- 1Department of Echocardiography, ChangZhou No.2 People’s Hospital Affiliated to Nanjing Medical University, Changzhou, China
- 2Cardio-Thoracic Surgery, ChangZhou No.2 People's Hospital Affiliated to Nanjing Medical University, Changzhou, China
Objective: This study aims to investigate the correlation between sleep duration and all-cause and cardiovascular mortality in the general population.
Methods: A total of 26,977 participants aged ≥18 years were included in the analysis from the National Health and Nutrition Examination Survey (NHANES) database covering the period from 2005 to 2014. Data on cardiovascular and all-cause deaths were collected until December 2019. Sleep duration was assessed using a structured questionnaire, and participants were categorized into five groups based on their reported sleep duration (≤5, 6, 7, 8, or ≥9 h). Kaplan-Meier survival curves were employed to examine the mortality rates across different sleep duration groups. Multivariate Cox regression models were utilized to explore the association between sleep duration and mortality. Additionally, a restricted cubic spline regression model was employed to identify the non-linear relationship between sleep duration and all-cause and cardiovascular mortality.
Results: The average age of participants was 46.23 ± 18.48 years, with 49.9% of the subjects being male. Over a median follow-up period of 9.42 years, 3,153 (11.7%) participants died from all-cause mortality, among which 819 (3.0%) were attributed to cardiovascular causes. The groups with sleep durations of ≥9 and ≤5 h exhibited the lowest cumulative survival rates for all-cause mortality and cardiovascular mortality, respectively. When using a sleep duration of 7 h as the reference, the hazard ratios (with 95% confidence intervals) for all-cause mortality were 1.28 (1.14–1.44) for ≤5 h, 1.10 (0.98–1.23) for 6 h, 1.21 (1.10–1.34) for 8 h, and 1.53 (1.35–1.73) for ≥9 h. The hazard ratios (with 95% confidence intervals) for cardiovascular mortality were 1.32 (1.04–1.67) for ≤5 h, 1.22 (0.97–1.53) for 6 h, 1.29 (1.05–1.59) for 8 h, and 1.74 (1.37–2.21) for ≥9 h. A U-shaped non-linear relationship between sleep duration and all-cause and cardiovascular mortality was observed, with inflection point thresholds at 7.32 and 7.04 h, respectively.
Conclusion: The findings suggest that the risk of all-cause and cardiovascular mortality is minimized when sleep duration is approximately 7 h.
1. Introduction
Sleep is a fundamental physiological process that plays a critical role in maintaining human health and overall well-being. It serves as a natural adaptation to the alternation of day and night, regulated by intricate neural mechanisms and following a strict rhythm (1). However, the fast-paced nature of modern life has resulted in significant changes in sleep patterns, posing a significant public health concern. Recent research has placed considerable emphasis on sleep duration and its impact on cardiovascular health (1).
Previous studies have highlighted associations between sleep duration and the prevalence of cardiovascular disease (CVD), suggesting a potential link between insufficient sleep and an elevated risk of CVD and all-cause mortality (2). Some researchers have even proposed sleep duration as a potential predictor of cardiovascular outcomes (3). Additionally, inadequate sleep duration has been linked to a higher risk of developing or dying from coronary heart disease (CHD) and stroke, although not for total CVD (4). On the other hand, an increased risk of CHD, stroke, and total CVD has been associated with long sleep duration (4). Both short and long sleep durations serve as predictors or markers and are associated with a heightened risk of all-cause mortality and cardiovascular events (4, 5). Nevertheless, studies focusing on healthy individuals (6) and middle-aged participants (7) have reported no significant association or correlation between sleep duration and mortality. It is crucial to consider various factors such as differences in research objectives, study designs, sample sizes, follow-up periods, and confounding variables that may influence these findings. Consequently, further investigations are warranted to comprehensively evaluate the relationship between sleep duration and all-cause and cardiovascular mortality.
Given the existing gaps in knowledge, our study aims to explore the association between sleep duration and all-cause and cardiovascular mortality using data obtained from a large cohort of participants included in the National Health and Nutrition Examination Survey (NHANES). As an observational study, our research contributes to the expanding body of evidence on this topic and provides valuable insights into the potential relationship between sleep duration and cardiovascular outcomes.
2. Materials and methods
2.1. Study population and design
The National Center for Health Statistics, a division of the Centers for Disease Control and Prevention, has conducted a series of cross-sectional surveys in the United States known as NHANES since the 1960s. NHANES adheres to the guidelines outlined in the Helsinki Declaration, and all research-related agreements for this survey have undergone review and approval. Written informed consent was obtained from all participants. The NHANES database, containing the information utilized in this study, is publicly accessible online at no cost.
