- 1Department of Cardiology, the 1st affiliated Hospital of Wenzhou Medical Unversity, Wenzhou, China
- 2School of Pharmaceutical College, Wenzhou Medical University, Wenzhou, China
- 3Laboratory Animal Center of Wenzhou Medical University, Wenzhou, China
- 4Department of Endocrinology, the 3rd Affiliated Hospital of Wenzhou Medical University, Ruian People’s Hospital, Wenzhou, China
Objectives: Obesity, especially abdominal obesity, increases the prevalence of metabolic and cardiovascular disease (CVD). Fibroblast growth factor 21 (FGF21) has been identified as a critical regulator playing a therapeutic role in diabetes and its complications. This study aims to evaluate the relationship between serum FGF21 levels and body shape parameters in patients with hypertension (HP) and type 2 diabetes mellitus (T2DM).
Methods: Serum FGF21 levels were determined in 1,003 subjects, including 745 patients with T2DM, and 258 individuals were selected as a healthy control in this cross-sectional study.
Results: Serum FGF21 levels were significantly higher in T2DM patients with HP than those without [534.9 (322.6–722.2) vs. 220.65 (142.8–347.55) pg/ml, p < 0.001], and levels in both of these two groups were significantly increased compared with that of healthy control [123.92 (67.23–219.32) pg/ml, all p < 0.001]. These differences were also observed in body shape parameters, including weight, waistline, body mass index (BMI), body shape index (ABSI), and the percentage of abdominal obesity. Serum FGF21 levels in T2DM patients were positively correlated with body shape parameters, including weight, waistline, neck circumference, BMI, ABSI, percent of abdominal obesity, and triglyceride, while negatively with estimated glomerular filtration rate (all p < 0.01). The significance remained stable when adjusted for age and T2DM duration. In addition, both serum FGF21 concentrations and waistline were independently associated with HP in T2DM patients after the adjustment for risk factors (all p < 0.05). ROC analysis for FGF21 levels of 745 patients with T2DM identified 411.33 pg/ml as an optimal cut-off point to predict HP, with a sensitivity and specificity of 66.0% and 84.9%, respectively.
Conclusions: FGF21 resistance occurs in patients of HP in T2DM, and positively correlates with body shape parameters (especially waistline and BMI). High levels of FGF21 may be a compensatory reaction to offset HP.
1. Introduction
Metabolic syndrome is a combination of multiple metabolic disorders, including obesity, insulin resistance, hyperinsulinemia, abnormal lipid metabolism, abnormal glucose metabolism and hypertension (HP) (1). These metabolic disorders are the pathological basis of heart, cerebrovascular diseases, and diabetes. It is generally recognized that the common cause of these disorders is obesity, especially abdominal obesity, which results in the body's resistance to insulin, thus reducing the utilization of peripheral glucose and increase the utilization of fatty acids, leading to type 2 diabetes mellitus (T2DM) (2). In addition, it should be noted that similar manifestations of metabolic syndrome could also be observed in individuals with abdominal obesity but not overweight in total body weight (3). Obesity-induced insulin resistance and associated hyperinsulinemia, hyperglycemia, and adipokine may also cause vascular endothelial dysfunction, dyslipidemia, HP, and vascular inflammation, which contribute to the development of atherosclerotic cardiovascular disease (CVD) (4, 5). Controlling obesity is a standard preventive and therapeutic measure for metabolic disorders (6).
Recently, fibroblast growth factor 21(FGF21) has been considered as a novel metabolic risk factor, which is closely associated with a variety of metabolic and CVD (7, 8). Circulating FGF21 is mainly derived from the liver and acts by binding to its receptor FGFR1 and coreceptor β-klotho in regulating energy balance and glucose and lipid homeostasis (9). Surprisingly, however, individuals with metabolic disorders such as obesity, T2DM and fatty liver have high levels of FGF21 and respond poorly to exogenous FGF21, this phenomenon was defined as FGF21 resistance. FGF21 resistance is a state of the body's weakened response to FGF21, which is manifested by reduced biological effects of target tissues and increased compensatory synthesis of FGF21 in the body (10, 11). This may be due to decreased expression or sensitivity of the FGF21 receptor and β-klotho protein (12). Long-term lifestyle interventions such as diet, exercise, weight control, etc. may improve FGF21 resistance (10). These changes in daily habits are equally important in combination of antihypertensive drugs for controlling blood pressure. Therefore, it is of great importance to motivate people to keep their body in good shape.
In non-metabolic CVDs, FGF21 plays an essential role in the regulation of blood pressure. In mechanism, our previous study found that FGF21 participated in the regulation of HP by improving the function of endothelial cells, promoting the release of vasodilatory factors, inhibiting vascular remodeling, and antagonizing angiotensin II (Ang II). By using FGF21 gene knockout mice and overexpressed mice, we confirmed the effect of FGF21 on lowering blood pressure and protecting the cardiovascular system. FGF21 protects against Ang II-induced HP and vascular impairment by fine-tuning the multi-organ crosstalk between liver, adipose tissue, kidney, and blood vessels through the activation of the ACE2/Ang-(1–7) axis. It is a medium for multiple organs and systems to resist pathological changes jointly (13). In addition, the antihypertensive treatment prepared by FGF21 as the active substance has a significant improvement effect on HP symptoms caused by Ang II (14). Basic research and clinical application of FGF21 in blood pressure regulation has made preliminary progress in recent years (15). Compared with traditional antihypertensive drugs such as β-blockers, angiotensin-converting enzyme inhibitors, diuretics, etc., FGF21 not only improves blood pressure but also has the function of protecting the cardiovascular system and alleviating vascular injury, showing the potential of FGF21 in the development of drugs for dealing with HP. On the one hand, FGF21 promotes the development of HP, possibly through fluid retention. FGF21 is a critical mediator in PPARγ signal transduction. Mice with FGF21 gene knockout showed PPARγ signal defects and resistance to significant side effects (such as weight gain and edema) of rosiglitazone (PPARγ agonist) (16). On the other hand, FGF21 is also a hormone that acts on the central nervous system. It can enter the human blood circulation, cross the blood-brain barrier, and its receptor FGFR and cofactor β-clotho are distributed in key locations of pressure emission pathways and blood pressure regulation sites. Therefore, FGF21 may be involved in the regulation of central blood pressure by activating related signaling proteins in the central nervous system (17). However, more and more studies have reported that the elevated human serum FGF21 level was independently associated with HP, obesity, T2DM and fatty liver diseases, which led us to hypothesize that HP in fact may affect the raise of serum FGF21 level, especially in the state of diabetes.
