- 1School of Rehabilitation Sciences, Southern Medical University, Guangzhou, China
- 2Department of Rehabilitation Medicine, Zhujiang Hospital, Southern Medical University, Guangzhou, China
- 3School of Nursing, Southern Medical University, Guangzhou, China
- 4Faculty of Health and Social Sciences, The Hong Kong Polytechnic University, Hong Kong, China
Objective: To explore the effects of inspiratory muscle training (IMT) on hypertension and provide guidance for its clinical application as an auxiliary approach.
Methods: Articles published prior to July 2022 were searched in Cochrane Library, Web of Science, PubMed, Embase, CNKI, and Wanfang databases. Included were randomized controlled studies that used IMT to treat individuals with hypertension. The mean difference (MD) was computed using the Revman 5.4 software. In individuals with hypertension, the effects of IMT on systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and pulse pressure (PP) were compared and studied.
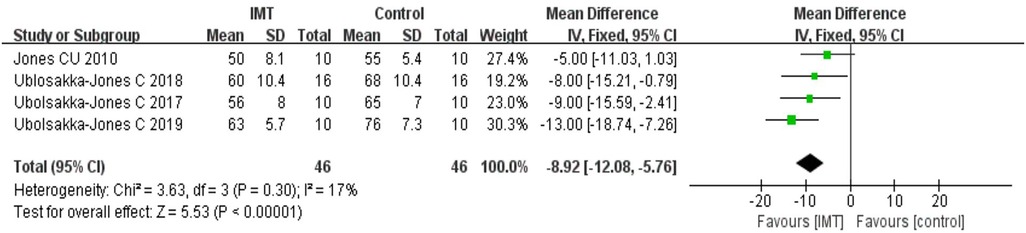
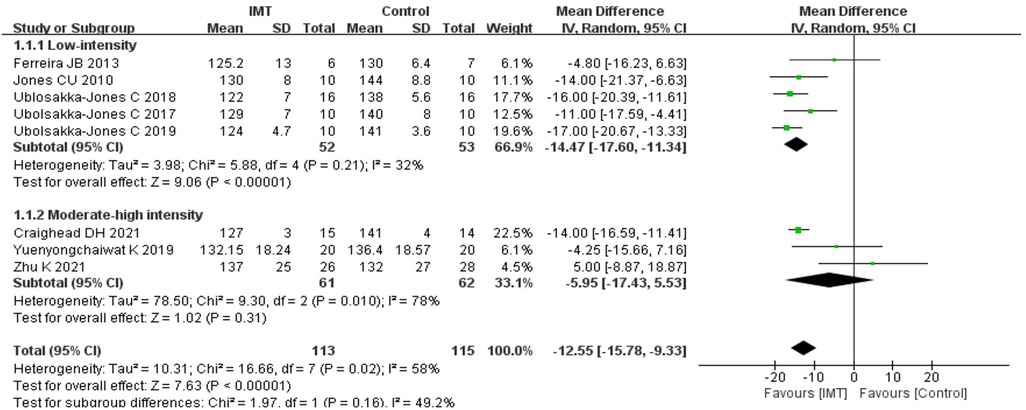
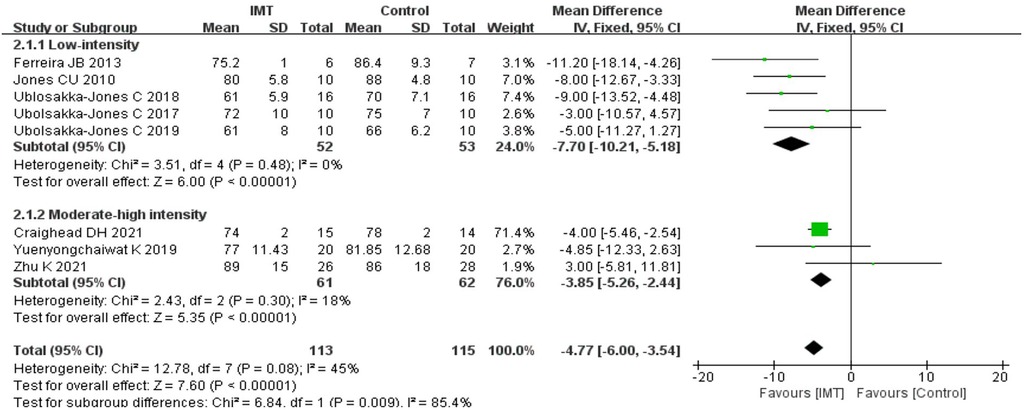
Results: There were found to be eight randomized controlled trials totaling 215 patients. According to a meta-analysis, the IMT reduced the SBP (MD: −12.55 mmHg, 95% CI: −15.78, −9.33), DBP (MD: −4.77 mmHg, 95% CI: −6.00, −3.54), HR (MD: −5.92 bpm, 95% CI: −8.72, −3.12), and PP (MD: −8.92 mmHg, 95% CI: −12.08, −5.76) in patients with hypertension. In subgroup analyses, low-intensity IMT showed a better reduction in SBP (MD: −14.47 mmHg, 95% CI: −17.60, −11.34), DBP (MD: −7.70 mmHg, 95% CI: −10.21, −5.18).
Conclusion: IMT may become an auxiliary means to improve the four hemodynamic indexes (SBP, DBP, HR and PP) in patients with hypertension. In subgroup analyses, low-intensity IMT was more effective in regulating blood pressure than medium-high-intensity IMT.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42022300908.
1. Introduction
In the world, hypertension affects 31.1% of adults, making it one of the most prevalent chronic illnesses (1). Type 2 diabetes, heart failure, and stroke could be secondary to hypertension (2–5), resulting in the death of patients with heart diseases and stroke, which are seriously endangering human health (6). Therefore, a novel treatment is urgently needed to control the further deterioration of hypertension. According to a meta-analysis, physical exercise helps people with hypertension lower their blood pressure (BP) (7). IMT has been shown to be a crucial component in the rehabilitation of hypertension as an innovative physical activity strategy (8).
Inspiratory muscle training (IMT) is performed using a small and special breathing device that can provide resistance for inhalation [such as PowerBreath® (9)], which, with better tolerance and efficiency, can be used as an important adjunct therapy for patients with hypertension (10). The underlying mechanism for the ability of IMT to lower BP may be the central respiratory network, and its interaction with the sympathetic nerve drive and vagus nerve activity may be affected by an increase in inspiratory muscle strength, which also promotes cardiopulmonary coupling (11). Recent research suggests (12) that IMT with a 30% MIP may be able to lower BP in people with essential hypertension, as well as isolated systolic hypertension patients whose resting BP is elevated (13). However, the impact of IMT on hypertension is still debatable. Beltrami (14) has regarded the effects of IMT on hypertension as exaggerated. It (15) shows that IMT has no obvious effects on the BP of patients with hypertension, and slow breathing is more effective than IMT in lowering BP (16). Da Silva (17) has shown that loaded respiratory training can reduce BP in hypertension, however, only two RCTs were analyzed in this literature resulting in low confidence in the results. To sum up, the effects of IMT on hypertension should be further explored.
