
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cardiovasc. Med. , 01 February 2023
Sec. Heart Failure and Transplantation
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1107672
 Longmei Yan1,2,3
Longmei Yan1,2,3 Yuzhen Ai4
Yuzhen Ai4 Yaxuan Xing1,2
Yaxuan Xing1,2 Biqing Wang1,2,3
Biqing Wang1,2,3 Anran Gao1,2,3
Anran Gao1,2,3 Qiwu Xu1,2,3
Qiwu Xu1,2,3 Hongzheng Li1,2,3
Hongzheng Li1,2,3 Keji Chen1,2
Keji Chen1,2 Jingchun Zhang1,2*
Jingchun Zhang1,2*Background: Depression is an independent factor to predict the hospitalization and mortality in the chronic HF patients. Citalopram is known as an effective drug for depression treatment. Currently, there is no specific recommendation in the HF guidelines for the treatment of psychological comorbidity. In recent years, many studies have shown that the citalopram may be safe in treating of chronic HF with depression.
Objective: To evaluate the efficacy and safety of the citalopram in the treatment of elderly chronic HF combined with depression.
Methods: PubMed, EMBASE, Cochrane, Web of Science, CNKI, VIP, CBM, and Wanfang were searched from their inception to May 2022. In the treatment of elderly chronic HF combined with depression, randomized controlled studies of the citalopram were included. Independent screening and extraction of data information were conducted by two researchers, and the quality was assessed by the Cochrane bias risk assessment tool. Review manager 5.4.1 was employed for statistical analysis.
Results: The results of meta-analysis prove that the citalopram treatment for depressed patients with chronic HF has a benefit for HAMD-24 (MD: −8.51, 95% CI: −10.15 to −6.88) and LVEF (MD: 2.42, 95% CI: 0.51 to 4.33). Moreover, the score of GDS decreases, and NT-proBNP (MD: −537.78, 95% CI: −718.03 to −357.54) is improved. However, the comparison with the control group indicates that there is no good effect on HAMD-17 (MD: −5.14, 95% CI: −11.60 to 1.32), MADRS (MD: −1.57, 95% CI: −3.47 to 0.32) and LVEDD (MD: −1.45, 95% CI: −3.65 to −0.76). No obvious adverse drug reactions were observed.
Conclusion: Citalopram treatment for depressed patients with chronic HF has a positive effect on LVEF and NT-proBNP. It can alleviate HAMD-24 and GDS, but the relative benefits for LVEDD, HAMD-17 and MADRS still need to be verified.
Systematic Review Registration: PROSPERO [CRD42021289917].
Heart failure (HF) is the end stage of various cardiovascular diseases. Due to the disease and psychological pressure, experience depression may prolonged duration of illness. The prevalence of depression is significantly higher in HF patients than that in the general population (1–3). The incidence of HF combined with depression ranged from 31.0 to 77.5% (4). As the severity of HF increases, the incidence of depression increases (3). It leads to the frequent hospitalization, high medical expenses, heavy burden to family and social medical treatment, which seriously reduces the life quality of patients (5).
Cardiovascular disease combined with psychological problems has attracted the increasing attention. In 2014, the American Heart Association issued a scientific statement that depression was one of the risk factors for heart disease (6). Depression can increase the morbidity and mortality of heart disease (7), while the mechanism is not clear. Depression is extremely common prevalent in HF patients (8), which is an independent predictor of hospitalization and mortality in HF patients (9). The European Society of Cardiology (ESC) and American College of Cardiology/American Heart Association (ACC/AHA) HF guidelines recommend screening and treating depression in HF patients (10, 11). Due to the overlap between cardiac and psychological symptoms, multiple challenges are encountered in the recognition and management of depression in patients with HF. Currently, HF guidelines are deficient in the management of depression (12). And the effectiveness of antidepressant therapy on the outcome for patients with chronic HF and depression is controversial.
