- 1Division of Cardiology, Department of Medicine, Samsung Medical Center, Heart Vascular Stroke Institute, Sungkyunkwan University School of Medicine, Seoul, South Korea
- 2Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea
Background: No data is available on delirium prediction models in the cardiac intensive care unit (CICU), although preexisting delirium prediction models [PREdiction of DELIRium in ICu patients (PRE-DELIRIC) and Early PREdiction of DELIRium in ICu patients (E-PRE-DELIRIC)] were developed and validated based on a population admitted to the general intensive care unit (ICU). Therefore, we externally validated the usefulness of the PRE-DELIRIC and E-PRE-DELIRIC models and compared their predictive performance in patients admitted to the CICU.
Methods: A total of 2,724 patients admitted to the CICU were enrolled between September 2012 and December 2018. Delirium was defined as at least one positive Confusion Assessment Method for the ICU (CAM-ICU) which was screened at least once every 8 h. The PRE-DELIRIC value was calculated within 24 h of CICU admission, and the E-PRE-DELIRIC value was calculated at CICU admission. The predictive performance of the models was evaluated by using the area under the receiver operating characteristic (AUROC) curve, and the calibration slope was assessed graphically by plotting.
Results: Delirium occurred in 677 patients (24.8%) when the patients were assessed thrice daily until 7 days of the CICU stay. The AUROC curve for the prediction of delirium was significantly greater for PRE-DELIRIC values [0.84, 95% confidence interval (CI): 0.82–0.86] than for E-PRE-DELIRIC values (0.79, 95% CI: 0.77–0.80) [z score of −6.24 (p < 0.001)]. Net reclassification improvement for the prediction of delirium increased by 0.27 (95% CI: 0.21–0.32, p < 0.001). Calibration was acceptable in the PRE-DELIRIC model (Hosmer-Lemeshow p = 0.170) but not in the E-PRE-DELIRIC model (Hosmer-Lemeshow p < 0.001).
Conclusion: Although both models have good predictive performance for the development of delirium, even in critically ill cardiac patients, the performance of the PRE-DELIRIC model might be superior to that of the E-PRE-DELIRIC model. Further studies are required to confirm our results and design a specific delirium prediction model for CICU patients.
Introduction
Delirium, defined as acute brain dysfunction characterized by a fluctuating disturbance of attention, awareness, and cognitive function caused by an underlying medical condition, is associated with prolonged hospital admission, increased health care costs, and substantially increased morbidity and mortality (1, 2). Therefore, efforts have been made to detect delirium in patients who may benefit from delirium prevention, and several delirium prediction models have been developed in patients admitted to a medical and/or mixed intensive care unit (ICU).
Based on the data from the general ICU patients, the PREdiction of DELIRium in ICu patients (PRE-DELIRIC) model was developed using 10 predictors that could be obtained within 24 h of ICU admission (3). For the early prediction of the risk of delirium in ICU patients, the Early PREdiction of DELIRium in ICu patients (E-PRE-DELIRIC) model was developed using nine predictors that could be collected at the time of ICU admission (4). Both models included data on age, blood urea concentrations, need for urgent admission, and main diagnosis at the time of admission as predictors. The PRE-DELIRIC model included data on the severity score, the use of opioids and sedatives, metabolic acidosis, mentality, and infection, and the E-PRE-DELIRIC model included data on the history of cognitive impairment and alcohol abuse, mean arterial blood pressure, use of corticosteroids, and present of respiratory failure, as additional predictors. These models showed acceptable performance in different cohorts and patients admitted to the general ICU (5–7).
Cardiac ICUs (CICUs) have evolved from units that focus exclusively on patients with acute myocardial infarction to units that provide comprehensive critical care for patients with various cardiovascular diseases, patients requiring hemodynamic monitoring, and patients with mechanical circulatory devices for cardiogenic shock (8). Furthermore, age, the severity of illness, and comorbidities in patients admitted to the CICU have increased, and patients requiring admission to the ICU and CICU overlap significantly (9). Accordingly, delirium, which has been reported to have prognostic implications, is a common symptom in critically ill cardiac patients (10). However, to date, there has been no evidence that delirium prediction models validated in the general ICU apply to patients admitted to the CICU.