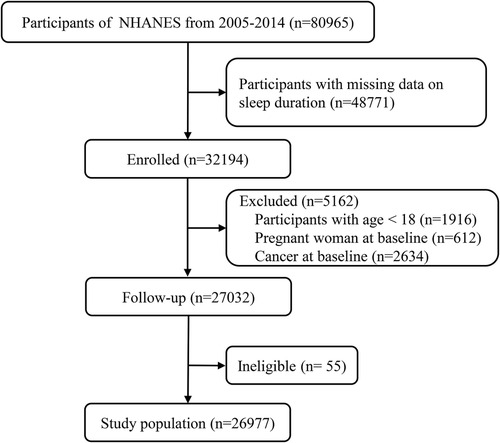
For our study, we analyzed data from a total of 80,965 respondents who participated in surveys conducted between 2005 and 2014. We excluded 48,771 participants due to the absence of sleep duration data, 1,916 participants under the age of 18 years, 612 participants with baseline pregnancy, and 2,634 participants with baseline cancer. The remaining 27,032 participants were tracked for survival until December 2019. During the follow-up period, 55 respondents were excluded due to missing or incomplete data. Ultimately, our final dataset included data from 26,977 respondents (Figure 1).
2.2. Assessment of sleep duration
Sleep pattern data were collected during NHANES surveys conducted from 2005 to 2014. Each participant completed a structured questionnaire that inquired about their sleep and waking times on weekdays and rest days, as well as any nocturnal awakenings. Sleep duration was determined using the following question: “How much sleep do you usually get at night on weekdays or workdays?” Participants provided the number of hours of sleep they typically obtained on a typical night, which was recorded as a continuous variable. Based on recommendations from the American Academy of Sleep Medicine, sleep duration was categorized as follows: ≤5, 6, 7, 8, or ≥9 h (8). The definition was based on the “NHANES Questionnaire” data on “sleep disorders,” and further comprehensive information can be found at the following website: https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/SLQ_H.htm#SLD010H.
2.3. Mortality outcome assessment
Mortality data for this study were extracted from publicly available NHANES mortality documents from 2005 to 2014 and subsequently matched with records from the National Death Index (NDI) to verify mortality status. The primary endpoints assessed in this study were all-cause mortality and cardiovascular mortality. All-cause mortality encompassed death from any cause, while cardiovascular mortality referred to deaths caused by cardiovascular or cerebrovascular disease, according to the International Classification of Diseases, Tenth Revision (ICD-10) (9).
2.4. Data collection
Data from 2005 to 2014 were collected in a standardized manner from structured documents, data sets, and questionnaires included in the NHANES database. Demographic information including age, sex, race (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, or Other Race), and education level (no high school diploma, high school diploma, or education beyond high school diploma) was collected for all participants. Body mass index (BMI) values were obtained (10), and participants were classified into the following categories: underweight (BMI <18.5), healthy weight (BMI 18.5–24.9), overweight (BMI 25–29.9), or obese (BMI ≥30). Hypertension was defined as a systolic blood pressure ≥140 mmHg or a diastolic blood pressure ≥90 mmHg. Participants taking antihypertensive medications or with a known history of hypertension were also considered hypertensive (11). Data regarding total cholesterol, fasting blood glucose, and glycosylated hemoglobin levels were collected, and the glomerular filtration rate (GFR) was estimated. The presence of diabetes was defined as a fasting blood glucose level ≥126 mg/dl or a hemoglobin A1c value ≥6.5%. Participants who self-reported having diabetes or used hypoglycemic medications were also considered diabetic (12). The GFR was calculated using the standard kidney disease formula (13). Participants with CVD were defined as those who had been diagnosed with at least one of the following conditions: CHD, congestive heart failure, angina pectoris, myocardial infarction, or stroke. Other covariates assessed included physical activity, smoking status, and drinking status. Physical activity levels were classified as inactive (no physical activity), insufficiently active (some physical activity), or active (≥5 sessions of moderate exercise or ≥3 sessions of strenuous exercise per week) (14). Smoking status was categorized as never smokers (participants who have smoked <100 cigarettes during their lifetime), former smokers (participants who have smoked >100 cigarettes but have quit smoking), or current smokers (participants who have smoked >100 cigarettes and currently smoke) (15). Drinking status was classified as nondrinker, low-to-moderate drinker (<2 drinks/day in men and <1 drink/day in women), or heavy drinker (≥2 drinks/day in men and ≥1 drinks/day in women) (16).
2.5. Statistical analysis
Data analysis and graphical visualization were performed using R project (version 4.1.1). Continuous variables with a normal distribution were reported as mean ± standard deviation (SD), while continuous variables with a non-normal distribution were presented as median (quartile interval). Categorical variables were expressed as numbers and percentages. Kaplan-Meier (KM) curves were generated to illustrate the relationship between sleep duration and all-cause and cardiovascular mortality.
