
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 02 August 2023
Sec. Cardiovascular Epidemiology and Prevention
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1127320
 Gulnur Zhakhina1
Gulnur Zhakhina1 Abduzhappar Gaipov1,2*
Abduzhappar Gaipov1,2* Alessandro Salustri1
Alessandro Salustri1 Arnur Gusmanov1
Arnur Gusmanov1 Yesbolat Sakko1
Yesbolat Sakko1 Sauran Yerdessov1
Sauran Yerdessov1 Makhabbat Bekbossynova3
Makhabbat Bekbossynova3 Anara Abbay1
Anara Abbay1 Antonio Sarria-Santamera1
Antonio Sarria-Santamera1 Oguz Akbilgic4
Oguz Akbilgic4
Background: Cardiovascular diseases contribute to premature mortality globally, resulting in substantial social and economic burdens. The Global Burden of Disease (GBD) Study reported that in 2019 alone, heart attack and strokes accounted for the deaths of 18.6 million individuals. Ischemic heart diseases, including acute myocardial infarction (AMI), accounted for 182 million disability-adjusted life years (DALYs) and it is leading cause of death worldwide.
Aim: The aim of this study is to present the burden of AMI in Kazakhstan and describe the outcome of hospitalized patients.
Methods: The data of 79,172 people admitted to hospital with ICD-10 diagnosis I21 between 2014 and 2019 was derived from the Unified National Electronic Health System and retrospectively analyzed.
Results: The majority of the cohort (53,285, 67%) were men, with an average age of 63 (±12) years, predominantly of Kazakh (38,057, 48%) and Russian (24,583, 31%) ethnicities. Hypertension was the most common comorbidity (61,972, 78%). In males, a sharp increase in incidence is present after 40 years, while for females, the morbidity increases gradually after 55. Throughout the observation period, all-cause mortality rose from 101 to 210 people per million population (PMP). In 2019, AMI account for 169,862 DALYs in Kazakhstan, with a significant proportion (79%) attributed to years of life lost due to premature death (YLDs). Approximately half of disease burden due to AMI (80,794 DALYs) was in age group 55–69 years. Although incidence is higher for men, they have better survival rates than women. In terms of revascularization procedures, coronary artery bypass grafting yielded higher survival rates compared to percutaneous coronary intervention (86.3% and 80.9% respectively) during the 5-year follow-up.
Conclusion: This research evaluated the burden and disability-adjusted life years of AMI in Kazakhstan, the largest Central Asian country. The results show that more effective disease management systems and preventive measures at earlier ages are needed.
Cardiovascular diseases (CVDs) continue to be one of the leading causes of premature mortality worldwide. According to the Global Burden of Disease (GBD) Study, in 2019, there were approximately 523 million prevalent cases of CVDs, constituting approximately 7% of the world population (1). Furthermore, statistics from the World Health Organization (WHO) indicate that more than three-quarters of cardiovascular disease-related deaths occur in low- and middle-income countries (2). While high-income countries have witnessed a decline in the incidence of acute myocardial infarction (AMI) and case-fatality rates associated to AMI (3), the increasing life expectancy, population growth, and aging population contribute to a heavier disease burden.
The quantifiable measure of fatal and non-fatal health consequences of diseases and injuries is a disability-adjusted life year (DALY). According to the data of the GBD Study, ischemic heart diseases accounted for 714,104 DALYs in Kazakhstan between 1990 and 2017 (4). Given these considerations, we aimed to assess the epidemiology of AMI in Kazakhstan, the largest Central Asian country.
The data for this retrospective study obtained from the Unified National Electronic Health System (UNEHS) for the period of 2014–2019. Detailed information on the UNEHS and its databases can be found elsewhere (5). Patients included in the study were identified based on the International Classification of Diseases (ICD) codes, specifically those with the ICD-10 code of I21 (acute myocardial infarction) as the primary diagnosis. Additional information regarding the diagnostic criteria and protocols for patient management can be found in the Supplementary Table S1 (6).
From the initial pool of 162,099 records related to AMI, after thorough data cleaning and management, a cohort of 79,172 people with unique RPN IDs remained for the analysis. Only information pertaining to the first-ever occurrence of AMI during the observation period was considered for analysis. Detailed information on cohort setup is presented in Figure 1.
Population numbers were obtained from the Statistics Committee of the Ministry of National Economy of the Republic of Kazakhstan. In 2021, the population of Kazakhstan was over 18 million people. Considering the gender composition, the percentage of males in the population (48.5%) was slightly lower than that of females. The detailed information on population size for each gender and age group is given in Supplementary Table S2.
The analysis included information on the date of birth, gender, ethnicity, living area, social status, date of hospital admission, date of hospital discharge, and date of death, if applicable. The birth date and death date were obtained from the Population Registry. Age was categorized as following: (1) below 34 years old, (2) 35–50 years old, (3) 51–70 years old, and (4) above 70 years old. In Kazakhstan, there are over 120 nationalities, with a significant prevalence of Kazakh followed by Russians and various other minority groups. Therefore, ethnicity was classified into Kazakhs (n = 38,397), Russians (n = 24,897), and others (n = 16,707).
Two primary revascularization procedures were examined in this study: coronary artery bypass graft surgery (CABG) (ICD-9 codes 36.10, 36.11, 36.12, 36.13, 36.14, 36.15, 36.16) and percutaneous coronary intervention (PCI) (ICD-9 codes 00.66, 36.01, 36.02, 36.06 and 36.07). The information on comorbidities such as cerebrovascular accident (CVA) (7), diabetes mellitus (DM) (8), hypertension (9), and chronic kidney disease (CKD) was collected by merging the databases using unique RPN IDs. All comorbid conditions were defined based on their respective ICD-10 codes.
The study assessed the incidence, all-cause mortality, 30-day mortality, and in-hospital mortality in the cohort based on the hospital admission and discharge status of patients. The incidence rate (IR) represents the rate of first-ever events. Death occurring at any time during the observation period was accounted as all-cause death. The rates were calculated by dividing the absolute numbers by the total general population size of the general population at the end of each year. For the survival analysis, the start date was defined as the first day of the initial admission, and the follow-up period extended until December 31 of 2019, or until the day of death, if it occurred.
DALY is a measure that combines the years of life lost due to premature death (YLLs) and years lived with disability (YLDs). The calculation follows the WHO methods for the global burden of disease estimates (10). The formula uses a simplified version of DALY, without age-weighting and time discounting.