Therefore, we sought to investigate the usefulness of the PRE-DELIRIC and E-PRE-DELIRIC models for detecting the risk of developing delirium and compare the predictive performance of the two models in patients admitted to the CICU.
Methods
Study population and cardiac intensive care unit setting
A retrospective cohort study was conducted and this study included 4,663 patients aged >18 years who were admitted to the CICU between September 2012 and December 2018. Exclusion criteria were as follows; (1) Patients who stayed in the ICU for <24 h (n = 1,397), (2) those who could not complete delirium assessment (n = 480), or (3) those whose data for calculation of delirium prediction models were not available (n = 62). Finally, 2,724 patients were included in this analysis (Figure 1).
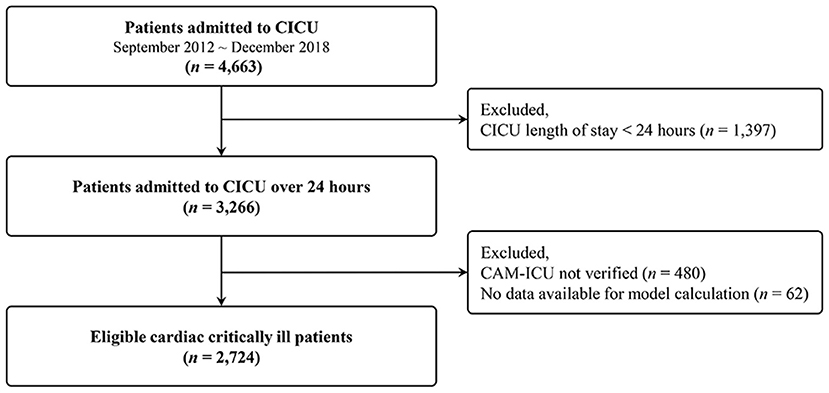
Figure 1. Study flow diagram. CICU, cardiac intensive care unit; CAM-ICU, confusion assessment method for the intensive care unit; LOS, length of stay.
Our CICU is a 12-bed unit that provides comprehensive critical care to patients with various cardiovascular diseases. Details of the Samsung Medical Center's CICU setting have been described in previous reports (11, 12). In brief, the CICU provides non-invasive and invasive devices for monitoring the hemodynamic and cardiovascular support statuses, including mechanical ventilation and extracorporeal membrane oxygenation (ECMO). The nurse-to-patient ratio is 1:2, and level 1 care is provided, which is managed by a dedicated cardiac intensivist (13). Cardiac surgery support is readily available. In addition, multidisciplinary care is provided through consultation with a dietitian, pharmacist, and respiratory care practitioner. For general intensive care, clinical practice guidelines published by the Society of Critical Care Medicine are adopted (14).
This study was approved by the Institutional Review Board of Samsung Medical Center. The requirement for written informed consent was waived because of the retrospective nature of the study (IRB No. 2020-10-102).
Data collection and definitions
Clinical, laboratory, and outcome data were collected by a trained study coordinator after reviewing the medical records. The confusion assessment method for the ICU (CAM-ICU) was performed by nurses thrice a day in patients with a Richmond agitation-sedation scale score of −3 (indicating movement or eye-opening to voice but no eye contact) or higher (15). Delirium was defined according to the CAM-ICU. The CAM-ICU was screened at least once every 8 h by well-trained intensive care nurses, and the recorded CAM-ICU value was re-checked daily by a senior nurse. In this study, we evaluated delirium within 7 days of the CICU stay. The PRE-DELIRIC model was calculated using predictors within 24 h of CICU admission, and the E-PRE-DELIRIC model was evaluated using predictors at CICU admission (3, 4). The detail of the calculation of PRE-DELIRIC and E-PRE-DELIRIC model was described in Supplementary Table 1.