To assess the impact of sleep duration on mortality, multivariate Cox proportional hazard regression analysis was conducted. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated for different sleep durations. The assumption of proportional hazards required by the Cox model was evaluated using Schoenfeld residuals, and no violations were observed. Additionally, variance inflation factors (VIF) were calculated to examine multicollinearity among the independent variables in the multiple Cox model. Three multivariate Cox regression models were constructed with different adjustments of covariates. Model 1 included adjustments for age, sex, and race. Model 2 included the covariates from Model 1 and further adjusted for education level, drinking status, smoking status, BMI, and physical activity. Model 3 incorporated the covariates from Models 1 and 2, with additional adjustments for total cholesterol level, GFR, and the presence of hypertension, diabetes, and CVD. A sleep duration of 7 h served as the reference category. To explore the potential nonlinear association between sleep duration and all-cause mortality as well as cardiovascular mortality, a multivariate adjusted Cox restricted cubic spline regression model was employed. If a nonlinear relationship was observed, the threshold point was estimated and further explored. Statistical significance was defined as p-values <0.05.
3. Results
3.1. Population characteristics
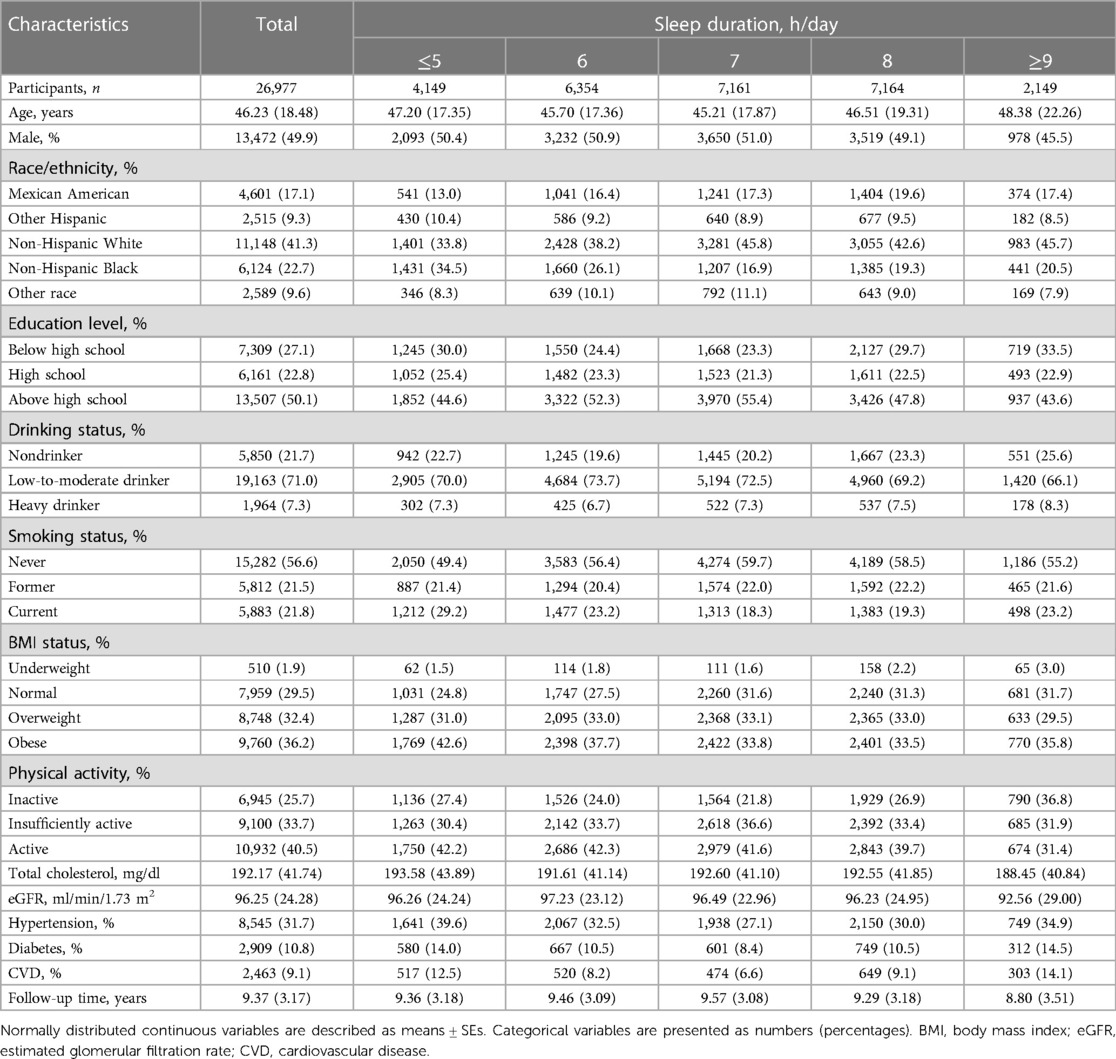
A total of 26,977 participants (49.9% male) were included in the final dataset, with a mean age of 46.23 ± 18.48 years. Among the participants, 41.3% were classified as Non-Hispanic White, 50.1% had an education level beyond a high school diploma, 71.0% were categorized as low to moderate drinkers, and 40.5% were considered physically active. Out of all participants, 8,545 (31.7%) were never smokers. The prevalence of hypertension, diabetes, and CVD was 31.7%, 10.8%, and 9.1%, respectively. The mean total cholesterol level was 192.17 ± 41.74 mg/dl, and the mean estimated GFR was 96.26 ± 24.28 ml/min/1.73 m2 (Table 1).
