drug-eluting stents was included in this retrospective study. These lesions had post-procedural Thrombolysis in Myocardial Infarction (TIMI) flow grade 3 in SBs, and documented angiographic images of index procedure and 6- to 24-month angiographic follow-up. Post-procedural SB μQFR was calculated. Long-term SB coronary blood flow was quantified with the TIMI grading system using angiograms acquired at angiographic follow-up.
Results: At follow-up, 8 (2.6%), 16 (5.1%), 61 (19.5%), and 228 (72.8%) SBs had a TIMI flow grade of 0, 1, 2, and 3, respectively. The incidences of long-term SB TIMI flow grade ≤1 and ≤2 both tended to decrease across the tertiles of post-procedural SB μQFR. The receiver operating characteristic curve analyses indicated the post-procedural SB μQFR ≤0.77 was the optimal cut-off value to identify long-term SB TIMI flow grade ≤1 (specificity, 37.50%; sensitivity, 87.20%; area under the curve, 0.6673; P = 0.0064), and it was independently associated with 2.57-fold increased risk (adjusted OR, 2.57; 95% CI, 1.02–7.25; P = 0.045) in long-term SB TIMI flow grade ≤1 after adjustment.
Discussion: Post-procedural SB μQFR was independently associated with increased risk in impaired SB TIMI flow at long-term follow-up. Further investigations should focus on whether PCI optimization based on μQFR may contribute to improve SB flow in the long term.
Coronary bifurcation lesions account for approximately 15%–20% of all the coronary lesions undergoing percutaneous coronary interventions (PCIs) (1, 2). PCI in coronary bifurcations lesions is challenging because of increased risks in peri-procedural complications and clinical failure, largely owing to the side branch (SB) compromise (3, 4). The one-stent strategy is recommended in the majority of non-left main (LM) coronary bifurcation lesions (5) following demonstration of being non-inferior to the upfront two-stent strategy in terms of clinical outcomes, while being associated with shorter procedure time and less contrast volume (6–8). These facts explain why in real-world clinical practice, around 80% of coronary bifurcation lesions undergoing PCI are treated with a one-stent strategy (9).
The ultimate common aims of all bifurcation PCI strategies are to avoid peri-procedural complications and to ensure a safe and effective result of PCI in the long term. A key aspect of the latter is preserving side branch patency and function in the long term. At least 10% of SBs with normal coronary blood flow [thrombolysis in myocardial infarction (TIMI) flow grade 3] had functional significance [fractional flow reserve (FFR) ≤ 0.75] in coronary bifurcation lesions after main vessel (MV) stent implantation (10). Thus, it is important to investigate the relationship between post-procedural SB compromise and long-term SB outcomes in non-LM coronary bifurcation lesions receiving the one-stent strategy.
Quantitative flow ratio (QFR) is a non-invasive tool recently developed to estimate FFR with a high diagnostic accuracy (11), and QFR-guided PCI could reduce 35% of major adverse cardiac events compared with angiography-guided PCI (12). However, QFR computation requires two angiographic views obtained with at least 25° in separation and is not always feasible in SB evaluation in the routine clinical practice. To overcome it, a modified version of QFR, Murray law–based QFR (μQFR), was recently developed. Its calculation was based on a single angiographic view and in both the main vessel and its side branches. μQFR had a high diagnostic accuracy to estimate FFR even using suboptimal angiographic image projection (13). It was recently shown that single view μQFR had a similar diagnostic accuracy as three-dimensional (3D) QFR (14, 15). Thus, μQFR could be used for SB functional assessment. Nonetheless, the association between post-procedural SB μQFR and long-term SB outcomes in non-LM coronary bifurcation lesions receiving the one-stent strategy remains unclear.
Accordingly, in this study, we aimed to explore the association between post-procedural SB μQFR and long-term SB coronary blood flow in non-LM coronary bifurcation lesions receiving one-stent strategy.
This single-center, retrospective study was performed in the Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine, according to the principles of the Declaration of Helsinki and local regulations. This study was approved by the Ethics Committee of Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine (ethics ID: IS2128). Written informed consents were waived.
We retrospectively screened adult patients (>18 years old) who (1) were admitted to the Department of Cardiology, Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine from January 2012 to May 2019, (2) received the one-stent strategy for de novo non-LM coronary bifurcation lesions, and (3) had documented coronary angiographic images at the index procedure and at 6- to 24-month angiographic follow-up. The de novo non-LM coronary bifurcation lesion was defined as a de novo coronary artery narrowing occurring adjacent to or involving significant SB origin (16), whose site was not at the distal left main coronary artery. Significant SB selection was based on the European Bifurcation Club consensus definition (a branch that the operator would not want to lose in the global context of an individual patient, including symptoms, ischemia location, branch responsible for symptoms or ischemia, viability, and collateralizing vessel) (16), but not the reference SB diameter in order to avoid missing visually small SBs with clinically significance. The mean reference SB diameter was 1.6 mm in this study. Exclusion criteria were ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), cardiomyopathy, myocarditis, valvular heart disease, chronic total occlusion, left main artery lesion, thrombus-containing lesion, and prior coronary artery bypass graft. Angiographic inclusion criterion was post-procedural SB TIMI flow grade 3. Angiographic exclusion criteria included (1) lesions without proper angiographic images for quantitative coronary angiography (QCA) or QFR analysis, (2) MV TIMI flow grade <3 at 6- to 24-month angiographic follow-up, and (3) SB lesion length that cannot be clearly measured.
The PCI strategy and instrumentation use in all the cases were at the discretion of the interventional operators, including coronary stent selection. Coronary angiography was conducted in the conventional manner following the current guidelines. Peri-procedural and long-term anti-platelet and anti-coagulant administration was determined based on the operator's discretion and current guidelines. Administration of aspirin 300 mg and clopidogrel 300–600 mg or ticagrelor 180 mg as the loading doses followed by aspirin 100 mg once daily and clopidogrel 75 mg once daily or ticagrelor 90 mg twice daily as the maintenance doses before the procedure was mandatory. Life-long aspirin (100 mg once day) was prescribed to all patients except for those who had aspirin intolerance. Clopidogrel 75 mg once daily or ticagrelor 90 mg twice daily administration for at least 12 months after procedure was recommended to all patients.
Clinical data were acquired through the medical chart review. A pre-specified data collection form was used to record age, sex, body mass index, diagnosis (stable angina/silent ischemia or unstable angina), co-morbidities (hypertension, diabetes mellitus, hyperlipidemia), smoking status, medical history [prior myocardial infarction (MI), prior PCI), low-density lipoprotein cholesterol, and left ventricular ejection fraction assessed by transthoracic echocardiogram.