Statistical analysis
The data are summarized using descriptive statistics: numbers and percentages are calculated for categorical variables, while continuous variables are summarized as medians with interquartile ranges (IQR; 25th and 75th percentiles). The discriminative power of the two models was assessed using the area under the receiver operating characteristic curve (AUROC), and their predictive performance was compared using DeLong's test (16). Calibration was assessed graphically by plotting the observed outcome frequencies against the mean predicted outcome probabilities or risks. For all analyses, statistical significance was set at p < 0.05. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and R 4.0.2 (Vienna, Austria; http://www.R-project.org).
Results
Patient characteristics
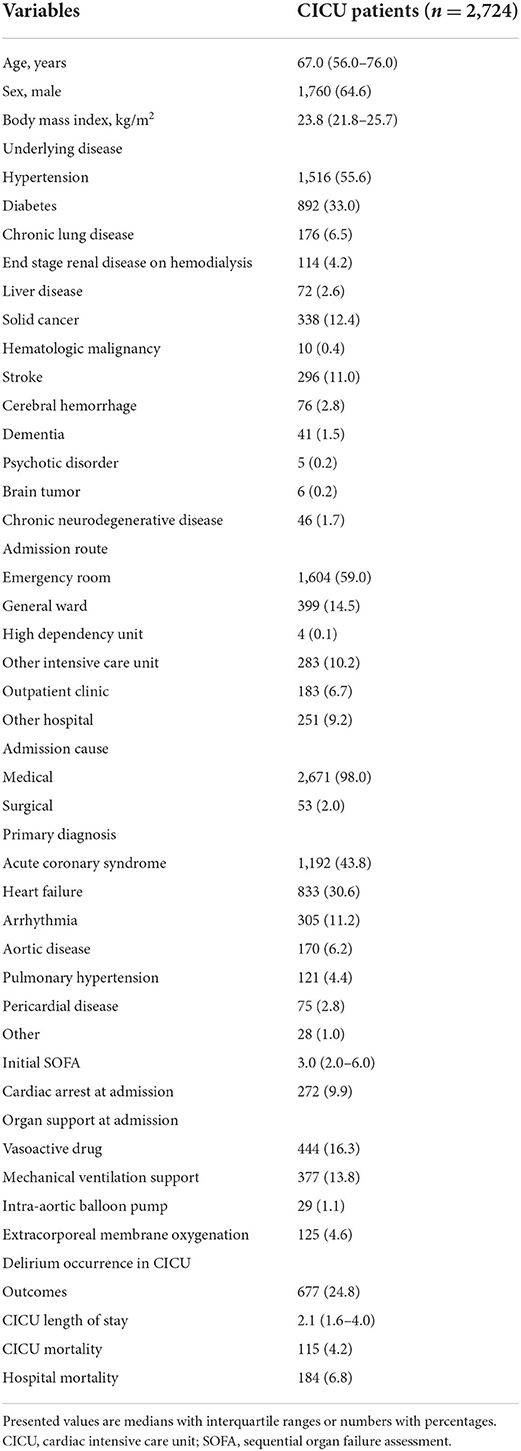
Table 1 provides an overview of the characteristics of the CICU patients. The median age was 67.0 (IQR 56.0–76.0) years, and 64.6% of the patients were males. The most common underlying disease was hypertension (55.5%), followed by diabetes mellitus (33.0%) and solid cancer (12.4%). Stroke (11.0%) was the most common underlying neurological disease, and 2.8% of all patients had a history of cerebral hemorrhage. Patients were commonly admitted from the emergency room (59.0%) and admitted for medical management (98.0%). Acute coronary syndrome (43.8%), heart failure (30.6%), and arrhythmia (11.2%) were the most frequent diagnoses at CICU admission. The median Sequential Organ Failure Assessment score was 3.0 (IQR 2.0–6.0). Two hundred and seventy-two (9.9%) patients received cardiopulmonary resuscitation at CICU admission, and vasoactive drugs were used in 16.3%, mechanical ventilators in 13.8%, and ECMO in 4.6% of the patients.