For the superior efficacy of FGF21in handling metabolic diseases, including HP, thus improving FGF21 resistance is a new idea for the treatment of obesity and related metabolic disease. In the general population, FGF21 level has been confirmed to be closely associated with metabolic syndrome, including obesity, non-alcoholic fatty liver disease, HP, and diabetes (18). Complex metabolic diseases such as obesity, HP, diabetes, etc. are isolated and interrelated. However, the relationship between FGF21, body shape, and blood pressure in patients with diabetes remains unknown. In this regard, the purpose of this study is to systematically explore the correlation between serum FGF21 levels of HP in patients with T2DM and to find out the risk factors of diabetes complicated with HP to provide new methods for the etiology, early screening, diagnosis, treatment, and prevention of chronic complications of diabetes.
2. Materials and methods
2.1. Participants
A total of 745 patients diagnosed with T2DM participated in this cross-sectional study recruited from July 1, 2019–January 28, 2023 from the Diabetes Center of Ruian People's Hospital. T2DM was diagnosed according to the criteria of DM proposed by the World Health Organization in 1999: Symptoms of diabetes, a blood glucose level of 11.1 mmol/L at any time, a fasting blood glucose (FPG) level of 7.0 mmol/L or a 2-hour blood glucose level of 11.1 mmol/L (19). HP was defined with systolic blood pressure (SBP) ≥ 140 mmHg, diastolic BP (DBP) ≥ 90 mmHg, or a history of HP, or use of antihypertensive drugs. Body mass index (BMI) was defined as weight over height2 (kg/m2), a body shape index (ABSI) was calculated as waistline/(BMI2/3height1/2) (m11/6kg−2/3), overall obesity was defined by BMI ≥ 28 kg/m2, and abdominal obesity was defined by waistline ≥ 90 cm for men and ≥85 cm for women. A complete history and thorough physical examination were obtained in each case. BP was measured using a mercury sphygmomanometer after a 10 min rest. Waistline to hipline ratio (WHR), headline, and neckline was also measured at baseline. In addition, routine laboratory tests were done. This study was performed with the approval of the Human Ethics Committee of Ruian People's Hospital, and written informed consent was obtained from each participant.
2.2. Clinical data collection and biochemical assessment
Additional laboratory data and detailed history of physician-diagnosed disease, drinking, and smoking histories were obtained and evaluated through questionnaires. Blood was drawn following an 8–12 h period of fasting for determination of FPG, hemoglobin A1c (HbA1c), triglyceride (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-c), and low-density lipoprotein cholesterol (LDL-c). The chronic kidney disease epidemiology collaboration formula was used to calculate the estimated glomerular filtration rate (eGFR). Serum samples obtained from all participants were stored in −80°C preparing for further detection. Human serum FGF21 levels were quantitatively determined in vitro by a standard enzyme-linked immunosorbent assay kit (Antibody and Immunoassay Service, HKU, HK). Serum FGF21 levels and other baseline characteristics were compared between T2DM patients with and without HP. Univariable and multivariable logistic regression analysis was used to identify factors most closely associated with HP. Furthermore, correlation analysis was performed to examine the determinant factors of circulating FGF21 levels in patients with T2DM.
2.3. Statistical analysis
All statistical analyses were performed using Statistical Package for Social Science Version 26.0 (IBM Corporation, NY, USA). Continuous data were expressed as mean ± standard deviation or median with interquartile range. Categorical data are expressed as percentages. Independent-sample t test, one-way ANOVA followed by Tukey's HSD test or the nonparametric Kruskal-Wallis test followed by Dunn's test, and χ2 test was used to determine differences between groups. Variables with statistical significance between groups and variables which were biologically likely to be related to HP were all included to determine independent factors of HP in T2DM, using univariable and multivariable logistic regression analysis. In addition, pearson correlation and partial correlation analysis adjusted for age and T2DM duration were applied to identify the association of FGF21 and body shape parameters or biochemical parameters. The predictive value of FGF21 against HP was determined with ROC curves. Two-sided p values < 0.05 were considered statistically significant.
