
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cardiovasc. Med., 04 January 2023
Sec. Cardiovascular Imaging
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.984326
This article is part of the Research TopicWomen in Cardiovascular ImagingView all 16 articles
 Lilia M. Sierra-Galan1*
Lilia M. Sierra-Galan1* Niti R. Aggarwal2
Niti R. Aggarwal2 Jadranka Stojanovska3
Jadranka Stojanovska3 Subha V. Raman4
Subha V. Raman4 Yuchi Han5
Yuchi Han5 Vanessa M. Ferreira6
Vanessa M. Ferreira6 Katharine Thomas6
Katharine Thomas6 Nicole Seiberlich7
Nicole Seiberlich7 Purvi Parwani8
Purvi Parwani8 Chiara Bucciarelli-Ducci9
Chiara Bucciarelli-Ducci9 Lauren A. Baldassarre10
Lauren A. Baldassarre10 Sophie Mavrogeni11
Sophie Mavrogeni11 Karen Ordovas12
Karen Ordovas12 Jeanette Schulz-Menger13
Jeanette Schulz-Menger13 W. Patricia Bandettini14*
W. Patricia Bandettini14*Women’s engagement in medicine, and more specifically cardiovascular imaging and cardiovascular MRI (CMR), has undergone a slow evolution over the past several decades. As a result, an increasing number of women have joined the cardiovascular imaging community to contribute their expertise. This collaborative work summarizes the barriers that women in cardiovascular imaging have overcome over the past several years, the positive interventions that have been implemented to better support women in the field of CMR, and the challenges that still remain, with a special emphasis on women physicians.
Women have long struggled for equal footing in many aspects of society. While, in recent years, their unique value in some areas traditionally dominated by men has become better understood, women still work to achieve recognition in many professional fields. Expressly, women in medicine often have not been granted the privileges that are afforded to men with the same degrees and training. In cardiovascular imaging and cardiovascular MRI (CMR), in particular, the challenges faced by women make it difficult for them to enter the field and reduce their likelihood of staying.
The first barrier to entry in the field of cardiovascular imaging is the long and challenging training, consisting of medical school and residency (in either diagnostic radiology or internal medicine), followed by cardiology and dedicated cardiac imaging or cardiovascular fellowships. Those who choose to engage in cardiovascular imaging research, either as a scientist pursuing a Ph.D. or a physician-scientist, must take on additional training. This lengthy process may cause women to hesitate when making the decision to pursue a career in cardiovascular imaging. The long career process is a gender-neutral consideration; however, in parallel, in the current era, women in some societies bear more responsibility for the family. As such, they must be capable of contributing more substantially to the support of their families and the inevitable family circumstances, including birth, death, divorce, relocation, and consequences of financial troubles. The long educational process before becoming fully-trained in cardiovascular imaging, along with the gender pay gap, may contribute to these obstacles.
Once this training is completed, women may still face challenges in clinical cardiovascular imaging practice. In many countries, cardiology and radiology have traditionally been viewed as “male” specialties, making it difficult for women to excel (if they even select these specialties in the first place). Among CMR experts, more men hold tenured academic positions than women (68% vs. 32%).1 As a result, women are outnumbered by men in the fields of cardiology and radiology (1). Although institutions may seemingly accept the female presence in their respective departments, they may still underappreciate the contributions of women colleagues and are more likely to appoint men to leadership positions.
These lower numbers of women physicians in fields such as cardiovascular imaging may reduce the quality of care offered to patients, as the presence of women in multi-disciplinary teams has resulted in improved outcomes measured by lower patients’ 30-day mortality and readmission rates (2, 3). Modern medical practice requires many individuals with different areas of expertise, and the advanced imager is an essential part of the team taking care of cardiovascular patients. Advanced imaging using approaches including cardiovascular magnetic resonance (CMR) has revolutionized the field of cardiology with high spatial resolution and three-dimensional capabilities. CMR is now indicated for various cardiovascular conditions, with extensive evidence available to showcase its impact on overall outcomes and clinical practice (4, 5). Unfortunately, as described above, women in the field of CMR—among other subspecialties—face the challenge of balancing personal life, family responsibilities, and career demands. Specialized training inherent to CMR adds to this challenge. Unfortunately, only a few dedicated centers provide advanced CMR training, the competition is hard, and a strong biographic sketch is necessary to be accepted.
This manuscript is meant to provide an understanding of the current state of women in cardiovascular imaging and CMR and to suggest some practical changes that could be enacted to help recruit and retain women in CMR. To this end, the historical role of women in cardiovascular imaging, the challenges women face in CMR, the current state of the field by the numbers, the importance of the presence of women in CMR, and the potential solutions to these challenges are discussed. While the importance of women in all aspects of CMR is acknowledged, this work is meant primarily to highlight those challenges faced by female cardiologists and radiologists in the field of cardiovascular imaging.
Women have played an essential role in the development of medical imaging. A prime example is Marie Curie, an early pioneer of “in-the-field” medical imaging. While best known for her research on radioactivity, Professor Curie was pivotal in implementing mobile x-ray units during World War I (6).
Compared to x-ray, cardiovascular magnetic resonance (CMR) is a relatively recent addition to the medical imaging toolbox, with its origins in the early 1980s. However, women were among the early developers of this emerging technology. For example, Dr. Joanne Ingwall was instrumental in promoting cardiovascular spectroscopy (7) and served as the first female president of the International Society for Magnetic Resonance in Medicine (ISMRM). In the 1990s, Daisy Chien, Ph.D., developed MRI pulse sequences for cardiovascular imaging, including magnetic resonance angiography, spin-echo T2 MRI for the detection of acute myocardial infarction, perfusion imaging, and left ventricular segmental TrueFISP imaging (8–11). Her scientific status led to a position on the ISMRM Board of Trustees. Katherine Wu, M.D. demonstrated microvascular obstruction as a predictor of adverse outcomes. Her work using CMR to predict sudden cardiac death outcomes helped push CMR into mainstream clinical use (9). Similarly, Brigitte Poncelet-Belliveau, Ph.D., developed a broad spectrum of CMR sequences and applications, including blood oxygen level-dependent contrast (BOLD), echo planar imaging, myocardial perfusion, and T2-TrueFISP (12–14). In the 2000s, Dr. Vivian Lee, a radiologist and ISMRM Gold Medal Winner, developed the MRI research program at New York University. She worked to improve methods of assessing vascular disease with 3D gadolinium MRA and non-contrast methods. She also developed CMR viability imaging (15–17) and served on the Board of Trustees and later as President of the ISMRM.
By the early-to-mid 2000s, an increasing number of women from many fields (physicists, cardiologists, radiologists, and technologists) had entered the field of CMR. Critical work in translating the CMR methods into cardiovascular applications was carried out by key individuals, such as Jeanette Schulz-Menger, M.D. with her work in inflammatory disease and myocarditis (18–20)—and the first female president of the Society for Cardiovascular Magnetic Resonance (SCMR), as well as a member of the ISMRM Board of Trustees, Subha Raman, M.D., the second female president of the SCMR, with her innovative treadmill CMR research (21), Chiara Bucciarelli-Ducci, M.D.’s—the second chief executive officer (CEO) and first female CEO of the SCMR—contributions to better understanding myocardial infarction in the setting of non-obstructive coronary arteries (MINOCA) (22) and many other women imaging experts. While CMR has become more widespread over the past 15 years, new methods are continuously being developed, validated, and deployed for patient care through integrated technological, translational, and clinical development.
Professional women in all careers face layered challenges. CMR is a physically and mentally demanding and fast-paced specialty. Here we describe some aspects of CMR that deter women from entering the field and the challenges of remaining engaged in the field. Although the field of CMR benefits from multi-disciplinary collaboration between specialists in cardiology, radiology, and physics/engineering, these different groups face different obstacles. While many similar challenges are experienced by women scientists in cardiovascular imaging, portions of this section are more applicable to women physicians, as the pathways for cardiologists and radiologists overlap more than that of the technical experts.
Historically, women were not allowed to train as doctors. As a result, parity in medical school intake has only been achieved in the last few decades (23, 24) with some countries continuing to lag (25). Fortunately, this recruitment barrier appears now largely resolved, with medical school graduates comprising an equal number of males and females. Improved female representation of women in medical schools is promising for increased representation of women in cardiology, diagnostic radiology, and cardiac imaging.
Even with this growing number of women in medical schools, it is interesting how medical professionals may mistakenly infer that women are now broadly well-represented, overestimating the true representation. The misperception could produce growing reservations or less support for gender equality initiatives and political support (26).
In reality, there is a progressive decline in female representation from each training step to clinical practice in cardiology. In the United States, women comprise 51% of medical school graduates and 43% of internal medicine residents, yet they are underrepresented in cardiology training and practice (27). Currently, 12–28% of cardiology trainees (23, 24, 28) and 24–30% of radiology trainees are female (29). In comparison, only 12–14% of fully trained cardiologists are women. Worldwide, women are less likely to reach the highest levels of cardiology (23, 24, 27, 28, 30–32). Though some of this disparity will inevitably improve as current trainees complete their training, the attrition rate remains high.
Literature reports that many women have been actively discouraged from becoming cardiologists. For example, numerous female cardiologists were told as young doctors not to become cardiologists because they are female (33) and sometimes because they were too “nice,” an assertion male doctors rarely encounter. Women also report being denied consultant, i.e., attending, cardiologist jobs, as other consultants would not work with women (33). In addition, although challenging to quantify formally, many women experience discrimination when applying for medical training posts or other career opportunities during their reproductive years, as it is often perceived that they may become pregnant and unavailable for clinical duties and call schedules. A male candidate is thus often preferred. When faced with these attitudes, many women will simply choose a specialty that demonstrates that they want them.
The demands of cardiology make an appropriate work-life balance difficult to maintain. Women looking to choose their specialty often consider this aspect carefully and are more likely than men to value family-friendly specialties, female-friendly specialties, and stable hours (34). Prospective trainees see the reality of life as a cardiologist: 38% of prospective female cardiology trainees report their female mentors not having a reasonable work-life balance (35). There is also the issue of long hours: in Japan, 50% of female cardiologists work more than 960 h of overtime a year, with more than 60% considering leaving the field due to gender discrimination, pregnancy, and children (36). Once within the cardiology specialty, trying to maintain a reasonable work-life balance can hinder training and career opportunities (35).
Similarly, for radiology, the rigors of rotations, an ever-increasing workload, and call schedule make at least half of the female radiology trainees and junior faculty prone to burn-out stemming from a poor work-life balance (37). In fact, burn-out is more prevalent among female radiology trainees entering parenthood because the radiology and cardiothoracic radiology training and early junior faculty years occur during the prime childbearing ages (38). Given this inference and the demographic shift of increasing mean childbearing age, radiology trainee-parents become a minority, with only 21% having one or more children (39). Additionally, 27% of radiology trainees are women likely experiencing work-life imbalance during early motherhood, thus precipitating burn-out among female diagnostic radiologists, making the specialty unattractive to women.
