
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 22 August 2022
Sec. Cardiovascular Therapeutics
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.991293
This article is part of the Research TopicEffects of Oral Anticoagulant Therapy in Atrial Fibrillation Patients with ComorbiditiesView all 15 articles
 So-Ryoung Lee1†
So-Ryoung Lee1† Jin-Hyung Jung2†
Jin-Hyung Jung2† Eue-Keun Choi1,3*
Eue-Keun Choi1,3* Seung-Woo Lee2
Seung-Woo Lee2 Soonil Kwon1
Soonil Kwon1 Ji-Suck Park1
Ji-Suck Park1 Jeehoon Kang1
Jeehoon Kang1 Kyung-Do Han4
Kyung-Do Han4 Kyung Woo Park1,3
Kyung Woo Park1,3 Seil Oh1,3
Seil Oh1,3 Gregory Y. H. Lip3,5,6
Gregory Y. H. Lip3,5,6Objectives: To compare the net clinical benefit of oral anticoagulant (OAC) monotherapy to OAC plus single antiplatelet therapy (SAPT) in patients with atrial fibrillation (AF) and stable coronary artery disease (CAD) at 1- and 3-year after percutaneous coronary intervention (PCI).
Background: It has not been studied whether the net clinical benefit of the antithrombotic treatment options differs depending on the elapsed time from the index PCI.
Methods: Using the Korean nationwide claims database, we included AF patients who underwent PCI from 2009 to 2019 and constructed two cohorts: 1- and 3-year after PCI. In each cohort, the baseline characteristics of two groups were balanced using propensity score weighting. Ischemic stroke, myocardial infarction, major bleeding, and composite clinical outcomes were analyzed.
Results: Among patients with 1-year after PCI, OAC monotherapy (n = 678), and OAC plus SAPT (n = 3,159) showed comparable results for all clinical outcomes. In patients with 3-year after PCI, OAC monotherapy (n = 1,038) and OAC plus SAPT (n = 2,128) showed comparable results for ischemic stroke and myocardial infarction, but OAC monotherapy was associated with a lower risk of composite clinical outcomes (HR 0.762, 95% CI 0.607–0.950), mainly driven by the reduction of major bleeding risk (HR 0.498, 95% CI 0.345–0.701).
Conclusion: Oral anticoagulant monotherapy may be a comparable choice for patients with AF and stable CAD compared to OAC plus SAPT. In patients with stable CAD more than 3-year after index PCI, OAC monotherapy would be a better choice, being associated with less major bleeding and a positive net clinical benefit.
Oral anticoagulant (OAC) monotherapy is generally recommended in patients with atrial fibrillation (AF) and stable coronary artery disease (CAD) (1–4). In a previous meta-analysis, OAC monotherapy showed a comparable risk of major adverse cardiovascular events and a lower risk of major bleeding than OAC plus single antiplatelet agent (SAPT) (5). There have also been two randomized clinical trials that evaluated the optimal antithrombotic therapy for patients with AF and stable CAD (6, 7). The OAC-ALONE trial was the first randomized trial comparing OAC monotherapy vs. OAC plus SAPT in patients with AF and stable CAD beyond 1-year after undergoing percutaneous coronary intervention (PCI) (6). However, non-inferiority of OAC monotherapy to OAC plus SAPT for the composite of major adverse cardiovascular events was not established because of inadequate statistical power (6). Recently, the AFIRE trial showed that rivaroxaban monotherapy was non-inferior for efficacy and superior for safety to rivaroxaban plus SAPT in patients with AF and stable CAD (7).
Although the AFIRE trial demonstrated that rivaroxaban monotherapy is superior to rivaroxaban plus SAPT in primary safety outcomes, there have been conflicting data regarding the comparative effectiveness and safety of OAC monotherapy vs. OAC plus SAPT according to the time from index PCI to study enrollment (8, 9). Considering the temporal dynamic of the risk of stent thrombosis after PCI and thromboembolic risk in patients with AF (10), we can hypothesize that the efficacy and safety of antithrombotic treatment strategies can temporally vary. However, it has not been studied whether the net clinical benefit of the antithrombotic treatment options differs depending on the elapsed time from the index PCI.
In this study, we aimed to compare the effectiveness, safety, and net clinical benefit of OAC monotherapy to OAC plus SAPT in patients with AF and stable CAD at 1- and 3-year after PCI in a contemporary real-world observational cohort.
This analysis was performed based on the Korean nationwide claims database from the Korean Health Insurance Review Agency (HIRA) database. In South Korea, all citizens are subscribed to the medical insurance system, called the Korean National Health Insurance Service (NHIS) provided by the Korean government (11). Information on subscribers’ medical use is collected for NHIS operation, and information on medical use, which becomes insurance coverage, is submitted from health care providers. The submitted information is reviewed by the Korean HIRA, which is a quality control department that provides a review of the medical costs incurred. The Korean HIRA database contains all medical expenses claim data of the entire Korean population, including subscribers’ demographic information, diagnoses, examinations, prescriptions, and procedures for both inpatient and outpatient services (11, 12). Diagnoses were coded based on the International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) codes (11, 12).
Using the Korean nationwide claims database, we included AF patients who underwent PCI from January 1, 2009 to February 28, 2019. Considering dynamic changes in antithrombotic therapy according to the period after receiving PCI, the index antithrombotic treatment was independently defined at different times after receiving PCI and we constructed two cohorts: 1- and 3-year after PCI (Figure 1). Cohort 1 consisted of patients who had just passed 1 year after PCI. Patients with AF who underwent PCI between September 1, 2009 and June 30, 2017, were firstly identified. Patients who died before 1-year after PCI and underwent repeated PCI before 1-year after PCI were excluded. Among these, the OAC monotherapy group and OAC plus SAPT group were defined by identifying prescriptions between 12 and 15 months from PCI (Figure 1A). Cohort 2 was defined as patients 3 years after PCI. Patients with AF who underwent PCI between September 1, 2009 and June 30, 2015, were included. Similar to cohort 1, patients who died before 3-year after PCI and underwent repeated PCI before 3-year after PCI were excluded. OAC monotherapy group and OAC plus SAPT group were identified by the prescription between 36 and 39 months from PCI (Figure 1B).