3.2. Relationships between sleep duration and mortality
During a median follow-up of 9.42 years, a total of 3,153 (11.7%) participants died from all-cause mortality, including 819 (3.0%) cardiovascular deaths. The three multivariate Cox regression models consistently showed the association between sleep duration and all-cause and cardiovascular mortality across various subgroups (Table 2).

Table 2. Hrs (95% CIs) of all-cause and cardiovascular mortality according to sleep duration among adults in NHANES 2005–2014.
Overall, the group with sleep duration ≥9 h exhibited the highest risk for all-cause mortality (log-rank P for trend vs. reference <0.001) (Figure 2A). Across all three models, both longer sleep durations (≥9 and 8 h) and shorter sleep durations (≤5 h) were associated with a higher risk of all-cause mortality (Table 2).
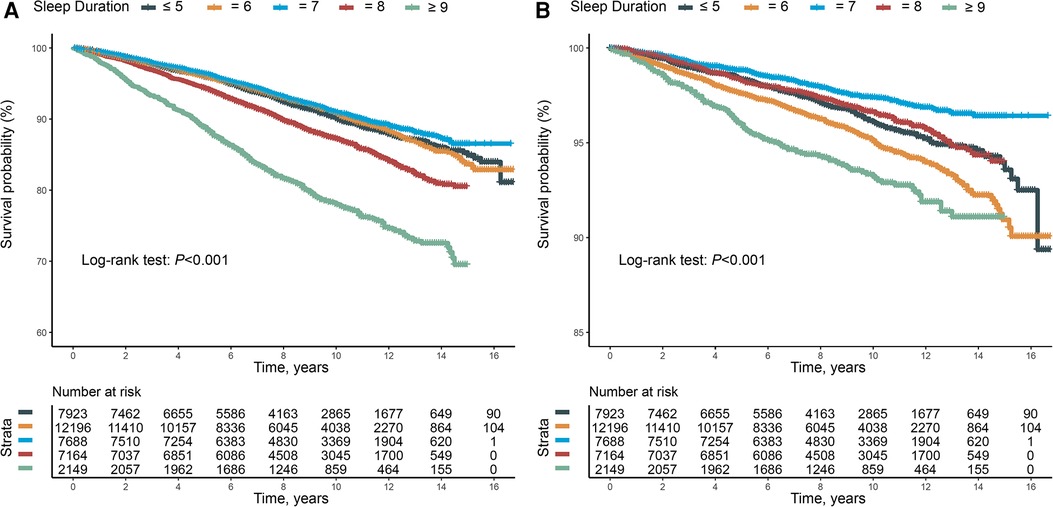
Figure 2. (A) Kaplan–Meier survival curve for all-cause mortality. (B) Kaplan–Meier survival curve for cardiovascular mortality.
Similarly, sleep durations longer or shorter than the reference of 7 h were associated with an increased risk of cardiovascular mortality (log-rank P for trend vs. reference <0.001) (Figure 2B). Consistent with the findings for all-cause mortality, both longer sleep durations (≥9 and 8 h) and shorter sleep durations (≤5 h) were associated with an increased risk of cardiovascular mortality across all three models (Table 2).
3.3. Nonlinear relationships between sleep duration and mortality
A U-shaped association was observed between sleep duration and both all-cause mortality (Figure 3A) and cardiovascular mortality (Figure 3B). The hazard ratio (HR) for all-cause mortality decreased to the lowest point when sleep duration was 7.32 h and increased significantly with longer sleep duration. The threshold for sleep duration in relation to cardiovascular mortality was 7.04 h. The HR for cardiovascular mortality showed a downward trend when sleep duration was less than 7.04 h and an upward trend when sleep duration exceeded 7.04 h, although the upward trend was not as pronounced as that observed for all-cause mortality.