In an American College of Cardiology (ACC) life survey, female cardiologists and cardiology trainees had a 7% higher burn-out prevalence than male peers (40). Based on a Medscape survey of physicians from June to September 2021, radiology was the seventh most common medical specialty to be associated with burn-out (49%), with the highest level occurring among women compared to men (65% vs. 44%) (41). This results in low self-esteem, decreased career satisfaction, social dysfunction, poor well-being, and inevitable attrition from the profession.
Despite improvement over the decades, there remains a paucity of female role models and mentors within cardiology. Women cite a lack of female role models that creates hesitancy to apply for cardiology specialty training (34). However, simply being able to see that female cardiologists exist and succeed may be sufficient to encourage young women to pursue cardiology training (42). The value of female role models for diagnostic radiology and engineering sciences also holds true.
Women face discrimination, bullying, and harassment more frequently than men. Discrimination occurs across the world and is reported by female cardiologists 62% of the time in the UK, 65% in the US, and 68% worldwide. In the US, this figure has changed little over the past two decades (31, 43–45). Examples of gender-based discrimination include women not being introduced by their professional titles, patients transferring their care to male colleagues, and an implicit assumption by some men that women are simply not up to the pressures of cardiology with a corresponding loss in career opportunities (46, 47).
Regarding bullying, surveys of both trainees and consultants in the UK found that women were significantly more likely to have experienced bullying than men, and this bullying was usually sexist in nature. Women also report high levels of sexual harassment (36% of British and 12% of worldwide female cardiologists) (43, 44, 48).
Women may turn to senior female role models to seek advice to deal with these problems; however, the limited number of women in leadership of institutions, professional societies, and editorial boards limits availability. Additionally, many of these female role models face impossible pressures to succeed themselves and, at times, may adopt a more stereotypically masculine behavior and shun other women, keeping solidarity with their male peers (49). Improved networking among women professionals might provide another level of support.
Female cardiologists frequently express concern about how to plan their family while also having a career (34). This is not helped by perceived unfriendliness from their employer—43% of female cardiologists in the US have been asked about family planning in an interview setting.
Female cardiologists are less likely to be married (75% women vs. 89% men) and less likely to have children (72% women vs. 87% men). Many factors contribute to this discrepancy: in addition to institutional hostility, women who adopt part-time work patterns or take more extended periods of maternity leave are frowned upon and miss out on opportunities at work (50). Female cardiologists are also more likely to require paid childcare, whereas male cardiologists often have spouses that care for their children (46, 51). The outdated yet prevalent cultural norm of the female shouldering most of the childcare burden appears to prevail even when the female is the primary salary earner.
Maternity leave policies differ significantly worldwide. In the US, an outlier in parental leave policies, 50% of female cardiologists took eight weeks or less of maternity leave, with only 3% taking more than 6 months. One-quarter reported that their maternity leave was unpaid, and more than half felt pressured to return to work early. Cardiologists in training felt particularly pressured compared to those that had completed training. One-third of female cardiologists in the US also reported being asked to do extra service or call prior to their maternity leave (50, 52).
Maternity leave of female cardiologists outside of the US has not been studied in as much detail as in the US; however, in a worldwide survey of female surgeons (a similar cohort to female cardiologists), average maternity leave was between 7 and 12 months. However, in this worldwide survey, only half felt that their employer was generally supportive, and 80% of female surgeons reported being told that a surgical career was incompatible with parenthood (53).
Likely for safety reasons, pregnant people were often excluded from any place where radiation exposure could occur. While CMR per se does not involve radiation, advanced imagers often train in both CMR and cardiovascular computed tomography (CCT), using X-rays for imaging. More recently, this level of extreme caution around pregnant people has been replaced by warnings coupled with more monitoring. For example, there are now guidelines regarding radiation exposure that set strict limits and include using a fetal monitoring badge (54, 55). These guidelines are not overly restrictive and allow training and career progression to continue even when pregnant safely. Despite this added vigilance, women are increasingly more concerned about radiation exposure than previous cohorts (50, 51, 54, 55). This concern may potentially result in less exposure to training or scanning involving radiation and fewer opportunities due to this reduced experience.
With arduous long hours, overnight calls, and at times, a competitive, cutthroat work environment, the fields of radiology or cardiology are often not conducive to family life, discouraging women from considering these fields as a career. As mentioned, female cardiologists often have more domestic responsibilities than their male counterparts, spending around 8.5 h more on household tasks per week than their male peers. They also shoulder more caretaking—for sick children and parents in need—compared to their male counterparts (56, 57). With average work weeks of 40–60 h, these extra responsibilities outside of work can quickly create unsustainable pressure (58). Flexible work patterns can help, but these can be difficult to negotiate and achieve (23, 51). Part-time working patterns are often unavailable to trainees, who are most likely to have very young children. Where part-time work is allowed, there is still very low uptake: only 4% of cardiology trainees in the UK work part-time (59). Once fully trained, working part-time is also uncommon: only 10% of female cardiologists in the UK work part-time as opposed to 4% of men (44). Part-time work brings its own challenges: lower pay, fewer career opportunities, and loss of status. A recent British survey showed that cardiologists who work part-time are perceived as having lower status (44).
Women are underrepresented in cardiovascular academia: only 17% of faculty appointments are women. Women have significantly lower rates of the first authorship, particularly in high-impact journals, and are cited less often (60–63). Female cardiologists are often neither involved in the high-impact trials nor on the writing committees of clinical guidelines (64–66). Women in academia also have less success in career development awards, with gender differences persisting in a number of awards for clinician-researchers in the US, even when adjusting for confounders (67). Similarly, women in radiology are under-represented, with only 34% of women joining academia in the US. However, this number declines at higher levels of leadership, reaching just 25% among section chiefs and vice chairs and 9% among chairs (68).
Significant gender inequity persists when it comes to compensation. Female cardiologists continue to earn, on average, $32,000 less than male cardiologists in both private practice and academia, even after controlling for location, subspecialty, and full-time status (65, 66, 69). This disparity in earnings is exacerbated by the cost of children, both in fewer work hours or hired child care: either women are predominantly responsible for looking after their children (and thus not able to work and earn), or they must arrange paid childcare, which will cost around 11–20% of their salary (44, 53, 56).
As mentioned above in their independent sections, societal habits and traditions, such as family planning, marriage, divorce, relocation, work-life balance and the risk of burn-out, lack of female role models, discrimination, harassment, and bullying, radiation exposure, responsibilities outside of work, academia and salary, among others, where women are submitted to more substantial constraints than men, have reached a political dimension in some countries in the world, leading to action and legislation specifically to help women with these aspects for better professional equity (70).
Utilizing the data obtained by a survey launched by the Society for Cardiovascular Magnetic Resonance (SCMR) in 2017 that is currently under review by the Journal of Cardiovascular Magnetic Resonance (see text footnote 1), an analysis was performed to identify women’s participation in CMR practice around the world. Of 1,086 respondents, 337 (31%) were women, as shown in Figure 1.
The percentage of female CMR practitioners who responded to the survey varied significantly depending on the geographical location (Figure 2). Female respondents were as follows: in New Zealand, Thailand, Romania, Indonesia, Egypt, Uruguay, and Kuwait, women represented 67–80% of respondents; in Norway, Malaysia, Sweden, Hong Kong, Lithuania, Algeria, Republic of Korea, and Finland, 50–57% of respondents were women; in Mexico, India, Canada, the UK, Italy, Singapore, Denmark, Spain, China, South Africa, Australia, Argentina, Colombia, Austria, South Korea, Chile, and Switzerland, 32–47% of respondents were women; in Saudi Arabia, the Czech Republic, Brazil, Germany, and the US, Greece, and Hungary, only 20–25% of respondents were women; in Portugal, Ireland, and Japan, 14–17% of respondents were women; and only 3% of the Netherlands respondents were women.
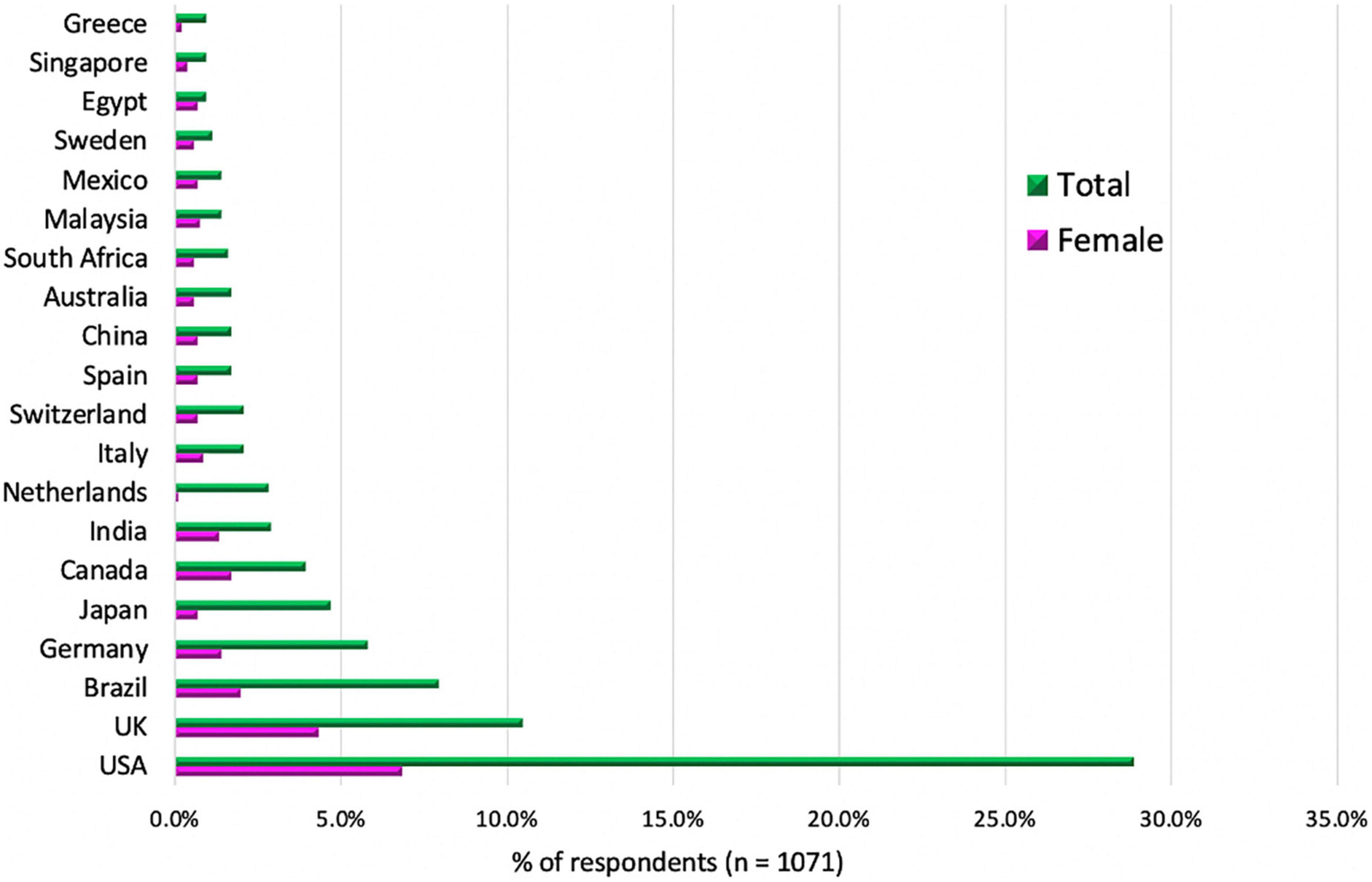
Figure 2. Top 20 countries of origin of surveyed respondents (n = 1,071). The top 20 countries with the most respondents are shown. The data from all other respondent countries are not displayed in the graph. The detailed description of the responders and their gender (within parentheses) were as follows, for USA 309 (F:73/M:236), UK 112 (F:46/M:66), Brazil 85 (F:21/M:64), Germany 62 (F:15/M:47), Japan 50 (F:7/M:43), Canada 42 (F:18/M:24), India 31 (F:14/M:17), the Netherlands 30 (F:1/M:29), Switzerland 22 (F:7/M:15), Italy 22 (F:9/M:13), China 18 (F:7/M:11), Australia 18 (F:6/M:12), Spain 18 (F:7/M:11), South Africa 17 (F:6/M:11), Malaysia 15 (F:8/M:7), Mexico 15 (F:7/M:8), Sweden 12 (F:6/M:6), Egypt 10 (F:7/M:3), Greece 10 (F:2/M:8), Singapore 10 (F:4/M:6). The rest of the surveyed countries are described in the Supplementary material.