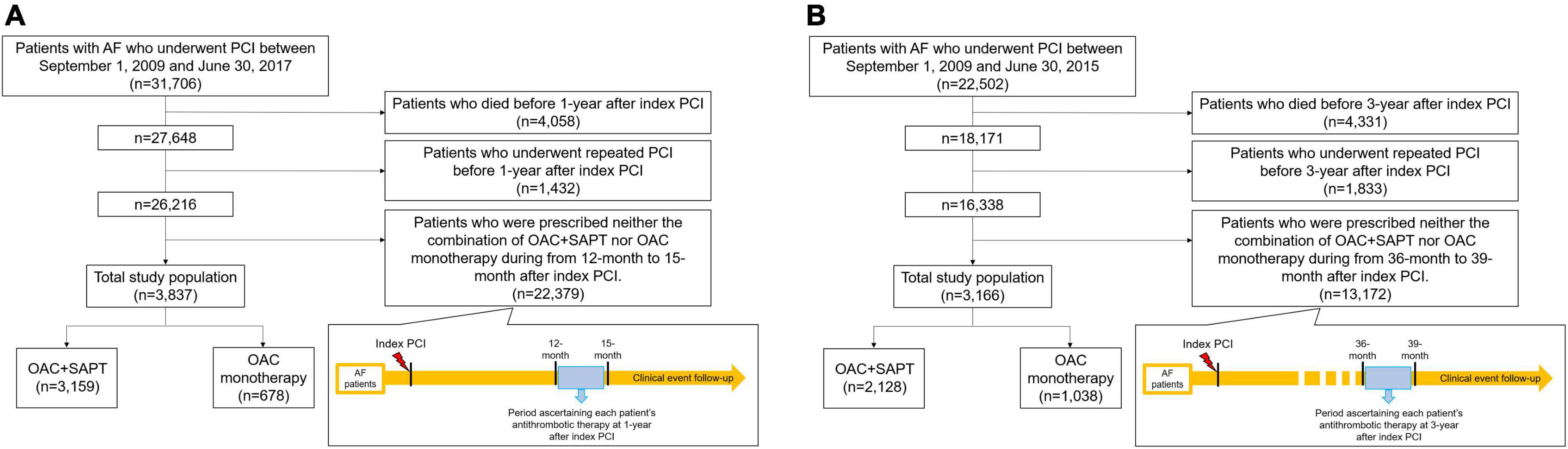
Figure 1. Study design and patient enrollment flow. (A) Cohort 1: patients with AF who underwent PCI, 1-year after index PCI. (B) Cohort 2: patients with AF who underwent PCI, 3-year after index PCI. AF, atrial fibrillation; OAC, oral anticoagulant; PCI, percutaneous coronary intervention; SAPT, single antiplatelet agent.
The study design was approved by the Institutional Review Board of the Seoul National University Hospital (E-1911-052-1078). The review board waived informed consent since each patient is de-identified and encrypted in the HIRA database to ensure patient privacy.
Subjects’ age, sex, comorbidities including hypertension, diabetes, dyslipidemia, heart failure, prior myocardial infarction, peripheral artery disease, prior ischemic stroke/transient ischemic attack/systemic embolism, prior intracranial hemorrhage, prior gastrointestinal bleeding, renal disease, and liver disease were ascertained by the prespecified operational definitions summarized in Supplementary Table 1 (13, 14). Concomitant medications include renin-angiotensin-aldosterone system inhibitors, beta-blockers, calcium channel blockers, loop diuretics, statins, non-steroidal anti-inflammatory drugs, and proton-pump inhibitors were ascertained based on the prescription records. The type of OAC [warfarin or direct oral anticoagulant (DOAC) including rivaroxaban, dabigatran, apixaban, and edoxaban], dose of DOAC, type of antiplatelet agents among aspirin, clopidogrel, prasugrel or ticagrelor were also identified. CHA2DS2-VASc score and modified HAS-BLED score were calculated by the operational definitions of comorbidities and medical history including concomitant medication (Supplementary Table 1) (13, 14).
During the follow-up period, composites of ischemic stroke and myocardial infarction occurrence were identified for effectiveness evaluation. For safety evaluation, major bleeding was defined as a composite of intracranial hemorrhage, gastrointestinal bleeding, and extracranial/unclassified major bleeding. We identified the major bleeding that occurred during the follow-up period. To assess net clinical benefit, composite clinical outcomes of ischemic stroke, myocardial infarction, and major bleeding were ascertained. Furthermore, we reported each component of effectiveness and safety outcome as follows: ischemic stroke, myocardial infarction, intracranial hemorrhage, gastrointestinal bleeding, and gastrointestinal bleeding requiring transfusion. Clinical outcomes were defined by the ICD-10-CM codes and detailed definitions of clinical outcomes are summarized in Supplementary Table 1.
To evaluate the accuracy of the operational definitions of clinical outcomes including ischemic stroke, myocardial infarction, intracranial hemorrhage, and gastrointestinal bleeding, we conducted a validation study in a tertiary hospital with 200 randomly chosen patients with the relevant ICD-10-CM codes for each event (15). Patients’ medical records were reviewed by two physicians (JP and SK). The positive predictive values of the operational definitions were 91.2, 92, 95.1, and 91.7% for ischemic stroke, myocardial infarction, intracranial hemorrhage, and gastrointestinal bleeding (15). In each cohort, the index date was the first date of OAC monotherapy or OAC plus SAPT prescription. Patients were censored at the outcome events or the end of the study period (February 28, 2019), whichever came first.
Continuous variables are presented as mean (standard deviation) and median (interquartile ranges, IQR). Categorical variables are presented as number and percentage. For each clinical outcome, the crude incidence rate for each clinical outcome was estimated by dividing the number of incidents during the follow-up period by the number of 100 person-years at risk. Unadjusted hazard ratios (HRs) and 95% confidence intervals (CIs) were analyzed for estimation of the risk of clinical outcomes using the Cox proportional hazards regression models.
To compare the OAC monotherapy and OAC plus SAPT groups, propensity score methods were used (16). A logistic regression model with all baseline factors (except for DOAC dose) was used to determine the probability score for being in each treatment group. To balance baseline characteristics across the two treatment groups, time-to-event analyses were conducted using inverse probability of treatment weighting (IPTW) analysis with stabilized weights computed from the propensity score (17, 18). Following IPTW, the covariate balance between the two groups was determined using the absolute standardized difference (ASD) (19). In a covariate, an ASD of ≤0.1 (10%) indicated that the two groups were well-balanced, with a negligible difference. The weighted number of events throughout the follow-up period was divided by 100 person-years at risk to calculate the weighted incidence rates. Survival analysis with the Kaplan-Meier method (log-rank test) and weighted Cox proportional hazards regression models with IPTW were used to determine the risk of clinical outcomes for OAC monotherapy and OAC plus SAPT (reference).
To provide complementary results, we conducted multivariable Cox analyses for a sensitivity analysis. Age, sex, hypertension, diabetes mellitus, dyslipidemia, heart failure, prior myocardial infarction, peripheral artery disease, prior stroke/transient ischemic attack/systemic embolism, prior intracranial hemorrhage, prior gastrointestinal bleeding, renal disease, liver disease, CHA2DS2-VASc score, modified HAS-BLED score, and OAC type (warfarin or DOAC) were included for the multivariable-adjusted Cox analyses.
SAS software, version 9.3 (SAS Institute, Cary, NC, United States), was used for all statistical analyses, and a two-tailed p-value of 0.05 was considered statistically significant.
