- Heart Center, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Paroxysmal atrial fibrillation originates most commonly in the pulmonary veins. However, the superior vena cava has proved to be arrhythmogenic in some cases. Pulsed field ablation, an emerging ablation technology, selectively affects myocardial tissue. Herein, we present a case of paroxysmal atrial fibrillation in a 64-year-old man who was admitted to our hospital for pulsed field ablation. The tachycardia was recurrent despite four successful pulmonary vein isolations. The superior vena cava was determined to be involved in arrhythmogenesis. The atrial fibrillation terminated immediately after the pulsed field ablation discharge at the superior vena cava.
Introduction
Atrial fibrillation is the most common sustained arrhythmia, and pulmonary vein isolation is the cornerstone for ablation of paroxysmal atrial fibrillation. Pulmonary vein isolation is commonly performed using cryoballoon or radiofrequency ablation. The “Fire and Ice” trial demonstrated that radiofrequency ablation and cryoballoon ablation were comparable with respect to efficacy and safety in paroxysmal atrial fibrillation ablation (1). Pulsed field ablation is an emerging ablation technique that selectively ablates myocardial tissue. Theoretically, the application of pulsed field ablation to paroxysmal atrial fibrillation is safer because it avoids damage to collateral tissues. Furthermore, the procedural and fluoroscopy time are shorter in pulsed field ablation than in radiofrequency ablation.
The superior vena cava is a common location of non-pulmonary vein foci of atrial fibrillation (2). In selected patients in whom the superior vena cava is identified as a trigger for atrial fibrillation, superior vena cava ablation significantly reduces atrial fibrillation recurrence (3). Pulsed field ablation has excellent effectiveness and safety in isolating pulmonary veins (4). However, pulsed field ablation applied to the superior vena cava in paroxysmal atrial fibrillation has not been reported. Herein, we report a case in which paroxysmal atrial fibrillation terminated after the discharge of pulsed field ablation at the superior vena cava.
Case presentation
A 64-year-old man with a two-year history of paroxysmal atrial fibrillation was admitted to our facility for palpitations. The tachycardia was recurrent despite four successful pulmonary vein isolations. His electrocardiogram at admission displayed sinus rhythm, whereas the electrocardiogram during palpitations displayed atrial fibrillation. His physical examination findings and blood test results were unremarkable. Transesophageal echocardiography revealed no thrombosis of the left atrial appendage. The left ventricular ejection fraction was 69% and the left atrial diameter was 40 mm. The left atrial volume was 112 ml according to a three-dimensional electroanatomical map. With the patient's informed consent, pulsed field ablation was performed under general anesthesia.
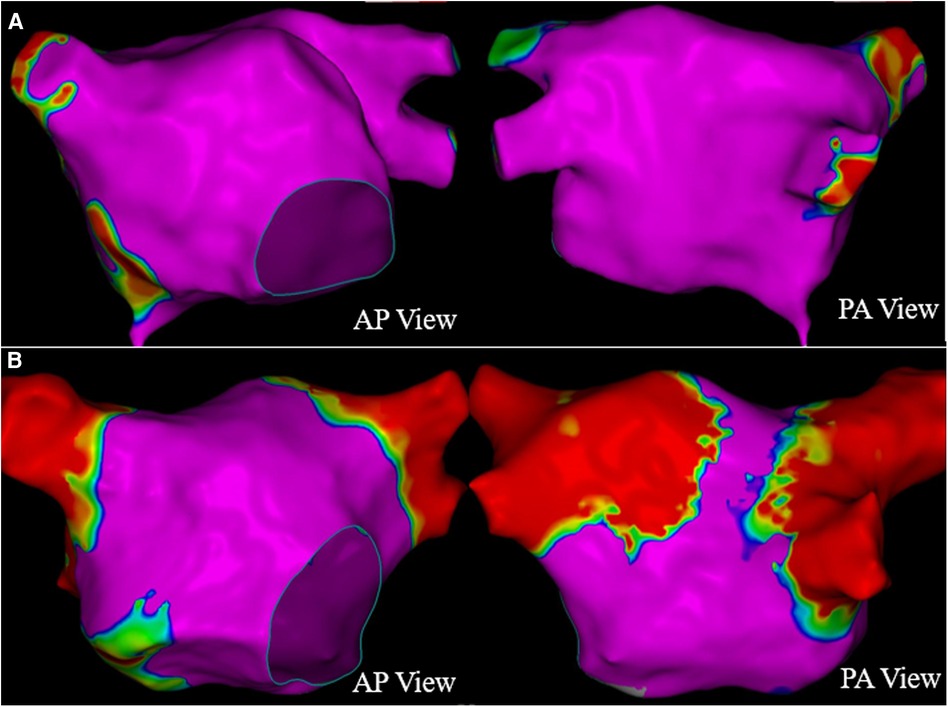
The patient presented sinus rhythm at the beginning of the procedure. However, atrial fibrillation recurred during left atrial mapping using a PentaRay catheter (Biosense Webster, Inc., Irvine, CA, USA). After all pulmonary veins were successfully isolated using an 8-F circular pulsed field ablation catheter (Shineyo Medical, Shanghai, China), atrial fibrillation persisted. The circular pulsed field ablation catheter was then placed within the superior vena cava, revealing some brief fractionated potentials and a local atrial fibrillation cycle length shorter than that in the coronary sinus (Figure 1). The atrial fibrillation terminated after a pulsed field ablation catheter discharge at the superior vena cava (biphasic, 1,400 V) (Figure 2). The left atrial voltage map pre- and post-pulsed field ablation is shown in Figure 3. The total procedure time was 2 h with a superior vena cava ablation time of 20 s.
