- West China School of Nursing, West China Hospital, Sichuan University, Chengdu, China
Background: Inflammation has been linked to the development of coronary heart disease (CHD). The systemic immune inflammation index (SII) is a useful biomarker of systemic inflammation. Our study aimed to explore the correlation between SII and CHD.
Methods: We conducted a multivariate logistic regression analysis, smoothing curve fitting, and segmented model comparison on 15,905 participants with a CHD prevalence of 3.31% and a mean age of 46.97 years.
Results: Adjusting for gender, age, and race, we found a negative association between SII and CHD [odds ratio (OR) 0.66; 95% confidence interval (CI) 0.48, 0.90]. There was an inverse trend where increasing SII was associated with decreasing odds of CHD (p for trend = 0.0017). After further adjustment, the association was strengthened, with a similar trend (p for trend = 0.0639). Smoothing curve fitting demonstrated a gender-specific association between SII and CHD.
Conclusions: Our findings suggest that higher SII values may be associated with a higher incidence of CHD, which varies by gender. SII may be a cost-effective and convenient method to detect CHD. Further studies are needed to confirm the causality of these findings in a larger prospective cohort.
1. Introduction
Coronary artery disease is a common heart disease and a leading cause of morbidity and mortality worldwide (1, 2). It causes approximately 1.78 million European and 360,000 American deaths each year (3). Coronary heart disease is a major cause of morbidity in developed countries and a major driver of healthcare-related costs (4). Coronary heart disease (CHD) accounts for 27% of Europe's total cost of cardiovascular disease (CVD). Patients with CHD often suffer from or even die from cardiovascular events, such as heart failure, stroke, myocardial infarction, and cerebral thrombosis (2). And in the United States, one in six deaths is due to coronary heart disease (4).
The pathological process of coronary heart disease includes atherosclerosis (the main cause) and spasm of the coronary arteries. Lipid metabolic disease, Endothelium damage, inflammation, and immune dysfunction can promote the occurrence and development of coronary atherosclerosis, which leads to CHD (3). Vulnerable plaque is easy to rupture, instability, and easy to forms thrombus plaque. Inflammation plays an important role in vulnerable plaque formation and plaque rupture, which can trigger the formation of blood clots and eventually lead to myocardial infarction (5).
The systemic immune-inflammation index (SII), a novel comprehensive inflammatory biomarker based on neutrophil, lymphocyte, and platelet counts (in 109 cells/L) (6), was created in 2014 by Hu et al., to reflect local immune responses and systemic inflammation (7). Inflammation plays a key role in the occurrence and development of coronary heart disease (CHD) (5). Studies have shown that SII is associated with a poor prognosis of coronary heart disease (CHD) (8). SII can also predict the survival of patients with a variety of tumor prognoses, screening and identification of high-risk patients have applied value (9–11). SII, as an off-the-shelf prognostic biomarker, can help clinicians rapidly identify high-risk patients and make better medical decisions in clinical practice. We hypothesized that SII is a predictor of coronary heart disease risk (12). We conducted the current study to investigate the association between SII and coronary heart disease.
2. Materials and methods
2.1. Data sources
Data were obtained from NHANES, a national population-based cross-sectional survey evaluated by the National Center for Health Statistics (NCHS) to collect information on potential health risk factors and nutritional status of non-institutionalized civilians in the United States. It uses a complex multistage probabilistic design to recruit a representative sample of the entire U.S. population (13–16). The protocol for the NHANES study was approved by the NCHS Research Ethics Review Committee and written informed consent was obtained from all survey participants. Participants completed a household interview to provide demographic, socioeconomic, and health-related information. Participants underwent a physical examination and laboratory tests at a mobile examination center (MEC) to assess their medical and physiological status. All detailed NHANES study designs and data are publicly available at https://www.cdc.gov/nchs/nhanes/. This study followed the reporting guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) cross-sectional study.
2.2. Study population
Our study combined five NHANES cycles (2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017–2018) and included the complete set of variables, recruiting a total of 49,693 participants, with exclusion criteria for subjects in our analysis being (1) missing data for SII (2), missing data for coronary artery disease, and (3) missing covariate data. A total of 15,905 participants were initially recruited; after excluding missing SII (n = 8,805), missing coronary heart disease (n = 14,527), and missing covariates (n = 10,456), 15,905 eligible participants ≥20 years of age were included in our final analysis (Figure 1).