Citalopram is a selective serotonin reuptake inhibitors (SSRIs), composed of two enantiomers, R-citalopram and S-citalopram, which exerts an antidepressant effect by inhibiting the neurological reuptake of 5-HT (13). As for Escitalopram (the S-(+)-enantiomer of citalopram), the inhibitory function on 5-HTT is approximately twice more than that of the citalopram (14). It has a good curative effect and patient acceptability (15). SSRIs can lead to QTc prolongation, the citalopram and escitalopram have also been confirmed as being responsible for QTc prolongation and thus the danger of possible arrhythmias (16, 17). It should be noted that SSRIs do cause the QTc prolongation, to a much lower degree than the older tricyclic antidepressants (TCAs) (17). As such, SSRIs appear to be a safe treatment option for depression in chronic HF patients (18). Depression can aggravate the patient progress, while the HF can further aggravate the depression. Regarding the patients with chronic HF and depression, we can learn from complex interplay of cardiac physiology and social psychology. The researches of depression and HF are very complex. However, there are a number of pathophysiological interaction mechanisms which are important in exploring available ways to alleviate the depression and improve cardiac function.
To date, there is no evidence that antidepressant treatment can improve the symptoms in patients with chronic HF, and the HF guidelines do not contain specific recommendations for treating psychological comorbidity (12). This study conducted a meta-analysis of data from domestic and international clinical trials to evaluate whether the citalopram is a safe and effective treatment for chronic HF with depression, which may provide a reference for clinical practice and research.
This systematic review is abided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (19). The study was registered at the PROSPERO (ID CRD 42021289917) in December 2021.
An article search was carried out in the following eight databases from its establishment to May 2022, including PubMed, Web of Science, Cochrane Library, Embase, CNKI, VIP, CBM, and Wanfang. The language was restricted to Chinese and English. In these databases, “citalopram,” “heart failure” and “depression” were used as the subject words. The combination of MeSH keywords and free words were used for the search. We also searched the conference abstracts, dissertations and other grey papers. Manual retrieval of all references was summarized in review. Specific retrieval strategy was presented in Supplementary Table 1, and the last retrieval was conducted in 2022.
The following studies were included in the meta-study: (1) Type of study: randomized controlled trials (RCTs); (2) Study object: included participants were adults aged 60 or older; (3) Content standard: met the diagnostic criteria for HF and depression, Diagnostic criteria for HF: met Chronic Heart Failure (20) or met New York Heart Association class (NYHA). Diagnostic criteria for depression: no clear standardized diagnostic criteria for depression, met diagnostic criteria for depression, such as (CCMD-3, DSM-IV, and ICD-10), or assessed with any validated depression scale (HAMD-17, HAMD-24, GDS, and MARDS); (4) Intervention measure: citalopram was used as an intervention drug (dosage form and manufacturer were not limited); and (5) Outcome indicators: Depression score (HAMD-17, HAMD-24, GDS, and MARDS) and Left ventricular ejection fractions (LVEF) as the primary outcome indicators; Left ventricular end diastolic diameter (LVEDD), N-terminal prohormone of brain natriuretic peptide (NT-proBNP) as the primary outcome indicators; adverse reactions such as nausea, vomiting, dizziness, fatigue, and insomnia were safety outcome indicators.
Studies meeting the following criteria were excluded: (1) duplicated publications; (2) animal studies, research protocols and review articles; (3) the use of any other herbal medicines during the research; and (4) the use of antidepressants other than the citalopram.
Two researchers (LY and XY) independently screened and extracted the data according to the inclusion and exclusion criteria. Then their results were cross-checked. Any disagreements were resolved by a third party (BW).
The risk bias assessment tool recommended by the Cochrane Collaboration was used to evaluate the quality of included literature. Several bias were successively assessed, such as Random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome date (attrition bias), selective reporting (reporting bias) and other. Risk bias was assessed for each project through three levels: “low risk, unclear and high risk.”
Review manager 5.4.1 was used for data meta-analysis. Q test and I2 value were used to evaluate the heterogeneity among the included studies. If p > 0.1 and I2 < 50%, the heterogeneity across studies were considered relatively small, and a fixed effect model was adopted; otherwise, a random effect model was used. For higher heterogeneity, subgroup analyses were conducted to explore the sources of heterogeneity. A sensitivity analysis was performed to check the result stability. More than 10 trials were included, publication bias would be evaluated by funnel plot.
A total of 164 studies were retrieved through the search strategy. After excluding 84 duplications, the remaining studies were screened based on their titles and abstracts, and 60 irrelevant studies were removed. Ten studies were excluded by reading the full text. Six articles were excluded due to age less than 60. Finally, eight randomized controlled studies were included in the meta-analysis (Figure 1).
A total of eight studies met the inclusion criteria, involving 1,141 patients (573 experimental and 568 control). The age of all the participants was over 60 years. These studies were carried out from 2011 to 2020. The basic characteristics of these included studies are shown in Table 1.
