
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 03 April 2023
Sec. Cardiovascular Epidemiology and Prevention
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1120543
This article is part of the Research Topic Insights in Cardiovascular Epidemiology and Prevention: 2022 View all 6 articles
 Xiao Yu1,†
Xiao Yu1,† Yu Ting Li2,†
Yu Ting Li2,† Hui Cheng1,†
Hui Cheng1,† Sufen Zhu3
Sufen Zhu3 Xiu-Jing Hu4
Xiu-Jing Hu4 Jia Ji Wang5,6
Jia Ji Wang5,6 Bedru H. Mohammed7
Bedru H. Mohammed7 Yao Jie Xie8
Yao Jie Xie8 Jose Hernandez9,10
Jose Hernandez9,10 Hua-Feng Wu11*
Hua-Feng Wu11* Harry H. X. Wang1,12,13*
Harry H. X. Wang1,12,13*
Aims: To assess longitudinal changes in blood pressure (BP) and fasting plasma glucose (FPG) in primary care patients with concomitant hypertension and type 2 diabetes mellitus (T2DM), and to explore factors associated with patients' inability to improve BP and FPG at follow-up.
Methods: We constructed a closed cohort in the context of the national basic public health (BPH) service provision in an urbanised township in southern China. Primary care patients who had concomitant hypertension and T2DM were retrospectively followed up from 2016 to 2019. Data were retrieved electronically from the computerised BPH platform. Patient-level risk factors were explored using multivariable logistic regression analysis.
Results: We included 5,398 patients (mean age 66 years; range 28.9 to 96.1 years). At baseline, almost half [48.3% (2,608/5,398)] of patients had uncontrolled BP or FPG. During follow-up, more than one-fourth [27.2% (1,467/5,398)] of patients had no improvement in both BP and FPG. Among all patients, we observed significant increases in systolic BP [2.31 mmHg, 95% confidence interval (CI): 2.04 to 2.59, p < 0.001], diastolic BP (0.73 mmHg, 0.54 to 0.92, p < 0.001), and FPG (0.12 mmol/l, 0.09 to 0.15, p < 0.001) at follow-up compared to baseline. In addition to changes in body mass index [adjusted odds ratio (aOR)=1.045, 1.003 to 1.089, p = 0.037], poor adherence to lifestyle advice (aOR = 1.548, 1.356 to 1.766, p < 0.001), and unwillingness to actively enrol in health-care plans managed by the family doctor team (aOR = 1.379, 1.128 to 1.685, p = 0.001) were factors associated with no improvement in BP and FPG at follow-up.
Conclusion: A suboptimal control of BP and FPG remains an ongoing challenge to primary care patients with concomitant hypertension and T2DM in real-world community settings. Tailored actions aiming to improve patients' adherence to healthy lifestyles, expand the delivery of team-based care, and encourage weight control should be incorporated into routine healthcare planning for community-based cardiovascular prevention.
Cardiovascular disease (CVD) represents one of the major public health challenges to population health worldwide (1). International evidence suggests that exposures to risk factors such as high systolic blood pressure (BP), high fasting plasma glucose (FPG), and high body mass index (BMI) have increased steadily (2). A recent modelling study on a global scale demonstrated that individuals presented with underlying long-term conditions, e.g., diabetes and cardiovascular disease, are at increased risk of severe COVID-19 (3). Hypertension and diabetes often occur together as a common modality of multimorbidity, which has become increasingly popular in the ageing population (4–7). The presence of concomitant hypertension and diabetes increases the risk for CVD events and mortality, and thus has imposed significant economic burdens on individuals, their families, and the healthcare system (8).
A substantial body of international guidelines suggest that primary care is one of the most cost-effective strategies for reducing morbidity, disability, and premature mortality attributed to hypertension and diabetes (8–12). Given the rising epidemic of both conditions, China's health-care reform has invested in a nationwide provision of free-of-charge, basic public health (BPH) service package to strengthen equitable primary care (13–16). Meanwhile, an emerging service delivery model entitled “family doctor team” has been piloted stepwise in primary care practice since 2016 as part of the “Healthy China Action (2019–2030)” national imitative (17–19). The family doctor team is characterised by general practice (GP) physicians working with public health practitioners, nurses and, if available and suitable, pharmacists and social workers, within a multidisciplinary primary care team (20). People with hypertension, type 2 diabetes mellitus (T2DM), or those aged 65 years and older are encouraged to actively enrol in the GP physician-led, team-based care through health-care registration. The team aims to serve as the first point of entry into the healthcare system, whilst enhancing preventive care through annual check-ups and tailor-made lifestyle advice alongside health education to support patients' self-management and population-based cardiovascular prevention.
However, there remain substantial physician- and system-level barriers to the management of hypertension and its complications, given the poor availability of manpower and limited clinical capacity in low-resource primary care settings where multi-component complex interventions are less common (21–23). The barriers are likely exacerbated by the traditional single disease approach (24, 25), coupled with “clinical inertia”, i.e., a common failure of physicians to initiate or intensify care regime when indicated (26), thus leading to difficulties in maintaining satisfactory control of BP and FPG over time (27, 28), with increased incidence of cardiovascular events (29). The hypothesis that multidisciplinary team-based care may overcome “clinical inertia” in the real-world community setting needs to be further tested. From a multimorbidity perspective, current knowledge on whether adherence to lifestyle advice and/or an active enrolment in routine health-care plans managed by the family doctor team may enhance patients' ability to achieve long-term improvement of BP and FPG in hypertensive patients with coexisting diabetes remains largely scant.