CICU patient characteristics according to the variables of the delirium prediction models are shown in Table 2. Of the 2,724 patients, 15.1% had drug-induced coma, and 8.8% were in coma due to miscellaneous within 24 h of CICU admission. In addition, 506 (20%) patients used opioids, and 1,315 (48.2%) patients received sedative drugs within 24 h of CICU admission. These data were used to calculate the PRE-DELIRIC model values. At CICU admission, 1,412 (52.0%) patients presented with respiratory failure, and 38 (1.0%) patients used corticosteroids. These data were also used to calculate the E-PRE-DELIRIC model values.
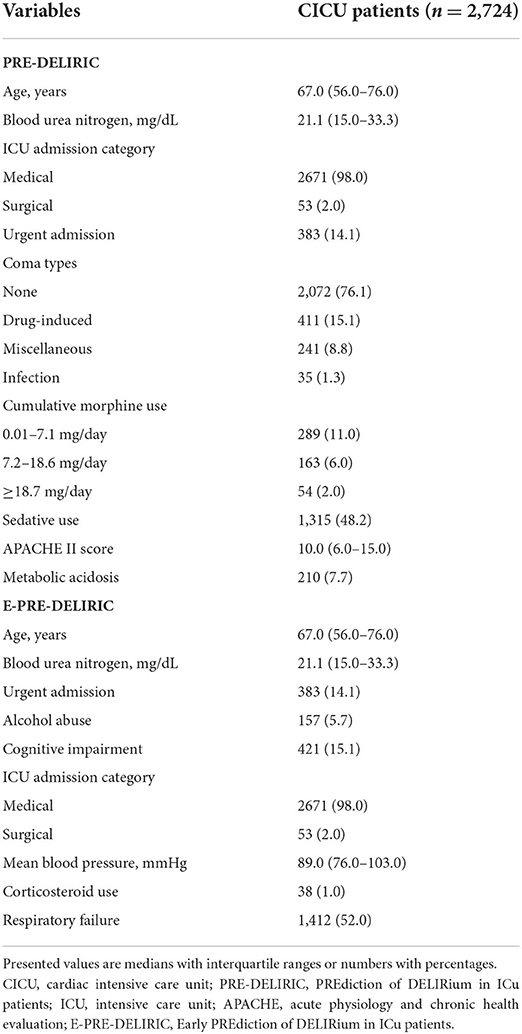
Table 2. Patient characteristics of the study with delirium assessment tools according to the original delirium study.
Predictive performances of the PRE-DELIRIC and E-PRE-DELIRIC models
Of all the patients, 677 (24.8%) experienced delirium during CICU admission within 7 days. Overall, 155 (4.2%) patients died in the CICU, and the hospital mortality rate was 6.8%. The predictive performance for the development of delirium and its comparison for the two models are presented in Figure 2. The AUROC of the PRE-DELIRIC model was 0.84 [95% confidence interval (CI): 0.82–0.86, p < 0.001], and the cut-off point was 0.56 (sensitivity and specificity were 0.68 and 0.78, respectively). The AUROC of the E-PRE-DELIRIC model was 0.79 (95% CI: 0.77–0.80, p < 0.001), and the cut-off point was 0.74 (sensitivity and specificity were 0.76 and 0.77, respectively). The PRE-DELIRIC model showed a significantly better statistical performance than the E-PRE-DELIRIC model for predicting the development of delirium [z score of −6.25 (p < 0.001)]. The PRE-DELIRIC and E-PRE-DELIRIC models were well-calibrated; however, calibration was only acceptable in the PRE-DELIRIC model (Hosmer-Lemeshow p = 0.17) but not in the E-PRE-DELIRIC model (p < 0.001) (Figure 3).
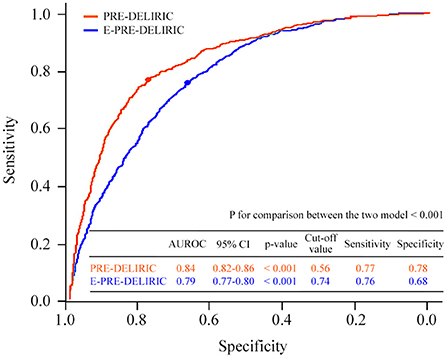
Figure 2. Comparison of the predictive performances of the two delirium models. AUROC, area under the receiver operating characteristic; PRE-DELIRIC, PREdiction of DELIRium in ICu patients; E-PRE-DELIRIC, Early PREdiction of DELIRium in ICu patients.
