- 1Intensive Care Unit, Jieyang People’s Hospital, Jieyang, China
- 2Emergency Department, Jieyang People’s Hospital, Jieyang, China
Background: The prognostic value of the serum albumin-to-creatinine ratio (sACR) in patients with ST-elevation myocardial infarction (STEMI) remains unclear. This study aims to investigate the impact of the sACR on incident major adverse cardiovascular events (MACEs) among revascularized patients with STEMI at long-term follow-up.
Methods: A total of 461 patients with STEMI who underwent successful primary percutaneous coronary intervention (PCI) were enrolled to explore the association between the sACR and MACE during a 30-month follow-up. The Cox regression proportional hazard model was used to evaluate the prognostic value of the sACR. Heterogeneity among specific groups was investigated by subgroup analysis.
Results: A total of 118 patients developed MACE during the follow-up. A negative association between the sACR and MACE was found after adjusting for other MACE-related risk factors. In subgroup analyses, the sACR was inversely associated with MACE in patients aged ≥ 60 years [hazard ratio (HR), 0.478; 95% confidence interval (CI), 0.292–0.784], male (HR, 0.528; 95% CI, 0.327–0.851), with hypertension history (HR, 0.470; 95% CI, 0.271–0.816), and with anterior wall myocardial infarction (HR, 0.418; 95% CI, 0.239–0.730). Meanwhile, the negative association between the sACR and MACE remained significant in a sensitivity analysis that excluded patients with low serum albumin levels (HR, 0.553; 95% CI, 0.356–0.860).
Conclusions: Patients with STEMI who underwent successful PCI with a low sACR had a higher risk of developing MACE, indicating that the sACR could be used to identify patients with STEMI who are at high risk of developing MACE.
1. Introduction
ST-segment elevation myocardial infarction (STEMI) is the most severe and time-sensitive disease with high mortality among patients with coronary artery disease (1). Worldwide, STEMI is the leading cause of death, which results in a high medical burden (2). Recent years have witnessed great advances in the treatment of acute myocardial infarction (AMI), but the risk of death remains high in patients with STEMI (2, 3). The decreasing trend in STEMI mortality is mainly attributed to the greater use of reperfusion therapy, especially primary percutaneous coronary intervention (PCI) (3, 4). Actually, the prognosis of post-STEMI following PCI is influenced by clinical, echocardiographic, and biochemical factors (5). Therefore, early risk stratification is extremely essential for clinicians to determine treatment strategy and long-term management.
Inflammation and platelet activation play an important role in the pathogenesis of AMI (6). Serum albumin, a stabilizing protein correlated with inflammation and platelet activation, has been found to be an essential biomarker for adverse events of AMI (7–9). Meanwhile, serum creatinine is an indicator of renal function and is associated with oxidative stress, endothelial function, inflammation, and systemic atherosclerosis (10, 11). The elevated serum creatinine levels at admission could also help in the prediction of the onset of adverse events in patients with AMI (11–14). Compared with serum albumin or creatinine alone, the serum albumin to creatinine ratio (sACR) has been proven to be a more valuable biomarker for adverse events in patients with AMI (15, 16). Unfortunately, whether the sACR is associated with the adverse events of STEMI after successful primary PCI remains unknown. More importantly, the clinical application of the sACR may be complicated by different age, gender, and clinical conditions. Hence, this study aims to investigate the impact of the sACR on incident major adverse cardiovascular events (MACEs) among revascularized patients with STEMI at long-term follow-up.
2. Materials and methods
2.1. Data source and study population
The data used in this present study were collected from the Dryad Digital Repository (https://datadryad.org/), which houses a large number of datasets from previously published papers (17). The original study was conducted in the First People's Hospital of Taizhou to explore the association of apelin-12 with MACE after primary PCI in patients with STEMI (18). A total of 464 consecutive patients with STEMI meeting the diagnostic criteria for STEMI between January 2010 and October 2014 were included in the original study. The diagnostic criteria of STEMI were typical persistent chest pain lasting more than 30 min, prolonged electrocardiograph alteration, and significantly elevated serum myocardial enzyme and troponin levels. All included patients had received successful standard primary PCI. The exclusion criteria and detailed treatment have been described previously (18). In addition, two patients with serum creatinine levels of more than 133 mmol/L and one patient with missing serum albumin were excluded, and the remaining 461 patients were included in the final analysis. All participants signed the informed consent form. Ethical approval was no longer required for this study because all data were anonymized, and data analysis adhered to the rules of the Dryad Digital Repository.