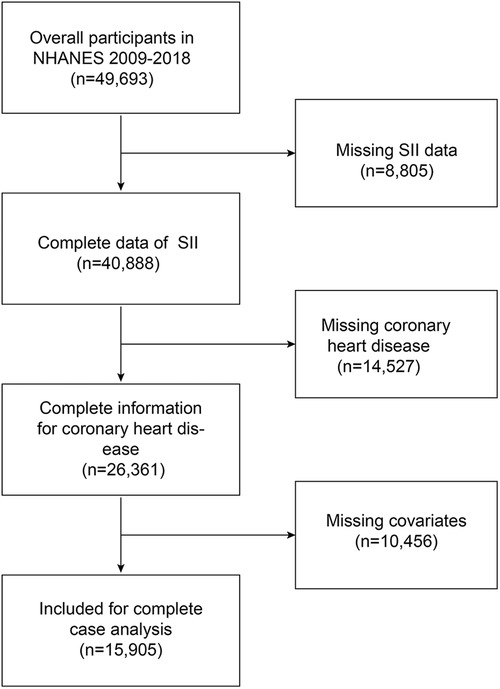
Figure 1. Overview of participants screening. NHANES, National Health, and Nutrition Examination Survey; SII, systemic immune-inflammation index. Definition and grouping of systemic immune-inflammation index (SII) and coronary artery disease (CHD).
2.3. Definition of systemic immune-inflammation index
The definition of SII is as follows: SII = P × N/L, where P, N, and L are peripheral platelet, neutrophil, and lymphocyte counts, respectively (7). In our analysis, SII was designed as an exposure variable.
2.4. Definition of coronary heart disease
In the health questionnaire, participants were asked “Ever told you had coronary heart disease” (3, 17), and if the answer was “yes”, the individual was considered to have coronary heart disease.
According to previous studies, participants were equally divided into four groups according to the SII distribution: low SII (Q1, <317.5), low-moderate SII (Q2, 317.5–445.7), intermediate SII (Q3, 445.7–625.1) and high SII (Q4, >625.7).
2.5. Covariates
Demographic parameters included gender (male/female), age (years), race (Mexican American/Other Hispanic/Non-Hispanic White/Non-Hispanic Black/Other race), marital status (with/without a partner), an education level (above/below high school), smoking (smoker/non-smoker), alcohol consumption (less/more than 15 drinks in the past year), BMI (normal/overweight/obese), household income to poverty ratio (PIR) (18, 19), total cholesterol, triglycerides, total protein, albumin, globulin, serum glucose, serum calcium, and leukocyte platelet, neutrophil, lymphocyte, and monocyte counts were included in the biochemical profile. The NLR is the ratio of neutrophils to lymphocytes. Health risk factors including angina and hypertension were recorded as “yes/no” (20–22).
2.6. Statistical analysis
All statistical analyses were conducted according to Centers for Disease Control and Prevention (CDC) guidelines, and an appropriate NHANES sampling all statistical analyses were conducted according to Centers for Disease Control and Prevention (CDC) guidelines and an appropriate NHANES sampling weight was applied, and accounted for complex multistage cluster survey design in the analysis.
Means ± standard errors (SE) were used to describe the distribution of sample means for continuous variables, and frequencies (percentages) were used for categorical variables. To explore the relationship between SII and coronary heart disease (CHD), multivariate logistic regression analysis was performed in three different models considering NHANES complex sampling design (sampling weight). In Model 1, the covariates were not adjusted. Model 2 was minimally adjusted for gender, age, and race. Model 3 was adjusted for age, gender, race, marital status, education level, smoking, BMI, household income-to-poverty ratio (PIR), total cholesterol, triglyceride, total protein, albumin, globulin, serum glucose, serum calcium, and white blood cell platelet, neutrophil, lymphocyte, and monocyte count. In addition, we performed subgroup analyses. All continuous covariates were converted to categorical variables and interaction effects were assessed by likelihood ratio tests. At the same time, we also used smoothed curve fitting to detect non-linearity between SII and coronary artery disease, segmented model comparison to find inflection points, and further explore their threshold effects. Forest plots show each model's hazard ratios and 95% confidence intervals of covariates.
All analyses were performed utilizing R software version 4.1 (http://www.R-project.org; The R Foundation) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc.). p < 0.05 (two-sided) was set for a significant difference.