The inclusion of eight randomized trials were evaluated by the Cochrane risk bias assessment tool. All studies used the random method, in which three of the studies were conducted using the random number table method. All studies failed to mention the allocation concealment method. Five studies described the blind method, and three of the studies reported the double-blind method for patients. The quality and bias risks of studies are assessed in Figures 2, 3.
There were six studies to report the LVEF results, involving 761 patients. The heterogeneity test showed the statistical significance (p = 0.0001, I2 = 80%), so we used the random effect model. We conducted a sensitivity analysis and removed the two studies. It was found that the heterogeneity was I2 = 47%, which might be related to its quality. The results of the meta-analysis showed that the difference between two groups was statistically significant (MD = 2.42, 95% CI: 0.51 to 4.33; p = 0.01; shown in Figure 4). This result indicated that the experimental group was better than the control group.
There were five studies to report the LVEDD results, involving 650 patients. The heterogeneity test showed statistical significance (p = 0.0004, I2 = 81%), so we used the random effect model. The results of the meta-analysis showed that the difference between two groups was statistically significant (MD = −1.45, 95% CI: −3.65 to 0.76; p = 0.20; shown in Figure 5). This result indicated that there was no significant difference between these two groups.
There were three studies to report the NT-proBNP results, involving 319 patients. The heterogeneity test showed statistical significance (p = 0.0001, I2 = 89%), so we used the random effect model. The results of the meta-analysis showed that the difference between two groups was statistically significant (MD = −537.78, 95% CI: −718.03 to −357.54; p < 0.00001; shown in Figure 6). This result indicated that the experimental group was better than the control group.
There were two studies to report the HAMD-17 score results, involving 218 patients. The heterogeneity test showed statistical significance (p < 0.00001, I2 = 95%), so we used the random effect model. The results of the meta-analysis showed that the difference between two groups was statistically significant (MD = −5.14, 95% CI: −11.60 to 1.32; p = 0.12; shown in Figure 7). This result indicated that the two groups had no significant difference.
There were two studies to report HAMD-24 score results, involving 142 patients. The heterogeneity test showed statistical significance (p = 0.56, I2 = 0%), so we used the random effect model. The results of the meta-analysis showed that the difference between two groups was statistically significant (MD = −8.51, 95% CI: −10.15 to −6.88; p < 0.00001; shown in Figure 8). This result indicated that the experimental group was better than the control group.
There were two studies to report MADRS score results, involving 272 patients. The heterogeneity test showed the statistical significance (p = 0.042, I2 = 0%), so we used the fix effect model. The results of the meta-analysis showed that the difference between two groups was statistically significant (MD = −1.57, 95% CI: −3.47 to 0.32; p = 0.10; shown in Figure 9). This result suggested that the two groups had no significant difference.
A study (25) using the GDS showed that both the observation and control groups had lower GDS scores after treatment than before treatment (12.53 ± 3.61 vs. 17.45 ± 4.31; 11.73 ± 2.96 vs. 17.22 ± 3.87, p = 0.000). The GDS score of observation group was significantly lower than that in the control group for moderate–severe depression patients (12.78 ± 2.46 vs. 14.96 ± 3.41, p = 0.012).
Since less than 10 articles were included, the evaluation of publication bias was not performed.
Five studies were conducted to evaluate the safety and adverse drug reactions, such as nausea, vomiting, dizziness, fatigue, and insomnia occurred during treatment. There were 45 adverse reactions in the treatment group and 20 adverse reactions in the control group. The heterogeneity test showed the statistical significance (p = 0.80, I2 = 0), so we used the fixed effect model. The results of meta-analysis showed that there was no statistical differences between the groups (OR = 0.88, 95% CI: 0.65 to 1.20; p = 0.43; shown in Figure 10). Therefore, the experimental group did not increase the incidence of adverse reactions.
According to the further evaluation, the quality of evidence and the GRADE evidence profile was formed (in Table 2).