In the Philippines, El Salvador, Nicaragua, Iran, Georgia, Russia, Panama, Myanmar, Morocco, and Monaco, there were 1–3 respondents, and all of them were only women.
There were no responses from Turkey, France, Belgium, United Arab Emirates, Qatar, Bangladesh, Slovakia, Poland, Pakistan, Ecuador, Andorra, Venezuela, Oman, Mongolia, Lebanon, Vietnam, and Kazakhstan women.
The age distribution by ranges showed almost a consistent trend of 30% of women respondents for ages less than 60 years; women made up a smaller percentage of older respondents (8% in the range of 61 to 70 years old, and 0% older than 70 years). This is concordant with the history of CV imaging and CMR, mainly dominated by males in the past. However, an exciting and encouraging fact revealed is that the highest percentage of women respondents was in the youngest surveyed range (from 21 to 30 years old), demonstrating an apparent increase in women joining the field in recent years (Figure 3).
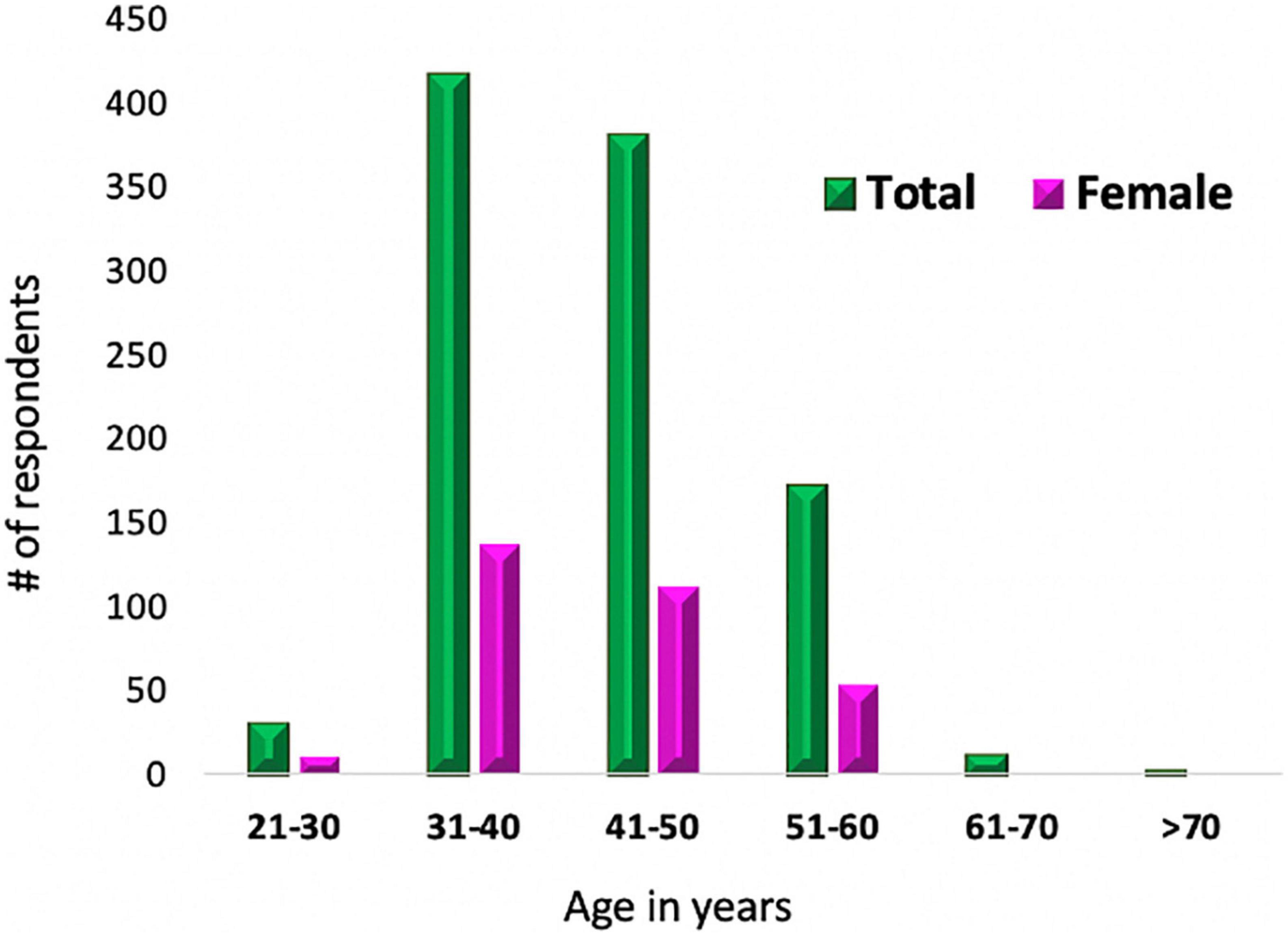
Figure 3. Age distribution of surveyed CMR practitioners. This graph displays the age range distribution of the CMR surveyed practitioners with the breakdown of the percentage of women respondents.
When examining the most common practice types of those working in CMR, it is interesting to note that for both men and women, there is more CMR practice in the academic and government scenarios compared to private practice, as displayed in Figures 4, 5. One might speculate that the economics of performing, interpreting, and reimbursement of CMR may contribute to this difference. However, there may also be less representation of private practices and small private hospitals within the SCMR; thus, the data should not be overinterpreted.
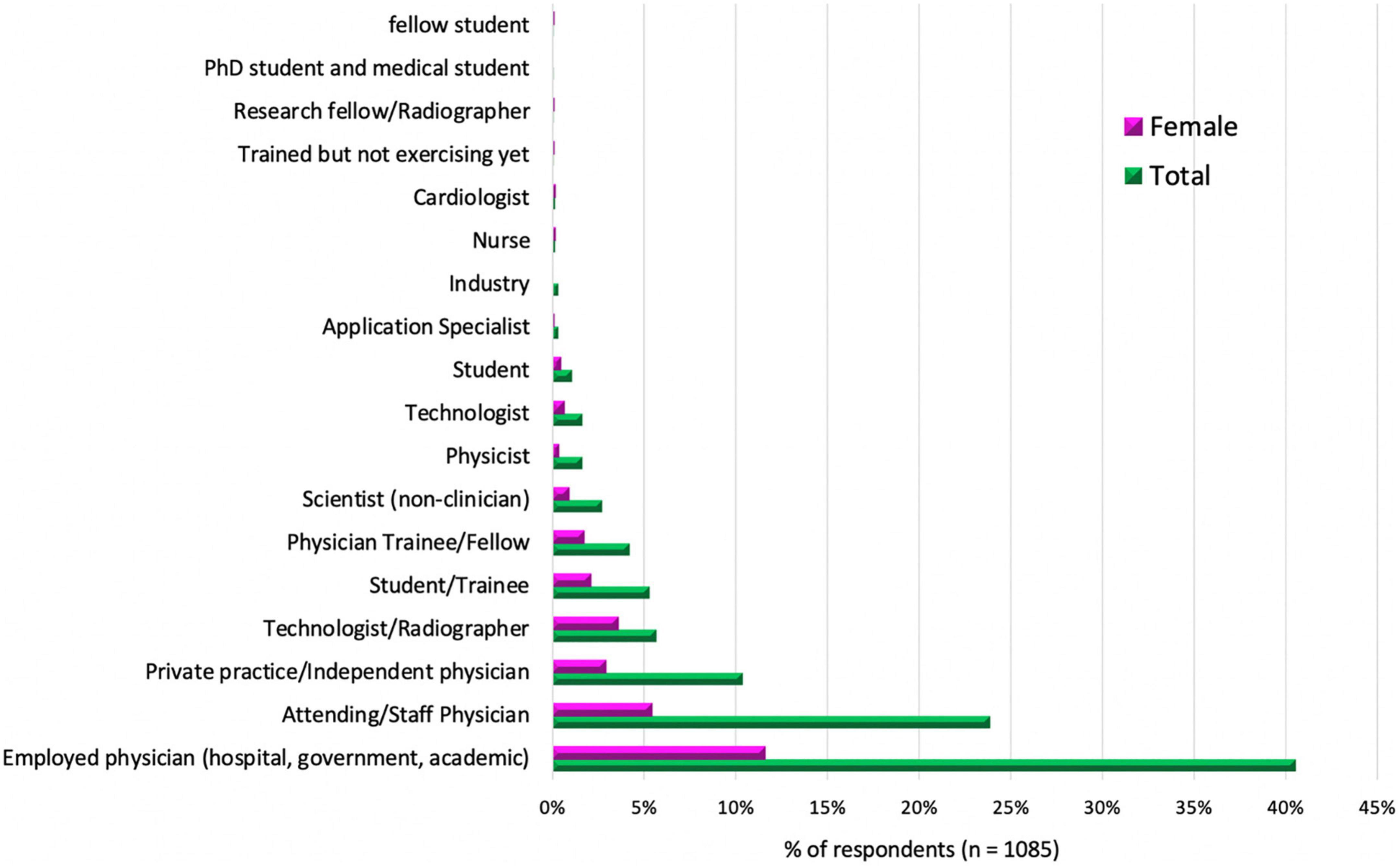
Figure 4. Stage of training or primary practice type of the CMR survey practitioners. This bar graph shows the different types of primary practice or stages of training of those CMR surveyed practitioners. The distribution is shown in percentages of total (male and female) in green and just female respondents in pink.