3. Results
3.1. Baseline characteristics of the population stratified by SII
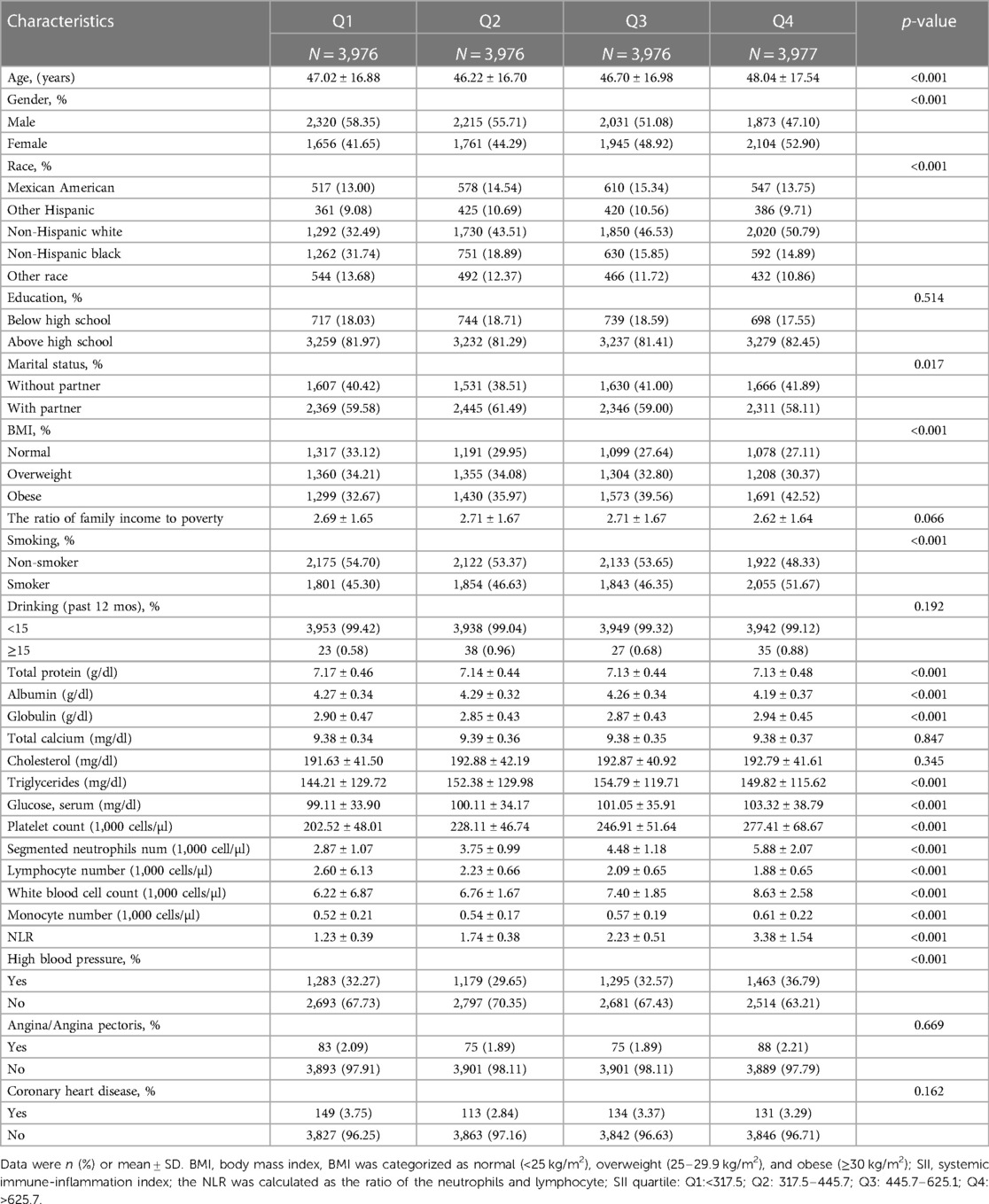
This study analyzed data from 15,905 participants with a mean age of 46.97 years ± 17.04 years and a CHD prevalence of 3.31%. The study population was categorized into Qs (Q1–Q4) based on their SII levels. The Qs were found to have significant differences in age, gender, race, marital status, BMI, smoking, total protein, albumin, globulin, triglycerides, and glucose levels (p < 0.05), while there were no significant differences in education level, the ratio of family income to poverty, drinking, total calcium, and cholesterol levels among the Qs (Table 1).
