
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 15 August 2022
Sec. Hypertension
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.936018
This article is part of the Research Topic Physical Activity and Exercise for the Prevention and Management of Cardiovascular Risk and Cardiovascular Disease View all 8 articles
Background: As a therapy to prevent and treat hypertension, exercise is widely used in clinical practice. But due to the lack of documentary evidence, Baduanjin as a relaxed and convenient mode of exercise is not currently recommended by professional health organizations to treat hypertension. The purpose of this article is to examine the efficacy of Baduanjin as an antihypertensive exercise therapy.
Methods: Our systematic retrieved of the entire relevant literatures in 12 databases. Finally, 28 eligible trials involving Baduanjin intervention in hypertension were included. After the quality assessment and bias risk assessment of the included trials, we analyzed the blood pressure values before and after the intervention, and performed meta-analysis on the random effect results. In order to explore the factors influencing the decrease of blood pressure, we also performed a subgroup analysis of the results.
Results: Participants (n = 2121) were adults (61.74 ± 5.85years of age, mean ± SD), with baseline blood pressure (systolic blood pressure (SBP) = 150.7 ± 9.2 mmHg, diastolic blood pressure (DBP) = 93.2 ± 8.8 mmHg). Baduanjin was practiced 7.5 ± 3.8 sessions / week for 28.2 ± 12.8 min /session for 16.7 ± 9.2 weeks. Overall, Baduanjin resulted in SBP (−9.3 mmHg, d = −1.49, 95%CI: −1.73 to −1.13) and DBP (−6.3 mmHg, d = −1.20, 95%CI: −1.51 to −0.88) vs. the control group (p < 0.001). After a subgroup analysis of age, we found that SBP heterogeneity was significantly reduced in the elderly group.
Conclusion: Our results indicate that Baduanjin can effectively reduce blood pressure (i.e., 9.3 mmHg and 6.3 mmHg of SBP and DBP reductions, respectively), and reduce the incidence rate of cardiovascular disease in hypertensive patients. In addition, we will be more likely to recommend that the elderly exercise Baduanjin.
Hypertension is a preventable risk factor of cardiovascular disease, which is closely linked to people's lifestyle. Both aerobic exercise (1) and resistance exercise (2) have been demonstrated to effectively reduce blood pressure. Through regular aerobic exercise, blood pressure (BP) can be typically decreased overall by 5 mmHg (3), the mortality of coronary heart disease (CHD) reduces 9%, the mortality of stroke reduces 14% and all-cause mortality also reduces 7% (4). Therefore, compared to using drug which may cause side effects, regular moderate- and low-intensity aerobic training should be more recommended for hypertensive patients and healthy adults. Nevertheless, due to the high requirements of aerobic exercise and resistance training on physical strength and endurance, most adults with high blood pressure are unwilling or unable to adhere to exercise, thus choose safer, less strenuous forms of exercise like Taijiquan, yoga and Baduanjin. However, compared with other forms of movement, Baduanjin is simply, convenient, inexpensive, serviceable (5), less time in practice and easier to learn. Therefore, Baduanjin is more suitable for those adults who are reluctant to exercise than Taijiquan and yoga.
Baduanjin pays attention to the rhythm coordination of breathing and movement, and improves the morphology and physiological function of the human body (1, 2). Its curative effects include improving the strength of the upper and lower limbs, promoting the cardiovascular function, promoting the respiratory system function, improving the joint flexibility, improving the balance ability and the sensibility of the middle-aged and elderly people and so on (6). Among them, the antihypertensive effect in adult patients with hypertension is one of the most commonly used curative effects in clinic (7, 8). However, due to the lack of documentary evidence, professional associations and organizations, such as the International Society of Hypertension (9), do not currently recommend Baduanjin as a non-pharmacological treatment equivalent to aerobic exercise.