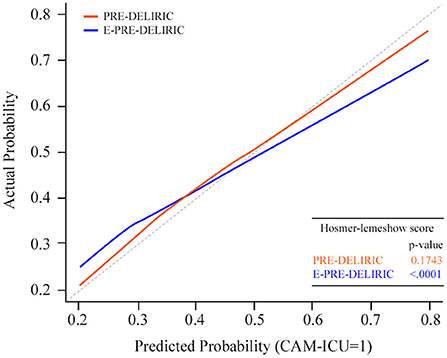
Figure 3. Calibration plot of both prediction models. Calibration plot [with 95% confidence interval (CI), blue line] by 10 prediction values for the PRE-DELIRIC model. Calibration plot (with 95% CI, red line), using nine prediction values for the E-PRE-DELIRIC model. The dashed line indicates perfect calibration. PRE-DELIRIC, PREdiction of DELIRium in ICu patients; E-PRE-DELIRIC, Early PREdiction of DELIRium in ICu patients.
Discussion
We externally validated the usefulness of two delirium prediction models (PRE-DELIRIC and E-PRE-DELIRIC) and compared their performance in CICU patients. The major findings of this study were that both prediction models for the development of delirium had fair to good predictive performance even in critically ill cardiac patients; in particular, the PRE-DELIRIC model predicted the development of delirium better and was well-calibrated. To the best of our knowledge, this is the first study to apply preexisting delirium prediction models to patients admitted to the CICU.
Some differences between the general ICU and CICU remain, such as the patient population, ICU environment, management of mechanical circulatory support devices, and medication prescriptions. However, since coronary care units were designed in the 1960's to monitor and treat the acute phase of myocardial infarction, profiles of patients with cardiovascular disease admitted to these units are gaining complexity and diversity (17). In addition, patients admitted to the CICU are often elderly and present with multiple comorbidities. Therefore, the incidence of delirium in the CICU has substantially increased (18), and several studies have shown that delirium is associated with morbidity and mortality in patients admitted to the CICU (19, 20). Falsini et al. reported that delirium is associated with a long and complicated hospital stay and increased mortality in elderly CICU patients (19). Similar results were found in a nationwide data analysis of patients with myocardial infarction in the United States (20). Recently, studies on delirium in patients admitted to the CICU have been actively conducted; however, there has been no study that validated delirium prediction models in the general ICU for patients admitted to the CICU.
The PRE-DELIRIC model was developed and validated in 2,361 mixed ICU patients, and this model comprised 10 variables that were available within 24 h after ICU admission. The AUROC for temporal validation showed good performance (3). However, up to 25% of ICU patients develop delirium within 24 h of admission to the ICU; therefore, a model for the early detection of the risk of developing delirium was needed (21). The E-PRE-DELIRIC model was developed for this purpose at the time of ICU admission. The E-PRE-DELIRIC model was developed and validated in 2,914 patients at 13 ICUs from 7 countries and comprised nine variables that could be evaluated upon admission to the ICU. In this study, we evaluated the usefulness of the PRE-DELIRIC and E-PRE-DELIRIC models for detecting the risk of developing delirium; the PRE-DELIRIC model showed good performance, and the E-PRE-DELIRIC model showed fair performance in critically ill cardiac patients. One unanticipated finding was that the performance of the two models for patients admitted to the CICU was better than that for patients admitted to the general ICU, as reported in a previous study (5). In particular, the PRE-DELIRIC model showed better accuracy than the E-PRE-DELIRIC model documented using a calibration plot, and the results were similar to those of a previous study conducted in a general ICU (5). Since our study was conducted in a large-scale cohort admitted to the CICU in the era of mechanical circulatory support, these findings reflect the modern CICU environment, and the two delirium prediction models might be useful in CICU patients, as well as general or mixed ICU patients.
