- Cardiovascular Center, CARIM School for Cardiovascular Disease, University Hospital Maastricht, University of Maastricht, Maastricht, Netherlands
Treatment of aortic arch aneurysms and dissections require highly complex surgical procedures with devastating complications and mortality rates. Currently, repair of the complete arch until the proximal descending thoracic aorta consists of a two-stage procedure, called elephant trunk (ET) technique, or a single stage a single-stage technique referred to as frozen elephant trunk (FET). There is conflicting evidence about the perioperative results of ET in comparison with FET. We carried out a meta-analysis to investigate possible differences in perioperative and early (up to 30 days) outcomes of ET vs. FET, particularly for mortality, spinal cord injury (SCI), stroke, and renal failure. We also performed a meta-regression to explore the effects of age and sex as possible cofactors. Twenty-one studies containing data from interventions conducted between 1997 and 2019 and published between 2008 and 2021 with 3153 patients (68.5% male) were included. ET was applied to 1,693 patients (53.7%) and FET to 1460 (46.3%). Overall mortality after ET was 250/1693 (14.8%) and after FET 116/1460 (7.9%). Relative risk (RR) and 95% confidence interval (CI) were 1.37 [1.04 to 1.81], p = 0.027. There was no significant effect of age and sex. SCI occurrence after the second stage of ET was 45/1693 (2.7%) and after FET 70/1,460 patients (4.8%) RR 0.53 [0.35 to 0.81], p = 0.004. Age and sex were not associated with the risk of SCI. No significant differences were observed between ET and FET in the incidence of stroke and renal failure. Our results indicate that ET is associated with higher early mortality but lower incidence of SCI compared to FET. When studies published in the last 5 years were analyzed, no significant differences in mortality or SCI were found between ET and FET. This difference is attributed to a decrease in mortality after ET, as the mortality after FET did not change significantly over time.
Introduction
The incidence of aortic aneurysms and dissections is on the rise during the last two decades and can affect between 2 and 6 out of 100,000 people every year (1–4).
Aortic arch dissections arise from intimal tears within an aneurysm and are highly deadly with a mortality rate reaching up to 80% if there is a rupture. The risk of dying is around 21% for patients who reach the hospital alive (5, 6).
With increasing incidence and high mortality, there is a need for better management and treatment of both aortic aneurysms and dissections.
Aneurysms are permanent dilatations of the aorta with at least 50% increase of the expected normal diameter of the aorta. Dissections are highly fatal conditions in which disruptions (tears) of the aortic intimal layer cause rushing of blood within the vessel wall, forcing the layers to dissect (7). Aneurysms can occur without dissections and vice versa (7, 8). Current guidelines indicate that “total aortic arch replacement with or without an elephant trunk extension is indicated when a tear within the arch extends into the proximal descending aorta or extends throughout the arch on the greater curve’s aspect, i.e., involves separation or disruption of the Ostia of the brachiocephalic vessels, precluding the ability to reconstruct a neomedia effectively” (9).
Treatment of both dissections and aneurysms in the aortic arch can be done with a two-stage surgical technique called “elephant trunk” (ET) (10). The first stage of ET involves a sternotomy and a reconstruction of the ascending aorta and the aortic arch. At the second stage, a floating extension (elephant trunk) in the descending aorta is used in order to extend the repair toward descending thoracic aorta. An important limitation of this technique is the fact that almost half of the patients that undergo the first step, never arrive at the second step, usually because they die or because they refuse a second operation (11).
The evolution of surgical and endovascular techniques has resulted in the development of a composite prosthesis, known as the “Frozen elephant trunk” (FET) (9, 11). In this technique a stent graft is implanted in the proximal descending thoracic aorta through the aortic arch prosthesis, during the primary procedure (9).
The use of FET instead of the conventional ET is increasing in the last years. However, there is contrasting evidence about which intervention has less complications and whether a real difference exists in their outcomes (12, 13).
Our aim in this meta-analysis was to assess the outcomes of the two techniques for Debakey type I or Stanford type A aortic dissections. We also analyzed separately the data from papers published during the last 5 years (2017–2021) in order to detect possible different outcomes, as newer devices are being developed and techniques evolved (14).
Materials and methods
Search strategy
The literature search was performed in accordance with the principles of the Cochrane Handbook (8) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (15, 16).
An unrestricted literature search was performed in PubMed, Web of Science, Scopus, and the Cochrane library.
The search aimed at finding articles reporting outcomes in patients undergoing aortic arch surgery with ET or FET and contained separate relevant data for each type of intervention.
A systematic search was conducted in PubMed combining MeSH and free terms for the clinical situations, the treatments, and the outcomes. An additional search was conducted in the references of the examined articles.
The search strategy was designed by two authors (AM and JR), and their decisions were approved by a third author (SG). The literature search was performed by one author (AM). The eligibility of the selected articles eligibility and the risk of bias were assessed independently by two independent reviewers (EN, EB). The Risk of Bias in Non-randomized Studies-of Interventions (ROB-INS-I) tool (17) was used by two reviewers (GP and OP) for the assessment of bias of each study. A third reviewer (JGM) resolved any possible differences in the assessment.
The following domains were examined in each study for the risk of bias, according to the Cochrane Handbook: (1) in the confounding; (2) in the participant selection of each study; (3) in the classification of interventions; (4) in cases of deviations from intended interventions; (5) in cases of missing data; (6) in the estimation of outcomes; (7) in the selection of the result to be reported; and (8) overall assessment of bias. The Risk-of-Bias VISualization (robvis) software was used for producing the plot for ROBINS-I (17).
Selection process
The following inclusion criteria were used for the selection of articles: (1) human studies; (2) full research articles containing data on the outcomes of both ET and FET and (3) studies including at least 10 patients.
The exclusion criteria for the article selection were: (1) non-human studies, (2) case reports, (3) previous reviews and/or meta-analyses, (4) editorials, and (5) studies without adequate demographic and/or outcome information on both ET and FET interventions, and (6) studies in languages other than English.
Quality assessment
A rating scale based on the Downs and Black checklist for measuring was used for assessing the quality of included studies (18). The assessment was done using a version with 18 items. The items were ranked with the use of a binary score (0 or 1) except for two items that were rated on a scale from 0 to 2 and from 0 to 5, respectively.
The ratings were collected by two independent researchers (AIM and JLRR). A third reviewer (OP) resolved divergences and quantified the ratings with the use of Cohen’s kappa (19).
Statistical analysis
The R software v. 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) was used for conducting the meta-analysis. The relative risk (RR) was used as index statistics. The results of RR are presented with two decimal points followed by the 95% confidence interval (CI) in brackets in the form: RR (lower CI, upper CI). As heterogeneity among studies was expected, the random effects model was used. The statistical inconsistency Higgin’s I2 test was used for the evaluation of heterogeneity (20). I2 values > 75% were considered to have high heterogeneity and I2 values < 40% were considered to have low heterogeneity. The Egger’s test of the intercept was used for assessing publication bias. A meta-regression analysis was conducted in order to assess the impact of the potential interaction factors, such as age and sex p-values < 0.05 were considered statistically significant.
Endpoints
The primary endpoints of this study were: early mortality, defined as the occurrence of mortality during hospitalization or up to 30 days after the intervention, spinal cord injury/ischemia (SCI) and/or paraplegia and/or quadriplegia, stroke, and renal failure. The possible impact of age and sex on the above-mentioned parameters was also examined.
Results
Search results and characteristics of the studies
The initial search resulted in 695 results from PubMed, 368 from Web of Science, 361 from Scopus, and 8 from the Cochrane library. After the elimination of duplicates and the application of the inclusion and exclusion criteria, 29 articles containing data on ET and FET were found. The full text of these articles was then examined. Fourteen articles did not contain separate data for patients treated with ET and FET and were excluded. An additional search in the references of the selected articles resulted in 6 additional articles that were also included (Figure 1). Overall, twenty-one studies were included in the analysis.
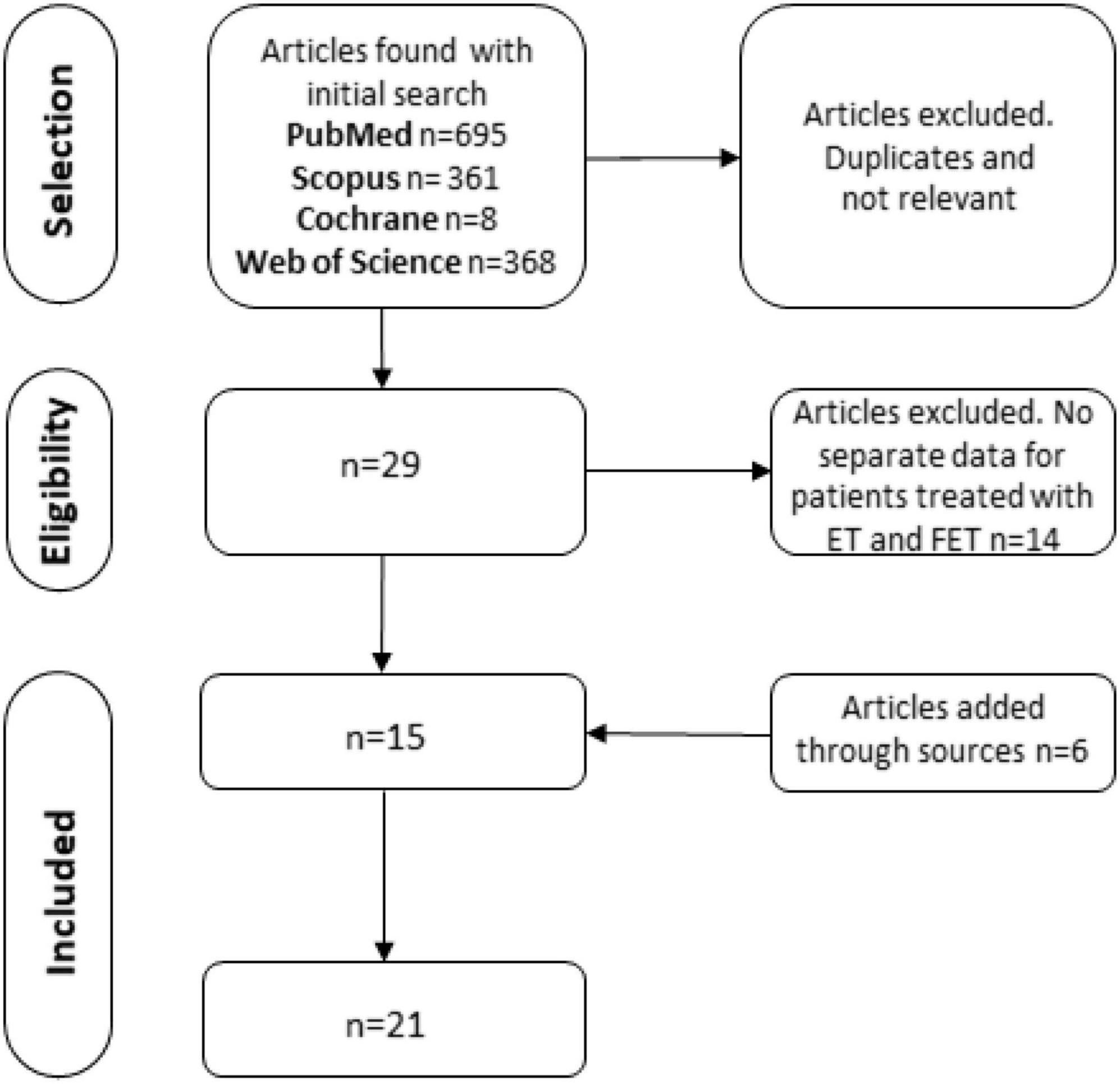
Figure 1. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart of the article selection process. ET, elephant trunk; FET, frozen elephant trunk.