Three meta-analyses currently published in English [10 to 12] had quantified the BP-lowering effect of Baduanjin, one of the meta-analyses for essential hypertension reported a standardized mean difference (SMD) of 1.80 mmHg for systolic blood pressure (SBP) and 0.22 mmHg for diastolic blood pressure (DBP) (12). A meta-analysis reported a clinical non-standardized mean difference MD of 8.52 mmHg for SBP and 4.65 mmHg for DBP (11). The 3rd meta-analysis used weighted mean differences (WMD) to quantify the resulting of 13.00 mmHg for SBP and 6.13 mmHg for DBP (10). Despite these quantitative results are meaningful, these meta-analyses have the following limitations: (a) The sample size for all meta-analyses was very small (k = 8 to 14; n = 572–1058), and only 6 to 8 databases were retrieved. (b) Heterogeneity was high (10, 11) (I2 ranged from 90 to 93%), but none of the analysis reduced the heterogeneity was performed.
To address the limitations in the above meta-analysis, we conducted a meta-analysis of the largest sample to examine the efficacy of Baduanjin in reducing blood pressure, and to explore the antihypertensive mechanism of Baduanjin. In addition, we performed a subgroup analysis to investigate the causes affecting the changes in blood pressure to provide ideas for the clinical prevention and treatment of hypertension through exercise.
The protocol of this systematic evaluation and meta-analysis procedures was registered in PROSPERO (registration number: CRD42021291953), and was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses Statement (13). According to seven inclusion criteria, the trials were eligible if the following conditions were observed: (a) adults older than 18. (b) there were no more physical diseases except for hypertension. (c) stating the intervention was Baduanjin. (d) the participant's health could support at least 4weeks of Baduanjin exercise. (e) including the non-exercise / non-dietary controls. (f) trials included BP reports pre- and post-intervention the intervention in Baduanjin and control groups and (g) all trials were peer-reviewed articles published in either English or Chinese language journals. Trials were excluded if they (a) were literature reviews, case-control trials, or animal research literature. (b) had repeated publications, unclear outcome measures, or obvious data errors. (c) included fewer than 10 samples. (d) included samples of other diseases (e.g., cardiovascular disease, diabetes). (e) involved a single Baduanjin session (i.e., an acute intervention).
We systematically searched all articles in 8 English electronic databases and 4 Chinese electronic databases (Supplementary Table 1, the complete search strategy for all queried electronic databases). Team coders screened the report twice, first with the title and abstract, and then with the full text. Additional reports were also searched in the reference lists of included trials, related reviews and meta-analysis.
We extracted the SBP and DBP as outcome indicators. We also extracted some basic characteristics that might effect a change in blood pressure, such as the mean age of trials, intervention studies, exercise intensity, teacher qualifications, medications, dietary maintenance and exercise habits. In the collection of resting BP, we used the BP value before the start of the Baduanjin intervention as the baseline BP (pre-intervention value) (14), used the BP value taken at the time point after and closest to the end of the Baduanjin intervention as the outcome indicator (post-intervention value). Since most of the trials in this literature were conducted prior to the publication of the 2020 ISH guidelines, we followed the 2020 International Society of Hypertension Global Hypertension Practice Guidelines definitions of hypertension and normotensive in our meta-analysis (9).
The Cochrane Risk-of-Bias Tool for Randomized Trials (ROB 1.0) (15) was used to evaluate the quality of methodological research, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting (RCT) and other bias.
Furthermore, we used the Methodological Index for Non-randomized Studies (MINORS) (16) to assess risk of bias in various areas, including clearly gave the research purpose, the coherence of the participants, expected data collection, the end index can properly reflect the objective, objectivity of the endpoint index evaluation, adequate follow-up time, follow-up rate is <5%, whether the sample size is estimated, whether the choice of the control group is appropriate, whether the control group is synchronized, whether the baseline is comparable among the groups, and whether the statistical analysis is appropriate (NRCTs). There were 12 evaluation indicators, each one could be scored from 0 to 2 points, the highest score was 24 points, 0 to 8 was low quality, 9 to 16 was medium quality, and 17 to 24 was high quality.