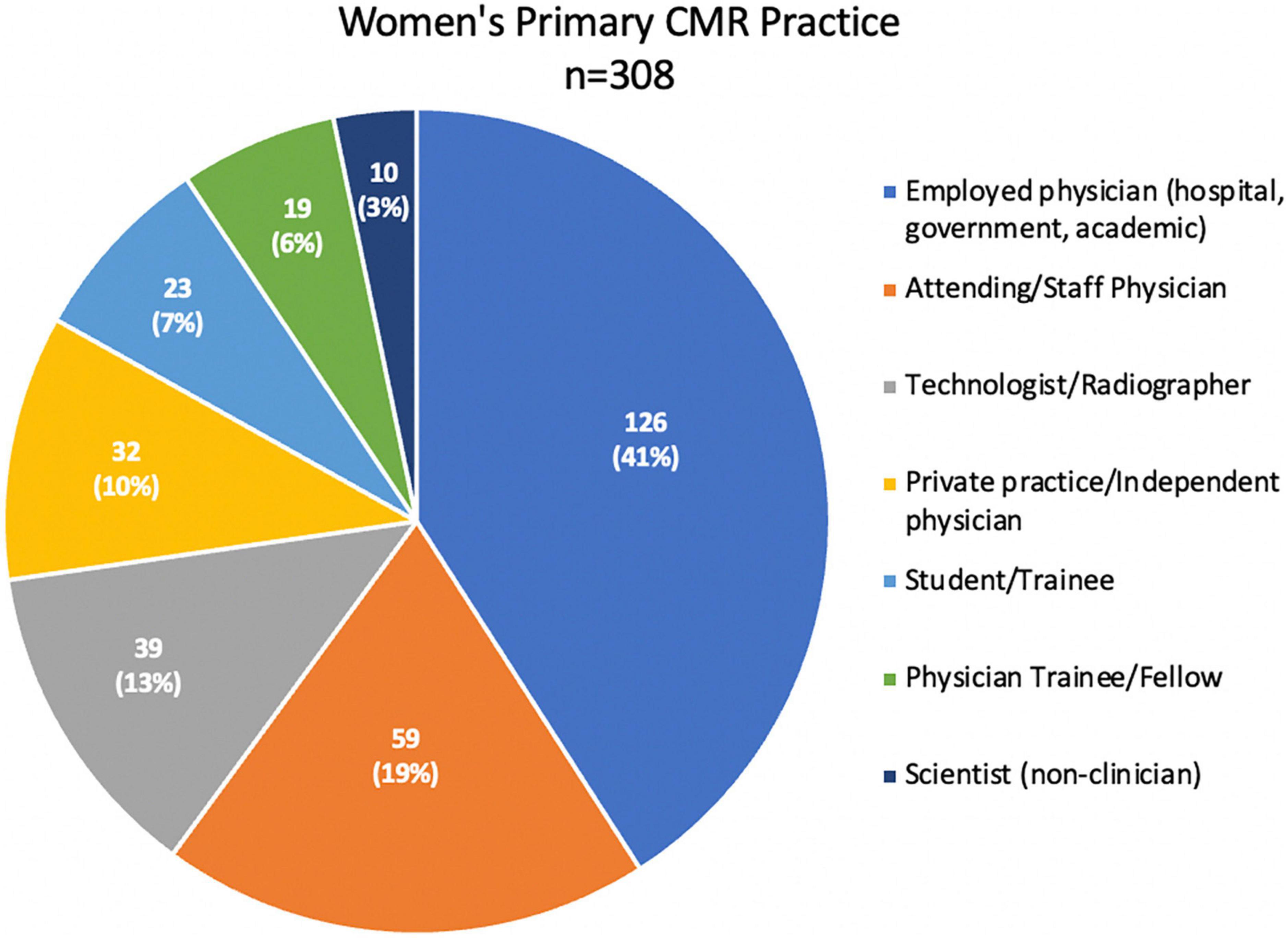
Figure 5. Women’s primary CMR practice of the CMR survey practitioners. Responses in this category = 308. This pie graph shows the distribution of the women’s primary CRM practice as employed physicians at different kinds of institutions such as academic, community, or government hospitals (n = 126, 41%), attending or staff physicians (n = 59, 19%), technologists or radiographers (n = 39, 13%), private practice or independent physicians (32, 10%), pre-grade students or trainees (23, 7%), physician trainees, residents or fellows (19, 6%), and scientist (non-clinician) (10, 3%).
Both recruiting women and retaining women physicians and scientists in cardiovascular imaging are essential to increasing their numbers. Progress is slow, but it is also encouraging: the proportion of women is increasing in medical school and in cardiology and radiology training programs (23, 27). Likewise, the number of women physicists and engineers is growing. However, over the past decade, the percentage of women in diagnostic radiology training has remained steady at 30% (29, 71). As women’s numbers and leverage increase, they will begin to assert themselves to negotiate more favorable conditions: good parental leave policies, flexible work patterns, and equal pay (51, 72). These should be available for both women and men to help eliminate tendencies to avoid hiring female candidates. Those running training programs should consider optimizing work conditions for everyone to continue attracting the best candidates.
To increase the number of women entering cardiology, diagnostic radiology, and cardiac imaging, it is essential to target women interested in medicine or a biomedical career early in the process while in high school, college, or medical school. Additionally, there are too few mentors targeted explicitly toward working with women. Imaging societies must provide avenues for trainees and early career professionals to interact with expert advanced cardiovascular imagers. In addition to increasing the number of mentors from both genders, educating and engaging those in leadership about gender disparities and biases are essential. Professional societies should create initiatives to ensure that diversity is a priority and that women advanced imagers are supported to increase representation. This should happen both at the level of societal leadership, societal committees, and core groups.
Despite rising awareness of women’s unique challenges, the need for flexible working patterns, and better family planning policies, barriers remain. The recent global pandemic has shown how quickly progress can be eroded: women have faced a disproportionate impact, taking on increased domestic and childcare responsibility, affecting jobs and salaries (73, 74).
The early career remains a challenging period for female professionals due to the tension between job requirements and additional family responsibilities, including childbearing. Supporting female physicians and scientists during this difficult time by instituting policies for maternity leave and ensuring flexible work hours (including part-time positions, telework, and different adaptable strategies) can help retain women as advanced imagers in the field. The increasing burn-out rate among female physicians should serve as an impetus for many institutions to adopt and support physician-parent wellness, such as a prolonged family leave policy and sustaining gender diversity and parity in advancements and leadership for female faculty. Establishing and supporting groups, such as women in radiology or parenting mentorship, will pay dividends in the form of improved retention of female faculty and well-being. This premise is based on the literature that radiology trainees and junior faculty reported increased networking (94%) compared to senior faculty (69%) and increased research involvement, which accelerated the professional development and contributed to a more diverse and enabled workforce (75).
Institutions and professional societies must enforce a no-tolerance policy for sexual harassment or bullying in the workplace. Institutional leadership’s responsibility is to create a culture to promote a safe environment where victims of sexual harassment and gender bias feel empowered to report it.
Additionally, institutions should regularly conduct reviews and analyses of faculty salaries to uncover any unconscious biases in salary negotiation.
The empowerment strategies in cardiovascular imaging parallel women’s empowerment in cardiology, diagnostic radiology, and physics/engineering, which include increasing opportunities for leadership training and women in leadership positions who can serve as role models such as advocates, coaches, and mentors for other women (Figure 6).
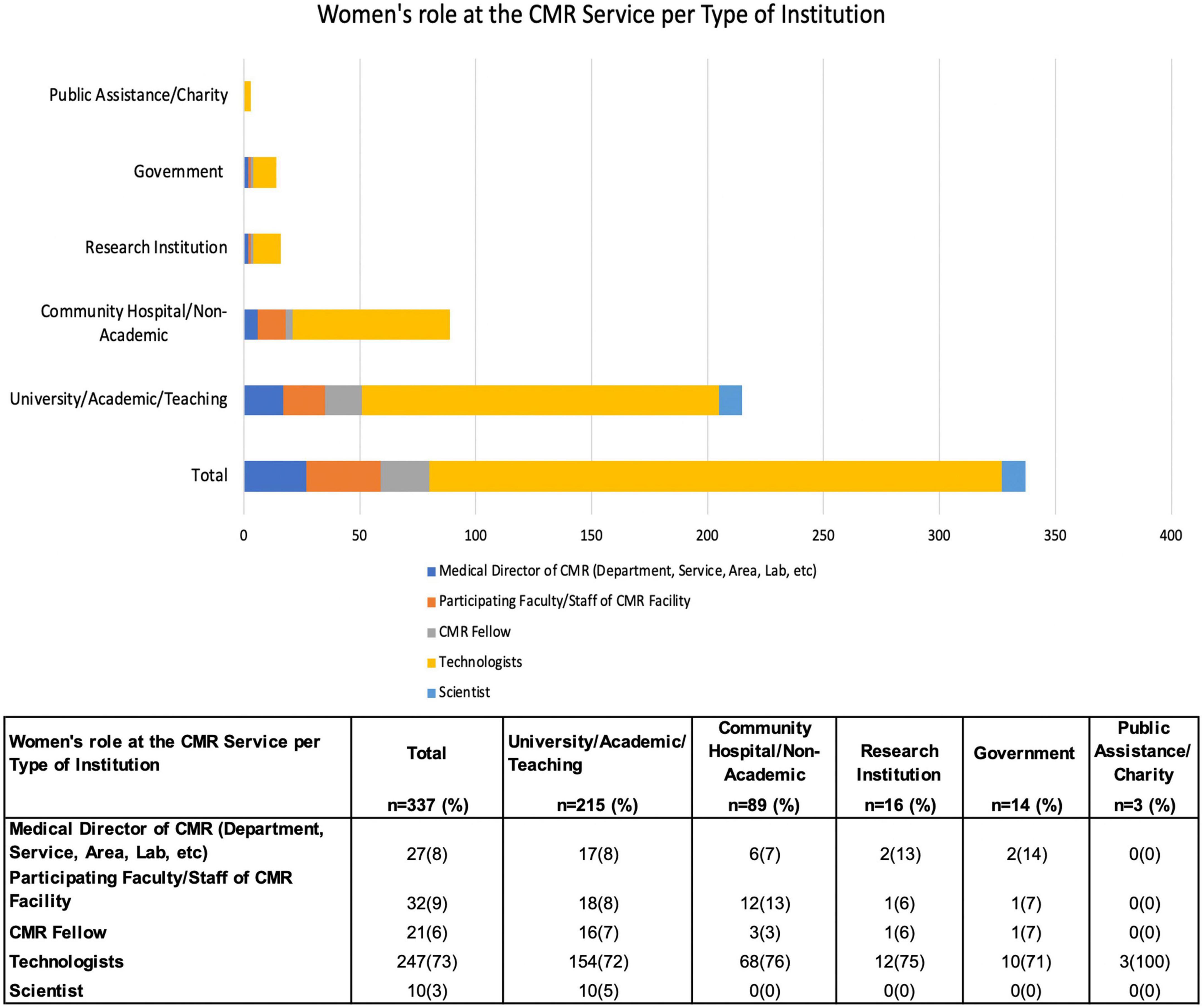
Figure 6. Women’s role at the CMR Service per Type of Institution of the CMR survey practitioners. Responses in this category = 337. This stacked bar graph shows the women’s role at the CMR service per type of institution, where 64% practice in the university, academic, or teaching environment. Although it is where women primarily participate in leadership roles, 26% of women develop their professional activities in the community or non-academic institutions, where 76% participate as technologists. Women scientists are working only in universities or academic institutions. Detailed data shown in the graph description is in the table at the bottom of the figure.