The documented cineangiograms were used to review the baseline lesion and procedural characteristics. For the lesion characteristics, bifurcation location, bifurcation type classified using Medina criteria, true bifurcation (defined as Medina 1,1,1, 1,0,1, or 0,1,1) (17), plaque location, coronary calcification, angulation, and irregular plaque were recorded. Moderate calcification was defined as radiopacities noted only with the cardiac motion before contrast injection. Severe calcification was defined as radiopacities noted without cardiac motion before contrast injection generally compromising both sides of the arterial lumen (18). Moderate–severe angulation was defined as lesion angulation >45° (19). Irregular plaque was defined as the plaque with visually unsmooth surface (20). For the procedural characteristics, MV characteristics (i.e., dissection before MV stenting, stent type, stent diameter, stent length, maximal balloon pressure, and maximal balloon diameter) and SB [i.e., SB pre-dilation, kissing balloon inflation (KBI) before MV stenting, dissection before MV stenting, SB TIMI flow grade before MV stenting, SB protection use including jailed wire technique, and jailed balloon technique, SB TIMI flow grade after MV stenting, SB opening after MV stenting, drug-coated balloon use, final KBI, and final SB TIMI flow grade] were recorded.
Clinical outcomes data were also collected by reviewing the medical charts and the patients or their families were contacted for verification via telephone. The Academic Research Consortium-2 consensus was accordingly used to define death, MI, target vessel revascularization, and stent thrombosis (21).
Post-procedural SB μQFR was analyzed. The AngioPlus Core software (Pulse Medical, Shanghai, China) were used to perform offline QFR analyses following standard operation procedures as described in previous studies (13, 22). QFR analyses were conducted by two independent, well-trained investigators (YJ and WT) who were blinded to patient clinical characteristics and follow-up.
QCA analysis was performed offline following the standard analysis procedure using a computer-based system dedicated to bifurcation (QAngio XA, version 7.3, Medis, Leiden, Netherlands) (23). The bifurcation lesions were divided into the proximal MV, distal MV, and SB segments. Bifurcation angle, lesion length, minimal lumen diameter (MLD), reference vessel diameter (RVD), diameter stenosis (DS), acute gain, and late loss were detected. The bifurcation angle was defined as the angle between the distal MV and SB segments. Binary restenosis was defined as QCA DS >50% (24). QCA analyses were conducted by two independent well-trained investigators (DW and YZ) who were blinded to patient clinical characteristics and follow-up.
Coronary blood flow was quantified with the TIMI grading system according to a previous study (25) and determined by visual estimation. TIMI flow grade were assessed by two independent well-trained investigators (KX and WZ) who were blinded to patient clinical characteristics, QCA analyses, and follow-up. The κ coefficient was used to detect the inter-operator variability.
Data for clinical characteristics were presented on a per-patient basis and on a per-vessel basis for the remaining calculations. All the included lesions were divided into three tertile groups according to the post-procedural SB μQFR and then included in analyses. Continuous data were present as the mean ± standard deviation and compared using the one-way analysis of variance (ANOVA) tests. Categorical data were present as the number (%) and compared using the chi-square tests. Receiver operating characteristic (ROC) curve analyses were used to determine the ability of post-procedural SB μQFR and SB DS to distinguish between SBs with and without SB TIMI flow grade ≤1 at angiographic follow-up, respectively, and to identify the optimal cut-off value of post-procedural SB μQFR that provided the greatest sum of specificity and sensitivity. Logistic regression models were adopted to detect the association of post-procedural SB μQFR with the incidences of long-term SB TIMI flow grade ≤1. Characteristics of clinical information (age, sex, hypertension, hyperlipidemia, diabetes, smoking status), lesion (true coronary bifurcation, bifurcation location), and procedure (stent diameter, stent type, MV RVD, and SB RVD) were included in multivariable regression analyses. DeLong's method was used to compare ROC curves between post-procedural SB μQFR and SB DS. Subgroups analyses were performed according to baseline SB RVD: ≤1.5, 1.5–2.0 mm, and >2.0 mm. Results were presented as the odds ratios (ORs) with 95% confidence intervals (CIs).
All analyses were conducted with Stata/SE software version 17.0 (Stata Corp, College Station, TX, USA) and GraphPad Prism version 9.4.0 (GraphPad Software, San Diego, CA, USA). A two-sided P-value of <0.05 was considered statistically significant.
We screened 554 non-LM coronary bifurcation lesions receiving one-stent strategy in 280 patients, and finally included 313 lesions in 146 patients who met all the inclusion criteria and had none of any exclusion criteria in this study (see Figure 1).
Clinical characteristics are detailed in Table 1. The mean age was 64.5 years. Of them, 111 (76.0%) patients were male. Lesion characteristics are detailed in Table 2. A total of 227 (72.5%) were located at the left anterior descending artery (LAD) and 53 (16.9%) were true bifurcation lesions. Procedural characteristics are detailed in Table 3. The stent diameter was 2.98 mm ± 0.36 mm, and stent length was 29.33 mm ± 6.91 mm.
Baseline clinical characteristics of patients with and without long-term SB TIMI flow grade ≤1 are shown in Supplementary Table S1. All the characteristics were comparable. Lesion characteristics in lesions with and without long-term SB TIMI flow grade ≤1 are shown in Supplementary Table S2. More complex lesions and more true bifurcation lesions were observed in lesions with long-term SB TIMI flow grade ≤1. Procedural characteristics in lesions with and without long-term SB TIMI flow grade ≤1 are detailed in Supplementary Table S3. More lesions with impaired SB TIMI flow before and after MV stenting were observed in lesions with long-term SB TIMI flow grade ≤1.
The distribution of pre- and post-procedural SB μQFR is presented in Figure 2. In the entire cohort, the median and interquartile post-procedural SB μQFR range were 0.89 and 0.15 (0.81–0.96). All the included lesions were divided into three tertile groups according to the post-procedural SB μQFR: low tertile group (SB μQFR ≤ 0.84, n = 108), middle tertile group (0.84 < SB μQFR ≤ 0.93, n = 106), and high tertile group (SB μQFR > 0.93, n = 99).