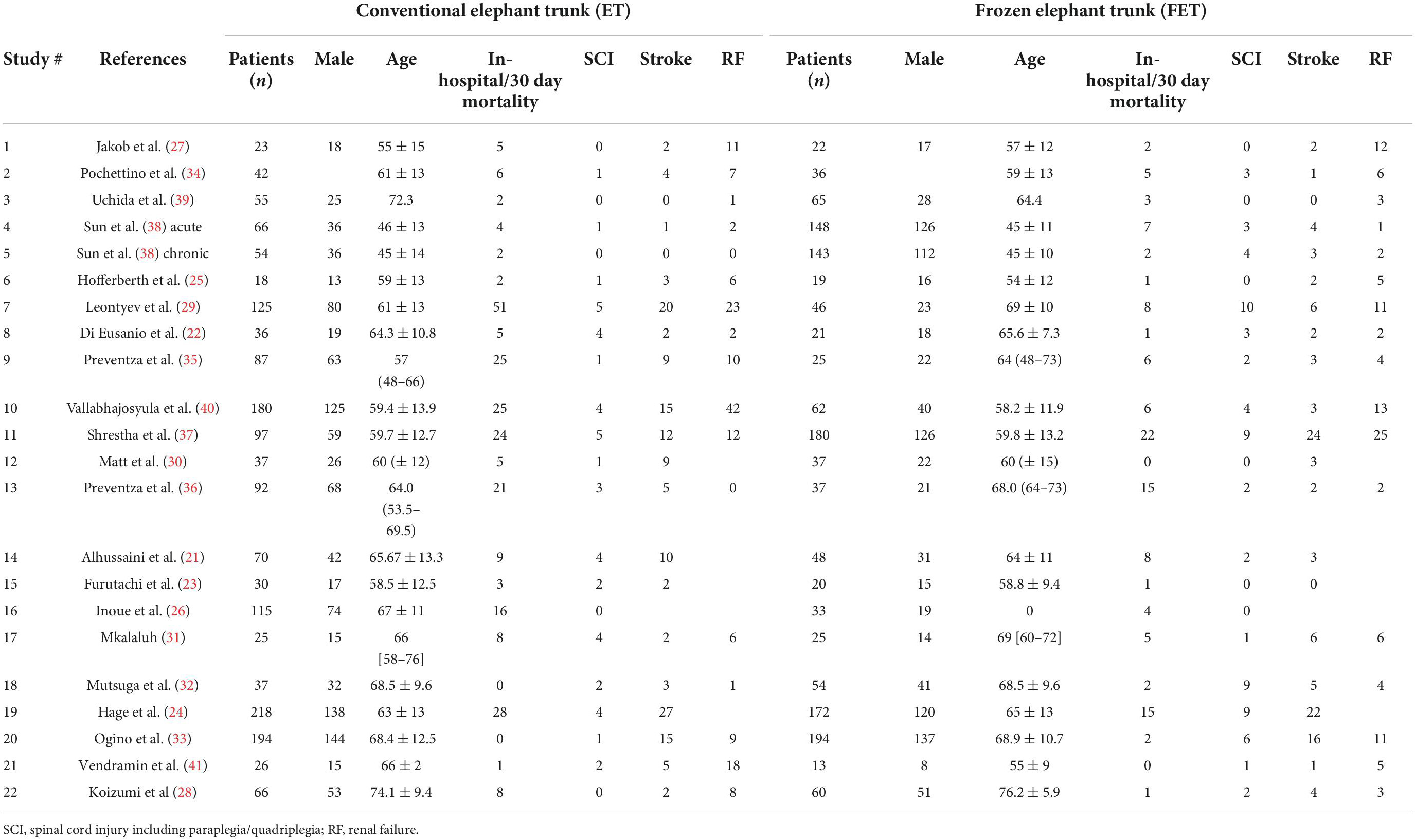
The 21 selected studies (21–41) included a total of 3153 patients. The studies contained data from interventions conducted between 1997 and 2019 and were published between 2008 and 2021. The ET was applied in 1693 patients (53.7%) and FET in 1460 (46.3%). In 17 out of the 18 studies that contained detailed data about sex, 2,105 of 3,075 patients (68.5%) were male. One of the selected studies (38) contained two different cohorts, one with acute and one with chronic dissections. These cohorts were included as separate. One article contained two overlapping cohorts, one cohort with all the patients examined and one with propensity-matched patients (33). Only the matched cohort was included in the statistical evaluation.
The studies that were included in this meta-analysis are shown in Table 1. The patients’ characteristics are shown in Table 2.
Of the 21 selected studies, 10 were published until 2016 and 11 were published in the last 5 years between 2017 and 2021. The studies published until 2016 included data on interventions conducted from 1997 to 2013. The 11 most recent studies published in 2017 and after, included data on more recent interventions ranging until 2021. A total of 1,603 patients, of which 1103 (72.3%) were male were included in these studies. ET was applied in 910 patients (56.8%) and FET in 693 (43.2%).
Quality of the studies
The average quality rating of all the studies was 0.83 ± 0.08. The quality assessment is shown in Supplementary Table 1 in the supplement. The studies were rated with a median rating of 0.83 [IQR 0.78 to 0.89], ranging from 0.67 to 1.00.
Elephant trunk vs. frozen elephant trunk
The RR of ET vs. FET, the I2 values and respective p-values, the Egger’s test results, the funnel plot asymmetry tests p-values, and the p-values of the meta-regression for the effects of age and sex are presented in Table 3. T he results for all the examined papers published between 2008 and 2021 and for those published between 2017 and 2021 are presented in separate lines in the table.
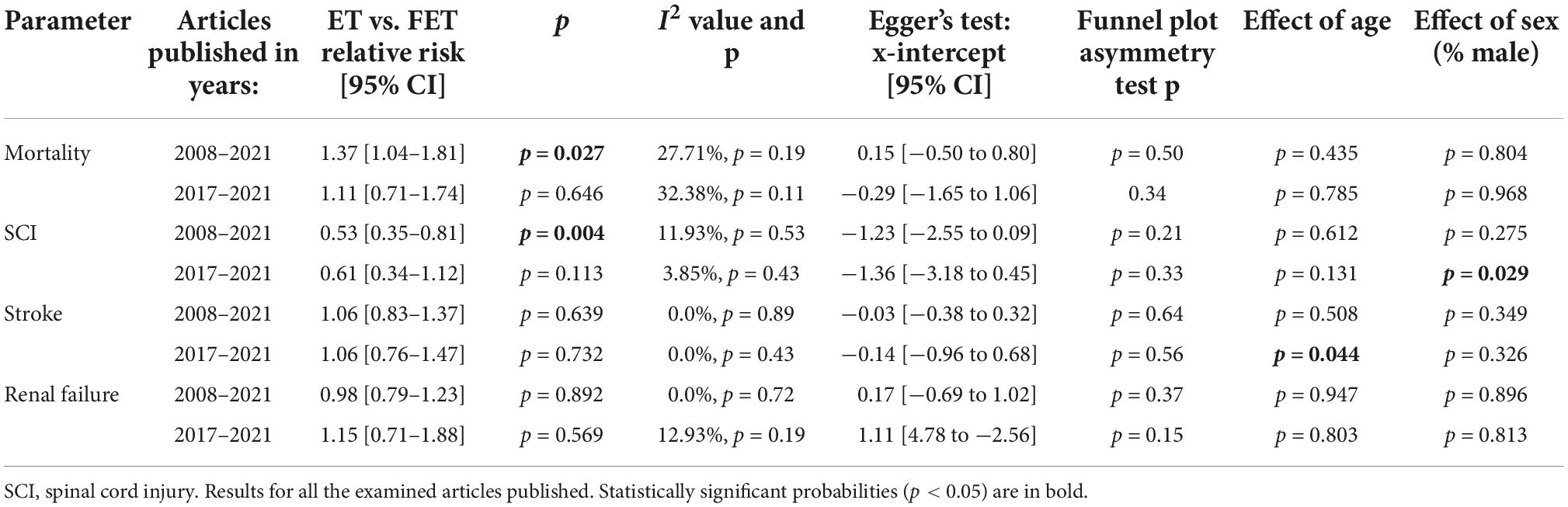
Table 3. Elephant trunk (ET) vs frozen elephant trunk (FET) odds ratios and 95% confidence intervals (CI) and probability (p) of effects of age and sex (% male patients).
