- 1Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, National Clinical Research Center for Cardiovascular Diseases, Beijing, China
- 2Department of Cardiology, Peking University Third Hospital, Beijing, China
Background: Multimorbidity, polypharmacy and inappropriate prescribing is common in elderly patients worldwide. We aimed to explore the current status of multimorbidity, polypharmacy and the appropriateness of pharmacological therapy among elderly patients with atrial fibrillation (AF) in China.
Materials and methods: We randomly selected 500 patients aged 65 years or older from the China AF Registry study. Multimorbidity was defined as ≥2 comorbidities and polypharmacy was defined as ≥5 long-term prescribed drugs. Appropriateness of prescribing was evaluated using the Screening Tool of Older People’s Prescriptions/Screening Tool to Alert to Right Treatment (STOPP/START) criteria version 2. Patients’ attitudes toward polypharmacy were evaluated by the Patients’ Attitudes Towards Deprescribing (PATD) questionnaire.
Results: Among the 500 patients included (mean age 75.2 ± 6.7 years, 49.0% male), 98.0% had multimorbidity and 49.4% had polypharmacy. The prevalence of potentially inappropriate medications (PIMs) and potential prescribing omissions (PPOs) was 43.6% (n = 218) and 71.6% (n = 358), respectively. Traditional Chinese medicine attributed largely to PIMs. Anticoagulants were the most common PPOs. Many clinical factors increased the risk of PIMs and PPOs. However, polypharmacy increased the risk of PIMs (OR 2.70, 95%CI 1.78–4.11; p < 0.0001), but not PPOs. In addition, 73.7% patients with polypharmacy were willing to have one or more of their medications prescribed if advised by their doctor.
Conclusion: Multimorbidity and polypharmacy were highly prevalent in elderly patients with AF in China. A high prevalence of inappropriate prescribing was also observed. Therefore, much more attention should be paid to the serious health problem in the elderly population.
Introduction
As a popular cardiovascular disease, atrial fibrillation (AF) poses significant burden to our society, and about five million new cases are diagnosed annually (1, 2). As is well known, the prevalence and incidence of AF increases significantly with age (3). Older adults often have multiple clinically significant comorbidities, for example, hypertension, hyperlipidemia, diabetes mellitus and coronary artery disease, with the need for multiple medications for symptoms and diseases control (4, 5). Therefore, polypharmacy, generally defined as administration of five or more concomitant drugs, is common in elderly patients with AF (6, 7). However, polypharmacy is associated with increased risk of inappropriate medication use, adverse drug reactions, drug-drug interactions, and poor clinical outcomes (8–10). In fact, patients’ attitudes toward their medications exert a great impact on optimizing therapy (8).
Currently, data is limited as to the current status of polypharmacy and the appropriateness of pharmacological therapy among Asian patients with AF. In this study, we aimed to (1) describe the patterns of comorbidities and medications among elderly patients with AF; (2) identify potentially inappropriate medications (PIMs), potential prescribing omissions (PPOs) and the associated factors in this population; and (3) measure patients’ attitudes toward prescribing.
Materials and methods
Study design and participants
This was a cross-sectional survey of 500 randomly selected participants of the China AF Registry (China-AF) study enrolled between 2011 and 2017. The rationale and design of the study have been previously published (11). In brief, it is an on-going, prospective, hospital-based registry study of AF patients in Beijing, China. Out-patients and in-patients from 19 tertiary and 12 non-tertiary hospitals were enrolled. All the enrolled patients had AF documented via either ECG or Holter within the past 6 months. Patients with transient and reversible AF, life expectancy less than 1 year, and those diagnosed with rheumatic heart disease were excluded from the study. All participants were managed by their local physicians or general practitioners during follow up.
Participants were eligible for inclusion in this survey if they were aged 65 years or older, and did not have moderate or severe cognitive impairment. We randomly selected eligible individuals from the pool of patients registered in the China-AF study using a computer-generated random number method.
The China-AF study was reviewed and approved by the Ethics committee of Beijing Anzhen Hospital. All patients provided their written informed consent to be followed up and contacted for future sub-studies. We obtained a separate ethic approval from the same hospital for this study. Randomly selected participants were contacted and provided additional verbal consent to be involved in this sub-study for further information collection.
Data collection and measurement
Key data elements like demographic and socioeconomic characteristics, medical conditions and medications related to AF were collected by trained cardiologists and research coordinators from medical records and interviews with patients at the time of enrollment, and updated every 6 months. Further information of general comorbidities and medication use for this analysis were collected via participant self-report during sampling investigation. Recorded medications included all over-the-counter, prescription and herbal/complementary medicines with long-term use (≥1 month). Similar to previous studies (6, 12), we defined polypharmacy as ≥5 long-term prescribed drugs and multimorbidity as 2 or more long-term health conditions (≥3 months).
Inappropriate prescribing encompasses PIMs and PPOs. We used the Screening Tool of Older People’s Prescriptions/Screening Tool to Alert to Right Treatment (STOPP/START) criteria version 2 to evaluate the appropriateness of prescribing (13, 14). The criteria, including 80 STOPP items and 34 START items, are widely used to screen PIMs and PPOs respectively (13). And the screening tool has been translated and adapted from English into several languages to facilitate the application worldwide (15, 16).
For our study population and setting, we made two modifications to the STOPP/START tool. Firstly, we added a condition for START criteria A1: Vitamin K antagonists or direct thrombin inhibitors or factor Xa inhibitors in the presence of chronic AF with high-risk of stroke. High risk patients were defined by a CHA2DS2-VASc score (one point each for hypertension, heart failure, diabetes mellitus, vascular disease, age between 65 and 74 years, female sex; two points each for prior stroke/transient ischemic attack/thromboembolism and age ≥75 years) ≥2 in male and ≥3 in female (17). Secondly, because of insufficient evidence of traditional Chinese medicine (TCM) in the management of AF, we defined the use of TCM for AF as PIMs, referred to the STOPP criteria “drugs without an evidence-based clinical indication” (18).
We used the Patients’ Attitudes Towards Deprescribing (PATD) questionnaire to measure patients’ attitudes and beliefs toward their medicines and potential deprescribing (19). And “deprescribing” is referred as appropriate cessation or reduction of medications to optimize medication regimens (20). In consideration of different acceptance of medication and surrounding beliefs between polypharmacy and non-polypharmacy individuals, the PATD questionnaire was administrated only in participants who were currently taking more than five medications. The questionnaire was originally developed and validated in Australia. In our study, it was translated into the Chinese (with permission from PATD authors) by three bilingual investigators. The translated version was then piloted in 50 older adults to ensure that the wording and content was appropriate for the population and setting.