Furthermore, studies (18) have also demonstrated that patients with hypertension can have their BP under control by monitoring hemodynamic indicators, like systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and pulse pressure (PP). The goal of this study was to conduct a meta-analysis evaluating the benefits of IMT for individuals with hypertension in order to determine how IMT affects people with hemodynamic indices of hypertension and to provide guidance and evidence for the clinical application of IMT.
2. Methods
The Cochrane Cooperation Organization's (19) and PRISMA guidelines for systematic evaluation and meta-analysis (20) were followed in conducting this meta-analysis. The protocol has a PROSPERO registration (registration code CRD42022300908). This study was based on the existing published literature, therefore, ethical approval is not required.
2.1. Eligibility criteria
Using PICOS elements as a basis, the eligibility criteria were defined (21): (1) population: patients enrolled in clinical trials who have SBP greater than 130 mmHg and/or DBP greater than 80 mmHg (22); (2) intervention: IMT was utilized in the intervention group; (3) comparison: in the control group, a blank control, sham IMT therapy, or traditional training, were implemented; (4) outcome: mean BP or PP in mmHg, HR in bpm, and standard deviation or standard error; (5) study type: randomized controlled trials. Additionally, we excluded trials according to the exclusion criteria: (1) study types were conference abstracts, non-randomized controlled trials, retrospective studies, animal experiments, case reports, etc.; (2) participants in clinical trials who had other cardiovascular and cerebrovascular diseases or metabolic diseases; (3) inability to obtain the full text and complete data.
2.2. Search strategy
To locate any pertinent randomized controlled trials (RCTs), the following databases were thoroughly searched: Web of Science, the Cochrane Library, PubMed, Embase, CNKI, and Wanfang databases. The literature search was carried out without language restrictions or a beginning date until July 2022 using the following terms: “high blood pressure”, “hypertension”, “blood pressure”, “diastolic blood pressure”, “systolic blood pressure”, “systolic blood pressure”, “pulse pressure”, “heart rate”, “breathing exercise”, “inspiratory muscle training”, “inspiratory loaded breathing training”, “high-resistance inspiratory muscle strength training”, “slow load breathing training”, and “IMT.” We contacted the authors via email for additional information in cases of insufficient data, and the available data were used to run analyses if they failed to respond within 14 days.
2.3. Study selection
Relevant literature was searched using the following process: The first step was a preliminary screening using the title and abstract, which was then loaded into Endnote X9 software, where duplicate literature was then removed. The remaining full text of literature was carefully examined in light of the established inclusion and exclusion criteria, and any content that did not meet the standards was eliminated. The whole screening process was independently performed by two reviewers (GL and LC). The third reviewer (YZ) was ready for consultation if there were any discrepancies between the two independent reviewers.
2.4. Data extraction
Two researchers (SZ and SYL) independently retrieved the following information: the first author, publication year, sample size, average age, type of hypertension, gender, medication, load intensity, intervention time, training time, training frequency, respiratory rate, training equipment, data (SBP, DBP, HR, and PP) of the intervention group and control group data, time of measurement, equipment of measurement, and position of measurement. When there was insufficient data, we emailed the authors for additional information, and if they didn't reply within a week, we ran analyses using the data that were available instead.
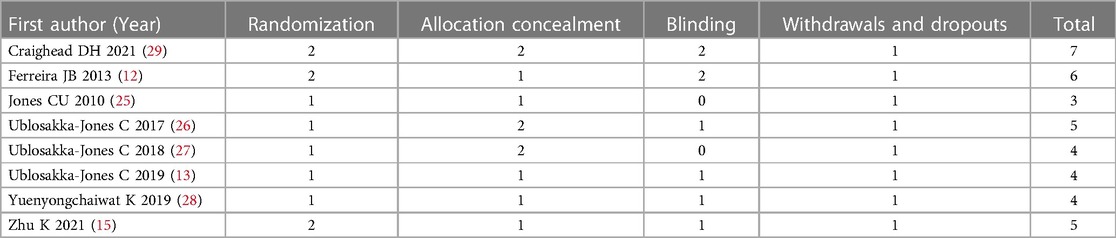
2.5. Quality assessment
The quality of each study was assessed by two researchers (QZh and SZ) using a modified Jadad quality scale (23) that included four questions related to scientific rigor, such as the generation of a random sequence, randomization concealment, blind method, withdrawal number, and reasons. The highest score on the modified Jadad quality scale is 7, with 1, 2, and 3 denoting low quality and 4, 5, 6, and 7 denoting high quality (24).
2.6. Data analysis
The Cochrane Handbook for Systematic Reviews of Interventions was used to analyze the data. For continuous variables, the mean difference (MD) and 95% confidence interval (CI) were used to compare net changes (i.e., IMT vs. control group). For each study group and important outcome, mean and standard deviations (SD) were gathered in order to calculate the effect size. A negative effect size indicated that IMT effectively reduced SBP, DBP, HR, and PP. Using the heterogeneity chi-square test and I2 statistics, this study quantitatively discussed the heterogeneity of various studies. These relevant data results were analyzed using the Revman5.4 software. The pooled MD and the 95% CI were represented graphically using a forest plot. According to its weight in the meta-analysis, each study was represented in the plot by a square. The threshold for statistical significance was a two-sided P value of 0.05. As the number of included researches was lower than ten pieces of research, we did not use statistical or graphical methods to evaluate publication bias.
3. Results
3.1. Selection
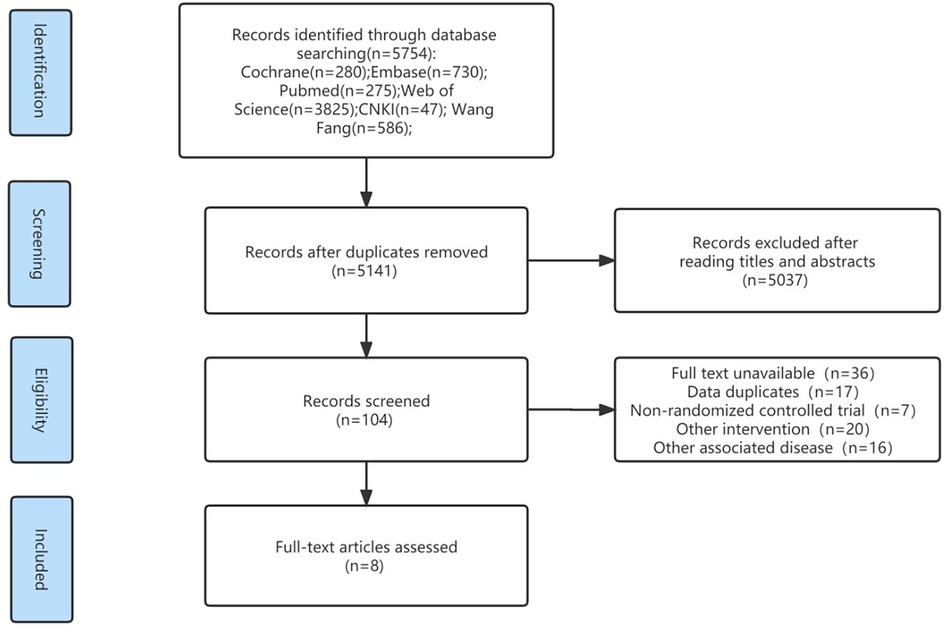
The initial search identified 5,754 pieces of literature, 5,141 of which were left after eliminating duplicate literature using the EndNote x9 software. Only 104 publications, chosen based on titles and abstracts, were used for the rest of the analysis. Eight RCTs (12, 13, 15, 25–29), seven in English and one in Chinese, were eventually included in this study after carefully reading the whole text (Figure 1). Following a full-text analysis, the main reasons for exclusion were: full text not being accessible; duplicate data; non-RCTs; other interventions; and other connected disorders.