3. Results
3.1. Serum FGF21 levels are significantly increased in T2DM patients with or without HP compared to healthy controls
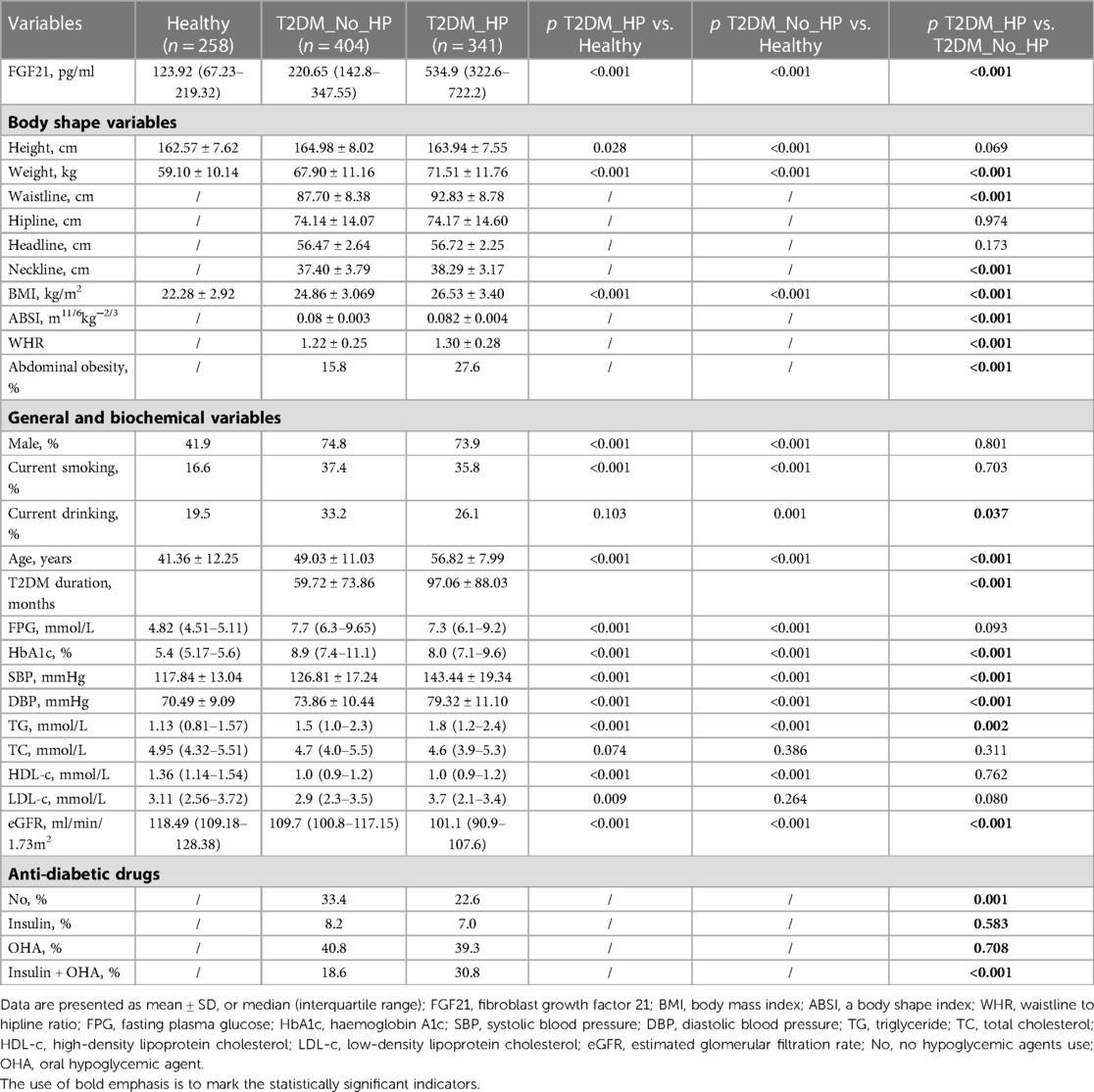
The physical and biochemical characteristics of T2DM patients and healthy controls including FGF21 levels, body shape parameters, and biochemical parameters likely to be related to HP risks are summarized in Table 1. Serum FGF21 levels was increased in T2DM patients compared with those in healthy [220.65 (142.8–347.55) vs. 123.92 (67.23–219.32) pg/ml, all p < 0.001]. Moreover, T2DM patients with HP expressed at the FGF21level of more than twice as high as those without [534.9 (322.6–722.2) vs. 220.65 (142.8–347.55) pg/ml, p < 0.001]. There was no statistically significant difference between patients of diabetes with or without HP on height, significant differences were only found when compared with healthy, however, there was a gradual increase in weight in these three groups (59.10 ± 10.14 vs.67.90 ± 11.16 vs. 71.51 ± 11.76 kg, all p < 0.001), so was BMI (22.28 ± 2.92 vs. 24.86 ± 3.069 vs. 26.53 ± 3.40 kg/m2, all p < 0.001). WHR was equal to waistline/hipline. The mean hipline of the patients of diabetes with or without HP was nearly equal (74.14 ± 14.07 vs. 74.17 ± 14.60 cm, p = 0.974); interestingly, however, both waistline (92.83 ± 8.78 vs. 87.70 ± 8.38 cm, p < 0.001) and WHR (1.30 ± 0.28 vs. 1.22 ± 0.25, p < 0.001) were increased in diabetes with HP as compared to those without. Similarly, elevated ABSI (0.082 ± 0.004 vs. 0.08 ± 0.003 m11/6kg−2/3) and neckline (38.29 ± 3.17 vs. 37.40 ± 3.79 cm) were found in these T2DM individuals with HP compared with those without (all p < 0.001). In addition, the prevalence of abdominal obesity was significantly higher in diabetes with HP (27.6 vs. 15.8%, p < 0.001) than that of diabetes alone. No significant difference was found in headline between the two groups (56.47 ± 2.64 vs. 56.72 ± 2.25 cm, p = 0.173). Although there was a significant difference in anti-diabetic drugs use (Table 1), no correlation was found between the anti-diabetic treatments and serum FGF21 levels (Table 2).
In sum, FGF21 is increased, and a worse of body shape parameters, including elevated weight, waistline, neckline, BMI, ABSI, and WHR, was found in these T2DM individuals with HP compared with those without this complication (all p < 0.05). These data suggest FGF21 resistance occurs in diabetes, especially those with HP.