In cohort 1 among patients 1-year after PCI, 678 patients with OAC monotherapy and 3,159 patients with OAC plus SAPT were included. In cohort 2 among patients 3-years after PCI, 1,038 patients with OAC monotherapy and 2,128 patients with OAC plus SAPT were enrolled.
Baseline characteristics are presented in Tables 1, 2. In cohort 1, the OAC monotherapy group were older, more likely to be women, and had higher CHA2DS2-VASc scores than OAC plus SAPT group. OAC monotherapy group showed a higher prevalence of prior ischemic stroke/transient ischemic attack/systemic embolism than the OAC plus SAPT group. Regarding OAC types, the OAC monotherapy group was more likely to be prescribed DOAC rather than warfarin compared to OAC plus SAPT group. Among DOAC users, the OAC plus SAPT group was more likely to be prescribed a reduced dose of DOAC than the OAC monotherapy group. Among SAPT for OAC plus SAPT group, clopidogrel was the most commonly prescribed (65.9%), followed by aspirin (33.8%). In cohort 2, similar differences between the two groups were observed as in cohort 1. OAC monotherapy group were older, more likely to be women, and had higher CHA2DS2-VASc scores compared to OAC plus SAPT group. Diabetes mellitus was more prevalent in OAC plus SAPT group than in the OAC monotherapy group. DOAC prescription was more common in the OAC monotherapy group. Among DOAC users, reduced dose DOAC use was more common in patients with OAC plus SAPT. Among SAPT for OAC plus SAPT group, aspirin was the most commonly prescribed (52.2%), followed by clopidogrel (47.7%). The baseline characteristics were well-balanced after IPTW between the two groups in both cohorts except for the DOAC dose (Tables 1, 2 and Supplementary Figure 1).
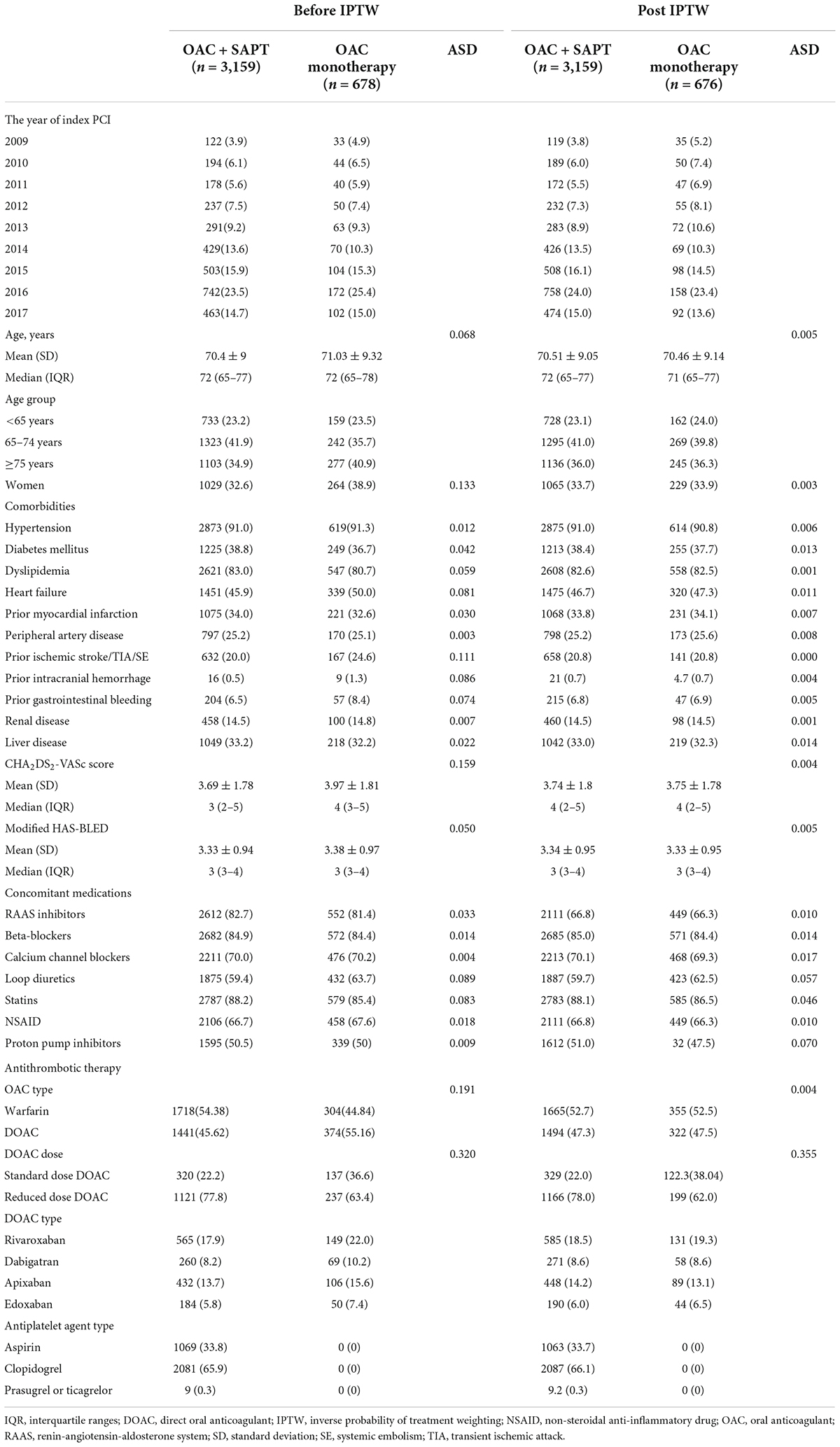
Table 1. Baseline characteristics of oral anticoagulant (OAC) plus single antiplatelet therapy (SAPT) and OAC monotherapy groups at 1-year after index percutaneous coronary intervention (PCI).