In this study, we aimed to assess the longitudinal changes in BP and FPG in Chinese primary care patients with concomitant hypertension and T2DM, and to explore independent factors associated with patients' inability to improve BP and FPG at follow-up.
We constructed a closed cohort of primary care patients who attended free-of-charge, annual check-ups in the context of the national basic public health (BPH) service provision in an urbanised township consisting of 47 communities in southern China. The annual check-ups were performed onsite at community health centres (CHCs). The BPH service information platform has become routinely operational since 2016. At each check-up, public health staff at CHCs documented individuals' health reports electronically on the information platform. In this study, computerised data were retrospectively captured between 2016 and 2019.
The target participants were adult primary care service users with concomitant hypertension and T2DM who attended annual check-ups at CHCs. Patients' earliest check-up attendance during the study period was regarded as a baseline and their most recent attendance in 2019 was considered a follow-up. Data from patients who had the coexistence of physician-diagnosed hypertension and T2DM were retrieved. Hypertension was considered present if an individual had systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg on repeated clinical measurements, or had antihypertensive medication. Diabetes was defined as FPG ≥ 7.0 mmol/L, or on glucose-lowering therapies. Patients whose health records were inactive due to death or move-out and those with incomplete socio-demographic information were excluded from the analysis (Figure 1).
A data management checklist of variables needed for data analysis was jointly reviewed by a research panel consisting of two public health specialists (HHXW and YTL), two medical practitioners (XJH and HFW), and one epidemiologist (JH). The main outcome variables were systolic BP, diastolic BP, and FPG. The clinical measurement of BP was conducted in a seated position by routinely-validated automatic sphygmomanometers. The arm with the higher pressure was used. The average of two BP readings, 1–2 min apart, was recorded. A venous blood sample at fasting was collected on-site. FPG was determined by enzymatic methods according to standard operating procedures. All clinical measurements and laboratory tests had internal quality control in accordance with the national standard. The achievement of controlled BP and FPG at baseline was defined according to guidelines that advocate treating hypertension in people with diabetes to a BP goal <130/80 mmHg, along with FPG <7.0 mmol/L (10–12, 28, 30, 31). Age, sex, educational attainment, duration of follow-up, number of chronic diseases, number of antihypertensive and glucose-lowering medications taken, anthropometric parameters, adherence to lifestyle advice, and active enrolment in team-based care were patient-level independent variables captured in the study.
Weight was measured with light clothing and without shoes by a calibrated weighing scale, and height was measured using a wall-mounted stadiometer. The BMI was calculated as weight in kilograms divided by squared height in meters (kg/m2). Chronic diseases documented in the health records included hypertension, diabetes, coronary heart disease, stroke, chronic obstructive pulmonary disease, cancer, mental disorders, tuberculosis, and chronic kidney disease. Adherence to lifestyle advice was determined based on the presence of at least one of the following self-reported habits on a regular basis, i.e., salt consumption of <6 g per day, no smoking, moderate-intensity aerobic exercise for ≥180 min per week, and restricted daily alcohol intake (≤25 g for males or ≤15 g for females) (13, 30). Patients who had no responsible physician documented in the health record or who did not attend all consecutive annual check-ups (e.g., lipid profile test measuring the amount of cholesterol and triglycerides, body constitution assessment, and medication review if applicable, etc.) for a comprehensive set of health assessments since baseline registration were not deemed active enrolment in health-care plans managed by the family doctor team. The duration of follow-up was calculated as the time period between the earliest check-up attendance and the most recent check-up attendance in 2019 for each patient.
Descriptive analysis was conducted to describe the basic information of study participants according to control of BP and FPG at baseline, and by improvement of BP and FPG at follow-up, respectively. The paired t test was used to compare the changes in BP and FPG between baseline and follow-up within each subgroup. The independent two-sample t test was used to compare within-group changes for patients with and without improved outcomes at follow-up. A patient's inability to improve BP and FPG was defined as having no reduction in both outcomes at follow-up compared to baseline. Multivariable logistic regression models were constructed in a backward stepwise approach to explore all independent predictor variables that were significantly associated with no improvement in both BP and FPG at follow-up. The baseline BP and FPG were fitted as covariates. We also assessed the regression model accuracy metrics, i.e., Akaike information criterion (AIC) and Bayesian information criterion (BIC). The incremental value of risk factors identified in the regression model for predicting no improvement in BP and FPG was explored by applying C-statistic, net reclassification index (NRI), and integrated discrimination index (IDI) (32). The predicted probability of no improvement in health outcomes was calculated using the marginal standardisation approach, which was considered appropriate for making inferences on the overall source population where the study sample was drawn (33). We also performed sensitivity analysis on top of the fitted regression models to visualise the extent to which the association of adherence to lifestyle advice or active enrolment in multidisciplinary team-based care with BP and FPG improvements may vary across subgroups with different BP and FPG levels at baseline. Data analyses were performed using Stata (version 15.1, StataCorp, TX) and R (version 4.1.1, Core Team, Vienna). A p value < 0.05 was considered statistically significant.