The overall mortality after ET was 250 of 1,693 patients (14.8%) and after FET 116 of 1,460 patients (7.9%). The relative risk of mortality after ET vs. after FET was 1.37 [1.04 to 1.81], (p = 0.027, I2 = 27.71%, p-value I2 = 0.19; Egger’s test 0.15 [−0.50 to 0.80], indicating a trend for higher mortality risk with conventional ET (Figure 2, Forest plot). The funnel plot is shown in Figure 3 (asymmetry test: p = 0.50). There was no significant effect of age and sex (percentage of male patients) on mortality according to the meta-regression analysis (Table 3).
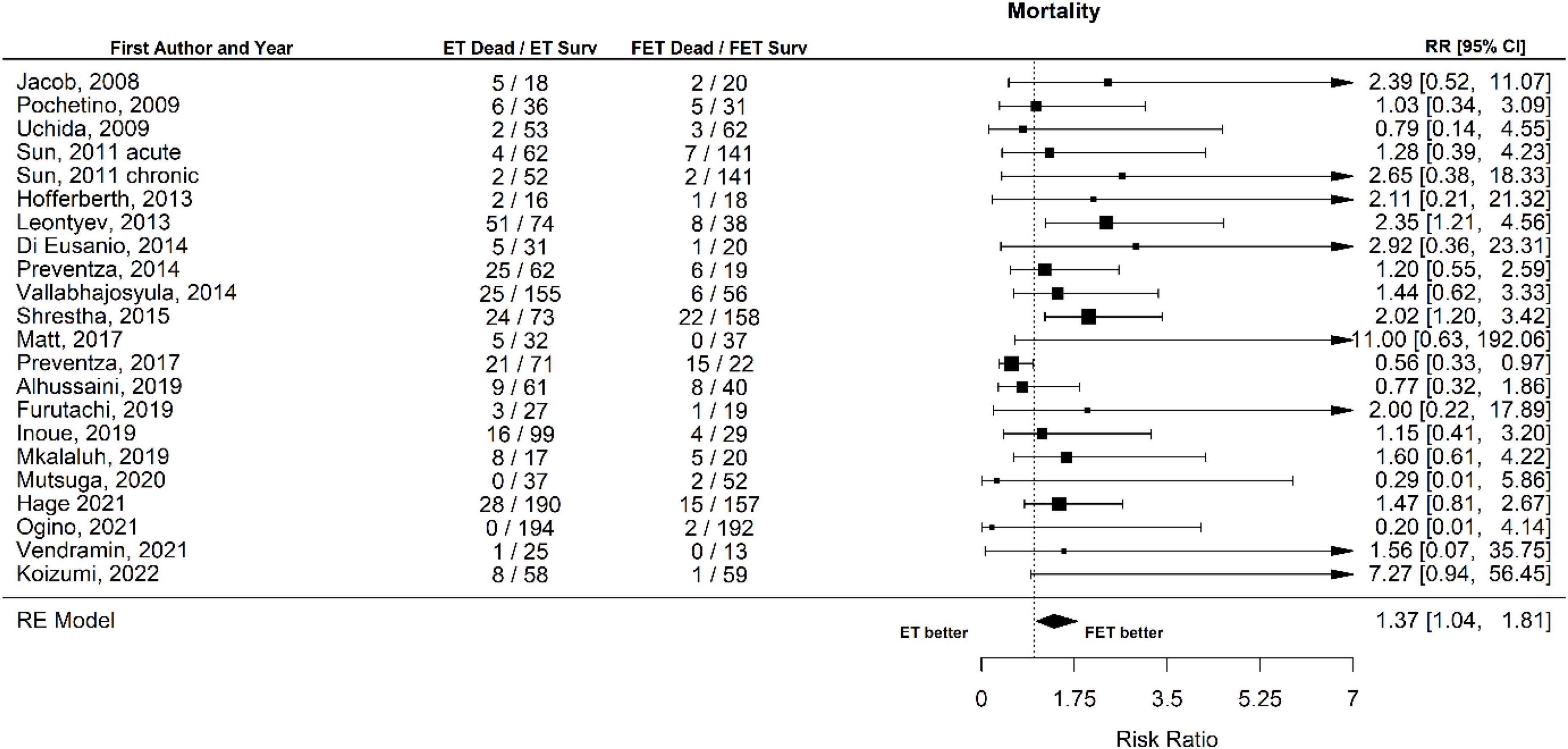
Figure 2. Relative risk of mortality in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Forest plot. ET vs. FET p = 0.027.
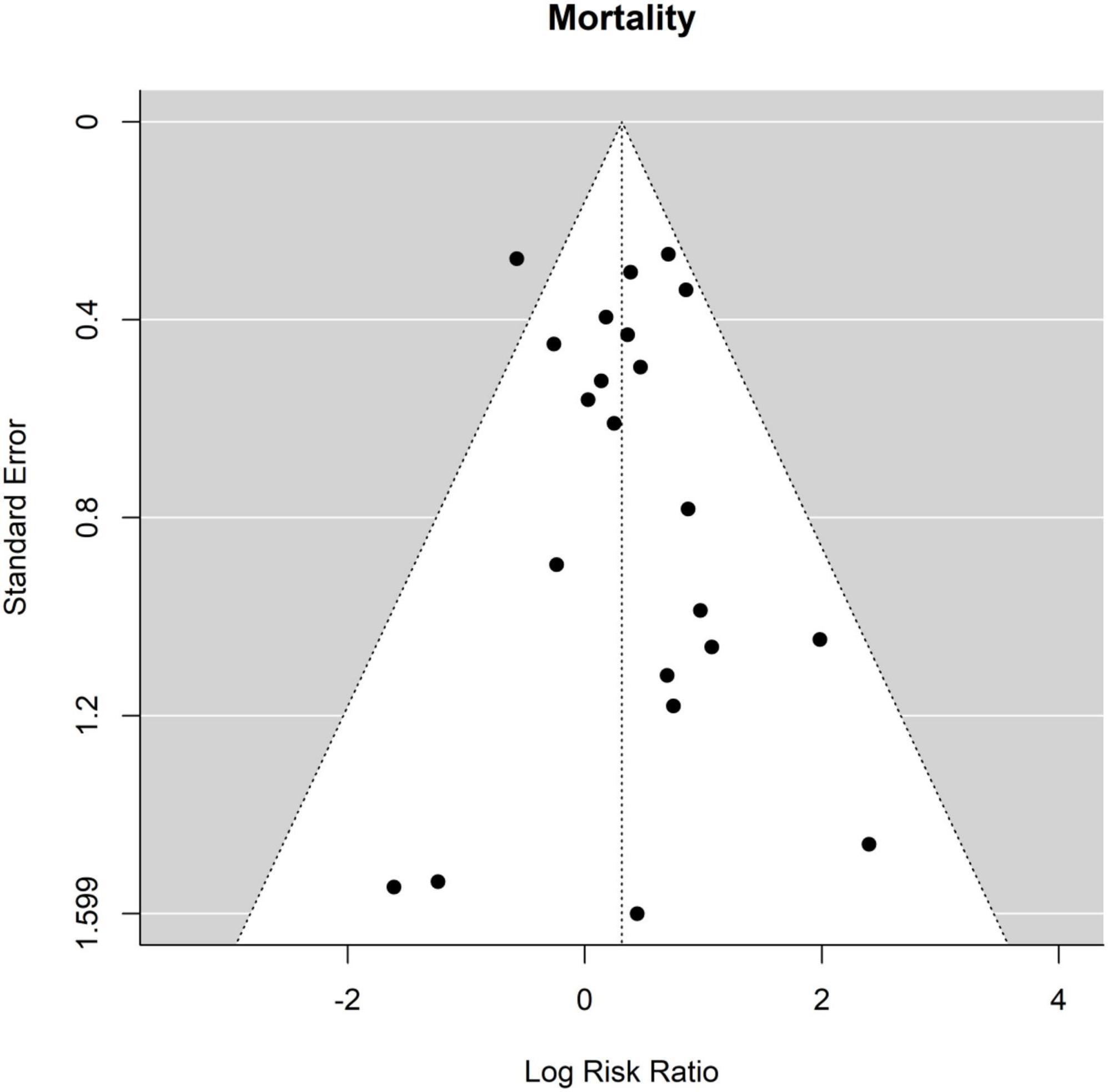
Figure 3. Relative risk of mortality in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Funnel plot.
The occurrence of SCI after ET was 45 out of 1693 patients (2.7%) and after FET was 70 out of 1,460 patients (4.8%). The RR for SCI of ET vs. FET was found to be 0.53 [0.35 to 0.81], (p = 0.004, I2 = 11.93%, p-value I2 = 0.53; Egger’s test −1.23 [−2.55 to 0.09]. FET was associated with a significantly higher risk for SCI (Figure 4, Forest plot). The funnel plot is shown in Figure 5 (asymmetry test: p = 0.21). Age and sex were not associated with the risk of SCI (Table 3).