All data extractions and risk of bias assessment were carried out by teams of assessors working in pairs, and any uncertainties or disagreements were resolved by involving a third assessor, and all differences were resolved through discussion and high reliability was achieved.
Our meta-analysis was conducted to explore the antihypertensive effect of Baduanjin. Since we observed large differences in the distribution of standard deviations of baseline blood pressure in the included trials SBP (the SD ranged from 1.7 to 12.6) and DBP (the SD ranged from 0.9 to 10.8), we chose to use standardized effect sizes. Which were more robust and less biased, and have better effective compared to unstandardized effect sizes across many statistical circumstances (17).
We evaluated the potential publication bias and other reporting bias of SBP and DBP by visually observing the symmetry and distribution of funnel plots, used the tests of Begg and egger et al (18).
Notably, we included all RCT and nRCT samples. In fact, RCT (92.9%, k = 26) was much more than nRCT (7.1%, k = 2). Therefore, a sensitivity analysis was used to compare the SMD values for all trials (including RCT and nRCT) and the RCT-only trials (19). The mean effect sizes showed no difference between experiments that contained both RCT and nRCT and experiments that contained RCT-only, confirming the decision to combine RCT and nRCT for analysis.
The analysis was performed using the Stata15 version (20), and the Stata command appeared in Supplementary Table 2 (Stata command). Descriptive statistics were reported as mean ± standard deviations unless noted otherwise. Two-sided significance level was p < 0.05.
We finally included 28 Baduanjin controlled trials that met the inclusion criteria (Figure 1). A detailed list of included trials was shown in Supplementary Table 3 (reference list for the included trials).
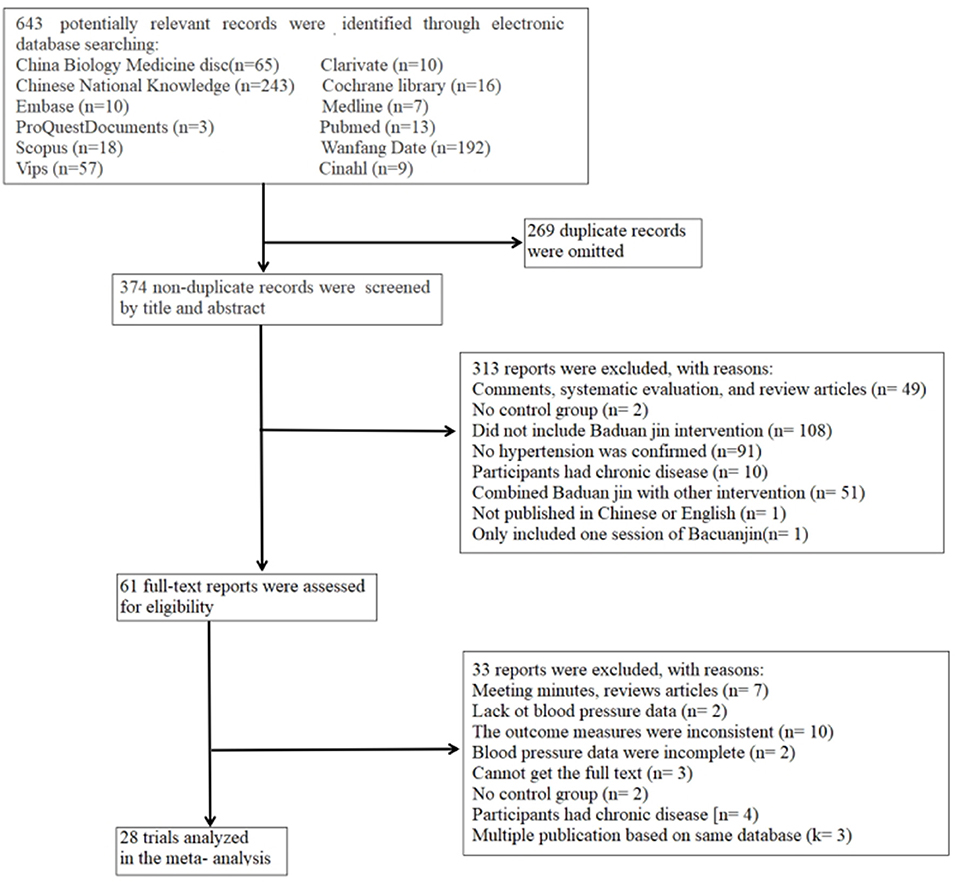
Figure 1. Flow chart detailing the systematic search of potential reports and selection process of included Baduanjin trials.