Statistical analysis
Categorical variables were reported as frequencies and percentages. And continuous variables were expressed as mean ± standard deviation or medians with interquartile range (IQR), as appropriate. To observe the patterns of polypharmacy and PIMs/PPOs, patients were stratified by age (65–69 years, 70–74 years, 75–79 years, and ≥80 years) and number of comorbidities. The trend was tested using trend Chi-square tests.
Multivariable logistic regression was performed to identify independent risk factors associated with PIMs/PPOs. Apart from variables that were significant in the univariate analysis, we also adjusted for variables with potential influence, regardless of their statistical significance at univariate analysis. Potential confounders included age, sex, hospital level, AF type, education, health insurance coverage, cardiovascular disease, endocrine disease, previous bleeding and systemic embolism. For the first 10 questions of PATD questionnaire, participants who “agreed” or “strongly agreed” were grouped together and analyzed against those responding “unsure,” “disagree” or “strongly disagree.” All data was processed using SPSS (version 21.0; SPSS Inc., Chicago, IL, United States. P-value < 0.05 was considered statistically significant.
Results
Participant characteristics
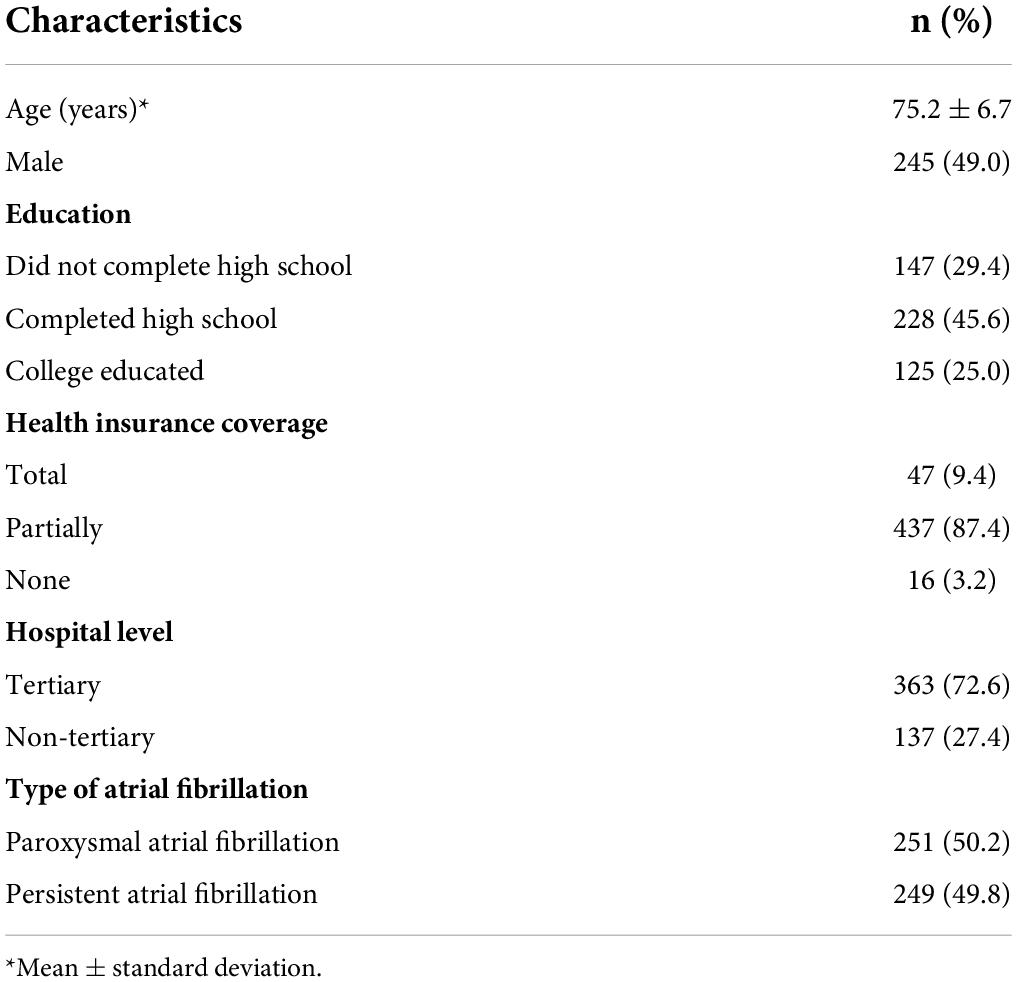
Characteristics of randomly selected participants were shown in Table 1. The mean age was (75.2 ± 6.7) years, and 49.0% of the participants were men. Among the participants, 249 (49.8%) had persistent AF and 353 (70.6%) were high school or college educated. The vast majority of participants (96.8%) were totally or partially covered by medical insurance.
Burden of comorbidities
Cardiovascular conditions accounted for the largest burden of comorbidities (86.0%), followed by endocrine conditions (60.8%) and musculoskeletal conditions (23.8%) (Figure 1). The most common cardiometabolic comorbidities were hypertension (74.8%), hyperlipidemia (43.0%), diabetes mellitus (28.8%), coronary artery disease (27.8%), congestive heart failure (17.6%), and stroke/transient ischemic attack/peripheral embolism (18.0%). Almost all participants (98.0%) had at least one comorbidity in addition to AF, 32.6% had five or more medical conditions and 1.4% had 10 or more. The median number of comorbidities was 4 (IQR 2–5).

Figure 1. Prevalence of comorbidities in participants. Autoimmune: systemic lupus erythematosus, Sjögren’s syndrome, psoriatic arthritis, rheumatoid arthritis and Takayasu’s arteritis; Bleeding: a history of bleeding with clinical symptoms significantly; Cancer: all kinds of malignant tumors; Cardiovascular: atherosclerosis, arrhythmia other than atrial fibrillation, coronary artery disease, congestive heart failure, hypertension, cardiomyopathy, peripheral arterial disease, deep vein thrombosis; Endocrine: diabetes mellitus, hyperlipidemia, hyperuricemia, hyperhomocysteinemia, gout and adrenal disease; Gastrointestinal: chronic gastritis, ulcer disease, gastroesophageal reflux disease, Crohn’s disease, ulcerative colitis, hepatobiliary calculus, liver dysfunction and cirrhosis; Musculoskeletal: spondyloarthritis, fibromyalgia, osteoarthritis, osteoporosis and osteopenia; Nervous system: dementia, Parkinson’s disease, Alzheimer’s disease, epilepsy, vertigo, migraine and peripheral neuropathy; Others: anemia, implantation of cardiac implantable electronic devices, chronic pain, chronic infectious disease and gynecological disease; Mental health condition: depression, anxiety, phobias, bipolar disorder and sleep disorder; Respiratory: asthma, chronic bronchitis, emphysema, chronic obstructive pulmonary disease chronic rhinitis, allergic rhinitis, obstructive sleep apnea and pulmonary embolism; Embolic event: a history of stroke, transient ischemic attack or systemic embolism; Thyroid: hyperthyroidism and hypothyroidism; Urologic: chronic kidney disease, urolithiasis and benign prostatic hyperplasia.