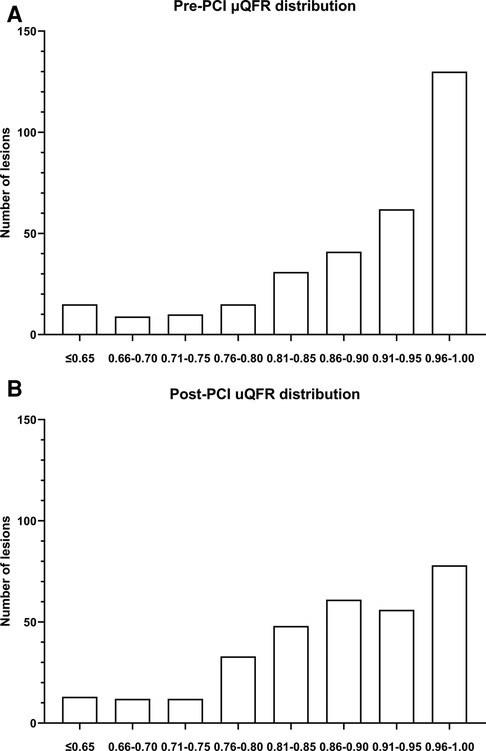
Figure 2. Pre- (A) and post-procedural (B) μQFR distribution of SBs in all the included lesions (n = 313). The median and interquartile range of post-procedural SB μQFR were 0.89 and 0.15 (0.81–0.96), respectively.
Pre-stenting, post-stenting, and follow-up μQFR in MV and SB in the three groups are shown in Tables 4, 5, respectively. The post-stenting and follow-up SB μQFR both significantly increased across the tertiles of post-procedural SB μQFR (all P < 0.05). The post-stenting and follow-up SB μQFR were both found to significantly increase across the tertiles of post-procedural SB μQFR (all P < 0.05), but the absolute difference among groups was small.
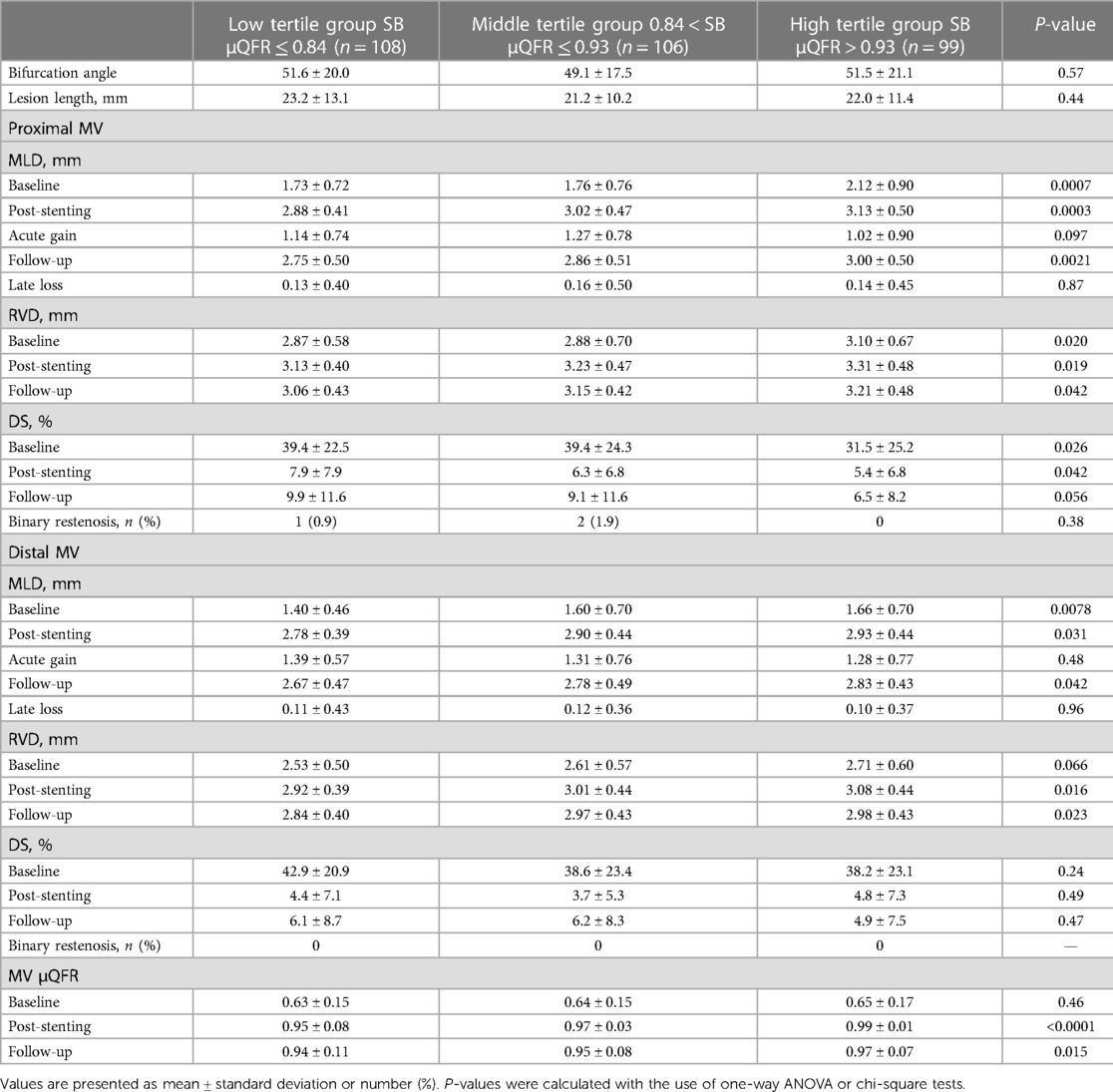
Table 4. Quantitative coronary angiography and Murray law–based quantitative flow ratio analysis in main vessel.
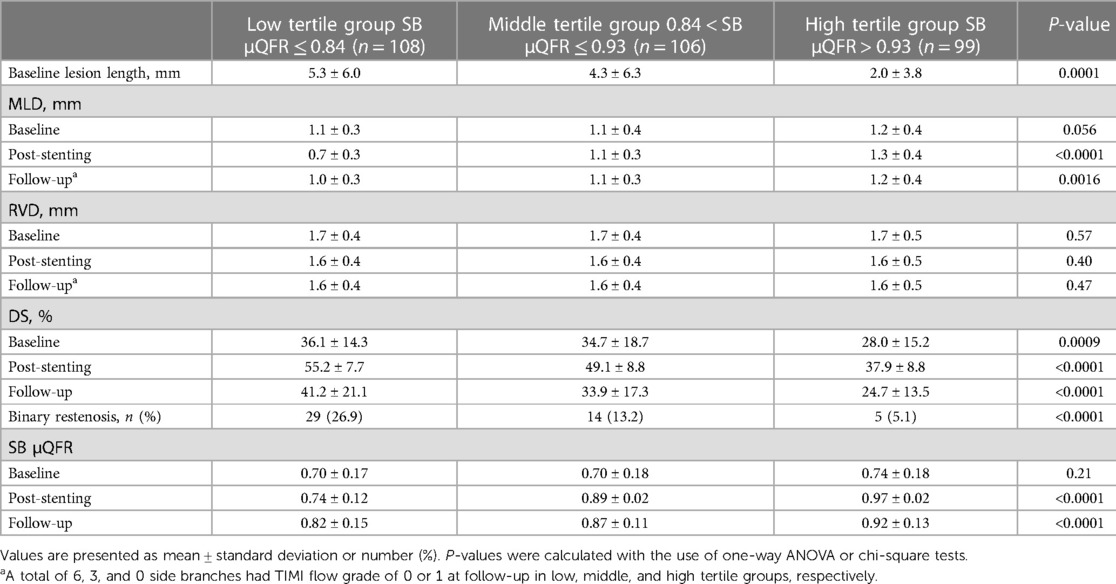
Table 5. Quantitative coronary angiography and Murray law–based quantitative flow ratio analysis in side branch.
