
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 08 September 2022
Sec. Heart Failure and Transplantation
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.967780
 Zhican Liu1,2††
Zhican Liu1,2†† Yiqun Peng1†
Yiqun Peng1† Wenjiao Zhao1†
Wenjiao Zhao1† Yunlong Zhu1
Yunlong Zhu1 Mingxin Wu1
Mingxin Wu1 Haobo Huang1
Haobo Huang1 Ke Peng3
Ke Peng3 Lingling Zhang1
Lingling Zhang1 Sihao Chen1,2
Sihao Chen1,2 Xin Peng1,2
Xin Peng1,2 Na Li1,2
Na Li1,2 Hui Zhang1,2
Hui Zhang1,2 Yuying Zhou1,2
Yuying Zhou1,2 Yongliang Chen1,2
Yongliang Chen1,2 Sha Xiao1,2
Sha Xiao1,2 Jie Fan1
Jie Fan1 Jianping Zeng1,2*†
Jianping Zeng1,2*†Background: High body mass index increases the risk of heart failure morbidity and mortality. It is unclear whether a high body mass index is associated with prognosis in patients with heart failure with mildly reduced left ventricular ejection fraction (HFmrEF). We retrospectively analyzed the effect of a high body mass index on the prognosis of patients with HFmrEF.
Methods: We investigated the association between body mass index and cardiovascular death (death from any cardiovascular mechanism) in 1,691 HFmrEF patients (mean age, 68 years; 35% female) in Xiangtan Central Hospital. Using Cox proportional hazards models, body mass index was assessed as a continuous and a categorical variable.
Results: Cardiovascular death occurred in 133 patients (82 males and 51 females) after 1 year of follow-up. After adjustment for established risk factors, there was a 7.5% increase in the risk of cardiovascular death for females for each increment of 1 in BMI. In contrast, changes in male body mass index were not significantly associated with cardiovascular death (P = 0.097). Obese subjects had a 1.8-fold increased risk of cardiovascular death compared with subjects with a normal body mass index. The hazard ratio for females was 2.163 (95% confidence interval: 1.150–4.066). Obesity was not significantly associated with cardiovascular death in males (P = 0.085).
Conclusion: An increased body mass index is associated with an increased risk of cardiovascular death in patients with HFmrEF; however, this risk was mainly associated with female patients with HFmrEF and less with male patients with HFmrEF.
The global obesity epidemic is a significant public health concern (1). Approximately 39–49% of adults are overweight or obese (2). Cardiovascular disease (CVD) accounts for more than two-thirds of deaths due to a high body mass index (BMI) (3). Numerous studies have identified obesity as a significant risk factor for hypertension, CVD, and left ventricular hypertrophy. These are all important risk factors for heart failure (HF) (4, 5). HF is also a global epidemic that places enormous pressure on patients, caregivers, and the healthcare system (6, 7). Currently, patients with HF are classified as having reduced ejection fraction (HFrEF; LVEF ≤ 40%), mildly reduced ejection fraction (HFmrEF; LVEF 41–49%), or preserved ejection fraction (HFpEF; LVEF ≥50%) (8). Recent studies have shown that a higher BMI is more strongly associated with HFpEF risk than HFrEF (9), and since there are no studies on the association between BMI and patients with HFmrEF, it is unclear whether high BMI affects the prognosis of HFmrEF patients. Therefore, we retrospectively analyzed the effect of BMI on outcome events in patients with HFmrEF.
According to the World Health Organization (WHO) criteria, BMI is divided into underweight (BMI <18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), and obesity (BMI ≥ 30 kg/m2) (10). Therefore, we included patients with a BMI of 18.5–24.9 kg/m2 (normal weight) as the reference group based on accumulated epidemiological evidence (11).