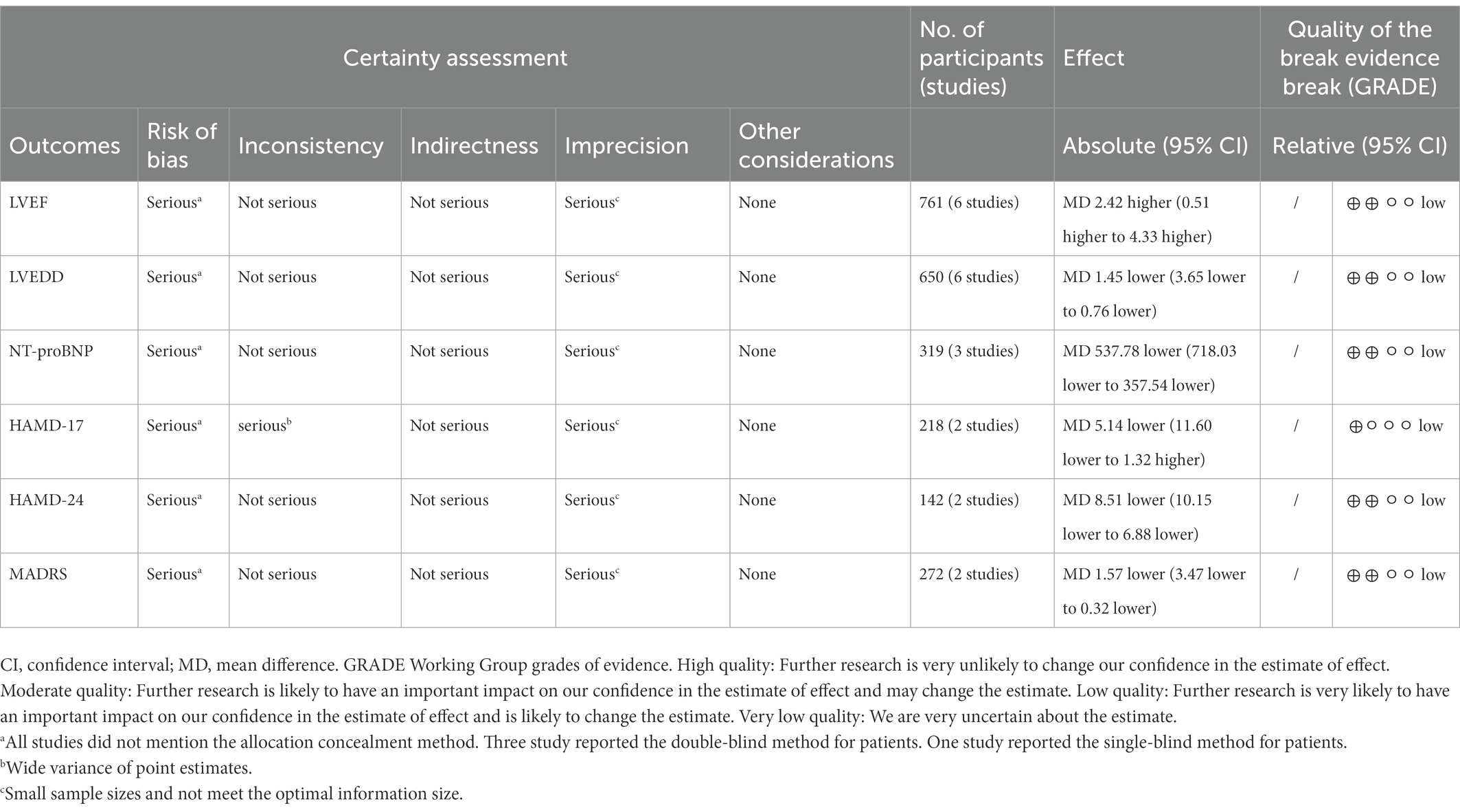
Table 2. The GRADE evidence profile for citalopram in the treatment of chronic heart failure combined with depression.
In this study, we included a total of eight randomized controlled trials of the citalopram for elderly chronic HF combined with depression in a meta-analysis, involving 1,141 patients. This study preliminarily indicated that the citalopram would show a benefit in LVEF (MD: 2.42, 95% CI: 0.51 to 4.33, p = 0.01) and NT-proBNP (MD: −537.78, 95% CI: −718.03 to −357.54, p < 0.0001) associated with people of elderly chronic HF combined with depression. However, there was no positive effect on improving LVEDD (MD: −1.45, 95% CI: −3.65 to 0.76, p = 0.20). It was found that the citalopram could improve the depression instruments HAMD-24 (MD: −8.51, 95% CI: −10.15 to −6.88; p < 0.0001) in patients with elderly chronic HF and depression, while did not exhibit a statistically significant improvement in HAMD-17 (MD: −5.14, 95% CI: −11.60 to 1.32; p = 0.12) and MARDS (MD: −1.57, 95% CI: −3.47 to 0.32; p = 0.10).