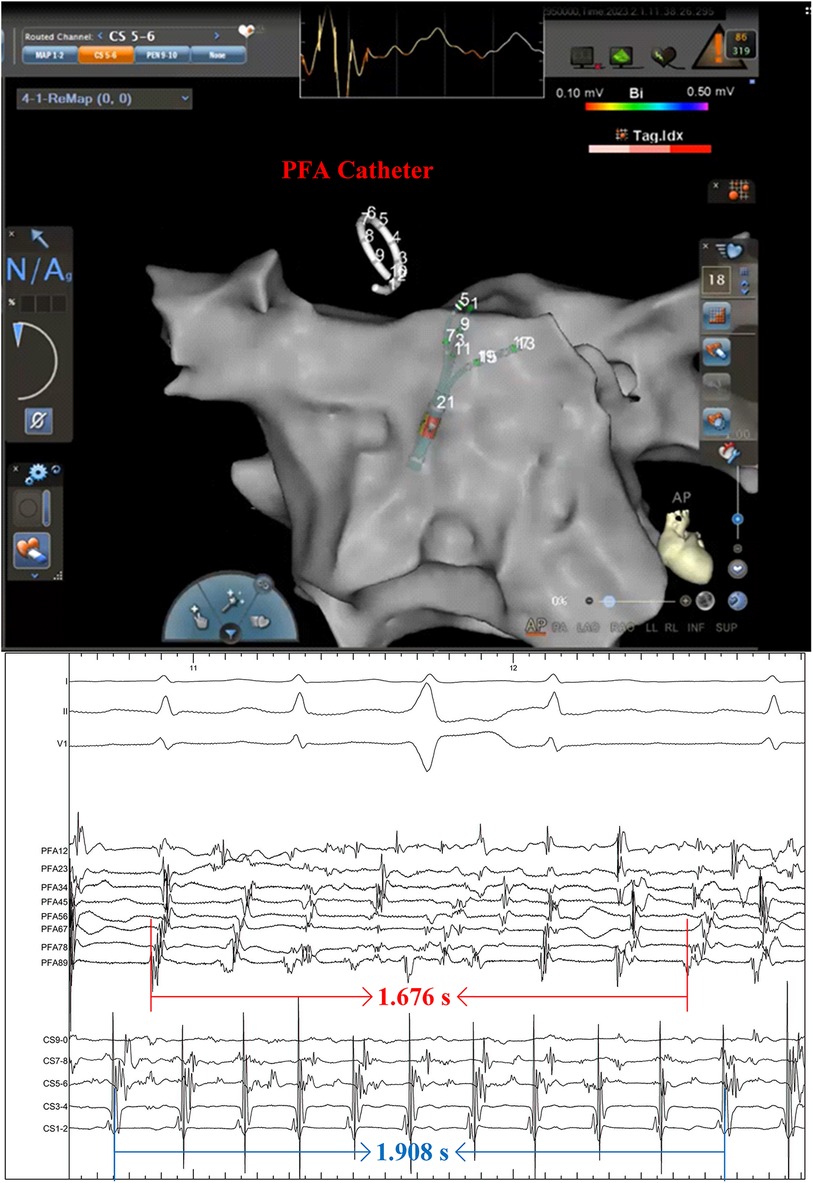
Figure 1. A pulsed field ablation catheter was positioned within the superior vena cava, revealing the disorganized electrical activity. The intracardiac electrocardiogram was recorded at a speed of 100 mm/s.