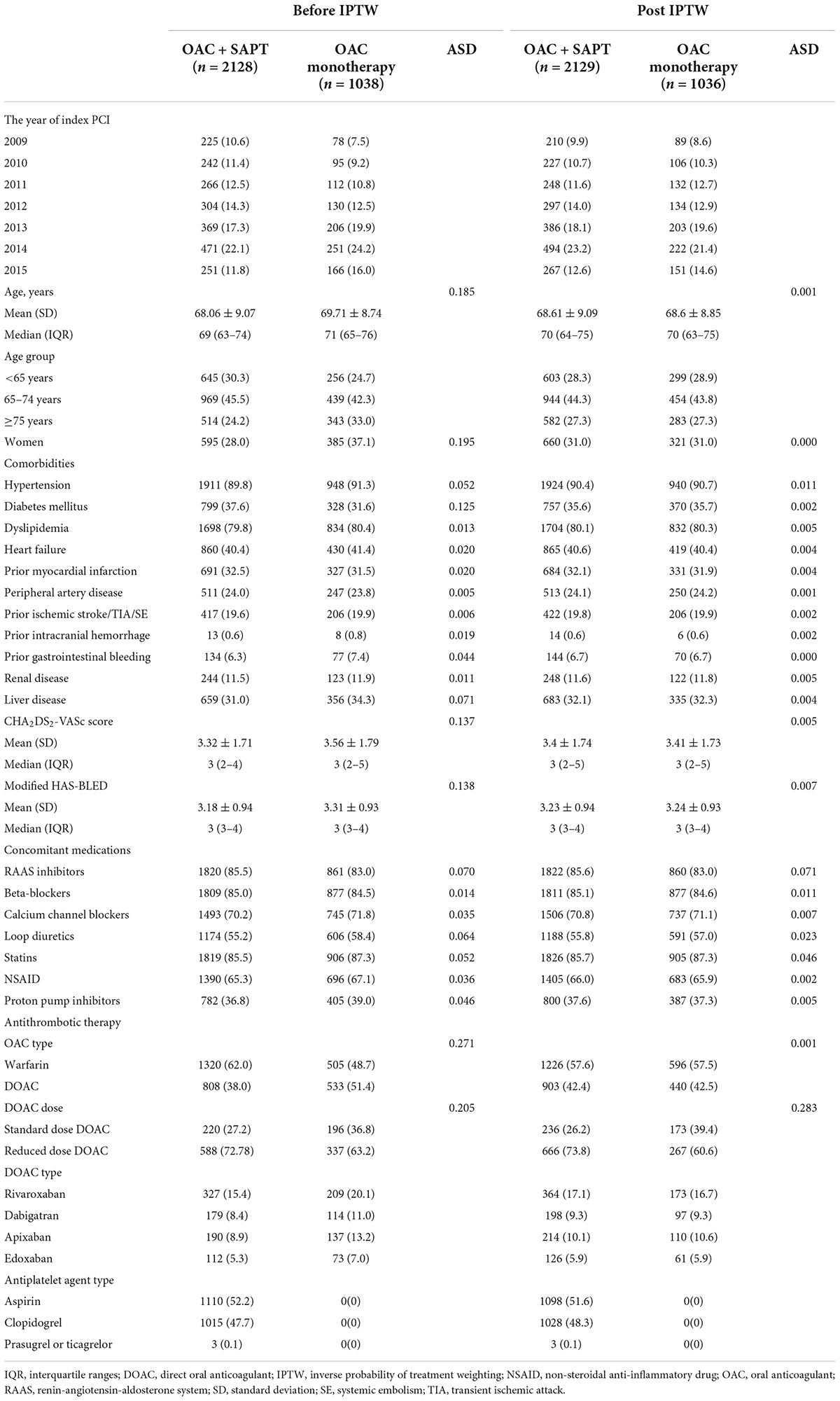
Table 2. Baseline characteristics of OAC plus SAPT and OAC monotherapy groups at 3-year after index PCI.
A median follow-up duration of cohort 1 was 2.3 (IQR, 1.2–4.2) years. Crude incidence rates of clinical outcomes and unadjusted HRs for clinical outcomes are presented in Supplementary Table 2. Figure 2A showed weighted cumulative incidence curves of effectiveness, safety, and composite clinical outcomes of cohort 1. Weighted incidence rates and weighted HRs are presented in Figure 3A. After IPTW, OAC monotherapy and OAC plus SAPT showed comparable risks for a composite of ischemic stroke and myocardial infarction, major bleeding, and composite clinical outcomes (Figures 2A, 3A). OAC monotherapy and OAC plus SAPT did not show any significant differences for the individual components of the effectiveness and safety outcomes.
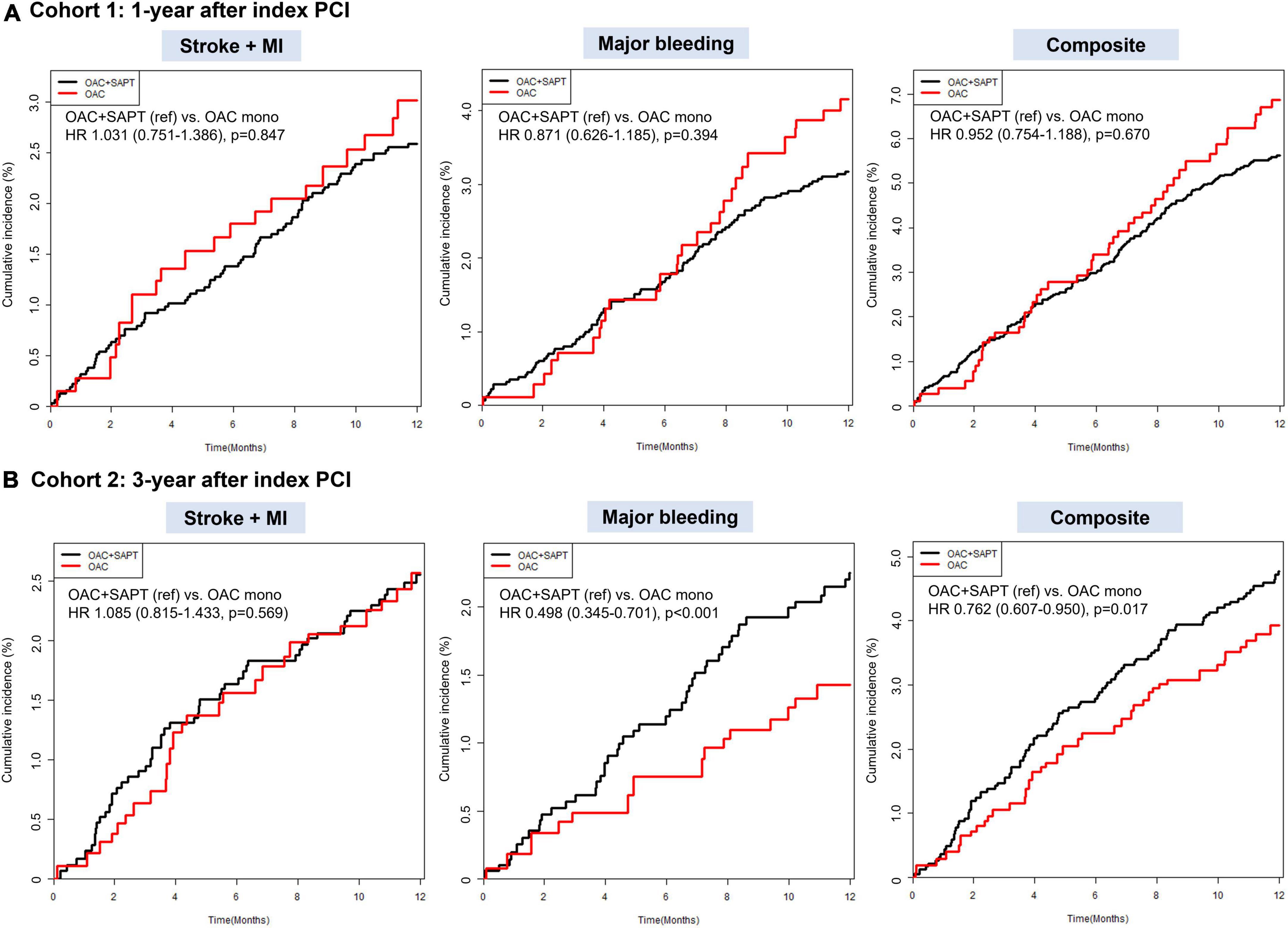
Figure 2. Weighted cumulative incidence curves for ischemic stroke/myocardial infarction, major bleeding, and composite clinical outcome: OAC plus SAPT vs. OAC monotherapy. (A) Cohort 1: patients with AF who underwent PCI, 1-year after index PCI. (B) Cohort 2: patients with AF who underwent PCI, 3-year after index PCI. HR, hazard ratio; OAC, oral anticoagulant; SAPT, single antiplatelet agent.