Polypharmacy
The median number of concomitant medication types and tablets/capsules taken daily was 4 (IQR, 3–6) and 8 (IQR, 4–13). About half of the patients (49.4%) received five or more different types of medications (polypharmacy). The number of medications increased significantly with age (p < 0.05) and comorbidities (p < 0.001). Polypharmacy was present in 38.8, 44.1, 56.7, and 57% of participants aged 65–69, 70–74, 75–79 years, and aged ≥80 years respectively, and from 9.1 to 48.0%, 66.1 and 80.7% in patients with 0–1, 3, 5, and ≥7 comorbidities (Figure 2).
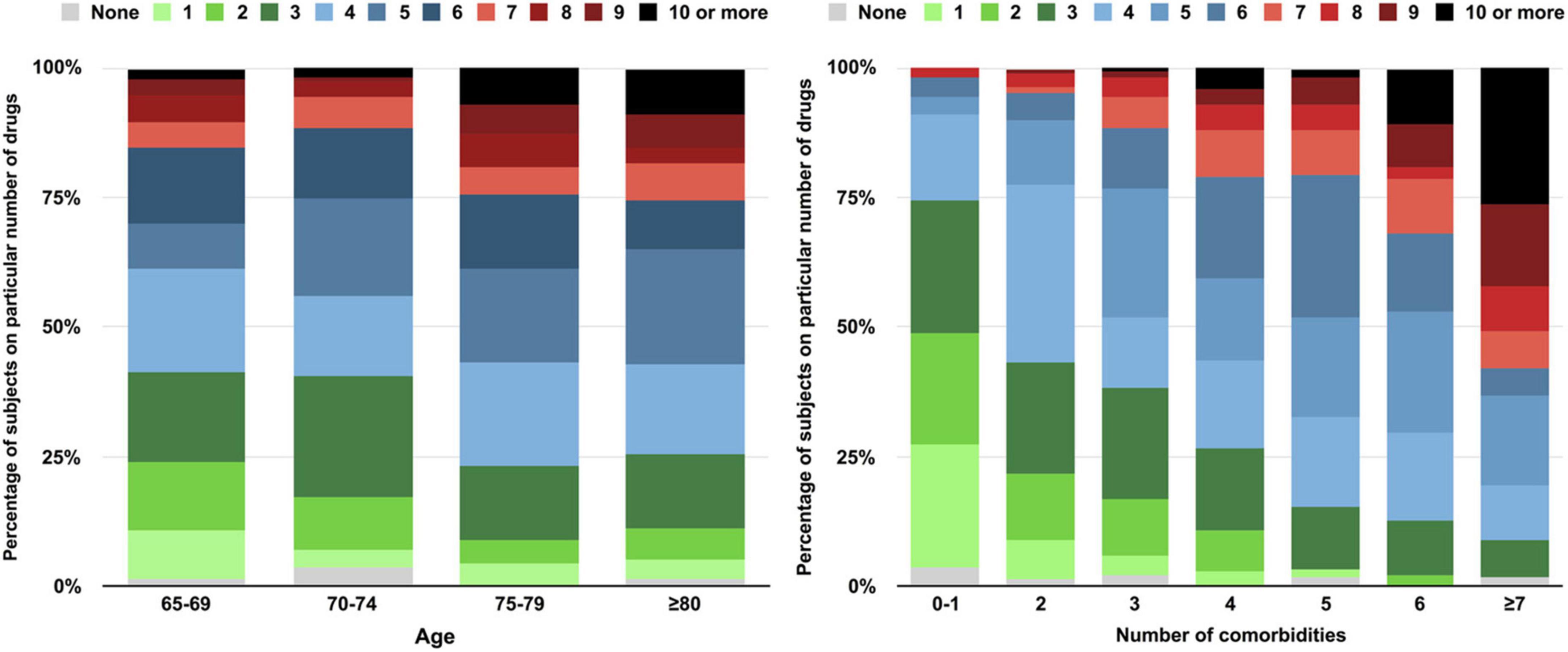
Figure 2. Number of medications taken by participants stratified by age and number of comorbidities.
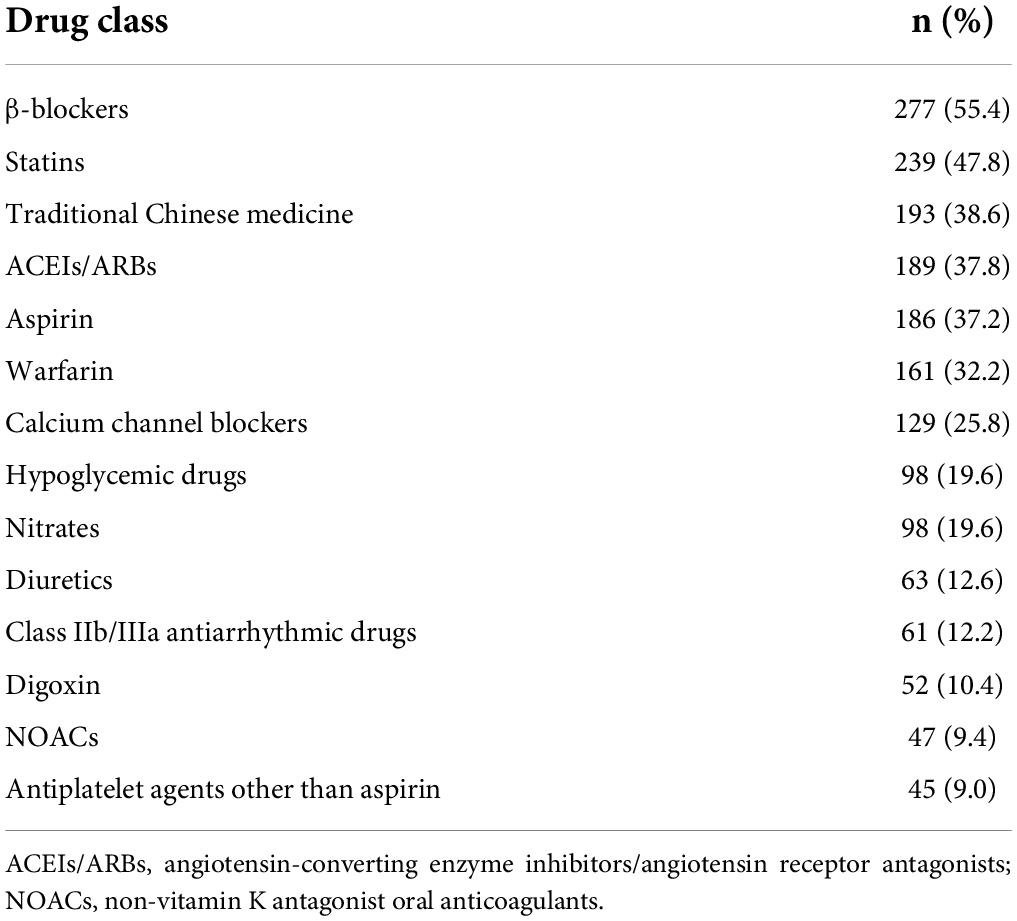
The most common used drugs were β-blockers (55.4%), followed by statins (47.8%) and angiotensin-converting enzyme inhibitors/angiotensin receptor antagonists (ACEIs/ARBs, 37.8%). Oral anticoagulant agents were used in 41.6% of participants (32.2% on warfarin and 9.4% on non-vitamin K antagonist oral anticoagulants). More than a third of participants were taking TCM which was prescribed for symptom relief or an alternative for anticoagulants (Table 2).
