
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 10 March 2023
Sec. Cardiovascular Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fcvm.2023.1081162
This article is part of the Research Topic Case Reports in Heart Surgery: 2022 View all 21 articles
 Ahmed Ouda1,†
Ahmed Ouda1,† Anna Maria Schürner2,†
Anna Maria Schürner2,† Martin Oliver Schmiady1
Martin Oliver Schmiady1 Gerrolt Nico Jukema3
Gerrolt Nico Jukema3 Paul Robert Vogt1
Paul Robert Vogt1 Thierry Carrel1*
Thierry Carrel1*
We report an unusual case of multiple penetrating cerebral, cardiac and abdominal injuries following a suicidal attempt using a nail gun. Successful treatment required several emergency procedures and resulted from a wise interdisciplinary management and timing of surgery.
A 59-year-old male was admitted to the emergency department following a suicidal attempt using an automatic nail gun less than 1 h before. He presented with a Glasgow scale of 15 and was in a hemodynamically stable condition. Inspection revealed multiple nails penetrating the head, the neck, the thorax and the left upper abdomen (Figure 1). Total body computer tomography was performed (Figure 2) and demonstrated eighteen 7.5 cm long nails: two nails penetrated the skull, one from left paramedian and the other from right parietal causing a small subarachnoid and a thin subdural hematoma with a small amount of blood in both ventricles. One nail penetrated the neck at the level of the 7Th cervical vertebra with the tip close to the left subclavian artery. Ten nails penetrated the left chest with the tips both in the right and left ventricle, some of them were shot through the interventricular septum. As expected, pericardial effusion was noticed but without signs of tamponade. Two nails penetrated the left chest: one superficially into the pectoralis muscle and the other one into the lingula lobe of the left lung. Finally, three nails entered the upper abdomen and perforated the stomach with a small amount of sub-diaphragmatic air. The patient was discussed at an interdisciplinary meeting including all concerned medical specialists to decide on the optimal sequence of surgical explorations.
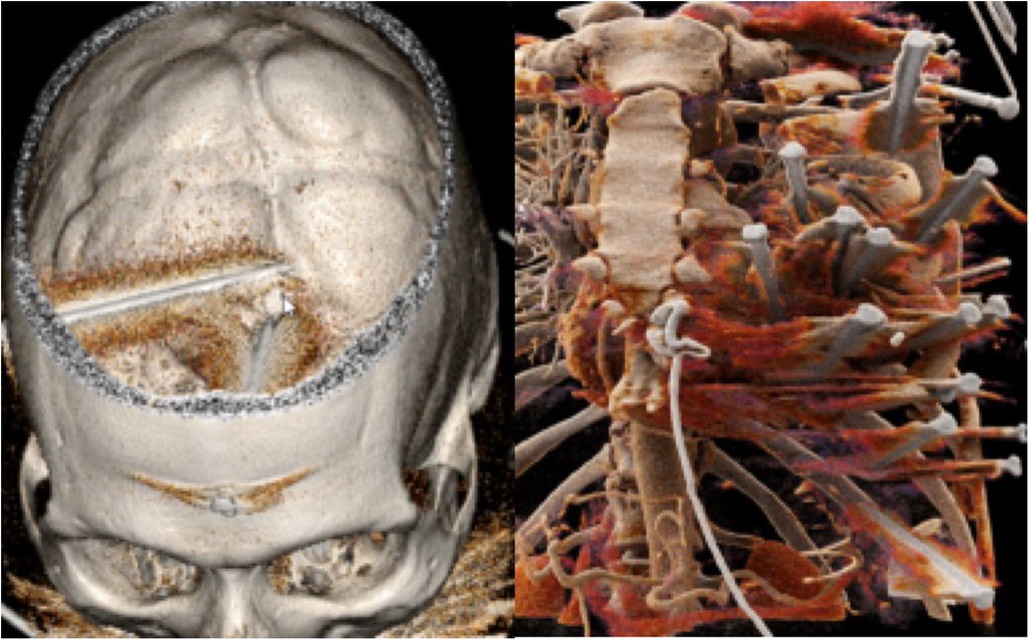
Figure 2. 3d reconstruction of the CT-scan showing nails in the head (left) and those penetrating into the heart, the left lung and the stomach (right).
The main concerns were the following:
• occurrence of cerebral bleeding following removal of the intracranial nails,
• pericardial tamponade if removal of the intracardiac nails would be delayed,
• need for full heparinization with the potential of delayed cerebral bleeding in case extracorporeal circulation would be required to allow safe cardiac repair.
Finally, decision was taken to remove the nails from the skull first and to proceed thereafter with chest and especially cardiac exploration since the patient was in a hemodynamic stable condition. The procedure was performed in a multipurpose trauma operating room, in which immediate cardiac exploration would have been possible.