The Baduanjin intervention trials were published before 2021, including RCTs (k = 26, 92.9%) or NRCTs (k = 2, 7.1%), and all trials use BP as the primary outcome. Among them, 25 trials (89.3%) disclosed the intervention measures of the control group (Supplementary Table 4, main characteristics of the Baduanjin intervention), including activities of daily living (k = 7, 25.0%), daily care (k = 2, 7.1%), health education (k = 14, 50.0%) and daily walking (k = 2, 7.1%). The remaining 3 (10.7%) control groups did not disclose the intervention measures. All of these trials were published in English (k = 1, 3.6%) and Chinese (k = 27, 96.4%) language journals.
The risk of bias score for individual trials was shown in Supplementary Table 5 (Risk of bias for RCTs) and Supplementary Table 6 (Risk of bias for NRCTs). Based on ROB1.0, the majority of RCTs (k = 12, 80%) appeared high levels of risk of bias. Especially, blinding of outcome assessment was rated as the area with the highest risk of bias (k = 24, 92.3%). Meanwhile, nRCTs (k = 2,100%) appeared lower risk of bias based on MINORS, and objectivity of the endpoint index evaluation was rated as the area with a higher risk of bias proportion of trials with risk (k = 2,100%).
The baseline sample characteristics of Baduanjin (n = 1061) group and control group (n = 1060) were similar (p > 0.05) (Supplementary Table 7 baseline sample characteristics). On average, participants (n = 2121) were adults of all ages with hypertension (SBP = 150.7 ± 9.2mmHg / DBP = 93.2 ± 8.8 mmHg), mostly of whom were older adults (61.8 ± 6.0 years), and the proportion of male and female participating was proximity, including the proportion of female (49.91 ± 7.81%). In the included sample, the baseline pulse pressure (PP) was 57.54 ± 8.47 mmHg, and the different value of pulse pressure was 5.69 ± 4.24 mmHg between a comparison pre-and post-Intervention. A total of 17 trials (60.7%) explicitly reported regarding medication use. Among them, 9 trials reported specific information on the blood pressure drugs used, and Amlodipine (a calcium channel blocker) was the most popular (7 trials reported). Three trials were reported using the Micardis (telmisartan), Lercanidipine, Thiazide diuretics, losartan potassium. Nifedipine and traditional Chinese medicine had been reported by one trial respectively.
We also summarized the characteristics of Baduanjin intervention. On average, Baduanjin was practiced 7.5 ± 3.8 sessions / week for 28.2 ± 12.8 min / session for 16.7 ± 9.2 weeks. Among the trials, eight of them explicitly appeared that the daily workouts were once in the morning and once in the afternoon. In addition, there are two styles of Baduanjin interventions included sitting Baduanjin (k = 3, 10.7%) and standing Baduanjin (k = 25, 89.2%).
All trials (k = 28, 100.0%) supervised and instructed participants, but less than half of the trials disclosed the information of teachers (k = 11, 39.3%), including Traditional Chinese Medicine (TCM) professionals (k = 9, 32.1%) and professional certificates (k = 2, 7.1%). Two trials disclosed the number of teachers involved in the training. In addition, a few parts of the trials used video-assisted to instruct Baduanjin (k = 4, 14.3%). It is worth noting that all of these 4 trials took the method of punch the clock on the Internet, in order to urge the enthusiasm for and sustainability of Baduanjin training. Only one trial emphasized the attention to breathing skills and the consistency and stability of the movement (21). Finally, in our sample, 2 trials (3.2%) indicated that some participants withdrew from the study due to loss to follow-up. The remaining trials (k = 26, 92.9%) did not provide any information on adverse events.