3.2. Relationship between SII and coronary heart disease
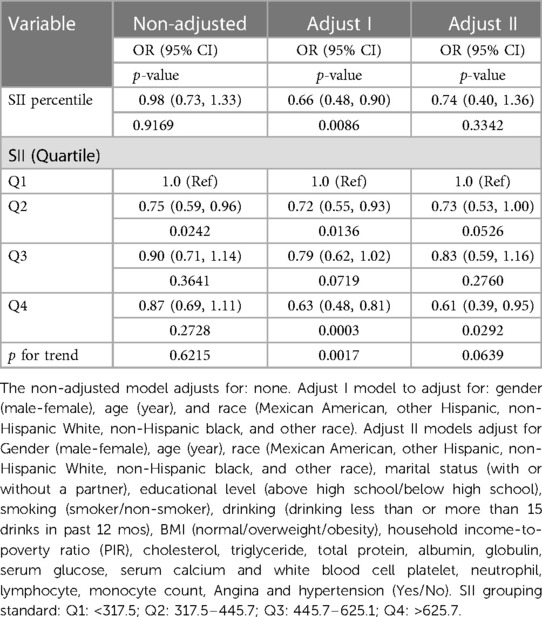
To better quantify the effect size, we multiplied the SII by 100 (SII percentile) (Table 2). At first, we found no significant association between the SII percentile and CHD (OR 0.98, 95% CI: 0.73, 1.33, p = 0.9169) in the non-adjusted model. However, after adjusting for gender, age, and race in the adjusted model I, the association became significant (OR 0.66, 95% CI: 0.48, 0.90, p = 0.0086), indicating that higher SII percentiles were associated with lower odds of CHD, and this association showed a trend of decreasing odds of CHD with increasing SII percentile (p for trend = 0.0017). Further adjustment for additional variables in adjusted model II strengthened the association, with an OR of 0.74 (95% CI: 0.40, 1.36) and a trend showing decreasing odds of CHD with increasing SII percentile (p for trend = 0.0639). The OR for SII Qs also showed a significant trend in Adjusted models I and II, with Q2 showing a lower OR than Q1, and Q4 showing a significantly lower OR than Q1. However, the OR for Q3 was not significantly different from that for Q1. These findings suggest that higher SII values may be associated with a higher incidence of CHD (see Table 2).
3.3. Subgroup analysis
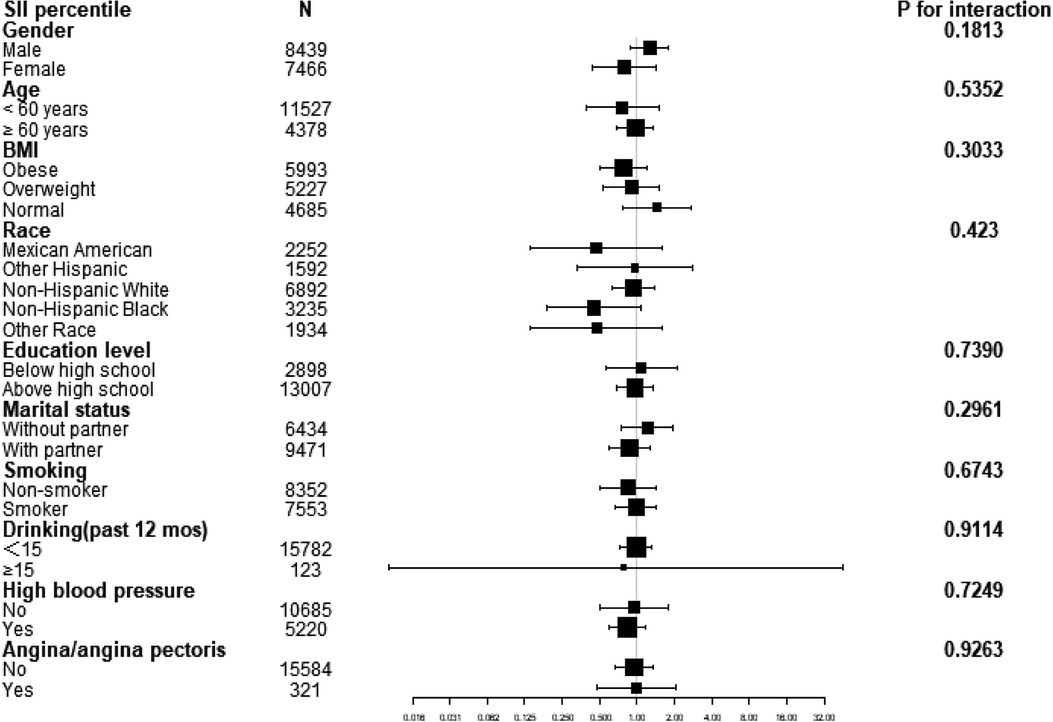
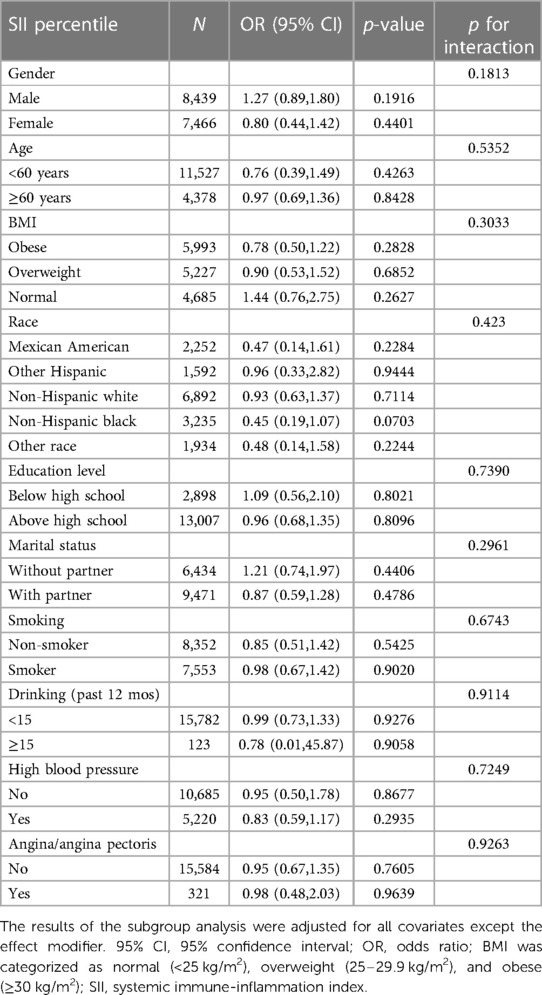