The study protocol was approved by the Ethics Committee of the Xiangtan Central Hospital (Xiangtan, China) and conformed to the principles outlined in the Declaration of Helsinki (12). Informed consent was obtained from all patients or their guardians before the study protocol was initiated. The requirement for written informed consent was waived because of the retrospective nature of the study, and only oral or telephonic consent was obtained. This study was based on the Outcome of Discharged HFmrEF Patients (OUDI-HF; ClinicalTrials.gov, number NCT05240118). The OUDI-HF study included 1,691 patients with HFmrEF who were admitted to our hospital between January 1, 2015, and August 31, 2020. Inclusion criteria included patients with HF with an LVEF of 41%−49% and a New York Heart Association HF score between II and IV. We are using Simpson's method to calculate the ejection fraction. The exclusion criteria were malignancies or other non-cardiac diseases with an expected survival of <1 year. After excluding 56 underweight patients, 966 were normal weight, 269 were overweight, and 400 were obese (Figure 1).
Demographic and procedural data were collected from hospital charts or databases. All study participants were followed-up on August 31, 2021. A panel of seven experienced physicians reviewed suspected cardiovascular events by examining the information obtained from hospital records and follow-ups, including clinical telephone interviews and community visits. In this investigation, the primary outcome of interest was cardiovascular death 1 year after discharge. Cardiovascular death was defined as “death from any cardiovascular mechanism, including acute myocardial infarction, sudden cardiac death, heart failure, stroke, cardiovascular surgery, cardiovascular hemorrhage, and other cardiovascular causes”.
We used the Cox proportional hazards regression models stratified by cohort to examine the association of BMI and incidence of cardiovascular death. Sex-specific and sex-stratified analyses were performed. BMI was assessed as a continuous variable (increased risk was calculated for each increase of 1) and as a categorical variable. We adjusted for the following baseline covariates: age, smoking status, alcohol use, hypertension, hyperlipidemia, diabetes, coronary heart disease, atrial fibrillation, previous stroke, chronic obstructive pulmonary disease, renal insufficiency, New York Heart Association functional class, myocardial infarction, and percutaneous coronary intervention.
Clinical characteristics between the groups were compared using t-tests for continuous variables and chi-squared tests for categorical variables. The Kaplan–Meier method was used to estimate the incidence of cumulative events. P-values were obtained using the Kruskal–Wallis rank-sum test for continuous variables and the Fisher's exact probability test for count variables. The results were considered significant when the P-value was P < 0.05. All analyses were performed using R (http://www.R-project.org) and EmpowerStats (www.empowerstats.com, X & Y Solutions, Inc. Boston MA).
Approximately 17% of the males and 15% of the females were overweight. The prevalence of obesity was ~23% in males and 26% in females. Females had higher rates of hypertension and diabetes than did males (Table 1).
After 1 year of follow-up, cardiovascular death occurred in 133 participants (82 males and 51 females). The crude cumulative incidence (Figure 2) and age-adjusted incidence rates (Table 2) of cardiovascular deaths increased across the female's BMI categories. In contrast, changes in male BMI were not significantly associated with cardiovascular death.
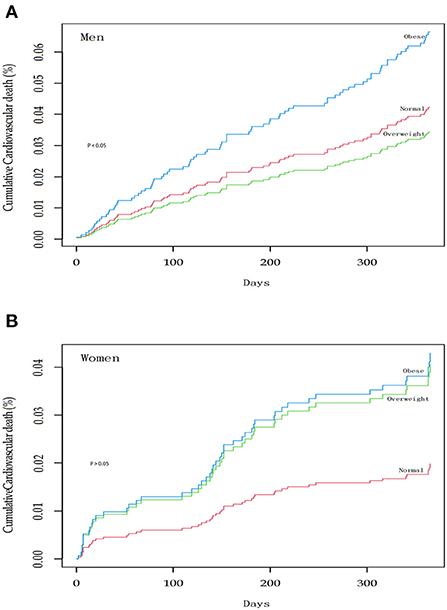
Figure 2. Cumulative incidence of 1-year cardiovascular death according to category of body-mass index at the base-line examination. The body-mass index was 18.5–24.9 in normal subjects, 25.0–29.9 in overweight subjects, and 30.0 or more in obese subjects. (A) One-year cumulative cardiovascular death in men. (B) One-year cumulative cardiovascular death in women.
