
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med., 18 August 2022
Sec. Cardiovascular Epidemiology and Prevention
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.960096
This article is part of the Research TopicSports CardiologyView all 19 articles
A growing body of research examines the effect of aerobic exercise on pulse wave velocity (PWV) in middle-aged and elderly people, while findings of available studies were conflicting. The aim of this study was to explore the effect of aerobic exercise on PWV in middle-aged and elderly people. Searches were performed in PubMed, Web of Science, and EBSCO databases. Cochrane risk assessment tool was used to evaluate the methodological quality of the included literature. We included studies that satisfied the following criteria: (1) eligible studies should be randomized controlled trials (RCTs); (2) eligible studies should include both an intervention and a control group; (3) eligible studies should use the middle-aged or elderly people as subjects; and (4) eligible studies should use PWV as the outcome measure. From 972 search records initially identified, 11 studies with a total of 12 exercise groups (n = 245) and 11 control groups (n = 239) were eligible for meta-analysis. There was a significant effect of aerobic exercise on reducing PWV in middle-aged and elderly people [weighted mean difference (WMD), –0.75 (95% CI, –1.21 to –0.28), p = 0.002]. Specifically, a higher intensity [vigorous-intensity, –0.74 (–1.34 to –0.14), p = 0.02; moderate-intensity, –0.68 (–1.49 to 0.12), p = 0.10], a younger age [45 years ≤ age < 60 years, –0.57 (–0.78 to –0.37), p < 0.00001; age ≥ 60 years, –0.91 (–2.10 to 0.27), p = 0.13], a better health status [healthy, –1.19 (–2.06 to –0.31), p = 0.008; diseased, –0.32 (–0.64 to –0.01), p = 0.04], and a lower basal body mass index (BMI) [BMI < 25, –1.19 (–2.06 to –0.31), p = 0.008; 25 ≤ BMI < 30, –0.52 (–0.92 to –0.12), p = 0.01; BMI ≥ 30, –0.09 (–0.93 to 0.76), p = 0.84] were associatedwith larger reductions in PWV. Aerobic exercise, especially vigorous-intensity aerobic exercise, contributed to reducing PWV in middle-aged and elderly people. The effect of aerobic exercise on improving PWV was associated with characteristics of the participants. Specifically, a younger age, a better health status, and a lower basal BMI contributed to more significant reductions in PWV.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022337103], identifier [CRD42022337103].
With aging, cardiovascular function gradually declines, especially in middle-aged and elderly people, which is mainly manifested as the aging of the cardiovascular and the decline of blood supply. Cardiovascular diseases (CVDs) are the primary chronic disease affecting human health and quality of life. In recent years, with the change of lifestyle, the prevalence and mortality of CVDs have increased year by year. At the same time, the onset age of CVDs also presents a younger trend. CVDs, such as atherosclerosis, congenital and rheumatic heart disease, and hypertension, are the leading cause of disability and death in middle-aged and elderly people, accounting for more than 40% of the deaths in people aged 65 years and above (1).
Arterial stiffness, which is considered to be one of the earliest pathophysiological processes in the progression of atherosclerosis-related metabolic diseases, is a prominent manifestation of vascular aging, and it has become an independent risk factor for atherosclerosis (2), coronary heart disease (3), diabetes (4), stroke (5), and other CVDs (6, 7). Increased arterial stiffness or decreased vascular elasticity can impair arterial function, leading to increased systolic blood pressure, left ventricular hypertrophy, and reduced ventricular diastolic function (8, 9), and thus increases the risk of arteriosclerosis and coronary artery disease (10, 11). Therefore, the prevention and treatment of arterial stiffness is crucial (1, 12).
Previous studies have shown that pulse wave velocity (PWV), especially carotid-femoral pulse wave velocity (cfPWV), has been recommended as the gold standard for assessing arterial stiffness as a non-invasive measurement (8, 11, 12). In addition, PWV is considered to be negatively correlated with vascular health (13). However, these results show more negative outcomes when the blood vessels are stiffer and the lumen is narrowed and thickened, suggesting increased arteriosclerosis, decreased vascular elasticity levels, arteriosclerosis, and an increased risk of coronary artery disease (9). Therefore, reducing PWV is one of the main goals for improving cardiovascular function (14, 15).
Exercise is considered to be an effective measure to prevent CVD and improve its prognosis. In recent years, a large number of studies on exercise and cardiovascular function have shown that appropriate exercise can effectively improve arterial stiffness and reduce the risk of CVDs (10, 12, 16). Older adults who are physically active have less decline in physical function and health and a lower incidence of CVDs than those who are inactive (17, 18). However, there is substantial evidence that high-intensity exercise may lead to CVDs (19). Furthermore, exercise can increase the risk of acute CVDs in sedentary older adults who are not used to sudden high-intensity exercise (19).
At present, there are various intervention methods for middle-aged and elderly people, such as aerobic exercise, resistance exercise, and combined exercise. Totosy de Zepetnek et al. (20) showed that combined exercise had no significant effect on cardiovascular function in middle-aged and elderly people, which is in line with a meta-analysis conducted by Zhang et al. (21). However, aerobic exercise is considered to be an effective method for improving arterial stiffness, whereas the results of resistance exercise are controversial (20). Among different types of intervention methods, aerobic exercise has a higher degree of freedom, is simpler and more convenient, and is more suitable for middle-aged and elderly people. Therefore, aerobic exercise is recommended as the preferred exercise for middle-aged and elderly people (11).
A growing body of research examines the effect of aerobic exercise on PWV in middle-aged and elderly people, while findings of available studies were conflicting. Many studies have confirmed that aerobic exercise can effectively reduce PWV in middle-aged and elderly people (13, 22, 23), while some studies have shown that aerobic exercise has no significant effect on the PWV (16, 19, 24–27). Therefore, we conducted a comprehensive systematic review and meta-analysis of randomized controlled trials (RCTs) to explore whether aerobic exercises have a role in improving PWV in middle-aged and elderly people.
This systematic review and meta-analysis was conducted following the guidelines of the Cochrane Selection Manual (28) and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (29). The protocol for this systematic review has been registered on PROSPERO (CRD42022337103).
For this systematic review and meta-analysis, we searched through PubMed, Web of Science, and EBSCO electronic databases from the inception of indexing until October 11, 2021. The initial search contained the following terms: (a) exercise, aerobic exercise, endurance exercise, aerobic training, endurance training, cardio training, physical endurance, physical exertion; (b) pulse wave velocity, PWV, pulse wave analysis, (analyses, pulse wave), (analysis, pulse wave), pulse wave analyses, (wave analyses, pulse), (wave analysis, pulse), pulse wave velocity, pulse wave velocities, (velocities, pulse wave), (velocity, pulse wave), (wave velocities, pulse), (wave velocity, pulse), pulse transit time, pulse transit times, (time, pulse transit), (times, pulse transit), (transit time, pulse), (transit times, pulse), pulse wave transit time; (c) elderly, aged, geriatrics, eldest, old, older, middle-aged, middle aged, middle age, elderly, aged, geriatrics, eldest, old, older, middle-aged, middle aged, middle age. We also hand-searched reference lists of all identified studies. We excluded studies based on the review of the title, abstract, and full text. Two authors (GL and YL) conducted the process independently using a standardized form. In case of any discrepancies between the two authors, a third author (LY) was involved in the discussion until a consensus was made.
We included studies that satisfied the following criteria: (1) eligible studies should be RCTs; (2) eligible studies should include both an intervention and control group with the only difference between them being the addition of aerobic exercise in the intervention group; (3) eligible studies should use the middle-aged or elderly people as subjects; and (4) eligible studies should use cfPWV as the outcome measure. Non-English language publications, animal model publications, reviews, and conference articles were excluded from the analysis.
Two authors (GL and YL) of this study performed the data extraction independently using the same and standardized form created in Microsoft Excel. If there were any discrepancies between the authors in the extracted data, the accuracy of the information was rechecked in the studies. The extracted variables mainly included: (a) characteristics of included studies (first author’s last name, year of study publication); (b) characteristics of aerobic exercise (type of exercise, intensity, duration of intervention, session duration, frequency); (c) participant’s characteristics [n, age, gender, basal body mass index (BMI), basal systolic blood pressure (SBP), basal diastolic blood pressure (DBP), health status]; and (d) treatment effects [mean and standard deviation (SD) values reflecting the change in PWV from baseline to post-intervention in the aerobic exercise and control groups].