Most trials (k = 16, 57.1%) reported the use of BP measurement instruments, including automatic/digital sphygmomanometers (k = 3, 10.7%) or manual sphygmomanometers (k = 13, 46.4%). A portion of the trials (k = 7, 25.0%) reported a sitting posture during BP measurement. Six trials (k = 6, 21.4%) reported that blood pressure was measured between 8 a.m. and 10 a.m. at a fixed time. However, one-quarter of the trials (k = 8, 28.6%) did not report any details of the resting blood pressure measurement procedures.
Due to the high heterogeneity of SBP (I2 = 89.6% > 50%, 95%CI: 86.18–92.20%, P < 0.001) and DBP (I2 = 91.1 > 50%, 95%CI: 88.28%−93.21%, P < 0.001), the standardized effect sizes lacked homogeneity. Therefore, we selected random effects meta to analysis. Overall, compared with the control group (p < 0.001), there was significant reduction in SBP (to 9.3 mmHg, SMD = −1.49, 95%CI: −1.73 to −1.13) and DBP (to 6.3 mmHg, SMD = −1.20, 95%CI: −1.51 to −0.88) in the Baduanjin group (Figure 2, Forest plots of the SBP and DBP response to Baduanjin vs. control). Furthermore, for SBP (to 1.49 vs. −1.38) and DBP (to 1.20 vs. −1.19), the mean effect size contained both RCT and nRCT, which was similar to the mean effect size that contained RCT to only. This supported our decision to combine RCT to nRCT in the final analysis.
Regarding the mechanisms of the hypotensive effect of Baduanjin (Supplementary Table 4), 17 trials (60.7%) discussed the potential mechanisms of hypotensive. However, only 5 trials (21.4%) attempted to verify the mechanism discussed. Inside, 3 trials (10.7%) examined the relationship between the BP changes and the measurement mechanisms (22–24). Lin Q compared serum C to reactive protein (CRP) and found that Baduanjin could inhibit the secretion of inflammatory cytokine CRP, reduce the expression level of serum CRP, and actively promote the control of blood pressure. Chen Z considered that Baduanjin exercise could improve Nitric Oxide Synthase (NOS) expression and promote Nitric Oxide (NO) synthesis. Chunmei considered that Baduanjin decreased the level of Endothelin to 1 (ET to 1) in skeletal muscle plasma and increased serum NO in patients with essential hypertension.
In the process of data extraction, we found that some trials explicitly defined participants as the aged, but others did not have a strict age limit (18–70 years). Therefore, in order to explain the exercise effect of the elderly patients after Baduanjin exercise, we divided the included trials into the elderly group (group 1, clearly defined participants as the elderly or defined participants ≥ 60 years old) and the adult group (group 2).
In the age subgroup analysis of SBP (Figure 3, Age subgroup analysis of SBP and DBP), after the removal of three trials that greatly affected the heterogeneity (possibly affected by the study characteristics, sample characteristics) (25–27), seven trials were included in the elderly group. Moreover, the heterogeneity of the elderly group was significantly reduced (I2 = 0.0%). The results displayed that Baduanjin significantly reduced SBP compared with the control group, and SBP was statistically significant (to 11.2 mmHg, SMD = −1.06, 95%CI: −1.24 to −0.88). In the adult group (I2 = 75.4%), thirteen trials were included after removing five trials that greatly affected the heterogeneity. Compared with the control group, blood pressure decreased significantly, and SBP was statistically significant (to 8.2 mmHg, SMD = −1.00, 95%CI: −1.13 to −0.87).