The overall YLL was determined by summing the years of life lost for each age category group, ranging from 20 to 24 years old to 85+ years old. The number of deaths in each group was multiplied by the life expectancy at the age of death. According to the GBD 2010 reference life table, the life expectancy at birth for both males and females was 86.0 years (10).
The calculation of YLD follows a prevalence-based approach, as used by WHO and GBD 2010. The formula for YLD involves multiplying the prevalence of a condition by its corresponding disability weight (DW). In the case of AMI, the DW was found to be 0.432 during the first two days after the infarction episode and 0.074 from days 3 to 28 (10). The prevalence of AMI cases from 2014 to 2019 was multiplied by each DW, and the results were summed to obtain overall years lived with disability.
All characteristics in the study are presented as categorical variables. Incidence and all-cause mortality rates, based on hospital admission and discharge status, were evaluated as both absolute numbers and rates per 1,000,000 population for each year of the observation period. Crude survival was demonstrated using Kaplan-Meier estimates, and the significance of difference was assessed using Log-rank tests.
Cox regression analyses were conducted after verifying the corresponding assumptions. Crude and adjusted hazard ratios were reported. Model 1 adjusted HR for socio-demographic factors such as age category, gender, and ethnicity. Model 2 included socio-demographic variables and comorbidities such as CVA, essential hypertension, DM, and CKD. Model 3 accounted for all the abovementioned factors, as well as revascularization strategies (CABG and PCI). The significance level was set at 0.05. All statistical analyses were performed using STATA 16.1.
The study utilized secondary data derived from the UNEHS. Since patients were not directly involved in the study, the requirement for informed consent from study participants was waived by the Nazarbayev University Institutional Review Ethics Committee (NU-IREC 490/18112021).
The baseline characteristics of the cohort are presented in Table 1. During 2014–2019, a total of 79,172 people were admitted to the hospital due to acute myocardial infarction, with 33% being women and 67% men. Among the cohort, 68,628 (86%) were older than 50, and 42,052 (53%) were retired. Concurrent CVA, DM, hypertension, and CKD were present in 5%, 17%, 78%, and 12% of the cohort, respectively. The mortality rate per 100,000 patient-years in urban areas was calculated to be 20.4 [95% CI: 20.1–20.8], while in rural areas the corresponding rate was 17.4 [95% CI: 17.0–17.9], p < 0.001 (Table 1).
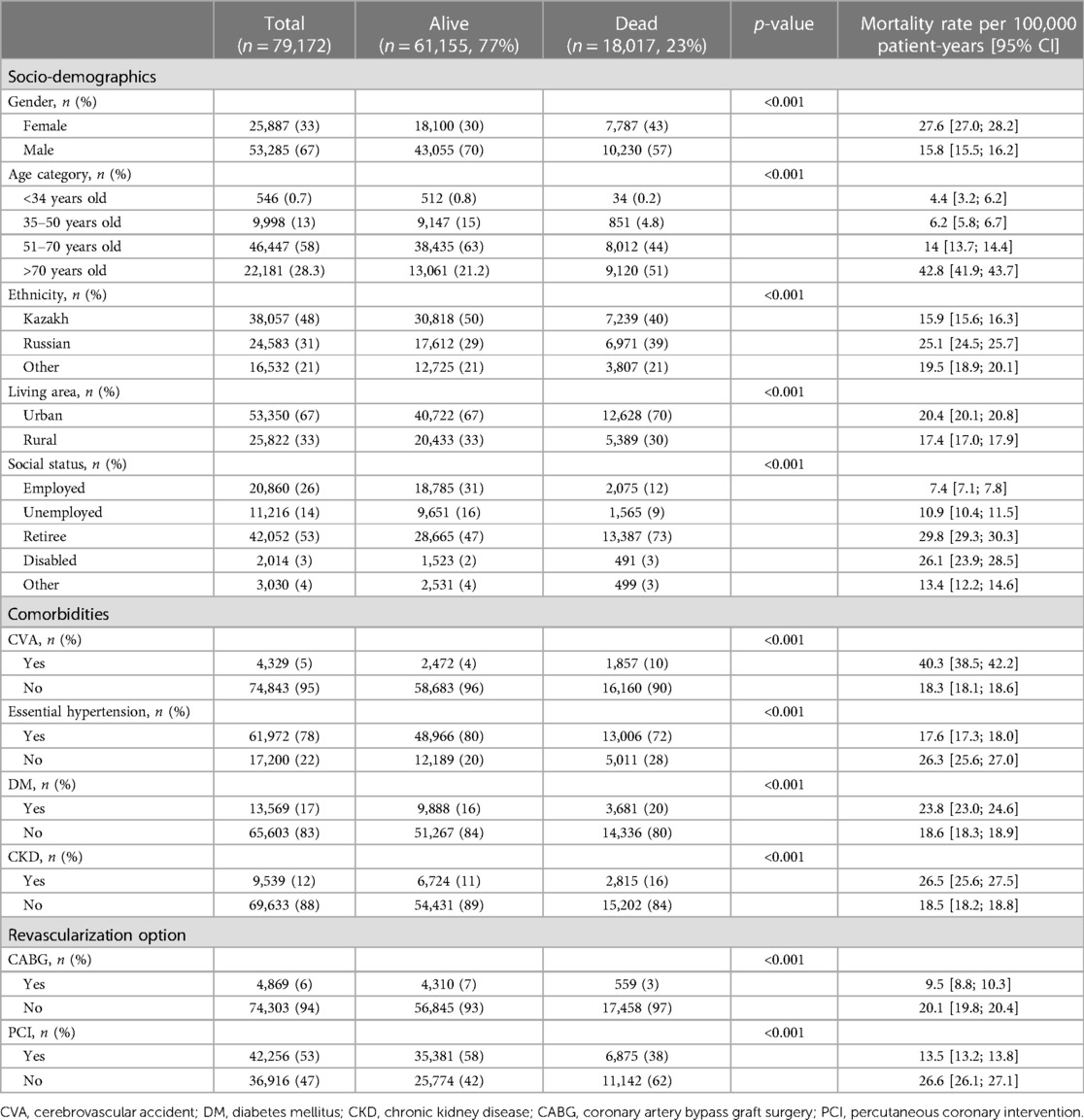
Table 1. Socio-demographic and medical characteristics of patients, who had MI between 2014 and 2019.