2.2. Data collection
The following basic characteristics of all patients were collected at hospital admission: age, gender, history of hypertension, history of diabetes mellitus, history of myocardial infarction, systolic blood pressure, heart rate, Killip's grade, and anterior wall myocardial infarction. The following laboratory test parameters were determined within 48 h of admission to hospital: white blood cell (WBC), percentage of neutrophils, hemoglobin, platelets, albumin, urea nitrogen, fasting blood glucose (FBG), uric acid, total cholesterol (TC), triglyceride (TG), high-density lipoprotein (HDL-C), low-density lipoprotein-cholesterol (LDL), peak cardiac troponin I (cTnI), and peak creatine kinase-MB (CK-MB). Echocardiographic and electrocardiographic data such as left atrial diameter, left ventricular diastolic diameter (LVEDD), and pathological Q wave were collected. Stent number, culprit vessel, and Gensini score were determined by interventional surgeons.
2.3. Definitions
The sACR is defined as the serum albumin divided by the serum creatinine. All patients were followed up for 30 months after primary PCI or until the occurrence of MACE. MACE is a combination of clinically driven target lesion revascularization, recurrent target vessel myocardial infarction, cardiogenic shock, congestive heart failure, or cardiac death.
2.4. Statistical analysis
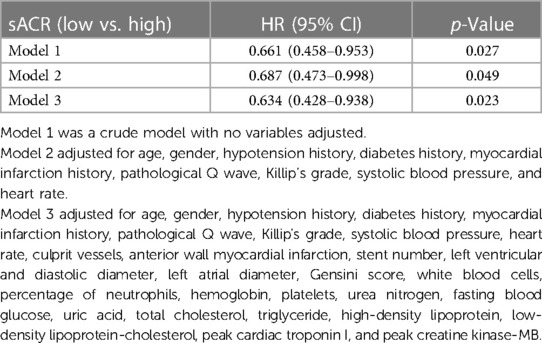
Patients were divided into two groups according to the median of the sACR (0.513): high (>0.513) and low (≤0.513) levels. Continuous variables were expressed as mean ± standard deviation (mean ± SD) for normally distributed data or median (25th and 75th percentiles) for non-normally distributed data, while categorical variables were presented as numbers and percentages. Continuous variables were compared by using the Mann–Whitney U test or Student’s t-test as appropriate, and categorical variables were analyzed by using the chi-square test. A Kaplan–Meier analysis was performed to acquire a graphical presentation of time to the incidence of MACE, and the log-rank test was used to compare the difference between the two groups according to the sACR. The hazard ratio (HR) and the 95% confidence interval (CI) were calculated to explore the association between the sACR and the incidence of MACE using Cox proportional hazard models. All predictors were included in the multiple Cox regression models based on their clinical importance. Model 1 was the crude model with no variables adjusted. Model 2 was adjusted for age, gender, history of hypotension, history of diabetes, history of myocardial infarction, pathological Q wave, Killip's grade, systolic blood pressure, and heart rate. Model 3 was based on Model 2 and all other covariates. Then, subgroup analyses were performed according to age, gender, history of hypertension, history of diabetes mellitus, pathological Q wave, and anterior wall myocardial infarction. All statistical analyses were performed using the R package (version 3.4.3). A P-value < 0.05 (two-sided) was considered statistically significant.
3. Results
The baseline characteristics of the enrolled patients are summarized in Table 1, according to the median of the sACR. Two hundred and thirty-two patients with an sACR ≤ 0.513 were assigned to the low sACR group, while the remaining patients with an sACR ≤ 0.513 were assigned to the high sACR group. No significant differences were found in most of the analyzed variables between the high sACR group and the low sACR group, except in terms of age, WBC count, percentage of neutrophils, albumin, creatinine, LDL, culprit vessels, and MACE occurrence. Figure 1 shows Kaplan–Meier analysis illustrating the cumulative incidence of MACE stratified by the sACR. Patients with a lower sACR showed a higher risk of MACE compared with those with a higher sACR (P = 0.026).