The heterogeneity of HAMD-24 and MARDS was small (I2 = 0%), which was no significant correlation with drugs or oral methods. The heterogeneity of the HAMD-17 was large (I2 = 95%). Unfortunately, the cause of heterogeneity had not been found. Moreover, the association needs to be included more studies to explore. The study of GDS score was significantly lower in moderate–severe depression patients of the citalopram treatment group than in that of control group after treatment (25). The results of the meta-analysis proved that the citalopram treatment for depressed patients with chronic HF had a benefit in LVEF, NT-proBNP, and HAMD-24, while data indicated there was no good effect on LVEDD, HAMD-17 and MADRS.
In addition, in terms of safety evaluation, four studies reported that patients had no adverse reactions during the medication. Seven studies reported that patients experienced nausea, vomiting, dizziness, fatigue, and insomnia during medication, which may be related to the patients’ physical condition or underlying disease. However, the difference between the two groups was not statistically significant. Therefore, it was shown that the citalopram had a better safety profile in the treatment of CHF combined with depression.
The primary outcomes of the meta-analysis were changed in cardiac function and whether depression improved. As we know, LVEF, LVEDD, and NT-proBNP have proven to be important indicators for assessing cardiac function. Due to the different criteria for evaluating depression in the included articles, including HAMD-17, HAMD-24, MARDS, and GDS, the improvement of depression was analyzed separately. However, this adversely affected the analysis of the reliability of the results through Meta-analysis. Future studies of more uniform depression criteria will provide the potential for analysis of these outcome indicators. Citalopram has the effects of inhibiting platelet function, promoting endothelial stability and anti-inflammation (29, 30). It can improve cardiac function by relieving depression in patients with HF. This beneficial effect is a reduction in myocardial oxygen consumption (31), resulting in a significant improvement in LVEF and a significant reduction in NT-proBNP levels.
This study provides preliminary evidence that the citalopram can alleviate depression and improve cardiac function in patients with HF. In the included studies, the patients’ depression may be relieved through standardized medical treatment of HF. As a result of taking antidepressants at the same time, the patient’s depression status has been improved to a greater extent. Reduction of depression, improved mood and quality of life, promote the recovery of cardiac function. The relationship between chronic HF and depression is mutual.
The common pathophysiological mechanism is related to the following: endothelial function (32, 33); inflammation, including interleukin (IL)-6, C-reactive protein (CRP) and tumor necrosis factor alpha (34–36). Unfortunately, a number of articles included in this study about the inflammatory factor test were not sufficient for a meta-analysis. So, the study did not provide relevant data to observe the changes in inflammatory factors.
At present, some strategies may be beneficial for depressed patients with chronic HF, such as exercise programs, cognitive behavioral therapy and antidepressant medication (37). Exercise therapy significantly improves the symptoms of depression in patients with chronic HF, and improves both mental and physical health (38). Meanwhile, the cognitive behavioral therapy (39) has been shown to improve mental health outcomes in patients with HF. Due to the intersection of cardiac and psychological symptoms, it is not clear whether antidepressants can improve cardiac function. There are no clear findings on the choice of medication for patients with depression in HF. Currently, the citalopram is safe (30, 39) for treating patients in HF with depression, and no obvious adverse reactions have been found, which is consistent with our meta-analysis.
However, the inclusion of two studies (26, 27) showed that the citalopram did not have more effective over placebo in the treatment of depression. This inconsistency with the results of the meta-analysis may be related to several reasons. Firstly, populations domestically and internationally may be closely related to the results of the experiment, which had differences in drug sensitivity and tolerance. Secondly, the level of depression in the patient may be influenced by other underlying factors during treatment. For example, interpersonal communication, exercise, etc. To reduce the impact of potential factors on the results, we will try to explore the daily routine of patients of different races or ethnicities enrolled in future studies.
We have only studied the efficacy of the citalopram in the treatment of depression in the elderly with chronic HF, and will expand the scope to study young people in the future. In the past, we paid more attention to cardiac physiology and often ignored social and psychological factors (40, 41).