We assessed the methodological quality of the included studies using the Cochrane risk of bias criteria, which included seven items, namely, randomization sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. Each item was judged as “low risk,” “unclear risk,” or “high risk” based on responses to the signaling questions, to make an overall bias judgment for the specific study outcome being assessed (28). Two reviewers (GL and YL) performed the methodological quality assessment independently. Disagreements in the assessments between the reviewers were resolved through discussion and consensus with a third author (LY).
The mean and SD values reflecting the change in PWV from baseline to post-intervention were extracted from each study for pooling effects. SD was calculated using a previously described formula for studies reporting standard error (SE) or 95% confidence intervals (CIs) (30). When the data could not be extracted or there was a dispute, two authors negotiated or contacted the author of the article to resolve it. Otherwise, the platform was used to extract the information (31).
The majority of included studies provided mean and SD values before and after the intervention. We calculated the changes in the mean and SD values for PWV. When analyzing whether aerobic exercise could improve the PWV of middle-aged and elderly people, the Chi-square (χ2) test was used. The negative value of I2 was defined as zero, so the value of I2 was between 0 and 100%. As mentioned by Chiarito et al. (32), an I2 value of 0% indicates no observed heterogeneity, and larger values indicate increasing heterogeneity. The I2 values of < 25%, 25–75%, and > 75% were considered to represent low, moderate, and high levels of heterogeneity, respectively (33). If there was a high level of heterogeneity (I2 ≥ 50%), we used subgroup analyses to interpret the results (29). When I2 is < 50%, data were pooled using fixed effects models to obtain the weighted mean difference (WMD) and 95% CIs; when I2 is ≥ 50%, data were pooled using random effects models to obtain the WMD and 95% CIs. In the subgroup analyses, we tried to use intensities of aerobic exercise (moderate-intensity and vigorous-intensity), age of participants (45 years ≤ age < 60 years and age ≥ 60 years), basal BMI (BMI < 25, 25 ≤ BMI < 30, and BMI ≥ 30), and health status (healthy and diseased) to explore the impact on PWV. The analysis result, funnel plot, and forest chart were generated using the software RevMan.5. In terms of overall impact, p < 0.05 was considered statistically significant.
As shown in Figure 1, a total of 969 search records were preliminarily retrieved, and three records were identified through other sources. After excluding the duplicates, 740 studies were remaining, and 704 studies were not eligible for inclusion through the title and abstract screening. Twenty-five studies were excluded by reading the full text of 36 studies: (1) the experimental group combined with other treatments (n = 5); (2) outcomes were not relevant (n = 15); and (3) no control group (n = 5). Finally, 11 studies (13, 19, 22, 23, 25, 27, 34–38) examining the effect of aerobic exercise on PWV in middle-aged and elderly people were considered eligible for systematic review and meta-analysis.
The main characteristics of the participants and exercise interventions are shown in Supplementary Table 1. The included studies involved 245 participants in the 12 exercise groups and 239 participants in the 11 control groups. One study (22) involved only women, and the other 10 studies (13, 19, 23, 25, 27, 34–38) involved both men and women. Three studies (22, 23, 27) involved healthy participants, and eight studies (13, 19, 25, 34–38) involved diseased participants. The average age of the participants was ranging from 45 to 74.3 years. Among them, seven studies (13, 22, 25, 34, 36–38) involved participants with an average age of < 60 years, and four studies (19, 23, 27, 35) involved participants with an average age of ≥ 60 years. There studies (22, 23, 27) involved participants with basal BMI < 25, five studies (19, 25, 34, 37, 38) involved participants with 25 ≤ BMI < 30, and two studies (13, 35) involved participants with BMI > 30.
According to the position statement of physical activity and training intensity (39), we adjusted the intensity classification of aerobic exercise according to the included research situation: 20% < maximal oxygen uptake (VO2max) ≤ 40%, 40% < maximum heart rate (HRmax) ≤ 55%, or 20% < heart rate reserve (HRR) ≤ 40% were determined as light-intensity; 40% < VO2max ≤ 60%, 55% < HRmax ≤ 70%, or 40% < HRR ≤ 60% were determined as moderate-intensity; 60% < VO2max ≤ 85%, 70% < HRmax ≤ 90%, or 60% < HRR ≤ 85% were determined as vigorous-intensity. Among the included studies, the intensity of two studies (19, 36) could not be defined, two studies (13, 34) were defined as moderate-intensity, and seven studies (22, 23, 25, 27, 35, 37, 38) were defined as vigorous-intensity.
Cochrane risk assessment tool was used to evaluate the methodological quality of the included literature, mainly from six aspects, namely, selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. The quality score was determined according to three levels (low risk, high risk, and unclear). The quality of the included literature was divided into three levels from high to low, namely, high quality, medium quality, and low quality (see Figure 2). Publication bias was assessed visually by inspecting the funnel plot (see Figure 3).
After analyzing the data of all included studies, we found that compared with the control group, aerobic exercise had a significant effect on reducing PWV in middle-aged and elderly people [WMD, –0.75 (95% CI, –1.21 to –0.28), p = 0.002], while there was a high heterogeneity (I2 = 84%) (Figure 4). Therefore, we used subgroup analyses to interpret the results.
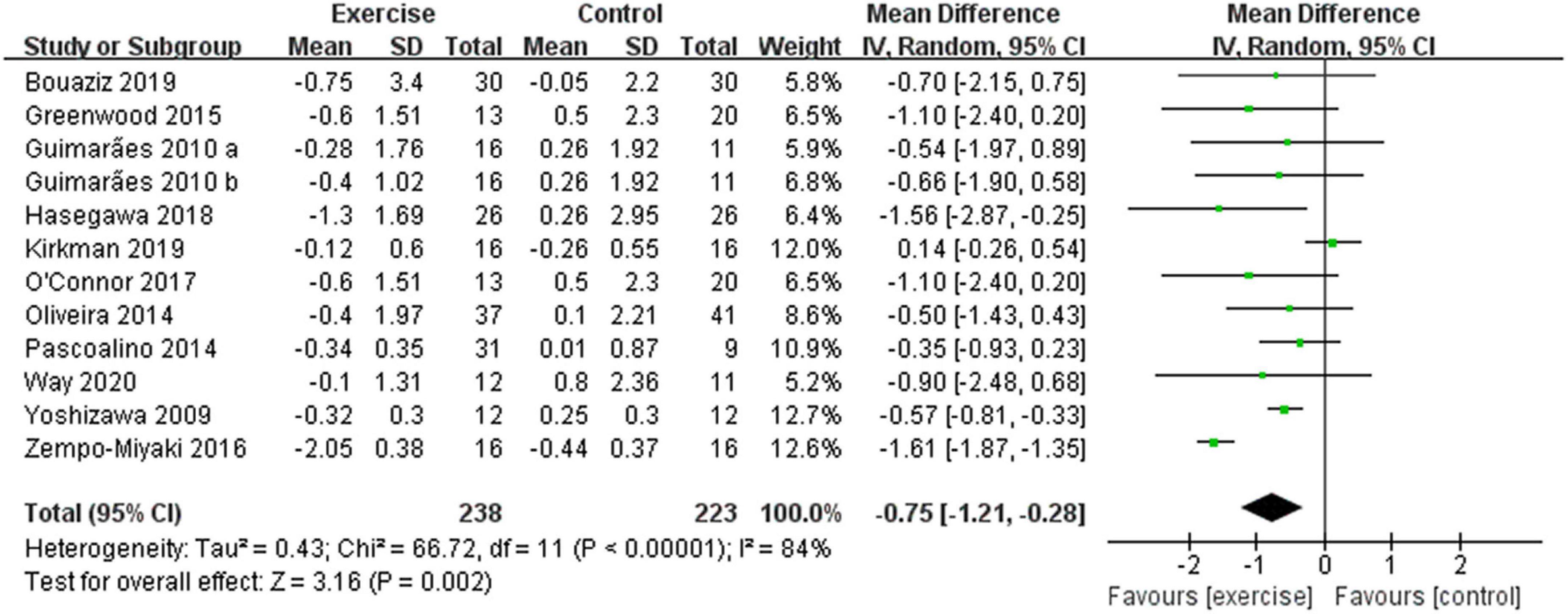
Figure 4. Meta-analysis results of the effect of aerobic exercise on the PWV of middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicate the effect size of each study summarized as WMD. The size of the shaded squares is proportional to the percentage weight of each study. Horizontal lines represent the 95% CI and the vertical line represents the overall effect.