Following removal of the nails from the head, decision was made to observe the situation for a short interval. Cerebral CT-scan was repeated and showed a slight increase of the hematoma in the left frontal and right temporal regions (Figure 3). Since echocardiography did not show any increase of pericardial effusion, the patient was transferred to the intensive care unit and reassessed 2 and 4 h later. There, during careful removal of the clothes that had been transfixed by the nails, the patient's condition suddenly deteriorated very rapidly and echocardiography showed pericardial tamponade. Because of circulatory collapse, mechanical resuscitation would have been necessary but chest compression was not possible because of the nails still in situ. For this reason, emergency left thoracotomy was performed on the intensive care unit but adequate manual cardiac massage was not possible with the nails still in situ.
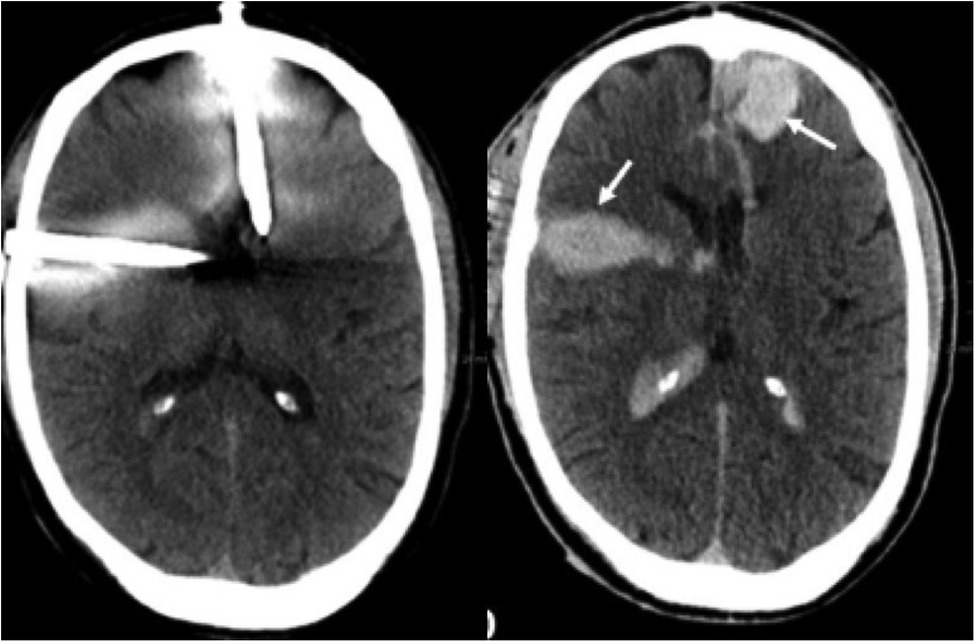
Figure 3. Cranial CT-scan before removal of the nails from the skull (left) with discrete bleeding and after removal with a progressive hematoma (arrow) (right).
Opening the pericardium allowed immediate decompression of the tamponade. Following removal of the nails, quick inspection revealed seven myocardial lesions, some of them very close to the left anterior descending branch. Median sternotomy to improve exposure and allow better access to all injuries was performed: during that time, control of the most important myocardial injuries was performed with fingers and swabs. The lesions of the ventricular wall were closed using 2.0 polypropylene, while a diffuse epicardial venous bleeding was covered with a xeno-pericardial patch under which bio-glue (CryoLife Inc. GA, USA) was injected (Figure 4). Despite sufficient hemostasis within the chest, the patient remained unstable. Median laparotomy was performed to exclude intra-abdominal bleeding; this allowed removal of the last two nails that had perforated the stomach. These injuries were sutured with 4.0 Polydiaxone. The patient received 6 units of red blood cells.
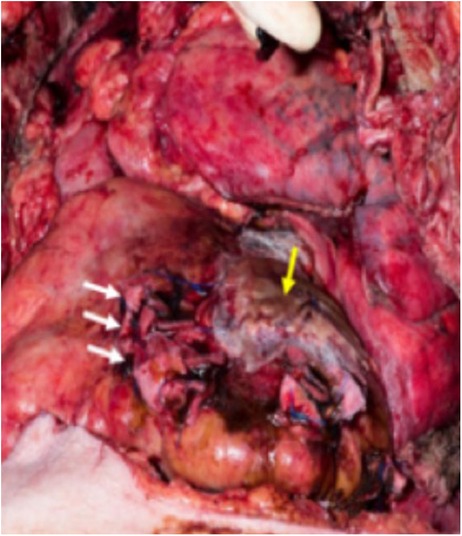
Figure 4. Intraoperative picture during repair of the right ventricular lesions (white arrows) and pericardial patch covering the left ventricular lesion (yellow arrow).