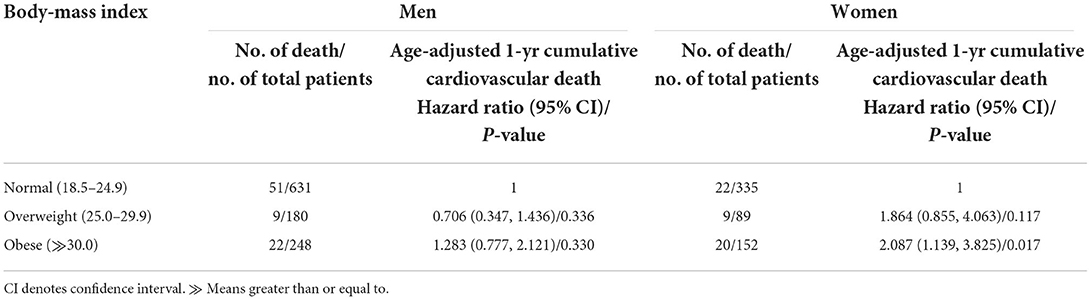
Table 2. Cumulative incidence of cardiovascular death among study participants according to the category of body-mass index at base line.
After adjusting for age, an increase of 1 in BMI was associated with a 4.8% increase in the overall risk of cardiovascular death [hazard ratio (HR) 1.048; 95% confidence interval (95% CI) 1.004–1.095; P = 0.033]. Among them, the risk of cardiovascular death was increased by 7.1% in females (HR 1.071; 95% CI 1.002–1.144; P = 0.042), and the association between changes in BMI and cardiovascular death in males was not significant (HR 1.029; 95% CI 0.971–1.090; P = 0.334) (Table 3, Model IA). There was no difference in the odds of cardiovascular death between overweight subjects and subjects with a normal BMI (P > 0.05). Obesity had a 57% increased risk of cardiovascular death (HR 1.570; 95% CI 1.073–2.298; P = 0.020), including a 108.7% increase in females (HR 2.087; 95% CI 1.139–3.825; P = 0.017), and males were not associated with cardiovascular death (HR, 1.283; 95% CI 0.777–2.121; P = 0.330) (Table 3, Model IB).
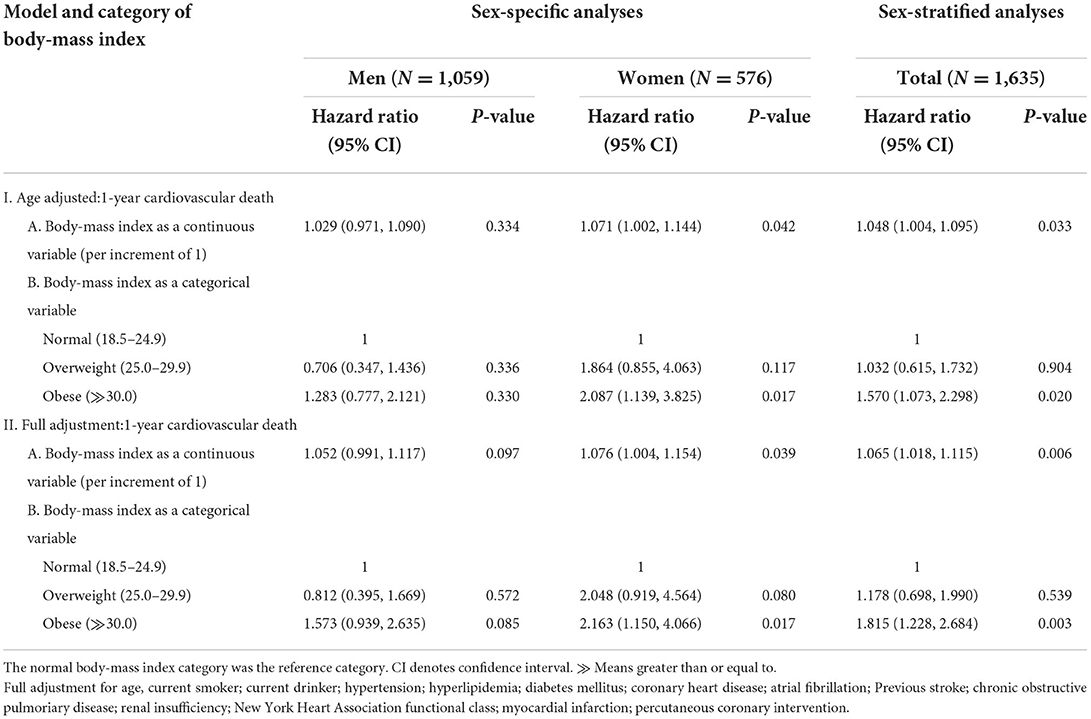
Table 3. Results of multivariable cox proportional-hazards models examining the relation of body-mass index to the risk of heart failure.