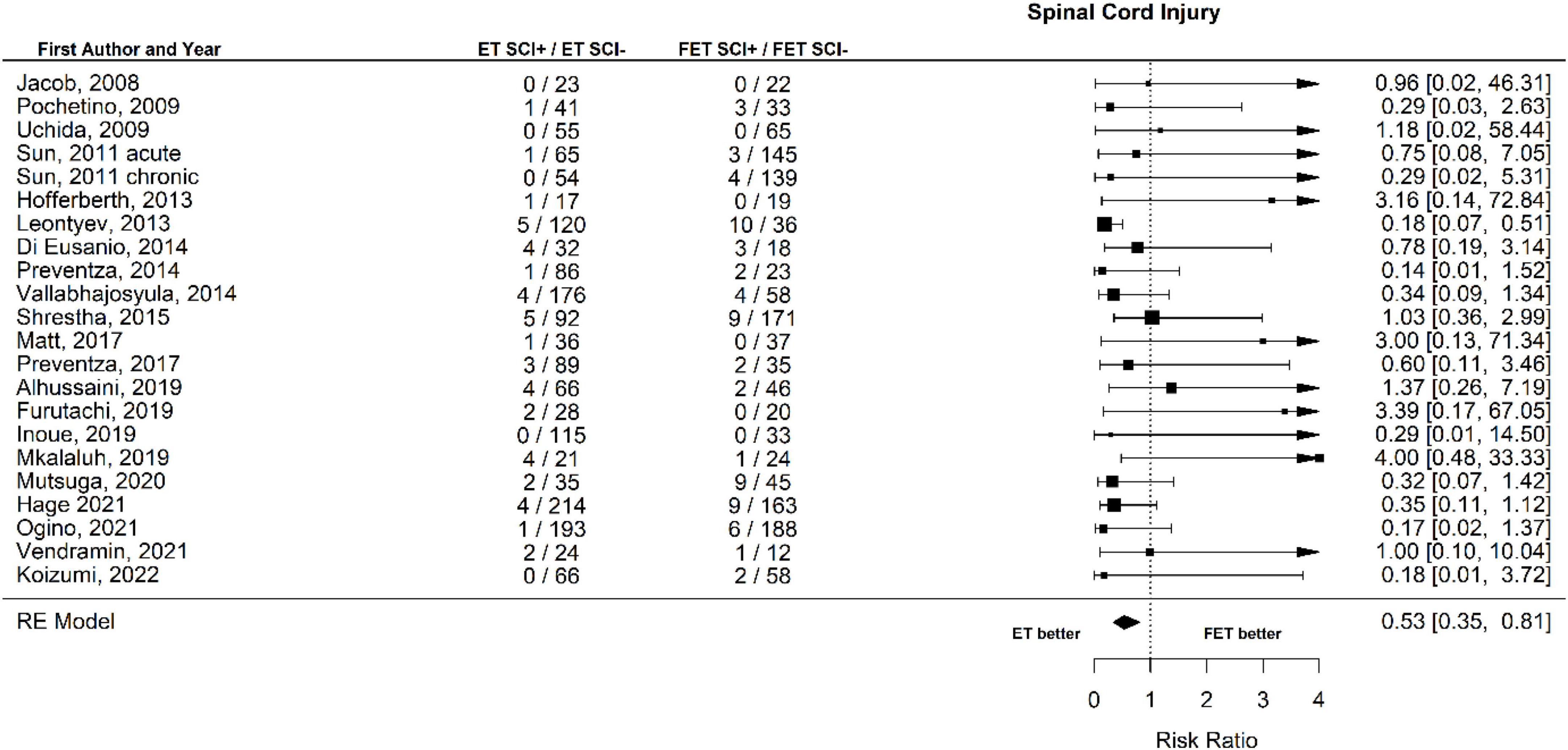
Figure 4. Relative risk of spinal cord injury (SCI) and hemiplegia/paraplegia in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Forest plot. ET vs. FET: p = 0.004.
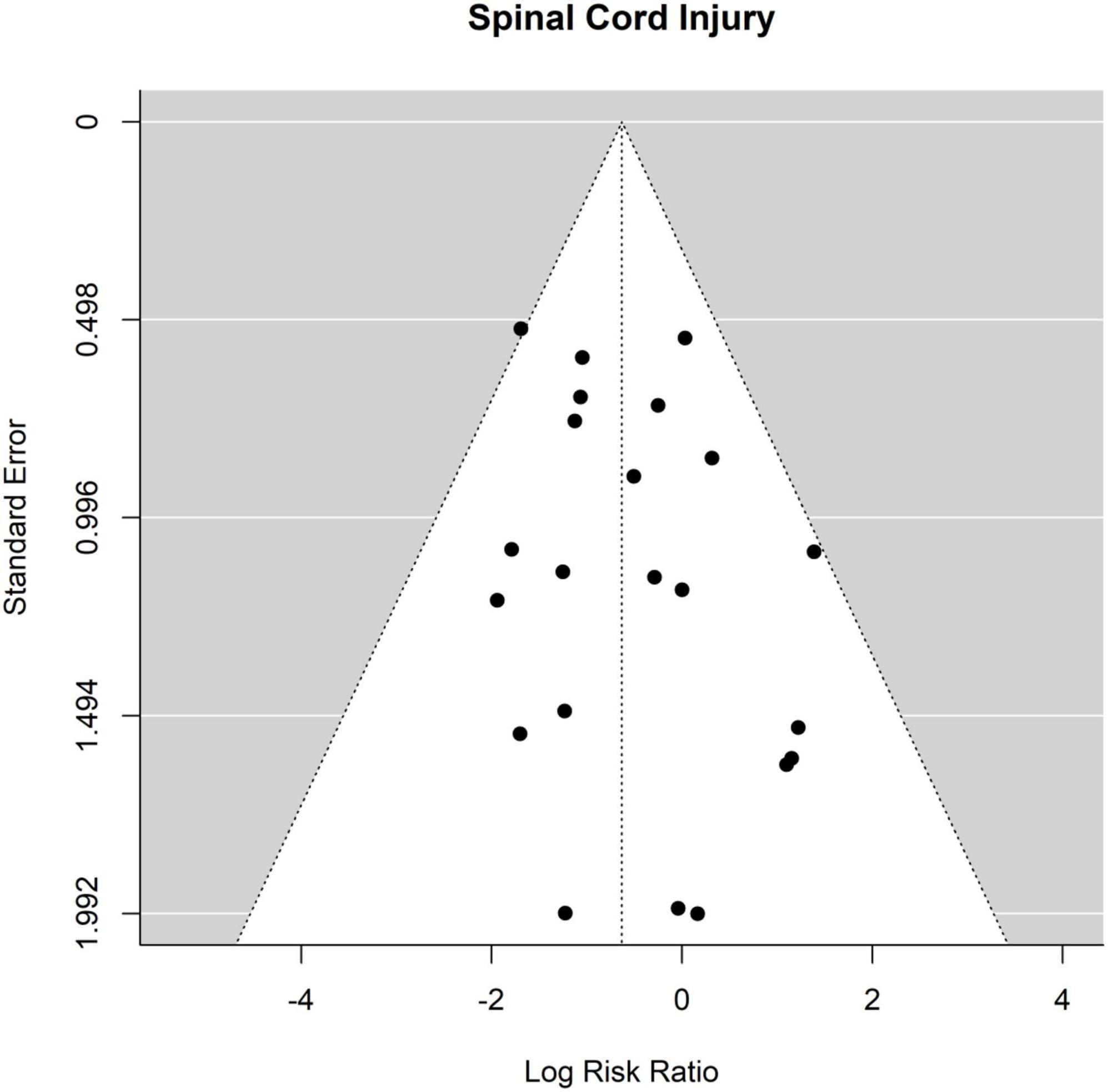
Figure 5. Relative risk of spinal cord injury (SCI) and hemiplegia/paraplegia in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Funnel plot.
Twenty out of the twenty-one studies contained sufficient data on the occurrence of stroke. No significant differences were found between ET and FET in the risk of stroke. The occurrence of stroke was 9.4% (148 of 1,578 patients) after ET and 7.8% (112 of 1,427 patients) (Figure 6, Forest plot). The RR was 1.06 [0.83 to 1.37] (p = 0.64, I2 = 0.0%, p-value I2 = 0.89; Egger’s test −0.03 [−0.38 to 0.32]. The funnel plot is shown in Figure 7 (asymmetry test: p = 0.64). There was no effect of age or sex on the outcome of stroke (Table 3).
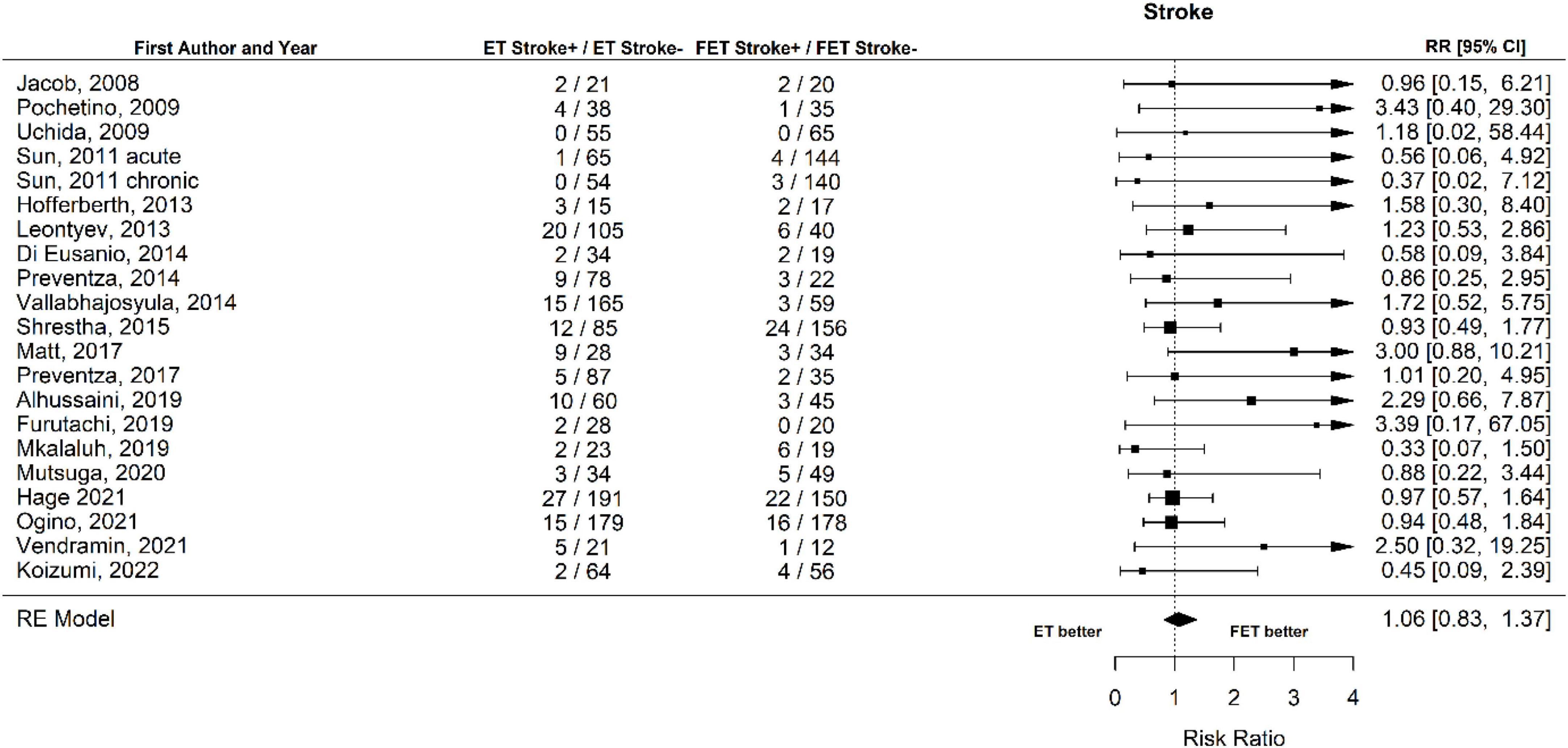
Figure 6. Relative risk of stroke in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Forest plot p = 0.89.