Different results were shown when considering exercise intensity (see Figure 5). Specifically, compared with the control group, vigorous-intensity exercise significantly reduced PWV [WMD, –0.74 (95% CI, –1.34 to –0.14), p = 0.02, I2 = 91%], while moderate-intensity exercise had no significant effect on PWV in middle-aged and elderly people [WMD, –0.68 (95% CI, –1.49 to 0.12), p = 0.10, I2 = 0%]. Subgroup analysis indicated that a higher intensity was associated with larger reductions in PWV.
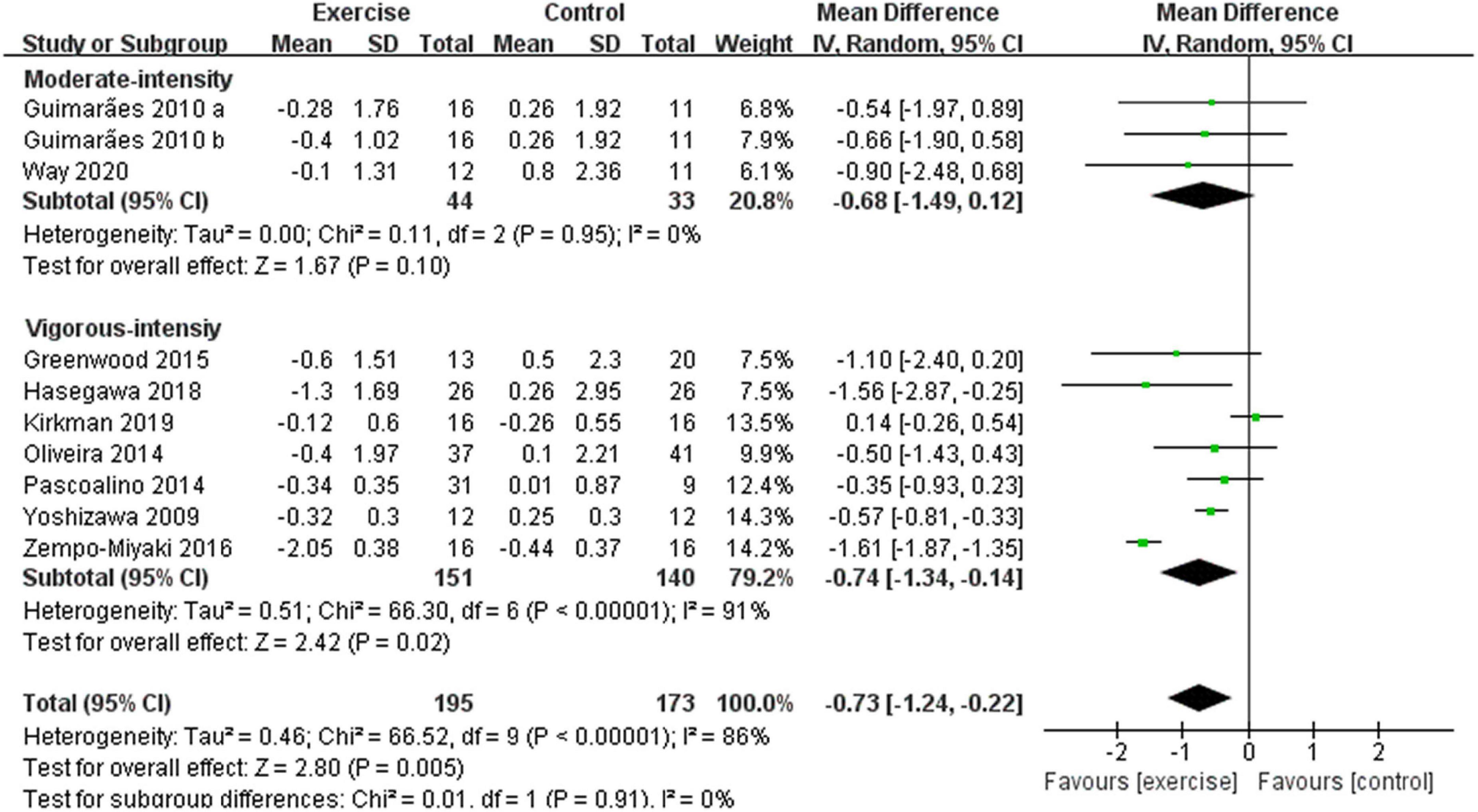
Figure 5. Meta-analysis results of the effect of different intensities of aerobic exercise on the PWV of middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicate the size of the effect of each study summarized as WMD. The size of the shaded square is proportional to the percentage weight of each study. Horizontal lines represent the 95% CI and the vertical dashed line represents the overall effect.
In addition, different results were shown when considering participants’ characteristics. The subgroup analysis indicated that a younger age [45 years ≤ age < 60 years, –0.57 (95% CI, –0.78 to –0.37), p < 0.00001, I2 = 0%; age ≥ 60 years, –0.91 (95% CI, –2.10 to 0.27), p = 0.13, I2 = 94%. see Figure 6], a better health status [healthy, –1.19 (95% CI, –2.06 to –0.31), p = 0.008, I2 = 94%; diseased, –0.32 (95% CI, –0.64 to –0.01), p = 0.04, I2 = 11%. see Figure 7], and a lower basal BMI [BMI < 25, –1.19 (95% CI, –2.06 to –0.31), p = 0.008, I2 = 94%; 25 ≤ BMI < 30, –0.52 (95% CI, –0.92 to –0.12), p = 0.01, I2 = 0%; BMI ≥ 30, –0.09 (95% CI, –0.93 to 0.76), p = 0.84, I2 = 36%. see Figure 8] were associated with larger reductions in PWV.
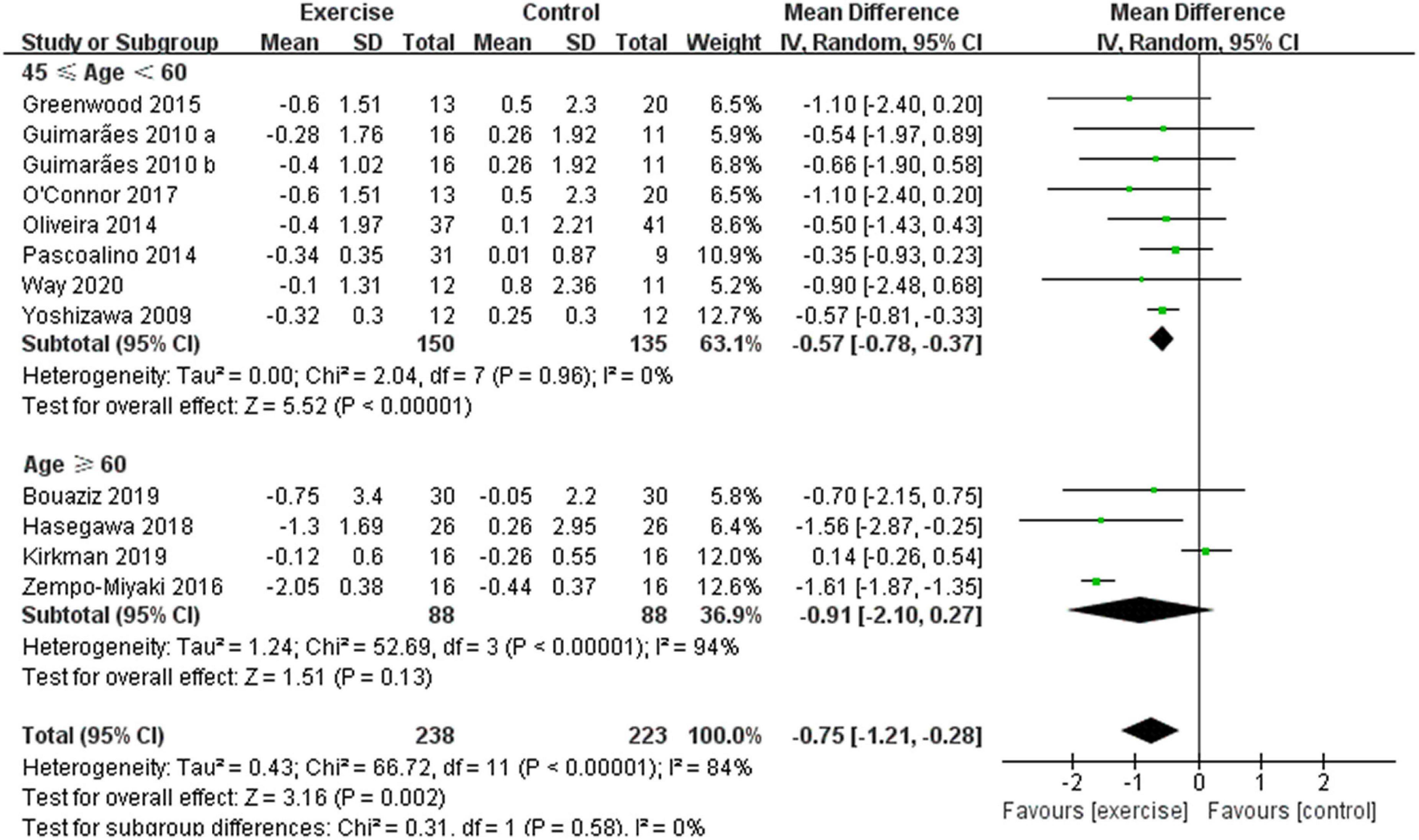
Figure 6. Meta-analysis results of the effect of aerobic exercise on the PWV of middle-aged people or elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicate the size of the effect of each study summarized as WMD. The size of the shaded square is proportional to the percentage weight of each study. Horizontal line represents the 95% CI and the vertical dashed line represents the overall effect.