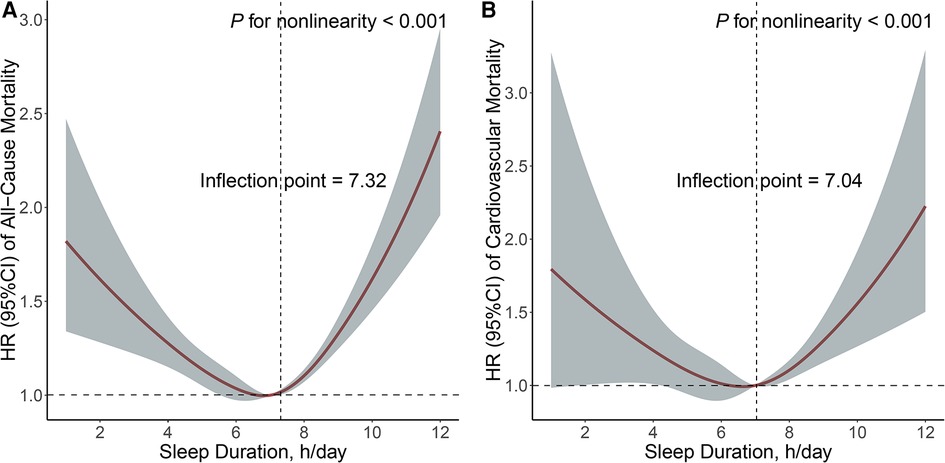
Figure 3. Non-linear relationship between sleep duration and all-cause (A) and cardiovascular (B) mortality. Adjusted for age, sex, and race, education level, drinking status, smoking status, BMI, physical activity, total cholesterol, GFR, hypertension, diabetes, and CVD.
4. Discussion
In this large, long-term study, we observed that the optimal sleep duration associated with the lowest risk of all-cause and cardiovascular mortality was approximately 7 h. These results confirm the findings from a previous cross-sectional study of sleep duration and cardiovascular health (17) and reinforce the detrimental impact of sleep disorders on cardiovascular health.
The American Academy of Sleep Medicine, the Sleep Research Society, and the National Sleep Foundation define “short sleep” as a duration of less than 7 h per night (18, 19). Although there is some variation in the definitions used across studies, it is important to note that our results align with the recommendation of 7 h of sleep per night as outlined in a 2015 consensus statement by the American Academy of Sleep Medicine and the Sleep Research Society (20). This statement emphasized that sleep durations below 7 h can impair immune function, affect metabolism, and have adverse effects on cardiovascular, cerebrovascular, and mental health. Furthermore, insufficient sleep has been associated with increased risks of obesity, diabetes, hypertension, heart disease, stroke, depression, and mortality (20). Several population-based cohort studies have consistently shown that individuals with shorter sleep durations are at higher risk of all-cause and cardiovascular death (21–23). Our findings reinforce these previous observations, indicating that a sleep duration of approximately 7 h represents a threshold for increased risk, with significantly shorter sleep durations corresponding to higher mortality risk.
Researchers have made efforts to elucidate the underlying mechanisms linking short sleep duration and increased cardiovascular risk. One potential mechanism involves metabolic dysregulation associated with inadequate sleep. Abnormalities in the release of peptides and leptin, which are involved in regulating energy intake, may contribute to this process. Peptides stimulate hunger and increase appetite, while leptin inhibits hunger and reduces appetite (24). Recent studies have demonstrated that shorter sleep durations can promote peptide release and inhibit leptin release, leading to increased food intake, weight gain, decreased insulin sensitivity, and elevated blood glucose levels, ultimately contributing to obesity and impaired glucose tolerance (25). Sleep duration has also been correlated with lipid metabolism. A recent study revealed a significant nonlinear association between short sleep duration and low high-density lipoprotein (HDL) levels and high triglyceride levels (26). Another proposed mechanism involves the neuro regulation of central body tissues. In individuals with insufficient sleep, increased stimulation of the cardiovascular sympathetic nerves results in heightened tension, reduced parasympathetic activity, elevated heart rate, and heightened reactivity, ultimately leading to increased blood pressure and vascular endothelial cell damage (27). Additionally, a study found that short sleep duration leads to decreased blood flow velocity in the cerebral basilar artery and midbrain, resulting in regional inadequate blood supply to the brain and triggering oxidative stress, inflammation, platelet dysfunction, and metabolic disorders (28).
The definition of “long sleep” is not well-defined, similar to “short sleep.” The consensus statement from the American Academy of Sleep Medicine and the Sleep Research Society stated that it remains uncertain whether sleep durations exceeding 9 h per night are associated with health risks for the general population, excluding individuals who are ill or have missed sleep (7). Recent Mendelian randomization studies have suggested a potential causal link between short sleep duration and CVD, but not for long sleep duration (29, 30). While our study found an increased risk of all-cause and cardiovascular mortality among individuals who slept more than 7 h per night, even after adjusting for covariates, we acknowledge that our findings do not establish a causal relationship. It is important to consider confounding factors in observational studies, such as conditions like depression, antidepressant use, or poor sleep quality, which can lead to longer sleep duration. These factors may confound the observed association, and the increased risk of CVD associated with long sleep duration could reflect underlying health conditions or residual confounding rather than a direct causal relationship.