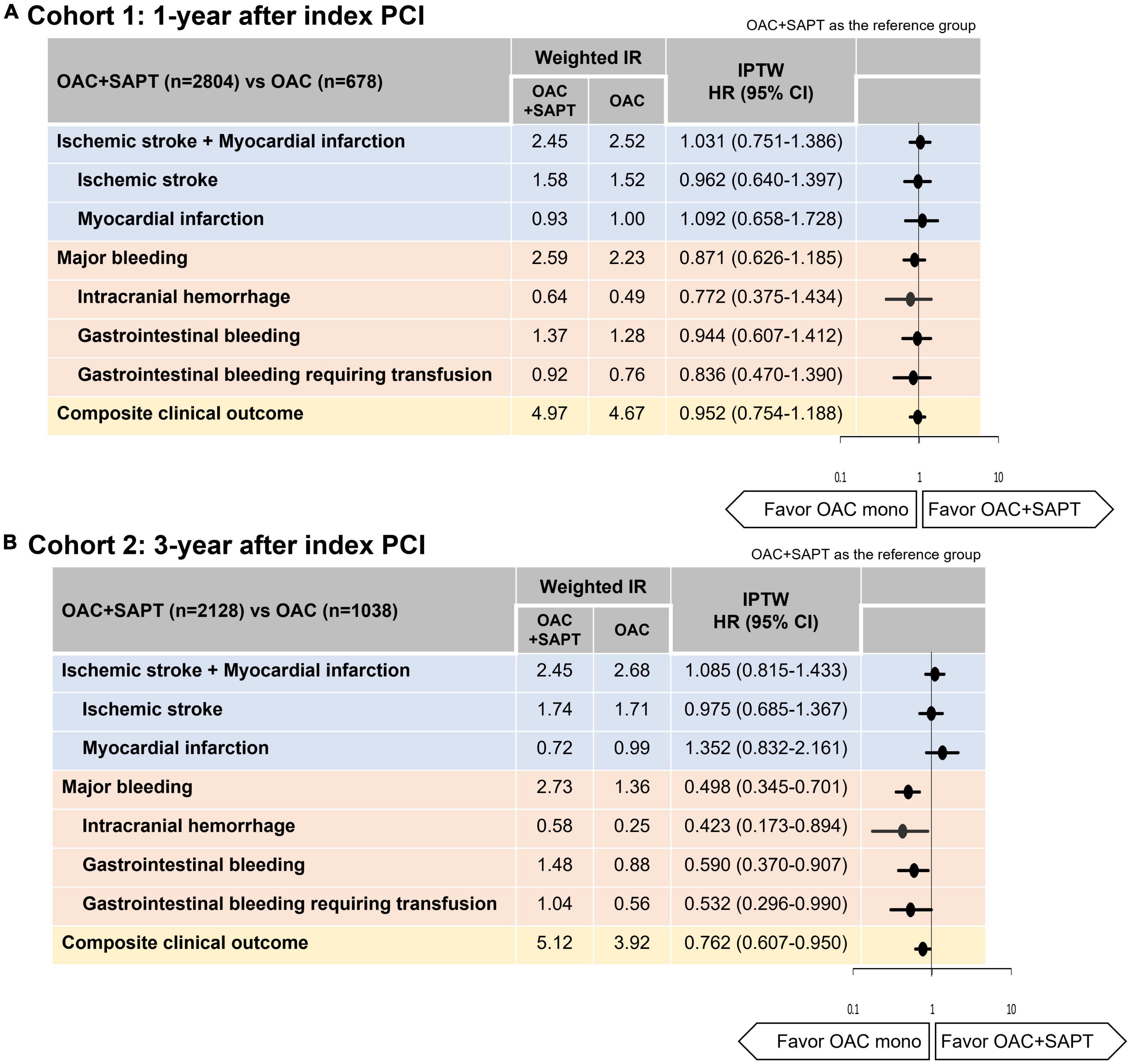
Figure 3. Hazard ratios of ischemic stroke, myocardial infarction, major bleeding, and composite clinical outcome: OAC plus SAPT vs. OAC monotherapy. (A) Cohort 1: patients with AF who underwent PCI, 1-year after index PCI. (B) Cohort 2: patients with AF who underwent PCI, 3-year after index PCI. IR, 100 person-years. CI, confidence interval; HR, hazard ratio; IR, incidence rate; IPTW, inverse probability of treatment weighting; OAC, oral anticoagulant; SAPT, single antiplatelet agent.
A median follow-up duration of cohort 2 was 2.5 (IQR, 1.3–4.2) years. Crude incidence rates of clinical outcomes and unadjusted HRs for clinical outcomes are presented in Supplementary Table 2. Figure 2B showed weighted cumulative incidence curves of effectiveness, safety, and composite clinical outcomes of cohort 2. Weighted incidence rates and weighted HRs are presented in Figure 3B. In cohort 2 with 3-year after PCI, OAC monotherapy and OAC plus SAPT showed a comparable risk for a composite of ischemic stroke and myocardial infarction, however, OAC monotherapy was associated with a lower risk of composite clinical outcomes (HR 0.762, 95% CI 0.607–0.950), mainly driven by a reduction of major bleeding risk (HR 0.498, 95% CI 0.345–0.701) compared to OAC plus SAPT (Figures 2B, 3B).
For each component of effectiveness and safety outcomes, OAC monotherapy and OAC plus SAPT group showed comparable risks for both ischemic stroke and myocardial infarction (Figure 3B). OAC monotherapy was associated with lower risks of intracranial hemorrhage, gastrointestinal bleeding, and gastrointestinal bleeding requiring transfusion than OAC plus SAPT (Figure 3B).
Multivariable Cox analyses showed consistent results with the IPTW analyses in two cohorts (Supplementary Table 2).