To improve retention rates of women in cardiology, societies such as the British Cardiac Society (BCS) and American College of Cardiology (ACC) have created Women in Cardiology (WIC) groups that serve as important leadership, career development, and advocacy forums for female cardiologists (76). In addition, the ACC has introduced several initiatives, including courses such as “Upping your game – clinical trials training,” aimed at providing opportunities for learning and networking for underrepresented minorities and women in the field. Furthermore, the Association of American Medical Colleges (AAMC) offers a “Mid Mid-Career Women Faculty Leadership Development Seminar” every year for mid-career women faculty who have been at the associate professor level for at least two years with “the knowledge and skills necessary to support their continued progress along the path to leadership in academic medicine and science.” The seminar includes organizational leadership topics and career-advancing strategies considered highly important for effective leadership throughout “various mission-critical activities.”
Some institutions have programs to mentor and promote women faculty. For example, at the University of Pennsylvania, there is a program called FOCUS (77) that focuses on the health and leadership of women with separate sections for medical students, residents and fellows, junior faculty, and senior faculty. This program addresses the key national issue of the underrepresentation of women in senior levels of academic medicine. Moreover, with the support from the Dean of the Medical School, FOCUS launched initiatives including seminars, workshops, and conferences related to career development and mentoring; faculty research seed grants and recognition awards, and medical student fellowships in mentored projects involving women’s health research to recruit, retain, and promote female leadership. These kinds of institutional and medical societal programs are crucial to providing leadership training and empowerment for female academic physicians.
Similarly, on the radiology side, there is a very active American Association for Women Radiologists (AAWR) that educates and enhances the professional fulfillment of female radiologists. In addition, almost every academic radiology department in the United States has adopted and supported women in radiology groups providing bona fide opportunities for mentorship and leadership growth (75). The Radiological Society of North America (RSNA) has embraced several committees empowering women across subspecialties. One such example is the Committee for Diversity, Equity, and Inclusion (DEI), whose member efforts are geared toward increasing the visibility of women in the field. For example, 57% of RSNA committee chairs are women; nine women have served on the RSNA Board of Directors, and seven women have served as RSNA President. Recognizing the need for women’s empowerment in radiology, the AAWR was formed 25 years ago to promote, educate, and advocate for women radiologists. The AAWR holds regular meetings and workshops tailored to meet women’s needs in radiology.
While there are no explicitly tailored programs/workshops for women empowerment in the cardiovascular imaging subspecialty, the North American Society of Cardiovascular Imaging (NASCI) has worked diligently to increase the representation and visibility of women within the society. In terms of women’s reputation in leadership (as tabulated below), NASCI follows closely with the Society for Cardiovascular Magnetic Resonance (SCMR). Table 1 (78–89) shows a current year comparison of the women’s participation in main US-based international cardiovascular imaging societies, using the leadership roles in executive officer positions and committees chairs as a surrogate of female involvement in the field. Note that the comparison is limited by what was available on each society’s publicly available website and differences between each organizational governance rule and represents more of an “at-a-glance” assessment of women’s representation in these societies. The American Society of Echocardiography (ASE) seems to be particularly successful in elevating women to leadership roles.
Although women are well-represented in NASCI, gender parity has not been reached in all reaches of the society. The number of women speakers and moderators (n = 35; 33%) at the 2021 annual meeting indicates that we need to understand women’s needs better and increase their engagement in future meetings. These findings are reproduced at other organizations’ meetings. Improved support for women’s engagement may include providing childcare during the meeting, lactation rooms, work and life integration workshops, one-on-one mentor-mentee sessions, and/or short-term coaching sessions, which describe how to navigate through the system to offset any future decline of leadership role or active participation during the annual meetings.
From the highest leadership perspective, women are still underrepresented in imaging, as shown in Table 1. In addition, the percentage of female presidents of the imaging societies was lower than its female membership. However, in the executive officers (defined differently among societies but typically in addition to the president, including positions like the vice president, treasurer, and secretary, among other offices) and committee chairs, there is a higher representation of women than traditionally seen. To increase female leadership at the top, a pipeline of leaders must be developed through leadership education and mentoring. Both the American Society of Echocardiography (ASE) and the American Society of Nuclear Cardiology (ASNC) have leadership programs, although not explicitly geared toward women.
Recently, in 2020, The European Association of Cardiovascular Imaging (EACVI) formed its Task Force of Women in CV Imaging. The task force represents an initiative within the EACVI to connect members interested in promoting women’s representation both in the career setting and leadership roles and in clinical research development in CV diseases in women. This task force intends to unite women in CV imaging worldwide and provide opportunities that may not be available to all women professionals. The main goal intends to help low-to-middle-income country women imagers train within a European country with strong CV imaging expertise with a plan to then return to their home country and serve the community, providing continuous support by addressing challenging cases via remote communication (88).
The increasing involvement of women in the SCMR also corresponds to the initiation and sustained activities of the SCMR Women in CMR Group, which was the brainchild of Dr. Dara Kraitchman (Figure 7). The Women in CMR group meets at the annual SCMR Scientific Sessions and throughout the year. Since the advent of this group, a steady increase in women’s engagement in leadership positions within the SCMR over the past decade has been evident (Figure 7). In addition, women leaders have also stimulated and founded new interest groups like those focused on cardio-rheumatology and cardio-oncology, as well as the CMR translation working group that has advocated for the translation of key CMR documents into other languages to promote international dissemination of the field. These data indicate a shift in thinking and demonstrate positive support for women’s engagement within the CMR community. Intersocietal joint activities (e.g., between the SCMR and ISMRM or other imaging societies) may help to amplify awareness of women’s issues within the field of CMR and imaging, as well as help to jointly work on action items to solve some of the ongoing challenges.
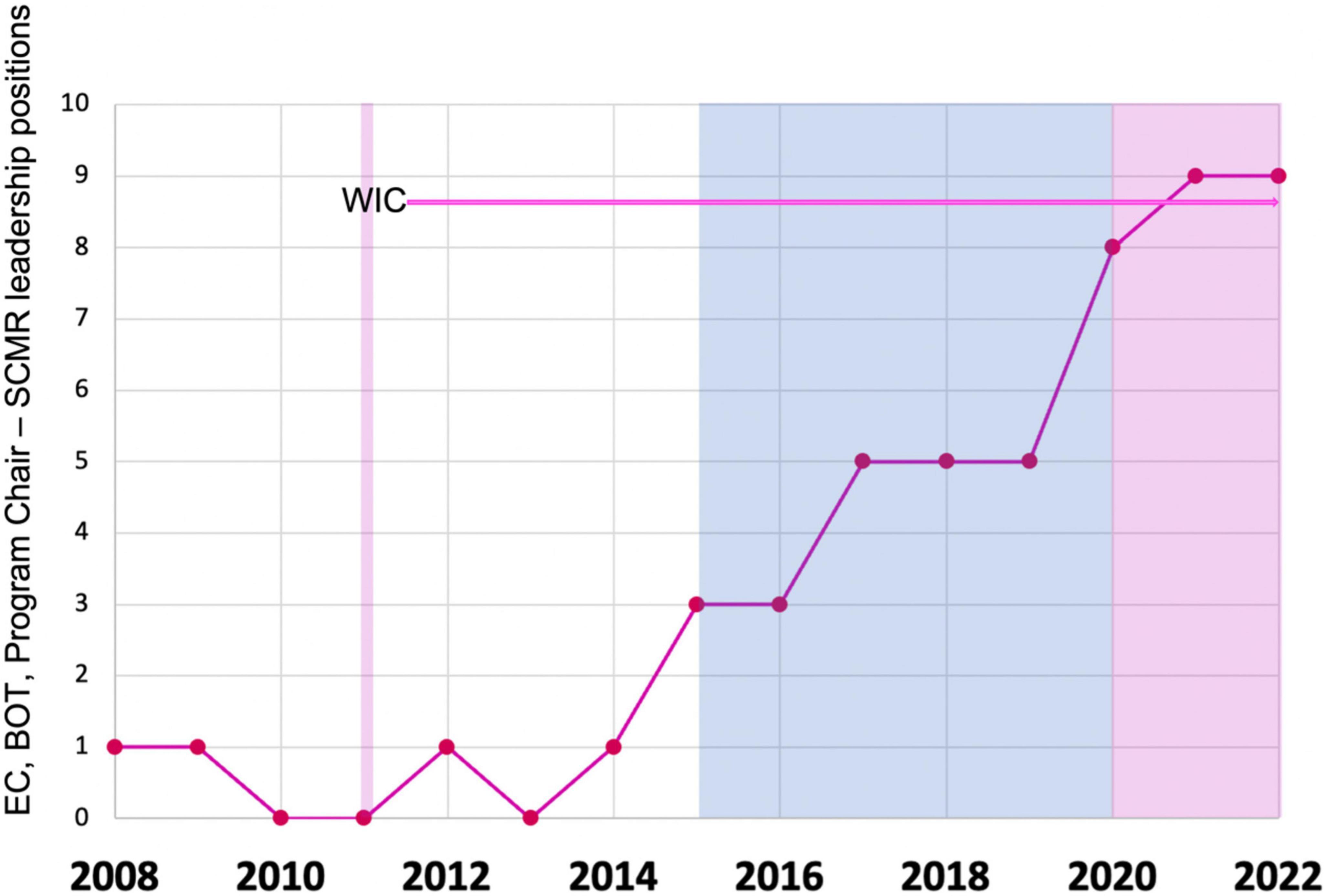
Figure 7. Women’s representation in SCMR leadership. The blue background represents the first CEO (male) and the pink the second and current CEO (female) of SCMR. The thick pink line marks the Women in CMR (Special group of SCMR) establishment as a Task Force by Dara L. Kraitchman, Ph.D., and supported by the E.C. leadership by Victor A. Ferrari, MD. EC, Executive Committee; BOT, Board of Trustees; WIC, women in CMR (Special group of SCMR).