Delirium prevention involves understanding predisposing and precipitating risk factors. The development of delirium is complex and depends on several non-modifiable and modifiable clinical factors (22). Therefore, understanding the characteristics of patients admitted to the CICU is important. First, patients with acute heart failure complicated by coexisting acute and chronic comorbidities have increased in the CICU (23), and these patients are highly vulnerable and more elderly. In this study, we also showed that 30.6% of all CICU patients were admitted for the management of heart failure. Patients with low cardiac output due to pump failure might be easily affected by invasive procedures, sedatives, sleep deprivation, and medications during CICU stay. In addition, a previous study reported that heart failure alone was an independent risk factor for delirium (24). Second, various temporary and permanent mechanical supports and advanced procedures are often applied to critically ill cardiac patients (25, 26). These interventions might induce prolonged immobility and increased need for sedatives, resulting in an increased occurrence of delirium (27). Third, since patients with cardiogenic shock are easily affected by cerebral hypo-perfusion, which is related to systemic hypotension known to be associated with the development of delirium, delirium might be a common issue in modern and future CICUs with advanced medical devices (28, 29). Finally, the length of ICU stay differs between the CICU and medical ICU (30, 31). Indeed, there are certain differences, such as the patient characteristics, ICU environments, and ICU stay period between patients admitted to the CICU and medical or mixed ICU. The incidence rate of delirium according to age, CICU length of stay, and SOFA score were described as bar plots (Supplementary Figure 1). Accordingly, further work is required to develop a specific delirium prediction model for critically ill cardiac patients with good performance, given the unique characteristics of patients admitted to the CICU.
Our study has several limitations. First, it was subject to a selection bias, which may have influenced our findings due to its retrospective and single-center observational nature. Second, the development of delirium was counted until 7 days of ICU stay because it was relatively shorter in the CICU than in the general or mixed ICU. Only 323 (6.9%) patients were admitted for over 7 days in our cohort. Third, admission categories in our study were limited to only two types, medical and surgical, based on the CICU characteristics, while there are four types of admission categories for delirium predictive values, such as medical, surgical, traumatic, and neurological/neurosurgical in previous studies that developed two delirium models (3, 4). Forth, although delirium can be evaluated with various tools, the CAM-ICU was only used to evaluation in our CICU. Therefore, discriminative power of two models might be changed when delirium was assessed with other tools. Lastly, one of the variables for the PRE-DELIRIC model, cognitive impairment, was not evaluated by the cognitive impairment assessment tools.
Conclusion
The PRE-DELIRIC model has an excellent predictive performance for the development of delirium and its performance is better than that of the E-PRE-DELIRIC model, although the E-PRE-DELIRIC model also has good predictive performance in critically ill cardiac patients admitted to the CICU. Further studies are required to confirm our results and design a specific delirium prediction model for CICU patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the Institutional Review Board of Samsung Medical Center. The requirement for written informed consent was waived because of the retrospective nature of the study (IRB No. 2020-10 102).
Author contributions
SK, R-EK, and JY: data collection, statistical analysis, manuscript draft, and responsible for the overall content as guarantors. All authors: data analysis and interpretation, critical revision, editing, and approval of the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.947149/full#supplementary-material
Abbreviations
AUROC, area under the receiver operating characteristic curve; CAM-ICU, confusion assessment method for the intensive care unit; CI, confidence interval; CICU, cardiac intensive care unit; ECMO, extracorporeal membrane oxygenation; E-PRE-DELIRIC, Early PREdiction of DELIRium in ICu patients; ICU, intensive care unit; IQR, interquartile ranges; PRE-DELIRIC, PREdiction of DELIRium in ICu patients.