In this nationwide population-based observational study, our principal findings are as follows: (1) a substantial proportion of AF patients who had been receiving PCI for more than a year was prescribed OAC plus SAPT rather than OAC monotherapy; (2) among patients who had just passed 1 year after PCI, OAC monotherapy showed comparable risks for ischemic stroke, myocardial infarction, and major bleeding compared to OAC plus SAPT; (3) among patients 3 years after PCI, OAC monotherapy was associated with a lower risk of the composite clinical outcomes of ischemic stroke, myocardial infarction, and major bleeding than OAC plus SAPT, mainly driven by a lower risk of major bleeding. From these results, OAC monotherapy results in positive net clinical benefits by reducing bleeding risk in AF patients with sufficiently stable CAD after PCI (Figure 4). From the results of this study and previous clinical trials, OAC monotherapy would be the most reasonable option for patients with AF with stable CAD (1-year beyond PCI) as the current guidelines (1–4).
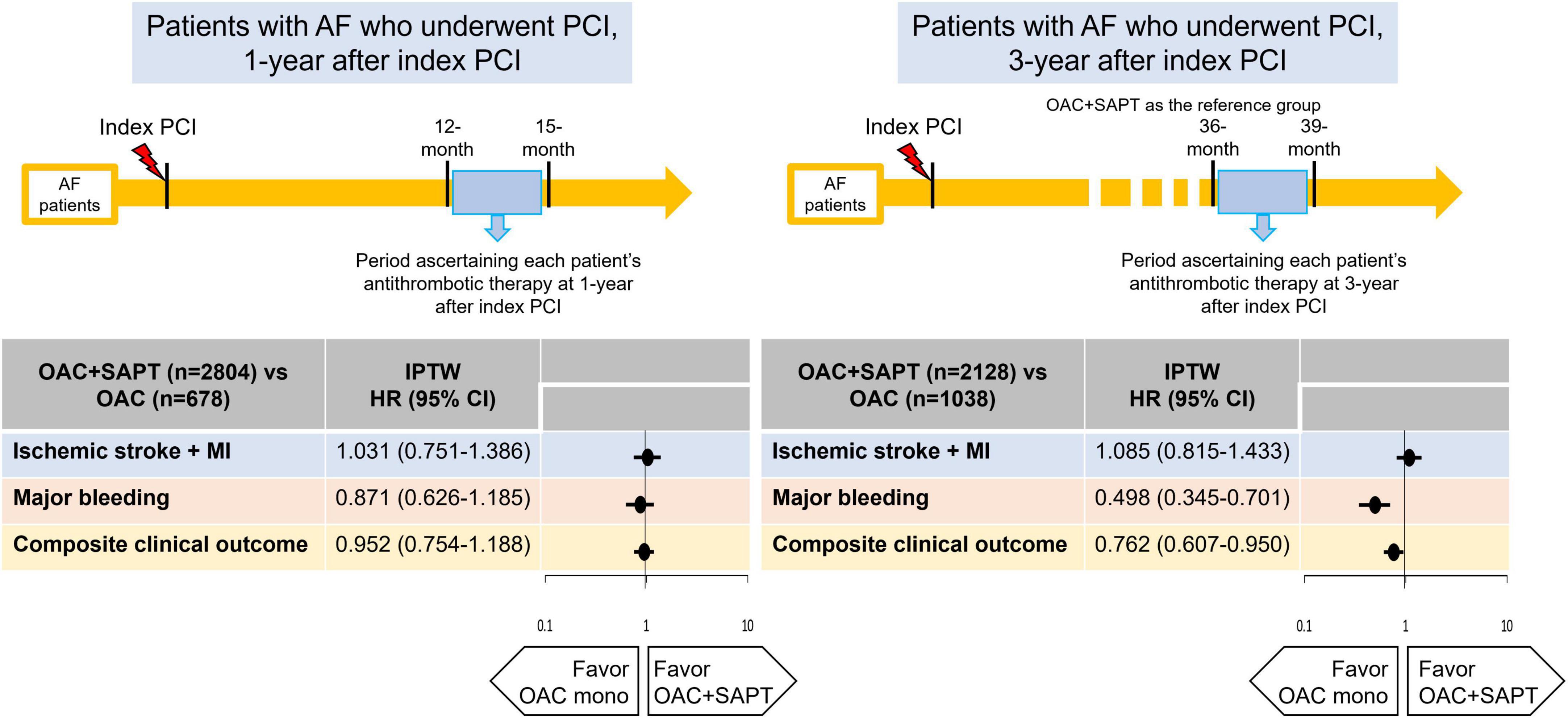
Figure 4. Hazard ratios of ischemic stroke, myocardial infarction, major bleeding, and composite clinical outcome: OAC plus SAPT vs. OAC monotherapy. AF, atrial fibrillation; CI, confidence interval; HR, hazard ratio; IPTW, inverse probability of treatment weighting; MI, myocardial infarction; OAC, oral anticoagulant; PCI, percutaneous coronary intervention; SAPT, single antiplatelet agent.
In a previous observational study based on the Danish nationwide cohort, warfarin-based OAC monotherapy was suggested as the most optimal antithrombotic therapy regimen in patients with stable CAD defined as 12 months from an acute coronary event (20). Compared to warfarin, single or dual antiplatelet therapy without anticoagulation was associated with increased risks of myocardial infarction, thromboembolism, death from the coronary event, and all-cause death. A combination of warfarin and single or dual antiplatelet therapy was related to the excessive bleeding risk compared to warfarin monotherapy.
Based on the consistent results of several observational studies (5), the guidelines have therefore advocated prescribing OAC monotherapy in AF patients 1 year following PCI as a Class IIa recommendation (21). However, the evidence generated through RCTs per se may be insufficient. The first RCT comparing OAC alone vs. OAC plus SAPT in patients with AF beyond 1 year after PCI, the OAC-ALONE trial, was reported (6). The median time from the last PCI was 4.4 (IQR 1.8–7.7) years in the OAC monotherapy group or 4.6 (IQR 2.4–7.4) years in OAC plus SAPT group, respectively. Among the total study population, only 25% were prescribed DOAC. Hence, the main results of the OAC-ALONE trial were inconclusive. More recently, the results of the AFIRE study, which included a large number of patients and used rivaroxaban as anticoagulation therapy, were published (7). This trial showed rivaroxaban monotherapy was significantly safer and more effective than rivaroxaban plus SAPT in patients with AF and stable CAD.
Despite the recommendations of the latest guidelines and updated evidence, a substantial proportion of patients with AF and stable CAD still do not receive guideline adherent antithrombotic therapy (22, 23). In contrast to the high rates of dual antiplatelet treatment, the overall rates of OAC were low after PCI in patients with AF. Since the emergence of DOACs, the usage of triple anti-thrombotic therapy in periprocedural antithrombotic regimens has shifted significantly, particularly in DOAC-based regimens. Regarding antithrombotic therapy 1 year after PCI, DAPT was more prevalent than OAC therapy. Also, OAC monotherapy 1 year after PCI was significantly lower than OAC plus SAPT therapy even in the DOAC era. In clinical practice, most patients with AF who underwent PCI continued to receive antiplatelet agents beyond 1-year post-PCI (23). This could be seen as a reflection of physicians’ preference for continuing to utilize the antiplatelet therapy in patients undergone PCI while omitting anticoagulation therapy because of the concern of excessive bleeding.