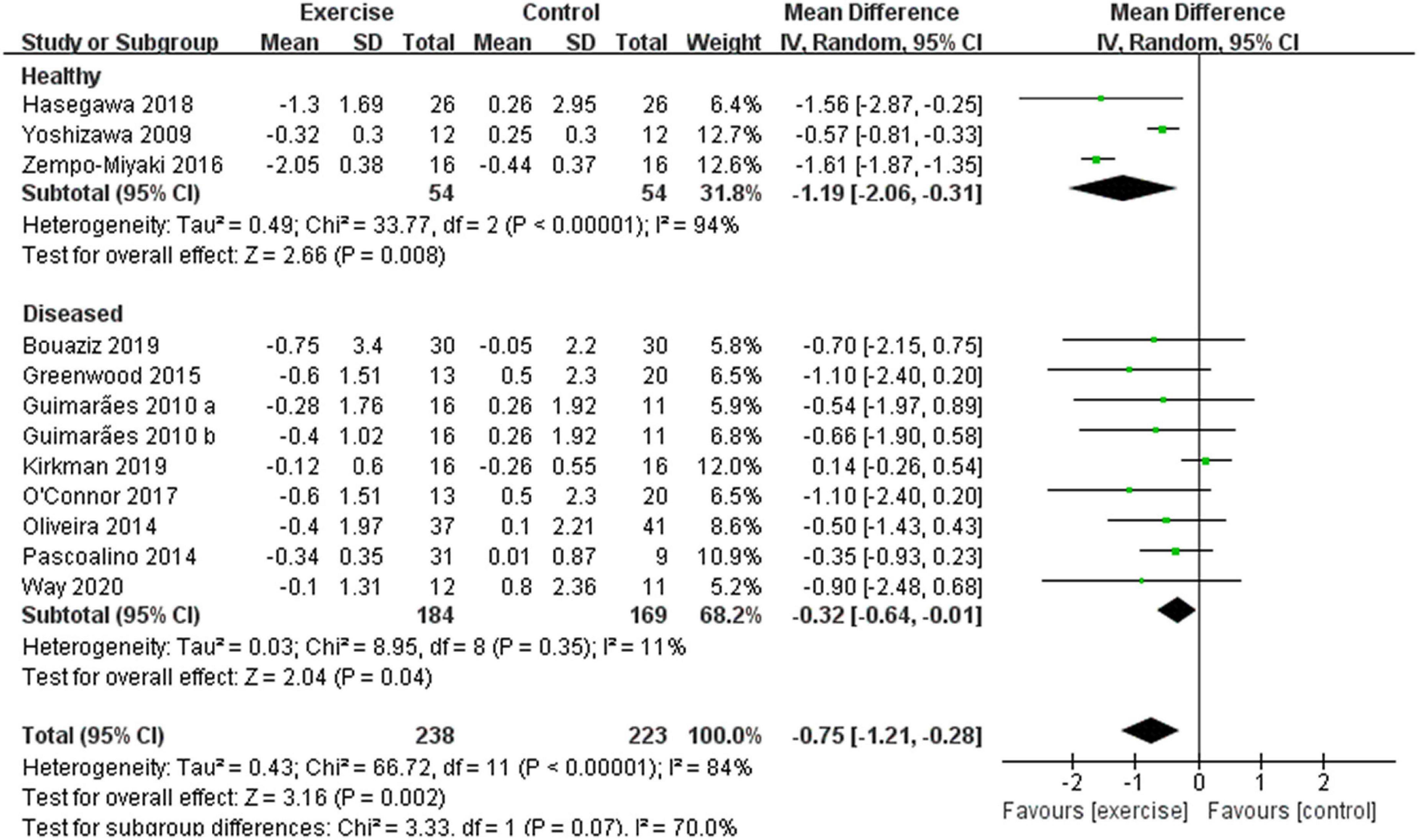
Figure 7. Meta-analysis results of the effect of aerobic exercise on the PWV of healthy or diseased middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicate the size of the effect of each study summarized as WMD. The size of the shaded square is proportional to the percentage weight of each study. Horizontal line represents the 95% CI and the vertical dashed line represents the overall effect.
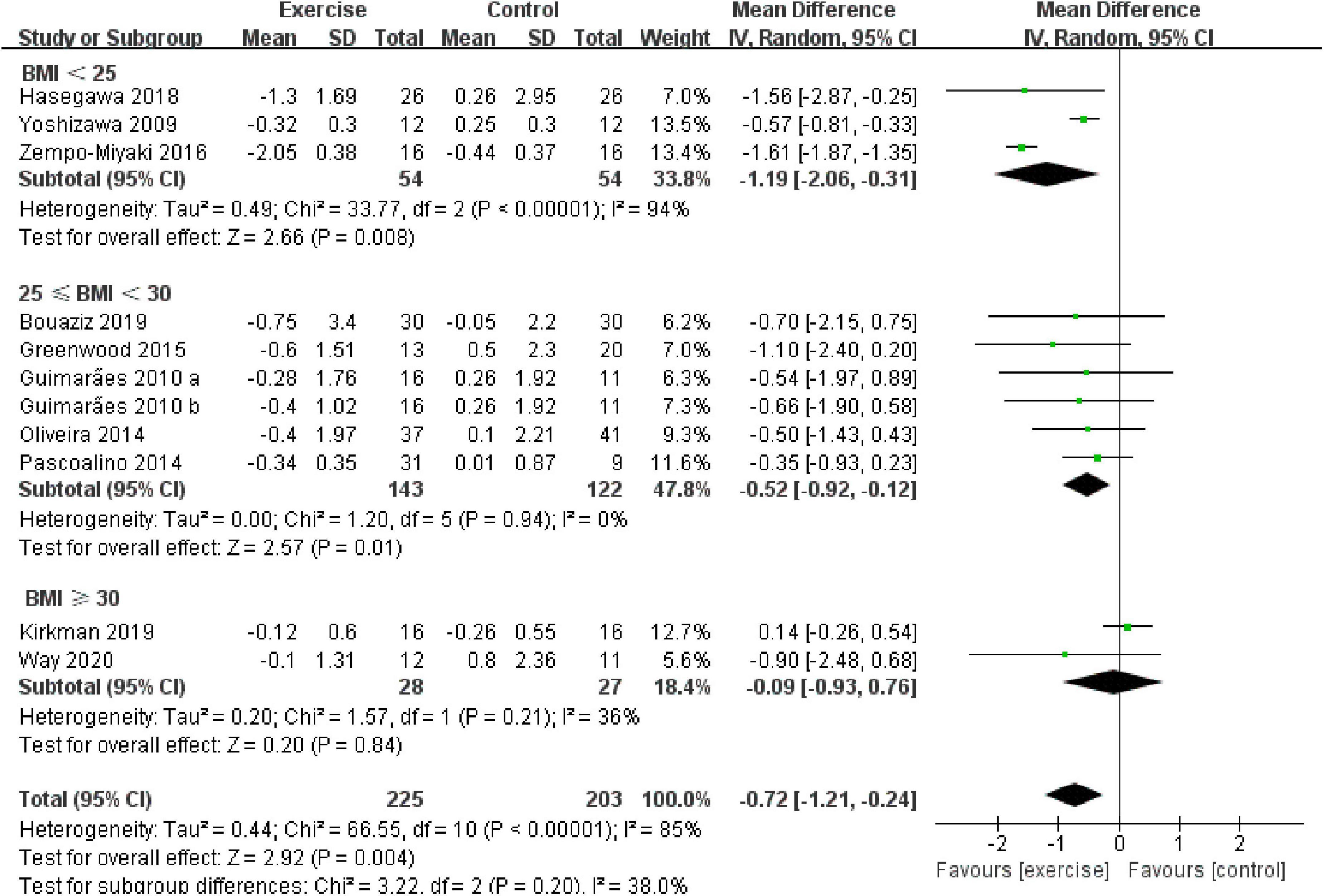
Figure 8. Meta-analysis results of the effect of aerobic exercise on the PWV of normal weight, overweight, or obese middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamond indicated the size of the effect of each study summarized as WMD. The size of the shaded square is proportional to the percentage weight of each study. Horizontal line represents the 95% CI and the vertical dashed line represents the overall effect.