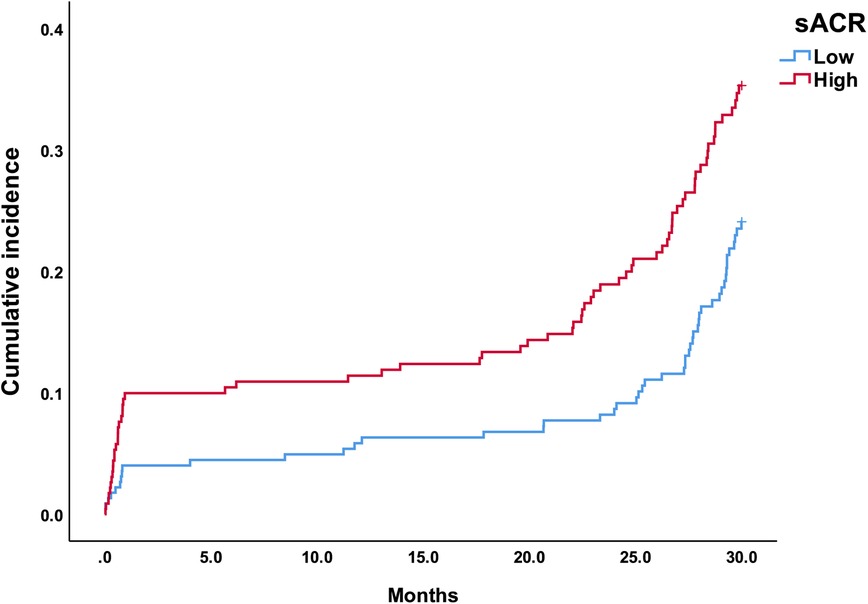
Figure 1. Kaplan–Meier curves stratified by the sACR. The curves show different incidences of MACE in patients with STEMI with different sACRs.

Table 1. Relationships between clinical and laboratory data and the sACR in patients with ST-elevation myocardial infarction.
The results of the Cox hazard model of the sACR on incident MACE are presented in Table 2. In Model 1, the sACR was negatively associated with MACE (HR, 0.661; 95% CI, 0.458–0.953). After adjustment for confounding factors, the negative association still remained in Model 2 (HR, 0.687; 95% CI, 0.473–0.998) and Model 3 (HR, 0.637; 95% CI, 0.410–0.989).
The sACR was inversely associated with MACE among participants aged ≥ 60 years (HR, 0.478; 95% CI, 0.292–0.784), males (HR, 0.528 95% CI, 0.327–0.851), with a history of hypertension (HR, 0.470; 95% CI, 0.271–0.816), and with anterior wall myocardial infarction (HR, 0.418; 95% CI, 0.239–0.730) (Figure 2). After excluding patients with low serum albumin levels (more than 35 g/L), the sACR was still inversely associated with MACE among patients with STEMI (HR, 0.553; 95% CI, 0.356–0.860).
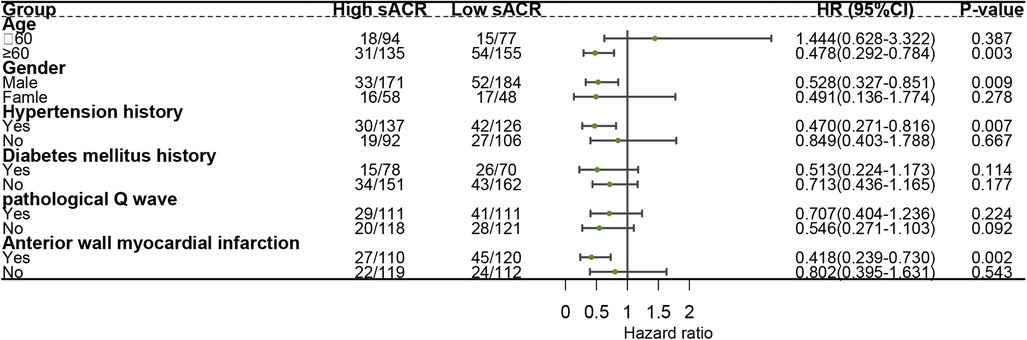
Figure 2. Effect size of the sACR on incident MACE in different subgroups. Each stratification was adjusted for age, gender, hypotension history, diabetes history, myocardial infarction history, pathological Q wave, Killip's grade, systolic blood pressure, heart rate, culprit vessels, anterior wall myocardial infarction, stent number, left ventricular and diastolic diameter, left atrial diameter, Gensini score, white blood cells, percentage of neutrophils, hemoglobin, platelets, urea nitrogen, fasting blood glucose, uric acid, total cholesterol, triglyceride, high-density lipoprotein, low-density lipoprotein-cholesterol, peak cardiac troponin I, and peak creatine kinase-MB, except the stratification factor itself.