The relationship between the cardiac function and psychology studied vigorously. Regarding the improvement of depression in patients with HF by the citalopram, we can focus on the physical and chemical indicators of the brain in the future to obtain the meaningful answers from them. During the research process, we found that nursing staff (42) played an important role in alleviating patients’ depression. The goal in the future is not only to rely on drug treatment, but also to alleviate the suffering of patients from multifaceted interventions.
However, this study has some limitations. Firstly, none of the included trials explained the method of allocation concealment, and most of them were published in Chinese, which adversely affected the reliability of the results. Secondly, fewer indicators were included in the English articles and we tried to contact the authors by email, but unfortunately without success. Thirdly, the chemical structure of the citalopram differs in the included studies, and this would have a biased effect on the reliability of the results.
According to this study, the citalopram treatment for depressed patients with HF have a benefit in LVEF and NT-proBNP, improve HAMD-24 and GDS, while data needed to verify the relative benefits of LVEDD, HAMD-17, and MADRS. More large-scale, multicenter, long-term, randomized, and double-blind clinical trials are needed to demonstrate this conclusion in the future.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
KC and JZ directed and supervised the study. LY conceived this study, analyzed the data and drafted the manuscript. YA, YX, and AG extracted the data. LY and QX rechecked the data. BW and HL provided valuable suggestions for article. All authors contributed to the article and approved the submitted version.
This study was supported by the CACMS Innovation Fund (Grant No. CI2021A00915) and National Natural Science Foundation of China (Grant No. 81573817).
The authors thank Xiyuan Hospital, China Academy of Chinese Medical Sciences, for their support of this work and the reviewers for allowing us to make improvements to the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1107672/full#supplementary-material
1. Vaccarino, V, Kasl, SV, Abramson, J, and Krumholz, HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. (2001) 38:199–205. doi: 10.1016/S0735-1097(01)01334-1
2. Easton, K, Coventry, P, Lovell, K, Carter, LA, and Deaton, C. Prevalence and measurement of anxiety in samples of patients with heart failure: meta-analysis. J Cardiovasc Nurs. (2016) 31:367–79. doi: 10.1097/JCN.0000000000000265
3. Angermann, CE, and Ertl, G. Depression, anxiety, and cognitive impairment: comorbid mental health disorders in heart failure. Curr Heart Fail Rep. (2018) 15:398–410. doi: 10.1007/s11897-018-0414-8
4. Westlake, C, Dracup, K, Fonarow, G, and Hamilton, M. Depression in patients with heart failure. J Card Fail. (2005) 11:30–5. doi: 10.1016/j.cardfail.2004.03.007
5. Mensah, GA, and Brown, DW. An overview of cardiovascular disease burden in the United States. Health Aff. (2007) 26:38–48. doi: 10.1377/hlthaff.26.1.38
6. Lichtman, JH, Froelicher, ES, Blumenthal, JA, Carney, RM, Doering, LV, Frasure-Smith, N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. (2014) 129:1350–69. doi: 10.1161/CIR.0000000000000019
7. Rutledge, T, Reis, VA, Linke, SE, Greenberg, BH, and Mills, PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. (2006) 48:1527–37. doi: 10.1016/j.jacc.2006.06.055
8. Kessler, RC, Berglund, P, Demler, O, Jin, R, Koretz, D, Merikangas, KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. (2003) 289:3095–105. doi: 10.1001/jama.289.23.3095
9. Jiang, W, Alexander, J, Christopher, E, Kuchibhatla, M, Gaulden, LH, Cuffe, MS, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. (2001) 161:1849–56. doi: 10.1001/archinte.161.15.1849
10. Ponikowski, P, Voors, AA, Anker, SD, Bueno, H, Cleland, JG, Coats, AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the heart failure association (HFA) of the ESC. Eur J Heart Fail. (2016) 18:891–975. doi: 10.1002/ejhf.592
