Abstract
Background/introduction:
Currently, despite continued issues with durability ( 1), biological prosthetic valves are increasingly chosen over mechanical valves for surgical aortic valve replacement (SAVR) in adult patients of all ages, at least in Western countries. For younger patients, this choice means assuming the risks associated with a redo SAVR or valve-in-valve procedure.
Purpose:
To assess the use of mechanical vs. biological valve prostheses for SAVR relative to patient's age and implant time in a large population extracted from the French National Database EPICARD.
Methods:
Patients in EPICARD undergoing SAVR from 2007 to 2022 were included from 22 participating public or private centers chosen to represent a balanced representation of centre sizes and geographical discrepancies. Patients with associated pathology of the aorta (aneurysm or dissection) and requiring a vascular aortic prosthesis were excluded. Comparisons were made amongst centers, valve choice, implant date range, and patient age.
Results:
We considered 101,070 valvular heart disease patients and included 72,375 SAVR (mean age 71.4 ± 12.2 years). We observed a mechanical vs. biological prosthesis ratio (MBPR) of 0.14 for the overall population. Before 50 years old (y-o), MBPR was >1.3 (p < 0.001) while patients above 60 years-old received principally biological SAVR (p < 0.0001). Concerning patients between 50 and 60 years-old patients, MPVR was 1.04 (p = 0.03). Patients 50–60 years-old from the first and second study duration quartile (before August 2015) received preferentially mechanical SAVR (p < 0.001). We observed a shift towards more biological SAVR (p < 0.001) for patients from the third and fourth quartile to reach a MBPR at 0.43 during the last years of the series. Incidentally, simultaneous mitral valve replacement were more common in case of mechanical SAVR (p < 0.0001), while associated CABGs were more frequent in case of biological SAVR (p < 0.0001).
Conclusion:
In a large contemporary French patient population, real world practice showed a recent shift towards a lower age-threshold for biological SAVR as compared to what would suggest contemporary guidelines.
Introduction
Currently, despite continued issues with durability (1), biological prosthetic valves are increasingly chosen over mechanical valves for surgical aortic valve replacement (SAVR) in adult patients of all ages, at least in Western countries. For younger patients, this choice means assuming the risks associated with a redo SAVR or valve-in-valve procedure.
Mechanical prosthetic valves (MPVs), for which oral direct Factor Xa inhibitors failed to be a valid option (2, 3), are not generally considered in patients above 65 years-old, even if a long-standing anticoagulant therapy is required and despite the fact that acceptable outcomes with a MPV may be achieved in selected elderly patients (4). To avoid imposing to a young patient a life-long anticoagulant therapy whenever a Ross procedure or an aortic valvular repair is out of reach, a BPV in aortic position is often perceived to be the best second choice. Thus, in Western countries and despite consensus recommendations (5–7), BPVs are nowadays implanted in a significant proportion of young and middle-aged patients requiring SAVR (8) therefore assuming the risks associated with a subsequent redo SAVR or with a valve-in-valve trans catheter aortic valve replacement (ViV-TAVR). Concerning TAVR, lowering the age-threshold and extending indications towards low-risk patients will further amplify this global move towards BPV with an exponential rise (9).
Potentially as a consequence of results of TAVR in patients at intermediate risk (10), we aimed at illustrate how much, in France, the pendulum has reached towards BPVs especially for middle-aged patients requiring a SAVR during the past 15 years. We therefore launched a large multi-centric survey to assess the use of mechanical vs. biological valve prostheses for SAVR relative to patient's age and implant time in a large population extracted from the French National Database EPICARD.
Material and methods
Starting 20 years ago, the French National Database EPICARD is hosted on a central computer server headed by the Federation of Medical Specialities, Issy les Moulineaux, France and is prospectively implemented via internet by each logged-in participant through a dedicated e-Form including pre, per and post operative data. There has been no restriction, in France, to the availability of devices and funding for world wide marketed devices or for warfarin and other anticoagulant therapies during the study's period of time and physicians had full influence on which devices they used.
Ethics
The EPICARD database was declared to the French National Commission for Data Protection and Liberties (CNIL ⋕1221925). Patients were informed of the potential utilization of their anonymized data for scientific purpose and could ask that their case would not be entered into the dataset. Provided that no commercial use of the data would be made and that no indication of trade mark or label of any specific prosthetic valves used would be published, our survey was approved by the Scientific Committee of the French National Database EPICARD. The study was performed in accordance with the ethical standards of in the 1964 Declaration of Helsinki and its later amendments. Use of all data strictly followed the General Data Protection Regulations.
Study population
Patients in EPICARD undergoing SAVR from 2007 to 2022 were included from 22 participating public or private centers chosen to represent a balanced representation of centre sizes and geographical discrepancies (Figure 1). Patients aged under 19 years-old or patients with associated pathology of the aorta (aneurysm or dissection) and requiring a vascular aortic prosthesis were excluded. Comparisons were made amongst centers, valve choice, implant date range, and patient age.
Figure 1
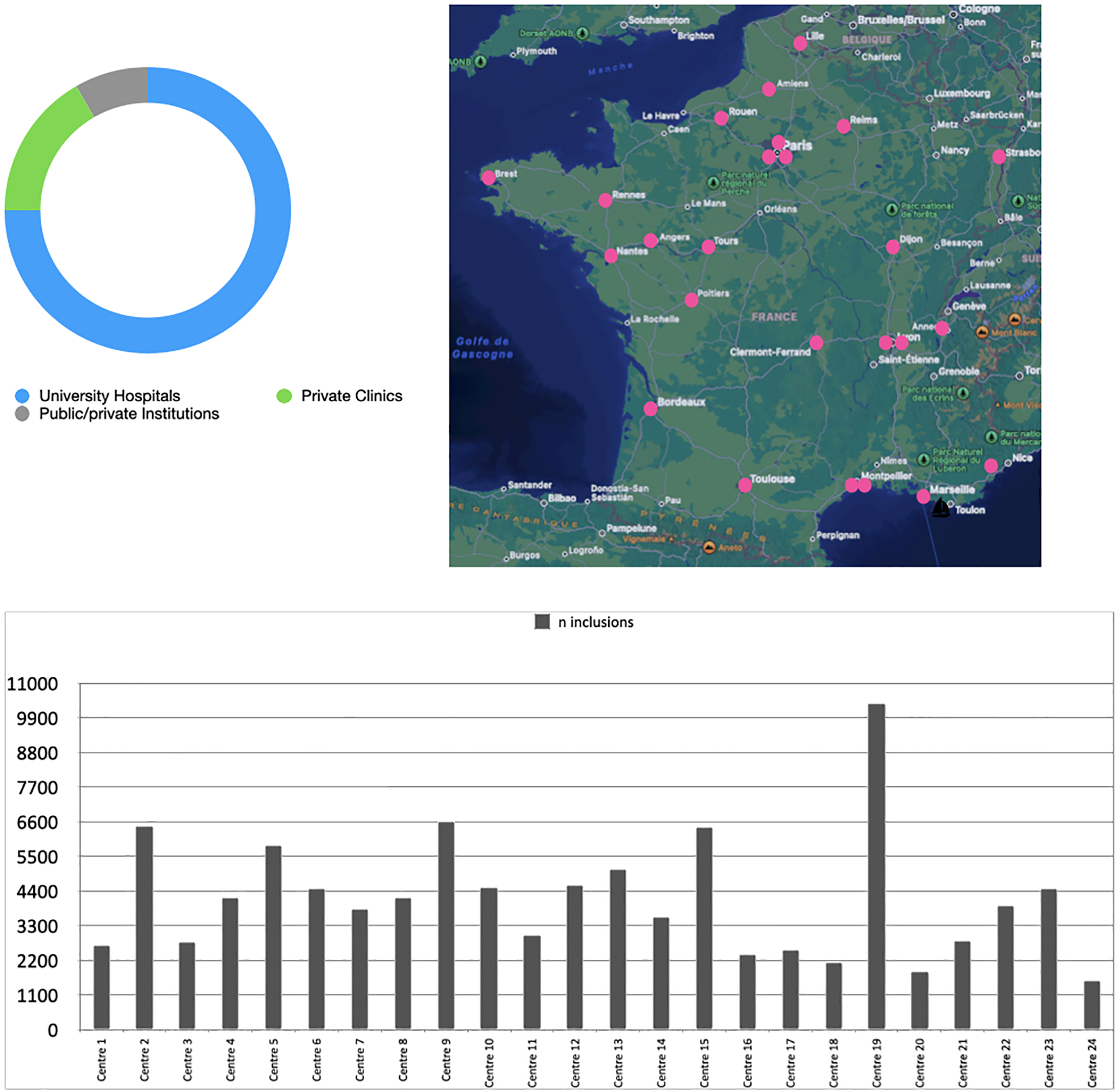
Carbon-Free survey, distribution of participating centres.