Because of the contaminated operative field and semi-sterile operative conditions, the sternotomy wound was covered with a vacuum-dressing and delayed chest closure was performed five days later. Antibiotic regime consisted in cephalosporine until the chest was closed and vancocin for 48 h. The patient required prolonged ventilation and tracheotomy for weaning from ventilator. He was discharged on postoperative day 28, with full recovered motoric and cognitive functions.
The pre-discharge echocardiography showed normal biventricular function without valvular lesion or intracardiac shunts. Cardiac CT-scan showed patent coronary arteries (Figure 5).
Combined penetrating cerebral and cardiac injuries constitute a particular challenge for decision-making regarding the optimal sequence of surgical explorations (1, 2). Especially patients who may need cardiopulmonary bypass and full heparinization have to be considered very carefully in presence of concomitant cerebral and/or abdominal injuries. In case of polytrauma and unstable hemodynamics, the lesion with the highest blood loss has to be treated first. Whenever possible, repair of cardiac injuries should be attempted without cardiopulmonary bypass to avoid full heparinization in a situation with multiple injuries. Adenosine administration to decrease pulse rate and blood pressure may be helpful (3). When this is not possible, heparinization should be quickly reversed by protamine in a 1 : 1 dosage to minimize the bleeding risk. Since simple algorithms for such situations are not available, multi-disciplinary evaluation of each individual case is of utmost importance to balance advantages and disadvantages of the different operative sequences.
In this case, the decision to proceed with cerebral extraction of the nails first and delay explorative thoracotomy was suboptimal since it led to an emergency situation on the intensive care unit and cardiac massage was not possible until the nails were removed. Nevertheless, the situation could be controlled and the final control of all cardiac injuries was realized through sternotomy.
In addition, postponing the removal of the intra-cranial nails would probably have avoided the progression of cerebral bleeding. Extraction could have been performed after optimization of the coagulation.
The choice of the optimal access to the heart was also an important aspect in this patient. Although median sternotomy is usually suitable for a single penetrating injury, it was thought inappropriate in this case because the nails in situ would have made spreading of the sternum impossible before removal of the nails.
Fortunately, the nails could be removed and the myocardial lesions successfully treated without the need for extracorporeal circulation. If this would not have been possible either ECMO or CPB with coated tubes would have been attractive options to avoid full heparinization. Despite all challenges encountered, this case ended successfully without wound infection despite the hardly sterile operative conditions and the patient could be discharge at home with a psychiatric supervision.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Informed consent could not be obtained before treatment because of the emergency condition but the patient signed the institutional consent for anonymous use of patient’s data for scientific purposes. Since the patient was further treated in a psychiatric institution, we received the permission of the brother (document signed by U.F.), as his legal representative, to re-use the full material in an anonymized form, including: clinical details of the hospital chart, pre-, intra- and post-operative pictures, and intraoperative video. As soon as the patient recovered, he was informed by the brother and gave his approval too (document signed by F. F.). Written informed consent was obtained from the patient and from his relatives for the publication of this case report.
AO, MOS, TC contributed to conception and design of the study. AO, AMS, GJ organized the database. AO and AMS wrote the first draft of the manuscript. TC and PRV wrote sections of the manuscript and made substantial contributions to the final version of the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ye CN, Lin MC, Huang CL. Double penetration wound: a nail gun injury involving the head and the heart. Radiol Case Rep. (2020) 15:334–8. doi: 10.1016/j.radcr.2019.11.021
2. Fang X, Yu C, He F. The self-inflicted multiple organs injury with nail gun. Heart Surg Forum. (2021) 24:E1049–51. doi: 10.1532/hsf.4201
Keywords: penetrating cardiac trauma, head injury, cerebral bleeding, anticoagulation, surgical treatment
Citation: Ouda A, Schürner AM, Schmiady MO, Jukema GN, Vogt PR and Carrel T (2023) Case report: Eighteen nails gun shots in the head, thorax and abdomen but still conscious at admission: A challenging patient for the cardiac surgeon!. Front. Cardiovasc. Med. 10:1081162. doi: 10.3389/fcvm.2023.1081162
Received: 26 October 2022; Accepted: 20 February 2023;
Published: 10 March 2023.
Edited by:
Salah D. Qanadli, Université de Lausanne, SwitzerlandReviewed by:
Sandeep Sainathan, University of Miami Health System, United States© 2023 Ouda, Schürner, Schmiady, Jukema, Vogt and Carrel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thierry Carrel dGhpZXJyeS5jYXJyZWxAZ21haWwuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Heart Surgery, a section of the journal Frontiers in Cardiovascular Medicine
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.