3.2. Serum FGF21 levels are closely correlated with a cluster of body shape parameters and HP in patients with T2DM
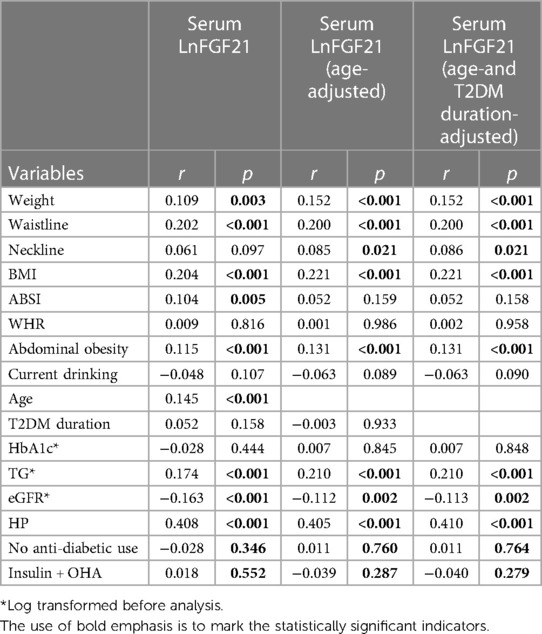
The prevalence of abdominal obesity is high, and an increased serum level of FGF21 was observed in HP individuals with diabetes (Table 1). Is there any relationship between serum FGF21 levels and body shape in these T2DM individuals? We next investigated the relationship between serum FGF21 levels and a cluster of body shape parameters. Correlation analysis showed a significant positive association of serum FGF21 levels with body shape parameters, including weight, waistline, BMI, ABSI, abdominal obesity, and TG, respectively (all p < 0.05). However, serum FGF21 was negatively correlated with eGFR (p < 0.001). After the adjustment for age, the significance remained stable, with a bit of change in neckline (p < 0.05) and ABSI (p > 0.05). Furthermore, the correlation of serum FGF21 with these parameters, except for ABSI remained significant even after the adjustment for age and T2DM duration (Table 2). To clarify whether HP is correlated with FGF21, we also analyzed the relationship of serum FGF21 with HP by partial correlation analysis. As shown in Table 2, HP was strikingly positively correlated with serum FGF21 levels when adjusted by age and T2DM duration (r = 0.410, p < 0.001). These data suggest that serum FGF21 levels are closely related to body shape and HP in patients with T2DM.
3.3. Serum FGF21 levels and waistline are independently associated with HP in T2DM patients
To investigate whether FGF21 is related to the morbidity of HP in patients with T2DM, we first explored the risk factors of HP in these T2DM subjects. As shown in Table 1, an increased manner of serum FGF21 levels was observed in these T2DM subjects with HP compared with those without. Consistent with the change of FGF21, a higher prevalence of abdominal obesity was observed in these individuals. In univariable logistic regression analyses (Table 3), body weight, waistline, neckline, BMI, ABSI, and WHR, but not standing height or hipline, predicted the occurrence of HP in these T2DM subjects, suggesting that body weight, waistline, neckline, BMI, ABSI, and WHR screening in diabetic patients could be helpful in detecting high-risk individuals of cardiovascular complications such as HP as early as possible. In addition, current drinking, age, T2DM duration, HbA1c, TG, and eGFR were also found to be independent risk factors for the established HP. In stepwise multiple regression analysis (Table 4), the predictors of HP were FGF21, weight, and waistline in the model adjusted by body shape parameters. FGF21, age, T2DM duration, HbA1c, TG, and eGFR are risk factors for HP in the model adjusted by general and biochemical parameters. Interestingly, the association of serum FGF21, waistline, age, HbA1c, and eGFR with HP remained significant in model 3, which was adjusted by parameters with p < 0.05 in models 1–2.
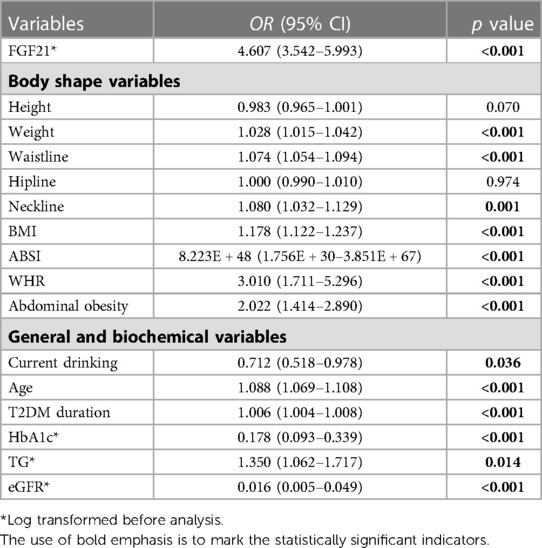
Table 3. Factors associated with HP in patients with T2DM in univariable logistic regression analyses (n = 745).
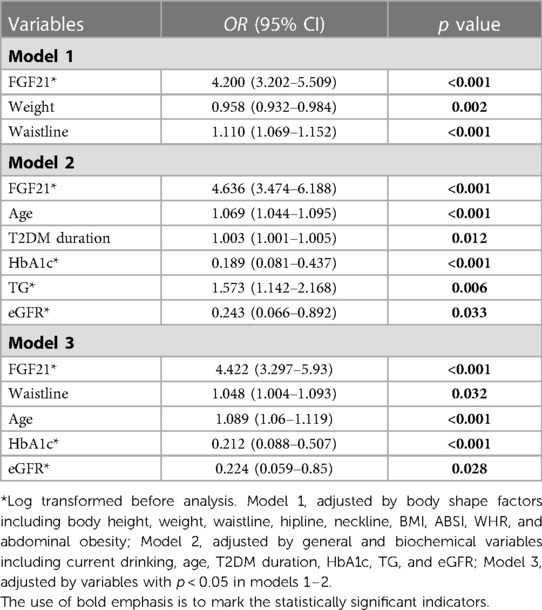
Table 4. Factors associated with HP in patients with T2DM in stepwise multivariable logistic regression analysis (n = 745).
In addition, Receiver operating characteristic (ROC) curve analysis and 95% confidence interval (CI) were applied to judge the value of FGF21 on HP high-risk score. In this study, the area under the curve (AUC) was found to be statistically significant (AUC: 0.789, 95% CI: 0.756–0.823, p < 0.001) in the total sample (Figure 1). Furthermore, a combined analysis of FGF21, waistline, and age got a more considerable AUC value compared with these three parameters alone (AUC: 0.854, 95% CI: 0.827–0.881, p < 0.001), moreover, the sensitivity and specificity of combined detection of FGF21, waistline and age were significantly higher than those of single detection. As an optimal cutoff point, high risk LnFGF21 value of 6.02 pg/ml (FGF21 value of 411.33 pg/ml) was determined with a 66.0% sensitivity and 84.9% specificity. Taken together, serum FGF21 levels (411.33 pg/ml or more), waistline (87.75 cm or more), and age (53.5 year or more) may be good predictors for the incidence of HP in patients with T2DM.