Data on preoperative (demographic, clinical and echocardiographic) characteristics, perioperative characteristics, EuroSCORE, and in-hospital mortality/morbidity after cardiac surgery were collected for each patient. Patients who underwent an associated valvular procedure or associated CABGs were included. Anonymized data were extracted under a Excel-sheet format which allowed for further statistical analysis with MedCalc. Means are expressed with SD deviation, rates are expressed with their Poisson 95% Confidence Interval (95% CI). Continuous and categorial variables were compared with a t-test, a Wilcoxon rank-sum test, or a Pearson χ2-statistic whenever required. Tests were based on a two tailed p-value for an α-risk at 5%. Because data about long term follow-up remain seldom in the EPICARD database, results were restricted to the in-hospital period. Patients were categorized into duration quartiles according to the date of operation: Q1 (18,093 patients) between 01/01/2007 and 24/10/2011; Q2 (18,093 patients) between 24/10/2011 and 02/07/2015; Q3 (18,093 patients) between 02/07/2015 and 29/01/2019; Q4 (18,096 patients) between 29/01/2019 and 31/12/2022.
Results
Population
Out of 411,375 patients entered into the EPICARD Database during the study period, a population still including a very large amount of patients operated on for CABG only, we considered 101,070 valvular heart disease patients and included 72,375 SAVR (mean age 71.4 ± 12.2 years) 26,185 of which were women (36.1%). SAVR was performed as a redo surgery in 5,434 cases (7.5%). SAVR was an isolated procedure in most cases and was associated with another valve procedure in 7,123 cases (9.8%) or with CABG in 15,621 cases (21.6%). A total of 63,466 patients (87.7%) received a BPV and 8,909 patients received a MPV. Therefore we observed a mechanical vs. biological prosthesis ratio (MBPR) of 0.14 for the overall population. Patient's preoperative characteristics for each prosthetic valve type are detailed in Table 1 and overall age distribution where percentages are representative of the proportion of patients from our population in each class of age is presented in Figure 2.
Table 1
| Mechanical valves 8,909 | Biological valves 63,466 | p | |
|---|---|---|---|
| Age, mean. (SD) | 57.1 (11.6) | 73.5 (10.9) | <0.0001 |
| Women, No. (%; 95% CI) | 2,841 (31.9; 30.7–33.1) | 23,344 (36.8; 36.3–37.3) | <0.0001 |
| BMI (kg/m2), mean. (SD) | 27.91 (10.73) | 27.79 (8.76) | 0.2 |
| EuroSCORE II, mean. (SD) | 2.83 (5.2) | 3.96 (6.1) | <0.0001 |
| Left ventricular ejection fraction (LVEF), mean. (SD) LVEF < 30 (%; 95% CI) | 58.4 (12.4) | 58.6 (11.9) | 0.31 |
| 276 (3.1) | 1,901 (3) | 0.72 | |
| Systolic pulmonary arterial pressure (SPAP), mmHg, mean (SD) SPAP > 55 mmHg, No. (%; 95% CI) | 32.9 (11.9) | 33.8 (12.9) | <0.0001 |
| 490 (5.5; 5–6) | 3,053 (4.8; 4.6–4.9) | 0.006 | |
| Previous AF (%; 95% CI) | 62 (0.7; 0.5–0.8) | 1,495 (2.36; 2.23–2.47) | <0.0001 |
| Previous Anticoagulation (%; 95% CI) VKA | 645 (7.2; 6.6–7.8) | 4,800 (7.6; 7.3–7.8) | 0.27 |
| Direct Anticoagulant | 38 (0.4; 0.3–0.6) | 1,091 (1.7; 1.6–1.8) | <0.0001 |
| Diabetes (%; 95% CI) | 1,483 (16.6; 15.8–17.5) | 14,055 (22.1; 21.8–22.5) | <0.0001 |
| Extracardiac arteriopathy (%; 95% CI) | 711 (7.9; 7.4–8.5) | 7,765 (12.2; 12–12.5) | <0.0001 |
| COPD (%; 95% CI) | 554 (6.2; 5.7–6.7) | 4,953 (7.8; 7.6–8) | <0.0001 |
| Endocarditis (%; 95% CI) | 506 (5.7; 5.2–6.1) | 2,626 (4.1; 3.9–4.3) | <0.0001 |
| Aortic regurgitation None, No. (%; 95% CI) | 4,238 (47.5; 46.1–49) | 40,113 (63; 62.6–63.8) | <0.0001 |
| Mild, No. (%; 95% CI) | 932 (10.5; 9.8–11.1) | 6,477 (10.2; 9.9–10.5) | 0.47 |
| Moderate, No. (%; 95% CI) | 1,131 (12.7; 11.9–13.4) | 4,366 (6.9; 6.7–7.1) | <0.0001 |
| Severe, No. (%; 95% CI) | 1,460 (16.4; 15.6–17.2) | 5,068 (8.4; 7.7–9) | <0.0001 |
| Mitral regurgitation None, No. (%; 95% CI) | 7,823 (87.8; 85.9–89.8) | 58,134 (91.6; 90.9–92.3) | 0.0005 |
| Mild, No. (%; 95% CI) | 179 (2; 1.7–2.3) | 1,506 (2.3; 2.2–2.5) | 0.03 |
| Moderate, No. (%; 95% CI) | 385 (4.3; 3.9–4.7) | 1,442 (2.2; 2.1–2.4) | <0.0001 |
| Severe, No. (%; 95% CI) | 387 (4.3; 3.9–4.8) | 1,420 (2.2; 1.8–2.4) | <0.0001 |
| Tricuspid regurgitation None, No. (%; 95% CI) | 8,504 (95,4; 93.4–97.5) | 61,458 (96.8; 96.1–97.6) | 0.21 |
| Mild, No. (%; 95% CI) | 73 (0.8; 0.6–1) | 443 (0.7; 0.6–0.8) | 0.2 |
| Moderate, No. (%; 95% CI) | 134 (1.5; 1.3–1.7) | 513 (0.8; 0.7–0.9) | <0.0001 |
| Severe, No. (%; 95% CI) | 147 (16.5; 14–19.4) | 399 (6.3; 5.6–6.9) | <0.0001 |
| Aortic stenosis (%; 95% CI) | 5,856 (65.7; 64–67.4) | 49,525 (78; 77–79) | <0.0001 |
| Mitral stenosis (%; 95% CI) | 609 (6.8; 6.3–7.4) | 1,309 (2; 1.9–2.1) | <0.0001 |
Preoperative characteristics at admission and echocardiography.