3.2. Participant characteristics
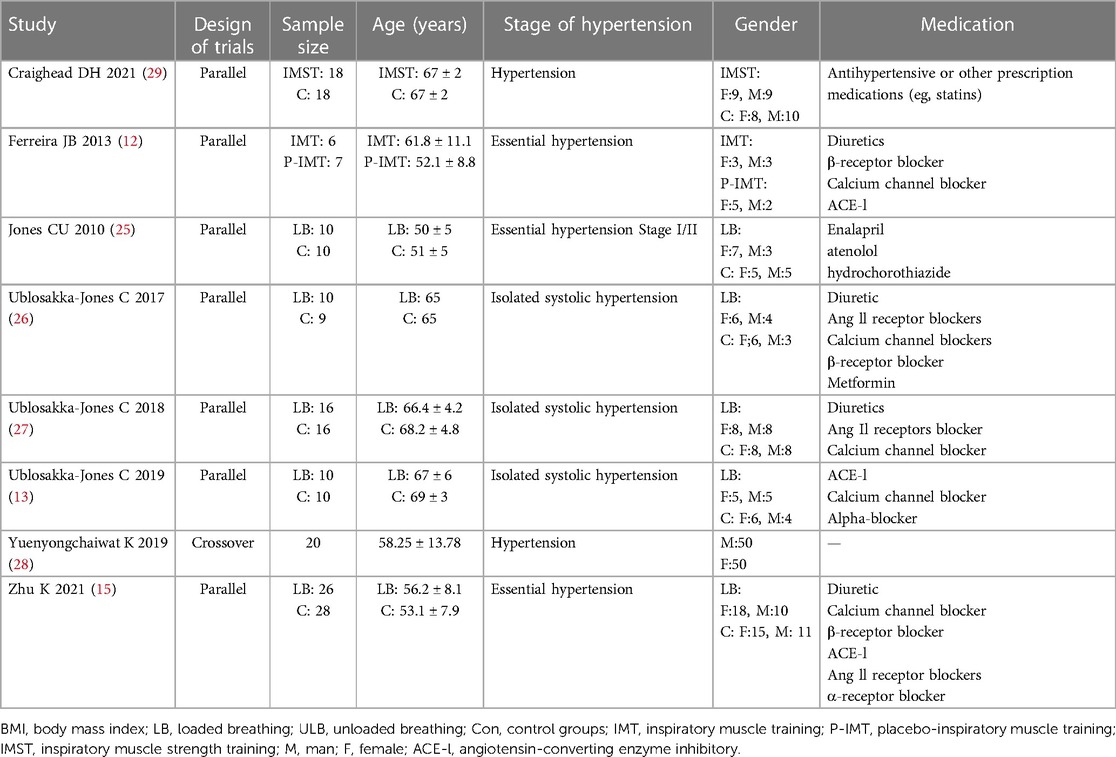
Eight studies with a total sample size of 215 patients aged between 50 and 70 years were finally analyzed: seven clinical trials were designed as parallel trials (12, 13, 15, 25–29) and only one study (28) was a cross-over trial. Based on the type of hypertension, three studies (12, 15, 25) essential hypertension, three (13, 26, 27) isolated systolic hypertension, and two (28, 29) only described as hypertension. One study (28) did not record the drug information of patients, while the other seven studies (12, 13, 15, 25–27, 29) had records of drug information, mainly including angiotensin-converting enzyme inhibitors, calcium blockers, angiotensin II receptor blockers, and beta-blockers. Characteristics of the participants was shown in Table 1.
3.3. Measurements on hemodynamic parameters
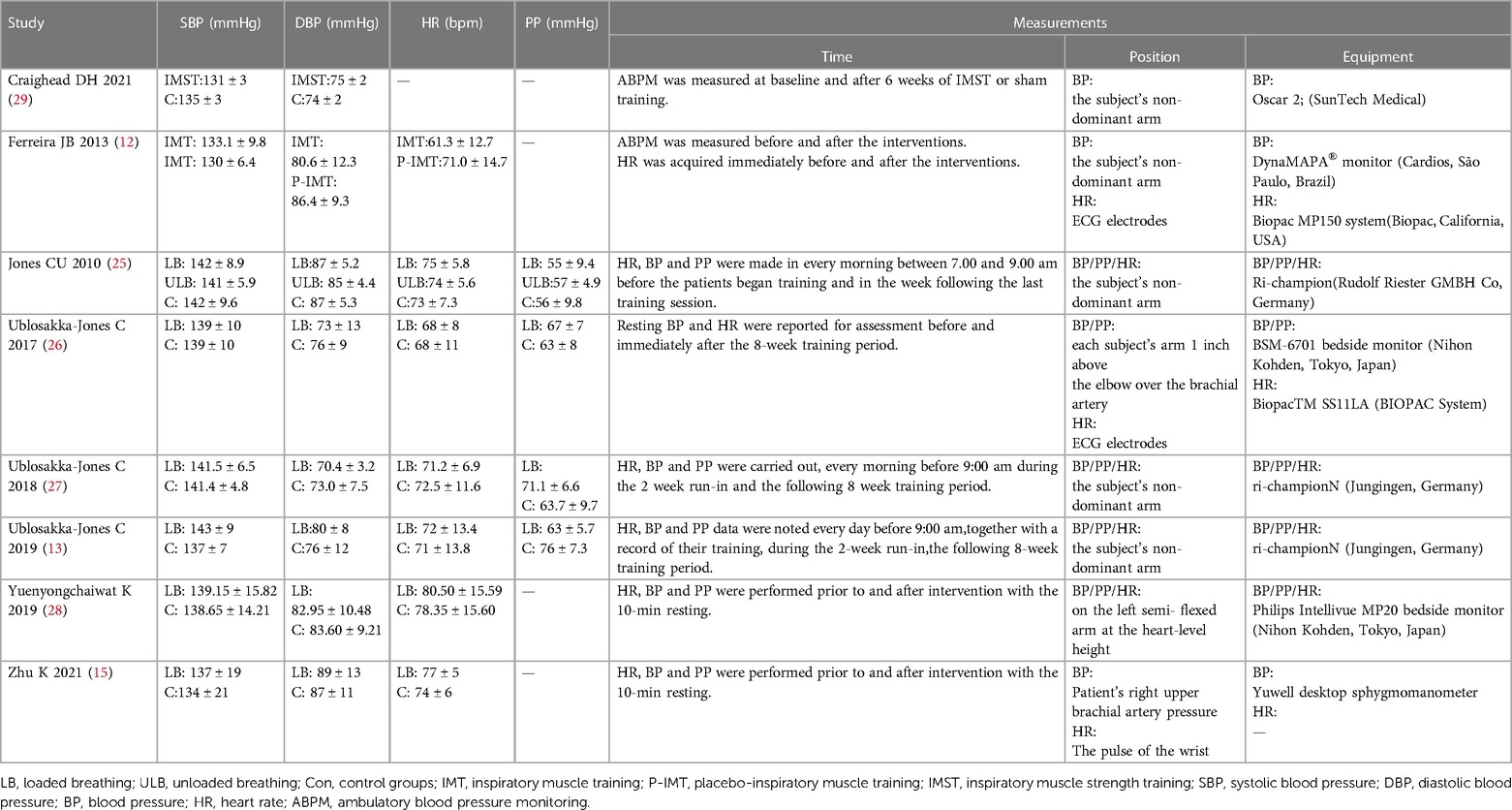
Ambulatory BP and PP were measured in two studies (12, 29) and resting BP and PP were measured before and 10 min after intervention in the other two studies (15, 28). BP and PP were measured every morning in three studies (13, 25, 27). Resting BP and PP were measured before and 8 weeks after training (26). The position of BP measurements was simply described in the patient's non-dominant arm in five articles (12, 13, 24, 26, 28). In one study, the position was depicted on the left semi-flexed arm at the heart-level height (28), but another article said the position was the patient's right upper brachial artery pressure (15). The remaining RCT indicated that this position was on each subject's arm 1 inch above the elbow over the brachial artery (26). As for measuring equipment, these studies used Oscar 2 (SunTech Medical) (29), DynaMAPA® monitor (Cardios, São Paulo, Brazil) (12), Ri-champion (Rudolf Riester GMBH Co, Germany) (13, 25, 27), BSM-6701 bedside monitor (Nihon Kohden, Tokyo, Japan) (26), Philips Intellivue MP20 bedside monitor (Nihon Kohden, Tokyo, Japan) (28), and Yuwell desktop sphygmomanometer (15) respectively. The measurement time, position, and equipment of PP and HR in 8 RCTS were also shown in Table 2.