During the hospital stay, 4,869 (6%) patients underwent CABG, while 42,256 (53%) had PCI (Table 1). The frequency of CABG per 1,000 patients was significantly lower compared to PCI during the observation period (Figure 2). Both interventions showed a gradual increase in rates from 2014 to 2019: CABG increased from 46 to 73 per 1,000 patients, while the rate for PCI escalated from 447 to 594 per 1,000 patients. Throughout the observation period, there were 5,956 (7.5%) in-hospital deaths and 7,121 (9%) deaths within 30 days.
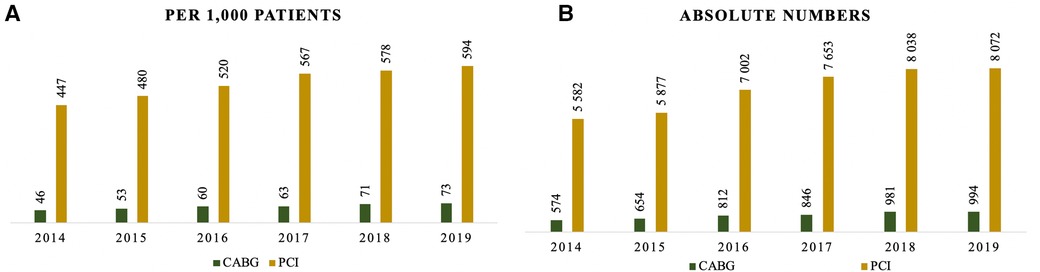
Figure 2. Frequency of cardiovascular surgeries by years: (A) per 1,000 patients; (B) absolute numbers.
The age and sex-specific incidence rate (IR) among MI patients over the observation period is presented in Figure 3. According to the diagram, the IR among males rises dramatically till 60–65 years old; while for females, the growth is more gradual, peaking at 75–80 years of age. The IR based on hospital admission and discharge status did not change significantly over the observation period: 727 people per million population (PMP) in 2014 and 739 PMP in 2019 (Figure 4A). However, the all-cause mortality rate notably increased from 101 PMP in 2014 to 210 PMP in 2019 (Figure 4B).
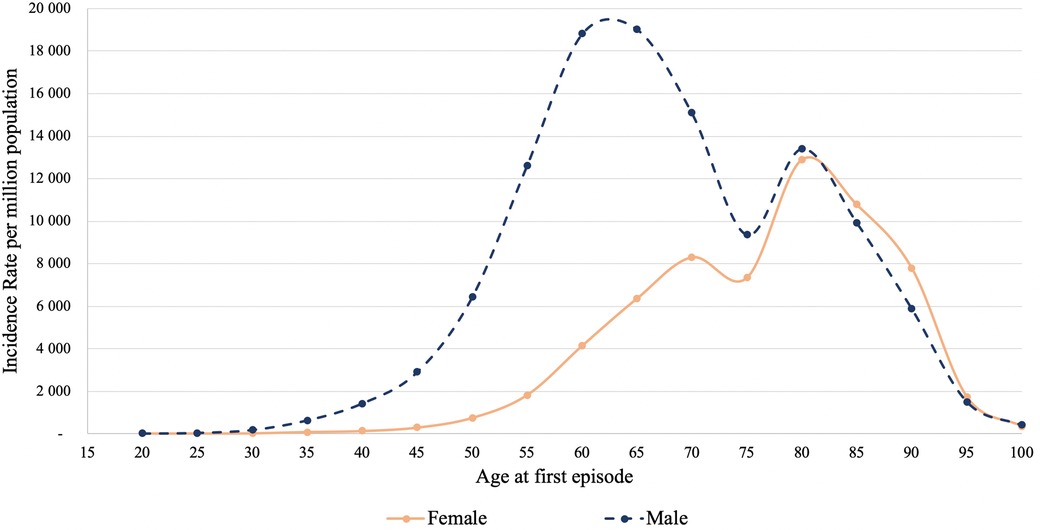
Figure 3. Age and sex-specific incidence rate of MI per 1,000,000 population for the years 2014–2019.
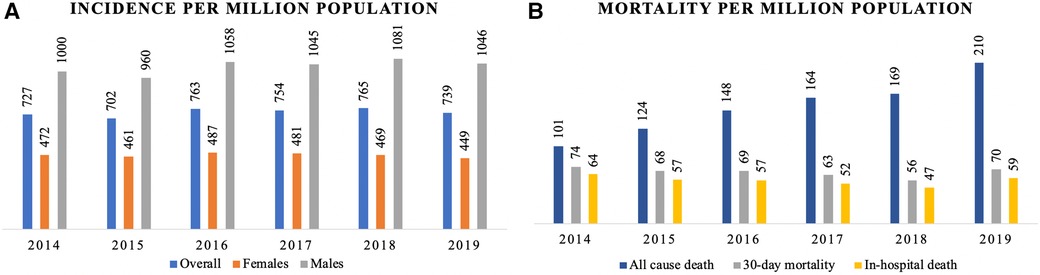
Figure 4. Burden of MI in Kazakhstan by years based on admission and discharge status: (A) incidence (overall, females, males) per 1,000,000 population; (B) mortality (all-cause, 30-day and in-hospital) per 1,000,000 population.
The life expectancy, years of life lost due to premature death (YLL), years lived with disability (YLD), and disability-adjusted life years (DALY) by age groups are presented in Table 2. In 2019, AMI accounted for 169,862.4 DALYs in Kazakhstan. The weight of premature death is significantly higher than the time lost due to ill health: 134,260.4 years of life lost (YLLs) vs. 35,602 YLDs, respectively. The highest burden of MI was observed in the 60–69-year-old age group, with an overall burden of 56,216.3 DALYs. There is a higher proportional contribution of YLLs to DALYs in all age groups, with the overall contribution being 79%. The highest burden of premature death and disability-adjusted life years is observed in the age group of 55–69 years, with 80,793.8 YLLs and 17,878.5 YLDs, respectively.