Figure 2. The atrial fibrillation terminated after the pulsed field ablation catheter discharged at the superior vena cava. The electrocardiogram was recorded at a speed of 100 mm/s.
According to the monitoring parameters, such as heart rate, cerebrovascular risk assessment, and diaphragm mobility, there were no peri-procedural complications. The patient was free of atrial fibrillation at the three-month follow-up.
Discussion
To the best of our knowledge, this is the first reported case of pulsed field ablation of the superior vena cava in a patient with paroxysmal atrial fibrillation. Pulsed field ablation appears to be safe and effective for superior vena cava isolation.
Pulsed field ablation is a novel and promising ablation technique in which ultrafast electrical fields (in seconds) are applied to myocardial tissue (5). In a 2019 human trial, Reddy et al. (6) first demonstrated that pulsed field ablation has excellent tissue selectivity and preferentially ablates myocardial tissue. Furthermore, pulsed field ablation can rapidly and durably isolate pulmonary veins (6). Therefore, the pulsed field ablation was deemed to be a promising method in pulmonary vein isolation.
Atrial fibrillation is most frequently initiated by the pulmonary veins. However, 10% to 20% of atrial fibrillation originates from extra-pulmonary vein locations, such as the superior vena cava, posterior left atrial wall, Marshall ligament, crista terminalis, coronary sinus ostium, and left atrial appendage (7–9). Among non-pulmonary vein triggers, superior vena cava origins account for approximately 37%, next to the posterior left atrial wall (7). Superior vena cava isolation is commonly performed using radiofrequency energy. However, stenosis of the superior vena cava and injury to the sinoatrial node and phrenic nerve are potential complications of radiofrequency ablation of the superior vena cava (10–12). Furthermore, as compared with pulsed field ablation, superior vena cava isolation using radiofrequency has a more complex workflow because of point-by-point ablation and tagging the location of the phrenic nerve on the three-dimensional map. In contrast, pulsed field ablation has exceptional tissue selectivity and no effect on the phrenic nerve (13). Moreover, pulsed field ablation delivers electric pulses of very short duration that result in irreversible tissue injury. In the present case, the superior vena cava was isolated in 20 s, as compared with an average of 7.8 min for radiofrequency ablation and 36.9 s for cryoballoon ablation in previous studies (14, 15).
The feasibility and safety of pulsed field ablation of the superior vena cava were demonstrated in a previous animal trial (16). We preliminarily demonstrated that pulsed field ablation is effective and safe for superior vena cava isolation in patients with atrial fibrillation. Regrettably, anatomical mapping of the right atrium and superior vena cava were not performed.
Conclusion
We have reported a case of successful superior vena cava isolation using pulsed field ablation in a patient with atrial fibrillation. Pulsed field ablation is an alternative method to isolate the arrhythmogenic superior vena cava, with potential advantages of shorter procedure time and fewer complications than radiofrequency.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YT and YZ drafted the manuscript. XS and WL researched the literature. LS and YW performed the procedure. XL reviewed and critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kuck KH, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KR, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. (2016) 374:2235–45. doi: 10.1056/NEJMoa1602014
2. Miyazaki S, Takigawa M, Kusa S, Kuwahara T, Taniguchi H, Okubo K, et al. Role of arrhythmogenic superior vena cava on atrial fibrillation. J Cardiovasc Electrophysiol. (2014) 25:380–6. doi: 10.1111/jce.12342
3. Arruda M, Mlcochova H, Prasad SK, Kilicaslan F, Saliba W, Patel D, et al. Electrical isolation of the superior vena cava: an adjunctive strategy to pulmonary vein antrum isolation improving the outcome of AF ablation. J Cardiovasc Electrophysiol. (2007) 18:1261–6. doi: 10.1111/j.1540-8167.2007.00953.x