3.4. Intervention characteristics
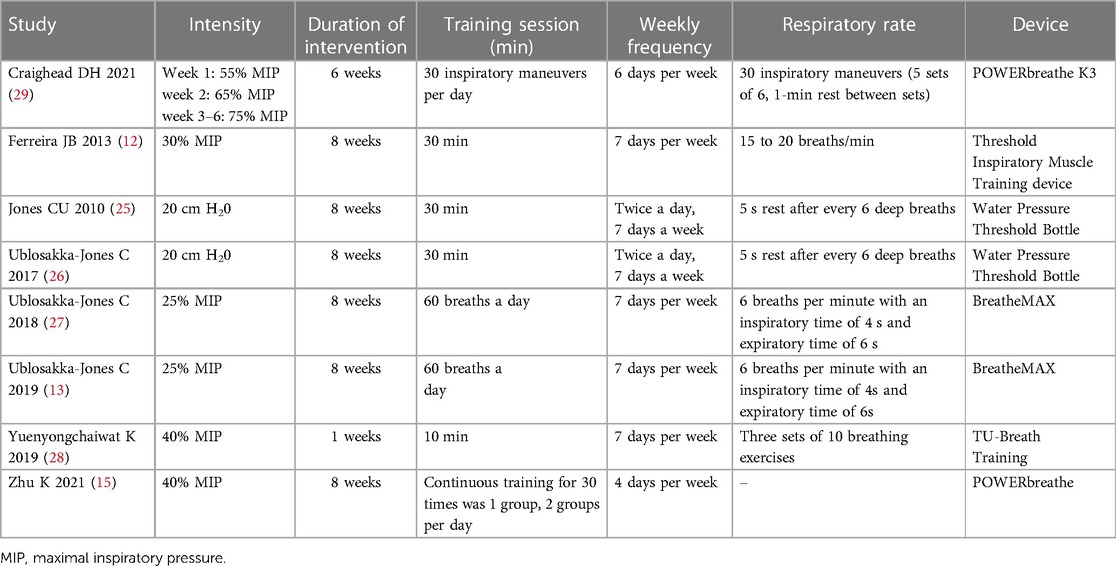
Five (12, 13, 25–27) intervention groups were low-intensity IMT; two (15, 28) were medium-intensity IMT; and one study (29) was high-intensity IMT. Six studies (13, 15, 26–29) showed no intervention in the control group; one study (12) showed placebo-IMT; and another study (27) included both the control group without intervention measures and placebo-IMT. Two studies (13, 27) used the BreatheMAX device; two studies (15, 29) used the POWERbreathe device; two studies (25, 26) used a water pressure threshold bottle; one study (12) used the Threshold Inspiratory Muscle Trainer (HealthScan Products Inc., Cedgrove, New Jersey), and one study (28) used the TU-Breath Training device. The intervention duration of one (29) study was 6 weeks' one study (28) was 1 week, and the remaining six studies (12, 13, 15, 25–27) were 8 weeks. Characteristics of the intervention was described in Table 3.
3.5. Quality assessment results including research
According to the improved Jadad scale, low quality was defined as 1–3 points and high quality as 4–7 points. Seven studies (12, 13, 15, 26–29) scored >3 points and were classified as high-quality literature, while one study (25) received 3 points and was labeled as low-quality literature. The quality of the included RCT studies was shown in Table 4.
3.6. Main results
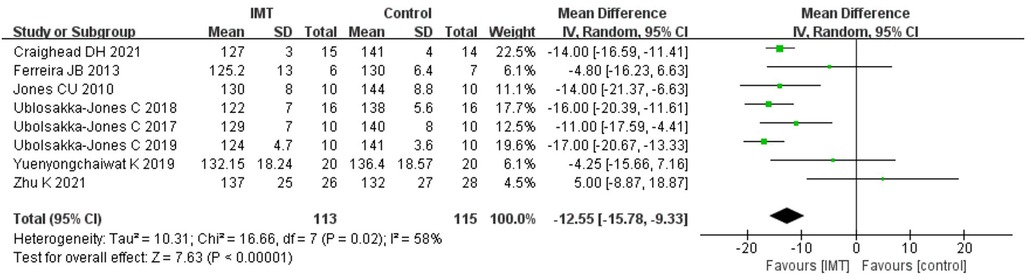
3.6.1. Effects of IMT on systolic blood pressure
SBP after treatment was compared between the intervention group using IMT and the control group. The results demonstrated that IMT might lower the SBP of patients with hypertension; According to data analysis from seven trials using a random effect model, IMT could improve the SBP of patients with hypertension. [n = 228, MD = −12.55 mmHg, 95%CI (−15.78, −9.33), P < 0.01] (Figure 2).