After adjusting for all covariates, a BMI increase of 1 was associated with a 6.5% increase in the overall risk of cardiovascular death (HR 1.065; 95% CI 1.018–1.115; P = 0.006). Among them, the risk of cardiovascular death was increased by 7.6% in females (HR 1.076; 95% CI 1.004–1.154; P = 0.039), and the change in BMI was not significantly associated with cardiovascular death in males (HR 1.052; 95% CI 0.991–1.117; P = 0.097) (Figure 3 and Table 3, Model IIA). There was no difference in the odds of cardiovascular death among overweight subjects compared to those with a normal BMI (P > 0.05). The risk of cardiovascular death was increased by 81.5% in obese individuals (HR 1.815; 95% CI 1.228–2.684; P = 0.003), including 116.3% in females (HR 2.163; 95% CI 1.150–4.066; P = 0.017), whereas males were not associated with cardiovascular death (HR 1.573; 95% CI 0.939–2.635; P = 0.085) (Figure 3 and Table 3, Model IIB).
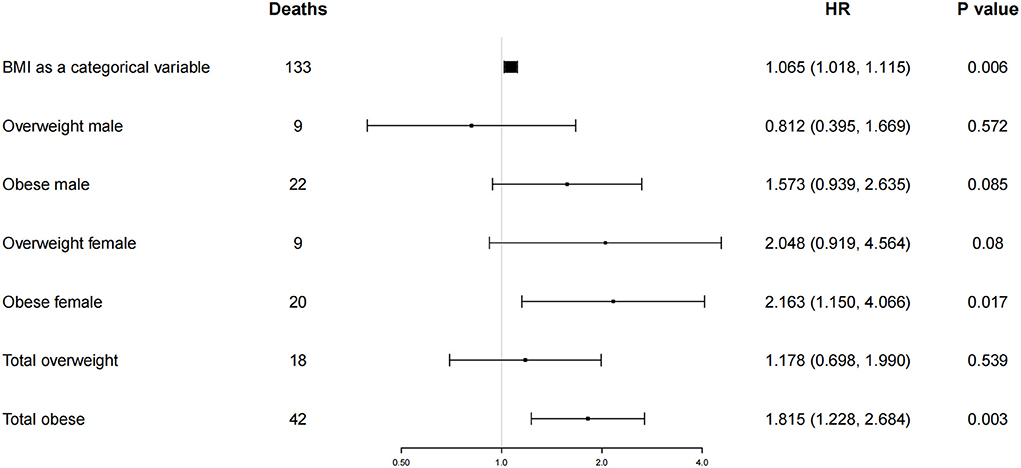
Figure 3. Risk of cardiovascular death in overweight and obese subjects according to body mass index category at baseline examination. I bars represent the 95 percent confidence intervals for the hazard ratios. Hazard ratios were adjusted for age, smoking status, alcohol use, hypertension, hyperlipidemia, diabetes, coronary heart disease, atrial fibrillation, previous stroke, chronic obstructive pulmonary disease, renal insufficiency, New York Heart Association functional class, myocardial infarction, and percutaneous coronary intervention at base line. Normal weight (body-mass index,18.5 to 24.9) was the reference category.