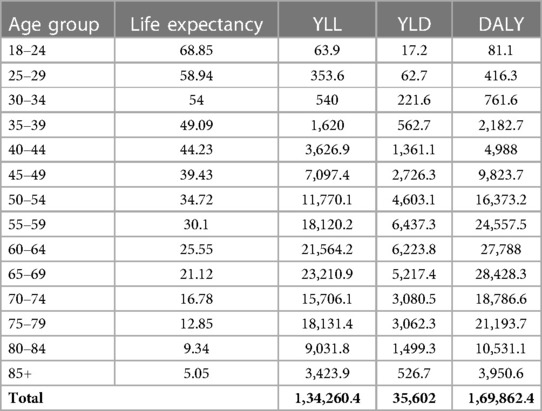
Table 2. Life expectancy, years of life lost due to premature death (YLLs) and years lived with disability (YLDs), and disability-adjusted life years (DALYs) by age groups in Kazakhstan over 2014–2019.
According to the survival analysis of AMI patients, males have better survival compared to females: 78.3% vs. 66.7% with a log-rank test p-value of <0.001 (Figure 5A). The crude 5-year survival of patients with a history of stroke is remarkably lower compared to patients without a history of stroke (51.8% and 75.9% respectively, p < 0.001) (Figure 5B). People without diabetes have higher survival rates compared to those with diabetes (75.6% and 68.8% respectively, p < 0.001) (Figure 5C). CKD is associated with decreased survival rate, showing a crude probability of 65.8% (Figure 5E). Opposite tendency is related to hypertension (Figure 5D).
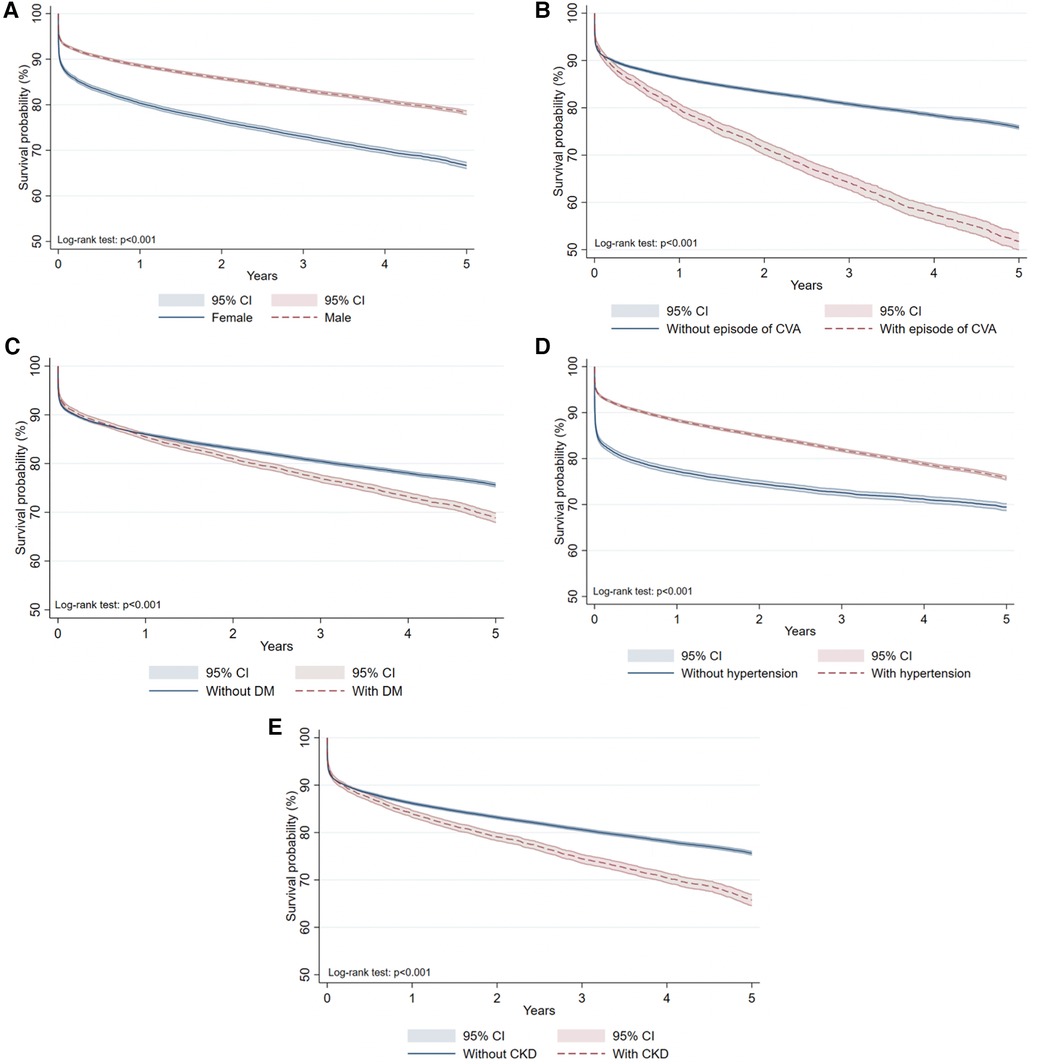
Figure 5. Kaplan-Meier survival curves due to all-cause mortality based on discharge status: (A) by gender; (B) by the history of CVA; (C) by DM comorbidity; (D) by hypertension comorbidity; (E) by CKD.
According to the Cox regression analysis in Table 3, males have a substantially lower risk of death [HR = 0.59, 95% CI: 0.57–0.61]; however, after adjustment for age and ethnicity, the difference becomes negligible [HR = 0.92, 95% CI: 0.89–0.94]. After adjustment for all sociodemographic factors, comorbidities, and revascularization procedures, Russians had a 37% higher risk of death compared to Kazakhs [HR = 1.37, 95% CI: 1.33–1.42]. The adjusted model showed that a history of stroke was associated with 84% [HR = 1.84, 95% CI: 1.75–1.93], diabetes with 29% [HR = 1.29, 95% CI: 1.24–1.34], and CKD with 45% [HR = 1.45, 95% CI: 1.39–1.51] higher risk of death in AMI patients. On the other hand, results show that hypertension was associated with 43% [HR = 0.57, 95% CI: 0.55–0.58] lower risk of death in the cohort. In terms of revascularization procedures, patients who underwent CABG had a lower risk of death by 57% [HR = 0.43, 95% CI: 0.39–0.47], and patients who underwent PCI had a lower risk of death by 44% [HR = 0.56, 95% CI: 0.54–0.57].