4. Discussion
In this cohort study, the sACR was found to be inversely associated with MACE in patients with STEMI after primary PCI. After excluding patients with low serum albumin levels, this inverse association remained. A subgroup analysis indicated that a low sACR was a risk factor for STEMI patients aged ≥ 60 years, male, with hypertension history, and with anterior wall myocardial infarction.
The sACR is a reproducible, low-cost parameter that is easy to collect in routine clinical management. Therefore, this investigation enriches the recent evidence that a low sACR could be used for predicting the occurrence of adverse events among patients with AMI (15, 16). In China, only one study that included 2,250 patients with a 20-month follow-up reported that a low sACR is associated with an increased risk of all-cause mortality among patients with AMI after PCI (15). The study by Turkyilmaz et al. showed that the sACR was an independent predictor of in-hospital mortality, as well as contrast-induced nephropathy, congestive heart failure, and stent thrombosis at 30 days among patients with STEMI (16). However, no research has been done to investigate the link between the sACR and the risk of MACE during long-term follow-up among patients with STEMI after primary PCI. Hence, this study was the first evaluation of the predictive potential of the sACR for MACE among revascularized patients with STEMI at long-term follow-up (30 months).
The exact mechanisms underlying the association of the sACR and the risk of MACE among revascularized patients with STEMI have still not been fully understood. Inflammation and thrombosis play important pathological roles in STEMI (6). Decreased serum albumin is associated with an increased risk of adverse events in patients with AMI (7, 9). For each 1 g/dl reduction in serum albumin levels in patients with first-onset AMI, the risk of all-cause mortality and cardiovascular death increased by 66% and 47%, respectively (8). Inflammation not only reduces serum albumin synthesis but also increases serum albumin catabolism (19). Physiological concentrations of serum albumin would exert its anti-inflammatory effect on endothelial cells (20). Moreover, decreased serum albumin has been shown to be related to the promotion of oxidative stress, platelet activation, and aggregation, which further increase the risk of thrombotic events (7, 9, 21). Creatinine is an indicator of kidney function and an important marker of oxidative stress, endothelial dysfunction, inflammatory status, and progressive atherosclerosis (10, 11, 14). The elevated serum creatinine levels at admission have an independent ability to predict adverse events in patients with AMI (11–14). However, it must be noted that patients with serum creatinine levels of more than 133 mmol/L were excluded from this study. Increased serum creatinine levels within the normal range can increase the risk of cardiovascular disease among participants without metabolic syndrome (22). Increased serum creatinine levels within the normal range could increase the risk of cardiovascular disease by mediating an inflammatory state augmented by dysfunctional apolipoprotein A-I (22). Therefore, combining serum albumin and creatinine in patients with STEMI suffering from an acute inflammatory and thrombotic process may help effectively identify patients with a high risk of adverse events.
The study by Plakht et al. found that decreased serum albumin within the normal clinical range also increases the long-term all-cause mortality in hospital survivors after AMI (7). After excluding patients with low serum albumin levels, the inverse association between the sACR and the risk of MACE among revascularized patients with STEMI remained significant. Therefore, it is necessary to calculate the sACR to assess the risk of MACE among patients with STEMI with normal serum albumin levels.
Previous studies have not evaluated the relationship between the sACR and the risk of MACE in different subgroups. Our subgroup analysis demonstrated that a low sACR was a risk factor for patients aged ≥60 years, male, with hypertension history, and with anterior wall myocardial infarction. Owing to the limited number of patients included in the present study, this result should be interpreted with caution. More importantly, more prospective studies are needed in this area.