Data anonymisation was achieved by removing all patient identifiers from the dataset prior to data analysis. Ethics approval was initially granted and subsequently renewed by the School of Public Health Biomedical Research Ethics Review Committee at Sun Yat-Sen University (Refs: SPH2016027 and SPH2019032) following the Declaration of Helsinki 2013.
A total of 5,398 primary care patients who fulfilled the eligibility criteria were included in the final analysis (Figure 1). Patients with uncontrolled BP or FPG at baseline were older (i.e., aged 60 years and above), had a longer duration of follow-up, and had a greater number of medications taken compared to their counterparts with controlled BP and FPG at baseline (Table 1). At follow-up, slightly over half [54.3% (797/1,467)] of patients who had no improvement in BP and FPG were able to adhere to lifestyle advice, which were less than that [64.1% (2,518/3,931)] of patients with improved clinical parameters. The proportion of patients actively enrolled in GP-led team-based care was also significantly lower in the non-improved subgroup than in their counterparts (Table 2).
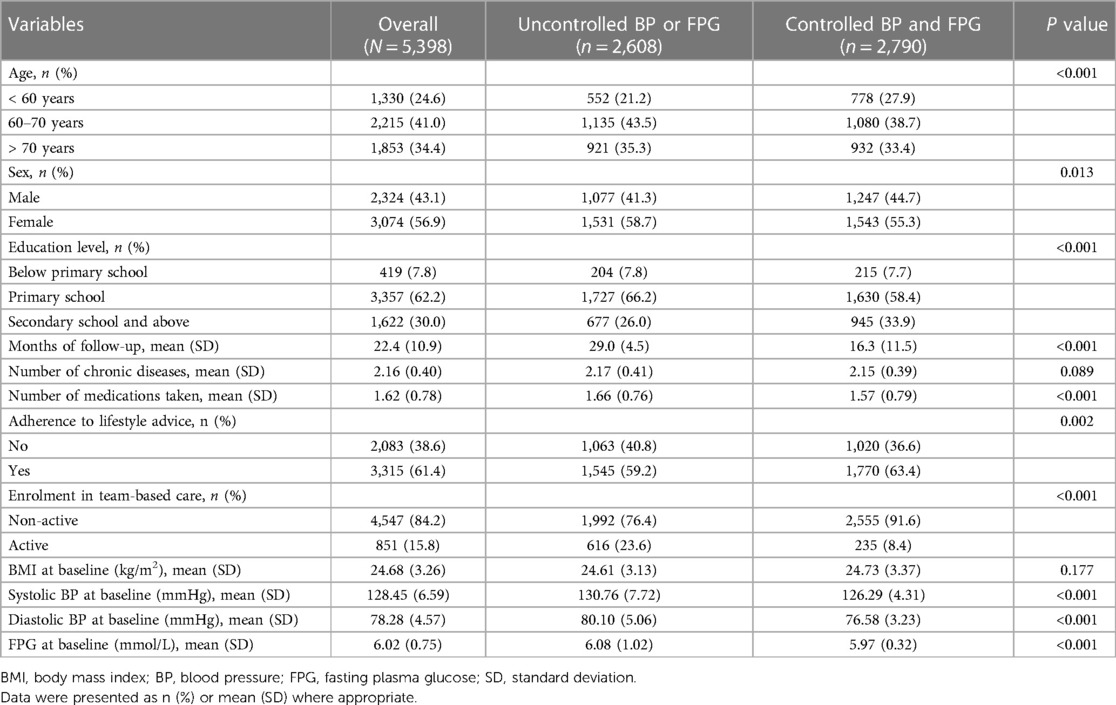
Table 1. Characteristics of study participants according to control of blood pressure and fasting plasma glucose at baseline.
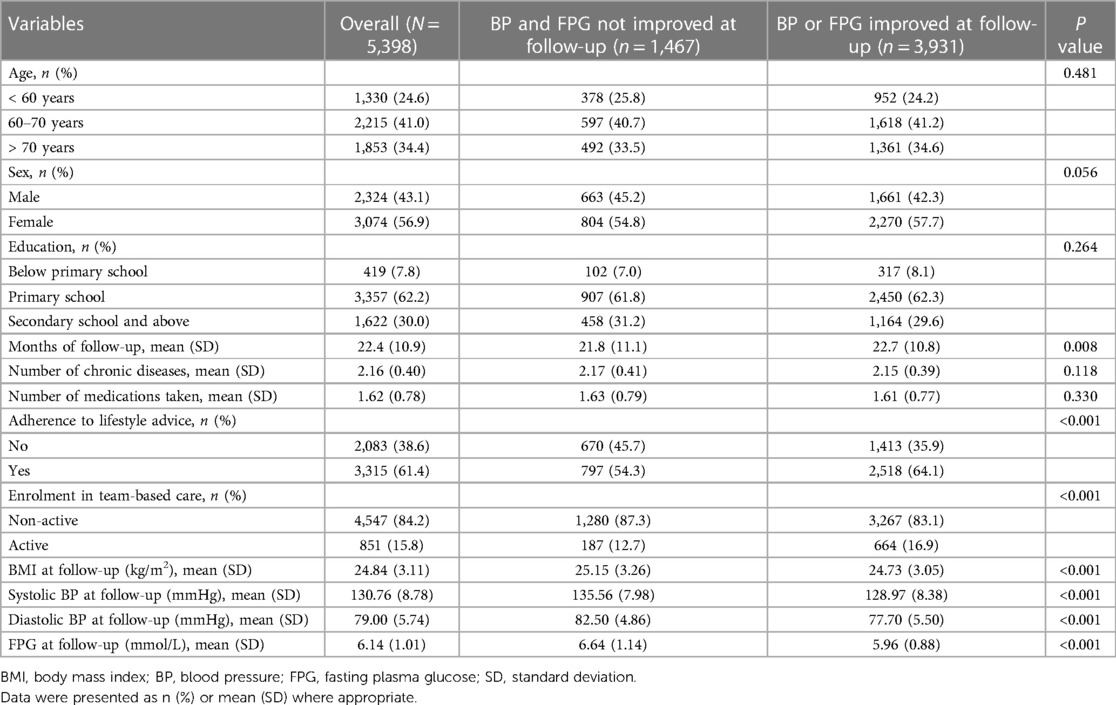
Table 2. Characteristics of study participants according to the improvement of blood pressure and fasting plasma glucose at follow-up.