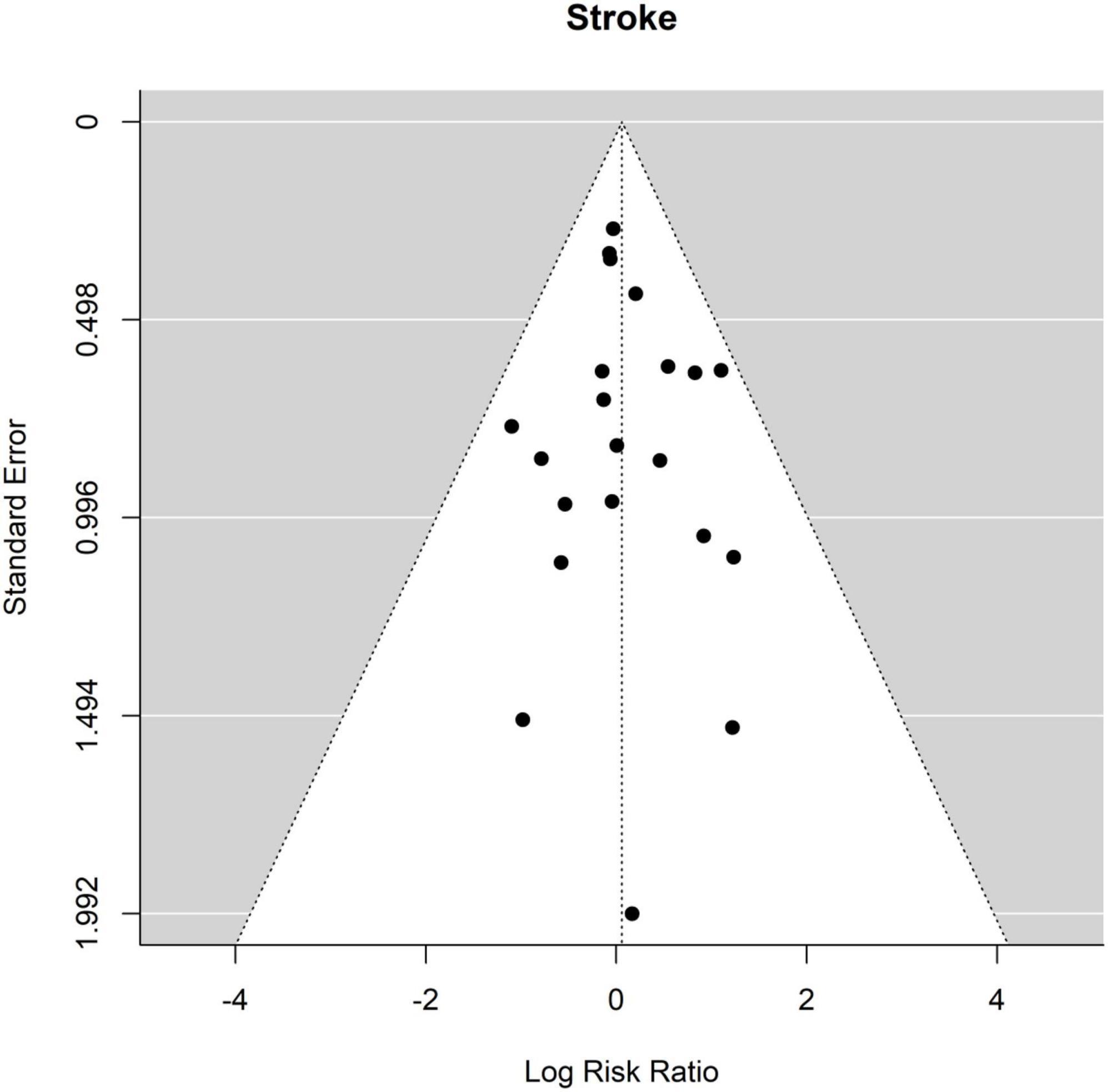
Figure 7. Relative risk of stroke in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Funnel plot.
Sixteen of the twenty-one studies contained data about renal failure. The occurrence of renal failure was 12.9% (158 of 1,223 patients) after ET and 10.0% (115 of 1,150 patients) (Figure 8 Forest plot). The RR of ET vs. FET was 0.98 [0.79 to 1.23] (p = 0.89, I2 = 0.0%, p-value I2 = 0.72; Egger’s test 0.17 [−0.69 to 1.02]. The funnel plot is shown in Figure 9 (asymmetry test: p = 0.37). There was no significant effect of age or sex on the outcome of renal failure (Table 3).
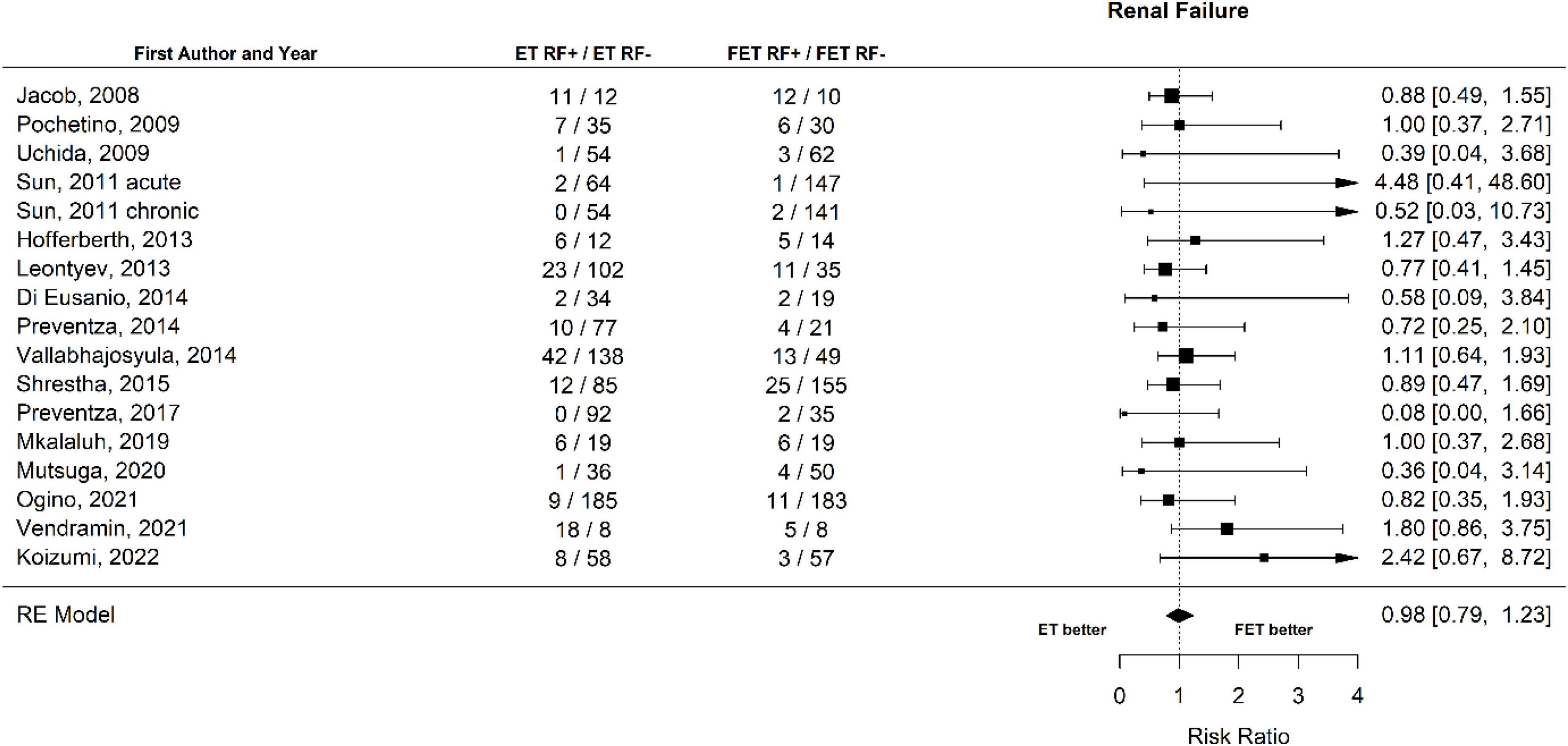
Figure 8. Relative risk of renal failure (RF) in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Forest plot p = 0.72.