Inappropriate prescribing (potentially inappropriate medications and potential prescribing omissions)
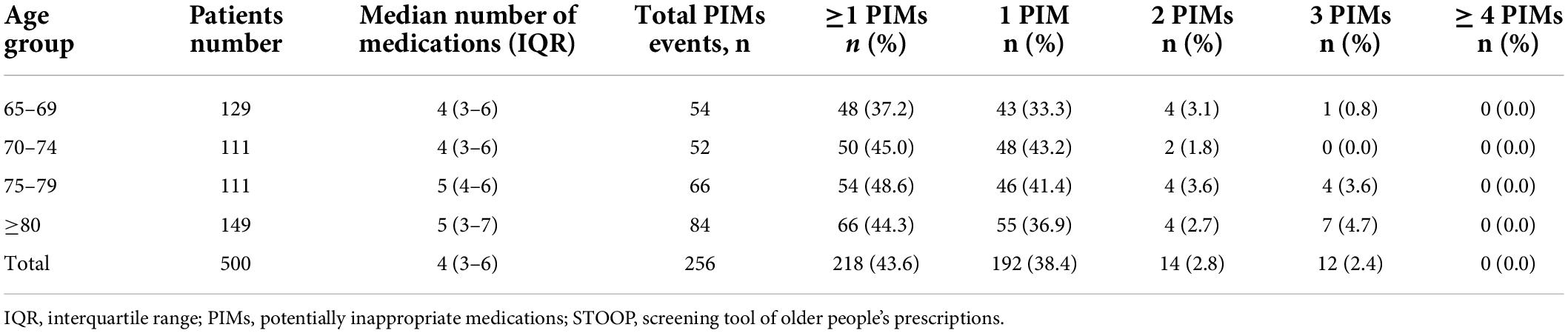
According to the STOPP criteria, a total of 256 PIMs events were identified, and PIMs use occurred in 43.6% of participants. Moreover, 38.4, 2.8, and 2.4% were prescribed one, two, and three PIMs, respectively. No patient was prescribed four or more PIMs (Table 3). The most frequent PIM used was TCM, and the rate was as high as 38.6% in all enrolled patients, which also account for 75.3% of all PIMs events (Supplementary Table 1).
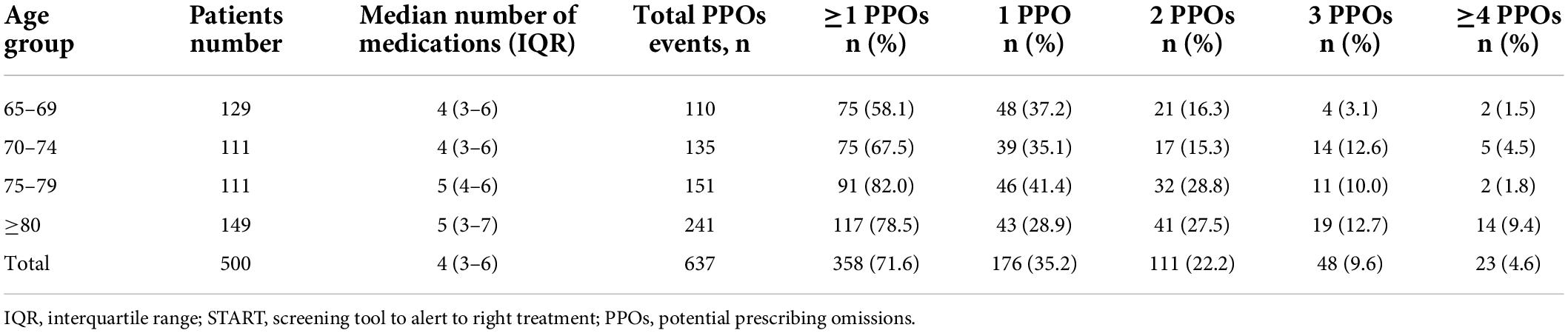
According to the START criteria, a total of 637 PPOs events were identified, and the prevalence of PPOs was 71.6%. One, two, three, and four or more PPOs were identified in 35.2, 22.2, 9.6, and 4.6% of participants, respectively (Table 4). Over half (58.1%) of high-risk participants did not receive adequate anticoagulant therapy. Of the 197 participants with systolic heart failure, 124 (62.9%) were not taking ACEIs/ARBs. Similarly, statins were not prescribed in 69 out of 189 (36.5%) participants with an indication for lipid-lowering therapy. And β-blockers were also underused (Supplementary Table 2).