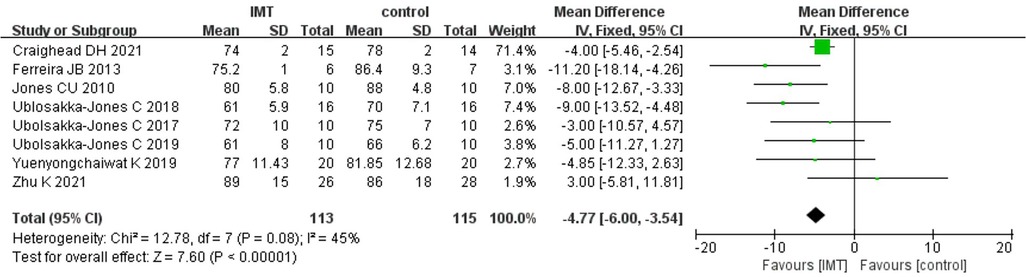
3.6.2. Effects of IMT on diastolic blood pressure
After analyzing the DBP data in the IMT and control groups, high heterogeneity was found (I2 = 45%). Therefore, for the meta-analysis, we used a fixed effects model. The results demonstrated that IMT training was more successful than a control group in decreasing DBP in patients with hypertension [n = 228, MD = −4.77 mmHg, 95% CI (−6.00, −3.54), P < 0.01] (Figure 3).
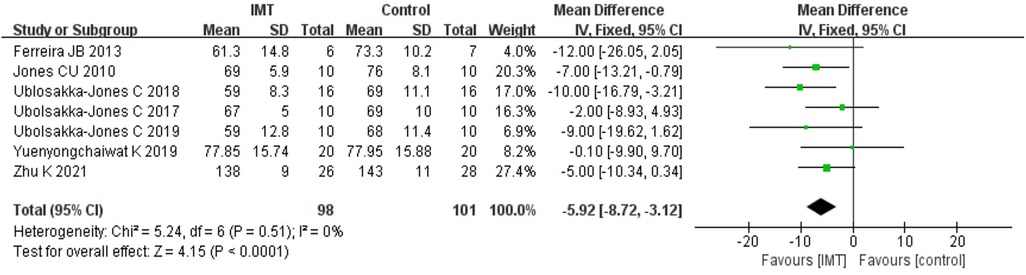
3.7. Secondary results
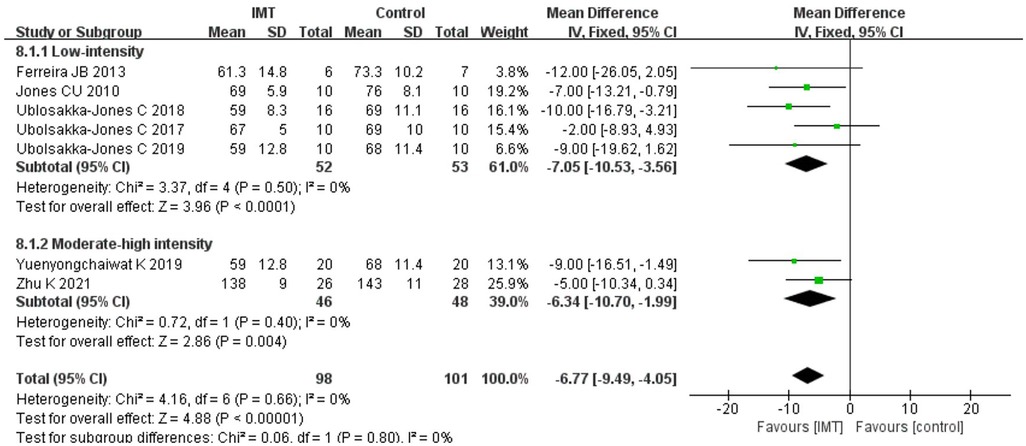
3.7.1. Effects of IMT on heart rate
Because Daniel H 2021 (29) study could not obtain relevant data, we analyzed the data from two groups of patients post-treatment in the other seven trials. According to the results of the fixed effect model, IMT had a stronger impact on lowering the HR of patients with hypertension than the control group [n = 199, MD = −5.92 bpm, 95% CI (−8.72, −3.12), P < 0.01] (Figure 4).
3.7.2. Effects of IMT on pulse pressure
Four studies provided results for PP with a total of 92 patients. The heterogeneity (I2 = 17%) was small; thus, it was decided to use the fixed effect model, and the analysis's findings revealed that IMT could reduce the PP of patients with hypertension [n = 92, MD = −8.92 mmHg, 95% CI (−12.08, −5.76), P < 0.01] (Figure 5). As interventions in these four studies were all low-intensity IMT, the subgroup analysis was not performed.
3.8. Subgroup analysis
3.8.1. Effects of IMT on systolic blood pressure
About 30% of MIP is considered low-intensity IMT (30), whereas >30% MIP is medium-high-intensity IMT. Eight studies were divided into two groups: low-intensity IMT and medium-high-intensity IMT, and two subgroup analyses were conducted. Subgroup analyses showed that low-intensity IMT was effective in decreasing SBP of patients with hypertension [n = 105, MD = −14.47 mmHg, 95% CI (−17.60, −11.34), P < 0.01] (Figure 6); however, medium-high-intensity IMT had no positive effects on reducing SBP of patients with hypertension [n = 123, MD = −5.95 mmHg, 95% CI (−17.43, 5.53), P = 0.31] (Figure 6).
3.8.2. Effects of IMT on diastolic blood pressure
Similarly, a subgroup analysis was carried out on the DBP data from eight trials, which were separated into two groups: low-intensity IMT and medium-high-intensity IMT. Sub-group analysis showed that low-intensity IMT could improve the DBP of patients with hypertension [n = 106, MD = −7.70 mmHg, 95% CI (−10.21, −5.18), P < 0.01] (Figure 7); however, medium-high-intensity IMT did not help reduce the DBP of patients with hypertension [n = 123, MD = −3.85 mmHg, 95% CI (−5.26, −2.44), P = 0.01] (Figure 7).
3.8.3. Effects of IMT on heart rate
Since the relevant data could not be obtained in Daniel H 2021 (29), a subgroup analysis was carried out on the remaining seven studies. According to the results of the subgroup analysis, low-intensity IMT [n = 199, MD = −7.05 bpm, 95% CI (−10.53, −3.56), P < 0.01] (Figure 8) and medium-high-intensity IMT [n = 74, MD = −6.34 bpm, 95% CI (−10.70, −1.99), P = 0.004] (Figure 8) could effectively slow down the HR of patients with hypertension.