Pre-PCI, post-PCI, and follow-up μQFR in lesions with and without long-term SB TIMI flow grade ≤1 are shown in Supplementary Table S4. Pre-stenting, post-stenting, and follow-up μQFR were significantly lower in lesions with long-term SB TIMI flow grade ≤1 than those with long-term SB TIMI flow grade >1 (all P < 0.05). No significant change of μQFR between post-stenting and follow-up was observed.
The results of QCA analyses in MV and SB are detailed in Tables 4, 5, respectively. The lesion length, DS, and incidences of SB binary restenosis at angiographic follow-up decreased significantly across the post-procedural SB μQFR tertiles (all P < 0.05). SB RVDs among the three groups were comparable.
QCA analyses in lesions with and without long-term SB TIMI flow grade ≤1 are detailed in Supplementary Table S5. Pre-PCI and follow-up distal % DS; post-PCI and follow-up SB MLD; and pre-PCI, post-PCI, and follow-up SB % DS were significantly different between lesions with and without long-term SB TIMI flow grade ≤1 (all P < 0.05). Binary restenosis was more observed in lesions with long-term SB TIMI flow grade ≤1 than those without long-term SB TIMI flow grade ≤1 (62.5% vs. 10.4%, P < 0.0001).
A total of 8 (2.6%), 16 (5.1%), 61 (19.5%), and 228 (72.8%) SBs had a TIMI flow grade of 0, 1, 2, and 3 at follow-up, respectively. Supplementary Table S6 presented the SB TIMI flow grade in the three groups at angiographic follow-up. The incidence of SB TIMI flow grade ≤1 and ≤2 both numerically decrease across the post-procedural SB μQFR tertiles (SB TIMI flow ≤ 1: P = 0.086; SB TIMI flow ≤ 2: P = 0.052; Figure 3).
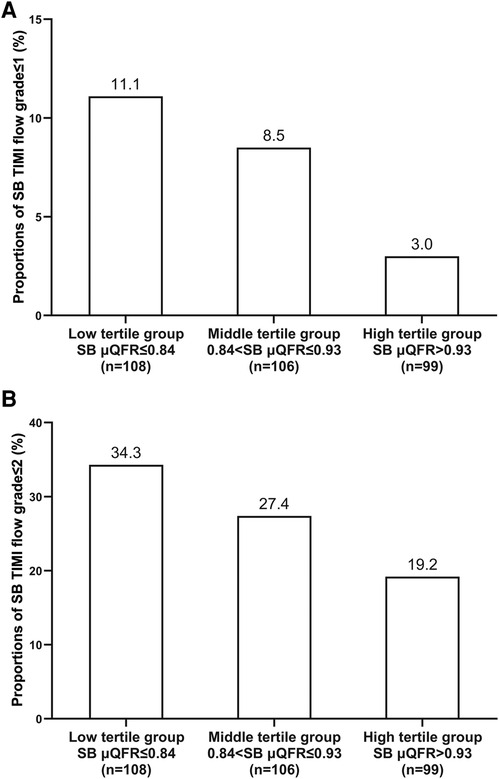
Figure 3. Incidences of SB TIMI flow grade ≤1 (A) and ≤2 (B) assessed at angiographic follow-up across the post-procedural SB μQFR tertiles.
Also, collateral flow from other coronary artery was observed in six (75.0%) SBs with long-term SB TIMI flow of 0, six (37.5%) with long-term SB TIMI flow of 1, two (3.3%) with long-term SB TIMI flow of 2, and zero with long-term SB TIMI flow of 3.
The κ coefficient for inter-operator variability in assessing SB TIMI flow grade was 0.78, and the κ coefficient for inter-operator variability in assessing SB TIMI flow grade ≤1 or >1 was 0.95.
Figure 4 shows the ROC curve. The area under the curve was 0.6673 (95% CI, 0.5610–0.7737; P = 0.0064), and the optimal cut-off value of post-procedural SB μQFR for identifying long-term SB TIMI flow grade ≤1 was 0.77, with the specificity of 37.50% (21.16%–57.29%) and the sensitivity of 87.20% (82.85%–90.57%). In the univariable logistic regression model, post-procedural SB μQFR ≤0.77 was associated with a 3.25-fold increased risk in long-term SB TIMI flow grade ≤1. After adjusting the characteristics of patient (age, gender, hypertension, hyperlipidemia, diabetes, smoking status), lesion [true coronary bifurcation, LAD bifurcation], and procedure (stent diameter, stent type), post-procedural SB μQFR ≤0.77 was independently associated with a 2.57-fold increased risk (adjusted OR, 2.57; 95% CI, 1.02–7.25; P = 0.045) in long-term SB TIMI flow grade ≤1 in a multivariable logistic regression model (Table 6).
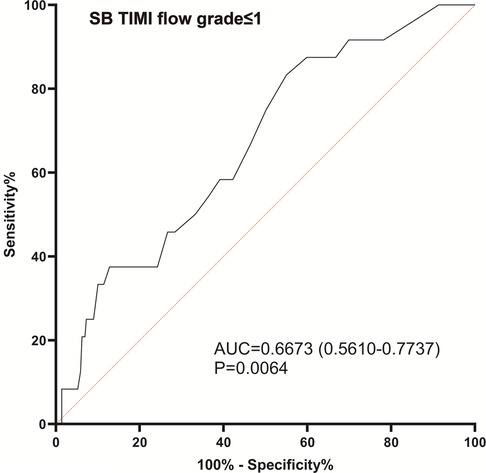
Figure 4. Receiver operating characteristic curve analyses for post-procedural SB μQFR to identify long-term SB TIMI flow grade ≤1 assessed at angiographic follow-up.