Several limitations can be found in this study. First, unmeasured confounding factors such as smoking, high-sensitivity C-reactive protein, and the use of statins or beta blockers and antiplatelet drugs, may be attributed to the occurrence of MACE. This study was a secondary analysis based on previous studies, and related information about other confounders was limited. Second, repeated evaluations of serum creatinine levels during hospitalization can help improve risk assessment among patients with AMI (23), but the sACR was measured only once on admission. The variations in the sACR during hospitalization and its predictive value of adverse events were not clarified in this study. Third, we excluded patients with serum creatinine levels exceeding 133 mmol/L. However, chronic kidney disease and atherosclerotic cardiovascular disease often coexist. A significant proportion of patients with STEMI present with serum creatinine levels higher than 133 mmol/L. Therefore, the exclusion of these patients may affect the results of the study. Finally, this study had a relatively small sample size, especially when subgroup analysis was performed. Therefore, further research is needed to generalize our conclusions.
5. Conclusion
A low sACR was associated with an increased risk of MACE in patients with STEMI after primary PCI. Screening the sACR of individuals could be used to stratify patients with STEMI at risk of MACE.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://datadryad.org/stash/dataset/doi:10.5061%2Fdryad.pf56m.
Ethics statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XH, YL, and BZ contributed to the conception and design of the study. XH, YL, CZ, and ZL performed the statistical analysis. XH and YL wrote the first draft of the manuscript. XH and BZ reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank Yang, Lingchang, and their collaborators who prepared the publicly available data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer YF declared a shared affiliation with the authors to the handling editor at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yildiz M, Wade SR, Henry TD. STEMI Care 2021: addressing the knowledge gaps. Am Heart J Plus. (2021) 11:100044. doi: 10.1016/j.ahjo.2021.100044
2. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2018) 39(2):119–77. doi: 10.1093/eurheartj/ehx393
3. Gale CP, Allan V, Cattle BA, Hall AS, West RM, Timmis A, et al. Trends in hospital treatments, including revascularisation, following acute myocardial infarction, 2003–2010: a multilevel and relative survival analysis for the National Institute for Cardiovascular Outcomes Research (NICOR). Heart. (2014) 100(7):582–9. doi: 10.1136/heartjnl-2013-304517
4. Puymirat E, Simon T, Steg PG, Schiele F, Guéret P, Blanchard D, et al. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. Jama. (2012) 308(10):998–1006. doi: 10.1001/2012.jama.11348
5. Vogel B, Claessen BE, Arnold SV, Chan D, Cohen DJ, Giannitsis E, et al. ST-segment elevation myocardial infarction. Nat Rev Dis Primers. (2019) 5(1):39. doi: 10.1038/s41572-019-0090-3
6. Nagareddy P, Smyth SS. Inflammation and thrombosis in cardiovascular disease. Curr Opin Hematol. (2013) 20(5):457–63. doi: 10.1097/MOH.0b013e328364219d
7. Plakht Y, Gilutz H, Shiyovich A. Decreased admission serum albumin level is an independent predictor of long-term mortality in hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction II (SAMI-II) project. Int J Cardiol. (2016) 219:20–4. doi: 10.1016/j.ijcard.2016.05.067
8. Xia M, Zhang C, Gu J, Chen J, Wang LC, Lu Y, et al. Impact of serum albumin levels on long-term all-cause, cardiovascular, and cardiac mortality in patients with first-onset acute myocardial infarction. Clin Chim Acta. (2018) 477:89–93. doi: 10.1016/j.cca.2017.12.014
9. Zhu L, Chen M, Lin X. Serum albumin level for prediction of all-cause mortality in acute coronary syndrome patients: a meta-analysis. Biosci Rep. (2020) 40(1). doi: 10.1042/bsr20190881
10. Shulman NB, Ford CE, Hall WD, Blaufox MD, Simon D, Langford HG, et al. Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the hypertension detection and follow-up program. The Hypertension Detection and Follow-up Program Cooperative Group. Hypertension. (1989) 13(5 Suppl):I80–93. doi: 10.1161/01.hyp.13.5_suppl.i80