Figure 2
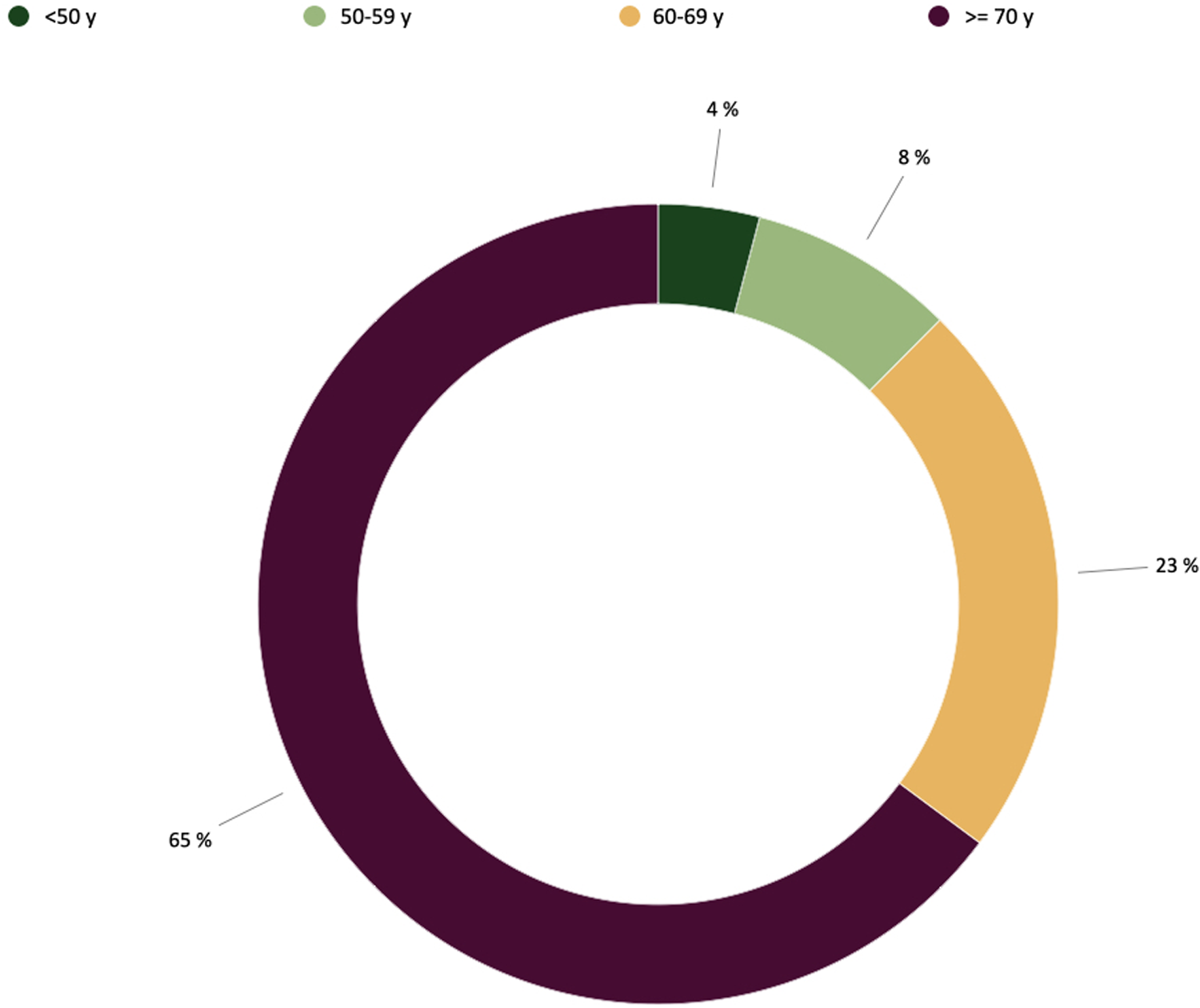
Proportion of patients with regards to age for each type of valvular prothesis in aortic position according to the ESC and AHA-ACC recommendations.
Proportion of biological vs. mechanical prosthesis according to age
Out of the 8,909 patients who received a mechanical prosthetic valve, most patients who received a mechanical SAVR (6,913) were under 50 years-old. In this class of age, MBPR was >1.3 (p < 0.001) while patients above 60 years-old received principally biological SAVR (p < 0.0001). Concerning patients between 50 and 60 years-old patients, MPVR was 1.04 (p = 0.03). Patients 50–60 years-old from the first and second study duration quartile (before August 2015) received preferentially mechanical SAVR (p < 0.001). We observed a shift towards more biological SAVR (p < 0.001) for patients from the third and fourth quartile to reach a MBPR at 0.43 during the last years of the series.
Figure 3 describes the distribution for each type of valvular prothesis per age decade throughout the overall 15 years of the survey. Figure 4 shows the trend across time of mechanical vs. biological SAVR in this sub-group population together with a landmark of the Partner II study (10) which may have affected the implantation policy.