Among all participants, systolic BP (2.31 mmHg, 95%CI: 2.04 to 2.59 mmHg, p < 0.001), diastolic BP (0.73 mmHg, 0.54 to 0.92 mmHg, p < 0.001), and FPG (0.12 mmol/L, 0.09 to 0.15 mmol/L, p < 0.001) increased consistently between baseline and follow-up. Compared to participants who had improved clinical parameters at follow-up, the between-group net changes in systolic BP, diastolic BP, and FPG were 9.22 mmHg (8.65 to 9.79 mmHg), 7.20 mmHg (6.82 to 7.58 mmHg), and 0.99 mmol/L (0.92 to 1.06 mmol/L), respectively, at follow-up (Table 3).
Multiple regression analysis revealed that non-adherence to lifestyle advice (aOR = 1.548, 95%CI: 1.356 to 1.766, p < 0.001), non-active enrolment in health-care plans managed by the family doctor team (aOR = 1.379, 1.128 to 1.685, p = 0.001), and increases in BMI during follow-up (aOR = 1.045, 1.003 to 1.089, p = 0.037) were independently associated with no improvement in BP and FPG after adjusting for confounding (Table 4). The estimates of NRI and IDI suggested that the predictive accuracy significantly increased by adding the three risk factors identified for the study outcome (Supplementary Table S1). We further conducted subgroup analysis to explore the predicted probability of no improvement in BP and FPG based on fitted multivariable regression models. When broken down by quartiles of changes in BMI from baseline to follow-up, we saw consistent associations between non-adherence to lifestyle advice or non-active enrolment in team-based care and no improvement in BP and FPG, accompanied by a synergistic effect. Compared with patients who had the least weight gain, adhered to lifestyle advice, and were actively enrolled in team-based care, those who had the greatest weight gain, failed to adhere to lifestyle advice, and were not actively enrolled in health-care plans managed by the family doctor team were most likely to have no improvement in BP and FPG at follow-up (Figure 2). Results were consistently visualised across different subgroups according to patients' BP and FPG levels at baseline, suggesting the robustness of the study findings (Supplementary Figure S1).

Figure 2. Predicted probability of no improvement in BP and FPG at follow-up. Note: Changes from baseline to follow-up in body mass index were divided into quartiles from greatest weight gain (Quartile 4; median change: 1.46 kg/m2) to least gain or loss (Quartile 1; median change: −1.00 kg/m2).
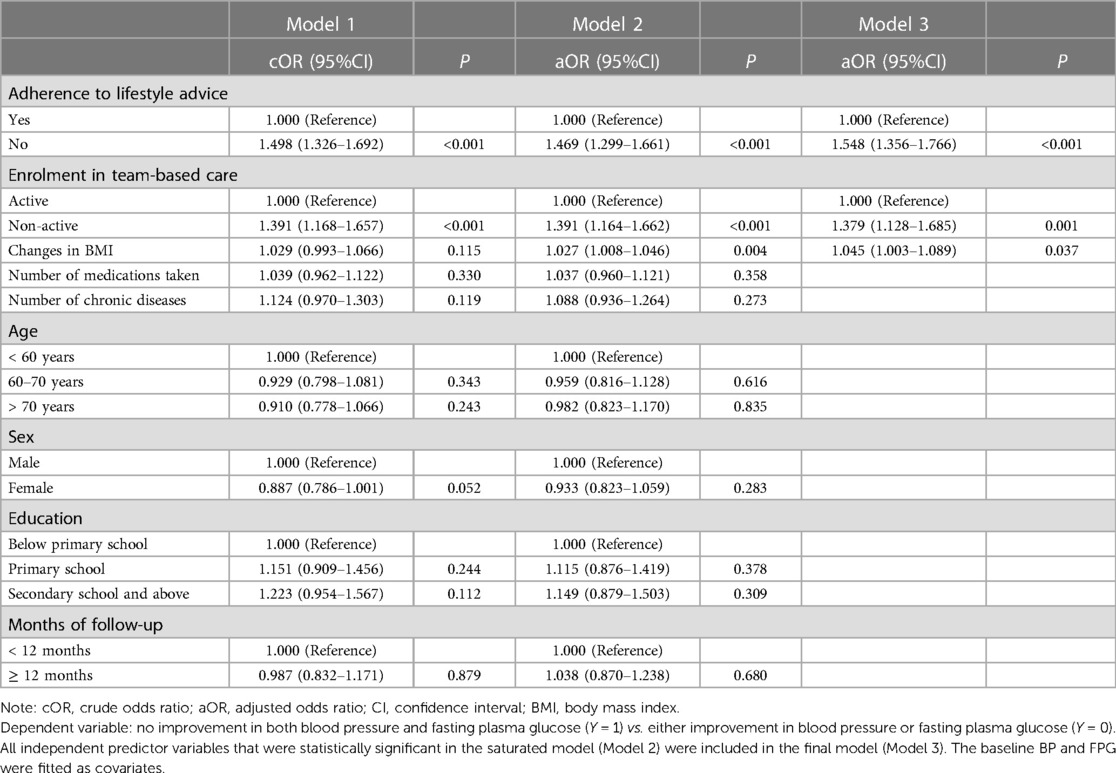
Table 4. Factors associated with no improvement in blood pressure and fasting plasma glucose at follow-up.