This systematic review and meta-analysis indicated that aerobic exercise had the potential to reduce arterial stiffness in middle-aged and elderly people, as manifested by a reduction in PWV. Previous studies were consistent with our results, for example, 10 weeks of shallow water aerobic exercise significantly reduced PWV in elderly people (40), 20 weeks of walking training significantly reduced PWV in elderly people (41), and 21 weeks of aerobic exercise effectively reduced PWV in kidney transplant recipients (25). However, the mechanism by which aerobic exercise improves arterial stiffness has not been fully revealed.
Many studies have shown that the lack of exercise may lead to fat accumulation and disorders of glycolipid metabolism (42–44). Adipose tissue produces the pro-inflammatory cytokine interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), plasminogen activator inhibitor, and adiponectin. Therefore, the accumulation of fat may be related to the increased inflammatory response during atherosclerosis, which is consistent with the study of Jennersjö et al. (45), and that the inflammatory response can accelerate the process of arteriosclerosis (46, 47). Previous studies have shown that regular aerobic exercise can reduce fat content and increase adiponectin secretion, which in turn reduces arterial stiffness (27, 30, 48). In addition, a previous study also showed that exercise can reduce risk factors for arterial stiffness associated with metabolic disorders (20). Metabolic syndrome, which can lead to impaired glucose tolerance, hypertension, dyslipidemia, and abdominal obesity, has been reported to be associated with changes in the arterial system, mainly manifested by changes in vascular structure and function, including increased arterial wall thickness and increased vascular wall stiffness (46, 47, 49). Above all, metabolic disorders can accelerate arterial aging through elastin fiber fragmentation, increased pressure on the collagen fibers of the arterial wall (50), and vascular damage, ultimately leading to increased arterial stiffness (51, 52). Aerobic exercise has been shown to have a dampening effect on metabolic disorders (53). There is increasing evidence that aerobic exercise promotes the clearance of triacylglycerol and low-density lipoprotein cholesterol (54–56), thereby preventing oxidative stress, which in turn reduces arterial stiffness.
In addition, Beck et al. (57) found that an increase in PWV may be associated with a decrease in endothelial function. The increase in PWV is manifested by the decrease in the bioavailability of endothelial-derived nitric oxide (NO) (58). NO is produced by L-arginine through endothelial nitric oxide synthase (eNOS) in the vascular endothelium, which has the effect of dilating blood vessels. Maeda et al. suggested that exercise increases the bioavailability of NO and reduces PWV (58), which was in line with the report by Taddei et al. showing that regular exercise restores the utilization of NO after oxidative stress and prevents age-induced endothelial dysfunction. A previous study showed that NO increased and PWV decreased after 24 weeks of aerobic exercise, and a significant negative correlation between NO and PWV was observed (59). Taken together, aerobic exercise in middle-aged and elderly people can increase the synthesis and bioavailability of NO, reduce circulating endothelin-1 (ET-1), increase flow-mediated dilation (FMD) of the brachial artery, improve the endothelial function, and ultimately reduce PWV (60).
In conclusion, aerobic exercise in middle-aged and elderly people can reduce fat accumulation and improve glycolipid metabolism and endothelial function, thereby reducing arterial stiffness and playing an important role in preventing arteriosclerosis.
According to the studies we included, aerobic exercise significantly reduced PWV in middle-aged and elderly people, but the heterogeneity between groups was high. Therefore, we used subgroup analysis to interpret the results. In the subgroup analyses, we sought to determine the effects of exercise intensity and characteristics of the participants.
Previous studies have demonstrated that aerobic exercise has a positive effect on arterial stiffness (61–63). However, some studies have found that PWV does not always decrease with increasing aerobic exercise intensity, for example, Zempo-Miyaki et al. (23) showed that 8 weeks of aerobic exercise (60–70% peak oxygen uptake) significantly reduced PWV in middle-aged and elderly people, while Oudegeest-Sander et al. (64) reported that 12 months of cycling exercise (70–85% of individual HRR) had no effect on PWV in elderly people, suggesting that exercise intensity was a key factor affecting the impact of the intervention. Therefore, we divided the study into a moderate-intensity group and a vigorous-intensity group. Compared with the control group, vigorous-intensity exercise significantly reduced PWV, while moderate-intensity exercise had no significant effect on PWV. Previous studies have demonstrated that vigorous-intensity exercise may generate greater shear stress in endothelial cells, thereby improving endothelial function, reducing oxidative stress, and improving vascular function (25, 50, 65, 66), which is consistent with our study showing that vigorous-intensity exercise can significantly reduce the arterial stiffness in middle-aged and elderly people. However, recent studies have shown that exercise intensity definition based on percentages of peak HR and VO2peak may misclassify the effective exercise intensity, and the discrepancy between the individually determined and the recommended exercise intensity is particularly relevant in cardiac patients. And a ventilatory threshold-based rather than a range-based approach is advisable to define an appropriate level of exercise intensity (67, 68). In addition, according to the European Association of Preventive Cardiology (EAPC) position statement on the assessment and prescription of aerobic exercise intensity in cardiovascular rehabilitation, the assessment of ventilatory threshold 1 (VT1) and VT2 during cardiopulmonary exercise test (CPET) should be used for the determination of the aerobic exercise intensity in the majority of CVD patients (69). Therefore, since studies included in this systematic review and meta-analysis used HR and VO2max to define the exercise intensity, those focused on CVD populations need to be cautious when referring to our finding.
A previous study showed that blood pressure increases more rapidly in adults after the age of 60 years, which is the critical point for a higher incidence of CVDs (70). Therefore, the included studies in this meta-analysis were divided into two subgroups by the age of participants, namely, middle-aged group and elderly group. Compared with the control group, aerobic exercise significantly reduced PWV in middle-aged people, while aerobic exercise had no significant effect on PWV in elderly people, indicating that aerobic exercise had a better effect on PWV in middle-aged people than in elderly people. Aging is an inevitable part of life, and aerobic exercise has a limited effect on improving vascular endothelial function. For example, Ha et al. (11) found that 12 weeks of aerobic exercise did not reduce PWV in women aged 70–80 years, which may be related to sex hormone levels of middle-aged and elderly people. Cross-sectional studies have also reported an age-related decline in sex hormones, with a sharp decline in sex hormones after the age of 65 years (71, 72). Additionally, a previous study reported that sex hormone levels may influence the effect of aerobic exercise on improving cardiovascular function (73). In addition, one study found that the benefit of aerobic exercise on vascular function was diminished in estrogen-deficient postmenopausal women, but in this group, estrogen treatment appeared to restore improvements in endothelial function (73). Furthermore, studies have shown that aortic PWV increases by approximately 0.10 m/s per year with age, with a weak annual increase in PWV (less than 0.10 m/s) in subjects before the age of 45 years, indicating a low rate of arteriosclerosis in young adults (74, 75). Therefore, the insignificant decline in PWV in the elderly may also be due to the insufficient effect of exercise against vascular aging.