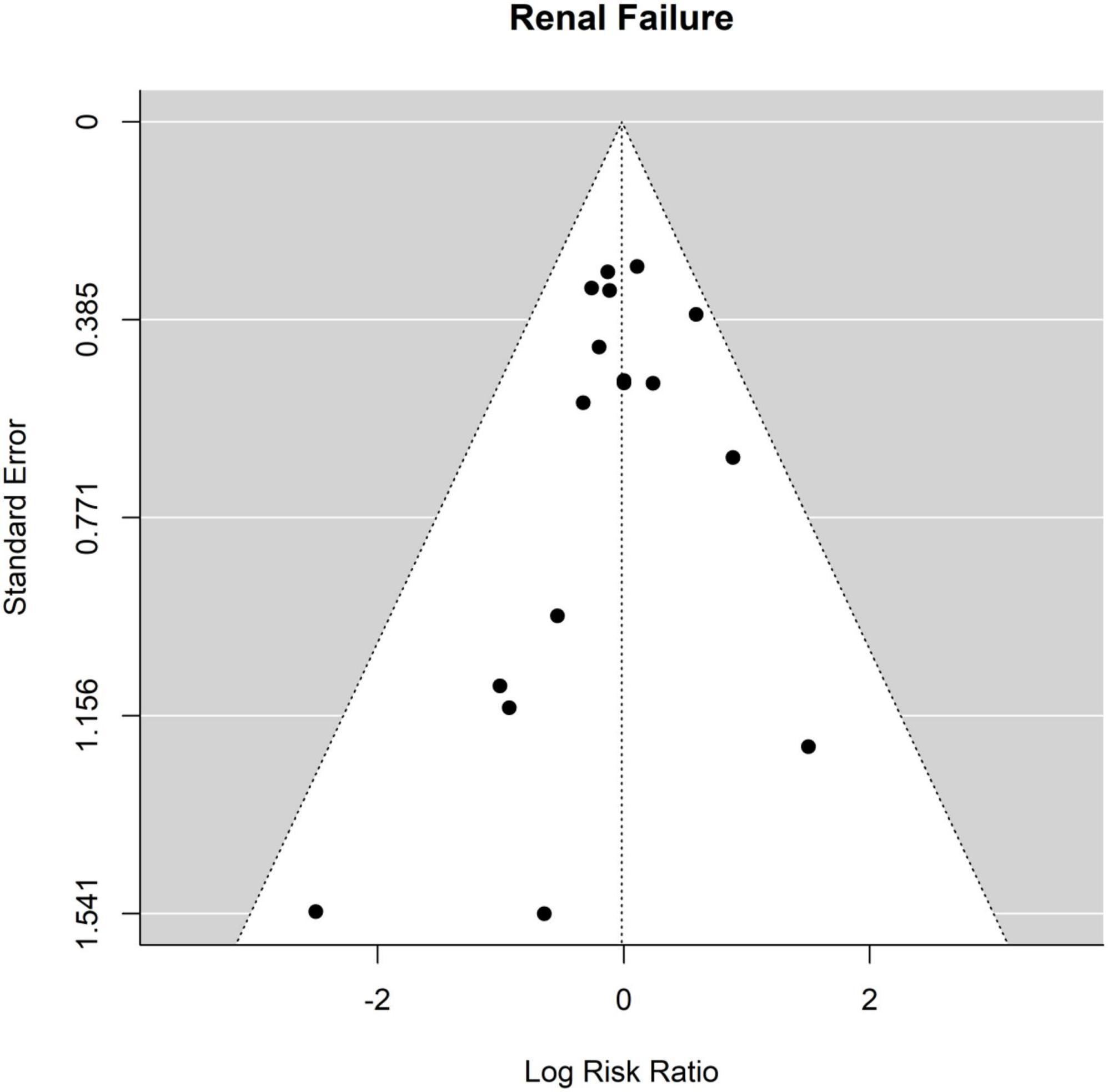
Figure 9. Relative risk of renal failure (RF) in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Funnel plot.
We hypothesized that the evolution of techniques and the availability of newer devices, and the subsequent experience, particularly for FET, could have a positive impact on the outcomes and likely reduce mortality and perioperative complications. To test this hypothesis, the statistics were re-run including only the articles that were published between 2017 and 2021 and contained data from newer studies ranging up to 2021. The results of this second analysis are presented below and are shown in Table 3 and Figures 10, 11 and Supplementary Figures 1–8.
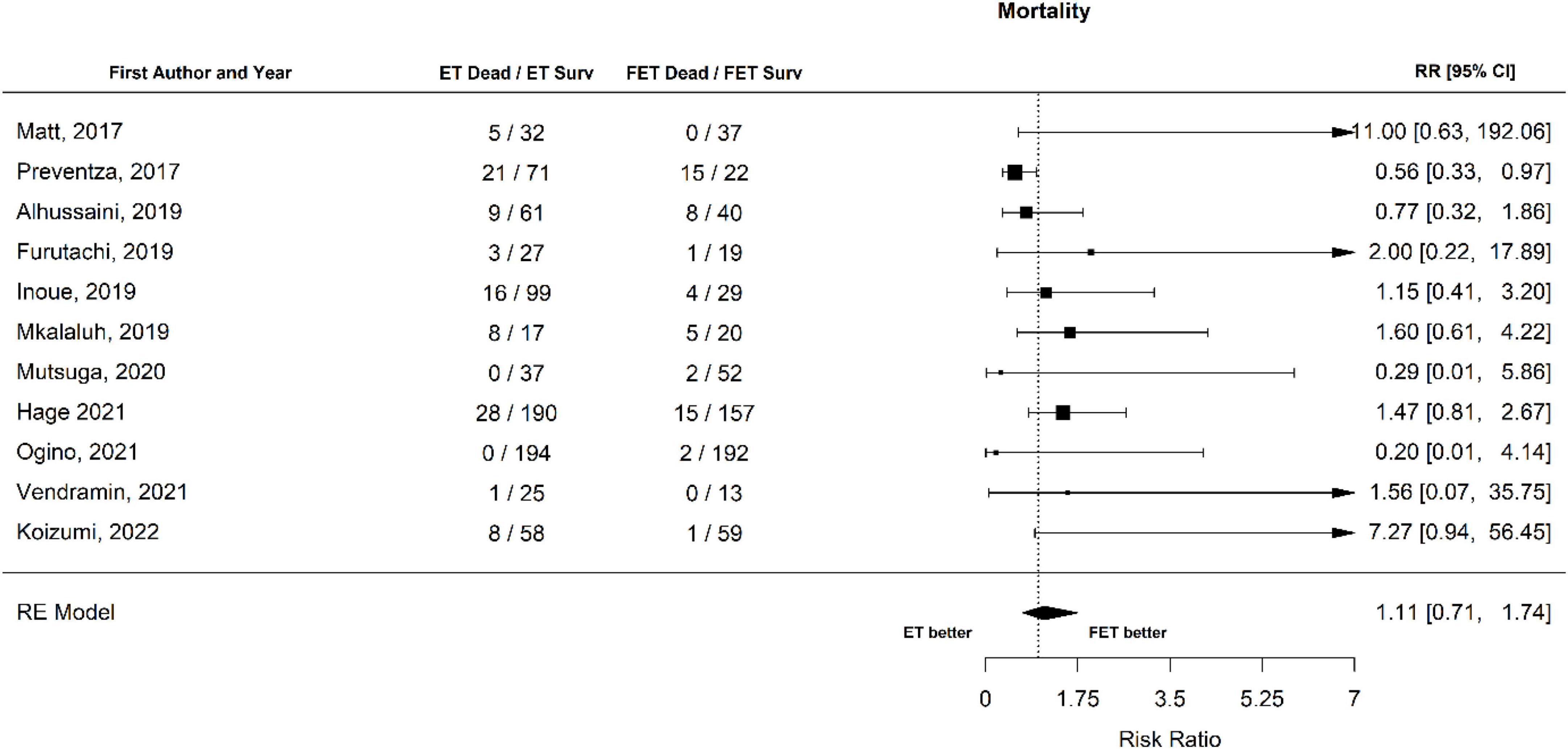
Figure 10. Relative risk of mortality in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Data only from studies published between 2017 and 2021. Forest plot p = 0.646.
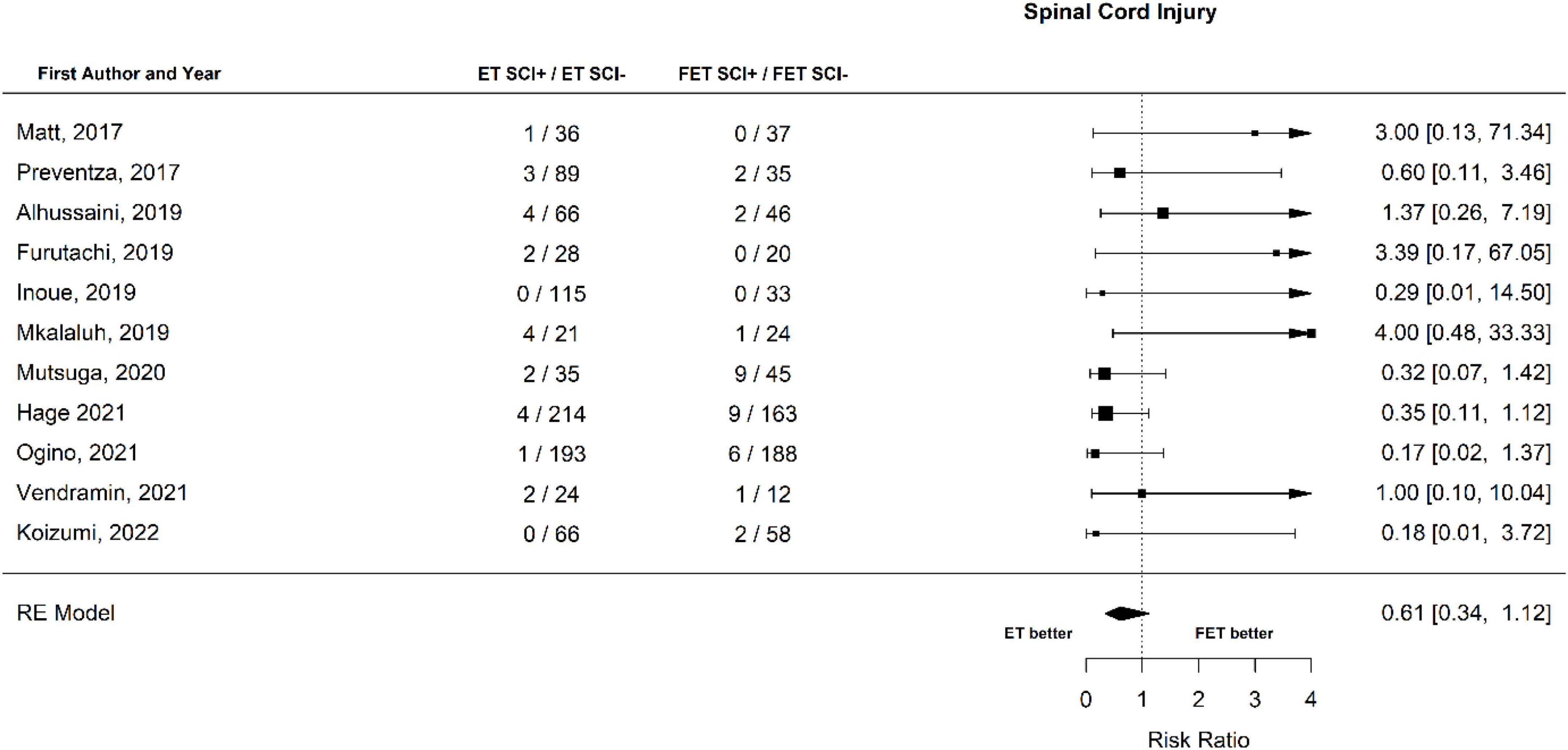
Figure 11. Relative risk of spinal cord injury (SCI) and hemiplegia/paraplegia in patients undergoing aortic interventions with conventional elephant trunk (ET) vs. frozen elephant trunk (FET). Data only from studies published between 2017 and 2021. Forest plot. ET vs. FET: p = 0.113.