A subgroup analysis was conducted to investigate the association between the SII percentile and CHD across various demographic and clinical characteristics, as shown in Figure 2. The subgroups included gender, age, BMI, race, education level, marital status, smoking, drinking, high blood pressure, and angina/angina pectoris. The results of the subgroup analysis indicated no statistically significant associations between the SII percentile and CHD in any of the subgroups, with all p-values >0.05. However, it is worth noting that there is a suggestion of a positive association between the SII percentile and high blood pressure in the “yes” subgroup, as the odds ratio (OR) is less than 1 and the p-value is close to 0.05 (Table 3).
The smooth curve fitting analysis showed an inverted U-shaped relationship between SII and CHD risk in both genders, with a significant effect above the fold point (in Figure 3).
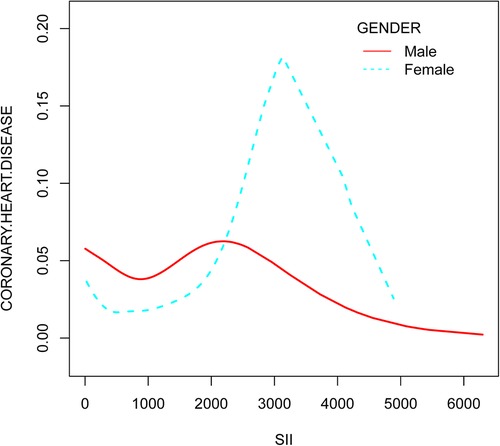
Figure 3. The relationship between systemic immune-inflammation index and coronary heart disease risk stratified by gender.
4. Discussion
This study analyzed data from the NHANES database for 2009–2018. In our cross-sectional study of 15,905 participants, a negative association between SII and coronary heart disease was observed across quartiles of SII, and smooth curve fitting shows the same result. Subgroup analyses and interaction tests showed that the association was similar across population settings.