4. Discussion
This meta-analysis set out to assess the impact of IMT hemodynamic indexes on hypertension. Through analysis of eight RCT items (12, 13, 15, 25–29), IMT was proven to improve the hemodynamic indexes (SBP, DBP, HR, and PP) of patients with hypertension. However, low-intensity IMT was superior to medium-high-intensity IMT in regulating BP.
Having a high prevalence and incidence of hypertension is a significant public health concern because deaths and diseases of hypertension and cardiovascular systems are closely linked (31). Physical activity is one of the treatments for patients with hypertension (7). In these meta-analyses, it could be concluded that aerobic exercise (32), isometric exercise (32), breathing-control (33), and unload respiratory muscle training (17) had the effect in reducing BP in patients with hypertension. Our meta-analysis showed that IMT, an innovative physical activity, also had an active reduction in BP which was consistent with the conclusion of the analysis showing that the antihypertensive drug was effective in SBP and DBP within 6 months (−4.2/−2.0 mmHg) (34). Among the RCTs included in this literature, seven studies (12, 13, 15, 25–27, 29) clearly indicated that patients were still receiving medication and one study (28) did not clearly indicate whether patients were receiving medication or not. Combined with the effect size of the antihypertensive drug, we speculated that IMT may further reduce BP in hypertensive patients on the basis of medication. The reason for the inconsistency between these two studies may be that fewer articles have been published on hypertension in the latter study and the heterogeneity among RCTs is high. Lowering BP is quite important in the clinic. Studies suggested that every reduction of 5 mmHg BP can significantly reduce the risk of type 2 diabetes (5), heart failure (35), and stroke (36), thus it is possible that lowering BP is a means of preventing type 2 diabetes, heart failure, and stroke. And the safety of IMT in these diseases has been established (37–39). Therefore, IMT can be used as adjunct training for hypertension to lower BP and minimize the chance of developing secondary conditions in clinic.
It is possible that IMT lowers BP through a variety of mechanisms. IMT may have decreased BP based on changes in breathing patterns and reflex mechanisms (25). For example, the respiratory muscle metaboreflex activation in patients with hypertension will be activated in advance during exercise, whereas increasing the inspiratory muscle strength of patients with hypertension through IMT can slow down the early appearance of this reflex, thus reducing the hyperactivity of peripheral sympathetic nerves, which could control the rise in BP (40). In addition, arterial stiffness is one of the important inducements to develop and maintain hypertension (41). IMT could reduce SBP in patients with hypertension, which may be related to IMT altering endothelial and smooth muscle function, thereby affecting aortic stiffness (16). Regarding DBP, respiratory resistance can raise intrathoracic pressure, lower cardiac output, and decrease systemic venous return due to pulmonary artery compression (42). As a result of the significant decrease in cardiac output, which also causes a reduction in ventricular filling, the result is a reduction in DBP. Low-intensity IMT reduced BP more than high-intensity IMT; this may be related to the greater contraction intensity of respiratory muscles in medium-high-intensity IMT, which more likely stimulates mechanoreceptors in the muscles, and muscle contraction leads to increased vasculature pressure, which results in increased BP (43).
The role of HR in hypertension has been established. Patients with hypertension frequently have an increase in HR, which has been linked to an independent predictor of poor cardiovascular and death outcomes (44). Therefore, there is a need to evaluate how IMT affects HR in individuals with hypertension. Our meta-analysis showed a result that IMT was linked to an effect size of −5.29 bpm on the HR, which was similar to the results of pursed-lip breathing (−3.85 bpm) (45) and high-intensity interval training (−2.17 bpm) (46) decreasing in HR. This reduction in HR has important clinical implications for patients with hypertension. A 10 bpm rise in HR resulted in an 8% increase in the incidence of hypertension (47), while a drop in HR was associated with a reduced cardiovascular death rate in the long-term follow-up procedure (48). IMT can regulate HR probably because it can decrease cardiac sympathetic nerve activity and increase the expression of parasympathetic nerves at rest (49). In the included studies, only four RCTs evaluated PP in hypertension before and after IMT. PP is another predictor of hypertension events that, in some cases, has a superior predictive capability to SBP or DBP alone (50, 51). Our meta-analysis discovered an improvement in PP in patients with hypertension, which is associated with the outcome of the present study that SBP decreases more obviously than DBP. Therefore, IMT may reduce HR and PP while dropping BP, minimizing the risk of unfavorable cardiovascular and fatal consequences.
It is the first meta-analysis to focus on the impact of IMT on the four hemodynamic indexes of patients with hypertension, and our analysis provides evidence for IMT as a clinical auxiliary means for improving hemodynamic indexes and decreasing the risk of some secondary disorders in individuals with hypertension. However, future research will be required to establish the most appropriate type, timing, number of sessions each week, and sessions per breath for optimal treatment outcomes. Moreover, in order to better understand the circadian behavior of BP and HR, it would also be interesting to evaluate 24-hour ambulatory BP and HR measurements.
The study limitations are mainly manifested in the following aspects: (1) a small number of RCTs were included in this investigation, and the bulk of them had modest sample sizes; therefore, the total sample size was small; (2) some heterogeneity problems encountered in this study may be due to different equipment, training frequency, training duration, intervention time, and intervention intensity; (3) since the respective number of different types of hypertension was very small in the included studies, this study did not do a subgroup analysis of distinct kinds of hypertension.
5. Conclusion
IMT may become an auxiliary means to improve the four hemodynamic indexes (SBP, DBP, HR and PP) in patients with hypertension. Furthermore, low-intensity IMT was preferred over medium-high-intensity IMT in subgroup analyses for regulating SBP and DBP. Both low and medium-high-intensity IMT could reduce the HR of patients with hypertension. However, the training time, respiratory rate, and training frequency of IMT, as well as the therapeutic effects on different types of hypertension, should be further explored.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Author contributions
QZe, JZ and LH: conceptualization and design, article typographic logic; GL, LC and YZ: Study selection and data extraction; QZh, SZ and SYL: data analysis and interpretation, article editing; SLL, QY, XZ and SC: study supervision and article revising. The article's submission was reviewed and approved by all authors.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Nature Science Foundation of China (NSFC) (Project No. 82002380 and No. 82205245), College Student's Innovative Entrepreneurial Training Plan Program for Southern Medical University (Project No. X202012121325S and No. X202112121184), and Southern Medical University Scientific Research Enlightenment Project (Project No. B521ZJ0102), Guangdong Province Health Appropriate Technology Promotion Project (Project No. 202206252011533513).