In a community-based, longitudinal cohort of Chinese primary care patients with concomitant hypertension and T2DM who were followed for a mean of 22.4 months, we found that more than one-fourth of patients had no improvement in both BP and FPG. Greater increases in BMI, poor adherence to lifestyle advice, and unwillingness to actively enrol in team-based care were factors independently associated with no improvement in BP and FPG over time.
Hypertension and T2DM are among the most prevalent chronic conditions worldwide. The two conditions often occur together, which not only complicate treatment strategy and increase healthcare costs, but also heightens the risk for CVDs considerably (4). A recent study suggested that people at high risk for either hypertension or diabetes share common risk factors including abdominal obesity, hyperinsulinemia, and hypertriglyceridemia, and that weight gain may contribute to the development of both hypertension and diabetes mellitus (34). Although lowering BP and blood glucose has been recommended in the prevention of CVDs, control of BP and blood glucose in real-world settings is often unsatisfactory (35, 36). Consistent with our results, a cross-sectional, population-based study showed that fewer than half of the participants on medication for hypertension or diabetes had adequately controlled BP or FPG, suggesting the unmet need for effective health system intervention to improve access to care (37). Evidence from community-based, randomised controlled trials conducted in resource-rich settings such as the UK and Hong Kong showed that “real-world” prevention programmes may not always lead to successful reduction in BP, blood glucose, and other cardiovascular risk factors (38, 39). Hence, numerous efforts are still needed to translate trials from research-based settings that are effective to daily practice where intensive efforts at CVD risk reduction are less likely to be sustained regularly due to the possible co-existence of clinical inertia and physician burnout (40, 41).
Consistent with previous findings from the mendelian randomisation study and cross-sectional investigation that suggested a strong association between BMI and cardiometabolic disease (42, 43), longitudinal analysis of data in our cohort showed that patients who had their BMI levels increased during the follow-up tended to have no improvement in BP and FPG, implying the need for maximising the patient's motivation to maintain continuous monitoring of weight gain and engage in regular aerobic exercises that are necessary to primary prevention of CVD (44). A most recent review discussed the main physiological mechanisms that underpinned the beneficial effects of optimal lifestyles on BP control and overall cardiovascular health, advocating the use of lifestyle interventions for the prevention and adjuvant treatment of hypertension (45). Despite solid evidence on the association between lifestyles and cardiovascular-related clinical outcomes (46), the rising epidemic of unhealthy lifestyles remains a major challenge to the traditional medical practice model (47).
Our findings provided evidence to fill in the gaps in understanding of whether multidisciplinary team-based primary care may overcome “clinical inertia” in the real-world setting. International experiences from Canada and Israel demonstrated that inter-professional teams could contribute to facilitating the transfer of knowledge, skills and attitudes, and thus are capable of enhancing clinical competencies and overcoming traditional barriers in the delivery of cardiovascular care (48–50). Alongside the transformation of practice paradigm to empower hypertensive patients with the coexistence of common long-term conditions such as T2DM, team-based educational programmes and tools that accommodate the needs of and provide support for underserved subpopulations might create opportunities to deepen patients' insights into the clustering of disease components and improve their intrinsic motivation to build self-management skills for cardiovascular health (51, 52).
We constructed a primary care cohort of a large sample of hypertensive patients with coexisting diabetes whose data were retrieved from a computerised system, where healthcare record was documented according to standard procedures which ensured the accuracy of data. Objective measures were used to assess the longitudinal changes of BP and FPG to avoid subjective bias. The analysis was conducted from a multimorbidity perspective and the non-improvement in BP and FPG were considered as a combined outcome to take into account the joint or synergistic effect of CVD risk factors. However, there are several limitations of this study. First, we did not adopt a trial design where a “pure” control group is included, given that the main purpose of the present study was not to evaluate the effectiveness of either a particular lifestyle advice or a well-designed health-care plan managed by the family doctor team per se. Instead, we are interested in assessing factors associated with poor control of clinical parameters, i.e., BP and FPG, that are commonly seen in the context that real-world, routine primary care is delivered. Second, the study population was drawn from an urbanised township, which may limit the application of our findings to other populations in more socio-economically developed regions. Third, self-report lifestyle habits may be subject to recall bias, although adherence to lifestyle advice was conceptualised as a composite variable to minimise the extent to which the actual situation may deviate from single measures. Last but not least, confounding factors such as income, family history, dietary intake, medication adherence, and sleep history may also play a role but were not captured in the study due to the absence or inconsistent measurements of these variables in the original healthcare record across different years.