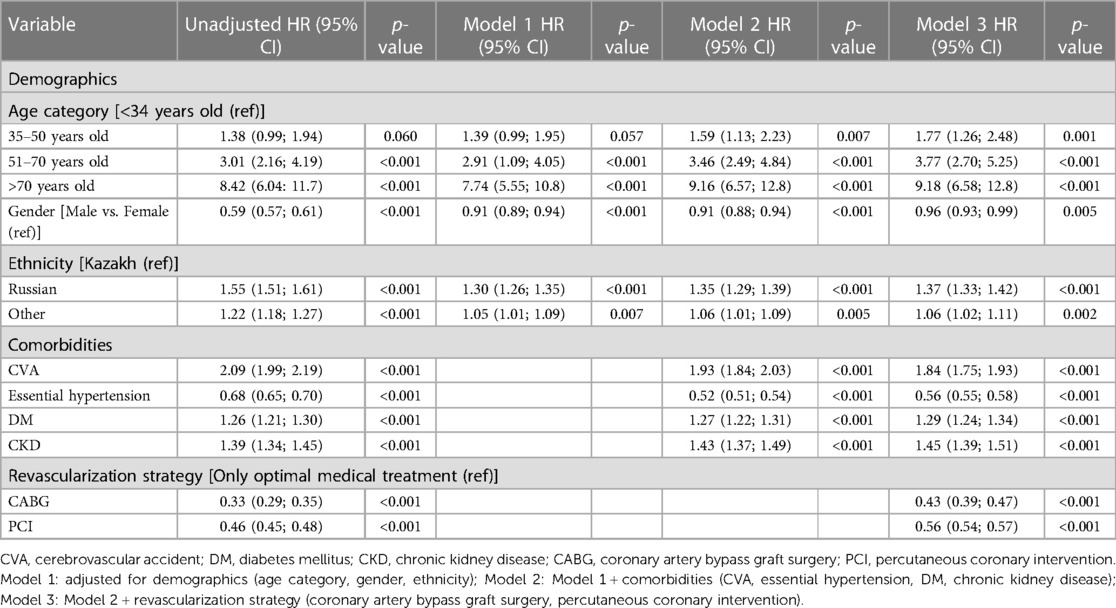
Table 3. Association between socio-demographic and medical parameters and all-cause mortality rates from MI for the years 2014–2019.
This study evaluates the burden of AMI based on hospitalization records between 2014 and 2019 in Kazakhstan. In the cohort, the female-to-male ratio was 1:3, with the majority being Kazakhs, older than 50, and living in an urban area. A considerable proportion of the patients had hypertension, whereas stroke, diabetes, and CKD were not commonly observed. The incidence rate, 30-day death rate, and in-hospital death rate per million population did not change remarkably over the observation period, while all-cause mortality doubled. However, crude mortality among AMI patients decreased significantly during the follow-up time.
In Kazakhstan, between 2014 and 2019, the incidence rate of hospital admissions for AMI did not change significantly. In the Norwegian study based on national data from 2001 to 2014, researchers found that AMI rates declined by 2.7% per year over the observation period (11). It is important to note that the data used in this study only includes hospital admission and discharge reports, and therefore, it may not reflect the true incidence rate in the general population of Kazakhstan. It is worth considering that between 2011 and 2019, Kazakhstan implemented two State Programs for the Development of Healthcare, which placed significant emphasis on health education and promotion among the population (12, 13). The campaigns could have influenced the level of awareness about AMI in the community and led to improvements in the disease management system.
According to hospital admission records, the incidence of AMI is significantly higher for men. This observation is consistent with findings from a Chinese prospective, nationwide, multicenter observational study conducted on patients diagnosed with AMI (14). Women, on the other hand, tend to be older at the time of the first AMI admission, and the incidence gradually increases after the age of 50, while for men, it rises after the age of 35. Similar patterns of age and sex-specific AMI occurrence rates have been observed in epidemiologic studies.
The lower risk of AMI in young women can be attributed to their pre- and peri-menopausal state and higher estrogen levels (15). Known risk factors for cardiovascular disease include family history of coronary diseases, smoking, diabetes, and obesity. The difference in age at which the first AMI occurs between males and females can be explained by variations in the occurrence of these factors over time between the two groups or the presence of healthier lifestyle patterns in women (16). Moreover, during the fertile period, high estrogen levels in females significantly reduce the risk of cardiovascular diseases compared to males of the same age (17).
This study identified two peaks of incidence for men. The first peak occurring at a younger age is consistent with findings from other research (18). However, the presence of the second peak for males at an older age is not observed in the existing literature. Further investigation and specific studies are required to address this issue and explore possible explanations. Nonetheless, these findings have implications for improving the recognition and timely management of infarction both in men and women. Implementing this knowledge can inform health policy decisions in this regard.
Age alone does not appear to be the primary reason for the high morbidity of AMI. As individuals age, they develop various comorbidities. This study specifically examined the impact of CVA, hypertension, DM, and CKD on the outcome of AMI patients. Stroke and AMI share common risk factors and are closely related in terms of their pathophysiology (19). The prevalence of CVA in this study cohort was found to be low. This finding is consistent with other studies that indicate a low likelihood of myocardial infarction occurring after a stroke (19). The lower occurrence of AMI after stroke can be attributed to preventive drug therapy administered following the initial cardiovascular event (20). However, individuals who experience CVD following a stroke have a lower survival probability (21), as observed in this study.
Literature data regarding the association between essential hypertension and AMI are consistent. Elevated systolic and diastolic blood pressure contributes to the damage of blood vessels, increasing the risk of cardiovascular diseases. While essential hypertension is an independent risk factor for AMI, its combination with older age further elevates the morbidity of the illness (22). It is important to note that factors not considered in this research may have confounding effects and could potentially explain the finding of lower mortality rates among individuals with essential hypertension. Additionally, the inclusion of information on CVDs and CKDs, which are closely linked to hypertension, may influence the true effect of hypertension on AMI patients.
A cross-sectional study conducted among the Kazakhstani population revealed that a majority of hypertensive individuals were taking antihypertensive medications (23), indicating a potentially high rate of blood pressure control. The existing literature consistently highlights the strong association between hypertension and adverse outcomes (22). Further research should focus on investigating the impact of medication, lifestyle changes, and the reduction of modifiable risk factors reduction in relation to hypertension and its outcomes.
Diabetes mellitus is recognized as another risk factor for AMI. The results of this study are in line with previous research, indicating higher mortality rates among diabetic patients (24). Interestingly, after adjusting for all socio-demographic factors, the mortality rate for diabetic patients was found to be less than 30%, which contrasts with earlier research conducted before 2010 that reported a probability of adverse outcomes exceeding 70% (25). The advancements in diagnostic tools, medical treatments, and healthcare management systems may have played a role in improving the life of individuals with diabetes.