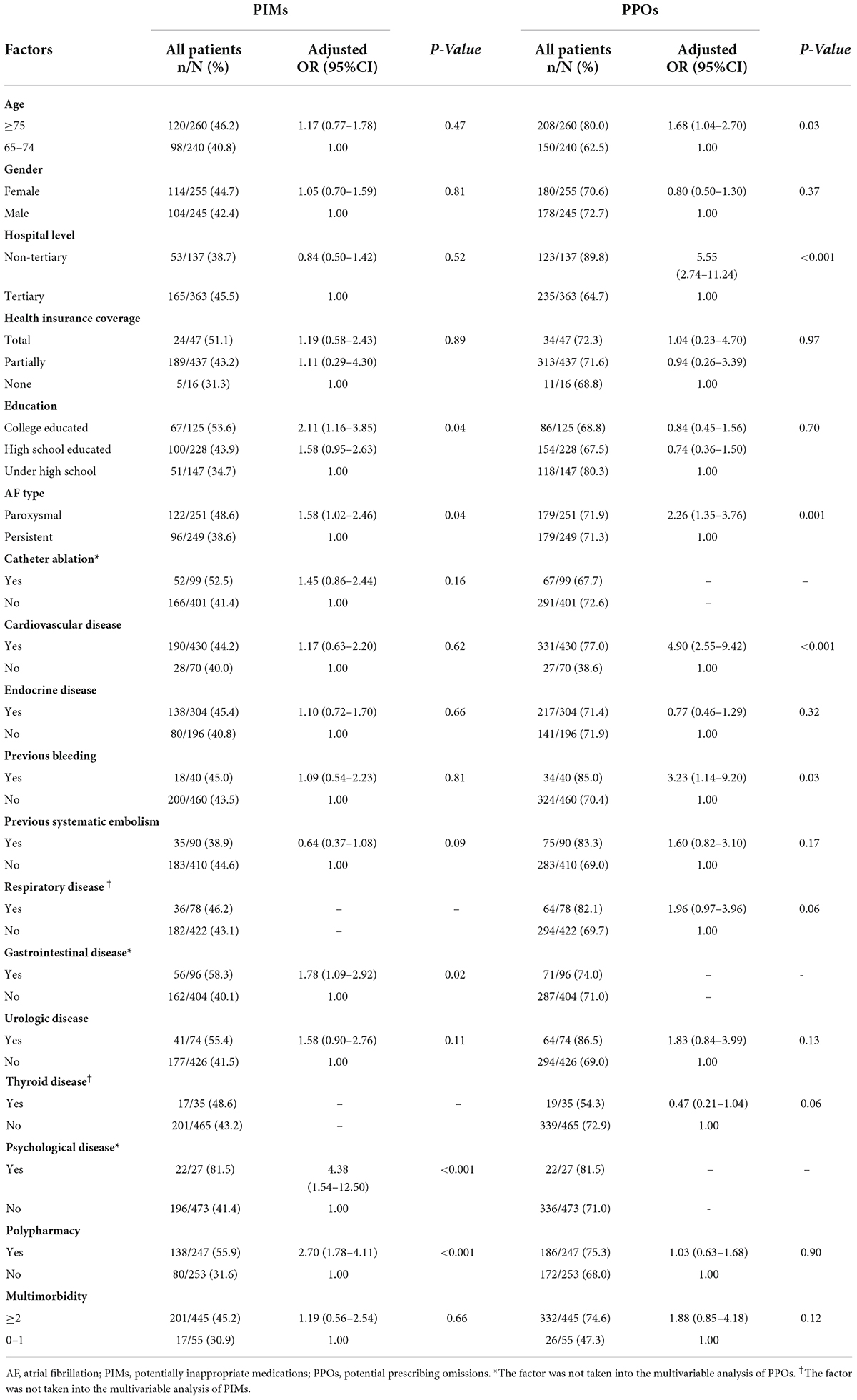
Factors associated with potentially inappropriate medications and potential prescribing omissions
After adjustment for potential confounders, the following factors were found to be independently associated with PIMs: education level [college education: odds ratio (OR) 2.11, 95% confidence interval (CI) 1.16–3.85; p = 0.04], paroxysmal AF (OR 1.58, 95%CI 1.02–2.46; p = 0.04), gastrointestinal disease (OR 1.78, 95%CI 1.09–2.92; p = 0.02), mental health condition (OR 4.38, 95%CI 1.54–12.50; p < 0.001), and polypharmacy (OR 2.70, 95%CI 1.78–4.11; p < 0.001) (Table 5).
Independent predictors of PPOs were age over 75 years (OR 1.68, 95%CI 1.04–2.70; p = 0.03), non-tertiary hospital management (OR 5.55, 95%CI 2.74–11.24, p < 0.001), paroxysmal AF (OR 2.26, 95%CI 1.35–3.76, p = 0.001), history of cardiovascular diseases (OR 4.90, 95%CI 2.55–9.42; p < 0.0001), and history of bleeding (OR 3.23, 95%CI 1.14–9.20; p = 0.03). No significant association was observed between polypharmacy and PPOs (OR 1.03, 95%CI 0.63–1.68; p = 0.90) (Table 5).
Attitudes toward deprescribing
The PATD questionnaire was administrated to 247 participants with polypharmacy, and the response was presented in Figure 3. 61.0% of participants agreed that they were taking a large number of medications (Question 1) and 50.6% reported to be uncomfortable with current number of medications (Question 2). Approximately three quarters (73.7%) of participants agreed or strongly agreed that they would be willing to have one or more of their medications prescribed if advised by their doctor (Question 4). Experiencing a side-effect and financial burden as a consideration for deprescribing were reported by 25.5 and 32.0% of participants (Question 9 and 10). At the meantime, most participants (76.1%) believed the medications they were taking were necessary (Question 3) and 42.5% were willing to accept taking more medications for their health conditions (Question 7). The maximum ideal number of medications was reported in 30.8% for 8 tablets/capsules taken daily, 25.6% for 12 and 21.1% for 16 (Question 13) (Supplementary Table 3).