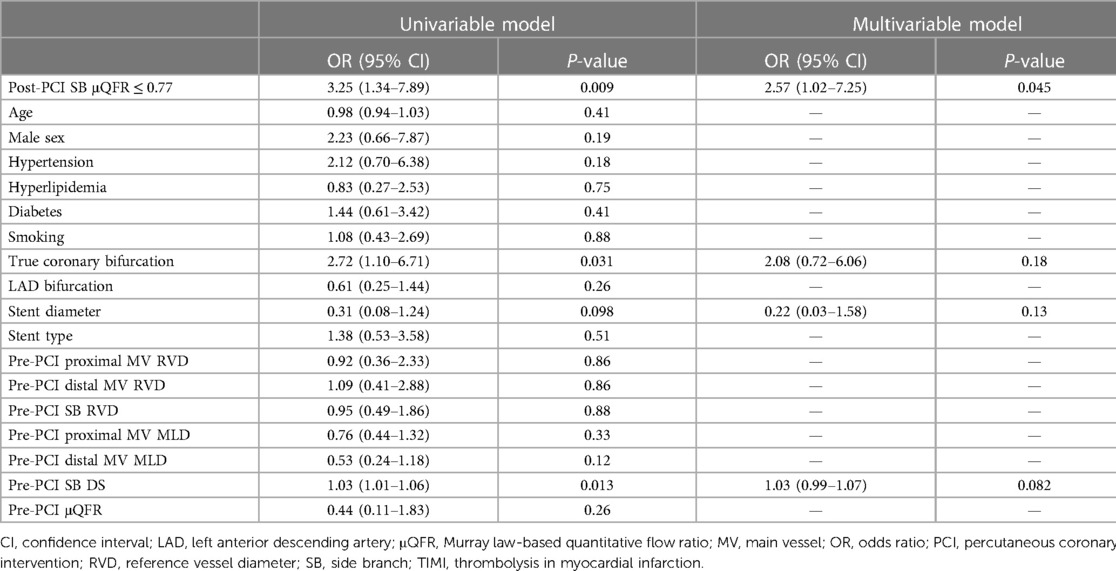
Table 6. Univariable and multivariable logistic regression analyses for long-term SB TIMI flow grade ≤1.
Supplementary Table S7 detailed the ROC analyses results of post-procedural SB μQFR and SB DS to identify the SB TIMI flow grade ≤1 at angiographic follow-up in the all included lesions and in groups with different SB RVD. No significant differences in diagnostic accuracy between post-procedural SB μQFR and SB DS were observed in all included lesions and in groups with different SB RVDs.
The follow-up duration was 12.3 ± 3.0 months. No death or stent thrombosis occurred in the overall population. MI occurred in two (1.5%) patients. A total of 14 (9.6%) patients received target vessel revascularization.
The main finding of our study is a relationship between post-PCI μQFR values in the SB and long-term SB TIMI grade flow. The incidence of SB TIMI flow grade ≤1 or ≤2 at angiographic follow-up both tended to decrease across the post-procedural SB μQFR tertiles. Post-procedural SB μQFR ≤0.77 was found to be independently associated with a 2.57-fold increased risk in long-term SB TIMI flow grade ≤1 after adjustment.
The occurrence of SB compromise is the most important concern of PCI operators when MV bifurcation lesions are treated with a one-stent strategy approach. The SB compromise severity may vary from anatomic stenosis alone with no flow limitation to complete SB occlusion, which might lead to clinical outcome impairment. The prognostic impact of SB occlusion in the long term varies with the amount of subtended myocardium and patient characteristics, with overall higher incidences in clinically significant MI or even death associated to this complication of PCI (26, 27). Subsequent reintervention after PCI may be required when significant SB flow limitation occurs after MV stenting in clinical trials for coronary bifurcation lesions (6, 7, 24, 28) and suggested by expert consensus (29). However, the prediction of the occurrence of impaired long-term SB conductance based on the angiographic results of PCI is difficult. One study showed that in 230 jailed side branches with TIMI flow grade 3, vessel size >2 mm, and lesion length <10 mm, 10.4% had FFR ≤0.75 (10). Koo et al. assessed the FFR of 65 lesions both immediately after procedure and 6 months after the index procedure, and found no significant changes in FFR for SB during follow-up (0.87 ± 0.06 vs. 0.87 ± 0.09) (30). Among them, 5% of patients without KBI had functionally patent side branch and 20% of those with functional restenosis had new or worsening angina during follow-up. Functional late loss might exist (ΔFFR: −0.02 ± 0.09) in lesions with KBI. Thus, a substantial proportion of jailed SBs with acceptable angiographic results and normal coronary blood flow may develop functional impairment over time, leading to clinical events, angina, or reinterventions. However, no useful and clinically feasible tools for SB functional compromise in routine practice are currently available.
The severity of SB compromise was most commonly assessed under visual estimation using angiograms. Although it is easy in routine practice, it is inaccurate and subjective because (1) visual assessment for anatomical compromise often overestimate the “true” jailed SB severity, (2) the consistency between anatomical narrowing and coronary physiology was not high, and (3) inter-operator variability is wide (31). Koo et al. had showed that in 73 jailed SB lesions with ≥75% stenosis by visual estimation after MV stenting, only 20 had functional significance (FFR ≤ 0.80) (32). Ahn et al. found that in 230 jailed SB lesions after MV stenting, the correlation (r = −0.21) between the post-procedural SB DS and FFR was poor, and the incidence (17.8%) of functional significance (FFR ≤0.80) was low. Only 28.4% had FFR ≤0.80 among 67 SBs with >50% DS (10). Both studies indicated that coronary angiographic characteristics had poor accuracy to predict functional SB significance after MV stenting. One explanation is that the carina shift leads to the eccentric luminal SB ostium narrowing, which leads to the true residual lumen area underestimation in jailed SB lesions (31). Also, a 4,000-lesion cohort study showed that about one-third of lesions had discordance between angiographic DS % ≥50% and FFR ≤0.80 (33), indicating that anatomical coronary narrowing assessment might be influenced by other factors, such as technical limitations for lesion detection and physiological factors. Thus, visual assessment may be not an accurate, objective, and repeatable approach for SB compromise. Intracoronary imaging tools, such as intravascular ultrasound and optical coherence tomography, may help improve SB anatomical compromise assessment (34, 35). However, the use of both intracoronary physiology and imaging devices to interrogate SB after stenting is not always easy and free of risks. Out of proximal and accessible LM bifurcation stenoses, SB in stented bifurcation lesions is not easy to reach and to instrument with guidewires or imaging catheters, particularly in stenosis located in vessels of moderate size, angulated or with calcification. Even when performed with care, instrumentation of SB with diagnostic devices may cause peri-procedural complications, such as dissection, spasm, embolism, and MV stent deformation.