Figure 3
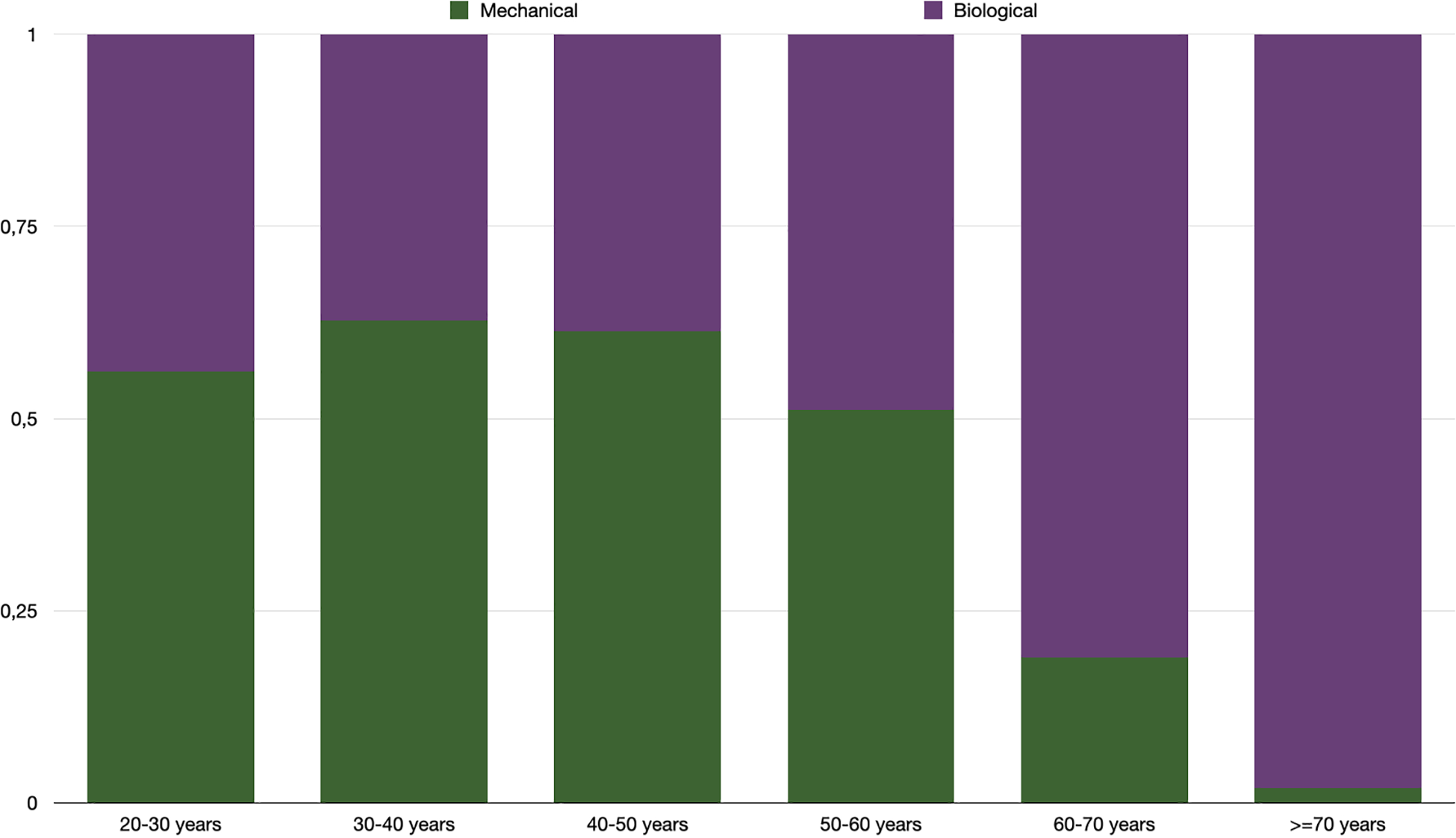
Proportion of SAVR with mechanical versus biological prosthetic valve per class of age during the overall study time (2007–2022).
Figure 4
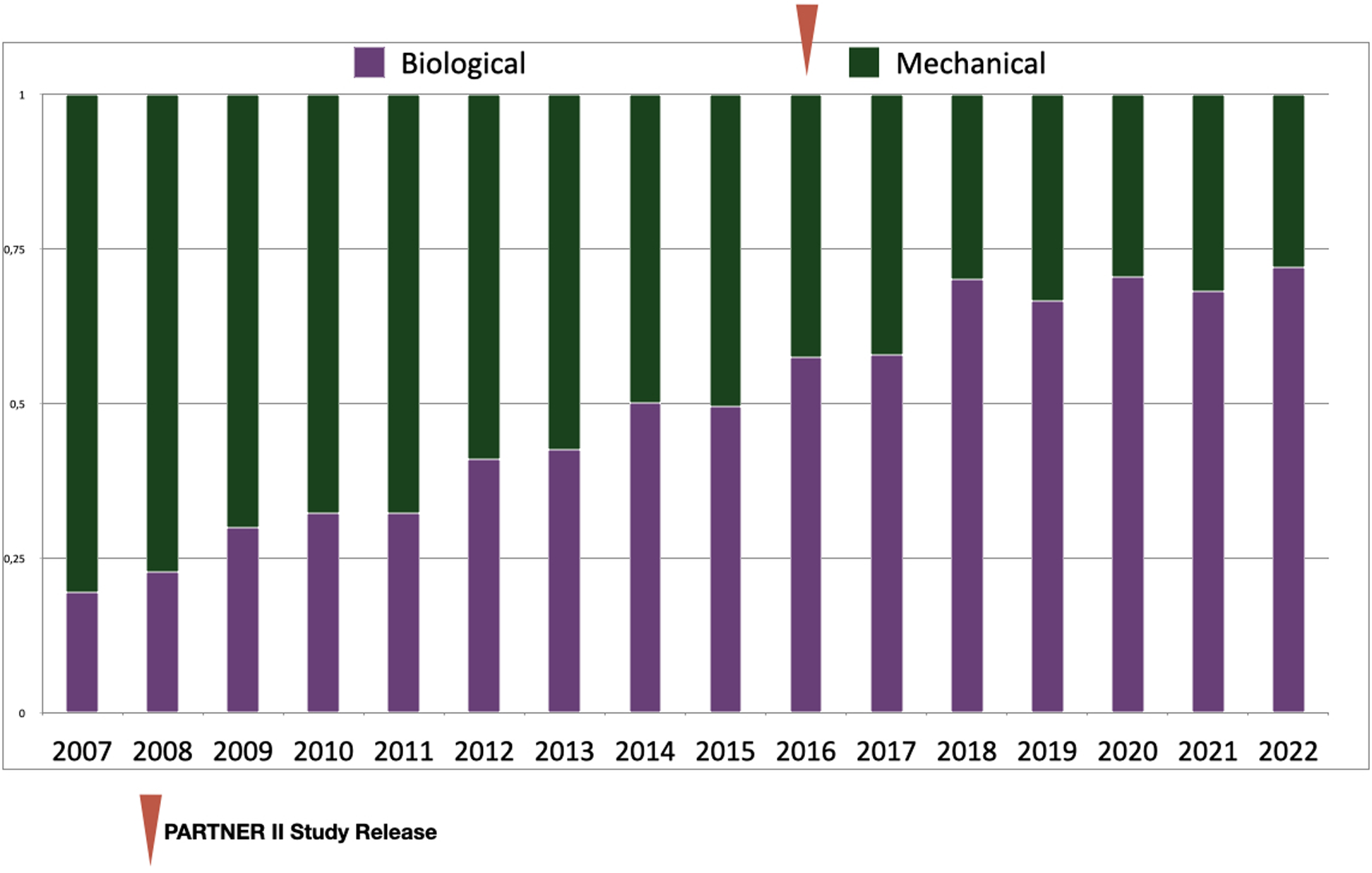
Proportion of SAVR with biological versus mechanical prosthetic valves for patients between 50 and 60 years-old per year during study time (2007–2022).