One additional comorbidity examined in this research is CKD at any stage. The prevalence of renal dysfunction in the cohort was found to be 12%, which aligns with findings from other studies that have utilized large health administrative datasets (26). Patients with CKD are known to have an increased risk of atherosclerosis and higher mortality rates following acute myocardial infarction. Due to the kidney dysfunction and the heightened likelihood of infections or organ failure, AMI patients with CKD may not receive invasive treatments such as CABG or PCI (27). Consequently, the long-term survival rates of AMI patients with CKD tend to be low. It is important to conduct separate studies to investigate the efficacy of invasive therapies specifically for this high-risk group, in order to enhance the healthcare management system.
The results of this study indicate a significantly higher mortality rate among Russians compared to Kazakhs. However, it is challenging to attribute this difference in survival solely to race. Other social determinants, including education level, employment status, socioeconomic situation, and cultural disparities in lifestyle and dietary habits, should be taken into account. In the population-based study conducted by Sharygin and Gulliot, it was shown that Russians have higher adult mortality rates than Central Asians, even after adjusting for socioeconomic status (28). The mortality gap in that study was attributed to an increased risk of death associated with alcohol consumption.
The development of cardiovascular services in Kazakhstan was relatively delayed, with significant advancements occurring in the 2010s (12, 13). Throughout the observation period, there was a threefold increase in human resources and technical equipment, which positively impacted the survival of AMI patients. In terms of mortality in Kazakhstan, it is noteworthy that the country has implemented a national guideline for the diagnosis and treatment of acute myocardial infarction (AMI) (6). This guideline aligns with the diagnostic algorithms endorsed by the international cardiology communities (29, 30). Early diagnosis and intervention of AMI cases are crucial for improving outcomes, and the implementation of early screening programs holds great significance. These initiatives aim to enhance the timely identification and management of AMI, ultimately leading to improved patient outcomes and reduced mortality rates. Despite improvements in the disease management system over the observation period, it is important to consider that higher life expectancy and an aging population could contribute to increased mortality rates from AMI in the later years.
Myocardial infarction is an acute disease that carries an elevated risk of cardiac dysfunction for approximately a month (31). The cardiovascular system is primarily damaged in the first two days after initial symptoms, resulting in disability, and the rest of the month is needed to restore normal cardiac functioning (32). Therefore, the contribution of years lived with a disability to the total DALY is low. It is not appropriate to compare the burden of AMI in terms of disability-adjusted life years between Kazakhstan and other countries without proper country-level adjustments on population size, cohort set-up, and observation period. In this study, DALYs for 50–69 years old people were twice as high as those individuals older than 70. In comparison, a Portuguese study reported a higher DALY burden for the latter group. This finding is significant considering that the proportion of elderly individuals and the median age are higher in Portugal (33, 34).
The results of this study revealed a significant decrease in the crude mortality rate among AMI patients over the observation period. This finding is consistent with the impact of Kazakhstani healthcare programs (12, 13) that have focused on improving the management of cardiovascular diseases. These programs have prioritized the development of heart and stroke centers, reducing CV mortality, and enhancing cardiovascular services (35). This research primarily focused on two revascularization interventions, namely PCI and CABG, which aim to restore adequate blood supply through the cardiovascular system. Given that the development of cardiovascular services in Kazakhstan is a relatively recent phenomenon, there have been variations in the accessibility of these procedures and the overall management of AMI patients. Consequently, the frequency of PCI was notably higher compared to CABG. Although the unadjusted model did not demonstrate a significant difference between the two, after adjusting for sociodemographic factors and comorbidities, CABG proved to be more effective in reducing mortality.
Previous studies have elucidated this finding by highlighting that myocardial infarction is often associated with non-flow-limiting stenosis, which is effectively addressed by CABG (36), whereas PCI is more suitable for treating flow-vessel occlusions (37). Furthermore, a recent systematic review evaluated randomized clinical trials comparing these interventions and concluded that CABG provides benefits in terms of protection against new myocardial infarctions (38). However, considering the difference in medical facility levels depending on hospital location, patient characteristics, and access to revascularization, intervention strategies should be examined separately to accurately assess their impact on reducing mortality rates.
The evaluation of epidemiology and the burden of disease in this study has several advantages. Firstly, it provides a comprehensive overview of acute myocardial infarction in Kazakhstan. Large cohort studies assessing the incidence, mortality, and disability-adjusted life years of AMI using nationwide databases in Central Asian countries are scarce, making these findings particularly valuable. They can contribute to the development of improved protocols and strategies for managing the disease in healthcare settings, taking into account socio-demographic factors and cultural differences. In addition, it may increase community awareness campaigns and raise concerns about a healthy lifestyle to avoid early AMI morbidity. Finally, the results of this study may stimulate further research on the cost-effectiveness of surgical interventions and the management of AMI management to evaluate the economic burden of disease.
Despite the aforementioned advantages, there are several limitations. First of all, the use of hospitalization records only captures a subset of AMI cases, and it does not account for pre-hospital morbidity and mortality. This means that the true incidence and mortality rates of AMI may be underestimated since cases occurring outside of the hospital setting are not included. This is particularly relevant for the older age groups, where a significant proportion of AMI cases may not result in hospitalization. Additionally, the database used in this study does not provide information on important factors such as tobacco use, blood cholesterol or triglyceride levels, congestive heart failure, arrhythmias, obesity, family history of heart attack, stress levels, illicit drug use, and autoimmune conditions, which are known to be comorbidities that can impact survival in AMI patients. The absence of these data limits the ability to fully understand the factors influencing outcomes in this population. Furthermore, errors during disease coding are possible, which could introduce inaccuracies in the analysis. The lack of cause of death information is also a limitation, as it restricts the ability to calculate cause-specific mortality rates and understand the specific factors contributing to mortality in AMI cases. These limitations should be taken into account when interpreting the findings of the study and further research should aim to address these gaps to provide a more comprehensive understanding of AMI in the population.