FFR is the gold standard for coronary functional assessment and helps guide revascularization (36, 37). Its use in SB functional assessment had been reported in clinical studies (30). Angiography-guided provisional SB stenting was compared with FFR-guided provisional stenting in 320 patients with true coronary bifurcations lesions in the DKCRUSH-VI trial (24). Although 1-year clinical outcomes were comparable, FFR-guided strategy may lead to somewhat lesser stent implantations and a numerally lower restenosis rate. The 12th consensus document from the European Bifurcation Club suggested deferring the SB treatment when the FFR value is above 0.80 in a jailed SB (38). However, FFR measurement after MV stenting is technically challenging and warrants upfront cost in all patients. Patients who are allergic to vasodilators (i.e., adenosine, adenosine triphosphate) or ineligible due to the lesion characteristics (i.e., severe tortuous and heavily calcified lesion) also cannot receive FFR assessment. For these reasons, its routine use is not feasible for SB assessment.
An interesting alternative to intracoronary tools for the assessment of SB after bifurcation PCI is QFR, a pressure wire–free technique for coronary functional assessment that has demonstrated a high diagnostic accuracy (92.7%) compared with FFR (11). However, QFR is limited in estimating FFR in SB because QFR requires two satisfactory angiographic views obtained with at least 25° in separation, which is not always available in routine practice. The modified version called μQFR has been recently developed to overcome it and is based on a single angiographic view, supported by artificial intelligence for automatic MV and SB delineation. It was found to have an excellent diagnostic performance even when suboptimal angiographic image projection is used (13). In our study, post-procedural SB μQFR was found to be clinically feasible. Post-procedural SB μQFR ≤0.77 was found to be independently associated with about threefold increased risk in long-term SB TIMI flow grade ≤1. Thus, μQFR can be used to evaluate the SB compromise severity and identify the SBs with higher risk in impaired TIMI flow grade at follow-up. Explanations on this association between lower post-PCI μQFR and impaired TIMI flow grade at follow-up might be that (1) since operators routinely inject intracoronary nitroglycerin before performing the post-PCI angiogram, coronary blood flow might appear to be better especially for SB; (2) SB TIMI flow might be of grade (3) but the absolute blood flow velocity in SB might be lower than that in MV because of SB compromise. Due to the aggravation of SB residual lesion and insufficient perfusion of SB-related coronary microvascular bed, long-term SB TIMI flow grade might be impaired. We suggest that future studies might focus on testing whether procedural SB optimization based on µQFR leads to improved SB conductance in the long term.
As a pressure wire–free technique, μQFR could overcome the technical difficulty of crossing a pressure wire to the stent struts, avoid FFR-related peri-procedural complications, and reduce the upfront cost of pressure wire in all the patients when assessing SB compromise. Also, μQFR can be performed in patients allergic to vasodilators or ineligible due to the lesion characteristics of those who could not receive FFR assessment. Thus, μQFR can be used to optimize PCI strategy in more patients than FFR. Moreover, μQFR could improve clinical feasibility in SB evaluation as compared with the original QFR version because it requires two satisfied angiographic views acquired with a minimal of 25° in separation. The μQFR is a safe and easy approach to assess SB functional compromise in routine practice and is thus potentially useful for optimizing non-LM coronary bifurcation lesion interventional strategy in routine clinical practice. This requires further investigation. Given the complexity of coronary bifurcation intervention, the decision-making on further SB intervention after MV stenting may need to involve additional information under consideration, such as clinical importance, technical difficulty, and complication risk.
First, as a retrospective study, the incidences of different SB TIMI flow grades at follow-up in non-LM coronary bifurcation lesions receiving the one-stent strategy might be biased by patient selection. Large-scale prospective studies with controlled angiographic follow-up may provide more useful information. Second, the μQFR computation was performed offline. Online μQFR performance requires further investigation. Third, historical angiographic image records for analyses were used, which might challenge the μQFR computation due to the suboptimal projections for bifurcation lesions and images quality. A previous study revealed that μQFR had high diagnostic accuracy in estimating FFR in suboptimal projections (13). Also, agreement between QFR and FFR was observed to be good in vessels with angiograms acquired under low x-ray frame and pulse rate setting (7.5 fps and 7 pps modes) (39). Thus, μQFR computation can be used in poor-quality angiograms. Fourth, the mean SB RVD was 1.6 mm, smaller than most of previous studies on coronary bifurcation lesions. Thus, the incidence of SBs with TIMI flow grade ≤2 might be higher than that in previous studies (40). Fifth, the baseline proximal MV RVD increased across the tertiles of post-procedural SB μQFR in this study, from 2.87 mm in the low tertile group to 3.10 mm in the high tertile group. One explanation is that lesions in the low tertile group had more diffused coronary atherosclerotic plaques affecting accurate RVD assessment. The absolute difference in baseline RVD of proximal MV between the low and high tertile groups was low (0.23 mm), which might have little clinical significance. We had also included the RVDs of both MV and SB into multivariable models for adjustment. Results showed that no association existed between MV RVD and long-term SB TIMI coronary blood flow, and the association between post-procedural SB μQFR and long-term SB TIMI coronary blood flow was not influenced by the MV RVD. Sixth, the specificity of μQFR <0.77 as 37.50% was low. Considering that the cut-off value of SB μQFR is used for identifying SB at higher risk in long-term impaired blood flow and might be helpful to determine the SB reintervention immediately after index procedure, the sensitivity might be more clinically important. In this study, the sensitivity of μQFR <0.77% as 87.20% was satisfactory. Also, other cofounders may be also important for long-term SB TIMI flow grade. Seventh, since this study was a retrospective study, we did not record data regarding angina severity. Future prospective studies are required to address these questions.
In this study, post-procedural SB μQFR was found to be independently associated with approximately threefold increased risk in impaired SB TIMI flow at long-term follow-up. Further investigations are warranted for prospective validations and exploring its use in optimizing interventional strategy for non-LM coronary bifurcation lesions.
The datasets presented in this article are not readily available because of regulation restrictions. Requests to access the datasets should be directed to LS,cmpzaGVubGluZ2hvbmdAMTI2LmNvbQ==.