4. Reddy VY, Dukkipati SR, Neuzil P, Anic A, Petru J, Funasako M, et al. Pulsed field ablation of paroxysmal atrial fibrillation: 1-year outcomes of IMPULSE, PEFCAT, and PEFCAT II. JACC Clin Electrophysiol. (2021) 7:614–27. doi: 10.1016/j.jacep.2021.02.014
5. Reddy VY, Koruth J, Jais P, Petru J, Timko F, Skalsky I, et al. Ablation of atrial fibrillation with pulsed electric fields: an ultra-rapid, tissue-selective modality for cardiac ablation. JACC Clin Electrophysiol. (2018) 4:987–95. doi: 10.1016/j.jacep.2018.04.005
6. Reddy VY, Neuzil P, Koruth JS, Petru J, Funosako M, Cochet H, et al. Pulsed field ablation for pulmonary vein isolation in atrial fibrillation. J Am Coll Cardiol. (2019) 74:315–26. doi: 10.1016/j.jacc.2019.04.021
7. Lin WS, Tai CT, Hsieh MH, Tsai CF, Lin YK, Tsao HM, et al. Catheter ablation of paroxysmal atrial fibrillation initiated by non-pulmonary vein ectopy. Circulation. (2003) 107:3176–83. doi: 10.1161/01.cir.0000074206.52056.2d
8. Santangeli P, Zado ES, Hutchinson MD, Riley MP, Lin D, Frankel DS, et al. Prevalence and distribution of focal triggers in persistent and long-standing persistent atrial fibrillation. Heart Rhythm. (2016) 13:374–82. doi: 10.1016/j.hrthm.2015.10.023
9. Di Biase L, Burkhardt JD, Mohanty P, Sanchez J, Mohanty S, Horton R, et al. Left atrial appendage: an underrecognized trigger site of atrial fibrillation. Circulation. (2010) 122:109–18. doi: 10.1161/circulationaha.109.928903
10. Sacher F, Jais P, Stephenson K, O'Neill MD, Hocini M, Clementy J, et al. Phrenic nerve injury after catheter ablation of atrial fibrillation. Indian Pacing Electrophysiol J. (2007) 7:1–6. PMID: 1723536717235367
11. Kühne M, Schaer B, Osswald S, Sticherling C. Superior vena cava stenosis after radiofrequency catheter ablation for electrical isolation of the superior vena cava. Pacing Clin Electrophysiol. (2010) 33:e36–8. doi: 10.1111/j.1540-8159.2009.02588.x
12. Chen G, Dong JZ, Liu XP, Zhang XY, Long DY, Sang CH, et al. Sinus node injury as a result of superior vena cava isolation during catheter ablation for atrial fibrillation and atrial flutter. Pacing Clin Electrophysiol. (2011) 34:163–70. doi: 10.1111/j.1540-8159.2010.02903.x
13. Yavin H, Brem E, Zilberman I, Shapira-Daniels A, Datta K, Govari A, et al. Circular multielectrode pulsed field ablation catheter lasso pulsed field ablation: lesion characteristics, durability, and effect on neighboring structures. Circ Arrhythm Electrophysiol. (2021) 14:e009229. doi: 10.1161/circep.120.009229
14. Iacopino S, Osório TG, Filannino P, Artale P, Sieira J, Ströker E, et al. Safety and feasibility of electrical isolation of the superior vena cava in addition to pulmonary vein ablation for paroxysmal atrial fibrillation using the cryoballoon: lessons from a prospective study. J Interv Card Electrophysiol. (2021) 60:255–60. doi: 10.1007/s10840-020-00740-y
15. Wang XH, Liu X, Sun YM, Shi HF, Zhou L, Gu JN. Pulmonary vein isolation combined with superior vena cava isolation for atrial fibrillation ablation: a prospective randomized study. Europace. (2008) 10:600–5. doi: 10.1093/europace/eun077
Keywords: pulsed field ablation, paroxysmal atrial fibrillation, superior vena cava, arrhythmogenesis, radiofrequency ablation
Citation: Tao Y, Zhou Y, Sun X, Liao W, Wang Y, Shi L and Liu X (2023) Pulsed field ablation of superior vena cava in paroxysmal atrial fibrillation: a case report. Front. Cardiovasc. Med. 10:1211674. doi: 10.3389/fcvm.2023.1211674
Received: 25 April 2023; Accepted: 16 June 2023;
Published: 30 June 2023.
Edited by:
Alexander H. Maass, University Medical Center Groningen, NetherlandsReviewed by:
Bart Mulder, University Medical Center Groningen, NetherlandsZhen Wang, Huazhong University of Science and Technology, China
Songyun Wang, Renmin Hospital of Wuhan University, China
© 2023 Tao, Zhou, Sun, Liao, Wang, Shi and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xingpeng Liu eHBsaXU3MUB2aXAuc2luYS5jb20=
 Yirao Tao
Yirao Tao Yang Zhou
Yang Zhou Xuerong Sun
Xuerong Sun Liang Shi
Liang Shi Xingpeng Liu
Xingpeng Liu