Acknowledgment
The author group would like to thank the English Language Institute (www.enago.cn) for providing the English touch-ups.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. (2016) 134(6):441–50. doi: 10.1161/circulationaha.115.018912
2. Chen Y, Ma J, Lu D, Fang Y. The risk factors of type 2 diabetes in hypertensive subjects. Front Endocrinol (Lausanne). (2022) 13:901614. doi: 10.3389/fendo.2022.901614
3. Qamar A, Braunwald E. Treatment of hypertension: addressing a global health problem. JAMA. (2018) 320(17):1751–2. doi: 10.1001/jama.2018.16579
4. Chen L, Li Q, Fang X, Wang X, Min J, Wang F. Dietary intake of homocysteine metabolism-related B-vitamins and the risk of stroke: a dose-response meta-analysis of prospective studies. Adv Nutr. (2020) 11(6):1510–28. doi: 10.1093/advances/nmaa061
5. Nazarzadeh M, Bidel Z, Canoy D, Copland E, Wamil M, Majert J, et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis. Lancet. (2021) 398(10313):1803–10. doi: 10.1016/s0140-6736(21)01920-6
6. Yin G, Zhou X. Current research status on the epidemiology of hypertension. Electr J Clin Med Literat. (2018) 5(04):189–90+92. doi: 10.16281/j.cnki.jocml.2018.04.106
7. Saco-Ledo G, Valenzuela PL, Ruilope LM, Lucia A. Physical exercise in resistant hypertension: a systematic review and meta-analysis of randomized controlled trials. Front Cardiovasc Med. (2022) 9:893811. doi: 10.3389/fcvm.2022.893811
8. Craighead DH, Heinbockel TC, Hamilton MN, Bailey EF, MacDonald MJ, Gibala MJ, et al. Time-efficient physical training for enhancing cardiovascular function in midlife and older adults: promise and current research gaps. J Appl Physiol (1985). (2019) 127(5):1427–40. doi: 10.1152/japplphysiol.00381.2019
9. Fernández-Lázaro D, Gallego-Gallego D, Corchete LA, Fernández Zoppino D, González-Bernal JJ, García Gómez B, et al. Inspiratory muscle training program using the PowerBreath(®): does it have ergogenic potential for respiratory and/or athletic performance? A systematic review with meta-analysis. Int J Environ Res Public Health. (2021) 18(13):6703. doi: 10.3390/ijerph18136703
10. Tavoian D, Ramos-Barrera LE, Craighead DH, Seals DR, Bedrick EJ, Alpert JS, et al. Six months of inspiratory muscle training to lower blood pressure and improve endothelial function in middle-aged and older adults with above-normal blood pressure and obstructive sleep apnea: protocol for the CHART clinical trial. Front Cardiovasc Med. (2021) 8:760203. doi: 10.3389/fcvm.2021.760203
11. de Abreu RM, Catai AM, Cairo B, Rehder-Santos P, da Silva CD, Signini ÉF, et al. A transfer entropy approach for the assessment of the impact of inspiratory muscle training on the cardiorespiratory coupling of amateur cyclists. Front Physiol. (2020) 11:134. doi: 10.3389/fphys.2020.00134
12. Ferreira JB, Plentz RD, Stein C, Casali KR, Arena R, Lago PD. Inspiratory muscle training reduces blood pressure and sympathetic activity in hypertensive patients: a randomized controlled trial. Int J Cardiol. (2013) 166(1):61–7. doi: 10.1016/j.ijcard.2011.09.069
13. Ubolsakka-Jones C, Tongdee P, Jones DA. The effects of slow loaded breathing training on exercise blood pressure in isolated systolic hypertension. Physiother Res Int. (2019) 24(4):e1785. doi: 10.1002/pri.1785
14. Beltrami FG. Is inspiratory muscle training a magic bullet to lower blood pressure? J Appl Physiol (1985). (2020) 129(6):1439. doi: 10.1152/japplphysiol.00803.2020
15. Zhu K, Li N, Peng P. Effects of inspiratory muscle endurance training on pulmonary function, respiratory muscle strength and exercise ability in patients with hypertension. Chin J Physical Med Rehabil. (2021) 43(08):707–11. doi: 10.3760/cma.j.issn.0254-1424.2021.08.009
16. Sangthong B, Ubolsakka-Jones C, Pachirat O, Jones DA. Breathing training for older patients with controlled isolated systolic hypertension. Med Sci Sports Exerc. (2016) 48(9):1641–7. doi: 10.1249/mss.0000000000000967
17. da Silva CD, de Abreu RM, Rehder-Santos P, De Noronha M, Catai AM. Can respiratory muscle training change the blood pressure levels in hypertension? A systematic review with meta-analysis. Scand J Med Sci Sports. (2021) 31(7):1384–94. doi: 10.1111/sms.13943
18. Smith BE, Madigan VM. Understanding the haemodynamics of hypertension. Curr Hypertens Rep. (2018) 20(4):29. doi: 10.1007/s11906-018-0832-8
19. Johnson CA, Burridge JH, Strike PW, Wood DE, Swain ID. The effect of combined use of botulinum toxin type A and functional electric stimulation in the treatment of spastic drop foot after stroke: a preliminary investigation. Arch Phys Med Rehabil. (2004) 85(6):902–9. doi: 10.1016/j.apmr.2003.08.081
20. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. (2009) 339:b2535. doi: 10.1136/bmj.b2535
21. Amir-Behghadami M, Janati A. Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. (2020) 37(6):387. doi: 10.1136/emermed-2020-209567
22. Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. (2018) 138(17):e484–594. doi: 10.1161/cir.0000000000000596
23. Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ. Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther. (2008) 88(2):156–75. doi: 10.2522/ptj.20070147
24. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17(1):1–12. doi: 10.1016/0197-2456(95)00134-4
25. Jones CU, Sangthong B, Pachirat O. An inspiratory load enhances the antihypertensive effects of home-based training with slow deep breathing: a randomised trial. J Physiother. (2010) 56(3):179–86. doi: 10.1016/s1836-9553(10)70023-0
26. Ubolsakka-Jones C, Sangthong B, Khrisanapant W, Jones DA. The effect of slow-loaded breathing training on the blood pressure response to handgrip exercise in patients with isolated systolic hypertension. Hypertens Res. (2017) 40(10):885–91. doi: 10.1038/hr.2017.54
27. Ublosakka-Jones C, Tongdee P, Pachirat O, Jones DA. Slow loaded breathing training improves blood pressure, lung capacity and arm exercise endurance for older people with treated and stable isolated systolic hypertension. Exp Gerontol. (2018) 108:48–53. doi: 10.1016/j.exger.2018.03.023
28. Yuenyongchaiwat K, Thanawattano C, Buranapuntalug S, Pongpanit K, Saengkrut P. Development and application of a respiratory device on blood pressure in adults with high blood pressure. Interv Med Appl Sci. (2019) 11(1):21–6. doi: 10.1556/1646.10.2018.34