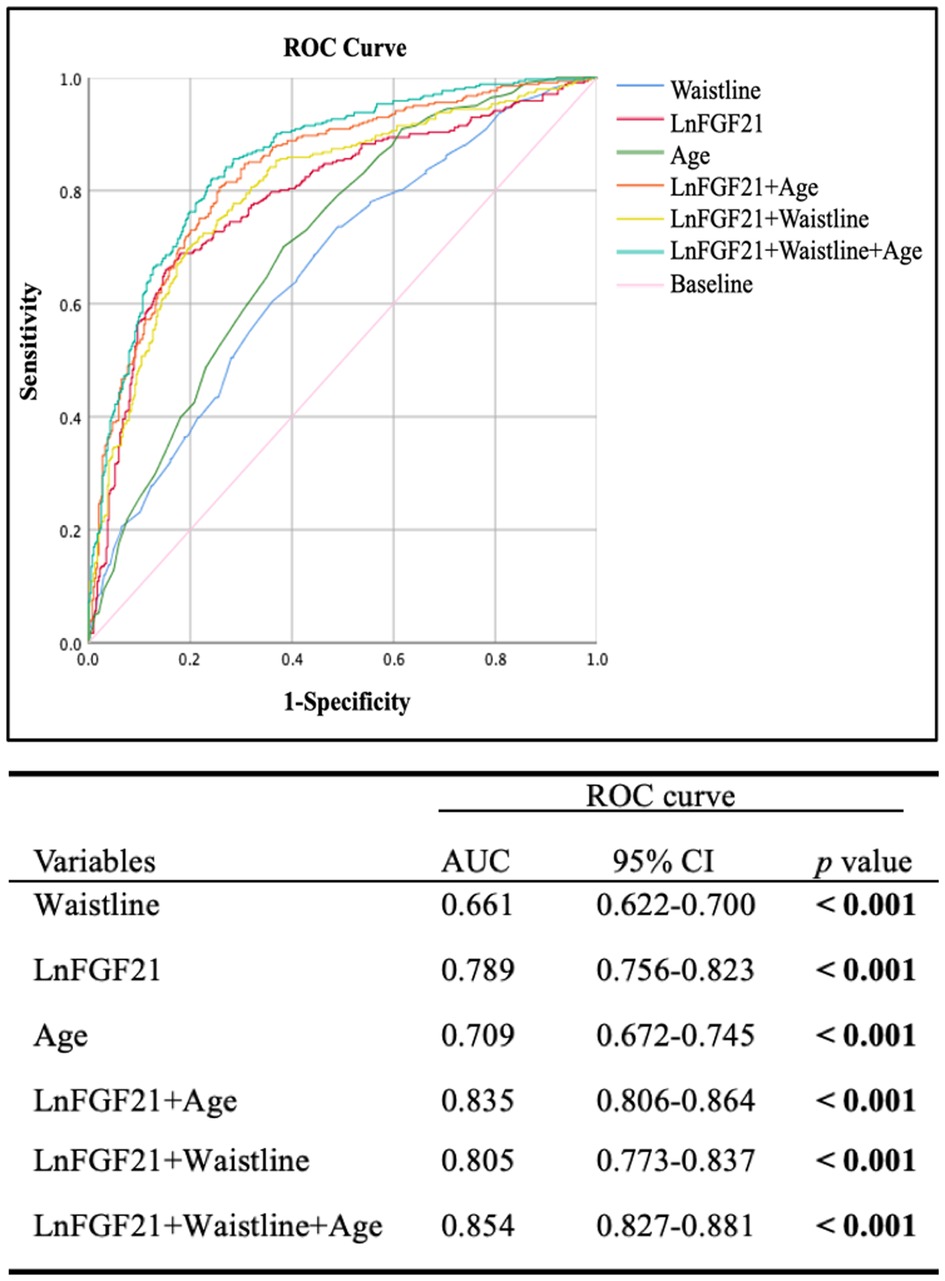
Figure 1. Curve analysis of serum FGF21, waistline, and age for predicting the HP of 745 patients with T2DM. Upper panel: ROC curve; Down panel: the area under ROC (AUC) curve.
4. Discussion
Patients with diabetes are most likely to have a high risk of CVD, which is the leading cause of death among patients with T2DM. HP is a cardiovascular syndrome with elevated systemic arterial pressure as the primary clinical manifestation. Our previous animal research demonstrated that FGF21 plays an essential role in regulating blood pressure (13). However, such a conclusion, even if well founded, is unsatisfactory for due to the few human studies for metabolic cardiovascular diseases evaluating the relationship between FGF21 and HP have been reported. Current studies on FGF21 mainly focus on glucose and lipid metabolism, obesity and diabetes. FGF21 levels in circulation (20), cord blood (21), and placenta (22) were elevated in pregnant women with diabetes mellitus, and positively correlated with human BMI. Surprisingly, however, these findings contradict the positive efficacy of FGF21 in rodents. Therefore, some researchers have questioned whether FGF21 resistance exists in patients with obesity and other related metabolic diseases (23). The expected beneficial effects of endogenous FGF21 are not present in obesity, which is a great challenge for clinical drug development based on FGF21. Given the close relationship between obesity, diabetes and other metabolic diseases and HP, scholars have begun to pay attention to the relationship between FGF21 level and HP in recent years, and studies have shown that circulating FGF21 level is significantly correlated with increased blood pressure (24). These data suggest that complicated metabolic cardiovascular problems may be an FGF21-resistant state.