In the papers published in the last 5 years, the overall mortality was 99 out of 910 (10.9%) in patients that underwent ET and 53 out of 693 (7.6%) in patients that underwent FET. There was no statistically significant difference in the risk between ET and FET. The RR for mortality of patients that underwent ET vs. patients that underwent FET was 1.11 [0.71 to 1.74] (p = 0.65), (Forest plot, Figure 10). There was no effect of age or sex on this outcome (Table 3).
When spinal cord injury and related neurological implications were examined in the papers published between 2017 and 2021, the RR of SCI of patients that underwent ET vs. patients that underwent FET was 0.61 [0.34 to 1.12]. In contrast with what was observed when all papers were examined, the trend for lower SCI did not reach statistical significance (p = 0.112) (Forest plot, Figure 11). A non-significant trend for SCI was observed with increasing age (p = 0.131). Male sex was associated with higher odds for SCI (p = 0.029).
The RR for stroke in the papers published between 2017 and 2021 was 1.06 [0.76 to 1.47] (Table 3). Increasing age was found to increase the risk for stroke (p = 0.044). There was no significant effect of sex on this outcome (Table 3).
When renal failure was examined in papers published in the last 5 years, the RR of ET vs. FET was 1.15 [0.71 to 1.88]. There was no significant effect of either age or sex on the outcome of renal failure (Table 3).
Discussion
The ET technique was introduced in the early 80 s for the correction of aortic arch aneurysms. The FET technique was introduced and developed between 1996 and 2003 in order to achieve similar results, to optimize the placement of the prosthesis in a single operative session and to combat the high interstage mortality that had been observed with the two-step ET technique (11, 13, 42). Since then, significant technical developments have occurred, including patient-tailored prostheses which are becoming increasingly popular (11).
The examined studies report conflicting results on the outcomes examined in this meta-analysis. Most of the examined studies reported no differences in mortality between ET and FET (21–23, 25–29, 31, 34–36, 38–41). Shrestha et al. (37) found significantly higher 30-day mortality in the ET group (24.7%) than in the FET group (12.2%), p = 0.011. Hage et al. (24) found a higher mortality rate after ET (13%) vs. FET (9%) (p = 0.022). According to a previous meta-analysis (12), the FET technique appears to have a lower perioperative mortality rate.
Our results also indicate that FET is probably associated with lower early mortality. As the RR (1.37 [1.04 to 1.81], p = 0.027) is relatively close to 1, this observation needs to be interpreted with caution. When papers published in the last 5 years (2017–2021) were examined, there was no statistically significant difference in early mortality. We hypothesized that the availability of better devices and the evolution of techniques and training of the personnel would contribute to a reduction of the mortality rate of FET. However, the mortality rate was similar in papers published in all years (7.9%) and in the last 5 years (7.6%). Notably, mortality in aortic arch replacement, especially type A dissection is confounded by several operative and patient specific factors, encumbering this comparison in a retrospective fashion.
Interestingly, while the FET technique has over the years a constant relatively low mortality rate, the ET technique has evolved and achieved reduced mortality rates in the last years. This improvement in mortality rate was observed in ET group within the last 5 years (10.9%) as compared to earlier years (14.8%). The improvement in mortality rates with primary procedure in conventional ET could be at least partially attributed to the evolution of the used techniques in cerebral protection and cardiopulmonary bypass.
It must be noted here, that this meta-analysis only examined early mortality up to 30 days after intervention. It is not known if the long-term mortality follows similar trends. In fact, the ET techniques is followed by a second procedure, which potentially increases the complication and mortality rate significantly. Nevertheless, the reported late mortality rates were conflicted and most studies report no differences after prolonged follow up. Jacob et al. (27) reported similar late mortality at follow-up (average follow-up ET 48 months, FET 23 months). Uchida et al. (39) found a survival rate of 69.0% after conventional arch replacement and 95.3% after FET after 5 years follow-up. Hofferberth et al. (25) reported survival rate 80% in ET vs. 87% in FET after a mean follow-up of 50 months. Mutsuga et al found an overall survival of 83% after ET and was 73% after FET at 5 years with no significant difference (p = 0.73). Koizumi et al. (28) reported no differences in mortality after 3 years follow-up.
According to previous studies there is a relatively high risk for a wide range of neurological complications in aortic arch surgery and these complications are well recorded (13, 43). However, there are studies showing that FET has more neurological complications when it comes to spinal cord injury, even suggesting that ET should be considered for patients who are expected to have more time under circulatory arrest in more moderate hypothermia. Leontyev et al. (29) reported lower occurrence of new-onset paraplegia after ET (4.0%) than after FET (21.7%), p < 0.001. Ogino et al reported lower rates of stroke (2.2 vs. 5.7% respectively, p = 0.022) and paraplegia (0 vs. 1.6%, p = 0.023) after ET as compared to FET respectively. These findings are partially confirmed by our analysis of all examined articles, where the RR for SCI of ET vs. FET was found to be 0.53 (p = 0.004). Nevertheless, when only the papers published within the last 5 years were examined, the RR was 0.61 and there was no statistical significance. It is possible that current evolution of the FET technique and improved devices have contributed to this outcome. Male sex was found to be associated with higher risk for SCI only in the analysis of the papers published in the last 5 years.
Renal failure resulting from hypoperfusion is another important complication related to aortic arch surgery. We found no significant difference in renal failure for both techniques, although comparing the most recent studies, a significant effect of increasing age in the occurrence of renal failure was observed.
Limitations
There are some limitations in this study.
There were no randomized controlled studies in this meta-analysis. Most of the studies were retrospective cohorts which results in selection bias.
Different types of devices were used in the examined studies and different operators with varying levels of experience performed the surgeries in centers with different settings and experiences. It is reasonable to assume that the outcomes of the interventions, particularly FET, are affected by the types of the devices used and the above mentioned parameters.
Not all the included studies contained data about all the examined outcomes (i.e., mortality, SCI, stroke, renal failure).
Further, it is also important to note that not all patients had the exact same type of lesion.
Conclusion
In conclusion, aortic arch surgery is a complex procedure where the outcome is related to a myriad of confounding factors including the surgical technique. In a retrospective fashion where the effect of inclusion bias is evident, we attempted to compare the evolution of outcomes of the commonly used ET and FET techniques. We found that the procedures show comparable results in complication and mortality rates, while the outcomes have improved in the most recent studies. Although there is a trend in higher rates of spinal cord injury in FET, for a complete comparison, the results of the second procedure in the ET technique should also be considered. Future studies should focus on prospective analysis of arch replacement techniques and consider less invasive hybrid procedures where debranching of aortic vessels are followed by stenting of the aneurysmatic arch.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AM: conceptualization and writing—original draft preparation. EB and EN: methodology. GP: software. SG: validation and writing—review and editing. OP: formal analysis and data curation. JR: investigation. JM: project administration. All authors have read and agreed to the published version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.999314/full#supplementary-material
References
1. Senser EM, Misra S, Henkin S. Thoracic aortic aneurysm: a clinical review. Cardiol Clin. (2021). 39:505–15. doi: 10.1016/j.ccl.2021.06.003
2. Cheng SW. Aortic arch pathologies - incidence and natural history. Gefasschirurgie. (2016) 21:212–6. doi: 10.1007/s00772-016-0155-5
3. Clouse WD, Hallett JW Jr, Schaff HV, Spittell PC, Rowland CM, Ilstrup DM, et al. Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. Mayo Clin Proc. (2004) 79:176–80. doi: 10.4065/79.2.176
4. LeMaire SA, Russell L. Epidemiology of thoracic aortic dissection. Nat Rev Cardiol. (2011) 8:103–13. doi: 10.1038/nrcardio.2010.187
5. Melvinsdottir IH, Lund SH, Agnarsson BA, Sigvaldason K, Gudbjartsson T, Geirsson A. The incidence and mortality of acute thoracic aortic dissection: results from a whole nation study. Eur J Cardiothorac Surg. (2016) 50:1111–7. doi: 10.1093/ejcts/ezw235
6. Baumann F, Makaloski V, Diehm N. [Aortic aneurysms and aortic dissection: epidemiology, pathophysiology and diagnostics]. Internist. (2013) 54:535–42. doi: 10.1007/s00108-012-3217-0
7. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American college of cardiology foundation/American heart association task force on practice guidelines, American association for thoracic surgery, American college of radiology, American stroke association, society of cardiovascular anesthesiologists, society for cardiovascular angiography and interventions, society of interventional radiology, society of thoracic surgeons, and society for vascular medicine. Circulation. (2010) 121:e266–369.
8. The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 Cochrane. (2019). Available online at: www.training.cochrane.org/handbook (accessed April 24, 2022).