Proportion of biological vs. mechanical prosthesis according to other factors
A significantly higher proportion of women received BPVs. Though childbearing considerations might have play a role, sex was however not a criteria of choice in patients under 40 years old for which 63% women vs. 60% men received a MPV in aortic position (NS). Probably more a consequence of an older age than a criteria of choice, patients receiving a BPV had more co-morbidity (Table 1) like diabetes, peripheral arteriopathy or chronic obstructive pulmonary disease (p < 0.0001) and a higher EuroSCORE II as well (p < 0.001). On another hand, when endocarditis was the underlying heart valve disease requiring SAVR, significantly more MPVs were used. Previous AF or anticoagulant therapy were a rare instance in both groups but were more common in recipients for a BPV in aortic position (direct anticoagulants). Incidentally, the type of valve for SAVR was influenced by associated procedures. Simultaneous mitral valve replacement and tricuspid annuloplasty were more common in case of mechanical SAVR (p < 0.0001) in relation to a more diffused and advanced heart valve disease, while associated CABGs were more frequent in case of biological SAVR (p < 0.0001) with the effect to avoid, in most cases, a combined life-long antiaggregant-anticoagulant therapy. Together with the fact that more recipients of MPVs had already experienced a previous surgery (p < 0.0001), discrepancies in associated procedures may have influenced both mean aortic clamping time and duration of ECC which were significantly increased for SAVR with a MPV. Finally, concerning the choice between a biological or a mechanical SAVR, we observed a centre effect which varied with time especially with regards to patients within the intermediate age of 50–60 years-old (Figure 5).
Figure 5
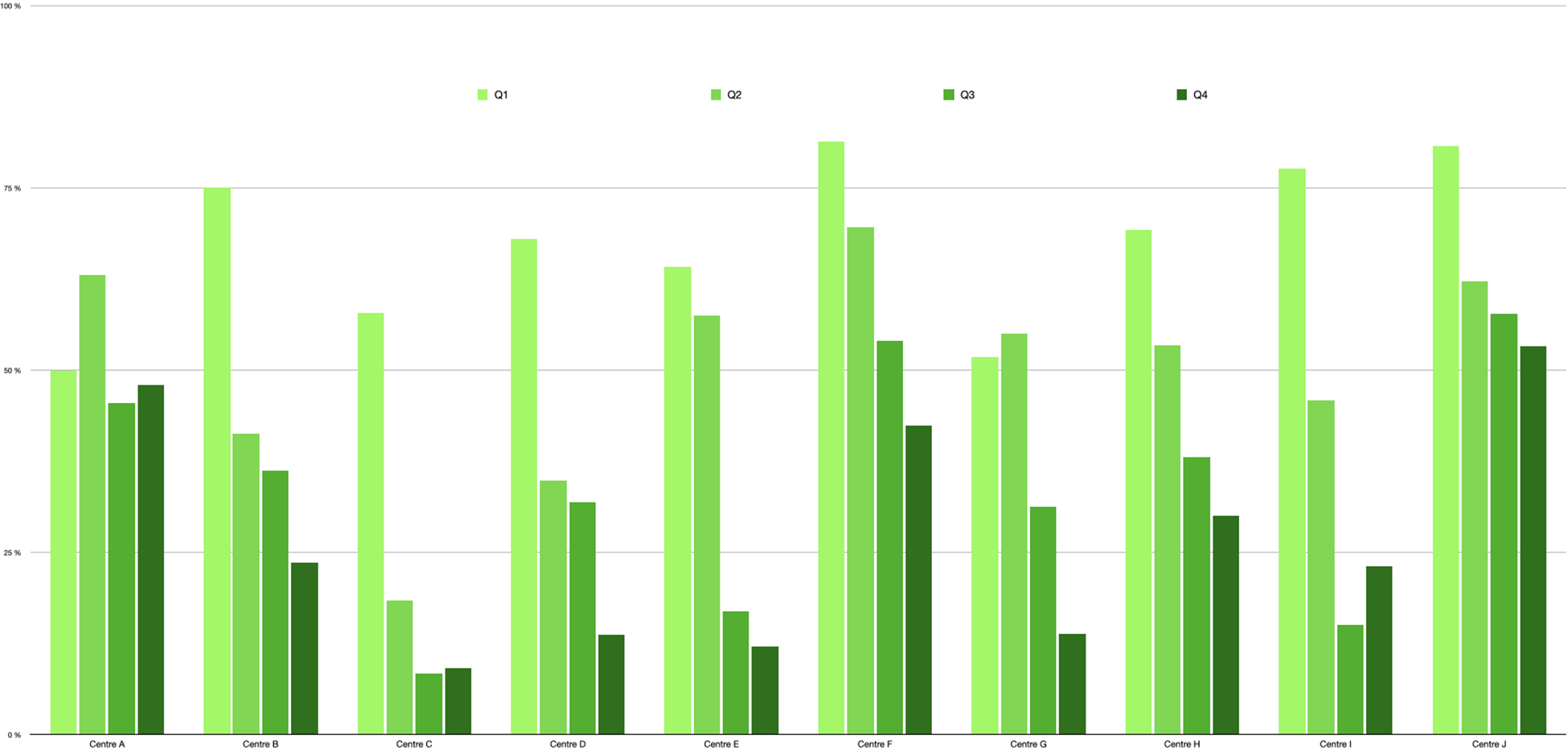
Proportion of mechanical valve for patients operated on for SAVR between 50 and 60 years-old per centre (sample) and per quartile during study time (2007–2022). Patients operated on between 01/01/2007 and 24/10/2011 (Q1); between 24/10/2011 and 02/07/2015 (Q2); between 02/07/2015 and 29/01/2019 (Q3) and between 29/01/2019 and 31/12/2022 (Q4).
In hospital outcomes
Per operative and in-hospital outcome data according to the type of SAVR are summarized in Table 2 and main outcomes regarding type of SAVR in the class of age 50–60 years-old are presented in Table 3. As a result of being significantly younger with less co-morbidity, early mortality was significantly lower in patients receiving a MPV as predicted by preoperative evaluation with the EuroSCORE II risk-scale. However, observed early mortality was below the one that was predicted by the EuroSCORE II for both type of valvular prosthesis and especially for patients between 50 and 60 years-old for which early outcomes were comparable with either type of SAVR in terms of early mortality and major morbidity. Pericardial revisions for tamponade were significantly more frequent after SAVR with a MPV, however excessive bleedings requiring heterologous blood transfusions were more frequent after SAVR with a BPV. Major thromboembolic complications were equally rare after SAVR no matter the type of valvular prosthesis, permanent strokes were however significantly more frequent in elderly patients. Mean postoperative length of stay was not significantly different though the standard deviations were too wide to allow for any conclusion.