Nevertheless, the causal relationship and potential effects between HP and FGF21 need to be better clarified. HP may be related to the improvement of insulin resistance and the influence of FGF21 on the afferent pathway of stress reflex. In fructose-induced hypertensive SD rats, FGF21 could improve the absorption and utilization of glucose, improve insulin resistance, increase the activity of NO synthase, stimulate endothelial cells to release strong vasodilator NO, improve endothelial function, and ultimately significantly reduce the SBP of SD rats (25). Our previous studies showed that the inhibition of FGF21 can promote Ang II production, leading to the occurrence of HP. Treatment with recombinant FGF21 can convert Ang II into Ang (1–7), expand the artery to reduce the peripheral resistance of blood vessels, reverse vascular damage, and lower high blood pressure (13). FGF21 can also prevent myocardial fibrosis caused by HP. During HP, both systemic and cardiac FGF21 will be induced and act on the heart to avoid hypertensive heart disease (26). HP is also a chronic inflammatory disease, which can cause the accumulation of pro-inflammatory cells including macrophages and T lymphocytes, which play a crucial role in the pathogenesis of HP (27). Depletion of FGF21 resulted in a significant increase in blood pressure, which led to increased infiltration of monocytes, macrophages and T cells, and aggravated aortic inflammation in Ang II-treated wild-type mice. These negative effects were significantly amplified in FGF21 knockout mice but were entirely reversed by infection with aav-FGF21, showing that FGF21 can inhibit HP and ameliorate HP-mediated vascular damage (28). These above results suggest that FGF21 can regulate blood pressure by regulating renin-angiotensin system, stress reflex afferent pathway, and inhibiting inflammatory response. With further research, FGF21 is expected to become a new biomarker to predict the occurrence of HP, and FGF21 or its agonists may become a new target for the treatment of HP.
It was firstly reported that the elevated serum FGF21 level was independently associated with HP in American community residents according to a prospective open cohort study (20), with the same results in Chinese (29, 30) and Japanese populations (31). In this study, we first evaluated the changes of circulating FGF21 in subjects with and without HP in T2DM patients, and we provided first clinical evidence showing that serum FGF21 levels were significantly increased in patients with T2DM than in healthy controls, and much higher FGF21 levels were observed in patients combined with HP. Serum FGF21 concentrations in these patients with T2DM were independently associated with HP in univariate and multivariate binary logistic regression analyses, similar results to other studies (29–31). There is a significant correlation between FGF21 and HP. However, the mechanisms of FGF21 involved in the development and progression of metabolic syndrome especially in HP plus T2DM as yet unexplored. One of the potential role of phosphatases or other molecules that may impair ERK pathway signaling on FGF21 remains to be determined (23). Further research is needed to investigate the mechanism of FGF21 on the development and progression of metabolic disorders in these T2DM individuals with HP.
Previous studies have shown that body shape is closely related to HP (32), and serum FGF21 level is higher in obese people (33). Similarly, in the current study, the body shape parameters, including body weight, waistline, neck circumference, BMI, ABSI, and WHR of T2DM patients with HP, were significantly higher than those without. The proportion of abdominal obesity in HP was also considerably increased, this may be related to the exacerbation of metabolic syndrome or diabetic chronic complications in these patients with T2DM. As expected, serum FGF21 levels were significantly associated with weight, waistline, BMI, ABSI, and abdominal obesity; the positive correlation remained highly significant when adjusted for age and T2DM duration. Interestingly, FGF21 appears to have similar mechanisms to lipid metabolism disorders in T2DM with HP. Correlation analysis showed that FGF21 was positively correlated with TG, negatively correlated with HDL-c, while no correlation with TC or LDL-c was found (Data not shown). Paradoxically, serum FGF21 in T2DM patients with HP was significantly higher than in control, which seems to contradict that the FGF21 can improve metabolic disorders. Many previous reports have confirmed that FGF21 is highly expressed in patients with chronic metabolic diseases such as obesity, diabetes, coronary heart disease, etc. The explanation of this paradox is that in these diseases, the human body has resistance to FGF21, and the sensitivity is reduced, which leads to the high compensatory increase of FGF21 in the circulation (34). FGF21 is primarily excreted by the kidney and is an independent risk factor for impaired kidney function. However, in the correlation analysis, FGF21 was not correlated with serum creatinine, blood urea nitrogen, serum uric acid, only negatively correlated with eGFR, after adjusting for age and sex, the correlation coefficients were reduced (Data not shown). This may be related to kidney function not being impaired in the early stage of diabetes. Moreover, it was reported that some kinds of anti-diabetic drugs have shown the potential effect the levels of FGF21. However, in the present study, no correlations were found between serum levels of FGF21 and anti-diabetic drugs use, possible confounding factors of anti-diabetic drugs that may hinder the obtained results were generally not considered.
Body shape parameters including weight, waistline, neck circumference, BMI, ABSI, WHR, and the proportion of abdominal obesity increased significantly. FGF21, waistline, age, HbA1c, and eGFR are independent risk factors for T2DM complicated with HP, suggesting that elderly individuals with abdominal obesity should pay more attention to weight control, not only blood-sugar control, to prevent the occurrence of HP, thus reduced the risk of cardiovascular death in patients with T2DM at high risk for cardiovascular events.
5. Limitations
This study has several limitations. First, the term “FGF21 resistance” during human obesity, in which circulating FGF21 levels are elevated, has been controversial partly due to difficulty in delineating the physiological and pharmacological mechanisms of FGF21 (10), weight loss and energy expenditure should be assessed to test chronic FGF21 sensitivity. However, FGF21 metabolism and signal transduction is a difficult challenge. Second, our present study is limited by the lack of measurements for coronary artery disease, in which FGF21 is significantly higher (35). Therefore, further studies are needed to elucidate the impact of coronary artery disease on the association of FGF21 and HP.
6. Conclusions
In this study, we have confirmed that the risk factors of diabetes complicated with HP are closely related to body shape, the frequency of chronic complications of diabetes such as HP is high, and an increased prevalence of abdominal obesity was observed with higher serum level of FGF21, in other words, FGF21 resistance occurs in obesity patients in T2DM with HP. The changes in FGF21 level in different populations showed the protective function of FGF21 on the circulatory system, such drugs targeting FGF21 for treating CVD and metabolic diseases will be an excellent boon for cardiovascular patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
This study involving human participants were reviewed and approved by Human Research Committee Affiliated Hospital of the Third Affiliated Hospital of Wenzhou Medical University (Ruian People’s Hospital). The patients/participants provided their written informed consent to participate in this study.