This study found that high BMI increased 1 year cardiovascular mortality in female patients with HFmrEF after adjusting for covariates. However, increased BMI was not associated with 1-year cardiovascular mortality in male HFmrEF patients.
Recent studies have shown that a higher BMI is more strongly associated with HFpEF risk than HFrEF (9), and other studies have confirmed this view (13). Participants with overweight and grade 1 obesity (BMI: 30.0–34.9 kg/m2) had a 38% and 56% higher risk of HFpEF (13), respectively. However, there are also different findings called the obesity paradox. These studies suggest that overweight or grade 1 obese patients have better clinical outcomes than normal weight patients with HF, which is more common in patients with HFrEF than in those with HFpEF (4, 5, 14). This may be related to lower epicardial adipose tissue in normal-weight HF patients, which increases the risk of death in HF patients (15–17). However, there are also different views. The Metabolic Exercise test data combined with Cardiac and Kidney Indexes (MECKI) Score Research Group found that the obesity paradox in HFrEF patients may be related to patient selection bias (18). This paradox may disappear after considering exercise capacity and other cardiopulmonary exercise test variables. The studies mentioned above, as well as ours, have demonstrated a correlation between HF and BMI. Nevertheless, the difference is that other studies have failed to explain the relationship between HFmrEF and BMI, while our study focused on the effect of BMI on the prognosis of patients with HFmrEF.
Despite the obesity paradox, weight loss is still recommended in patients with HF (19–23). Obesity is not only associated with diseases of the cardiovascular system, but also with diseases such as stroke, venous thromboembolic disease, and pulmonary hypertension (24, 25). Numerous studies have identified obesity as a significant risk factor for hypertension, CVD, and left ventricular hypertrophy. However, hypertension, CVD, and left ventricular hypertrophy are also important risk factors for HF development (4, 5). The Framingham Heart Study found that, with increasing BMI, the incidence of HF increased in both males and females (26). Several studies have confirmed this finding (15, 27). Studies on bariatric surgery have shown improved left ventricular systolic function in patients with post-operative HF (28, 29) and a reduction in HF hospitalizations (30). At the same time, the HF guidelines also consider a high risk associated with severe obesity (8).
This study had several limitations. First, this was a retrospective study to minimize bias in patient selection; however, unobserved confounders remained. Second, our study exclusively recruited patients from China from an isolated population at a local heart center, thereby lacking the diversity to justify the uniformity of the findings. Lastly, data from patients undergoing long-term treatment for heart disease with statins, renin/angiotensin blockers, and beta-blockers were not included in the protocol for this study. We were unable to assess the effects of these drugs or their effects on the long-term morbidity and mortality of the enrolled subjects.
The present study found that obesity increased the1year risk of cardiovascular death in females with HFmrEF (per an increase of 1 in the BMI in female patients, the risk of death increased by 7.6%, and the risk of death in obese patients was twice that of normal-weight patients), but not in males. Further research is warranted to understand complex sex-related risk differences among patients with HFmrEF. A better understanding of sex-specific risk factors may help in developing strategies to improve outcomes for this critical disease.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Xiangtan Central Hospital (No.20211036). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
ZL, YP, and WZ established the idea to study the heart failure with mildly reduced ejection fraction in Chinese population, and helped in writing main ideas for this research, main results and discussion of the findings. ZL was a major contributor in writing the manuscript. YZhu, MW, HH, KP, LZ, and JF interpreted statistical analysis and conducted multivariate analysis to prove the main findings of this project. SC, XP, NL, HZ, YZho, YC, and SX collected data and followed-up. JZ contributed on editing this manuscript and giving advice for the main authors to organize the manuscript and ideas of the project. All authors contributed to the article and approved the submitted version.