Table 2
| Mechanical valves n = 8,909 | Biological valves n = 63,466 | p | |
|---|---|---|---|
| Previous Surgery One, No. (%; 95% CI) | 1,062 (11.9; 11.2–12.6) | 4,260 (6,7; 6.5–6.9) | <0.0001 |
| Two or More, No. (%; 95% CI) | 112 (1.2; 1–1.5) | 212 (0.33: 0.29–0.28) | <0.0001 |
| Index Surgery Elective, No. (%; 95% CI) | 7,978 (89.5; 87.6–91.5) | 55,911 (88.1; 87.3–88.8) | 0.17 |
| Urgent, No. (%; 95% CI) | 673 (7.5; 6.9–8.1) | 5,482 (8.6; 8.4–8.8) | 0.001 |
| Emergent, No. (%; 95% CI) | 187 (2.1; 1.8–2.4) | 1,421 (2.2; 2.1–2.3) | 0.4 |
| Associated Procedure CABG, No. (%; 95% CI) | 1,368 (15.4; 14.5–16.2) | 14,253 (22.5; 22.1–22.8) | <0.0001 |
| Mitral, No. (%; 95% CI) | 1,355 (15.2; 14.4–16) | 3,929 (6.2; 6–6.3) | <0.0001 |
| Tricuspid, No. (%; 95% CI) | 407 (4.6; 4.1–5) | 1,432 (2.2; 2.1–2.3) | <0.0001 |
| ECC duration, mean. (SD) | 99 (54) | 91 (47) | <0.0001 |
| Aortic Cross Clamp Time, mean. (SD) | 75 (38) | 69 (33) | <0.0001 |
| Permanent Stroke, No. (%; 95% CI) | 44 (0.5; 0.3–0.6) | 380 (0.6; 0.5–0.7) | 0.23 |
| Myocardial infarction, No. (%; 95% CI) | 40 (0.4; 0.3–0.6) | 199 (0.3; 0.2–0.4) | 0.04 |
| Excessive bleeding, No. (%; 95% CI) | 364 (4; 3.6–4.5) | 3,617 (5.7; 5.5–5.9) | <0.0001 |
| Tamponnade, No. (%; 95% CI) | 294 (3.3; 2.9–3.7) | 1,494 (2.3; 2.2–2.5) | <0.0001 |
| Post operative AF, No. (%; 95% CI) | 427 (4.8; 4.3–5.3) | 5,245 (8.2; 8–8.5) | <0.0001 |
| Pace-Maker, No. (%; 95% CI) | 263 (2.9; 2.6–3.3) | 2,284 (3.6; 3.4–3.7 | 0.0008 |
| Para-valvular leak >2, No. (%; 95% CI) | 63 (0.7; 0.5–0.9) | 684 (1; 0.9–1.1) | 0.007 |
| Postop. length of stay, mean. (SD) | 15.8 (8.7) | 15.8 (8.6) | 1 |
| In-hospital mortality, No. (%; 95% CI) | 181 (2; 1.7–2.3) | 1,512 (2.4; 2.3–2.5) | 0.04 |
| Observed/expected mortality | 0.72 | 0.6 | – |
Surgical characteristics and main in-hospital outcomes according to the type of prosthetic valve.
Table 3
| Mechanical 3,032 | Biological 2,914 | Total 5,946 | p | |
|---|---|---|---|---|
| Permanent Stroke, No. (%) | 15 (0.5) | 21 (0.7) | 36 | 0.26 |
| Myocardial infarction, No. (%) | 12 (0.4) | 6 (0.2) | 18 | 0.18 |
| Excessive bleeding, No. (%) | 135 (4.4) | 211 (7.2) | 346 | <0.001 |
| Tamponnade, No. (%) | 101 (3.3) | 83 (2.8) | 184 | 0.28 |
| Post operative AF, No. (%) | 161 (5.3) | 193 (6.6) | 354 | 0.03 |
| Pace-Maker, No. (%) | 79 (2.6) | 64 (2.1) | 143 | 0.3 |
| Para-valvular leak >2, No. (%) | 26 (0.8) | 54 (1.8) | 80 | 0.0009 |
| In-hospital mortality, No. (%) | 41 (1.3) | 53 (1.8) | 94 | 0.14 |
| Observed/expected mortality | 0.68 | 0.61 | 0.61 | – |
Main in-hospital outcomes according to the type of valve for patients between 50 and 60 years-old.
Discussion
Our study reveals a pronounced tendency towards implanting much more BPVs than MPVs during the last 15 years for SAVR in a large French multi centric population of patients. This was expected with regards of our population's age characteristics which match with demography of Western countries. Considering that 75% of patients were over 65-years old, this tendency is in line with both ESC and AHA-ACC recommendations (5, 7). Because, the durability of most BPVs exceeds life expectancy after 65 years-old (1), redo-valve surgery in elderly are generally due to non-structural prosthetic valve dysfunctions or endocarditis (11). However surgeons should be aware that, especially with patients who have more than 10 years of life expectancy, the risk of tissue valve degeneration should be minimized, and that the possibility of a future ViV TAVR should be planed during the first operation (12). At least for such patients, surgeons should therefore choose a BPV for which the long-term durability is well documented and should implant a valve with a diameter at least 23 mm (13), preferably avoiding those prostheses with an inner stent (14). Those general considerations might be even more crucial in patients under 50-years-old, 38% of which received a BPV for SAVR, a percentage stable enough throughout the time of our study.
Most importantly, we found that BPVs recently tended to be preferred over MPVs in patients between 50 and 60 years-old, a trend which is not observed to this extent in some other western countries (15). Added to patients aged from 60 to 65 years-old, they represent the so called middle-aged patients which represent a significant proportion (20%) of the overall population included in our study. In those middle age patients biological SAVR were predominantly implanted. Presumably, beside usual contra-indications to long-term anticoagulant therapy, this reflects an evolution in patient's personal choice. It is certainly also supported by the informations given to the patient by physicians. Those informations are generally based on the notions that, (i) for middle-aged patients, life expectancy post SAVR is not influenced by the type of valvular prosthesis (16), (ii) the quality of life for middle-aged patients is improved with BPV by avoiding life-long anticoagulant therapy and (iii) even though the durability of the biological prosthesis could not be extended despite promising advances, there is an on-going evidence that a degenerated valve could be treated either with a low-risk redo surgery or with a ViV-TAVR.
It is debatable that this given information reflects evidences from the most recent literature. Looking at the hard end-point of late mortality, a recent large hazard ratio meta-analysis including 16,876 patients found a higher late mortality after SAVR with BPVs (hazard ratio: 1.22, 95% CI: 1.00–1.49) for patients younger than 70 years of age (17). Table 4 resumes the most important findings regarding mortality and morbidity outcomes of SAVR with both types of valves in recent comparative large series and totalizing 11,376 middle-aged patients (16, 19–21). Another recent meta-analysis (22) focussing on the risk of prosthetic endocarditis and including 43,941 found that the risk of secondary endocarditis was significantly higher with BPVs than with MPVs. Therefore to ensure that an accurate information has been delivered, the fact that their choice to receive a biological SAVR might result into a reduced life expectancy and a higher risk of endocarditis should not be hidden to middle-aged patients.
Table 4
| Study | n* | Matching | Follow-up | Death | Stroke | Major bleeding | Redo surgery |
|---|---|---|---|---|---|---|---|
| Chiang (2014) (16) | 2,002 | Propensity scoring | 15 years | 0.97 (0.74) | 1.04 (0.84) | 1.75 (0.001) | 0.52 (0.001) |
| Glaser (2016) (18) | 2,002 | Propensity scoring | 15 years | 0.71 (0.006) | 1.04 (0.84) | 2.04 (<0.001) | 0.42 (0.001) |
| Goldstone (2017) (19) | 3,608 | Inverse probability | 15 years | 0.81 (0.03) | (<0.05)** | (<0.05)** | – |
| Kytö (2020) (20) | 1,152 | Propensity scoring | 10 years | 0.72 (0.03) | 1.29 (0.15) | 1.19 (0.4) | 0.3 (0.009) |
| Traxler (2022) (21) | 2,612 | None*** | 10 years | 0.59 (<0.001) | 1.04 (0.82) | – | 0.3 (0.005) |
Hazard ratio (p-value) of main outcomes after SAVR with MPVs versus BPVs in most recent comparative large studies targeting at middle aged patients.