This is the first study to evaluate the incidence, mortality, and disability-adjusted life years of AMI in Kazakhstan. The current study retrospectively analyzed nationwide admission and discharge data of myocardial infarction cases between 2014 and 2019. The incidence and mortality rates per million population did not change significantly over the observation period. However, there was a noticeable decrease in the crude mortality rate among AMI patients during the follow-up period, indicating effective management of hospitalized patients. Further educational campaigns targeting disease prevention and reduction of risk factors are warranted.
The data analyzed in this study is subject to the following licenses/restrictions: The data that support the findings of this study are available from the Republican Center for Electronic Health of the Ministry of Health of the Republic of Kazakhstan but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author, Gaipov A., upon reasonable request and with permission of the Ministry of Health of the Republic of Kazakhstan. Requests to access these datasets should be directed to Abduzhappar Gaipov,YWJkdXpoYXBwYXIuZ2FpcG92QG51LmVkdS5reg==.
The study was approved by the Nazarbayev University Institutional Review Ethics Committee (NU-IREC 490/18112021), with exemption from informed consent.
All authors approved the final version of manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GZ analyzed and interpreted data and drafted the article; AbG and AlS involved in conception and design of study and drafted the article; ArG involved in interpretation of data and drafting the article; YS and SY involved in analysis of data and article drafting; MB, AA, and OA involved in acquisition of data and revision of article; AnS involved in conception and design of study and revised the article. All authors contributed to the article and approved the submitted version.
This study was supported by grants from the Nazarbayev University Faculty Development Research Grant Program FDCRGP 2023–2025 (Funder Project Reference: 20122022FD4104, title: In-depth epidemiology and modeling of the 10-year trends of cardiovascular diseases and their complications in Kazakhstan using aggregated big data from the Unified National Electronic Healthcare System). The funder had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript. AG is a PI of the project.
We thank all staff from the Republican Center of Electronic Healthcare for providing data and consultancy.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1127320/full#supplementary-material
1. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010
2. WHO. Cardiovascular diseases (CVDs). (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (Cited 2022 March 26).
3. Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, et al.. European cardiovascular disease statistics 2017. Brussels: European Heart Network (2017).
4. Lui M, Safiri S, Mereke A, Davletov K, Mebonia N, Myrkassymova A, et al. Burden of ischemic heart disease in central Asian countries, 1990–2017. Int J Cardiol Heart Vasc. (2021) 33:100726. doi: 10.1016/j.ijcha.2021.100726
5. Gusmanov A, Zhakhina G, Yerdessov S, Sakko Y, Mussina K, Alimbayev A, et al. Review of the research databases on population-based registries of unified electronic healthcare system of Kazakhstan (UNEHS): possibilities and limitations for epidemiological research and real-world evidence. Int J Med Inf. (2023) 170:104950. doi: 10.1016/j.ijmedinf.2022.104950
6. Joint Commission for the Quality of Medical Services of the Ministry of Health of the Republic of Kazakhstan. Myocardial infarction with ST elevation (2017). Available at: https://diseases.medelement.com/disease/инфаркт-миокарда-с-подъемом-сегмента-st/15487 (Accessed May 24, 2023).
7. Zhakhina G, Zhalmagambetov B, Gusmanov A, Sakko Y, Yerdessov S, Matmusaeva E, et al. Incidence and mortality rates of strokes in Kazakhstan in 2014–2019. Sci Rep. (2022) 12(1):1–12. doi: 10.1038/s41598-022-20302-8
8. Gaipov A, Galiyeva D, Gusmanov A, Sakko Y, Issanov A, Atageldiyeva K, et al. Epidemiology of type 1 and type 2 diabetes mellitus in Kazakhstan: data from unified national electronic health system 2014–2019. BMC Endocr Disord. (2022) 22:275. doi: 10.1186/s12902-022-01200-6
9. Yerdessov S, Kadyrzhanuly K, Sakko Y, Gusmanov A, Zhakhina G, Galiyeva D, et al. Epidemiology of arterial hypertension in Kazakhstan: data from unified nationwide electronic healthcare system 2014–2019. J Cardiovasc Dev Dis. (2022) 9(2):52. doi: 10.3390/jcdd9020052
10. WHO. WHO methods and data sources for global burden of disease estimates 2000–2019. Geneva: Department of Data and Analytics, Division of Data, Analytics and Delivery for Impact WHO (2020).
11. Sulo G, Igland J, Vollset SE, Ebbing M, Egeland GM, Ariansen I, et al. Trends in incident acute myocardial infarction in Norway: an updated analysis to 2014 using national data from the CVDNOR project. Eur J Prev Cardiol. (2018) 25(10):1031–9. doi: 10.1177/2047487318780033
12. On approval of the state health development program of the Republic of Kazakhstan “Salamatty Kazakhstan” for 2011–2015. In: Kazakhstan MoJotRo, editor. https://adilet.zan.kz/rus/docs/U10000011132010.
13. On approval of the state health development program of the Republic of Kazakhstan “Densaulyk” for 2016–2019. In: Kazakhstan MoJotRo, editor. https://adilet.zan.kz/rus/docs/P18000006342018.