In recent years, blood cell-based inflammatory parameters, including white blood cells, neutrophil, and neutrophil to lymphocyte ratios, have received increasing attention because they can predict some diseases, such as blunted rest-activity rhythm, psychiatry problems, and cardiovascular anomalies (6). Many studies have demonstrated that SII has a remarkable predictive ability (3, 6–9, 12, 22–29). Systemic immune inflammatory index (SII) was initially defined as the prognosis of cancer, intracerebral hemorrhage, and coronary artery stenosis (23). However, the relationship between SII itself and coronary heart disease has not been studied. SII measurements are based on standard laboratory methods of peripheral neutrophils, lymphocytes, and platelets in clinical practice. Simultaneously, SII was a widely available method with a non-intrusive methodology, simple accessibility, and low cost. The potential for therapeutic use is indeed positive (25). Arteriosclerosis is the basic mechanism of coronary heart disease. Abnormal apoptosis of Endothelium cells (VEC), macrophages, or vacs is a common feature of arteriosclerosis, leading to the formation or destabilization of arteriosclerosis plaques (1). Studies have shown that SII is associated with mortality of the cardiovascular system in patients (10, 11). Inflammation plays an important role in the formation and development of arteriosclerosis, and studies have found that they can serve as risk stratification markers and predict adverse events (30). Inflammation-endothelial dysfunction interaction triggers and promotes arteriosclerosis (5). Elevated inflammatory markers increase the risk of cardiovascular disease (CVD), but the underlying mechanisms and pathways remain to be elucidated (28). SII can reflect local immune response and systemic inflammatory response and is an important inflammatory marker. SII consists of three types of blood cells: platelets, neutrophils, and lymphocytes (30). Studies have shown that increased neutrophils can promote oxidative damage to blood vessel walls, while decreased lymphocytes can exacerbate oxidative and inflammatory damage (20, 30, 31). The neutrophil interacts with platelets to influence important biological processes related to arteriosclerosis, thrombosis, and ischemic attack. Following apoptosis of lymphocytes, the lipid core of atherosclerotic plaques ruptures and produces a thrombus (27).
Considering the Neyman bias (32), inherent in cross-sectional studies, our ability to ascertain the occurrence of a disease in individuals beyond the survey's time point is limited. We can only estimate disease prevalence based on the survey data, without definitive knowledge of past or future disease status. This constraint applies to our study as well.
Our study utilized NHANES data, benefiting from its reliable and well-designed cross-sectional framework. Notably, we employed a substantial sample size and conducted subgroup analyses to elucidate the distribution of SII in both coronary and non-coronary populations. Furthermore, our analyses included adjustments for relevant covariates, allowing us to explore potential confounding factors linked to coronary heart disease, encompassing sociodemographic and lifestyle variables. We employed various forms of independent variables, such as continuous and categorical variables, constructing robust multiple regression models to yield more reliable findings. Moreover, we applied smooth curve fitting to visually portray the interrelationships between variables in a more accessible manner. Nevertheless, it is imperative to acknowledge the limitations of our study. The cross-sectional design precludes establishing causal relationships, necessitating prospective investigations for causal determination. Additionally, the reliance on self-reported questionnaire data for coronary heart disease status and covariates introduces potential subjective biases. Furthermore, the measurement of immune cell counts was based on a single blood test, while a continuous monitoring approach would provide more reliable data considering the lifespan of blood cells. Notably, we should remain mindful of potential unobserved confounding factors, and further exploration of clinical conditions, such as diabetes, is warranted. Indeed, our study offers valuable insights that contribute to the current body of knowledge. Nonetheless, it is essential to carefully consider the limitations we have discussed when interpreting our findings. These limitations are crucial in providing a comprehensive understanding of the context and implications of our research.
In summary, our study suggests that SII may be a useful marker for predicting CHD risk, particularly in males and females above a certain SII level. However, further research is needed to confirm these findings and to determine the optimal SII level for predicting CHD risk in different genders.
5. Conclusion
To sum up, our findings add to the growing body of evidence supporting the clinical utility of SII as a predictive biomarker for disease outcomes. Future prospective studies are needed to establish causality and explore the potential clinical applications of SII in the prevention and treatment of coronary heart disease.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.cdc.gov/nchs/nhanes/.
Ethics statement
The study was conducted by the Declaration of Helsinki and was approved by the Institutional Review Board of the National Centre for Health Statistics. Informed consent was obtained from all subjects involved in the study.
Author contributions
JM conceptualized and designed the study, performed data curation and project administration, conducted the investigation and formal analysis, and wrote the original draft of the manuscript. KL contributed to the manuscript editing, manuscript review, and provided valuable input throughout the research process. All authors contributed to the article and approved the submitted version.
Funding
We received support from West China of Hospital, Sichuan University, grant number: ZYGD21006.