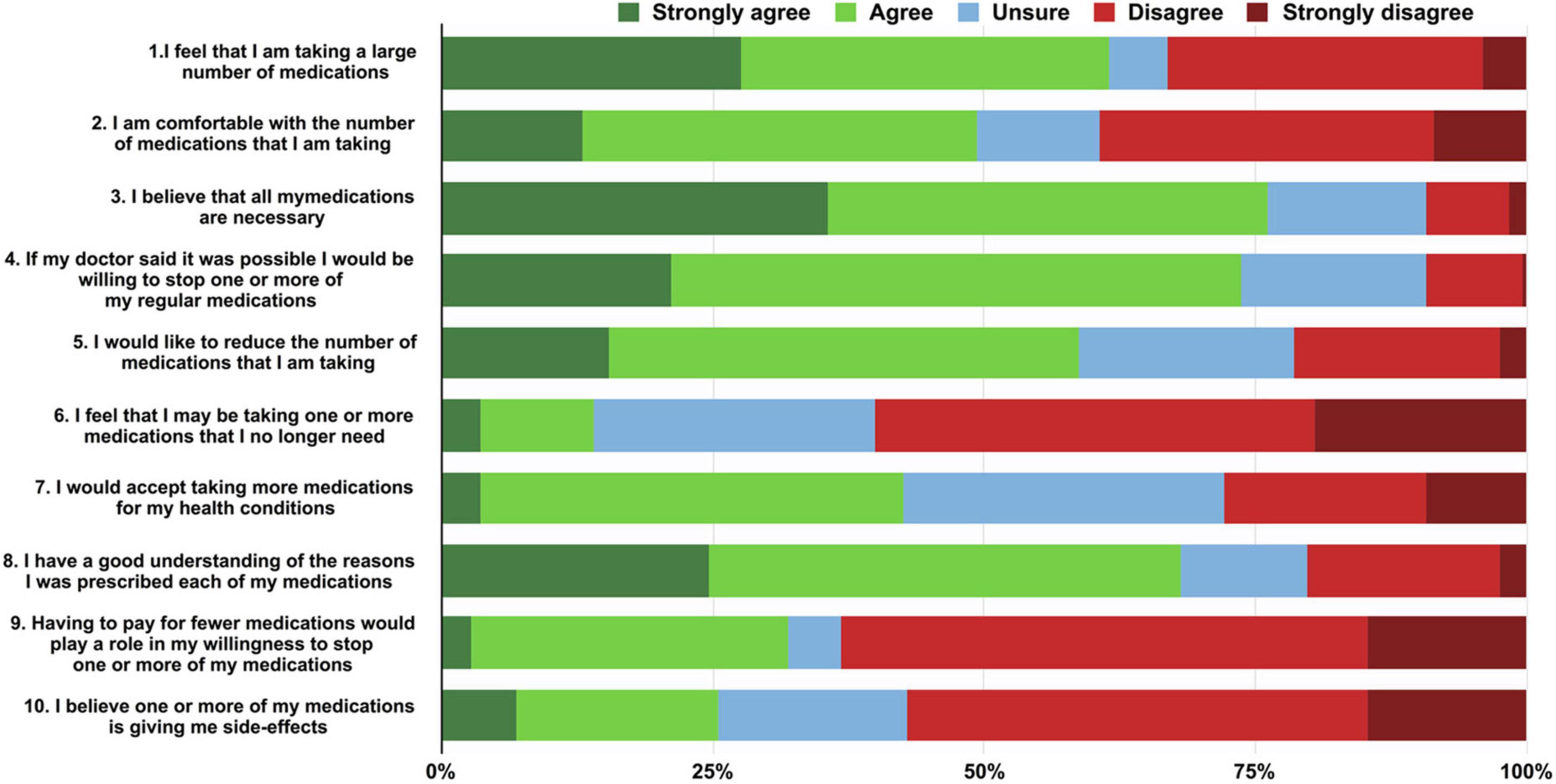
Figure 3. Participants responses to the PATD (patients’ attitudes toward deprescribing) questionnaire (questions 1–10).
Discussion
In this study, we found that multimorbidity was present in almost all older adults with AF. Nearly half of the participants had polypharmacy and both over- and under-treatment were identified in this population. More than half patients did not receive proper anticoagulant therapy. ACEIs/ARBs, β-blockers, and statins were also underused according to the STOPP/START criteria. However, agents without sufficient clinical indications were commonly used. About three quarters of participants with polypharmacy expressed the willingness to stop one or more medications under the guidance of the clinician.
We confirmed multimorbidity was common in elderly AF patients, and the rate was as high as 98.0%. Indeed, multimorbidity prevalence in AF was ranged from 69.5 to 98%, for different study setting and population (21–23). A Swedish study of 272186 AF patients reported 69.5% prevalence of at least one other comorbidity (21). A study in Belgium reported that 92% of patients with AF had 3 or more comorbidities (22). A study in the United States using the data from National Health and Wellness survey (NHWS) found that 98% of participants with AF had at least one additional comorbidity (23). Generally, the number of comorbidities increases with age in the older population (24). And in our study the mean age of the AF patients was 75.2 years old.
Moreover, we identified the general comorbidity pattern and drew a relatively comprehensive picture of the total disease burden in the elderly AF patients in China, which would help to improve treatment and health outcomes. The incidence of cardiovascular diseases other than AF was 86.0%, which exerted the biggest comorbidity burden in our population, and hypertension was the most prevalent comorbidity. In fact, hypertension is closely associated with the development of AF (25). Unlike with studies from western countries (23, 26), we found that the incidence of non-cardiometabolic conditions was low in our study.
Polypharmacy is becoming increasingly common in clinical practice due to the aging society and the high burden of comorbidities (27, 28). Indeed, multimorbidity acts as a driver of polypharmacy. In patients with high morbidity, the proportion of polypharmacy is also high (29). The prevalence of polypharmacy was 49.4% in our study. Previous studies have reported rates of polypharmacy in 40–77% of patients with AF, with varying prescription patterns and inclusion and exclusion criteria (6, 12, 30). The potential harms of polypharmacy have been widely reported, including inappropriate prescribing, increased risk of adverse drug events and poor clinical outcomes (8–10, 31). Unfortunately, polypharmacy may bring unique risk in older adults with AF. Several studies found that polypharmacy was an independent risk factor for bleeding and thromboembolic events in patients with AF (6, 12).
Inappropriate prescribing, including PIMs and PPOs, was also prevalent in our study population. Almost half of our enrolled participants were taking at least one PIMs, such as TCM. In fact, some TCMs were reported to have antithrombotic effect and interact with anticoagulant agents, for example, danshen (Salvia miltiorrhiza), danshen (Salvia miltiorrhiza), Asian ginseng (Panax ginseng) and so on (18, 32). Concomitant use of TCM would increase the risk of bleeding. Thus, clinicians may need to specifically ask about TCM use before prescribing anticoagulants.
Currently, anticoagulant therapy is recommended among AF patients with high or moderate risk of stroke (17). In this study, 90.8% of participants had an indication for anticoagulant therapy, but only 41.9% were prescribed these medications (35.5% on warfarin and 6.4% on NOACs). This proportion was similar to the number we observed in our previous China-AF sub-study (33). Although great improvement in anticoagulant usage has been achieved in recent years, the gap is still large between clinical practice and guideline recommended therapy in China (33, 34). As stated in our previous study (33), There are some reasons for the underuse of anticoagulants. First, the high risk of bleeding restricts use of anticoagulants in the elderly. Second, patient education and monitoring are inadequate, which impairs the clinicians from prescribing anticoagulants and patients to adhere to therapy. Compared with warfarin, the rate of NOACs was much lower, and the high cost of NOACs may be the reason, because NOACs are unaffordable for the vast majority of patients in China. Meanwhile, ACEIs/ARBs, β-blockers and statins were the most common PPOs in this study, which was consistent with prior data (34). It indicated that the importance of cardiovascular risk factor modification is often neglected. Thus, integrated care is in urgent need in the management of AF patients.
We identified that polypharmacy as well as several medical conditions, such as gastrointestinal disease and mental health condition, increased the risk of PIMs. This may explain the common overprescribing of drugs in specific conditions, such as long-term benzodiazepine use. On the other hand, it also indicated that increased complexity of the disease can lead to inappropriate prescribing (35). Furthermore, PIMs were more common in patients with high education level. The possible reason may be that patients with high education level always have good economic conditions, and they prefer to take TCM as complementary and alternative medicine. In addition, we observed that polypharmacy could not decrease the risk of PPOs. By reviewing the most commonly prescribed PIMs/PPOs, we assumed that the occurrence of PPOs (including anticoagulants, ACEIs/ARBs, etc.) might result in worse clinical outcomes than PIMs (like TCM) in older AF patients. Therefore, an evidence-based drug therapy but within limited number of concomitant medications is vital for this population. Single-pill combination may be a good solution for all the questions.