11. Yancy, CW, Jessup, M, Bozkurt, B, Butler, J, Casey, DE Jr, Drazner, MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. (2013) 62:e147–239. doi: 10.1016/j.jacc.2013.05.019
12. Ponikowski, P, Voors, AA, Anker, SD, Bueno, H, Cleland, JGF, Coats, AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. (2016) 37:2129–200. doi: 10.1093/eurheartj/ehw128
13. Owens, MJ, Knight, DL, and Nemeroff, CB. Second-generation SSRIs: human monoamine transporter binding profile of escitalopram and R-fluoxetine. Biol Psychiatry. (2001) 50:345–50. doi: 10.1016/s0006-3223(01)01145-3
14. Sanchez, C, Bergqvist, PB, Brennum, LT, Gupta, S, Hogg, S, Larsen, A, et al. Escitalopram, the S-(+)-enantiomer of citalopram, is a selective serotonin reuptake inhibitor with potent effects in animal models predictive of antidepressant and anxiolytic activities. Psychopharmacology. (2003) 167:353–62. doi: 10.1007/s00213-002-1364-z
15. Cipriani, A, Furukawa, TA, Salanti, G, Geddes, JR, Higgins, JPT, Churchill, R, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. (2009) 373:746–58. doi: 10.1016/S0140-6736(09)60046-5
16. Castro, VM, Clements, CC, Murphy, SN, Gainer, VS, Fava, M, Weilburg, JB, et al. QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ. (2013) 346:f288. doi: 10.1136/bmj.f288
17. Beach, SR, Kostis, WJ, Celano, CM, Januzzi, JL, Ruskin, JN, Noseworthy, PA, et al. Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. J Clin Psychiatry. (2014) 75:e441–9. doi: 10.4088/JCP.13r08672
18. Hedrick, R, Korouri, S, Tadros, E, Darwish, T, Cortez, V, Triay, D, et al. The impact of antidepressants on depressive symptom severity, quality of life, morbidity, and mortality in heart failure: a systematic review. Drugs Context. (2020) 9:2020-5-4. doi: 10.7573/dic.2020-5-4
19. Moher, DLA, Tetzlaff, J, and Altman, DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 31:367–79, W64. doi: 10.1097/JCN.0000000000000265
20. Tsutsui, H, Ide, T, Ito, H, Kihara, Y, Kinugawa, K, Kinugawa, S, et al. JCS/JHFS 2021 guideline focused update on diagnosis and treatment of acute and chronic heart failure. J Card Fail. (2021) 27:1404–44. doi: 10.1016/j.cardfail.2021.04.023
21. Kuang, JJ, Wen, Q, and Chen, CL. Efficacy and safety of escitalopram combined with carvedilol in the treatment of chronic heart failure with depression in elderly patients. J. China Prescription Drug. (2020) 18:68–9. doi: 10.3969/j.issn.1671-945X.2020.01.036
22. Jia, L, Xu, L, and Yang, R. Randomized controlled study on short-term efficacy and safety of Escitalopram in treating senile chronic heart failure complicating major depression. China Pharm. (2012) 21:23–5. doi: 10.3969/j.issn.1006-4931.2012.06.012
23. Jia, L, Meng, HQ, Xu, ZL, and Li, QY. Influences of escitalopram on cognitive function and cardiac function in elderly patients with chronic heart failure complicated with depression disorder. Chongqing Yixue. (2017) 46:2652–4. +2658. doi: 10.3969/j.issn.1671-8348.2017.19.018
24. Ding, P, Zhang, HL, Xie, F, and Wang, XH. Effect of citalopram on short-term and long-term prognosis of chronic heart failure patients with depression. J. Int. Psychiatry. (2017) 44:493–5+515. doi: 10.13479/j.cnki.jip.2017.03.034
25. Wang, T, Li, Y, and Wang, J. Clinical effect of citalopram in elderly chronic heart failure patients with depression. Chin. J. Geriatr. (2021) 23:172–5. doi: 10.3969/j.issn.1009-0126.2021.02.016
26. Fraguas, R, da Silva Telles, RM, Alves, TC, Andrei, AM, Rays, J, Iosifescu, DV, et al. A double-blind, placebo-controlled treatment trial of citalopram for major depressive disorder in older patients with heart failure: the relevance of the placebo effect and psychological symptoms. Contemp Clin Trials. (2009) 30:205–11. doi: 10.1016/j.cct.2009.01.007
27. Angermann, CE, Gelbrich, G, Stork, S, Gunold, H, Edelmann, F, Wachter, R, et al. Effect of Escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. (2016) 315:2683–93. doi: 10.1001/jama.2016.7635