11. Yamaguchi J, Kasanuki H, Ishii Y, Yagi M, Nagashima M, Fujii S, et al. Serum creatinine on admission predicts long-term mortality in acute myocardial infarction patients undergoing successful primary angioplasty: data from the Heart Institute of Japan Acute Myocardial Infarction (HIJAMI) Registry. Circ J. (2007) 71(9):1354–9. doi: 10.1253/circj.71.1354
12. Hobbach HP, Gibson CM, Giugliano RP, Hundertmark J, Schaeffer C, Tscherleniak W, et al. The prognostic value of serum creatinine on admission in fibrinolytic-eligible patients with acute myocardial infarction. J Thromb Thrombolysis. (2003) 16(3):167–74. doi: 10.1023/b:Thro.0000024055.13207.50
13. Zhao L, Wang L, Zhang Y. Elevated admission serum creatinine predicts poor myocardial blood flow and one-year mortality in ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. J Invasive Cardiol. (2009) 21(10):493–8. doi: 10.1111/j.1540-8183.2009.00483.x
14. Kamishima K, Yamaguchi J, Honda A, Ogawa H, Hagiwara N. Effect of concurrent elevation of serum creatinine and C-reactive protein values on the long-term outcome in patients with ST-elevation acute myocardial infarction. Int J Cardiol. (2015) 188:102–4. doi: 10.1016/j.ijcard.2015.04.048
15. Liu H, Zhang J, Yu J, Li D, Jia Y, Cheng Y, et al. Prognostic value of serum albumin-to-creatinine ratio in patients with acute myocardial infarction: results from the retrospective evaluation of acute chest pain study. Medicine (Baltimore). (2020) 99(35):e22049. doi: 10.1097/md.0000000000022049
16. Turkyilmaz E, Ozkalayci F, Birdal O, Karagoz A, Tanboga IH, Tanalp AC, et al. Serum albumin to creatinine ratio and short-term clinical outcomes in patients with ST-elevation myocardial infarction. Angiology. (2022) 73(9):809–17. doi: 10.1177/00033197221089423
17. Yang L, Zheng T, Wu H, Xin W, Mou X, Lin H, et al. Data from: predictive value of apelin-12 in ST-elevation myocardial infarction patients with different renal function: a prospective observational study. (2017). doi: 10.5061/dryad.pf56m
18. Yang L, Zheng T, Wu H, Xin W, Mou X, Lin H, et al. Predictive value of apelin-12 in patients with ST-elevation myocardial infarction with different renal function: a prospective observational study. BMJ open. (2017) 7(11):e018595. doi: 10.1136/bmjopen-2017-018595
19. Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial. (2004) 17(6):432–7. doi: 10.1111/j.0894-0959.2004.17603.x
20. Zhang WJ, Frei B. Albumin selectively inhibits TNF alpha-induced expression of vascular cell adhesion molecule-1 in human aortic endothelial cells. Cardiovasc Res. (2002) 55(4):820–9. doi: 10.1016/s0008-6363(02)00492-3
21. Lam FW, Cruz MA, Leung HC, Parikh KS, Smith CW, Rumbaut RE. Histone induced platelet aggregation is inhibited by normal albumin. Thromb Res. (2013) 132(1):69–76. doi: 10.1016/j.thromres.2013.04.018
22. Onat A, Yüksel H, Can G, Köroğlu B, Kaya A, Altay S. Serum creatinine is associated with coronary disease risk even in the absence of metabolic disorders. Scand J Clin Lab Invest. (2013) 73(7):569–75. doi: 10.3109/00365513.2013.821712
Keywords: serum albumin, creatinine, ST-elevation myocardial infarction, percutaneous coronary intervention, clinical outcomes
Citation: Huang X, Liu Y, Zhong C, Lin Z and Zheng B (2023) Association between serum albumin-to-creatinine ratio and clinical outcomes among patients with ST-elevation myocardial infarction after percutaneous coronary intervention: a secondary analysis based on Dryad databases. Front. Cardiovasc. Med. 10:1191167. doi: 10.3389/fcvm.2023.1191167
Received: 21 March 2023; Accepted: 15 June 2023;
Published: 29 June 2023.
Edited by:
Petar Otasevic, Institute for Cardiovascular Diseases Dedinje, SerbiaReviewed by:
Maja Milosevic, Institute for Cardiovascular Diseases Dedinje, SerbiaYongqiang Fan, Sun Yat-sen University, China
© 2023 Huang, Liu, Zhong, Lin and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binyun Zheng OTQ4NDc2OTQxQHFxLmNvbQ==
 Xiaoye Huang
Xiaoye Huang Yuchun Liu1
Yuchun Liu1