Number of middle age patients included in the study, HR refer to this sub-population.
HR is not indicated but a higher significant risk is mentioned.
Multivariable Cox regression.
Besides, considering tissue valve failure, physicians should be aware of a possible subsequent valve re-replacement when index surgery is performed before 60 years-old. This eventuality is easy to conceive since life expectancy then exceeds BPVs' durability (11). More, the procedural risk associated with aortic valve surgical re-replacement remains consistent in state or nation-wide registries (16, 20, 11, 23) and cardiac reoperations in octogenarians have a bad prognosis (24). A nation-wide study from France has shown a lower early mortality with ViV-TAVR as compared to re-SAVR (25). This reduced short-term mortality has been confirmed by a recent meta-analysis (26) but this latter also found no differences between ViV-TAVR and re-SAVR in all-cause and cardiovascular mortality at midterm follow-up. Therefore, as for the final assessment of durability for the newest BPVs in non-elderly patients, we still have to wait to know how the widespread use of ViV-TAVR may positively impact the prospects for biological-SAVR in the middle-age population.
Considering the growing evidence that MPVs might confer a survival advantage in middle-aged patients requiring SAVR, it has to be acknowledged that, despite the observed practice in France, present time is too soon to plea for an extensive use of biological SAVR in patients under 60 years-old. This is in phase with the reappraisal of MPVs use that is observed in the latest evolution of the STS database (27). Despite the ongoing research of an ideal valve that would combine a durability over two-decades and a total freedom from long-term anti-coagulant therapy, and while waiting for late results after the Ozaki technique (28), extending indications of aortic valve repair or Ross procedure towards 50–60 years-old very selected patients might represent a valid option.
Limitations
Our survey was restricted to a list of solicited centres which actively participate to the EPICARD national database and which volunteered to participate. The survey was closed when the number of 100,000 patients receiving heart valve surgery was obtained. Therefore it might be that a true nation-wide study including all French centres would have shown slightly different results, though it is unlikely that the tendency towards BPVs in middle-aged and young patients requiring a SAVR would have changed much. The EPICARD database is purely declarative and it might be that bad outcomes after surgery were under-reported. Items of the database include data from follow-up, however too much missing data made us unable to report on long term results. Therefore extrapolating from literature is the only option to anticipate what will be the consequences on late survival of middle-aged patients operated-on with the standards of actual practice. Finally the interpretation of the results and the considerations elaborated in the discussion engage the only responsibility of the authors and do not reflect personal opinion of the numerous surgeons who performed SAVRs included in this survey.
Conclusions
In a large contemporary French patient population, real world practice showed a recent shift towards a lower age-threshold for biological SAVR as compared to what would suggest contemporary guidelines. For those young and middle aged patients who prefer to avoid long term vitamin K antagonists with the hope to return to a normal live, evidences that MPVs in aortic position might confer a survival advantage should be explicitly discussed to give the patient an up-to-date evidence based information as required by contemporary guidelines (5, 6).
Statements
Author’s note
This paper has been presented at the ESC Congress 2023, Amsterdam.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The dataset is the property of the French Society of Thoracic and Cardiovascular Surgery. Requests to access these datasets should be directed to Mme Valérie LEBORGNE, valerie.leborgne@specialitesmedicales.org.
Author contributions
TC: conceptualization, data curation, formal analysis, methodology, writing—original draft, and writing—reviewing and editing. YC: data curation, methodology, writing—original draft, and writing—reviewing and editing. JN: data curation, formal analysis, methodology,—reviewing and editing. JF and JD: EPICARD database supervisors, data extraction and quality control—reviewing and editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Member of the EpiCard investigators
Collaborators: EpiCard investigators participating to the Carbon-Free Survey: Paul Achouh, MD, HEGP University-Hospital, Paris, France; Christophe Baufreton, MD, PhD, University Hospital of Angers, Angers, France; Eric Bezon, MD, PhD, Brest University Hospital, Brest, France; Olivier Bouchot, MD, PhD, Dijon University Hospital, Dijon, France; Thierry Bourguignon, MD, PhD, Hôpital Trousseau, Tours, France; Lionel Camilleri, MD, PhD, Clermont-Ferrand Universitary Hospital, Clermont-Ferrand, France; Thierry Caus, MD, PhD, University Hospital of Amiens, Amiens, France; Nicolas Chavanis, MD, Centre Hospitalier Annecy Genevois, Annecy, France; Frédéric Collart, Timone's Hospital, Marseille France; Pierre Corbi, MD, PhD, University Hospital of Poitiers, Poitiers, France; Alain Curtil, MD, Clinique de la Sauvegarde, Lyon, France; Jean Louis De Brux, MD, PhD, Angers University Hospital, Angers, France; Roland Demaria, MD, PhD, Montpellier University Hospital, Montpellier, France; François Bouchard, MD, Rouen University Hospital, Rouen, France; Jean-Marc Frapier, MD, PhD (in memory of), Montpellier University Hospital, Montpellier, France; Jean-Philippe Frieh, MD, Clinique du Tonkin, Villeurbanne, France; Louis Labrousse, MD, PhD, Hôpital du Haut Levêque, Bordeaux, France; Pascal Leprince, MD, PhD, Pitie-Salpétrière Hospital and Sorbonne University, Paris, France; Bertrand Marcheix, MD, PhD, Hôpital de Rangeuil, University Hospital of Toulouse, Toulouse, France; Jean Philippe Mazzucotelli, MD, PhD, Hôpitaux Universitaires de Strasbourg, Strasbourg, Joseph Nader, MD, PhD, Clinique du Millénaire, Montpellier, France; Jean-Christian Roussel, MD, PhD, Nord Laennec University Hospital, Nantes, France; Vito Giovanni Ruggieri, MD, PhD, Reims University Hospital, Reims, France; Michel Tapia, Institut Arnault Tzanck, Saint Laurent du Var, France; Jean-Philippe Verhoye, MD, PhD, Rennes University Hospital, Rennes, France; Andre Vincentelli, MD, PhD, University Hospital of Lille, Lille, France.
References
1.
FatimaBMohananeyDKhanFWJobanputraYTummalaRBanerjeeKet alDurability data for bioprosthetic surgical aortic valve: a systematic review. JAMA Cardiol. (2019) 4(1):71–80. 10.1001/jamacardio.2018.4045
2.
EikelboomJWConnollySJBrueckmannMGrangerGBKappeteinAPMackMJet alDabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. (2013) 369(13):1206–14. 10.1056/NEJMoa1300615
3.
GerdischMWSathyamoorthyMMichelenaHI. The role of mechanical valves in the aortic position in the era of bioprostheses and TAVR: evidence-based appraisal and focus on the on-X valve. Prog Cardiovasc Dis. (2022) 72:31–40. 10.1016/j.pcad.2022.06.001
4.
OkamotoYYamamotoKYoshiiS. Early and late outcomes of aortic valve replacement using bioprosthetic versus mechanical valve in elderly patients: a propensity analysis. J Card Surg. (2016) 31(4):192–202. 10.1111/jocs.12719
5.
VahanianABeyersdorfFPrazFMilojevicMBladesSBauersachsJet al2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. (2021) 60(4):727–800. 10.1093/ejcts/ezab389
6.