28. Cao, XC, Liu, X, Xu, XJ, Huang, GR, and Duan, MQ. Efficacy and safety of escitalopram on heart failure with preserved ejection fraction and depression in elderly patients. Chin. J. Geriatr. (2020) 39:1406–10. doi: 10.3760/cma.j.issn.0254-9026.2020.12.009
29. Serebruany, VL, Glassman, AH, Malinin, AI, Nemeroff, CB, Musselman, DL, van Zyl, LT, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the sertraline AntiDepressant heart attack randomized trial (SADHART) platelet substudy. Circulation. (2003) 108:939–44. doi: 10.1161/01.CIR.0000085163.21752.0A
30. Wozniak, G, Toska, A, Saridi, M, and Mouzas, O. Serotonin reuptake inhibitor antidepressants (SSRIs) against atherosclerosis. Med Sci Monit. (2011) 17:RA205–14. doi: 10.12659/msm.881924
31. Ma, JJ, Lu, LL, Zheng, YX, Liu, J, and Hu, J. Efficacy of citalopram in the treatment of chronic heart failure combined with depression. Chin J Integr Med on Cardio-/Cerebrovascular Disease. (2012) 10:1159–1160. doi: 10.3969/j.issn.1672-1349.2012.10.004
32. Fischer, D, Rossa, S, Landmesser, U, Spiekermann, S, Engberding, N, Hornig, B, et al. Endothelial dysfunction in patients with chronic heart failure is independently associated with increased incidence of hospitalization, cardiac transplantation, or death. Eur Heart J. (2005) 26:65–9. doi: 10.1093/eurheartj/ehi001
33. Katz, SD, Hryniewicz, K, Hriljac, I, Balidemaj, K, Dimayuga, C, Hudaihed, A, et al. Vascular endothelial dysfunction and mortality risk in patients with chronic heart failure. Circulation. (2005) 111:310–4. doi: 10.1161/01.CIR.0000153349.77489.CF
34. Kell, R, Haunstetter, A, Dengler, TJ, Zugck, C, Kübler, W, and Haass, M. Do cytokines enable risk stratification to be improved in NYHA functional class III patients? Comparison with other potential predictors of prognosis. Eur Heart J. (2002) 23:70–8. doi: 10.1053/euhj.2001.2780
35. Howren, MB, Lamkin, DM, and Suls, J. Associations of depression with C-reactive protein, IL-1, and IL-6:a meta-analysis. Psychosom Med. (2009) 71:171–86. doi: 10.1097/PSY.0b013e3181907c1b
36. Irwin, M. Psychoneuroimmunology of depression: clinical implications. Brain Behav Immun. (2002) 16:1–16. doi: 10.1006/brbi.2001.0654
37. Tully, PJ, Selkow, T, Bengel, J, and Rafanelli, C. A dynamic view of comorbid depression and generalized anxiety disorder symptom change in chronic heart failure: the discrete effects of cognitive behavioral therapy, exercise, and psychotropic medication. Disabil Rehabil. (2015) 37:585–92. doi: 10.3109/09638288.2014.935493
38. Tu, RH, Zeng, ZY, Zhong, GQ, Wu, WF, Lu, YJ, Bo, ZD, et al. Effects of exercise training on depression in patients with heart failure: a systematic review and meta-analysis of randomized controlled trials. Eur J Heart Fail. (2014) 16:749–57. doi: 10.1002/ejhf.101
39. Aloisi, G, Zucchelli, A, Aloisi, B, Romanelli, G, and Marengoni, A. Depression and heart failure: an intricate relationship. Monaldi Arch Chest Dis. (2019) 89:89. doi: 10.4081/monaldi.2019.1029
40. Rozanski, A, Blumenthal, JA, and Kaplan, J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. (1999) 99:2192–217. doi: 10.1161/01.cir.99.16.2192
41. Ziegelstein, RC. Depression in patients recovering from a myocardial infarction. JAMA. (2001) 286:1621–7. doi: 10.1001/jama.286.13.1621
Keywords: citalopram, elderly chronic heart failure, depression, systematic review, meta-analysis
Citation: Yan L, Ai Y, Xing Y, Wang B, Gao A, Xu Q, Li H, Chen K and Zhang J (2023) Citalopram in the treatment of elderly chronic heart failure combined with depression: A systematic review and meta-analysis. Front. Cardiovasc. Med. 10:1107672. doi: 10.3389/fcvm.2023.1107672
Received: 25 November 2022; Accepted: 12 January 2023;
Published: 01 February 2023.
Edited by:
Clement Delmas, Rangueil University Hospital, FranceReviewed by:
Federica Moscucci, Sapienza University of Rome, ItalyCopyright © 2023 Yan, Ai, Xing, Wang, Gao, Xu, Li, Chen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingchun Zhang, ✉ emhhbmdqaW5nY2h1bjI3NkAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.