In the abovementioned results, we suspected that the improvement of arterial stiffness by exercise was influenced by a variety of CVDs, so this report divided the included studies into two subgroups, namely, the healthy group and the diseased group. Compared with the control group, aerobic exercise significantly reduced PWV in both healthy and diseased individuals, while a better health status was associated with larger reductions, which was consistent with a previous study, showing that aerobic exercise had no long-term effect on arterial stiffness in older adults with cardiometabolic risk factors (76). Therefore, the lesser the number of risk factors for CVDs or the types of CVDs, the better the effect of aerobic exercise.
Obesity is an independent predictor of CVDs, and weight loss has been shown to improve many obesity-related risk factors; therefore, we divided the included studies into normal weight, overweight, and obese groups based on the basal BMI of the participants. Our results showed that compared with the control group, aerobic exercise significantly reduced PWV in normal weight and overweight people, whereas aerobic exercise had no significant effect on PWV in obese people. In addition, a lower BMI was associated with larger reductions in PWV, indicating that aerobic exercise had a better effect on PWV in lower BMI people than in higher BMI people, which was consistent with a previous study, showing that a mean weight loss of 8% resulted in a statistically and clinically significant PWV reduction of 0.6 m/s, suggesting that a lower BMI was associated with lower rates of arteriosclerosis (77). Therefore, arteriosclerosis in people with a higher BMI may be a major determinant of morbidity and mortality in this population.
Some potential limitations of this meta-analysis should be acknowledged. First, the included studies were all RCTs of aerobic exercise intervention, which could not be completely blinded. Therefore, in the quality evaluation process, subjective factors will cause a certain degree of deviation. Second, studies included in this systematic review and meta-analysis used HR and VO2max to define the exercise intensity, and studies focused on CVDs populations need to be cautious when referring to our finding. Finally, although the included studies did not specify any adverse events associated with the aerobic exercise intervention, it is unclear whether the researchers attempted to comprehensively document all possible adverse events. Therefore, future studies with more detailed data describing possible injury, pain, and/or any other potential adverse effects are encouraged, as this will expand our knowledge of the safety of aerobic exercise in middle-aged and elderly people.
Our analysis indicated that aerobic exercise, especially vigorous-intensity aerobic exercise, contributed to reducing PWV in middle-aged people. The effect of aerobic exercise on improving PWV was associated with characteristics of the participant. Specifically, a younger age, a better health status, and a lower basal BMI contributed to more significant reductions in PWV.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
GL wrote the manuscript. LY and YL contributed to the conception. GL and YL did the literature search. GL, YL, and LY extracted the data. QS and QY contributed to the acquisition. All authors have read and approved the final manuscript.
GL was supported by Graduate Students’ Innovative Scientific Research Program of Beijing Sport University (20212011) and LY was supported by Chinese Universities Scientific Fund (2021QN001).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.960096/full#supplementary-material
1. Lakatta EG. Age-associated cardiovascular changes in health: Impact on cardiovascular disease in older persons. Heart Fail Rev. (2002) 7:29–49. doi: 10.1023/a:1013797722156
2. Zanoli L, Lentini P, Briet M, Castellino P, House AA, London GM, et al. Arterial stiffness in the heart disease of CKD. J Am Soc Nephrol. (2019) 30:918–28. doi: 10.1681/ASN.2019020117
3. Ikonomidis I, Makavos G, Lekakis J. Arterial stiffness and coronary artery disease. Curr Opin Cardiol. (2015) 30:422–31. doi: 10.1097/hco.0000000000000179
4. Miyoshi T, Ito H. Arterial stiffness in health and disease: The role of cardio-ankle vascular index. J Cardiol. (2021) 78:493–501. doi: 10.1016/j.jjcc.2021.07.011
5. Spence JD, Azarpazhooh MR, Larsson SC, Bogiatzi C, Hankey GJ. Stroke prevention in older adults: Recent advances. Stroke. (2020) 51:3770–7. doi: 10.1161/strokeaha.120.031707
6. Lage JG, Bortolotto AL, Scanavacca MI, Bortolotto LA, Darrieux F. Arterial stiffness and atrial fibrillation: A review. Clinics (Sao Paulo). (2022) 77:100014. doi: 10.1016/j.clinsp.2022.100014
7. Boutouyrie P, Chowienczyk P, Humphrey JD, Mitchell GF. Arterial stiffness and cardiovascular risk in hypertension. Circ Res. (2021) 128:864–86. doi: 10.1161/circresaha.121.318061
8. Mills NL, Miller JJ, Anand A, Robinson SD, Frazer GA, Anderson D, et al. Increased arterial stiffness in patients with chronic obstructive pulmonary disease: A mechanism for increased cardiovascular risk. Thorax. (2008) 63:306–11. doi: 10.1136/thx.2007.083493
9. Miyachi M. Effects of resistance training on arterial stiffness: A meta-analysis. Br J Sports Med. (2013) 47:393–6. doi: 10.1136/bjsports-2012-090488
10. Bellia A, Iellamo F, De Carli E, Andreadi A, Padua E, Lombardo M, et al. Exercise individualized by TRIMPi method reduces arterial stiffness in early onset type 2 diabetic patients: A randomized controlled trial with aerobic interval training. Int J Cardiol. (2017) 248:314–9. doi: 10.1016/j.ijcard.2017.06.065
11. Ha MS, Kim JH, Kim YS, Kim DY. Effects of aquarobic exercise and burdock intake on serum blood lipids and vascular elasticity in Korean elderly women. Exp Gerontol. (2018) 101:63–8. doi: 10.1016/j.exger.2017.11.005
12. Brinkley TE, Leng I, Bailey MJ, Houston DK, Hugenschmidt CE, Nicklas BJ, et al. Effects of exercise and weight loss on proximal aortic stiffness in older adults with obesity. Circulation. (2021) 144:684–93. doi: 10.1161/CIRCULATIONAHA.120.051943
13. Way KL, Sabag A, Sultana RN, Baker MK, Keating SE, Lanting S, et al. The effect of low-volume high-intensity interval training on cardiovascular health outcomes in type 2 diabetes: A randomised controlled trial. Int J Cardiol. (2020) 320:148–54. doi: 10.1016/j.ijcard.2020.06.019
14. Szolnoky G, Gavallér H, Gönczy A, Bihari I, Kemény L, Forster T, et al. The effects of below-knee medical compression stockings on pulse wave velocity of young healthy volunteers. J Strength Cond Res. (2021) 35:275–9. doi: 10.1519/JSC.0000000000002636
15. Cavalcante JL, Lima JA, Redheuil A, Al-Mallah MH. Aortic stiffness: Current understanding and future directions. J Am Coll Cardiol. (2011) 57:1511–22. doi: 10.1016/j.jacc.2010.12.017
16. Alkatan M, Machin DR, Baker JR, Akkari AS, Park W, Tanaka H. Effects of swimming and cycling exercise intervention on vascular function in patients with osteoarthritis. Am J Cardiol. (2016) 117:141–5. doi: 10.1016/j.amjcard.2015.10.017
17. Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: A systematic review and meta-analysis. Eur J Epidemiol. (2018) 33:831–45. doi: 10.1007/s10654-018-0374-z
18. Li Z, Cui M, Yu K, Zhang XW, Li CW, Nie XD, et al. Effects of nutrition supplementation and physical exercise on muscle mass, muscle strength and fat mass among sarcopenic elderly: A randomized controlled trial. Appl Physiol Nutr Metab. (2021) 46:494–500. doi: 10.1139/apnm-2020-0643
19. Bouaziz W, Lang PO, Schmitt E, Leprêtre PM, Lefebvre F, Momas C, et al. Effects of a short-term interval aerobic training program with recovery bouts on vascular function in sedentary aged 70 or over: A randomized controlled trial. Arch Gerontol Geriatr. (2019) 82:217–25. doi: 10.1016/j.archger.2019.02.017
20. Totosy de Zepetnek JO, Pelletier CA, Hicks AL, MacDonald MJ. Following the physical activity guidelines for adults with spinal cord injury for 16 weeks does not improve vascular health: A randomized controlled trial. Arch Phys Med Rehabil. (2015) 96:1566–75. doi: 10.1016/j.apmr.2015.05.019
21. Zhang Y, Qi L, Xu L, Sun X, Liu W, Zhou S, et al. Effects of exercise modalities on central hemodynamics, arterial stiffness and cardiac function in cardiovascular disease: Systematic review and meta-analysis of randomized controlled trials. PLoS One. (2018) 13:e0200829. doi: 10.1371/journal.pone.0200829
22. Yoshizawa M, Maeda S, Miyaki A, Misono M, Saito Y, Tanabe K, et al. Effect of 12 weeks of moderate-intensity resistance training on arterial stiffness: A randomised controlled trial in women aged 32-59 years. Br J Sports Med. (2009) 43:615–8. doi: 10.1136/bjsm.2008.052126
23. Zempo-Miyaki A, Fujie S, Sato K, Hasegawa N, Sanada K, Maeda S, et al. Elevated pentraxin 3 level at the early stage of exercise training is associated with reduction of arterial stiffness in middle-aged and older adults. J Hum Hypertens. (2016) 30:521–6. doi: 10.1038/jhh.2015.105
24. Chacaroun S, Borowik A, Vega-Escamilla Y, Gonzalez I, Doutreleau S, Wuyam B, et al. Hypoxic exercise training to improve exercise capacity in obese individuals. Med Sci Sports Exerc. (2020) 52:1641–9. doi: 10.1249/MSS.0000000000002322
25. Greenwood SA, Koufaki P, Mercer TH, Rush R, O’Connor E, Tuffnell R, et al. Aerobic or resistance training and pulse wave velocity in kidney transplant recipients: A 12-week pilot randomized controlled trial (the exercise in renal transplant [ExeRT] Trial). Am J Kidney Dis. (2015) 66:689–98. doi: 10.1053/j.ajkd.2015.06.016
26. Hanssen H, Minghetti A, Magon S, Rossmeissl A, Papadopoulou A, Klenk C, et al. Superior effects of high-intensity interval training vs. moderate continuous training on arterial stiffness in episodic migraine: A randomized controlled trial. Front Physiol. (2017) 8:1086. doi: 10.3389/fphys.2017.01086
27. Hasegawa N, Fujie S, Horii N, Uchida M, Kurihara T, Sanada K, et al. Aerobic exercise training-induced changes in serum C1q/TNF-related protein levels are associated with reduced arterial stiffness in middle-aged and older adults. Am J Physiol Regul Integr Comp Physiol. (2018) 314:R94–101. doi: 10.1152/ajpregu.00212.2017
28. Higgins JP, Green S editors. Cochrane handbook for systematic reviews of interventions: The Cochrane Collaboration. Chichester, UK: Wiley (2008).
29. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
30. Zheng Q, Yuan Y, Yi W, Lau WB, Wang Y, Wang X, et al. C1q/TNF-related proteins, a family of novel adipokines, induce vascular relaxation through the adiponectin receptor-1/AMPK/eNOS/nitric oxide signaling pathway. Arterioscler Thromb Vasc Biol. (2011) 31:2616–23. doi: 10.1161/ATVBAHA.111.231050
31. You QP, Yu LK, Li G, He H, Lv YY. Effects of different intensities and durations of aerobic exercise on vascular endothelial function in middle-aged and elderly people: A meta-analysis. Front Physiol. (2022) 12:803102. doi: 10.3389/fphys.2021.803102
32. Chiarito M, Sanz-Sánchez J, Cannata F, Cao D, Sturla M, Panico C, et al. Monotherapy with a P2Y (12) inhibitor or aspirin for secondary prevention in patients with established atherosclerosis: A systematic review and meta-analysis. Lancet. (2020) 395:1487–95. doi: 10.1016/S0140-6736(20)30315-9
33. Ramirez-Campillo R, Gentil P, Negra Y, Grgic J, Girard O. Effects of plyometric jump training on repeated sprint ability in athletes: A systematic review and meta-analysis. Sports Med. (2021) 51:2165–79. doi: 10.1007/s40279-021-01479-w
34. Guimarães GV, Ciolac EG, Carvalho VO, D’Avila VM, Bortolotto LA, Bocchi EA. Effects of continuous vs. interval exercise training on blood pressure and arterial stiffness in treated hypertension. Hypertens Res. (2010) 33:627–32. doi: 10.1038/hr.2010.42
35. Kirkman DL, Ramick MG, Muth BJ, Stock JM, Pohlig RT, Townsend RR, et al. Effects of aerobic exercise on vascular function in nondialysis chronic kidney disease: A randomized controlled trial. Am J Physiol Renal Physiol. (2019) 316:F898–905. doi: 10.1152/ajprenal.00539.2018
36. O’Connor EM, Koufaki P, Mercer TH, Lindup H, Nugent E, Goldsmith D, et al. Long-term pulse wave velocity outcomes with aerobic and resistance training in kidney transplant recipients-A pilot randomised controlled trial. PLoS One. (2017) 12:e0171063. doi: 10.1371/journal.pone.0171063
37. Oliveira NL, Ribeiro F, Silva G, Alves AJ, Silva N, Guimarães JT, et al. Effect of exercise-based cardiac rehabilitation on arterial stiffness and inflammatory and endothelial dysfunction biomarkers: A randomized controlled trial of myocardial infarction patients. Atherosclerosis. (2015) 239:150–7. doi: 10.1016/j.atherosclerosis.2014.12.057
38. Pascoalino LN, Ciolac EG, Tavares AC, Castro RE, Ayub-Ferreira SM, Bacal F, et al. Exercise training improves ambulatory blood pressure but not arterial stiffness in heart transplant recipients. J Heart Lung Transplant. (2015) 34:693–700. doi: 10.1016/j.healun.2014.11.013
39. Norton K, Norton L, Sadgrove D. Position statement on physical activity and exercise intensity terminology. J Sci Med Sport. (2010) 13:496–502. doi: 10.1016/j.jsams.2009.09.008
40. Sherlock L, Fournier S, DeVallance E, Lee K, Carte S. Effects of shallow water aerobic exercise training on arterial stiffness and pulse wave analysis in older individuals. Int J Aquatic Res Educ. (2014) 8:310–20.
41. Okamoto T, Hashimoto Y, Kobayashi R. Effects of interval walking training compared to normal walking training on cognitive function and arterial function in older adults: A randomized controlled trial. Aging Clin Exp Res. (2019) 31:1451–9. doi: 10.1007/s40520-018-1093-8
42. Canepa M, AlGhatrif M, Pestelli G, Kankaria R, Makrogiannis S, Strait JB, et al. Impact of central obesity on the estimation of carotid-femoral pulse wave velocity. Am J Hypertens. (2014) 27:1209–17. doi: 10.1093/ajh/hpu038
43. Ferrara CM, Goldberg AP, Ortmeyer HK, Ryan AS. Effects of aerobic and resistive exercise training on glucose disposal and skeletal muscle metabolism in older men. J Gerontol A Biol Sci Med Sci. (2006) 61:480–7. doi: 10.1093/gerona/61.5.480
44. Geng L, Liao B, Jin L, Huang Z, Triggle CR, Ding H, et al. Exercise alleviates obesity-induced metabolic dysfunction via enhancing FGF21 sensitivity in adipose tissues. Cell Rep. (2019) 26:2738–52.e4. doi: 10.1016/j.celrep.2019.02.014
45. Jennersjö P, Ludvigsson J, Länne T, Nystrom FH, Ernerudh J, Östgren CJ. Pedometer-determined physical activity is linked to low systemic inflammation and low arterial stiffness in Type 2 diabetes. Diabet Med. (2012) 29:1119–25. doi: 10.1111/j.1464-5491.2012.03621.x
46. Lin HF, Liu CK, Liao YC, Lin RT, Chen CS, Juo SH. The risk of the metabolic syndrome on carotid thickness and stiffness: Sex and age specific effects. Atherosclerosis. (2010) 210:155–9. doi: 10.1016/j.atherosclerosis.2009.11.027
47. Tuttolomondo A, Di Raimondo D, Di Sciacca R, Pecoraro R, Arnao V, Buttà C, et al. Arterial stiffness and ischemic stroke in subjects with and without metabolic syndrome. Atherosclerosis. (2012) 225:216–9. doi: 10.1016/j.atherosclerosis.2012.08.027
48. Ouchi N, Kobayashi H, Kihara S, Kumada M, Sato K, Inoue T, et al. Adiponectin stimulates angiogenesis by promoting cross-talk between AMP-activated protein kinase and Akt signaling in endothelial cells. J Biol Chem. (2004) 279:1304–9. doi: 10.1074/jbc.M310389200
49. Di Pino A, Alagona C, Piro S, Calanna S, Spadaro L, Palermo F, et al. Separate impact of metabolic syndrome and altered glucose tolerance on early markers of vascular injuries. Atherosclerosis. (2012) 223:458–62. doi: 10.1016/j.atherosclerosis.2012.05.008
50. O’Rourke MF, Hashimoto J. Arterial stiffness: A modifiable cardiovascular risk factor? J Cardiopulm Rehabil Prev. (2008) 28:225–37. doi: 10.1097/01.HCR.0000327179.21498.38
51. Scuteri A, Cunha PG, Agabiti Rosei E, Badariere J, Bekaert S, Cockcroft JR, et al. Arterial stiffness and influences of the metabolic syndrome: A cross-countries study. Atherosclerosis. (2014) 233:654–60. doi: 10.1016/j.atherosclerosis.2014.01.041
52. Scuteri A, Najjar SS, Muller DC, Andres R, Hougaku H, Metter EJ, et al. Metabolic syndrome amplifies the age-associated increases in vascular thickness and stiffness. J Am Coll Cardiol. (2004) 43:1388–95. doi: 10.1016/j.jacc.2003.10.061
53. Vieira AF, Costa RR, Macedo RC, Coconcelli L, Kruel LF. Effects of aerobic exercise performed in fasted v. fed state on fat and carbohydrate metabolism in adults: A systematic review and meta-analysis. Br J Nutr. (2016) 116:1153–64. doi: 10.1017/S0007114516003160