The potential mechanisms underlying the association between long sleep duration and increased cardiovascular risk have also been investigated. An analysis of data from the Korea National Health and Nutrition Examination Survey (KNHANES) demonstrated a significant correlation between sleep duration of 9 h or more and low high-density lipoprotein cholesterol (HDL-C) levels (31). Another analysis found a positive correlation between longer sleep durations and increased levels of C-reactive protein (CRP) and interleukin-6 (IL-6) (32). In women, CRP levels were approximately 44% higher in those with habitual sleep duration of 9 h or more compared to those with 8 h of sleep after adjusting for age and BMI (33). CRP production is stimulated by IL-6, suggesting that the correlation between sleep duration and CRP levels may be secondary to the effect of sleep duration on IL-6 levels. Increased levels of CRP and IL-6 have previously been associated with an elevated risk of CVD and diabetes. Therefore, similar to short sleep duration, one potential mechanism by which long sleep duration may impact cardiovascular health is through the activation of inflammatory pathways. Insulin resistance may also play a role in the association between long sleep duration and cardiovascular risk. A study of nurses found that regular sleep durations exceeding 9 h were associated with a 47% increased risk of diabetes and a 57% increased risk of cardiac events (34, 35). Another recent study reported an increased risk of all-cause mortality among adult patients with type 2 diabetes who slept more than 7 h per night (36). Insulin resistance is a key risk factor for diabetes, and long sleep duration may contribute to an increased risk of insulin resistance through factors such as lack of physical activity, chronic inflammation, and disturbance of circadian rhythm. Furthermore, a prospective analysis of elderly individuals in China revealed that excessive sleep duration was associated with an increased risk of cognitive impairment, suggesting the need for early attention to neurodegeneration (37). Lastly, prolonged sleep duration may be associated with factors such as undiagnosed chronic conditions, depression, unemployment, low socioeconomic status, and reduced physical activity, which could further contribute to increased cardiovascular morbidity and mortality in these individuals (38).
A recent study found that both short sleep and long sleep were associated with an increased 10-year risk of CHD (39). However, a previous meta-analysis demonstrated that long sleep was more strongly correlated with adverse outcomes than short sleep, and the association between long sleep and mortality was not attenuated by improvements in health or lifestyle (40). In our study, the steep increase in the curve for all-cause mortality compared to cardiovascular mortality may be attributed to undiagnosed chronic complications among participants. This finding is highly consistent with previous studies that have reported an association between long sleep duration and increased mortality, particularly for non-cardiovascular cause (41, 42). Some researchers have even proposed using long sleep duration as a diagnostic tool for detecting subclinical or undiagnosed physical and mental disorders (43).
Our study had several strengths, including a relatively large sample size and a long follow-up period. However, it is important to acknowledge certain limitations inherent in our research. Firstly, while we were able to quantitatively measure the duration of sleep, the overall assessment of sleep is multifaceted and involves various aspects such as circadian rhythm, sleep initiation and maintenance difficulties, and sleep-related breathing disorders. Moreover, it is important to note that sleep patterns may change over time. Our study relied on a single assessment of sleep patterns at baseline, and we did not collect follow-up data to capture potential changes in sleep duration or quality during the study period. These aspects were not comprehensively captured in our study, which may have limited our understanding of the complexity of sleep patterns and their potential effects on health outcomes. Secondly, our study relied on self-reported sleep data, which introduces the possibility of memory biases and inaccuracies in reporting. Objective measures of sleep, such as polysomnography or actigraphy, could provide more precise and detailed information on sleep patterns and help overcome these limitations. Finally, while we made efforts to control for numerous confounding factors, it is possible that unmeasured confounders may exist. It is worth highlighting that our study did not include laboratory investigations such as inflammatory markers or hormone levels. As a result, our observations regarding potential underlying mechanisms remain largely speculative, and further research incorporating these measures is warranted to provide a more comprehensive understanding of the relationships between sleep duration and health outcomes.
5. Conclusion
In this large-scale, long-term study, we have further clarified the exact relationship between sleep duration and all-cause and cardiovascular mortality in American adults, demonstrating that the risk of all-cause and cardiovascular mortality was lowest when sleep duration was approximately 7 h. However, the pathophysiological mechanisms linking sleep disorders and negative prognosis require further investigation. Future studies should focus on understanding the underlying mechanisms and determining whether interventions targeting both sleep duration and quality can effectively reduce morbidity and mortality rates. These studies will be crucial in developing strategies to improve sleep-related health outcomes.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The local institutional ethics committee granted a waiver of review and approval for this study. The original research agreements for the NHANES study have been reviewed and approved, and written informed consent has been obtained from all participants. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JL and MZ made significant contributions to the design of this study. JL analyzed and interpreted the data and drafted the manuscript. QW, LF, ZY and DS reviewed the previous literature and made significant contributions to the revision of the manuscript. MZ was responsible for the quality of the entire manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Science and Technology Support Plan of Changzhou (CE20205047) and Bureau Level Project of Changzhou (ZD201605).