Author contributions
JG drafted the manuscript. HT, and WW have participated in data collection. ZD, JG, XP, and ZL performed the statistical analyses. YB, MW, XG, and NW have performed the laboratory measurements. ZL, HY, and LT have edited and revised the manuscript. All authors have read and approved the final manuscript submitted.
Funding
This research was supported by China National Funds for Distinguished Young Scientist (No: 81925004 to LZ.), National Natural Science Foundation of China (General program no: 81870317 to LZ.).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1168047/full#supplementary-material
References
1. Silveira Rossi JL, Barbalho SM, Reverete de Araujo R, Bechara MD, Sloan KP, Sloan LA. Metabolic syndrome and cardiovascular diseases: going beyond traditional risk factors. Diabetes Metab Res Rev. (2022) 38(3):e3502. doi: 10.1002/dmrr.3502
2. Liu YK, Ling S, Lui LMW, Ceban F, Vinberg M, Kessing LV, et al. Prevalence of type 2 diabetes mellitus, impaired fasting glucose, general obesity, and abdominal obesity in patients with bipolar disorder: a systematic review and meta-analysis. J Affect Disord. (2022) 300:449–61. doi: 10.1016/j.jad.2021.12.110
3. Bradshaw PT, Monda KL, Stevens J. Metabolic syndrome in healthy obese, overweight, and normal weight individuals: the atherosclerosis risk in communities study. Obesity (Silver Spring). (2013) 21(1):203–9. doi: 10.1002/oby.20248
4. de Chantemèle EJ B, Ali MI, Mintz J, Stepp DW. Obesity induced-insulin resistance causes endothelial dysfunction without reducing the vascular response to hindlimb ischemia. Basic Res Cardiol. (2009) 104(6):707–17. doi: 10.1007/s00395-009-0042-2
5. Jia G, Sowers JR. HP In diabetes: an update of basic mechanisms and clinical disease. Hypertension. (2021) 78(5):1197–205. doi: 10.1161/HPAHA.121.17981
6. La Sala L, Pontiroli AE. Prevention of diabetes and cardiovascular disease in obesity. Int J Mol Sci. (2020) 21(21):8178. doi: 10.3390/ijms21218178
7. Li S, Jia H, Liu Z, Wang N, Guo X, Cao M, et al. Fibroblast growth factor-21 as a novel metabolic factor for regulating thrombotic homeostasis. Sci Rep. (2022) 12(1):400. doi: 10.1038/s41598-021-00906-2
8. Keinicke H, Sun G, Mentzel CMJ, Fredholm M, John LM, Andersen B, et al. FGF21 Regulates hepatic metabolic pathways to improve steatosis and inflammation. Endocr Connect. (2020) 9(8):755–68. doi: 10.1530/EC-20-0152
9. Geng L, Lam KSL, Xu A. The therapeutic potential of FGF21 in metabolic diseases: from bench to clinic. Nat Rev Endocrinol. (2020) 16(11):654–67. doi: 10.1038/s41574-020-0386-0
10. Markan KR. Defining “FGF21 resistance” during obesity: controversy, criteria and unresolved questions. F1000Res. (2018) 7:289. doi: 10.12688/f1000research.14117.1
11. Stöhr O, Tao R, Miao J, Copps KD, White MF. Foxo1 suppresses Fgf21 during hepatic insulin resistance to impair peripheral glucose utilization and acute cold tolerance. Cell Rep. (2021) 34(12):108893. doi: 10.1016/j.celrep.2021.108893
12. Yang JP, Yang GR, Qin L, Wang XZ, Zhu GM, Li LM, et al. The role of exercise-regulated FGF21 in improving obesity-related metabolic diseases. Prog Biochem Biophys. (2022) 12(1):1–15. doi: 10.16476/j.pibb.2022.0333
13. Pan X, Shao Y, Wu F, Wang Y, Xiong R, Zheng J, et al. FGF21 Prevents angiotensin II-induced HP and vascular dysfunction by activation of ACE2/angiotensin-(1-7) axis in mice. Cell Metab. (2018) 27(6):1323–37. doi: 10.1016/j.cmet.2018.04.002
14. Lin ZF, Pan XB, Wu F, Zhang Y, Wang C. Application of FGF21 in the preparation of drugs for the treatment of HP and/or vascular injury caused by angiotensin II. People’s republic of China, CN108379555. (2018).