Inappropriate medication use in older patients is common, which indicates deprescribing is not happening as often as it should. Approximately three quarters of our participants with polypharmacy were willing to have one or more of their medications prescribed if their doctor said it was possible. In fact, deprescribing involves an implicit partnership between the doctor and the patient (36). Not only in China, older individuals in the other countries are also eager to undertake deprescribing, especially when they have a large number of medications, experience side effects or feel some medications are unnecessary (36–38). A meta-analysis of 40 studies and 10,816 participants found that the proportion of patients who agreed or strongly agreed with deprescribing was as high as 84% (39).
There are many factors influencing the patients’ attitudes toward medications, such as insurance coverage status and physician trust (40). Our data suggested that patients’ attitudes and beliefs were important factors in prescribing and deprescribing. Given the complicated nature and associated risks of polypharmacy, it is important to optimize the medication regimen in older adults with AF. In particular, this is a population with high prevalence of cognitive decline (41), which can impact self-medication management. Good communication about the reasons for prescribing and/or deprescribing may help facilitate shared-decision making with older adults and their caregivers. Compared with taking multiple pills, polypill-based regimens have emerged as a promising strategy to increase patient adherence and reduce burden (42). New technologies such as mobile applications may also facilitate optimizing medications (43).
Limitations
There are some limitations of our study. First, the sample population was recruited from hospitals in Beijing, and the majority of them were from high-volume tertiary medical centers. This may produce biased participant selection, for patients who attend tertiary hospitals usually have a high social economic status and degree of education. Second, our data was patient self-reported, and the estimate of polypharmacy was not validated. Third, the STOPP/START criteria version 2 was published in 2014, and due to the expanding therapeutics evidence base, it could not include every detail on potentially inappropriate prescribing. Finally, the PATD questionnaire was originally designed and validated in Australia, while we conducted piloting in our population, we did not conduct a formal validation process.
Conclusion
Multimorbidity and polypharmacy were highly prevalent in elderly patients with AF in China. Inappropriate prescribing, including over- and under-treatment, was common in this population. Moreover, many patients expressed their willingness to deprescribing. Thus, drug regimens should be adjusted timely, to satisfy the need of the patients. In the future, much more attention should be paid to the elderly AF population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics committee of Beijing Anzhen Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Funding
This work was supported by grant from the National Natural Science Foundation of China (81700299 to XG).
Acknowledgments
We express our sincere appreciation to all of the hospitals involved in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a shared parent affiliation with several of the authors, XG, XD, CJ, SL, RT, CS, RY, DL, JD, and CM at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.988799/full#supplementary-material
References
1. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC) developed with the special contribution of the European heart rhythm association (EHRA) of the ESC. Eur Heart J. (2021) 42:373.
2. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr., et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on practice guidelines and the heart rhythm society. Circulation. (2014) 130:e199–267.
3. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the an ticoagulation and risk factors in atrial fibrillation (ATRIA) study. JAMA. (2001) 285:2370–5.
4. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43.
5. Lip GYH, Tran G, Genaidy A, Marroquin P, Estes C, Harrelll T. Prevalence/incidence of atrial fibrillation based on integrated medical/pharmacy claims, and association with co-morbidity profiles/multi-morbidity in a large US adult cohort. Int J Clin Pract. (2021) 75:e14042.
6. Piccini JP, Hellkamp AS, Washam JB, Becker RC, Breithardt G, Berkowitz SD, et al. Polypharmacy and the efficacy and safety of rivaroxaban versus warfarin in the prevention of stroke in patients with nonvalvular atrial fibrillation. Circulation. (2016) 133:352–60.
7. Kotalczyk A, Guo Y, Wang Y, Lip GYH. On behalf of the chi ori. impact of multimorbidity and polypharmacy on clinical outcomes of elderly Chinese patients with atrial fibrillation. J Clin Med. (2022) 11:1370.
8. Scott IA, Hilmer SN, Reeve E, Potter K, Le Couteur D, Rigby D, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. (2015) 175:827–34.
9. Oktora MP, Alfian SD, Bos HJ, Schuiling-Veninga CCM, Taxis K. Trends in polypharmacy and potentially inappropriate medication (PIM) in older and middle-aged people treated for diabetes. Br J Clin Pharmacol. (2021) 87:2807–17.
10. Chae HW, Kim Y, Suh Y, Lee J, Lee E, Lee E, et al. Prevalence of potentially inappropriate medications based on the STOPP frail criteria in frail older patients with limited life expectancy: a cross-sectional study. BMC Geriatr. (2022) 22:367. doi: 10.1186/s12877-022-03067-7
11. Du X, Ma C, Wu J, Li S, Ning M, Tang R, et al. Rationale and design of the Chinese atrial fibrillation registry study. BMC Cardiovasc Disord. (2016) 16:130. doi: 10.1186/s12872-016-0308-1
12. Jaspers Focks J, Brouwer MA, Wojdyla DM, Thomas L, Lopes RD, Washam JB, et al. Polypharmacy and effects of apixaban versus warfarin in patients with atrial fibrillation: post hoc analysis of the ARISTOTLE trial. BMJ. (2016) 353:i2868.
13. O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. (2015) 44:213–8.
14. Barenholtz Levy H, Marcus EL. Potentially inappropriate medications in older adults: why the revised criteria matter. Ann Pharmacother. (2016) 50:599–603.
15. Delgado Silveira E, Montero Errasquin B, Munoz Garcia M, Velez-Diaz-Pallares M, Lozano Montoya I, Sanchez-Castellano C, et al. [Improving drug prescribing in the elderly: a new edition of STOPP/START criteria]. Rev Esp Geriatr Gerontol. (2015) 50:89–96.
16. Monteiro L, Monteiro-Soares M, Matos C, Ribeiro-Vaz I, Teixeira A, Martins C. Inappropriate prescriptions in older people-translation and adaptation to portuguese of the STOPP/START screening tool. Int J Environ Res Public Health. (2022) 19:6896.
17. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. (2010) 137:263–72.
18. Tsai HH, Lin HW, Lu YH, Chen YL, Mahady GB. A review of potential harmful interactions between anticoagulant/antiplatelet agents and Chinese herbal medicines. PLoS One. (2013) 8:e64255. doi: 10.1371/journal.pone.0064255
19. Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Development and validation of the patients’ attitudes towards deprescribing (PATD) questionnaire. Int J Clin Pharm. (2013) 35:51–6.