There have been two recent conflicting observational studies for patients with AF who underwent PCI beyond 1-year (8, 9). In a previous study including patients with AF who were at “early” stable period from PCI (immediate after 1-year), OAC plus SAPT seemed to be more effective than OAC monotherapy, without a difference in safety (8). In another previous study enrolled AF patients who were stable for more than 1-year after PCI, the mean time difference between the last PCI and the index date was 24 ± 18 months (9). OAC monotherapy showed similar efficacy to OAC plus SAPT and was associated with a lower risk of hospitalization due to bleeding compared to OAC plus SAPT. Neither net clinical benefit nor survival benefit of OAC monotherapy was documented.
Considering the results of previous studies and the trade-off of ischemic risk and bleeding risk after PCI (8–10, 24), the clinical benefits of OAC monotherapy over OAC plus SAPT may differ depending on how long it has elapsed since a year from PCI. However, there have been no studies attempting to analyze whether the benefit of treatment varies with the elapsed time after PCI in RCTs or observational studies. Recently, a post-hoc analysis of AFIRE study including patients who had undergone PCI has been reported which showed that in the PCI subgroup, the main results were consistently observed that rivaroxaban monotherapy was associated with lower risks of the primary efficacy and safety endpoints, compared to combination therapy (25). The median time from PCI to index date was 48 (IQR, 21–91) months, and most were more than 24 months after PCI. When analyzing the efficacy and safety endpoints over time after PCI, the differences in efficacy endpoints were not significant according to the time after PCI; however, in terms of safety endpoint, the longer the time elapsed after PCI, the more the OAC monotherapy benefits were accentuated compared to OAC plus SAPT. Overall, the net clinical benefit also became more evident with the longer time between PCI and enrollment. Our study showed consistent results through a large real-world observational cohort that the benefit of OAC monotherapy is more certain to reduce bleeding risk in patients with AF that are sufficiently stable after PCI.
While two RCTs have been reported (6, 7), more evidence is still needed for AF patients with stable CAD, and the results of the EPIC-CAD trial (NCT03718559), are awaited (26).
First, there is a possibility of residual confounding, although we ascertained available variables and matched the balance between the two treatment groups. Among possible confounders, these data did not include information about the characteristics and numbers of coronary stents, the complexity of PCI procedure, and the presence of remaining significant coronary lesions. Second, this study is an observational study, which would include more comprehensive patients than RCTs in which patients are highly selected, but patients who died within 1 or 3 years or who received repeated PCI were excluded from the study design. However, if a physician considers prescribing patients without additional coronary events for several years after PCI, our data can be applied practically. Third, OAC monotherapy and OAC plus SAPT do not represent the majority of prescriptions in AF patients with stable CAD in Korea, who are often prescribed with antiplatelet agents only (22, 23). Therefore, the number of study subjects is limited, and it should be considered when interpreting the results that patients who received OAC prescriptions in real-world practice were selected by physicians. Fourth, the Korean HIRA database did not include laboratory findings such as serum creatinine. Therefore, to indirectly measure renal dysfunction, we included “renal diseases” as one of the baseline covariates defined using the operational definition adopted in previous observational studies based on the claims database (14, 22, 23). Fifth, among DOAC users in OAC plus SAPT group, a higher proportion of patients were prescribed reduced dose DOAC than those in the OAC monotherapy group. In previous observational studies and even in the RCT (6, 9), reduced dose DOAC was preferred in OAC plus SAPT group. In this dataset, patients’ body weight and creatinine clearance were not available, thus, DOAC dosing adherence could not be evaluated. Notwithstanding the higher proportion of reduced dose DOAC in the OAC plus SAPT group than in the OAC monotherapy group, a combination of OAC and SAPT still showed a higher risk of bleeding than OAC monotherapy. Sixth, two types of antiplatelet agents (aspirin and clopidogrel) were prescribed for the most of patients in the OAC plus SAPT group. Although which antiplatelet agents are better than others also can be an important question for clinical practice, the primary objective of this study was the comparison between OAC and OAC plus SAPT in patients with AF and stable CAD. The number of the study population was not sufficient to explore the better antiplatelet type or the better OAC type for these populations. Further clinical or observational studies are needed to answer this question.
Oral anticoagulant monotherapy may be a comparable choice for patients with AF and stable CAD compared to OAC plus SAPT. In patients with stable CAD more than 3-year after index PCI, OAC monotherapy would be a better choice, being associated with less major bleeding and a positive net clinical benefit.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Seoul National University Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
S-RL and J-HJ: conceptualization, data curation, formal analysis, investigation, methodology, resources, software, validation, visualization, writing – original draft, figures and tables generation, and writing – review and editing. E-KC: conceptualization, formal analysis, investigation, methodology, resources, validation, funding acquisition, project administration, supervision, and writing – review and editing. S-WL, SK, and J-SP: conceptualization, data curation, formal analysis, investigation, methodology, resources, software, and validation. JK, K-DH, KP, SO, and GL: conceptualization, investigation, methodology, supervision, and writing – review and editing. All authors contributed to the article and approved the submitted version.
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health and Welfare, Republic of Korea, and the Ministry of Food and Drug Safety) (Project Number: 202013B14), the Korea National Research Foundation funded by the Ministry of Education, Science and Technology (grant no. 2020R1F1A106740), and the Seoul National University Hospital Research Fund (grant no. 3020200200).