References
1. Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. (2009) 180:1092–7. doi: 10.1164/rccm.200904-0537OC
2. van den Boogaard M, Schoonhoven L, Evers AW, van der Hoeven JG, van Achterberg T, Pickkers P. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. (2012) 40:112–8. doi: 10.1097/CCM.0b013e31822e9fc9
3. van den Boogaard M, Pickkers P, Slooter AJ, Kuiper MA, Spronk PE, van der Voort PH, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ. (2012) 344:e420. doi: 10.1136/bmj.e420
4. Wassenaar A, van den Boogaard M, van Achterberg T, Slooter AJ, Kuiper MA, Hoogendoorn ME, et al. Multinational development and validation of an early prediction model for delirium in ICU patients. Intensive Care Med. (2015) 41:1048–56. doi: 10.1007/s00134-015-3777-2
5. Wassenaar A, Schoonhoven L, Devlin JW, van Haren FMP, Slooter AJC, Jorens PG, et al. Delirium prediction in the intensive care unit: comparison of two delirium prediction models. Crit Care. (2018) 22:114. doi: 10.1186/s13054-018-2037-6
6. Green C, Bonavia W, Toh C, Tiruvoipati R. Prediction of ICU delirium: validation of current delirium predictive models in routine clinical practice. Crit Care Med. (2019) 47:428–35. doi: 10.1097/CCM.0000000000003577
7. Wassenaar A, Schoonhoven L, Devlin JW, van Haren FMP, Slooter AJC, Jorens PG, et al. External validation of two models to predict delirium in critically ill adults using either the confusion assessment method-ICU or the intensive care delirium screening checklist for delirium assessment. Crit Care Med. (2019) 47:e827–35. doi: 10.1097/CCM.0000000000003911
8. Frishman WH, Alpert JS, Killip T 3rd. The coronary (cardiac) care unit at 50 years: a major advance in the practice of hospital medicine. Am J Med. (2017) 130:1005–6. doi: 10.1016/j.amjmed.2017.05.022
9. Katz JN, Shah BR, Volz EM, Horton JR, Shaw LK, Newby LK, et al. Evolution of the coronary care unit: clinical characteristics and temporal trends in healthcare delivery and outcomes. Crit Care Med. (2010) 38:375–81. doi: 10.1097/CCM.0b013e3181cb0a63
10. Naksuk N, Thongprayoon C, Park JY, Sharma S, Gaba P, Rosenbaum AN, et al. Editor's choice-clinical impact of delirium and antipsychotic therapy: 10-Year experience from a referral coronary care unit. Eur Heart J Acute Cardiovasc Care. (2017) 6:560–8. doi: 10.1177/2048872615592232
11. Na SJ, Chung CR, Jeon K, Park CM, Suh GY, Ahn JH, et al. Association between presence of a cardiac intensivist and mortality in an adult cardiac care unit. J Am Coll Cardiol. (2016) 68:2637–48. doi: 10.1016/j.jacc.2016.09.947
12. Na SJ, Park TK, Lee GY, Cho YH, Chung CR, Jeon K, et al. Impact of a cardiac intensivist on mortality in patients with cardiogenic shock. Int J Cardiol. (2017) 244:220–5. doi: 10.1016/j.ijcard.2017.06.082
13. Morrow DA, Fang JC, Fintel DJ, Granger CB, Katz JN, Kushner FG, et al. Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. (2012) 126:1408–28. doi: 10.1161/CIR.0b013e31826890b0
14. Devlin JW, Skrobik Y, Gelinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. (2018) 46:e825–73. doi: 10.1097/CCM.0000000000003299
15. Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. (2001) 29:1370–9. doi: 10.1097/00003246-200107000-00012
16. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. (1988) 44:837–45. doi: 10.2307/2531595
17. Holland EM, Moss TJ. Acute noncardiovascular illness in the cardiac intensive care unit. J Am Coll Cardiol. (2017) 69:1999–2007. doi: 10.1016/j.jacc.2017.02.033
18. Grotti S, Falsini G. Delirium in cardiac patients. Eur Heart J. (2017) 38:2244. doi: 10.1093/eurheartj/ehx380