Our findings that most of hypertensive patients with coexisting T2DM have experienced no improvements in BP and FPG over time indicated the necessity of continuous efforts to engage patients as active participants, rather than passive recipients, and to deliver effective care that is sustainable and accountable to individuals at elevated cardiovascular risk. The association between an active enrolment in team-based care and a higher probability of improved BP and FPG levels may reflect the patient-centred approach and a public health perspective adopted by the family doctor team in their daily work across the continuum of care. Despite the debate about the target BP that should be attained in diabetic patients, a rich body of evidence has confirmed the benefits of BP reduction alongside glycaemic control (53, 54). In light of a rapid increase in the number of people living with hypertension and T2DM, strategies to target subjects who may be less likely to improve neither BP nor FPG over time shall be crucial in the research agenda. Our analysis further showed that those who were more likely to have no improvement in BP and FPG over time tended to have greater weight gain. This may reflect the complexity of managing hypertension and its comorbidities that require patients' excessive time and intrinsic motivation to tackle a variety of treatment workloads including doctor visits, self-monitoring, and lifestyle changes. In this regard, counselling skills that enable primary care practitioners to have effective communication with patients may be of paramount importance (55). This would help enhance patient engagement in team-based care and improve shared-decision making in the long-term behavioural changes to achieve the national and international goals in CVD prevention and control.
Suboptimal control of BP and FPG remains an ongoing challenge to primary care patients with concomitant hypertension and T2DM in real-world community settings. Tailored actions aiming to improve patients' adherence to healthy lifestyles, expand the delivery of family doctor team-based care, and encourage weight control should be incorporated into routine healthcare planning for community-based cardiovascular prevention.
The raw data supporting the conclusions of this article are available on reasonable request from the corresponding author.
The studies involving human participants were reviewed and approved by the School of Public Health Biomedical Research Ethics Review Committee at Sun Yat-Sen University (Refs: SPH2016027 and SPH2019032). The patients/participants provided their written informed consent to participate in this study.
Conceptualization: HHXW and XY; data curation: HFW; formal analysis: XY and XJH; methodology: HHXW, XY, and JJW; project administration: YTL; supervision: HHXW and YTL; validation: HC and SZ; writing—original draft: HHXW and XY; writing—review & editing: YTL, BHM, YJX, and JH. All authors (XY, YTL, HC, SZ, XJH, JJW, BHM, YJX, JH, HFW, and HHXW) contributed to the interpretation of data, and read and approved the final manuscript. All authors contributed to the article and approved the submitted version.
National Natural Science Foundation of China (grants 72061137002 and 71904212); and Basic and Applied Basic Research Foundation of Guangdong Province (grant 2019A1515011381). The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
We wish to acknowledge the tremendous support of the frontline primary care staff at community health facilities who were involved in delivering basic public health services, documenting routine check-up data on the computerised system, and assisting health-care plans managed by the family doctor team.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1120543/full#supplementary-material.
1. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010
2. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396(10258):1223–49. doi: 10.1016/S0140-6736(20)30752-2
3. Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HHX, Mercer SW, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. (2020) 8(8):e1003–17. doi: 10.1016/S2214-109X(20)30264-3
4. Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. (2018) 34(5):575–84. doi: 10.1016/j.cjca.2017.12.005
5. Dal Canto E, Ceriello A, Rydén L, Ferrini M, Hansen TB, Schnell O, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. (2019) 26(2_suppl):25–32. doi: 10.1177/2047487319878371
6. Tomita A, Leyna GH, Kim HY, Moodley Y, Mpolya E, Mogeni P, et al. Patterns of multimorbidity and their association with hospitalisation: a population-based study of older adults in urban Tanzania. Age Ageing. (2021) 50(4):1349–60. doi: 10.1093/ageing/afab046
7. Mercer SW, Wang HHX. Chapter 2 long-term conditions. In: Staten A, Staten P, editors. Practical general practice: Guidelines for effective clinical management (7th edition). ISBN 978-0-7020-5552-2. Edinburgh, UK: Elsevier (2019). p. 7–10.
8. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. (2021) 42(34):3227–337. doi: 10.1093/eurheartj/ehab484
9. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. (2019) 74(10):e177–232. doi: 10.1016/j.jacc.2019.03.010
10. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. J Hypertens. (2020) 38(6):982–1004. doi: 10.1097/HJH.0000000000002453
11. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the task force for diabetes, pre-diabetes, and cardiovascular diseases of the European society of cardiology (ESC) and the European association for the study of diabetes (EASD). Eur Heart J. (2020) 41(2):255–323. doi: 10.1093/eurheartj/ehz486
12. American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2022. Diabetes Care. (2022) 45(Suppl 1):S144–74. doi: 10.2337/dc22-S010
13. Department of Primary Health Care, National Health Commission, PRC. Standards for National Basic Public Health Services (3rd edition). http://www.nhc.gov.cn/jws/s3578/201703/d20c37e23e1f4c7db7b8e25f34473e1b.shtml. Accessed 14 November 2022 (2017).
