
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CORRECTION article
Front. Cardiovasc. Med. , 09 March 2023
Sec. Cardiovascular Pharmacology and Drug Discovery
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1143652
This article is a correction to:
Anti-embolism devices therapy to improve the ICU mortality rate of patients with acute myocardial infarction and type II diabetes mellitus
 Xiaxuan Huang1,2,†
Xiaxuan Huang1,2,† Luming Zhang2,3,†
Luming Zhang2,3,† Mengyuan Xu3
Mengyuan Xu3 Shiqi Yuan1,2
Shiqi Yuan1,2 Yan Ye3
Yan Ye3 Tao Huang2
Tao Huang2 Haiyan Yin3*
Haiyan Yin3* Jun Lyu2,4*
Jun Lyu2,4*
A Corrigendum on
By Huang X, Zhang L, Xu M, Yuan S, Ye Y, Huang T, Yin H, Lyu J. (2022) Front. Cardiovasc. Med. 9:948924. doi: 10.3389/fcvm.2022.948924.
Error in Figure/Table
In the published article, there was an error in Table 2 “Analysis of the associations between AE-device therapy and outcomes.” as published. We did not update the latest table in the final correction process, which resulted in its inconsistency with the text in the two sections of the abstract and results. The latest data should be “Adjusted: ICU mortality: HR = 0.48, 95% CI = 0.24–0.96, P = 0.039; Day 28 mortality: HR = 0.50, 95% CI = 0.27–0.90, P = 0.021”, not “Adjusted: ICU mortality: HR = 0.46, 95% CI = 0.23–0.93, P = 0.030; Day 28 mortality: HR = 0.49, 95% CI = 0.27–0.89, P = 0.020” as in the uncorrected table. The corrected Table 2 appears below.
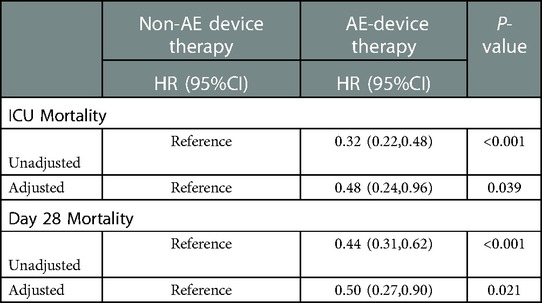
Table 2. Analysis of the associations between AE-device therapy and outcomes. Analysis of the associations between AE-device therapy and outcomes.
Analysis of the associations between AE-device therapy and outcomes. HR, hazard ratio; CI, confidence interval.
Models were derived from Cox proportional hazards regression models.
Model I was not adjusted for covariates.
Model II covariates were adjusted for Age, Weight, Ethnicity, Gender, First_careunit, APSIII, Anion_Gap, Heart_rate_mean, CKMB, WBC, Respiratory_rate_mean, Mbp_mean, SpO2_mean, Temperature_mean, Troponin_T_Max, Hemoglobin, Glucose_max, INR, Platelet, Potassium, Creatinine, Urea_Nitrogen, ALT, Urine_output, Lactate, Anti_Embolic, Antiplatelet, Anticoagulation, Congestive_heart_failue, Renal_disease, Malignant_cancer, Liver_disease, PCI, CABG, Ventilator, Vasopressor, CRRT, Peripheral_vascular_disease, Cerebrovascular_disease, Chronic_pulmonary_disease, Hypertensionid
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Text Correction
In the published article, there was an error. In the Abstract, the HR, 95% CI, and P-values corresponding to 28-day mortality are incorrectly written as those corresponding to ICU mortality and the HR, 95% CI, and P-values for ICU mortality are written as those corresponding to 28-day mortality and here should use HR instead of OR. A correction has been made to Abstract-“Results”, Line 3–6 of the first paragraph. This sentence previously stated:
“In the multivariate analysis, compared with no-AE device therapy, AE device therapy was a significant predictor of 28-day mortality (OR = 0.48, 95% CI = 0.24–0.96, P = 0.039) and ICU mortality (OR = 0.50, 95% CI = 0.27–0.90, P = 0.021).”
The corrected sentence appears below:
“In the multivariate analysis, compared with no-AE device therapy, AE device therapy was a significant predictor of ICU mortality (HR = 0.48, 95% CI = 0.24–0.96, P = 0.039) and 28-day mortality (HR = 0.50, 95% CI = 0.27–0.90, P = 0.021).”
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Text Correction
In the published article, there was an error. In the Results sections of this paper, the HR, 95% CI, and P-values corresponding to 28-day mortality are incorrectly written as those corresponding to ICU mortality and the HR, 95% CI, and P-values for ICU mortality are written as those corresponding to 28-day mortality, and here should use HR instead of OR. A correction has been made to Section of Results-“Cox Proportional-hazards Models”, Line 3–6 of the first paragraph. This sentence previously stated:
“As listed in Table 2, compared with no-AE device therapy, AE device therapy was a significant predictor of 28-day mortality (OR = 0.48, 95% CI = 0.24–0.96, P = 0.039) and ICU mortality (OR = 0.50, 95% CI = 0.27–0.90, P = 0.021) after adjusting for covariates.”
The corrected sentence appears below:
“As listed in Table 2, compared with no-AE device therapy, AE device therapy was a significant predictor of ICU mortality (HR = 0.48, 95% CI = 0.24–0.96, P = 0.039) and 28-day mortality(HR = 0.50, 95% CI = 0.27–0.90, P = 0.021) after adjusting for covariates.”
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Keywords: anti-embolic therapy, acute myocardial infarction, type II diabetes mellitus, mortality, ICU
Citation: Huang X, Zhang L, Xu M, Yuan S, Ye Y, Huang T, Yin H and Lyu J (2023) Corrigendum: Anti-embolism devices therapy to improve the ICU mortality rate of patients with acute myocardial infarction and type II diabetes mellitus. Front. Cardiovasc. Med. 10:1143652. doi: 10.3389/fcvm.2023.1143652
Received: 13 January 2023; Accepted: 16 February 2023;
Published: 9 March 2023.
Approved by: Xiaofeng Yang, Temple University, United States
© 2023 Huang, Zhang, Xu, Yuan, Ye, Huang, Yin and Lyu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haiyan Yin WWluaGFpeWFuMTg2N0AxMjYuY29t Jun Lyu bHl1anVuMjAyMEBqbnUuZWR1LmNu
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Cardiovascular Pharmacology and Drug Discovery, a section of the journal Frontiers in Cardiovascular Medicine
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.