Even as women have become more involved in the field of CMR, CMR has likewise impacted women’s cardiovascular health (90). Among the cardiovascular diagnoses affected are myocardial infarction in the setting of non-obstructive coronary arteries (MINOCA), small vessel disease ischemia, ischemic heart disease in general, rheumatological disorders, and cardio-oncology.
Historically, women with acute coronary syndrome exhibit symptoms that differ from men. Chest pain may be vague or completely absent. Women may present with fatigue or shortness of breath as a primary symptom. In the past, when women presented with an acute coronary syndrome with elevated cardiac enzymes but non-obstructive coronary arteries or MINOCA, the next steps in management were unclear. Implementing CMR in this diagnosis has helped to elucidate an underlying etiology clarifying if a patient has myocarditis, stress cardiomyopathy (Takotsubo), coronary dissection, or coronary spasm (22, 91). CMR’s strengths in comprehensively evaluating the myocardium and its pathophysiologic health (e.g., looking for edema, inflammation, and fibrosis), as well as other cardiac structures like the coronary arteries, elevate its importance in being used early in the patient presenting with chest pain.
In the non-acute chest pain setting, CMR is exceptional in identifying small vessel ischemia using vasodilator perfusion. In newer methods, myocardial perfusion may be quantified, and endocardial-to-epicardial myocardial blood flow ratios assessed. Dr. Noel Bairey Merz, a Professor of Medicine at the Cedars Sinai Heart Institute, and others demonstrated the utility of CMR in evaluating women with chronic chest pain who have non-obstructive coronary arteries (22). With a diagnosis of small vessel disease, clinicians then have a therapeutic target; whereas, in the past, without a definitive diagnosis, treatment was directed as a “best guess,” or worse yet, women were told that their chest pain was non-cardiac.
Diagnosing epicardial coronary artery disease in women has also not been straightforward. Exercise treadmill has a notoriously high false-negative rate in women; nuclear stress testing may yield false positive or equivocal results with breast attenuation. However, CMR stress testing provides a comprehensive assessment of myocardial ischemia, independent of a woman’s body mass index or body habitus (92).
Another field that CMR has changed is that of cardio-rheumatology. Rheumatological disorders such as systemic lupus erythematosus, dermatomyositis, and polymyositis affect women greater than men (e.g., 90% of patients with lupus are women between the ages of 15 and 45 years of age). Again, the ability to discern when the heart is actively affected helps guide the management of the rheumatological patient. Newer parametric mapping methods now offer the ability to serially follow patients, even without contrast, to monitor patients’ response to therapy (93, 94).
Cardio-oncology and a host of therapeutic-related adverse events affect both men and women. However, breast cancer cardio-toxicities have mainly utilized CMR effectively to monitor anthracycline toxicities. Active research is ongoing, using CMR to monitor chemo- and immunotherapeutic toxicities, parametric mapping, and myocardial strain. Beyond identification of cardiomyopathy, CMR may also detect therapy-related acute myocarditis. In women who have undergone chest irradiation and are at risk for premature atherosclerosis, CMR provides a comprehensive assessment of ischemic heart disease using pharmacologic or exercise stress testing (95, 96).
The aforementioned uses of CMR are not meant to comprise an exhaustive list but rather demonstrate a few common examples in which CMR has impacted women’s cardiovascular health. Research and clinical translation are ongoing in a multitude of disease processes. MRI pulse sequences and technology are continuously developing, and new CMR applications are constantly evolving.
It is of particular relevance to highlight the role of CMR in improving cardiovascular care since women are under-represented in clinical trials (97–99), limiting biological understanding and contributing to health inequities, social injustice (99), and impacting their health directly as the state-of-the-art treatments and recommendations have been historically mainly male-oriented (100). Within CMR clinical studies and trials, dedicated emphasis in understanding sex as a biologic variable also needs additional attention and should be a goal for current and future studies.
While there have been challenges to entering and remaining in the field, recent data show that women have become an integral part of the cardiovascular imaging workforce. However, additional work remains to support and increase women’s representation in cardiovascular imaging, academia, and multi-disciplinary societies. Recognition of the need for diversity is more widespread, as well as recognition of the need to better support women in all career stages. For example, women’s representation on moderator and speaking panels requires additional mindfulness and work on the part of the organizers, not simply to fulfill a quota but to add to the depth, breadth, and richness of the meetings as there are qualified women who have valuable and unique expertise to share in the scientific sessions. Similarly, active women’s participation in leadership roles within professional societies adds valuable insights and diversity to the growing field. It should be restated clearly that the entire effort to help engage women in cardiology and radiology is not only fair and proper but also enhances the field—increasing the resilience and level of care.
There has been significant progress in advancing cardiovascular magnetic resonance and cardiovascular imaging. Translational applications of cardiovascular imaging make a difference in cardiovascular diagnosis, management, and prognosis. While the initial involvement of women professionals was low, the engagement of creative, thoughtful physicists, engineers, cardiologists, and radiologists within the field has grown and continues to grow. At this moment, we are just beginning to bend the curve. However, sustained vigilance and creative effort will ensure that the future of women in cardiovascular imaging is hopeful and bright.
LS-G designed the project. LS-G, NA, JS, SR, YH, VF, KT, NS, PP, CB-D, LB, SM, KO, JS-M, and WB discussed the content, wrote the manuscript, reviewed, and approved the final version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, nor the U.S. Department of Health and Human Services.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.984326/full#supplementary-material
1. Association of American Medical Colleges. Workforce. Physician Specialty Data Report. Active Physicians by Sex and Specialty. Washington, DC: AAMC (2019).
2. Tsugawa Y, Jena A, Figueroa J, Orav E, Blumenthal D, Jha A. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med. (2017) 177:206–13. doi: 10.1001/jamainternmed.2016.7875
3. Greenwood B, Carnahan S, Huang L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U.S.A. (2018) 115:8569–74. doi: 10.1073/pnas.1800097115
4. Budoff M, Achenbach S, Blumenthal R, Carr J, Goldin J, Greenland P, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American heart association committee on cardiovascular imaging and intervention, council on cardiovascular radiology and intervention, and committee on cardiac imaging, council on clinical cardiology. Circulation. (2006) 114:1761–91. doi: 10.1161/CIRCULATIONAHA.106.178458
5. Leiner T, Bogaert J, Friedrich M, Mohiaddin R, Muthurangu V, Myerson S, et al. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J Cardiovasc Magn Reson. (2020) 22:76. doi: 10.1186/s12968-020-00682-4
6. Jorgensen T. Marie Curie and her X-ray Vehicles’ Contribution to World War I Battlefield Medicine. (2017). Available online at: https://theconversation.com/marie-curie-and-her-x-ray-vehicles-contribution-to-world-war-i-battlefield-medicine-83941?xid=PS_smithsonian (accessed May 22, 2022).
7. Goldman M, Pohost G, Ingwall J, Fossel E. Nuclear magnetic resonance imaging: potential cardiac applications. Am J Cardiol. (1980) 46:1278–83. doi: 10.1016/0002-9149(80)90299-4
8. Edelman R, Chien D, Atkinson D, Sandstrom J. Fast time-of-flight MR angiography with improved background suppression. Radiology. (1991) 179:867–70. doi: 10.1148/radiology.179.3.2028008
9. Lim T, Hong M, Lee J, Mun C, Park S, Park S, et al. Novel application of breath-hold turbo spin-echo T2 MRI for detection of acute myocardial infarction. J Magn Reson Imaging. (1997) 7:996–1001. doi: 10.1002/jmri.1880070611