29. Craighead DH, Heinbockel TC, Freeberg KA, Rossman MJ, Jackman RA, Jankowski LR, et al. Time-Efficient inspiratory muscle strength training lowers blood pressure and improves endothelial function, NO bioavailability, and oxidative stress in midlife/older adults with above-normal blood pressure. J Am Heart Assoc. (2021) 10(13):e020980. doi: 10.1161/jaha.121.020980
30. Romer LM, McConnell AK. Specificity and reversibility of inspiratory muscle training. Med Sci Sports Exerc. (2003) 35(2):237–44. doi: 10.1249/01.Mss.0000048642.58419.1e
31. Du Z, Bian W, Wu S, Gao B, Sun Y, Kang Z, et al. Effects of blood pressure goals on cardiovascular outcomes in hypertensive patients. Arch Med Sci. (2019) 15(6):1381–7. doi: 10.5114/aoms.2018.80013
32. Shao T, Liang L, Zhou C, Tang Y, Gao W, Tu Y, et al. Short-term efficacy of non-pharmacological interventions for global population with elevated blood pressure: a network meta-analysis. Front Public Health. (2022) 10:1051581. doi: 10.3389/fpubh.2022.1051581
33. Fu J, Liu Y, Zhang L, Zhou L, Li D, Quan H, et al. Nonpharmacologic interventions for reducing blood pressure in adults with prehypertension to established hypertension. J Am Heart Assoc. (2020) 9(19):e016804. doi: 10.1161/jaha.120.016804
34. Canoy D, Copland E, Nazarzadeh M, Ramakrishnan R, Pinho-Gomes AC, Salam A, et al. Antihypertensive drug effects on long-term blood pressure: an individual-level data meta-analysis of randomised clinical trials. Heart. (2022) 108(16):1281–9. doi: 10.1136/heartjnl-2021-320171
35. Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis. Lancet. (2021) 398(10305):1053–64. doi: 10.1016/s0140-6736(21)01921-8
36. Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J Hypertens. (2011) 29(7):1253–69. doi: 10.1097/HJH.0b013e3283469976
37. Pinto MB, Bock PM, Schein ASO, Portes J, Monteiro RB, Schaan BD. Inspiratory muscle training on glucose control in diabetes: a randomized clinical trial. Int J Sport Nutr Exerc Metab. (2021) 31(1):21–31. doi: 10.1123/ijsnem.2020-0175
38. Azambuja ACM, de Oliveira LZ, Sbruzzi G. Inspiratory muscle training in patients with heart failure: what is new? Systematic review and meta-analysis. Phys Ther. (2020) 100(12):2099–109. doi: 10.1093/ptj/pzaa171
39. Zhang X, Zheng Y, Dang Y, Wang L, Cheng Y, Zhang X, et al. Can inspiratory muscle training benefit patients after stroke? A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. (2020) 34(7):866–76. doi: 10.1177/0269215520926227
40. de Abreu RM, Rehder-Santos P, Minatel V, Dos Santos GL, Catai AM. Effects of inspiratory muscle training on cardiovascular autonomic control: a systematic review. Auton Neurosci. (2017) 208:29–35. doi: 10.1016/j.autneu.2017.09.002
41. AlGhatrif M, Lakatta EG. The conundrum of arterial stiffness, elevated blood pressure, and aging. Curr Hypertens Rep. (2015) 17(2):12. doi: 10.1007/s11906-014-0523-z
42. Luecke T, Pelosi P. Clinical review: positive end-expiratory pressure and cardiac output. Crit Care. (2005) 9(6):607–21. doi: 10.1186/cc3877
43. Tuttle WW, Horvath SM. Comparison of effects of static and dynamic work on blood pressure and heart rate. J Appl Physiol. (1957) 10(2):294–6. doi: 10.1152/jappl.1957.10.2.294
44. Dalal J, Dasbiswas A, Sathyamurthy I, Maddury SR, Kerkar P, Bansal S, et al. Heart rate in hypertension: review and expert opinion. Int J Hypertens. (2019) 2019:2087064. doi: 10.1155/2019/2087064
45. Mitsungnern T, Srimookda N, Imoun S, Wansupong S, Kotruchin P. The effect of pursed-lip breathing combined with number counting on blood pressure and heart rate in hypertensive urgency patients: a randomized controlled trial. J Clin Hypertens. (2021) 23(3):672–9. doi: 10.1111/jch.14168
46. de Souza Mesquita FO, Gambassi BB, de Oliveira Silva M, Moreira SR, Neves VR, Gomes-Neto M, et al. Effect of high-intensity interval training on exercise capacity, blood pressure, and autonomic responses in patients with hypertension: a systematic review and meta-analysis. Sports Health. (2022):19417381221139343. doi: 10.1177/19417381221139343. [Epub ahead of print]36529986
47. Wang A, Liu X, Guo X, Dong Y, Wu Y, Huang Z, et al. Resting heart rate and risk of hypertension: results of the kailuan cohort study. J Hypertens. (2014) 32(8):1600–5; discussion 5. doi: 10.1097/hjh.0000000000000230
48. Paul L, Hastie CE, Li WS, Harrow C, Muir S, Connell JM, et al. Resting heart rate pattern during follow-up and mortality in hypertensive patients. Hypertension. (2010) 55(2):567–74. doi: 10.1161/hypertensionaha.109.144808
49. Mello PR, Guerra GM, Borile S, Rondon MU, Alves MJ, Negrão CE, et al. Inspiratory muscle training reduces sympathetic nervous activity and improves inspiratory muscle weakness and quality of life in patients with chronic heart failure: a clinical trial. J Cardiopulm Rehabil Prev. (2012) 32(5):255–61. doi: 10.1097/HCR.0b013e31825828da
50. Mullan SJ, Vricella LK, Edwards AM, Powel JE, Ong SK, Li X, et al. Pulse pressure as a predictor of response to treatment for severe hypertension in pregnancy. Am J Obstetr Gynecol MFM. (2021) 3(6):100455. doi: 10.1016/j.ajogmf.2021.100455
Keywords: hypertension, blood pressure, inspiratory muscle training, IMT, meta—analysis
Citation: Zheng S, Zhang Q, Li S, Li S, Yao Q, Zheng X, Li G, Zeng Y, Chen L, Chen S, He L, Zou J and Zeng Q (2023) Effects of inspiratory muscle training in patients with hypertension: a meta-analysis. Front. Cardiovasc. Med. 10:1113509. doi: 10.3389/fcvm.2023.1113509
Received: 1 December 2022; Accepted: 28 April 2023;
Published: 23 May 2023.
Edited by:
Guido Iaccarino, University of Naples Federico II, ItalyReviewed by:
Daniel Langer, KU Leuven, BelgiumAlexandre Prado, Federal University of Mato Grosso, Brazil
Erik Hulzebos, University Medical Center Utrecht, Netherlands
© 2023 Zheng, Zhang, Li, Li, Yao, Zheng, Li, Zeng, Chen, Chen, He, Zou and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qing Zeng emVuZ3Fpbmd5YW5nMjAzQDEyNi5jb20= Jihua Zou em91amlodWFAaS5zbXUuZWR1LmNu Longlong He OTU3OTk1ODE4QHFxLmNvbQ==
†These authors have contributed equally to this work
 ShuQi Zheng
ShuQi Zheng Qi Zhang
Qi Zhang ShuiYan Li
ShuiYan Li Shilin Li
Shilin Li Qiuru Yao1,3
Qiuru Yao1,3 Gege Li
Gege Li Yuting Zeng
Yuting Zeng Ling Chen
Ling Chen Shuping Chen
Shuping Chen Jihua Zou
Jihua Zou Qing Zeng
Qing Zeng