14. Wang HHX, Wang JJ, Wong SYS, Wong MCS, Mercer SW, Griffiths SM. The development of urban community health centres for strengthening primary care in China: a systematic literature review. Br Med Bull. (2015) 116(1):139–53. doi: 10.1093/bmb/ldv043
15. Wang HHX, Wang JJ. Developing primary care in China. In: Griffiths SM, Tang JL, Yeoh EK, editors. Routledge handbook of global public health in Asia. ISBN 978-0-415-64382-5. London: Routledge (2014). p. 584–600.
16. Wang HHX, Mercer SW. Perspective from China. In: Watt GCM, editors. The exceptional potential of general practice. ISBN 978-1-7852-3158-2. London: CRC Press (2018). p. 189–92.
17. Healthcare Reform Office of the State Council, PRC. No.1 document. http://www.gov.cn/xinwen/2016-06/06/content_5079984.htm. Accessed 07 November 2022 (2016).
18. Opinions on implementing Healthy China. State Council, PRC; 2019, No.13 document. http://www.gov.cn/zhengce/content/2019-07/15/content_5409492.htm. Accessed 07 November 2022.
19. Healthy China: deepening health reform in China building high-quality and value-based service delivery. Washington, DC: World Bank (2016).
20. Hu XJ, Wang HHX, Li YT, Wu XY, Wang Y, Chen JH, et al. Healthcare needs, experiences and treatment burden in primary care patients with multimorbidity: an evaluation of process of care from patients’ perspectives. Health Expect. (2022) 25(1):203–13. doi: 10.1111/hex.13363
21. Wang HHX, Mercer SW. Understanding barriers to adherence to optimal treatment of elevated blood pressure and hypertension-insights from primary care. JAMA Netw Open. (2021) 4(12):e2138651. doi: 10.1001/jamanetworkopen.2021.38651
22. Demaio AR, Nielsen KK, Tersbøl BP, Kallestrup P, Meyrowitsch DW. Primary health care: a strategic framework for the prevention and control of chronic non-communicable disease. Glob Health Action. (2014) 7:24504. doi: 10.3402/gha.v7.24504
23. Correia JC, Lachat S, Lagger G, Chappuis F, Golay A, Beran D, et al. Interventions targeting hypertension and diabetes mellitus at community and primary healthcare level in low- and middle-income countries:a scoping review. BMC Public Health. (2019) 19(1):1542. doi: 10.1186/s12889-019-7842-6
24. Salisbury C, Man MS, Bower P, Guthrie B, Chaplin K, Gaunt DM, et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet. (2018) 392(10141):41–50. doi: 10.1016/S0140-6736(18)31308-4
25. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2
26. Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia. Ann Intern Med. (2001) 135(9):825–34. doi: 10.7326/0003-4819-135-9-200111060-00012
27. Ali W, Bakris GL. How to manage hypertension in people with diabetes. Am J Hypertens. (2020) 33(10):935–43. doi: 10.1093/ajh/hpaa067
28. Passarella P, Kiseleva TA, Valeeva FV, Gosmanov AR. Hypertension management in diabetes: 2018 update. Diabetes Spectr. (2018) 31(3):218–24. doi: 10.2337/ds17-0085
29. Milman T, Joundi RA, Alotaibi NM, Saposnik G. Clinical inertia in the pharmacological management of hypertension: a systematic review and meta-analysis. Medicine (Baltimore). (2018) 97(25):e11121. doi: 10.1097/MD.0000000000011121
30. Liu LS, Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. Chinese Hypertension league and Chinese society of cardiology. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. (2019) 24(1):1–46. doi: 10.3969/j.issn.1007-5410.2019.01.002
31. Jia WP, Chinese Diabetes Society, National Office for Primary Diabetes Care. National guidelines for the prevention and control of diabetes in primary care (2018). Chin J Intern Med. (2018) 57(12):885–93. doi: 10.3760/cma.j.issn.0578-1426.2018.12.003
32. Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. (2008) 27(2):157–72. discussion 207-12. doi: 10.1002/sim.2929
33. Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. (2014) 43(3):962–70. doi: 10.1093/ije/dyu029
34. Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. (2018) 71(3):422–8. doi: 10.1161/HYPERTENSIONAHA.117.10546
35. Rahimi K, Bidel Z, Nazarzadeh M, Copland E, Canoy D, Ramakrishnan R, et al. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. (2021) 397(10285):1625–36. doi: 10.1016/S0140-6736(21)00590-0
36. Wright AK, Suarez-Ortegon MF, Read SH, Kontopantelis E, Buchan I, Emsley R, et al. Risk factor control and cardiovascular event risk in people with type 2 diabetes in primary and secondary prevention settings. Circulation. (2020) 142(20):1925–36. doi: 10.1161/CIRCULATIONAHA.120.046783
37. Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, Tafatatha T, et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol. (2018) 6(3):208–22. doi: 10.1016/S2213-8587(17)30432-1