OttoCMNishimuraRABonowROCarabelloBAErwindJPGentileFet al2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. J Thorac Cardiovasc Surg. (2020) 162(2):e183–353. 10.1016/j.jtcvs.2021.04.002
7.
InancIHCilingirogluMIliescuCNlniosVMatarFAtesIet alComparison of American and European guidelines for the management of patients with valvular heart disease. Cardiovasc Revasc Med. (2022) 47:76–85.
8.
SchnittmanSRAdamsDHItagakiS. Bioprosthetic aortic valve replacement: revisiting prosthesis choice in patients younger than 50 years old. J Thorac Cardiovasc Surg. (2018) 155(2):539–47.e9. 10.1016/j.jtcvs.2017.08.121
9.
NelsonJSMaulTMWeardenPDNajmHKBalogluOJohnstonDRet alAortic valve replacement in young and middle-aged adults: current and potential roles of TAVR. Ann Thorac Surg. (2021) 112(1):132–8. 10.1016/j.athoracsur.2020.05.180
10.
LeonMBSmithCRMackMJMakkarRRSvenssonLGKodaliSKet alTranscatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. (2016) 374:1609–20. 10.1056/NEJMoa1514616
11.
BourguignonTBouquiaux-StabloALCandolfiPMirzaALordCMayMAet alVery long-term outcomes of the carpentier-edwards perimount valve in aortic position. Ann Thorac Surg. (2015) 99(3):831–7. 10.1016/j.athoracsur.2014.09.030
12.
AttiasDNejjariMNappiFDreyfusJEleidMFRihalCS. How to treat severe symptomatic valve deterioration of aortic surgical bioprosthesis; trans catheter valve-in-valve implantation or redo valve surgery?Eur J Cardiothorac Surg. (2018) 54:977–85. 10.1093/ejcts/ezy204
13.
MartinCSunW?. Transcatheter valve under expansion limits leaflet durability: implications for valve-in-valve procedures. Ann Biomed Eng. (2017) 45(2):394–404. 10.1007/s10439-016-1738-8
14.
BernadiFLMDvirDRodes-CabauJRibeiroHB. Valve-in-valve challenges: how to avoid coronary obstruction. Front Cardiovas Med. (2019) 6:120. 10.3389/fcvm.2019.00120
15.
ChanJDimagliAFuduluDPSinceSNarayanPDongTet alTrend and early outcomes in isolated surgical aortic valve replacement in the United Kingdom. Front Cardiovasc Med. (2023) 9:1077279. 10.3389/fcvm.2022.1077279
16.
ChiangYPChikweJMoskowitzAItagakiSAdamsDHEgorovaNN. Survival and long term outcomes following bioprosthetic vs mechanical aortic valve replacement in patients aged 50–69 years. JAMA. (2014) 312(13):1323–29. 10.1001/jama.2014.12679
17.
LevinerDBWitbergGLeviALandesUSchwartzNShiranet alMechanical vs bioprosthetic aortic valve replacement in patients younger than 70 years of age: a hazard ratio meta-analysis. Can J Cardiol. (2022) 38(3):355–64. 10.1016/j.cjca.2021.12.008
18.
GlaserNJacksonVHolzmannMJCerecedaAFSatrapyU. Aortic valve replacement with mechanical vs. Biological prostheses in patients aged 50–69 years. Eur Heart J. (2016) 37:2658–67. 10.1093/eurheartj/ehv580
19.
GoldstoneABChiuPBaiocchiMLingalaBPatrickWLFischbeinMPet alMechanical or biologic prostheses for aortic-valve and mitral-valve replacement. N Engl J Med. (2017) 377(19):1847–57. 10.1056/NEJMoa1613792
20.
KytöVSipiläJAhtelaERautavaPGunnJ. Mechanical versus biologic prostheses for surgical aortic valve replacement in patients aged 50 to 70. Ann Thorac Surg. (2020) 110(1):102–10. 10.1016/j.athoracsur.2019.10.027
21.
TraxlerDKrotkaPLaggnerMMildnerMGrafAReichardtBet alMechanical aortic valve prostheses offer a better survival benefit in 50-65 year olds: aUTHEARTVISIT study. Eur J Clin Invest. (2022) 52:e13736. 10.1111/eci.13736
22.
Anantha-NarayananMReddyYNSundaramVMurradMHERrwinPJBaddourLMet alEndocarditis risk with bioprosthetic and mechanical valves: systematic review and meta-analysis. Heart. (2020) 106(18):1413–9. 10.1136/heartjnl-2020-316718
23.
KanekoTVassilevaCMEnglumBKimSYammineMBrennanMet alContemporary outcomes of repeat aortic valve replacement: a benchmark for transcatheter valve-in-valve procedures. Ann Thorac Surg. (2015) 100(4):1298–304. 10.1016/j.athoracsur.2015.04.062
24.
DeschkaHMachnerMWelpHDell’AquilaAMErlerSWimmer-GreineckerG. Cardiac reoperations in octogenarians: do they really benefit?Geriat Gerontol Int. (2016) 16(10):1138–44. 10.1111/ggi.12609
25.
DeharoPBissonAHerbetJLacourTSaint EtienneCPortoAet alTranscatheter valve-in-valve aortic valve replacement as an alternative to surgical re-replacement. JACC. (2020) 76:489–99. 10.1016/j.jacc.2020.06.010
26.
BrunoFEliaED’AscenzoFMarengoGDeharoPKanekoTet alValve-in-valve transcatheter aortic valve replacement or re-surgical aortic valve replacement in degenerated bioprostheses: a systematic review and meta-analysis of short and midterm results. Catheter Cardiovasc Interv. (2022) 100:122–30. 10.1002/ccd.30219
27.
KimKMArghamiAHabibRDaneshmandMAParsonsNElhalabiZet alThe society of thoracic surgeons adult cardiac surgery database: 2022 update on outcomes and research. Ann Thorac Surg. (2023) 115(3):566–74. 10.1016/j.athoracsur.2022.12.033
28.
MylonasKSTasoudisPTPavlopoulosDKanakisMStravridisGTAvgerinosDV. Aortic valve neocuspidization using the ozaki technique: a meta-analysis of reconstructed patient-level data. Am Heart J. (2023) 255:1–11. 10.1016/j.ahj.2022.09.003
Summary
Keywords
aortic valve, surgical aortic replacement, mechanical and biological prosthetic valves, trend, database, France, bioprosthesis, mechanical prosthesis
Citation
Caus T, Chabry Y, Nader J, Fusellier JF, De Brux JL and for the EpiCard investigators (2023) Trends in SAVR with biological vs. mechanical valves in middle-aged patients: results from a French large multi-centric survey. Front. Cardiovasc. Med. 10:1205770. doi: 10.3389/fcvm.2023.1205770
Received
14 April 2023
Accepted
16 June 2023
Published
28 August 2023
Volume
10 - 2023
Edited by
Stephanie Sellers, University of British Columbia, Canada
Reviewed by
Takashi Kakuta, National Cerebral and Cardiovascular Center, Japan Michael Seidman, University Health Network (UHN), Canada
Updates
Copyright
© 2023 Caus, Chabry, Nader, Fusellier, De Brux and for the EpiCard investigators.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thierry Caus caus.thierry@chu-amiens.fr
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.