15. Tabari FS, Karimian A, Parsian H, Rameshknia V, Mahmoodpour A, Majidinia M, et al. The roles of FGF21 in atherosclerosis pathogenesis. Rev Endocr Metab Disord. (2019) 20(1):103–14. doi: 10.1007/s11154-019-09488-x
16. Dutchak PA, Katafuchi T, Bookout AL, Choi JH, Yu RT, Mangelsdorf DJ, et al. Fibroblast growth factor-21 regulates PPARγ activity and the antidiabetic actions of thiazolidinediones. Cell. (2012) 148(3):556–67. doi: 10.1016/j.cell.2011.11.062
17. He JL, Liu Y, Wu D, Qiao GF, Li BY. Perspective of FGF21, a new metabolic regulator in neurocontrol of circulation and pathological process of HP. J Nat sci. (2015) 1(5):1–5. doi: 10.1002/bit.25243
18. Tillman EJ, Rolph T. FGF21: an emerging therapeutic target for non-alcoholic steatohepatitis and related metabolic diseases. Front Endocrinol. (2020) 11:601290. doi: 10.3389/fendo.2020.601290
19. Grimaldi A, Heurtier A. Diagnostic criteria for type 2 diabetes. Rev Prat. (1999) 49(1):16–21. PMID:99267119926711
20. Li SM, Wang WF, Zhou LH, Ma L, An Y, Xu WJ, et al. Fibroblast growth factor 21 expressions in white blood cells and sera of patients with gestational diabetes mellitus during gestation and postpartum. Endocrine. (2015) 48(2):519–27. doi: 10.1007/s12020-014-0309-8
21. Megia A, Gil-Lluis P, Näf S, Ceperuelo-Mallafré V, Gonzalez-Clemente JM, Llauradó G, et al. Cord blood FGF21 in gestational diabetes and its relationship with postnatal growth. Acta Diabetol. (2015) 52(4):693–700. doi: 10.1007/s00592-014-0705-9
22. Nitert M D, Barrett HL, Kubala MH, Scholz Romero K, Denny KJ, Woodruff TM, et al. Increased placental expression of fibroblast growth factor 21 in gestational diabetes mellitus. J Clin Endocrinol Metab. (2014) 99(4):E591–8. doi: 10.1210/jc.2013-2581
23. Fisher FM, Chui PC, Antonellis PJ, Bina HA, Kharitonenkov A, Flier JS, et al. Obesity is a fibroblast growth factor 21 (FGF21)-resistant state. Diabetes. (2010) 59(11):2781–9. doi: 10.2337/db10-0193
24. Semba RD, Crasto C, Strait J, Sun K, Schaumberg DA, Ferrucci L. Elevated serum fibroblast growth factor 21 is associated with HP in community-dwelling adults. J Hum Hypertens. (2013) 27(6):397–9. doi: 10.1038/jhh.2012.52
25. Zhang L, Ebenezer PJ, Dasuri K, Fernandez-Kim SO, Francis J, Mariappan N, et al. Aging is associated with hypoxia and oxidative stress in adipose tissue: implications for adipose function. Am J Physiol Endocrinol Metab. (2011) 301(4):E599–607. doi: 10.1152/ajpendo.00059.2011
26. Ferrer-Curriu G, Redondo-Angulo I, Guitart-Mampel M, Ruperez C, Mas-Stachurska A, Sitges M, et al. Fibroblast growth factor-21 protects against fibrosis in hypertensive heart disease. J Pathol. (2019) 248(1):30–40. doi: 10.1002/path.5226
27. Liang Q, Zhong L, Zhang J, Wang Y, Bornstein SR, Triggle CR, et al. FGF21 Maintains glucose homeostasis by mediating the cross talk between liver and brain during prolonged fasting. Diabetes. (2014) 63(12):4064–75. doi: 10.2337/db14-0541
28. He JL, Zhao M, Xia JJ, Guan J, Liu Y, Wang LQ, et al. FGF21 Ameliorates the neurocontrol of blood pressure in the high fructose-drinking rats. Sci Rep. (2016) 6:29582. doi: 10.1038/srep29582
29. Li Y, Huang J, Jiang Z, Jiao Y, Wang H. FGF21 Inhibitor suppresses the proliferation and migration of human umbilical vein endothelial cells through the eNOS/PI3K/AKT pathway. Am J Transl Res. (2017) 9(12):5299–307. PMID: 2931248429312484
30. Zhang X, Hu Y, Zeng H, Li L, Zhao J, Zhao J, et al. Serum fibroblast growth factor 21 levels is associated with lower extremity atherosclerotic disease in Chinese female diabetic patients. Cardiovasc Diabetol. (2015) 14(32):1–9. doi: 10.1186/s12933-015-0190-7
31. Jin QR, Bando Y, Miyawaki K, Shikama Y, Kosugi C, Aki N, et al. Correlation of fibroblast growth factor 21 serum levels with metabolic parameters in Japanese subjects. J Med Invest. (2014) 61(1–2):28–34. doi: 10.2152/jmi.61.28
32. Calderón-García JF, Roncero-Martín R, Rico-Martín S, De Nicolás-Jiménez JM, López-Espuela F, Santano-Mogena E, et al. Effectiveness of Body Roundness index (BRI) and a Body Shape index (ABSI) in predicting HP: a systematic review and meta-analysis of observational studies. Int J Environ Res Public Health. (2021) 18(21):11607. doi: 10.3390/ijerph182111607
33. Frayling TM, Beaumont RN, Jones SE, Yaghootkar H, Tuke MA, Ruth KS, et al. A common allele in FGF21 associated with sugar intake is associated with body shape, lower total body-fat percentage, and higher blood pressure. Cell Rep. (2018) 23(2):327–36. doi: 10.1016/j.celrep.2018.03.070
34. Lin Z, Wu Z, Yin X, Liu Y, Yan X, Lin S, et al. Serum levels of FGF21 are increased in coronary heart disease patients and are independently associated with adverse lipid profile. PLoS One. (2010) 5(12):e15534. doi: 10.1371/journal.pone.0015534
Keywords: FGF21 resistance, body shape, waistline, type 2 diabetes mellitus, hypertension
Citation: Gan J, Duan Z, Tang L, Liu Z, Tian H, Wu M, Bi Y, Pan X, Wang W, Gao X, Wang N, Lin Z and Yang H (2023) Fibroblast growth factor 21 resistance is associated with body shape in patients with type 2 diabetes complicating hypertension. Front. Cardiovasc. Med. 10:1168047. doi: 10.3389/fcvm.2023.1168047
Received: 17 February 2023; Accepted: 24 May 2023;
Published: 22 June 2023.
Edited by:
Liqiu Yan, Guangdong Medical University, ChinaReviewed by:
Ma Shouyuan, Chinese PLA General Hospital, ChinaPongpan Tanajak, Apinop Wetchakam Hospital, Thailand
© 2023 Gan, Duan, Tang, Liu, Tian, Wu, Bi, Pan, Wang, Gao, Wang, Lin and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhuofeng Lin emh1b2ZlbmdsaW5Ad211LmVkdS5jbg== Hong Yang eWg3MTE1QDEyNi5jb20=
†These authors have contributed equally to this work
 Jing Gan1,†
Jing Gan1,† Zhuofeng Lin
Zhuofeng Lin Hong Yang
Hong Yang