The studies involving human participants were reviewed and approved by the Ethics Committee of Shanghai Chest Hospital, Shanghai Jiao Tong University School of Medicine. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
KX, YJ, LiS, and BH conceptualized and undertook this study. WY, WZ, DW, YZ, SZ, and ZH participated in the data analysis and interpretation. LaS, LJ, XQ, JE, and ST contributed to the composing and criticizing of this work. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (Grant/Award Numbers: 81830010, 81770428, and 81900308), Shanghai Science and Technology Committee (Grant/Award Number: 18411950400), Emerging and Advanced Technology Programs of Hospital Development Center of Shanghai (Grant/Award Number: SHDC12018129), and Multi-Centered Clinical Research Foundation, Shanghai Jiaotong University, School of Medicine (Grant/Award Number: DLY201512). KX was supported by Shanghai Sailing Program (Grant Number: 20YF1444200). WZ was supported by Shanghai Sailing Program (Grant Number: 19YF1444600).
We thank Yunxiao Chang for the technical assistance with μQFR analyses performed at Biomedical Instrument Institute, School of Biomedical Engineering, Shanghai Jiao Tong University, Shanghai, China. We also thank Weituo Zhang from the Shanghai Jiao Tong University School of Medicine, Shanghai, China, for the statistical consultation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1217069/full#supplementary-material
1. Castro-Dominguez YS, Wang Y, Minges KE, McNamara RL, Spertus JA, Dehmer GJ, et al. Predicting in-hospital mortality in patients undergoing percutaneous coronary intervention. J Am Coll Cardiol. (2021) 78(3):216–29. doi: 10.1016/j.jacc.2021.04.067
2. Kimura T, Morimoto T, Nakagawa Y, Kawai K, Miyazaki S, Muramatsu T, et al. Very late stent thrombosis and late target lesion revascularization after sirolimus-eluting stent implantation: five-year outcome of the j-Cypher Registry. Circulation. (2012) 125(4):584–91. doi: 10.1161/CIRCULATIONAHA.111.046599
3. Sawaya FJ, Lefevre T, Chevalier B, Garot P, Hovasse T, Morice MC, et al. Contemporary approach to coronary bifurcation lesion treatment. JACC Cardiovasc Interv. (2016) 9(18):1861–78. doi: 10.1016/j.jcin.2016.06.056
4. Kralev S, Poerner TC, Basorth D, Lang S, Wolpert C, Haghi D, et al. Side branch occlusion after coronary stent implantation in patients presenting with ST-elevation myocardial infarction: clinical impact and angiographic predictors. Am Heart J. (2006) 151(1):153–7. doi: 10.1016/j.ahj.2005.01.034
5. Burzotta F, Lassen JF, Lefevre T, Banning AP, Chatzizisis YS, Johnson TW, et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15(th) consensus document from the European Bifurcation Club. Euro Interv. (2021) 16(16):1307–17. doi: 10.4244/EIJ-D-20-00169
6. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. (2006) 114(18):1955–61. doi: 10.1161/CIRCULATIONAHA.106.664920
7. Colombo A, Bramucci E, Sacca S, Violini R, Lettieri C, Zanini R, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) study. Circulation. (2009) 119(1):71–8. doi: 10.1161/CIRCULATIONAHA.108.808402
8. Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. (2010) 121(10):1235–43. doi: 10.1161/CIRCULATIONAHA.109.888297
9. Song YB, Hahn JY, Yang JH, Choi SH, Choi JH, Lee SH, et al. Differential prognostic impact of treatment strategy among patients with left main versus non-left main bifurcation lesions undergoing percutaneous coronary intervention: results from the COBIS (Coronary Bifurcation Stenting) Registry II. JACC Cardiovasc Interv. (2014) 7(3):255–63. doi: 10.1016/j.jcin.2013.11.009
10. Ahn JM, Lee JY, Kang SJ, Kim YH, Song HG, Oh JH, et al. Functional assessment of jailed side branches in coronary bifurcation lesions using fractional flow reserve. JACC Cardiovasc Interv. (2012) 5(2):155–61. doi: 10.1016/j.jcin.2011.10.015
11. Xu B, Tu S, Qiao S, Qu X, Chen Y, Yang J, et al. Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis. J Am Coll Cardiol. (2017) 70(25):3077–87. doi: 10.1016/j.jacc.2017.10.035
12. Xu B, Tu S, Song L, Jin Z, Yu B, Fu G, et al. Angiographic quantitative flow ratio-guided coronary intervention (FAVOR III China): a multicentre, randomised, sham-controlled trial. Lancet. (2021) 398(10317):2149–59. doi: 10.1016/S0140-6736(21)02248-0
13. Tu S, Ding D, Chang Y, Li C, Wijns W, Xu B. Diagnostic accuracy of quantitative flow ratio for assessment of coronary stenosis significance from a single angiographic view: a novel method based on bifurcation fractal law. Catheter Cardiovasc Interv. (2021) 97(Suppl 2):1040–7. doi: 10.1002/ccd.29592
14. Cortes C, Liu L, Berdin SL, Fernandez-Corredoira PM, Zhang R, Schafer U, et al. Agreement between Murray law-based quantitative flow ratio (muQFR) and three-dimensional quantitative flow ratio (3D-QFR) in non-selected angiographic stenosis: a multicenter study. Cardiol J. (2022) 29(3):388–95. doi: 10.5603/CJ.a2022.0030
15. Ding D, Tu S, Chang Y, Li C, Xu B, Wijns W. Quantitative flow ratio based on Murray fractal law: accuracy of single versus two angiographic views. JSCAI. (2022) 1:100399. doi: 10.1016/j.jscai.2022.100399
16. Louvard Y, Medina A. Definitions and classifications of bifurcation lesions and treatment. Euro Interv. (2015) 11(Suppl V):V23–6. doi: 10.4244/EIJV11SVA5
17. Lunardi M, Louvard Y, Lefevre T, Stankovic G, Burzotta F, Kassab GS, et al. Definitions and standardized endpoints for treatment of coronary bifurcations. J Am Coll Cardiol. (2022) 80(1):63–88. doi: 10.1016/j.jacc.2022.04.024
18. Salem H, Mintz GS, Matsumura M, Zhang M, Usui E, Seike F, et al. Reasons for lesion uncrossability as assessed by intravascular ultrasound. Catheter Cardiovasc Interv. (2022) 99(7):2028–37. doi: 10.1002/ccd.30202
19. Roberts EB, Grayson AD, Alahmar AE, Andron M, Perry R, Stables RH. Predicting angiographic outcome in contemporary percutaneous coronary intervention: a lesion-specific logistic model. J Interv Cardiol. (2010) 23(4):394–400. doi: 10.1111/j.1540-8183.2010.00566.x