Acknowledgments
We appreciate the personnel at the National Health and Nutrition Examination Survey for planning, collecting, and compiling NHANES data and establishing the public database.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dong Y, Chen H, Gao J, Liu Y, Li J, Wang J. Molecular machinery and interplay of apoptosis and autophagy in coronary heart disease. J Mol Cell Cardiol. (2019) 136:27–41. doi: 10.1016/j.yjmcc.2019.09.001
2. Ma R, Gao J, Mao S, Wang Z. Association between heart rate and cardiovascular death in patients with coronary heart disease: a NHANES-based cohort study. Clinical Cardiol. (2022) 45(5):574–82. doi: 10.1002/clc.23818
3. Hou XZ, Liu EQ, Liu SQ, Lv H, Cui HF, Han J. The negative association between serum albumin levels and coronary heart disease risk in adults over 45 years old: a cross-sectional survey. Sci Rep. (2023) 13(1):672. doi: 10.1038/s41598-023-27974-w
4. DiNicolantonio JJ, Lucan SC, O'Keefe JH. The evidence for saturated fat and for sugar related to coronary heart disease. Prog Cardiovasc Dis. (2016) 58(5):464–72. doi: 10.1016/j.pcad.2015.11.006
5. Wu L, Shi Y, Kong C, Zhang J, Chen S. Dietary inflammatory index and its association with the prevalence of coronary heart disease among 45,306 US adults. Nutrients. (2022) 14(21):2. doi: 10.3390/nu14214553
6. You Y, Chen Y, Fang W, Li X, Wang R, Liu J, et al. The association between sedentary behavior, exercise, and sleep disturbance: a mediation analysis of inflammatory biomarkers. Front Immunol. (2022) 13:1080782. doi: 10.3389/fimmu.2022.1080782
7. Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. (2014) 20(23):6212–22. doi: 10.1158/1078-0432.Ccr-14-0442
8. Gur DO, Efe MM, Alpsoy S, Akyüz A, Uslu N, Çelikkol A, Gur O. Systemic immune-inflammatory index as a determinant of atherosclerotic burden and high-risk patients with acute coronary syndromes. Arq Bras Cardiol. (2022) 119(3):382–90. doi: 10.36660/abc.20210416.
9. Lei H, Xu S, Mao X, Chen X, Chen Y, Sun X, et al. Systemic immune-inflammatory index as a predictor of lymph node metastasis in endometrial cancer. J Inflamm Res. (2021) 14:7131–42. doi: 10.2147/jir.S345790
10. Demir M, Özbek M. A novel predictor in patients with coronary chronic total occlusion: systemic immune-inflammation index: a single-center cross-sectional study. Rev Assoc Med Bras. (2022) 68(5):579–85. doi: 10.1590/1806-9282.20211097
11. Karaçalılar M, Demir M. A novel predictor in patients undergoing heart valve surgery: systemic inflammation response index: a single center cross-sectional study. Eur Rev Med Pharmacol Sci. (2023) 27(3):1016–22. doi: 10.26355/eurrev_202302_31196
12. Peng Y, Huang W, Shi Z, Chen Y, Ma J. Positive association between systemic immune-inflammatory index and mortality of cardiogenic shock. Clin Chim Acta. (2020) 511:97–103. doi: 10.1016/j.cca.2020.09.022
13. Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, Hirsch R, Burt VL, Johnson CL. National health and nutrition examination survey: sample design, 2007-2010. Vital Health Stat 2. (2013) 160:1–23. PMID: 25569458.
14. Curtin LR, Mohadjer LK, Dohrmann SM, Montaquila JM, Kruszan-Moran D, Mirel LB, Carroll MD, Hirsch R, Schober S, Johnson CL. The national health and nutrition examination survey: sample design, 1999-2006. Vital Health Stat 2. (2012) 155:1–39. PMID: 25093338.
15. Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National health and nutrition examination survey: sample design, 2011-2014. Vital Health Stat 2. (2014) 162:1–33. doi: 10.1016/j.puhe.2012.05.028
16. Mirel LB, Mohadjer LK, Dohrmann SM, Clark J, Burt VL, Johnson CL, Curtin LR. National health and nutrition examination survey: estimation procedures, 2007-2010. Vital Health Stat 2. (2013) 159:1–17. doi: 10.3346/jkms.2012.27.3.243
17. Pollack CE, Slaughter ME, Griffin BA, Dubowitz T, Bird CE. Neighborhood socioeconomic status and coronary heart disease risk prediction in a nationally representative sample. Public Health. (2012) 126(10):827–35. doi: 10.1016/j.puhe.2012.05.028
18. Park YS, Kim JS. Obesity phenotype and coronary heart disease risk as estimated by the framingham risk score. J Korean Med Sci. (2012) 27(3):243–9. doi: 10.3346/jkms.2012.27.3.243
19. Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. (2021) 373:n604. doi: 10.1136/bmj.n604
20. Chen Y, Wang W, Zeng L, Mi K, Li N, Shi J, Yang S. Association between neutrophil-lymphocyte ratio and all-cause mortality and cause-specific mortality in US adults, 1999-2014. Int J Gen Med. (2021) 14:10203–11. doi: 10.2147/ijgm.S339378
21. Li C, Shang S. Relationship between sleep and hypertension: findings from the NHANES (2007-2014). Int J Environ Res Public Health. (2021) 18(15):20. doi: 10.3390/ijerph18157867
22. Tang Y, Peng B, Liu J, Liu Z, Xia Y, Geng B. Systemic immune-inflammation index and bone mineral density in postmenopausal women: a cross-sectional study of the national health and nutrition examination survey (NHANES) 2007-2018. Front Immunol. (2022) 13:975400. doi: 10.3389/fimmu.2022.975400
23. Di X, Liu S, Xiang L, Jin X. Association between the systemic immune-inflammation index and kidney stone: a cross-sectional study of NHANES 2007-2018. Front Immunol. (2023) 14:1116224. doi: 10.3389/fimmu.2023.1116224
24. Guo W, Song Y, Sun Y, Du H, Cai Y, You Q, et al. Systemic immune-inflammation index is associated with diabetic kidney disease in type 2 diabetes mellitus patients: evidence from NHANES 2011-2018. Front Endocrinol. (2022) 13:1071465. doi: 10.3389/fendo.2022.1071465
25. Song Y, Guo W, Li Z, Guo D, Li Z, Li Y. Systemic immune-inflammation index is associated with hepatic steatosis: evidence from NHANES 2015-2018. Front Immunol. (2022) 13:1058779. doi: 10.3389/fimmu.2022.1058779
26. Xia Y, Xia C, Wu L, Li Z, Li H, Zhang J. Systemic immune inflammation index (SII), system inflammation response index (SIRI) and risk of all-cause mortality and cardiovascular mortality: a 20-year follow-up cohort study of 42,875 US adults. J Clin Med. (2023) 12(3):20. doi: 10.3390/jcm12031128
27. Xiao S, Wang Z, Zuo R, Zhou Y, Yang Y, Chen T, et al. Association of systemic immune inflammation index with all-cause, cardiovascular disease, and cancer-related mortality in patients with cardiovascular disease: a cross-sectional study. J Inflamm Res. (2023) 16:941–61. doi: 10.2147/jir.S402227
28. Zhang Y, Li S, Xu RX, Zhu CG, Guo YL, Wu NQ, et al. Systemic inflammatory markers are closely associated with atherogenic lipoprotein subfractions in patients undergoing coronary angiography. Mediat Inflamm. (2015) 2015:235742. doi: 10.1155/2015/235742
29. Zhang Y, Liu W, Yu H, Chen Z, Zhang C, Ti Y, et al. Value of the systemic immune-inflammatory index (SII) in predicting the prognosis of patients with peripartum cardiomyopathy. Front Cardiovasc Med. (2022) 9:811079. doi: 10.3389/fcvm.2022.811079
30. Li Q, Ma X, Shao Q, Yang Z, Wang Y, Gao F, et al. Prognostic impact of multiple lymphocyte-based inflammatory indices in acute coronary syndrome patients. Front Cardiovasc Med. (2022) 9:811790. doi: 10.3389/fcvm.2022.811790
31. Zhan Y, Xu T, Tan X. Two parameters reflect lipid-driven inflammatory state in acute coronary syndrome: atherogenic index of plasma, neutrophil-lymphocyte ratio. BMC Cardiovasc Disord. (2016) 16:96. doi: 10.1186/s12872-016-0274-7
Keywords: coronary heart disease, cross-sectional study, predictive biomarker, systemic immune-inflammation index, association analysis
Citation: Ma J and Li K (2023) Systemic immune-inflammation index is associated with coronary heart disease: a cross-sectional study of NHANES 2009–2018. Front. Cardiovasc. Med. 10:1199433. doi: 10.3389/fcvm.2023.1199433
Received: 6 April 2023; Accepted: 7 June 2023;
Published: 7 July 2023.
Edited by:
Panagiotis Xaplanteris, Université Libre de Bruxelles, BelgiumReviewed by:
I-Shiang Tzeng, National Taipei University, TaiwanMuhammed Demir, Dicle University, Türkiye
© 2023 Ma and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ka Li bGlrYTEyN0AxMjYuY29t
 Jiwen Ma
Jiwen Ma Ka Li*
Ka Li*