Acknowledgments
The authors acknowledge the efforts of all staff working on The National Health and Nutrition Examination Survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wolk R, Gami AS, Garcia-Touchard A, Somers VK. Sleep and cardiovascular disease. Curr Probl Cardiol. (2005) 30(12):625–62. doi: 10.1016/j.cpcardiol.2005.07.002
2. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. (2017) 32:246–56. doi: 10.1016/j.sleep.2016.08.006
3. Yin J, Jin X, Shan Z, Li S, Huang H, Li P, et al. Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc. (2017) 6(9):e005947. doi: 10.1161/JAHA.117.005947
4. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. (2011) 32(12):1484–92. doi: 10.1093/eurheartj/ehr007
5. Kakizaki M, Kuriyama S, Nakaya N, Sone T, Nagai M, Sugawara Y, et al. Long sleep duration and cause-specific mortality according to physical function and self-rated health: the Ohsaki cohort study. J Sleep Res. (2013) 22(2):209–16. doi: 10.1111/j.1365-2869.2012.01053.x
6. Magee CA, Holliday EG, Attia J, Kritharides L, Banks E. Investigation of the relationship between sleep duration, all-cause mortality, and preexisting disease. Sleep Med. (2013) 14(7):591–6. doi: 10.1016/j.sleep.2013.02.002
7. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. (2008) 31(8):1087–96.18714780
8. Mercy UC, Elenwa F, Ogunsola AS, Eniola OA, Yunusa I, Karaye IM. Sex differences in the association between short sleep duration and obesity among US adults: findings from NHANES, 2015-2020. Sleep Med. (2022) 92:59–63. doi: 10.1016/j.sleep.2022.03.004
9. Tan QH, Huang YQ, Liu XC, Liu L, Lo K, Chen JY, et al. A U-shaped relationship between selenium concentrations and all-cause or cardiovascular mortality in patients with hypertension. Front Cardiovasc Med. (2021) 8:671618. doi: 10.3389/fcvm.2021.671618
10. Caballero B. Humans against obesity: who will win? Adv Nutr. (2019) 10(Suppl_1):S4–9. doi: 10.1093/advances/nmy055
11. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. (2003) 42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2
12. Wang J, Thomas J, Byrd D, Nola K, Liu J. Status of diabetes care among community pharmacy patients with diabetes: analysis of the medical expenditure panel survey. J Am Pharm Assoc. (2010) 50(4):478–84. doi: 10.1331/JAPhA.2010.08173
13. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. (2002) 39(2 Suppl 1):S1–266.11904577
14. Beddhu S, Baird BC, Zitterkoph J, Neilson J, Greene T. Physical activity and mortality in chronic kidney disease (NHANES III). Clin J Am Soc Nephrol. (2009) 4(12):1901–6. doi: 10.2215/cjn.01970309
15. Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. National health and nutrition examination survey. J Periodontol. (2000) 71(5):743–51. doi: 10.1902/jop.2000.71.5.743
16. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American gastroenterological association, American association for the study of liver diseases, and American college of gastroenterology. Gastroenterology. (2012) 142(7):1592–609. doi: 10.1053/j.gastro.2012.04.001
17. Krittanawong C, Kumar A, Wang Z, Jneid H, Baber U, Mehran R, et al. Sleep duration and cardiovascular health in a representative community population (from NHANES, 2005 to 2016). Am J Cardiol. (2020) 127:149–55. doi: 10.1016/j.amjcard.2020.04.012
18. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. (2015) 38(8):1161–83. doi: 10.5665/sleep.4886
19. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1(1):40–3. doi: 10.1016/j.sleh.2014.12.010
20. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep. (2015) 38(6):843–4. doi: 10.5665/sleep.4716
21. Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. (2009) 32(3):295–301. doi: 10.1093/sleep/32.3.295
22. Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, et al. Insomnia with short sleep duration and mortality: the penn state cohort. Sleep. (2010) 33(9):1159–64. doi: 10.1093/sleep/33.9.1159
23. Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Med. (2011) 12(1):28–33. doi: 10.1016/j.sleep.2010.04.016
24. Prinz P. Sleep, appetite, and obesity–what is the link? PLoS Med. (2004) 1(3):e61. doi: 10.1371/journal.pmed.0010061
25. Reilly JJ, Ness AR, Sherriff A. Epidemiological and physiological approaches to understanding the etiology of pediatric obesity: finding the needle in the haystack. Pediatr Res. (2007) 61(6):646–52. doi: 10.1203/pdr.0b013e3180536667