10. Rosen B, Belliveau J, Chien D. Perfusion imaging by nuclear magnetic resonance. Magn Reson Q. (1989) 5:263–81.
11. Hänicke W, Merboldt K, Chien D, Gyngell M, Bruhn H, Frahm J. Signal strength in subsecond FLASH magnetic resonance imaging: the dynamic approach to steady state. Med Phys. (1990) 17:1004–10. doi: 10.1118/1.596452
12. Niemi P, Poncelet B, Kwong K, Weisskoff R, Rosen B, Brady T, et al. Myocardial intensity changes associated with flow stimulation in blood oxygenation sensitive magnetic resonance imaging. Magn Reson Med. (1996) 36:78–82. doi: 10.1002/mrm.1910360114
13. Poncelet B, Koelling T, Schmidt C, Kwong K, Reese T, Ledden P, et al. Measurement of human myocardial perfusion by double-gated flow alternating inversion recovery EPI. Magn Reson Med. (1999) 41:510–9. doi: 10.1002/(SICI)1522-2594(199903)41:3<510::AID-MRM13>3.0.CO;2-G
14. Huang T, Liu Y, Stemmer A, Poncelet B. T2 measurement of the human myocardium using a T2-prepared transient-state TrueFISP sequence. Magn Reson Med. (2007) 57:960–6. doi: 10.1002/mrm.21208
15. Pandharipande PV, Lee V, Reuss P, Charles H, Rosen R, Krinsky G, et al. Two-station bolus-chase MR angiography with a stationary table: a simple alternative to automated-table techniques. Am J Roentgenol. (2002) 179:1583–9. doi: 10.2214/ajr.179.6.1791583
16. Miyazaki M, Lee V. Nonenhanced MR angiography. Radiology. (2008) 248:20–43. doi: 10.1148/radiol.2481071497
17. Lee V, Resnick D, Tiu S, Sanger J, Nazzaro C, Israel G, et al. MR imaging evaluation of myocardial viability in the setting of equivocal SPECT results with (99m)Tc sestamibi. Radiology. (2004) 230:191–7. doi: 10.1148/radiol.2301030070
18. Schulz-Menger J, Abdel-Aty H. Use of integrated biomarkers in inflammatory disease of the heart: new insights applying cardiovascular magnetic resonance potential as a biomarker. Expert Opin Med Diagn. (2008) 2:883–9. doi: 10.1517/17530059.2.8.883
19. Wagner A, Schulz-Menger J, Dietz R, Friedrich M. Long-term follow-up of patients paragraph sign with acute myocarditis by magnetic paragraph sign resonance imaging. MAGMA. (2003) 16:17–20. doi: 10.1007/s10334-003-0007-7
20. Abdel-Aty H, Boye P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. (2005) 45:1815–22. doi: 10.1016/j.jacc.2004.11.069
21. Raman SV, Dickerson J, Mazur W, Wong T, Schelbert E, Min J, et al. Diagnostic performance of treadmill exercise cardiac magnetic resonance: the prospective, multicenter exercise CMR’s accuracy for cardiovascular stress testing (EXACT) trial. J Am Heart Assoc. (2016) 5:e003811. doi: 10.1161/JAHA.116.003811
22. Occhipinti G, Bucciarelli-Ducci C, Capodanno D. Diagnostic pathways in myocardial infarction with non-obstructive coronary artery disease (MINOCA). Eur Heart J Acute Cardiovasc Care. (2021) 10:813–22. doi: 10.1093/ehjacc/zuab049
23. Sinclair H, Joshi A, Allen C, Joseph J, Sohaib S, Calver A, et al. Women in cardiology: the British junior cardiologists’ association identifies challenges. Eur Heart J. (2019) 40:227–31. doi: 10.1093/eurheartj/ehy828
24. Oza N, Breathett K. Women in cardiology: fellows’ perspective. J Am Coll Cardiol. (2015) 65:951–3. doi: 10.1016/j.jacc.2015.01.011
25. Ramakrishnan A, Sambuco D, Jagsi R. Women’s participation in the medical profession: insights from experiences in Japan, Scandinavia, Russia, and Eastern Europe. J Womens Health. (2014) 23:927–34. doi: 10.1089/jwh.2014.4736
26. Begeny C, Grossman R, Ryan M. Overestimating womens representation in medicine: a survey of medical professionals estimates and their(un)willingness to support gender equality initiatives. BMJ Open. (2022) 12:e054769. doi: 10.1136/bmjopen-2021-054769
27. Khan M, Mahmood S, Khan S, Fatima K, Khosa F, Sharma G, et al. Women training in cardiology and its subspecialties in the United States: a decade of little progress in representation. Circulation. (2020) 141:609–11. doi: 10.1161/CIRCULATIONAHA.119.044693
28. Segan L, Vlachadis Castles A. Women in cardiology in Australia-are we making any progress? Heart Lung Circ. (2019) 28:690–6. doi: 10.1016/j.hlc.2018.12.010
29. Association of American Medical Colleges. Radiology-Diagnostic. ERAS 2014. Washington, DC: AAMC (2018).
30. Raymundo-Martínez G, Alanis-Estrada G, Araiza-Garaygordobil D, Delgado-Cruz IV, Gopar-Nieto R, Cabello-López A, et al. Gender differences in cardiology professionals: a Latin American survey. Arch Cardiol Mex. (2022) 92:11–8. doi: 10.24875/ACME.M22000294
31. Farhan H, Dakhil Z. Women in cardiology: critical status and a call to move forward. Egypt Heart J. (2020) 72:45. doi: 10.1186/s43044-020-00078-w
32. Kubik-Huch R, Vilgrain V, Krestin G, Reiser M, Attenberger U, Muellner A, et al. Women in radiology: gender diversity is not a metric-it is a tool for excellence. Eur Radiol. (2020) 30:1644–52. doi: 10.1007/s00330-019-06493-1
33. Timmis A, Baker C, Banerjee S, Calver A, Dornhorst A, English K, et al. Women in UK cardiology: report of a Working Group of the British cardiac society. Heart. (2005) 91:283–9. doi: 10.1136/hrt.2004.047340
34. Douglas P, Rzeszut A, Bairey Merz C, Duvernoy C, Lewis S, Walsh M, et al. Career preferences and perceptions of cardiology among US internal medicine trainees: factors influencing cardiology career choice. JAMA Cardiol. (2018) 3:682–91. doi: 10.1001/jamacardio.2018.1279
35. Yazdani M, Kotronias R, Joshi A, Camm C, Allen C. British cardiology training assessed. Eur Heart J. (2019) 40:2475–7. doi: 10.1093/eurheartj/ehz545
36. Fukue N, Ishida M, Taniyama M, Mukai-Yatagai N, Sakamoto T, Tamada T, et al. Current diversity issues in cardiovascular workplaces in the chugoku district results from 2 questionnaire surveys. Circ Rep. (2022) 4:59–65. doi: 10.1253/circrep.CR-21-0111
37. Bin Dahmash A, Alorfi F, Alharbi A, Aldayel A, Kamel A, Almoaiqel M. Burnout phenomenon and its predictors in radiology residents. Acad Radiol. (2020) 27:1033–9. doi: 10.1016/j.acra.2019.09.024
38. Stentz N, Griffith K, Perkins E, Jones R, Jagsi R. Fertility and childbearing among American female physicians. J Womens Health. (2016) 25:1059–65. doi: 10.1089/jwh.2015.5638
39. Guenette J, Smith S. Burnout: prevalence and associated factors among radiology residents in New England with comparison against United States resident physicians in other specialties. Am J Roentgenol. (2017) 209:136–41. doi: 10.2214/AJR.16.17541
40. Mehta L, Lewis S, Duvernoy C, Rzeszut A, Walsh M, Harrington R, et al. Burnout and career satisfaction among U.S. Cardiologists. J Am Coll Cardiol. (2019) 73:3345–8. doi: 10.1016/j.jacc.2019.04.031
41. Kane L. Physician Burnout & Depression Report 2022: Stress, Anxiety, and Anger. The Heart.org Medscape Cardiology (2022). Available online at: https://www.medscape.com/slideshow/2022-lifestyle-burnout-6014664 (accessed Jun 12, 2022).
42. Curtis A, Rodriguez F. Choosing a career in cardiology: where are the women? JAMA Cardiol. (2018) 3:691–2. doi: 10.1001/jamacardio.2018.1286
43. Sharma G, Douglas P, Hayes S, Mehran R, Rzeszut A, Harrington R, et al. Global prevalence and impact of hostility, discrimination, and harassment in the cardiology workplace. J Am Coll Cardiol. (2021) 77:2398–409. doi: 10.1016/j.jacc.2021.03.301
44. Jaijee S, Kamau-Mitchell C, Mikhail G, Hendry C. Sexism experienced by consultant cardiologists in the United Kingdom. Heart. (2021) 107:895–901. doi: 10.1136/heartjnl-2020-317837
45. Lewis S, Mehta L, Douglas P, Gulati M, Limacher M, Poppas A, et al. Changes in the professional lives of cardiologists over 2 decades. J Am Coll Cardiol. (2017) 69:452–62. doi: 10.1016/j.jacc.2016.11.027
46. Files J, Mayer A, Ko M, Friedrich P, Jenkins M, Bryan M, et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias. J Womens Health. (2017) 26:413–9. doi: 10.1089/jwh.2016.6044
47. Kittleson M. The trials of women in cardiology. J Am Coll Cardiol. (2020) 76:1931–3. doi: 10.1016/j.jacc.2020.09.014
48. Camm C, Joshi A, Moore A, Sinclair H, Westwood M, Greenwood J, et al. Bullying in UK cardiology: a systemic problem requiring systemic solutions. Heart. (2022) 108:212–8. doi: 10.1136/heartjnl-2021-319882
49. Salles A, Choo E. Queen bee phenomenon: a consequence of the hive. Lancet. (2020) 395:940. doi: 10.1016/S0140-6736(20)30597-3
50. Sarma A, Nkonde-Price C, Gulati M, Duvernoy C, Lewis S, Wood M. Cardiovascular medicine and society: the pregnant cardiologist. J Am Coll Cardiol. (2017) 69:92–101. doi: 10.1016/j.jacc.2016.09.978
51. Lau E, Wood M. How do we attract and retain women in cardiology? Clin Cardiol. (2018) 41:264–8. doi: 10.1002/clc.22921
52. Gulati M, Korn R, Wood M, Sarma A, Douglas P, Singh T, et al. Childbearing among women cardiologists: the interface of experience, impact, and the law. J Am Coll Cardiol. (2022) 79:1076–87. doi: 10.1016/j.jacc.2021.12.034
53. Au S, Bellato V, Carvas J, Córdoba C, Daudu D, Dziakova J, et al. Global parental leave in surgical careers: differences according to gender, geographical regions and surgical career stages. Br J Surg. (2021) 108:1315–22. doi: 10.1093/bjs/znab275
54. Best P, Skelding K, Mehran R, Chieffo A, Kunadian V, Madan M, et al. SCAI consensus document on occupational radiation exposure to the pregnant cardiologist and technical personnel. EuroIntervention. (2011) 6:866–74. doi: 10.4244/EIJV6I7A148
55. Wood A, Hussain S. Working with radiation in pregnancy: a guide for cardiologists. Heart. (2021) 107:1182–3. doi: 10.1136/heartjnl-2021-318993
56. Jolly S, Griffith K, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. (2014) 160:344–53. doi: 10.7326/M13-0974
57. Tsukada Y, Tokita M, Kato K, Kato Y, Miyauchi M, Ono I, et al. Solutions for retention of female cardiologists: from the survey of gender differences in the work and life of cardiologists. Circ J. (2009) 73:2076–83. doi: 10.1253/circj.CJ-09-0206
58. Vlachadis Castles A, Burgess S, Robledo K, Beale A, Biswas S, Segan L, et al. Work-life balance: a comparison of women in cardiology and other specialties. Open Heart. (2021) 8:e001678. doi: 10.1136/openhrt-2021-001678
59. Dobson R, Joshi A, Allen C, Sinclair H. Less than full-time training in cardiology. Heart. (2019) 105:1445–6. doi: 10.1136/heartjnl-2019-315226
60. Lerchenmüller C, Lerchenmueller M, Sorenson O. Long-term analysis of sex differences in prestigious authorships in cardiovascular research supported by the National Institutes of Health. Circulation. (2018) 137:880–2. doi: 10.1161/CIRCULATIONAHA.117.032325
61. Holman L, Stuart-Fox D, Hauser C. The gender gap in science: how long until women are equally represented? PLoS Biol. (2018) 16:e2004956. doi: 10.1371/journal.pbio.2004956
62. Blumenthal D, Olenski A, Yeh R, DeFaria Yeh D, Sarma A, Stefanescu Schmidt A, et al. Sex differences in faculty rank among academic cardiologists in the United States. Circulation. (2017) 135:506–17. doi: 10.1161/CIRCULATIONAHA.116.023520
63. Chatterjee P, Werner R. Gender disparity in citations in high-impact journal articles. JAMA Netw Open. (2021) 4:e2114509. doi: 10.1001/jamanetworkopen.2021.14509
64. Whitelaw S, Thabane L, Mamas M, Reza N, Breathett K, Douglas P, et al. Characteristics of Heart failure trials associated with under-representation of women as lead authors. J Am Coll Cardiol. (2020) 76:1919–30. doi: 10.1016/j.jacc.2020.08.062
65. Rai D, Kumar A, Waheed S, Pandey R, Guerriero M, Kapoor A, et al. Gender differences in international cardiology guideline authorship: a comparison of the US, Canadian, and European cardiology guidelines from 2006 to 2020. J Am Heart Assoc. (2022) 11:e024249. doi: 10.1161/JAHA.121.024249
66. Tong I, Griffin B, Trott J, Romano M, Stein A, Madsen T. The proportion of women authors and the inclusion of sex and gender content among the American college of cardiology clinical practice guidelines, 2008-2018. J Womens Health. (2021) 30:1616–25. doi: 10.1089/jwh.2020.8454
67. Jagsi R, Griffith K, Jones R, Stewart A, Ubel P. Factors associated with success of clinician-researchers receiving career development awards from the National institutes of health: a longitudinal cohort study. Acad Med. (2017) 92:1429–39. doi: 10.1097/ACM.0000000000001728
68. Kapoor N, Blumenthal D, Smith S, Ip I, Khorasani R. Sex differences in radiologist salary in U.S. public medical schools. Am J Roentgenol. (2017) 209:953–8. doi: 10.2214/AJR.17.18256
69. Jagsi R, Biga C, Poppas A, Rodgers G, Walsh M, White P, et al. Work activities and compensation of male and female cardiologists. J Am Coll Cardiol. (2016) 67:529–41. doi: 10.1016/j.jacc.2015.10.038
70. Biden J. Executive Order on Diversity, Equity, Inclusion, and Accessibility in the Federal Workforce. Washington, DC (2021). Available online at: https://www.whitehouse.gov/briefing-room/presidential-actions/2021/06/25/executive-order-on-diversity-equity-inclusion-and-accessibility-in-the-federal-workforce/ (accessed October 4, 2022).