In the age subgroup analysis of DBP, seven trials were included when the elderly group excluded three trials (26–28) with a great impact on heterogeneity. Meantime, the heterogeneity of the elderly group decreased (I2 = 72.6%). Compared with the control group, Baduanjin reduced blood pressure significantly, and the difference value of DBP was statistically significant (to 3.3 mmHg, SMD = −0.57, 95%CI: −0.75 to −0.38). In the adult group (I2 = 91.4%), twelve trials were included after removing six trials that greatly affected the heterogeneity. Meantime, blood pressure reduction was significant compared with the control group, and DBP difference value was significant (to 4.7 mmHg, SMD = −0.82, 95%CI: −0.95 to −0.69).
We also conducted a subgroup analysis for different types of Baduanjin (29) (Figure 4, subgroup analysis of Baduanjin types). The included trials were divided into the Standing Baduanjin group (group 1) and the Sitting Baduanjin group (group 2) based on different exercise movements, and these two groups included 25 trials and 3 trials respectively. Compared with the control group, the Sitting Baduanjin group (I2 = 90.1%) could significantly reduce SBP (to 12.8 mmHg, SMD = −1.26, 95%CI: −1.26 to –0.97), and the difference value was statistically significant. In the Standing Baduanjin group (I2 = 90.0%), BP reduction ability was statistically significant compared with the control group, and DBP difference value was statistically significant (to 7.1 mmHg, SMD = −1.22, 95%CI: −1.32 to 1.12). Compared with the control group, the Sitting Baduanjin group (I2 = 91.5%) could significantly reduce DBP (to 7.8 mmHg, SMD = −1.02, 95%CI: −1.11 to −0.92), and the difference value was statistically significant. The standing Baduanjin group (I2 = 87.7%) also significantly reduced the DBP (to 6.1 mmHg, SMD = −1.05, 95%CI: −1.15 to– 0.95) and the difference value was statistically significant.
Based on the above analysis, there was no heterogeneity in SBP reduction after Baduanjin intervention in the elderly group, and the heterogeneity of DBP was also relatively reduced since performing the subgroup analysis. The effect of BP reduction was statistically significant in both groups. Notably, the decrease of PP in the elderly group (PP = 8.91 ± 4.03 mmHg) was much greater than that in the adult group (PP = 3.90 ± 3.08 mmHg).
Funnel plots, test of Begg and test of Egger all suggested significant publication bias and other reporting bias in the SBP Baduanjin intervention (test of Begg: z = −3.16, p = 0.002; test of Egger: t = −3.68, p = 0.001). For the elderly group, publication bias was significantly reduced after excluding three trials with great impact on heterogeneity (test of Egger: P = 0.095 > 0.05). For the adult group, the test of Egger's (P = 0.249 > 0.005) showed no significant publication bias after excluding five trials that had a great impact on heterogeneity. These results indicated that meta to analysis was robust. (Supplementary Figure 1, Funnel plot of SBP reduction in age subgroups)
Meanwhile, the funnel plot, test of Begg and test of Egger all showed a significant publication bias and other reporting bias in the DBP response to Baduanjin (test of Begg: z = −2.41, p = 0.016; test of Egger: t = −3.06, p = 0.005). For the elderly group, the test of Egger's (P = 0.252 > 0.005) showed no significant publication bias after excluding three trials that had a great impact on heterogeneity. For the adult group, publication bias was significantly reduced after excluding six trials with great impact on heterogeneity (test of Egger: P = 0.806 > 0.05), indicating that the analysis result was robust (Supplementary Figure 2, Funnel plot of SBP reduction in age subgroups)
Our meta to analysis examined the efficacy of Baduanjin as an exercise therapy to reduce blood pressure, which is the largest sample size examined to date. We found that Baduanjin exercised an average of 7.5 ± 3.8 sessions / week for 28.2 ± 12.8 min /session for 16.7 ± 9.2 weeks, produced SBP reductions of 9.3 mmHg and DBP reductions of 6.3 mmHg. Since performing the subgroup analysis, our finding was that Baduanjin has low heterogeneity in reducing blood pressure in the elderly group. This may indicated that compared with adults, the curative effectiveness of Baduanjin training in elderly patients with hypertension was more controllable. In the elderly group, the Baduanjin intervention reduced 8.7 mmHg and 4.8 mmHg of SBP and DBP respectively. The reduction in blood pressure reduces the risk of heart disease by about 22% and the stroke risk by about 29% (30). These large BP reductions support the use of Baduanjin as a safe and effective exercise method to reduce patients' BP in daily life. In particular, it is recommended that Baduanjin be used as a lifestyle for the prevention and treatment of hypertension among the elderly.