54. Fahlman MM, Boardley D, Lambert CP, Flynn MG. Effects of endurance training and resistance training on plasma lipoprotein profiles in elderly women. J Gerontol A Biol Sci Med Sci. (2002) 57:B54–60. doi: 10.1093/gerona/57.2.b54
55. Mohanka M, Irwin M, Heckbert SR, Yasui Y, Sorensen B, Chubak J, et al. Serum lipoproteins in overweight/obese postmenopausal women: A one-year exercise trial. Med Sci Sports Exerc. (2006) 38:231–9. doi: 10.1249/01.mss.0000184584.95000.e4
56. Taddei S, Galetta F, Virdis A, Ghiadoni L, Salvetti G, Franzoni F, et al. Physical activity prevents age-related impairment in nitric oxide availability in elderly athletes. Circulation. (2000) 101:2896–901. doi: 10.1161/01.cir.101.25.2896
57. Beck DT, Martin JS, Casey DP, Braith RW. Exercise training reduces peripheral arterial stiffness and myocardial oxygen demand in young prehypertensive subjects. Am J Hypertens. (2013) 26:1093–102. doi: 10.1093/ajh/hpt080
58. Maeda S, Iemitsu M, Miyauchi T, Kuno S, Matsuda M, Tanaka H. Aortic stiffness and aerobic exercise: Mechanistic insight from microarray analyses. Med Sci Sports Exerc. (2005) 37:1710–6. doi: 10.1249/01.mss.0000175052.37087.f8
59. Kearney TM, Murphy MH, Davison GW, O’Kane MJ, Gallagher AM. Accumulated brisk walking reduces arterial stiffness in overweight adults: Evidence from a randomized control trial. J Am Soc Hypertens. (2014) 8:117–26. doi: 10.1016/j.jash.2013.10.001
60. McEniery CM, Wallace S, Mackenzie IS, McDonnell B, Yasmin, Newby DE, et al. Endothelial function is associated with pulse pressure, pulse wave velocity, and augmentation index in healthy humans. Hypertension. (2006) 48:602–8. doi: 10.1161/01.HYP.0000239206.64270.5f
61. Collier SR, Kanaley JA, Carhart R Jr., Frechette V, Tobin MM, Hall AK, et al. Effect of 4 weeks of aerobic or resistance exercise training on arterial stiffness, blood flow and blood pressure in pre- and stage-1 hypertensives. J Hum Hypertens. (2008) 22:678–86. doi: 10.1038/jhh.2008.36
62. Currie KD, Thomas SG, Goodman JM. Effects of short-term endurance exercise training on vascular function in young males. Eur J Appl Physiol. (2009) 107:211–8. doi: 10.1007/s00421-009-1116-4
63. Kakiyama T, Sugawara J, Murakami H, Maeda S, Kuno S, Matsuda M. Effects of short-term endurance training on aortic distensibility in young males. Med Sci Sports Exerc. (2005) 37:267–71. doi: 10.1249/01.mss.0000152733.12578.5a
64. Oudegeest-Sander MH, Olde Rikkert MG, Smits P, Thijssen DH, van Dijk AP, Levine BD, et al. The effect of an advanced glycation end-product crosslink breaker and exercise training on vascular function in older individuals: A randomized factorial design trial. Exp Gerontol. (2013) 48:1509–17. doi: 10.1016/j.exger.2013.10.009
65. Belardinelli R, Perna GP. Vasomotor reactivity evaluation in cardiac rehabilitation. Monaldi Arch Chest Dis. (2002) 58:79–86.
66. Smart NA, Dieberg G, Giallauria F. Intermittent versus continuous exercise training in chronic heart failure: A meta-analysis. Int J Cardiol. (2013) 166:352–8. doi: 10.1016/j.ijcard.2011.10.075
67. D’Ascenzi F, Cavigli L, Pagliaro A, Focardi M, Valente S, Cameli M, et al. Clinician approach to cardiopulmonary exercise testing for exercise prescription in patients at risk of and with cardiovascular disease. Br J Sports Med. (2022) bjsorts–2021–105261. [Epub ahead of print]. doi: 10.1136/bjsports-2021-105261
68. Anselmi F, Cavigli L, Pagliaro A, Valente S, Valentini F, Cameli M, et al. The importance of ventilatory thresholds to define aerobic exercise intensity in cardiac patients and healthy subjects. Scand J Med Sci Sports. (2021) 31:1796–808. doi: 10.1111/sms.14007
69. Hansen D, Abreu A, Ambrosetti M, Cornelissen V, Gevaert A, Kemps H, et al. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: Why and how: A position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. (2022) 29:230–45. doi: 10.1093/eurjpc/zwab007
70. Alecu C, Gueguen R, Aubry C, Salvi P, Perret-Guillaume C, Ducrocq X, et al. Determinants of arterial stiffness in an apparently healthy population over 60 years. J Hum Hypertens. (2006) 20:749–56. doi: 10.1038/sj.jhh.1002072
71. Brand JS, van der Schouw YT. Testosterone, SHBG and cardiovascular health in postmenopausal women. Int J Impot Res. (2010) 22:91–104. doi: 10.1038/ijir.2009.64
72. Davison SL, Bell R, Donath S, Montalto JG, Davis SR. Androgen levels in adult females: Changes with age, menopause, and oophorectomy. J Clin Endocrinol Metab. (2005) 90:3847–53. doi: 10.1210/jc.2005-0212
73. Ozemek C, Hildreth KL, Blatchford PJ, Hurt KJ, Bok R, Seals DR, et al. Effects of resveratrol or estradiol on postexercise endothelial function in estrogen-deficient postmenopausal women. J Appl Physiol (1985). (2020) 128:739–47. doi: 10.1152/japplphysiol.00488.2019
74. Benetos A, Adamopoulos C, Bureau JM, Temmar M, Labat C, Bean K, et al. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation. (2002) 105:1202–7. doi: 10.1161/hc1002.105135
75. Asmar R, Benetos A, London G, Hugue C, Weiss Y, Topouchian J, et al. Aortic distensibility in normotensive, untreated and treated hypertensive patients. Blood Press. (1995) 4:48–54. doi: 10.3109/08037059509077567
76. Madden KM, Lockhart C, Cuff D, Potter TF, Meneilly GS. Aerobic training-induced improvements in arterial stiffness are not sustained in older adults with multiple cardiovascular risk factors. J Hum Hypertens. (2013) 27:335–9. doi: 10.1038/jhh.2012.38
Keywords: aerobic exercise, arterial stiffness, pulse wave velocity, middle-aged people, elderly people
Citation: Li G, Lv Y, Su Q, You Q and Yu L (2022) The effect of aerobic exercise on pulse wave velocity in middle-aged and elderly people: A systematic review and meta-analysis of randomized controlled trials. Front. Cardiovasc. Med. 9:960096. doi: 10.3389/fcvm.2022.960096
Received: 02 June 2022; Accepted: 28 July 2022;
Published: 18 August 2022.
Edited by:
Flavio D’Ascenzi, University of Siena, ItalyReviewed by:
Nataša Marčun Varda, Maribor University Medical Centre, SloveniaCopyright © 2022 Li, Lv, Su, You and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laikang Yu, eXVsYWlrYW5nQDEyNi5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.