19. Falsini G, Grotti S, Porto I, Toccafondi G, Fraticelli A, Angioli P, et al. Long-term prognostic value of delirium in elderly patients with acute cardiac diseases admitted to two cardiac intensive care units: a prospective study (DELIRIUM CORDIS). Eur Heart J Acute Cardiovasc Care. (2018) 7:661–70. doi: 10.1177/2048872617695235
20. Abdullah A, Eigbire G, Salama A, Wahab A, Awadalla M, Hoefen R, et al. Impact of delirium on patients hospitalized for myocardial infarction: a propensity score analysis of the National Inpatient Sample. Clin Cardiol. (2018) 41:910–5. doi: 10.1002/clc.22972
21. Serafim RB, Dutra MF, Saddy F, Tura B, de Castro JE, Villarinho LC, et al. Delirium in postoperative nonventilated intensive care patients: risk factors and outcomes. Ann Intensive Care. (2012) 2:51. doi: 10.1186/2110-5820-2-51
23. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. (2011) 306:1669–78. doi: 10.1001/jama.2011.1474
24. Hutt E, Frederickson E, Ecord M, Kramer AM. Associations among processes and outcomes of care for Medicare nursing home residents with acute heart failure. J Am Med Dir Assoc. (2003) 4:195–9. doi: 10.1016/S1525-8610(04)70345-X
25. Vallabhajosyula S, Prasad A, Bell MR, Sandhu GS, Eleid MF, Dunlay SM, et al. Extracorporeal membrane oxygenation use in acute myocardial infarction in the United States, 2000 to 2014. Circ Heart Fail. (2019) 12:e005929. doi: 10.1161/CIRCHEARTFAILURE.119.005929
26. Mentias A, Sarrazin MV, Desai M, Kapadia S, Cram P, Girotra S. Expansion of transcatheter aortic valve replacement in the United States. Am Heart J. (2021) 234:23–30. doi: 10.1016/j.ahj.2020.12.018
27. Abawi M, Nijhoff F, Agostoni P, Emmelot-Vonk MH, de Vries R, Doevendans PA, et al. Incidence, predictive factors, and effect of delirium after transcatheter aortic valve replacement. JACC Cardiovasc Interv. (2016) 9:160–8. doi: 10.1016/j.jcin.2015.09.037
28. Yokota H, Ogawa S, Kurokawa A, Yamamoto Y. Regional cerebral blood flow in delirium patients. Psychiatry Clin Neurosci. (2003) 57:337–9. doi: 10.1046/j.1440-1819.2003.01126.x
29. Honda S, Nagai T, Sugano Y, Okada A, Asaumi Y, Aiba T, et al. Prevalence, determinants, and prognostic significance of delirium in patients with acute heart failure. Int J Cardiol. (2016) 222:521–7. doi: 10.1016/j.ijcard.2016.07.236
30. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. (2016) 315:788–800. doi: 10.1001/jama.2016.0291
31. Wirz Y, Meier MA, Bouadma L, Luyt CE, Wolff M, Chastre J, et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomized trials. Crit Care. (2018) 22:191. doi: 10.1186/s13054-018-2125-7
Keywords: delirium prediction, prediction model, cardiac intensive care unit, Early PREdiction of DELIRium, PREdiction of DELIRium
Citation: Kim SE, Ko R-E, Na SJ, Chung CR, Choi KH, Kim D, Park TK, Lee JM, Song YB, Choi J-O, Hahn J-Y, Choi S-H, Gwon H-C and Yang JH (2022) External validation and comparison of two delirium prediction models in patients admitted to the cardiac intensive care unit. Front. Cardiovasc. Med. 9:947149. doi: 10.3389/fcvm.2022.947149
Received: 18 May 2022; Accepted: 18 July 2022;
Published: 03 August 2022.
Edited by:
Gen-Min Lin, Hualien Armed Forces General Hospital, TaiwanReviewed by:
Yibo He, Guangdong Provincial People's Hospital, ChinaSabina Krupa, University of Rzeszow, Poland
Copyright © 2022 Kim, Ko, Na, Chung, Choi, Kim, Park, Lee, Song, Choi, Hahn, Choi, Gwon and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jeong Hoon Yang, jhysmc@gmail.com
†These authors have contributed equally to this work
 Sung Eun Kim1†
Sung Eun Kim1† Ryoung-Eun Ko
Ryoung-Eun Ko Soo Jin Na
Soo Jin Na Darae Kim
Darae Kim Young Bin Song
Young Bin Song Seung-Hyuk Choi
Seung-Hyuk Choi Jeong Hoon Yang
Jeong Hoon Yang