20. Davies SW, Marchant B, Lyons JP, Timmis AD, Rothman MT, Layton CA, et al. Irregular coronary lesion morphology after thrombolysis predicts early clinical instability. J Am Coll Cardiol. (1991) 18(3):669–74. doi: 10.1016/0735-1097(91)90787-A
21. Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, et al. Standardized end point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation. (2018) 137(24):2635–50. doi: 10.1161/CIRCULATIONAHA.117.029289
22. Li Z, Li G, Chen L, Ding D, Chen Y, Zhang J, et al. Comparison of coronary CT angiography-based and invasive coronary angiography-based quantitative flow ratio for functional assessment of coronary stenosis: a multicenter retrospective analysis. J Cardiovasc Comput Tomogr. (2022) S1934-5925(22):00100–9. doi: 10.1016/j.jcct.2022.06.002
23. Collet C, Onuma Y, Cavalcante R, Grundeken M, Genereux P, Popma J, et al. Quantitative angiography methods for bifurcation lesions: a consensus statement update from the European Bifurcation Club. Euro Interv. (2017) 13(1):115–23. doi: 10.4244/EIJ-D-16-00932
24. Chen SL, Ye F, Zhang JJ, Xu T, Tian NL, Liu ZZ, et al. Randomized comparison of FFR-guided and angiography-guided provisional stenting of true coronary bifurcation lesions: the DKCRUSH-VI trial (double kissing crush versus provisional stenting technique for treatment of coronary bifurcation lesions VI). JACC Cardiovasc Interv. (2015) 8(4):536–46. doi: 10.1016/j.jcin.2014.12.221
25. TIMI Study Group. The thrombolysis in myocardial infarction (TIMI) trial. Phase I findings. N Engl J Med. (1985) 312(14):932–6. doi: 10.1056/NEJM198504043121437
26. Muramatsu T, Onuma Y, Garcia-Garcia HM, Farooq V, Bourantas CV, Morel MA, et al. Incidence and short-term clinical outcomes of small side branch occlusion after implantation of an everolimus-eluting bioresorbable vascular scaffold: an interim report of 435 patients in the ABSORB-EXTEND single-arm trial in comparison with an everolimus-eluting metallic stent in the SPIRIT first and II trials. JACC Cardiovasc Interv. (2013) 6(3):247–57. doi: 10.1016/j.jcin.2012.10.013
27. Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II registry (coronary bifurcation stenting). J Am Coll Cardiol. (2013) 62(18):1654–9. doi: 10.1016/j.jacc.2013.07.041
28. Pan M, Medina A, Romero M, Ojeda S, Martin P, Suarez de Lezo J, et al. Assessment of side branch predilation before a provisional T-stent strategy for bifurcation lesions. A randomized trial. Am Heart J. (2014) 168(3):374–80. doi: 10.1016/j.ahj.2014.05.014
29. Albiero R, Burzotta F, Lassen JF, Lefevre T, Banning AP, Chatzizisis YS, et al. Treatment of coronary bifurcation lesions, part I: implanting the first stent in the provisional pathway. The 16th expert consensus document of the European Bifurcation Club. Euro Interv. (2022) 18(5):e362–76. doi: 10.4244/EIJ-D-22-00165
30. Koo BK, Park KW, Kang HJ, Cho YS, Chung WY, Youn TJ, et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. (2008) 29(6):726–32. doi: 10.1093/eurheartj/ehn045
31. Koo BK, De Bruyne B. FFR in bifurcation stenting: what have we learned? Euro Interv. (2010) 6(Suppl J):J94–8. doi: 10.4244/EIJV6SUPJA15
32. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. (2005) 46(4):633–7. doi: 10.1016/j.jacc.2005.04.054
33. Toth G, Hamilos M, Pyxaras S, Mangiacapra F, Nelis O, De Vroey F, et al. Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J. (2014) 35(40):2831–8. doi: 10.1093/eurheartj/ehu094
34. Ha J, Kim JS, Mintz GS, Kim BK, Shin DH, Ko YG, et al. 3D OCT versus FFR for jailed side-branch ostial stenoses. JACC Cardiovasc Imaging. (2014) 7(2):204–5. doi: 10.1016/j.jcmg.2013.06.011
35. Koh JS, Koo BK, Kim JH, Yang HM, Park KW, Kang HJ, et al. Relationship between fractional flow reserve and angiographic and intravascular ultrasound parameters in ostial lesions: major epicardial vessel versus side branch ostial lesions. JACC Cardiovasc Interv. (2012) 5(4):409–15. doi: 10.1016/j.jcin.2012.01.013
36. Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, Szekely L, et al. Fractional flow reserve-guided PCI as compared with coronary bypass surgery. N Engl J Med. (2022) 386(2):128–37. doi: 10.1056/NEJMoa2112299
37. De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. (2012) 367(11):991–1001. doi: 10.1056/NEJMoa1205361
38. Lassen JF, Burzotta F, Banning AP, Lefevre T, Darremont O, Hildick-Smith D, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. Euro Interv. (2018) 13(13):1540–53. doi: 10.4244/EIJ-D-17-00622
39. Jin C, Ramasamy A, Safi H, Kilic Y, Tufaro V, Bajaj R, et al. Diagnostic accuracy of quantitative flow ratio (QFR) and vessel fractional flow reserve (vFFR) estimated retrospectively by conventional radiation saving x-ray angiography. Int J Cardiovasc Imaging. (2021) 37(5):1491–501. doi: 10.1007/s10554-020-02133-8
Keywords: coronary bifurcation lesion, fractional flow reserve, one-stent strategy, percutaneous coronary intervention, quantitative flow ratio
Citation: Xu K, Jiang Y, Yang W, Zhang W, Wang D, Zhao Y, Zheng S, Hao Z, Shen L, Jiang L, Qiu X, Escaned J, Tu S, Shen L and He B (2023) Post-procedural and long-term functional outcomes of jailed side branches in stented coronary bifurcation lesions assessed with side branch Murray law–based quantitative flow ratio. Front. Cardiovasc. Med. 10:1217069. doi: 10.3389/fcvm.2023.1217069
Received: 4 May 2023; Accepted: 19 July 2023;
Published: 3 August 2023.
Edited by:
Yao-Jun Zhang, Xuzhou Medical University, ChinaReviewed by:
Tetsumin Lee, Musashino Red Cross Hospital, Japan© 2023 Xu, Jiang, Yang, Zhang, Wang, Zhao, Zheng, Hao, Shen, Jiang, Qiu, Escaned, Tu, Shen and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linghong Shen cmpzaGVubGluZ2hvbmdAMTI2LmNvbQ== Ben He cmpoZWJlbkAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.