14. Xu H, Li W, Yang J, Wiviott SD, Sabatine MS, Peterson ED, et al. The China acute myocardial infarction (CAMI) registry: a national long-term registry-research-education integrated platform for exploring acute myocardial infarction in China. Am Heart J. (2016) 175:193–201. doi: 10.1016/j.ahj.2015.04.014
15. Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. (2017) 8(1):1–16. doi: 10.1186/s13293-017-0152-8
16. Yang H-Y, Huang J-H, Hsu C-Y, Chen Y-J. Gender differences and the trend in the acute myocardial infarction: a 10-year nationwide population-based analysis. Sci World J. (2012) 2012:184075. doi: 10.1100/2012/184075
17. Maas AHEM, Appelman YEA. Gender differences in coronary heart disease. Neth Heart J. (2010) 18(12):598–603. doi: 10.1007/s12471-010-0841-y
18. Khamis RY, Ammari T, Mikhail GW. Gender differences in coronary heart disease. Heart. (2016) 102(14):1142–9. doi: 10.1136/heartjnl-2014-306463
19. Feng W, Hendry RM, Adams RJ. Risk of recurrent stroke, myocardial infarction, or death in hospitalized stroke patients. Neurology. (2010) 74(7):588–93. doi: 10.1212/WNL.0b013e3181cff776
20. Boulanger M, Béjot Y, Rothwell PM, Touzé E. Long-term risk of myocardial infarction compared to recurrent stroke after transient ischemic attack and ischemic stroke: systematic review and meta-analysis. J Am Heart Assoc. (2018) 7(2):e007267. doi: 10.1161/JAHA.117.007267
21. Dhamoon MS, Sciacca RR, Rundek T, Sacco RL, Elkind MSV. Recurrent stroke and cardiac risks after first ischemic stroke: the northern Manhattan study. Neurology. (2006) 66(5):641–6. doi: 10.1212/01.wnl.0000201253.93811.f6
22. Carrick D, Haig C, Maznyczka AM, Carberry J, Mangion K, Ahmed N, et al. Hypertension, microvascular pathology, and prognosis after an acute myocardial infarction. Hypertension. (2018) 72(3):720–30. doi: 10.1161/HYPERTENSIONAHA.117.10786
23. Supiyev A, Kossumov A, Utepova L, Nurgozhin T, Zhumadilov Z, Bobak M. Prevalence, awareness, treatment and control of arterial hypertension in Astana, Kazakhstan. A cross-sectional study. Public Health. (2015) 129(7):948–53. doi: 10.1016/j.puhe.2015.02.020
24. Fergus TS, Fazel R, Fang J, Chetcuti S, Smith DE, Kline-Rogers E, et al. Presentation, management, and outcomes of diabetic patients compared to non-diabetic patients admitted for acute coronary syndromes. Heart. (2004) 90(9):1051–2. doi: 10.1136/hrt.2003.027656
25. Koek HL, Soedamah-Muthu SS, Kardaun J, Gevers E, De Bruin A, Reitsma JB, et al. Short-and long-term mortality after acute myocardial infarction: comparison of patients with and without diabetes mellitus. Eur J Epidemiol. (2007) 22(12):883–8. doi: 10.1007/s10654-007-9191-5
26. Vallabhajosyula S, Ya’Qoub L, Kumar V, Verghese D, Subramaniam AV, Patlolla SH, et al. Contemporary national outcomes of acute myocardial infarction-cardiogenic shock in patients with prior chronic kidney disease and end-stage renal disease. J Clin Med. (2020) 9(11):3702. doi: 10.3390/jcm9113702
27. Vallabhajosyula S, Dunlay SM, Barsness GW, Vallabhajosyula S, Vallabhajosyula S, Sundaragiri PR, et al. Temporal trends, predictors, and outcomes of acute kidney injury and hemodialysis use in acute myocardial infarction-related cardiogenic shock. PLoS One. (2019) 14(9):e0222894. doi: 10.1371/journal.pone.0222894
28. Sharygin EJ, Guillot M. Ethnicity, russification, and excess mortality in Kazakhstan. Vienna Yearb Popul Res. (2013) 11:219. doi: 10.1553/populationyearbook2013s219
29. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. (2018) 39:119–77. doi: 10.1093/eurheartj/ehx393
30. Valgimigli M, Bueno H, Byrne RA, Collet J-P, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European society of cardiology (ESC) and of the European association for cardio-thoracic surgery (EACTS). Eur Heart J. (2018) 39(3):213–60. doi: 10.1093/eurheartj/ehx419
31. Young JB, Gauthier-Loiselle M, Bailey RA, Manceur AM, Lefebvre P, Greenberg M, et al. Development of predictive risk models for major adverse cardiovascular events among patients with type 2 diabetes mellitus using health insurance claims data. Cardiovasc Diabetol. (2018) 17(1):1–13. doi: 10.1186/s12933-018-0759-z
32. Burke AP, Virmani R. Pathophysiology of acute myocardial infarction. Med Clin N Am. (2007) 91(4):553–72. doi: 10.1016/j.mcna.2007.03.005
33. Statistics. MoNeotRoKCo. Demographic yearbook of Kazakhstan. Ministry on national economy of the Republic of Kazakhstan committee on statistics 2020. Available at: https://stat.gov.kz/official/industry/61/publication.
34. Instituto Nacional de Estatistica. Estatisticas Demográficas. www.ine.pt2019.
35. Bekbossynov S, Medressova A, Murzagaliyev M, Salov R, Dzhetybayeva S, Andossova S, et al. Surgical heart failure treatment program-the experience of Kazakhstan. G Ital Cardiol. (2014) 15(3):144–8.
36. Welsh RC, Granger CB, Westerhout CM, Blankenship JC, Holmes DR, O'Neill WW, et al. Prior coronary artery bypass graft patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. JACC Cardiovasc Interv. (2010) 3(3):343–51. doi: 10.1016/j.jcin.2009.12.008
37. De Bruyne B, Pijls NHJ, Kalesan B, Barbato E, Tonino PAL, Piroth Z, et al. Fractional flow reserve—guided PCI versus medical therapy in stable coronary disease. N Engl J Med. (2012) 367(11):991–1001. doi: 10.1056/NEJMoa1205361
Keywords: cardiovascular disease, acute myocardial infarction, risk factor, survival analysis, disability-adjusted life-years
Citation: Zhakhina G, Gaipov A, Salustri A, Gusmanov A, Sakko Y, Yerdessov S, Bekbossynova M, Abbay A, Sarria-Santamera A and Akbilgic O (2023) Incidence, mortality and disability-adjusted life years of acute myocardial infarction in Kazakhstan: data from unified national electronic healthcare system 2014–2019. Front. Cardiovasc. Med. 10:1127320. doi: 10.3389/fcvm.2023.1127320
Received: 19 December 2022; Accepted: 17 July 2023;
Published: 2 August 2023.
Edited by:
Sebhat Erqou, Brown University, United StatesReviewed by:
Weichieh Lee, Chi Mei Medical Center, Taiwan© 2023 Zhakhina, Gaipov, Salustri, Gusmanov, Sakko, Yerdessov, Bekbossynova, Abbay, Sarría-Santamera and Akbilgic. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abduzhappar Gaipov YWJkdXpoYXBwYXIuZ2FpcG92QG51LmVkdS5reg==
Abbreviations AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; CKD, chronic kidney disease; CVA, cerebrovascular accident; CVD, сardiovascular disease; GBD, global burden of disease; DALY, disability-adjusted life year; DM, diabetes mellitus; DW, disability weight; ICD, international classification of diseases; IR, incidence rate; PCI, percutaneous coronary intervention; PMP, per million population; RPN, population registry number; UNEHS, unified national electronic health system; WHO, world health organization; YLD, year lived with disability; YLL, year of life lost due to premature death.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.