This study was supported by Scientific Bureau of Xiangtan City (SF-YB20201023), Xiangtan City, Hunan Province, China and Committee of Development and Reform of Hunan Province (2019-875), Changsha, Hunan Province, China. The funders had no roles in study design, data collection and analysis, decision to publish or preparation of the manuscript.
We thank Joshua Anthony (http://app.editage.com/) for editing the English text of a draft of this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.967780/full#supplementary-material
1. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. (2016) 387:1377–96. doi: 10.1016/S0140-6736(16)30054-X
2. Maffetone PB, Rivera-Dominguez I, Laursen PB. Overfat and underfat: new terms and definitions long overdue. Front Public Health. (2017) 4:279. doi: 10.3389/fpubh.2016.00279
3. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. (2017) 377:13–27. doi: 10.1056/NEJMoa1614362
4. Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Reprint of: healthy weight and obesity prevention. J Am Coll Cardiol. (2018) 72:3027–52. doi: 10.1016/j.jacc.2018.10.024
5. Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. (2018) 61:142–50. doi: 10.1016/j.pcad.2018.07.003
6. Savarese G, Lund LH, Department Department Of Cardiology KUHS Division Division Of Cardiology DOMK. Global public health burden of heart failure. Card Fail Rev. (2017) 3:7–11. doi: 10.15420/cfr.2016:25:2
7. Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: Preventing disease and death worldwide. ESC Heart Fail. (2014) 1:4–25. doi: 10.1002/ehf2.12005
8. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure. J Am Coll Cardiol. (2022) 79:e263–421. doi: 10.1016/j.jacc.2021.12.012
9. Pandey A, Patel KV, Vaduganathan M, Sarma S, Haykowsky MJ, Berry JD, et al. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC Heart Fail. (2018) 6:975–82. doi: 10.1016/j.jchf.2018.09.006
10. Jensen MDDH. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. J Am Coll Cardiol. (2014) 63:2985–3023. doi: 10.1016/j.jacc.2013.11.004
11. Berrington DGA, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. (2010) 363:2211–9. doi: 10.1056/NEJMoa1000367
12. World Medical Association. World Medical association declaration of helsinki ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
13. Pandey AM, LaMonte MPM, Klein LMM, Ayers CM, Psaty BMMP, Eaton CBMM, et al. Relationship between physical activity, body mass index, and risk of heart failure. J Am Coll Cardiol. (2017) 69:1129–42. doi: 10.1016/j.jacc.2016.11.081
14. Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. (2018) 61:151–6. doi: 10.1016/j.pcad.2018.05.005
15. Bozkurt B, Aguilar D, Deswal A, Dunbar SB, Francis GS, Horwich T, et al. Contributory risk and management of comorbidities of hypertension, obesity, diabetes mellitus, hyperlipidemia, and metabolic syndrome in chronic heart failure: a scientific statement from the american heart association. Circulation. (2016) 134:e535–78. doi: 10.1161/CIR.0000000000000450
16. Futter JE, Cleland JGF, Clark AL. Body mass indices and outcome in patients with chronic heart failure. Eur J Heart Fail. (2011) 13:207–13. doi: 10.1093/eurjhf/hfq218
17. Doesch C, Suselbeck T, Leweling H, Fluechter S, Haghi D, Schoenberg SO, et al. Bioimpedance analysis parameters and epicardial adipose tissue assessed by cardiac magnetic resonance imaging in patients with heart failure. Obesity. (2010) 18:2326–32. doi: 10.1038/oby.2010.65