71. Baker S, Barry M, Chaudhry H, Hubbi B. Women as radiologists: are there barriers to entry and advancement? J Am Coll Radiol. (2006) 3:131–4. doi: 10.1016/j.jacr.2005.10.001
72. Sharma G, Sarma A, Walsh M, Hayes S, Sahni S, Brown S, et al. 10 recommendations to enhance recruitment, retention, and career advancement of women cardiologists. J Am Coll Cardiol. (2019) 74:1839–42. doi: 10.1016/j.jacc.2019.08.016
73. Jones Y, Durand V, Morton K, Ottolini M, Shaughnessy E, Spector N, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. (2020) 15:507–9. doi: 10.12788/jhm.3470
74. Nishida S, Nagaishi K, Motoya M, Kumagai A, Terada N, Kasuga A, et al. Dilemma of physician-mothers faced with an increased home burden and clinical duties in the hospital during the COVID-19 pandemic. PLoS One. (2021) 16:e0253646. doi: 10.1371/journal.pone.0253646
75. Gaetke-Udager K, Knoepp U, Maturen K, Leschied J, Chong S, Klein K, et al. A women in radiology group fosters career development for faculty and trainees. Am J Roentgenol. (2018) 211:W47–51. doi: 10.2214/AJR.17.18994
76. Sharma G, Lewis S, Singh T, Mehta L, Mieres J, Poppas A, et al. The pivotal role of women in cardiology sections in medical organizations: from leadership training to personal enrichment. CJC Open. (2021) 3(12 Suppl.):S95–101. doi: 10.1016/j.cjco.2021.07.015
77. Focus. Center for Clinical Epidemiology and Biostatistics (CCEB) at the University of Pennsylvania Perelman School of Medicine (PSOM). FOCUS On Health & Leadership for Women. (2004). Available online at: https://www.focusprogram.org/ (accessed June 22, 2022).
78. American Society of Echocardiography. ASE Past Presidents. Durham, NC: American Society of Echocardiography (2022).
79. American Society of Echocardiography. ASE Board of Directors. Durham, NC: American Society of Echocardiography (2022).
80. Society for Cardiovascular Magnetic Resonance. SCMR Past Presidents. (2022). Available online at: https://scmr.org/page/PastPresidents/Past-Presidents.htm (accessed June 27, 2022).
81. Society for Cardiovascular Magnetic Resonance. SCMR Committees. (2022). Available online at:https://scmr.org/page/SCMRCommittees (accessed June 27, 2022).
82. American Society of Echocardiography. ASE Committees. (2022). Available online at:https://www.asecho.org/about-ase/standing-committees-and-councils/ (accessed June 27, 2022).
83. North American Society for Cardiovascular Imaging. NASCI Committees. (2022). Available online at: https://nasci.org/about-nasci/committees/ (accessed June 27, 2022).
84. North American Society for Cardiovascular Imaging. NASCI Past Presidents. (2022). Available online at: https://nasci.org/about-nasci/past-presidents/ (accessed June 27, 2022).
85. North American Society for Cardiovascular Imaging. NASCI Executive Committee. East Dundee, IL: NASCT (2022).
86. American Society of Nuclear Cardiology. ASNC Board of Directors. (2022). Available online at: https://www.asnc.org/governance (accessed June 27, 2022).
87. American Society of Nuclear Cardiology. ASNC Committees. (2022). Available online at: https://www.asnc.org/committees (accessed June 27, 2022).
88. Society of Cardiovascular Computed Tomography. SCCT Past Presidents. (2022). Available online at: https://scct.org/page/PastPresidents (accessed June 27, 2022).
89. Society of Cardiovascular Computed Tomography. SCCT Committees & Board of Directors. (2022). Available online at: https://scct.org/page/About_SCCT#a4 (accessed June 27, 2022).
90. Ordovas K, Baldassarre L, Bucciarelli-Ducci C, Carr J, Fernandes J, Ferreira V, et al. Cardiovascular magnetic resonance in women with cardiovascular disease: position statement from the society for cardiovascular magnetic resonance (SCMR). J Cardiovasc Magn Reson. (2021) 23:52. doi: 10.1186/s12968-021-00746-z
91. Assomull R, Lyne J, Keenan N, Gulati A, Bunce N, Davies S, et al. The role of cardiovascular magnetic resonance in patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Eur Heart J. (2007) 28:1242–9. doi: 10.1093/eurheartj/ehm113
92. Cardona A, Zareba K, Raman SV. The role of stress cardiac magnetic resonance in women. J Nucl Cardiol. (2016) 23:1036–40. doi: 10.1007/s12350-016-0597-x
93. Markousis-Mavrogenis G, Bonou M, Vartela V, Kolovou G, Venetsanopoulou A, Markatseli T, et al. Cardiovascular magnetic resonance detects inflammatory cardiomyopathy in symptomatic patients with inflammatory joint diseases and a normal routine workup. J Clin Med. (2022) 11:1428. doi: 10.3390/jcm11051428
94. Lagan J, Schmitt M, Miller C. Clinical applications of multi-parametric CMR in myocarditis and systemic inflammatory diseases. Int J Cardiovasc Imaging. (2018) 34:35–54. doi: 10.1007/s10554-017-1063-9
95. Soufer A, Baldassarre L. The role of cardiac magnetic resonance imaging to detect cardiac toxicity from cancer therapeutics. Curr Treat Options Cardiovasc Med. (2019) 21:28. doi: 10.1007/s11936-019-0732-5
96. Saunderson C, Plein S, Manisty C. Role of cardiovascular magnetic resonance imaging in cardio-oncology. Eur Heart J Cardiovasc Imaging. (2021) 22:383–96. doi: 10.1093/ehjci/jeaa345
97. Brown S, Sparapani R, Osinski K, Zhang J, Blessing J, Cheng F, et al. Establishing an interdisciplinary research team for cardio-oncology artificial intelligence informatics precision and health equity. Am Hear J plus Cardiol Res Pract. (2022) 13:100094. doi: 10.1016/j.ahjo.2022.100094
98. Blakemore E. Women are Still Underrepresented in Clinical Trials. Washington, D.C: Washington Post (2022).
99. Bierer B, Meloney L, Ahmed H, White S. Advancing the inclusion of underrepresented women in clinical research. Cell Rep Med. (2022) 3:100553. doi: 10.1016/j.xcrm.2022.100553
100. Bird C. Women and health research: ethical and legal issues of including women in clinical studies: Volume 2: Workshop and commissioned papers. In: Mastroianni A, Faden R, Federman D editors. Women’s Representation as Subjects in Clinical Studies: A Pilot Study of Research Published in JAMA in 1990 and 1992. Washington, DC: National Academies Press (1999). p. 151–73.
Keywords: women, cardiovascular MRI, cardiovascular imaging, gender diversity, leadership, CMR, inclusion, equity
Citation: Sierra-Galan LM, Aggarwal NR, Stojanovska J, Raman SV, Han Y, Ferreira VM, Thomas K, Seiberlich N, Parwani P, Bucciarelli-Ducci C, Baldassarre LA, Mavrogeni S, Ordovas K, Schulz-Menger J and Bandettini WP (2023) Women physicians in cardiovascular magnetic resonance: Past, present, and future. Front. Cardiovasc. Med. 9:984326. doi: 10.3389/fcvm.2022.984326
Received: 01 July 2022; Accepted: 12 December 2022;
Published: 04 January 2023.
Edited by:
Adelina Doltra, Hospital Clinic of Barcelona, SpainReviewed by:
Sarah Moharem-Elgamal, NIHR Bristol Cardiovascular Biomedical Research Unit, United KingdomCopyright © 2023 Sierra-Galan, Aggarwal, Stojanovska, Raman, Han, Ferreira, Thomas, Seiberlich, Parwani, Bucciarelli-Ducci, Baldassarre, Mavrogeni, Ordovas, Schulz-Menger and Bandettini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lilia M. Sierra-Galan, ✉ bGlsaXNpZXJyYUB3ZGV2ZWwubmV0; W. Patricia Bandettini, ✉ aW5na2FuaXNvcm5AbmloLmdvdg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.