21. Andersson T, Magnuson A, Bryngelsson IL, Frøbert O, Henriksson KM, Edvardsson N, et al. All-cause mortality in 272,186 patients hospitalized with incident atrial fibrillation 1995-2008: a Swedish nationwide long-term case-control study. Eur Heart J. (2013) 34:1061–7.
22. Vanbeselaere V, Truyers C, Elli S, Buntinx F, De Witte H, Degryse J, et al. Association between atrial fibrillation, anticoagulation, risk of cerebrovascular events and multimorbidity in general practice: a registry-based study. BMC Cardiovasc Disord. (2016) 16:61. doi: 10.1186/s12872-016-0235-1
23. LaMori JC, Mody SH, Gross HJ, daCosta DiBonaventura M, Patel AA, Schein JR, et al. Burden of comorbidities among patients with atrial fibrillation. Ther Adv Cardiovasc Dis. (2013) 7:53–62.
24. Balakrishnan S, Karmacharya I, Ghimire S, Mistry SK, Singh DR, Yadav OP, et al. Prevalence of multimorbidity and its correlates among older adults in Eastern Nepal. BMC Geriatr. (2022) 22:425. doi: 10.1186/s12877-022-03115-2
25. van Mourik MJW, Artola Arita V, Lyon A, Lumens J, De With RR, van Melle JP, et al. Association between comorbidities and left and right atrial dysfunction in patients with paroxysmal atrial fibrillation: analysis of AF-RISK. Int J Cardiol. (2022) 360:29–35.
26. Jani BD, Nicholl BI, McQueenie R, Connelly DT, Hanlon P, Gallacher KI, et al. Multimorbidity and co-morbidity in atrial fibrillation and effects on survival: findings from UK Biobank cohort. Europace. (2018) 20:f329–36.
27. Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. (2021) 12:443–52.
28. Goldsmith R, Dichtiar R, Shimony T, Nitsan L, Axelrod R, Laxer-Asael I, et al. Comparisons in polypharmacy over a decade in community-dwelling older adults-findings from Israel national health and nutrition surveys. BMC Geriatr. (2022) 22:502. doi: 10.1186/s12877-022-03171-8
29. Wang J, Yang YM, Zhu J, Zhang H, Shao XH. Multimorbidity and polypharmacy in chinese emergency department patients with atrial fibrillation and impacts on clinical outcomes. Front Cardiovasc Med. (2022) 9:806234. doi: 10.3389/fcvm.2022.806234
30. Proietti M, Raparelli V, Olshansky B, Lip GY. Polypharmacy and major adverse events in atrial fibrillation: observations from the AFFIRM trial. Clin Res Cardiol. (2016) 105:412–20.
31. Fleg JL, Aronow WS, Frishman WH. Cardiovascular drug therapy in the elderly: benefits and challenges. Nat Rev Cardiol. (2011) 8:13–28.
32. Agbabiaka TB, Spencer NH, Khanom S, Goodman C. Prevalence of drug-herb and drug-supplement interactions in older adults: a cross-sectional survey. Br J Gen Pract. (2018) 68:e711–7.
33. Chang SS, Dong JZ, Ma CS, Du X, Wu JH, Tang RB, et al. Current status and time trends of oral anticoagulation use among chinese patients with nonvalvular atrial fibrillation: the Chinese atrial fibrillation registry study. Stroke. (2016) 47:1803–10.
34. Oldgren J, Healey JS, Ezekowitz M, Commerford P, Avezum A, Pais P, et al. Variations in cause and management of atrial fibrillation in a prospective registry of 15,400 emergency department patients in 46 countries: the RE-LY atrial fibrillation registry. Circulation. (2014) 129:1568–76.
35. Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995-2010. BMC Med. (2015) 13:74. doi: 10.1186/s12916-015-0322-7
36. Sirois C, Ouellet N, Reeve E. Community-dwelling older people’s attitudes towards deprescribing in Canada. Res Social Adm Pharm. (2017) 13:864–70.
37. Kua KP, Saw PS, Lee SWH. Attitudes towards deprescribing among multi-ethnic community-dwelling older patients and caregivers in Malaysia: a cross-sectional questionnaire study. Int J Clin Pharm. (2019) 41:793–803.
38. Buzancic I, Dragovic P, Pejakovic TI, Markulin L, Ortner-Hadziabdic M. Exploring patients’ attitudes toward deprescribing and their perception of pharmacist involvement in a european country: a cross-sectional study. Patient Prefer Adherence. (2021) 15:2197–208.
39. Weir KR, Ailabouni NJ, Schneider CR, Hilmer SN, Reeve E. Consumer attitudes towards deprescribing: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. (2022) 77:1020–34.
40. Reeve E, Wiese MD, Hendrix I, Roberts MS, Shakib S. People’s attitudes, beliefs, and experiences regarding polypharmacy and willingness to deprescribe. J Am Geriatr Soc. (2013) 61:1508–14.
41. Singh-Manoux A, Fayosse A, Sabia S, Canonico M, Bobak M, Elbaz A, et al. Atrial fibrillation as a risk factor for cognitive decline and dementia. Eur Heart J. (2017) 38:2612–8.
42. Mohamed MG, Osman M, Kheiri B, Saleem M, Lacasse A, Alkhouli M. Polypill for cardiovascular disease prevention: Systematic review and meta-analysis of randomized controlled trials. Int J Cardiol. (2022) 360:91–8.
Keywords: atrial fibrillation, elderly patients, multimorbidity, polypharmacy, inappropriate prescribing
Citation: Guo X, Li M, Du X, Jiang C, Li S, Tang R, Sang C, Yu R, Long D, Dong J and Ma C (2022) Multimorbidity, polypharmacy and inappropriate prescribing in elderly patients with atrial fibrillation: A report from the China Atrial Fibrillation Registry Study. Front. Cardiovasc. Med. 9:988799. doi: 10.3389/fcvm.2022.988799
Received: 07 July 2022; Accepted: 08 August 2022;
Published: 06 September 2022.
Edited by:
Yankun Yang, Capital Medical University, ChinaReviewed by:
Lingmin Wu, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaZhe Xu, Fujian Medical University Union Hospital, China
Copyright © 2022 Guo, Li, Du, Jiang, Li, Tang, Sang, Yu, Long, Dong and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changsheng Ma, Y2hzaG1hQHZpcC5zaW5hLmNvbQ==
†These authors have contributed equally to this work
 Xueyuan Guo
Xueyuan Guo Mengmeng Li1,2†
Mengmeng Li1,2† Ribo Tang
Ribo Tang Caihua Sang
Caihua Sang Deyong Long
Deyong Long Jianzeng Dong
Jianzeng Dong Changsheng Ma
Changsheng Ma