18. Piepoli MF, Corrà U, Veglia F, Bonomi A, Salvioni E, Cattadori G, et al. Exercise tolerance can explain the obesity paradox in patients with systolic heart failure: data from the MECKI Score Research Group. Eur J Heart Fail. (2016) 18:545–53. doi: 10.1002/ejhf.534
19. McDowell K, Petrie MC, Raihan NA, Logue J. Effects of intentional weight loss in patients with obesity and heart failure: a systematic review. Obes Rev. (2018) 19:1189–204. doi: 10.1111/obr.12707
20. Karwi QG, Zhang L, Altamimi TR, Wagg CS, Patel V, Uddin GM, et al. Weight loss enhances cardiac energy metabolism and function in heart failure associated with obesity. Diabetes Obesity Metab. (2019) 21:1944–55. doi: 10.1111/dom.13762
21. Lavie CJ, Ventura HO. Clinical implications of weight loss in heart failure. J Card Fail. (2014) 20:190–2. doi: 10.1016/j.cardfail.2014.01.002
22. Tabucanon T, Wilcox J, Tang WHW. Does weight loss improve clinical outcomes in overweight and obese patients with heart failure? Curr Diabetes Rep. (2020) 20. doi: 10.1007/s11892-020-01367-z
23. Lavie CJ, Alpert MA, Ventura HO. Risks and benefits of weight loss in heart failure. Heart Fail Clin. (2015) 11:125–31. doi: 10.1016/j.hfc.2014.08.013
24. Heit JA, Spencer FA, White RH. The epidemiology of venous thromboembolism. J Thromb Thrombolys. (2016) 41:3–14. doi: 10.1007/s11239-015-1311-6
25. Rahmani J, Haghighian Roudsari A, Bawadi H, Thompson J, Khalooei Fard R, Clark C, et al. Relationship between body mass index, risk of venous thromboembolism and pulmonary embolism: a systematic review and dose-response meta-analysis of cohort studies among four million participants. Thromb Res. (2020) 192:64–72. doi: 10.1016/j.thromres.2020.05.014
26. Kenchaiah SEJB. Obesity and the risk of heart failure. N Engl J Med. (2002) 347:305–13. doi: 10.1056/NEJMoa020245
27. Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference, and Waist-to-Hip ratio on the risk of heart failure. Circulation. (2010) 121:237–44. doi: 10.1161/CIRCULATIONAHA.109.887893
28. Koshino Y, Villarraga HR, Somers VK, Miranda WR, Garza CA, Hsiao J, et al. Changes in myocardial mechanics in patients with obesity following major weight loss after bariatric surgery. Obesity. (2013) 21:1111–8. doi: 10.1002/oby.20168
29. Marcela Rodriguez Flores CASM, Poirier AP. Effect of bariatric surgery on heart failure. Expert Rev Cardiovasc Ther. (2017) 15:567–79. doi: 10.1080/14779072.2017.1352471
Keywords: cardiovascular, mortality, body mass index, obese, heart failure, HFmrEF
Citation: Liu Z, Peng Y, Zhao W, Zhu Y, Wu M, Huang H, Peng K, Zhang L, Chen S, Peng X, Li N, Zhang H, Zhou Y, Chen Y, Xiao S, Fan J and Zeng J (2022) Obesity increases cardiovascular mortality in patients with HFmrEF. Front. Cardiovasc. Med. 9:967780. doi: 10.3389/fcvm.2022.967780
Received: 13 June 2022; Accepted: 18 August 2022;
Published: 08 September 2022.
Edited by:
Elisabetta Salvioni, Monzino Cardiology Center (IRCCS), ItalyReviewed by:
Chiara Minoia, ASST Valle Olona, ItalyCopyright © 2022 Liu, Peng, Zhao, Zhu, Wu, Huang, Peng, Zhang, Chen, Peng, Li, Zhang, Zhou, Chen, Xiao, Fan and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianping Zeng, eGhqaWFuZzJAaG51c3QuZWR1LmNu
† These authors have contributed equally to this work
†ORCID: Zhican Liu orcid.org/0000-0002-5532-1632
Jianping Zeng orcid.org/0000-0002-4485-6164
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.