26. Smiley A, King D, Harezlak J, Dinh P, Bidulescu A. The association between sleep duration and lipid profiles: the NHANES 2013-2014. J Diabetes Metab Disord. (2019) 18(2):315–22. doi: 10.1007/s40200-019-00415-0
27. Tamisier R, Weiss JW, Pépin JL. Sleep biology updates: hemodynamic and autonomic control in sleep disorders. Metab Clin Exp. (2018) 84:3–10. doi: 10.1016/j.metabol.2018.03.012
28. Yang D, Rundek T, Patel SR, Cabral D, Redline S, Testai FD, et al. Cerebral hemodynamics in sleep apnea and actigraphy-determined sleep duration in a sample of the hispanic community health study/study of latinos. J Clin Sleep Med. (2019) 15(1):15–21. doi: 10.5664/jcsm.7560
29. Ai S, Zhang J, Zhao G, Wang N, Li G, So HC, et al. Causal associations of short and long sleep durations with 12 cardiovascular diseases: linear and nonlinear Mendelian randomization analyses in UK biobank. Eur Heart J. (2021) 42(34):3349–57. doi: 10.1093/eurheartj/ehab170
30. Wang S, Li Z, Wang X, Guo S, Sun Y, Li G, et al. Associations between sleep duration and cardiovascular diseases: a meta-review and meta-analysis of observational and Mendelian randomization studies. Front Cardiovasc Med. (2022) 9:930000. doi: 10.3389/fcvm.2022.930000
31. Shin HY, Kang G, Kim SW, Kim JM, Yoon JS, Shin IS. Associations between sleep duration and abnormal serum lipid levels: data from the Korean national health and nutrition examination survey (KNHANES). Sleep Med. (2016) 24:119–23. doi: 10.1016/j.sleep.2016.05.012
32. Patel SR, Zhu X, Storfer-Isser A, Mehra R, Jenny NS, Tracy R, et al. Sleep duration and biomarkers of inflammation. Sleep. (2009) 32(2):200–4. doi: 10.1093/sleep/32.2.200
33. Williams CJ, Hu FB, Patel SR, Mantzoros CS. Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes. Diabetes Care. (2007) 30(5):1233–40. doi: 10.2337/dc06-2107
34. Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. (2003) 163(2):205–9. doi: 10.1001/archinte.163.2.205
35. Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. (2003) 26(2):380–4. doi: 10.2337/diacare.26.2.380
36. Wang Y, Huang W, O'Neil A, Lan Y, Aune D, Wang W, et al. Association between sleep duration and mortality risk among adults with type 2 diabetes: a prospective cohort study. Diabetologia. (2020) 63(11):2292–304. doi: 10.1007/s00125-020-05214-4
37. Zhang M, Lv X, Chen Y, Tu L, Fan Z, Yao Y, et al. Excessive sleep increased the risk of incidence of cognitive impairment among older Chinese adults: a cohort study based on the Chinese longitudinal healthy longevity survey (CLHLS). Int Psychogeriatr. (2022) 34(8):725–34. doi: 10.1017/s1041610221000168
38. Stranges S, Dorn JM, Shipley MJ, Kandala NB, Trevisan M, Miller MA, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the whitehall II study and the western New York health study. Am J Epidemiol. (2008) 168(12):1353–64. doi: 10.1093/aje/kwn337
39. Çakır H, Güneş A, Er F, Çakır H, Karagöz A, Yılmaz F, et al. Evaluating the relationship of sleep quality and sleep duration with framingham coronary heart disease risk score. Chronobiol Int. (2022) 39(5):636–43. doi: 10.1080/07420528.2021.2018453
40. Kwok CS, Kontopantelis E, Kuligowski G, Gray M, Muhyaldeen A, Gale CP, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. (2018) 7(15):e008552. doi: 10.1161/jaha.118.008552
41. Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. (2004) 27(1):51–4.14998237
42. Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. (2004) 27(3):440–4. doi: 10.1093/sleep/27.3.440
Keywords: NHANES, sleep duration, CVD, mortality, all-cause
Citation: Li J, Wu Q, Fan L, Yan Z, Shen D and Zhang M (2023) Nonlinear associations between sleep duration and the risks of all-cause and cardiovascular mortality among the general adult population: a long-term cohort study. Front. Cardiovasc. Med. 10:1109225. doi: 10.3389/fcvm.2023.1109225
Received: 27 November 2022; Accepted: 5 June 2023;
Published: 14 June 2023.
Edited by:
Donglan Zhang, University of Georgia, GeorgiaReviewed by:
Sizhi Ai, The First Affiliated Hospital of Xinxiang Medical University, ChinaFilippo Luca Gurgoglione, University Hospital of Parma, Italy
© 2023 Li, Wu, Fan, Yan, Shen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming Zhang emhhbmdtaW5nbHBAMTI2LmNvbQ==
 Jie Li
Jie Li Qiyong Wu
Qiyong Wu Li Fan1
Li Fan1