Regular aerobic exercise can lower BP, thereby reducing the risk of cardiovascular disease, hence it is a recommended exercise mode for many medical organizations around the world to prevent and treat hypertension. However, due to the high physical fitness requirements of aerobic exercise, most adults with hypertension are unwilling or unable to exercise. Therefore, in recent years, many alternative therapies for aerobic exercise, such as Taijiquan (31–33) and yoga (34–36), have been widely recommended in clinical practice. But after comparing with other exercises beneficial to blood pressure, we also recommend Baduanjin exercise as a way to treat hypertension in daily life. Yin Wu believed that Taijiquan elicited SBP reductions of 11.3 mmHg and DBP reductions of 4.8 mmHg (31), yoga elicited SBP reductions of 5.0 mmHg and DBP reductions of 3.9 mmHg (34). We found that Baduanjin elicited SBP reductions of 9.3 mmHg and DBP reductions of 6.3 mmHg. When the curative effects are similar, Baduanjin is safer, more convenient, simpler and easier to learn than Taijiquan and yoga. A complete set of Baduanjin exercise plus warm to up and stretching take < 20 min, and do not need other auxiliary required. It is more helpful to those adults who are not willing to exercise keep exercising. In addition, Baduanjin is also widely used in the prevention, treatment and rehabilitation research of nervous system diseases (stroke, etc.), respiratory system diseases (chronic obstructive pneumonia, COVID to 19, etc.), cardiovascular system diseases (coronary heart disease, etc.) and musculoskeletal system diseases. It can improve balance function, regulate blood glucose, regulate negative emotions, and improve cognitive function (37–40).
Our results showed that if the participants were limited to the elderly, the effect of reducing blood pressure after Baduanjin intervention was reliable. With the increase of age, a series of physiological changes will occur in the human body, such as increased arterial stiffness, elevated PP, changed in the sensitivity and function of the autonomic nervous system, changed in the endothelial function and so on (41). In fact, PP and arterial stiffness are significant predictors of morbidity and mortality in the elderly (42). Every 10 mmHg increases in PP increases the risk of cardiac insufficiency 32% and the risk of stroke 24% (43). Therefore, reducing the pulse pressure D to value can reduce the risk of atherosclerosis and cardiovascular disease. Our study observed that the decrease of PP in the elderly group (PP = 8.91 ± 4.03 mmHg) was much greater than that in the adult group (PP = 3.90 ± 3.08 mmHg). It proved the view that Baduanjin could prevent arteriosclerosis in the elderly.
We also tried to group according to different types of Baduanjin. Sitting Baduanjin (k = 3, 10.7%) has gentle movement and a small range of activities, focusing on the cultivation of Chinese Taoist "Qi.” Standing Baduanjin (k = 25, 89.2%) has forceful movement and a large range of activities, which is more like a kind of martial art (44). However, our results showed that the heterogeneity within and between groups were very high according to the different types of Baduanjin. The reasons for this result probable were that (a) the trials used sitting Baduanjin were rare. (b) there were also many differences categories in Standing Baduanjin. Therefore, based on the current trials, it is unable to classify according to the type of Baduanjin.
Due to space constraints or other unknown reasons, it was still possible that the included Baduanjin trials were inadvertently missing some study details. This limited our ability to extract information and analysis it. Therefore, we were unable to analyze the source of factors effecting blood pressure reduction, such as teachers' qualifications (39.3% reported), whether to emphasize the skills of Baduanjin practice (3.6% reported), blood pressure measurement methods (57.1% reported), baseline medication (60.7% reported) and medication during the intervention (60.7% reported), dietary maintenance (30.2% reported) and physical activity level (10.7% reported).