E-KC: research grants or speaking fees from Abbott, Bayer, BMS/Pfizer, Biosense Webster, Chong Kun Dang, Daewoong Pharmaceutical Co., Daiichi-Sankyo, DeepQure, Dreamtech Co., Ltd., Jeil Pharmaceutical Co. Ltd., Medtronic, Samjinpharm, Seers Technology, and Skylabs. GL: consultant and speaker for BMS/Pfizer, Boehringer Ingelheim, and Daiichi-Sankyo.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.991293/full#supplementary-material
1. Angiolillo DJ, Bhatt DL, Cannon CP, Eikelboom JW, Gibson CM, Goodman SG, et al. Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a north American perspective: 2021 update. Circulation. (2021) 143:583–96. doi: 10.1161/CIRCULATIONAHA.120.050438
2. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J. (2021) 42:373–498. doi: 10.1093/eurheartj/ehab648
3. Chao TF, Joung B, Takahashi Y, Lim TW, Choi EK, Chan YH, et al. 2021 focused update consensus guidelines of the Asia Pacific heart rhythm society on stroke prevention in atrial fibrillation: executive summary. Thromb Haemost. (2022) 122:20–47. doi: 10.1055/s-0041-1739411
4. Lip GYH, Collet JP, Haude M, Byrne R, Chung EH, Fauchier L, et al. 2018 Joint European consensus document on the management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous cardiovascular interventions: a joint consensus document of the European Heart Rhythm Association (EHRA), European society of cardiology working group on thrombosis, European association of percutaneous cardiovascular interventions (EAPCI), and European association of acute cardiac care (ACCA) endorsed by the heart rhythm society (HRS), Asia-Pacific heart rhythm society (APHRS), Latin America heart rhythm society (LAHRS), and Cardiac arrhythmia society of Southern Africa (CASSA). Europace. (2019) 21:192–3. doi: 10.1093/europace/euy174
5. Lee SR, Rhee TM, Kang DY, Choi EK, Oh S, Lip GYH. Meta-analysis of oral anticoagulant monotherapy as an antithrombotic strategy in patients with stable coronary artery disease and nonvalvular atrial fibrillation. Am J Cardiol. (2019) 124:879–85. doi: 10.1016/j.amjcard.2019.05.072
6. Matsumura-Nakano Y, Shizuta S, Komasa A, Morimoto T, Masuda H, Shiomi H, et al. Open-label randomized trial comparing oral anticoagulation with and without single antiplatelet therapy in patients with atrial fibrillation and stable coronary artery disease beyond 1 year after coronary stent implantation. Circulation. (2019) 139:604–16. doi: 10.1161/CIRCULATIONAHA.118.036768
7. Yasuda S, Kaikita K, Akao M, Ako J, Matoba T, Nakamura M, et al. Antithrombotic therapy for atrial fibrillation with stable coronary disease. N Engl J Med. (2019) 381:1103–13. doi: 10.1056/NEJMoa1904143
8. Yoon GS, Kim SH, Kang SH, Yoon CH, Cho YS, Youn TJ, et al. Prognosis of atrial fibrillation patients undergoing PCI according to anticoagulants and antiplatelet agents. J Clin Med. (2021) 10:3370. doi: 10.3390/jcm10153370
9. Choi Y, Lee Y, Kim SH, Kim S, Kim JY, Kim TS, et al. Single direct oral anticoagulant therapy in stable patients with atrial fibrillation beyond 1 year after coronary stent implantation. Heart. (2022) 108:285–91. doi: 10.1136/heartjnl-2020-318750
10. Buccheri S, Angiolillo DJ, Capodanno D. Evolving paradigms in antithrombotic therapy for anticoagulated patients undergoing coronary stenting. Ther Adv Cardiovasc Dis. (2019) 13:1753944719891688. doi: 10.1177/1753944719891688
11. Seong SC, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol. (2017) 46:799–800.
12. Choi EK. Cardiovascular research using the Korean national health information database. Korean Circ J. (2020) 50:754–72. doi: 10.4070/kcj.2020.0171
13. Lip GYH, Keshishian A, Li X, Hamilton M, Masseria C, Gupta K, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients. Stroke. (2018) 49:2933–44. doi: 10.1161/STROKEAHA.118.020232
14. Lee SR, Choi EK, Kwon S, Han KD, Jung JH, Cha MJ, et al. Effectiveness and safety of contemporary oral anticoagulants among Asians with nonvalvular atrial fibrillation. Stroke. (2019) 50:2245–9. doi: 10.1161/STROKEAHA.119.025536
15. Park J, Kwon S, Choi EK, Choi YJ, Lee E. Validation of diagnostic codes of major clinical outcomes in a national health insurance database. Int J Arrhythm. (2019) 20:5. doi: 10.1186/s42444-019-0005-0
16. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. (2014) 33:1242–58. doi: 10.1002/sim.5984
17. Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. (2008) 168:656–64. doi: 10.1093/aje/kwn164
18. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. (2015) 34:3661–79. doi: 10.1002/sim.6607
19. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. (2009) 28:3083–107. doi: 10.1002/sim.3697
20. Lamberts M, Gislason GH, Lip GY, Lassen JF, Olesen JB, Mikkelsen AP, et al. Antiplatelet therapy for stable coronary artery disease in atrial fibrillation patients taking an oral anticoagulant: a nationwide cohort study. Circulation. (2014) 129:1577–85. doi: 10.1161/CIRCULATIONAHA.113.004834
21. Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European society of cardiology (ESC) and of the European association for cardio-thoracic surgery (EACTS). Eur Heart J. (2018) 39:213–60. doi: 10.1093/eurheartj/ehx638
22. Kwon S, Jung JH, Choi EK, Lee SW, Park J, Lee SR, et al. Impact of non-vitamin K antagonist oral anticoagulants on the change of antithrombotic regimens in patients with atrial fibrillation undergoing percutaneous coronary intervention. Korean Circ J. (2021) 51:409–22. doi: 10.4070/kcj.2020.0407
23. Park J, Jung JH, Choi EK, Lee SW, Kwon S, Lee SR, et al. Longitudinal patterns in antithrombotic therapy in patients with atrial fibrillation after percutaneous coronary intervention in the non-vitamin K oral anticoagulant era: a nationwide population-based study. J Clin Med. (2021) 10:1505. doi: 10.3390/jcm10071505
24. Alexander JH, Wojdyla D, Vora AN, Thomas L, Granger CB, Goodman SG, et al. Risk/Benefit tradeoff of antithrombotic therapy in patients with atrial fibrillation early and late after an acute coronary syndrome or percutaneous coronary intervention: insights from AUGUSTUS. Circulation. (2020) 141:1618–27. doi: 10.1161/CIRCULATIONAHA.120.046534
25. Matoba T, Yasuda S, Kaikita K, Akao M, Ako J. Rivaroxaban monotherapy in patients with atrial fibrillation after coronary stenting: insights from the AFIRE trial. JACC Cardiovasc Interv. (2021) 14:2330–40.
Keywords: atrial fibrillation, coronary artery disease, antithrombotic therapy, oral anticoagulant, antiplatelet agent
Citation: Lee S-R, Jung J-H, Choi E-K, Lee S-W, Kwon S, Park J-S, Kang J, Han K-D, Park KW, Oh S and Lip GYH (2022) Net clinical benefit of antithrombotic therapy for atrial fibrillation patients with stable coronary artery disease. Front. Cardiovasc. Med. 9:991293. doi: 10.3389/fcvm.2022.991293
Received: 11 July 2022; Accepted: 08 August 2022;
Published: 22 August 2022.
Edited by:
Wengen Zhu, The First Affiliated Hospital of Sun Yat-sen University, ChinaCopyright © 2022 Lee, Jung, Choi, Lee, Kwon, Park, Kang, Han, Park, Oh and Lip. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eue-Keun Choi, Y2hvaWVrMTdAc251LmFjLmty
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.