9. Czerny M, Schmidli J, Adler S, van den Berg JC, Bertoglio L, Carrel T, et al. Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: an expert consensus document of the European association for cardio-thoracic surgery (EACTS) and the European society for vascular surgery (ESVS). Eur J Cardiothorac Surg. (2019) 55:133–62. doi: 10.1093/ejcts/ezy383
10. Borst HG, Walterbusch G, Schaps D. Extensive aortic replacement using “elephant trunk” prosthesis. Thorac Cardiovasc Surg. (1983) 31:37–40. doi: 10.1055/s-2007-1020290
11. Di Marco L, Murana G, Fiorentino M, Amodio C, Mariani C, Leone A, et al. The frozen elephant trunk surgery: a systematic review analysis. Indian J Thorac Cardiovasc Surg. (2019) 35(Suppl. 2):118–26. doi: 10.1007/s12055-019-00815-0
12. Hanif H, Dubois L, Ouzounian M, Peterson MD, El-Hamamsy I, Dagenais F, et al. Aortic arch reconstructive surgery with conventional techniques vs frozen elephant trunk: a systematic review and meta-analysis. Can J Cardiol. (2018) 34:262–73. doi: 10.1016/j.cjca.2017.12.020
13. Preventza O, Liao JL, Olive JK, Simpson K, Critsinelis AC, Price MD, et al. Neurologic complications after the frozen elephant trunk procedure: a meta-analysis of more than 3000 patients. J Thorac Cardiovasc Surg. (2020) 160:20–33.e4. doi: 10.1016/j.jtcvs.2019.10.031
14. Cekmecelioglu D, Koksoy C, Coselli J. The frozen elephant trunk technique in acute DeBakey type I aortic dissection. Turk Gogus Kalp Damar Cerrahisi Derg. (2020) 28:411–8. doi: 10.5606/tgkdc.dergisi.2020.20462
15. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. (2015) 350:g7647. doi: 10.1136/bmj.g7647
16. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. (2015) 162:777–84. doi: 10.7326/M14-2385
17. Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
18. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. (1998) 52:377–84. doi: 10.1136/jech.52.6.377
19. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. (2012) 22:276–82. doi: 10.11613/BM.2012.031
20. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
21. Alhussaini M, Abdelwahab A, Arnaoutakis GJ, Martin T, Salama Ayyad MAK, Ismail AIM, et al. Neurologic outcomes in aortic arch repair with frozen elephant trunk versus 2-stage hybrid repair. Ann Thorac Surg. (2019) 107:1775–81. doi: 10.1016/j.athoracsur.2018.11.042
22. Di Eusanio M, Borger M, Petridis FD, Leontyev S, Pantaleo A, Moz M, et al. Conventional versus frozen elephant trunk surgery for extensive disease of the thoracic aorta. J Cardiovasc Med. (2014) 15:803–9. doi: 10.2459/JCM.0b013e328364559c
23. Furutachi A, Takamatsu M, Nogami E, Hamada K, Yunoki J, Itoh M, et al. Early and mid-term outcomes of total arch replacement with the frozen elephant trunk technique for type A acute aortic dissection. Interact Cardiovasc Thorac Surg. (2019) 29:753–60. doi: 10.1093/icvts/ivz154
24. Hage A, Hage F, Dagenais F, Ouzounian M, Chung J, El-Hamamsy I, et al. Frozen elephant trunk for aortic arch reconstruction is associated with reduced mortality as compared to conventional techniques. Semin Thorac Cardiovasc Surg. (2021) 34:386–92. doi: 10.1053/j.semtcvs.2021.03.049
25. Hofferberth SC, Newcomb AE, Yii MY, Yap KK, Boston RC, Nixon IK, et al. Hybrid proximal surgery plus adjunctive retrograde endovascular repair in acute DeBakey type I dissection: superior outcomes to conventional surgical repair. J Thorac Cardiovasc Surg. (2013) 145:349–54. doi: 10.1016/j.jtcvs.2012.07.032
26. Inoue Y, Matsuda H, Omura A, Seike Y, Uehara K, Sasaki H, et al. Comparative study of the frozen elephant trunk and classical elephant trunk techniques to supplement total arch replacement for acute type A aortic dissectiondagger. Eur J Cardiothorac Surg. (2019) 56:579–86. doi: 10.1093/ejcts/ezz104
27. Jakob H, Tsagakis K, Tossios P, Massoudy P, Thielmann M, Buck T, et al. Combining classic surgery with descending stent grafting for acute DeBakey type I dissection. Ann Thorac Surg. (2008) 86:95–101. doi: 10.1016/j.athoracsur.2008.03.037
28. Koizumi S, Ishigami M, Tsubota H, Koyama T. Short- and mid-term outcomes of the frozen elephant-trunk procedure for degenerative aortic arch aneurysm. Surg Today. (2022) 52:324–9. doi: 10.1007/s00595-021-02337-y
29. Leontyev S, Borger MA, Etz CD, Moz M, Seeburger J, Bakhtiary F, et al. Experience with the conventional and frozen elephant trunk techniques: a single-centre study. Eur J Cardiothorac Surg. (2013) 44:1076–82. doi: 10.1093/ejcts/ezt252
30. Matt P, Banerjee P, Grapow M, Rueter F, Schurr U, Siegemund M, et al. Modified frozen elephant trunk for acute type A aortic dissection: a comparative study with standard repair technique. Eur J Cardiothorac Surg. (2017) 51:754–60. doi: 10.1093/ejcts/ezw412
31. Mkalaluh S, Szczechowicz M, Mashhour A, Zhigalov K, Easo J, Eichstaedt HC, et al. Total aortic arch replacement using elephant trunk or frozen elephant trunk technique: a case-control matching study. J Thorac Dis. (2018) 10:6192–200. doi: 10.21037/jtd.2018.10.42
32. Mutsuga M, Banno H, Narita Y, Komori K, Usui A. Editors’ Choice Which is superior, the frozen elephant trunk technique alone or the classical elephant trunk technique followed by second-stage thoracic endovascular aortic repair for extensive aortic arch repair? Nagoya J Med Sci. (2020) 82:657–66. doi: 10.18999/nagjms.82.4.657
33. Ogino H, Okita Y, Uchida N, Kato M, Miyamoto S, Matsuda H, et al. Comparative study of Japanese frozen elephant trunk device for open aortic arch repairs. J Thorac Cardiovasc Surg. (2021). [Epub ahead of print]. doi: 10.1016/j.jtcvs.2021.03.079
34. Pochettino A, Brinkman WT, Moeller P, Szeto WY, Moser W, Cornelius K, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg. (2009) 88:482–9. doi: 10.1016/j.athoracsur.2009.04.046
35. Preventza O, Cervera R, Cooley DA, Bakaeen FG, Mohamed AS, Cheong BY, et al. Acute type I aortic dissection: traditional versus hybrid repair with antegrade stent delivery to the descending thoracic aorta. J Thorac Cardiovasc Surg. (2014) 148:119–25. doi: 10.1016/j.jtcvs.2013.07.055
36. Preventza O, Coselli JS, Mayor J, Simpson K, Carillo J, Price MD, et al. The stent is not to blame: lessons learned with a simplified us version of the frozen elephant trunk. Ann Thorac Surg. (2017) 104:1456–63. doi: 10.1016/j.athoracsur.2017.03.072
37. Shrestha M, Beckmann E, Krueger H, Fleissner F, Kaufeld T, Koigeldiyev N, et al. The elephant trunk is freezing: the Hannover experience. J Thorac Cardiovasc Surg. (2015) 149:1286–93. doi: 10.1016/j.jtcvs.2015.01.044
38. Sun L, Qi R, Zhu J, Liu Y, Zheng J. Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch? Circulation. (2011) 123:971–8. doi: 10.1161/CIRCULATIONAHA.110.015081
39. Uchida N, Shibamura H, Katayama A, Shimada N, Sutoh M, Ishihara H. Operative strategy for acute type a aortic dissection: ascending aortic or hemiarch versus total arch replacement with frozen elephant trunk. Ann Thorac Surg. (2009) 87:773–7. doi: 10.1016/j.athoracsur.2008.11.061
40. Vallabhajosyula P, Szeto WY, Pulsipher A, Desai N, Menon R, Moeller P, et al. Antegrade thoracic stent grafting during repair of acute Debakey type I dissection promotes distal aortic remodeling and reduces late open distal reoperation rate. J Thorac Cardiovasc Surg. (2014) 147:942–8. doi: 10.1016/j.jtcvs.2013.10.047
41. Vendramin I, Lechiancole A, Piani D, Sponga S, Di Nora C, Muser D, et al. An integrated approach for treatment of acute type a aortic dissection. Medicina. (2021) 57:1155. doi: 10.3390/medicina57111155
42. Karck M, Chavan A, Hagl C, Friedrich H, Galanski M, Haverich A. The frozen elephant trunk technique: a new treatment for thoracic aortic aneurysms. J Thorac Cardiovasc Surg. (2003) 125:1550–3. doi: 10.1016/S0022-5223(03)00045-X
Keywords: elephant trunk, frozen elephant trunk, antegrade stent, aortic surgery, aortic aneurysm
Citation: Moula AI, Romeo JLR, Parise G, Parise O, Maessen JG, Natour E, Bidar E and Gelsomino S (2022) The evolution of arch surgery: Frozen elephant trunk or conventional elephant trunk? Front. Cardiovasc. Med. 9:999314. doi: 10.3389/fcvm.2022.999314
Received: 20 July 2022; Accepted: 20 September 2022;
Published: 20 October 2022.
Edited by:
Amer Harky, Liverpool Heart and Chest Hospital, United KingdomReviewed by:
Davut Cekmecelioglu, Cleveland Clinic, United StatesQipeng Luo, Peking University Third Hospital, China
Copyright © 2022 Moula, Romeo, Parise, Parise, Maessen, Natour, Bidar and Gelsomino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sandro Gelsomino, c2FuZHJvLmdlbHNvbWlub0BtYWFzdHJpY2h0dW5pdmVyc2l0eS5ubA==
 Amalia I. Moula
Amalia I. Moula Jamie L. R. Romeo
Jamie L. R. Romeo Gianmarco Parise
Gianmarco Parise Orlando Parise
Orlando Parise Sandro Gelsomino
Sandro Gelsomino