38. Smith JR, Greaves CJ, Thompson JL, Taylor RS, Jones M, Armstrong R, et al. The community-based prevention of diabetes (ComPoD) study: a randomised, waiting list controlled trial of a voluntary sector-led diabetes prevention programme. Int J Behav Nutr Phys Act. (2019) 16(1):112. doi: 10.1186/s12966-019-0877-3
39. Wong MCS, Wang HHX, Kwan MWM, Fong BCY, Chan WM, Zhang DX, et al. Dietary counselling has no effect on cardiovascular risk factors among Chinese grade 1 hypertensive patients: a randomized controlled trial. Eur Heart J. (2015) 36(38):2598–607. doi: 10.1093/eurheartj/ehv329
40. Veettil RA. Understanding clinical inertia in diabetes. J Soc Health Diab. (2019) 7:77–80. doi: 10.1055/s-0039-1694300
41. Ward ZD, Morgan ZJ, Peterson LE. Family physician burnout does not differ with rurality. J Rural Health. (2021) 37(4):755–61. doi: 10.1111/jrh.12515
42. Lyall DM, Celis-Morales C, Ward J, Iliodromiti S, Anderson JJ, Gill JMR, et al. Association of body mass index with cardiometabolic disease in the UK biobank: a Mendelian randomization study. JAMA Cardiol. (2017) 2(8):882–9. doi: 10.1001/jamacardio.2016.5804
43. Linderman GC, Lu J, Lu Y, Sun X, Xu W, Nasir K, et al. Association of body mass index with blood pressure among 1.7 million Chinese adults. JAMA Netw Open. (2018) 1(4):e181271. doi: 10.1001/jamanetworkopen.2018.1271
44. Fukumoto Y. Lifestyle intervention for primary prevention of cardiovascular diseases. Eur J Prev Cardiol. (2022) 29(17):2250–1. doi: 10.1093/eurjpc/zwac245
45. Valenzuela PL, Carrera-Bastos P, Gálvez BG, Ruiz-Hurtado G, Ordovas JM, Ruilope LM, et al. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol. (2021) 18(4):251–75. doi: 10.1038/s41569-020-00437-9
46. Arnett DK, Khera A, Blumenthal RS. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: part 1, lifestyle and behavioral factors. JAMA Cardiol. (2019) 4(10):1043–4. doi: 10.1001/jamacardio.2019.2604
47. Zhao D. Key roles of five lifestyle risk factors in the harmful transition from a healthy condition to multimorbidity in the Chinese population. Eur Heart J. (2021) 42(34):3385–7. doi: 10.1093/eurheartj/ehab516
48. Boeckxstaens P, Brown JB, Reichert SM, Smith CNC, Stewart M, Fortin M. Perspectives of specialists and family physicians in interprofessional teams in caring for patients with multimorbidity: a qualitative study. CMAJ Open. (2020) 8(2):E251–6. doi: 10.9778/cmajo.20190222
49. Fogelman Y, Goldfracht M, Karkabi K. Managing diabetes Mellitus: a survey of attitudes and practices among family physicians. J Community Health. (2015) 40(5):1002–7. doi: 10.1007/s10900-015-0024-2
50. Shani M, Wang HHX, Wong SYS, Griffiths SM. International primary care snapshots: israel and China. Br J Gen Pract. (2015) 65(634):250–1. doi: 10.3399/bjgp15X684913
51. Wang HHX, Li YT, Duan H, Wong MCS. Physician motivation and satisfaction matter in healthcare. Hong Kong Med J. (2023) 29(1):8–10. doi: 10.12809/hkmj235142
52. Brush JE Jr, Handberg EM, Biga C, Birtcher KK, Bove AA, Casale PN, et al. 2015 ACC health policy statement on cardiovascular team-based care and the role of advanced practice providers. J Am Coll Cardiol. (2015) 65(19):2118–36. doi: 10.1016/j.jacc.2015.03.550
53. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. (2016) 387(10022):957–67. doi: 10.1016/S0140-6736(15)01225-8
54. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. Br Med J. (2016) 352:i717. doi: 10.1136/bmj.i717
Keywords: long-term follow-up, blood pressure, fasting plasma glucose, hypertension, diabetes, routine primary care, cardiovascular prevention
Citation: Yu X, Li YT, Cheng H, Zhu S, Hu X-J, Wang JJ, Mohammed BH, Xie YJ, Hernandez J, Wu H-F and Wang HHX (2023) Longitudinal changes in blood pressure and fasting plasma glucose among 5,398 primary care patients with concomitant hypertension and diabetes: An observational study and implications for community-based cardiovascular prevention. Front. Cardiovasc. Med. 10:1120543. doi: 10.3389/fcvm.2023.1120543
Received: 10 December 2022; Accepted: 6 March 2023;
Published: 3 April 2023.
Edited by:
Gen-Min Lin, Hualien Armed Forces General Hospital, TaiwanReviewed by:
Nikolaos Stalikas, University General Hospital of Thessaloniki AHEPA, Greece© 2023 Yu, Li, Cheng, Zhu, Hu, Wang, Mohammed, Xie, Hernandez, Wu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Harry H.X. Wang aGFveGlhbmd3YW5nQDE2My5jb20= djFod2FuMjJAZWQuYWMudWs= Hua-Feng Wu aHVhZmVuZ3d1MjAyMkAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Cardiovascular Epidemiology and Prevention, a section of the journal Frontiers in Cardiovascular Medicine
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.