We recommend that readers make appropriate reference to our research results. First, all the included trials were evaluated using ROB1.0 and MINORS, most of them had high / serious bias risks. Second, almost all the participants in the trials were Chinese, lacking research samples from other countries.
Our meta to analysis also had several strengths. First, our research covered a wide range Baduanjin types. Second, we focused on the effectiveness of Baduanjin on the blood pressure of the elderly, which had certain reference value.
Our noteworthy analysis results are that Baduanjin interventions in the elderly group elicited SBP reductions of about 11.2 mmHg and DBP reductions of about 3.3 mmHg. Baduanjin may be another feasible choice for the treatment of hypertension, and can be appropriately popularized in the elderly. It can reduce the PP of the elderly and prevent the occurrence of cardiovascular disease. The current review also calls attention to the fact that future Baduanjin intervention studies need to (a) pay more attention to the research on the hypotensive mechanism of Baduanjin. (b) study the exercise effect of different age groups, and strictly distinguish age grades. (c) study the difference of curative effectiveness of different types of Baduanjin.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
ZM and XZ participated in the design of the study. HL, ZM, and KT contributed to data analysis and interpretation. ZL, YC, ZM, and HY contributed to data collection. XZ, HL, ZM, and KT contributed to data interpretation. All authors contributed to manuscript writing, agree with the order of presentation of the authors, read, and approved the final version of the manuscript.
This study was funded by a grant from the National Natural Science Foundation of China (No. 82105034).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.936018/full#supplementary-material
1. Esmailiyan M, Amerizadeh A, Vahdat S, Ghodsi M, Doewes RI, Sundram Y. Effect of different types of aerobic exercise on individuals with and without hypertension: an updated systematic review. Curr Probl Cardiol. (2021) 28:101034. doi: 10.1016/j.cpcardiol.2021.101034
2. Oliveira GF, Marin TC, Forjaz CLM, Brito LC. Exercise training and endothelial function in hypertension: effects of aerobic and resistance training. Arq Bras Cardiol. (2021) 116:948–9. doi: 10.36660/abc.20210111
3. Whelton PK, Carey RM, Aronow WS, CaseyJr DE, Collins KJ, Himmelfarb CD, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. (2018) 71:e127–48. doi: 10.1161/HYP.0000000000000076
4. Alpsoy S. exercise and hypertension. Adv Exp Med Biol. (2020) 1228:153–67. doi: 10.1007/978-981-15-1792-1_10
5. Chen G, Wang L, Bi H. Research progress on clinical rehabilitation of Baduanjin, a traditional Chinese skill. Massage Rehabilitation Med. (2022) 13:57–60. doi: 10.19787/j.issn.1008-1879.2022.10.017
6. Fang J, Zhang L, Wu F, Ye J, Cai S, Lian X. The safety of baduanjin exercise: a systematic review. eCAM. (2021) 2021:8867098. doi: 10.1155/2021/8867098
7. Zhou J, Yu Y, Cao B, Li X, Wu M, Wen T, et al. Characteristic of Clinical Studies on Baduanjin during 2000-2019: a comprehensive review. eCAM. (2020) 2020:4783915. doi: 10.1155/2020/4783915
8. Li R, Jin L, Hong P, He Z, Huang C, Zhao J, et al. The effect of baduanjin on promoting the physical fitness and health of adults. Evid Based Complement Alternat Med. (2014) 2014:784059. doi: 10.1155/2014/784059
9. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension (Dallas, Tex: 1979). (2020) 75:1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026
10. Xiong X, Wang P, Li S, Zhang Y, Li X. Effect of Baduanjin exercise for hypertension: a systematic review and meta-analysis of randomized controlled trials. Maturitas. (2015) 8:370–78. doi: 10.1016/j.maturitas.2015.01.002
11. Shao B, Zhang X, Vernooij R, Lv Q, Hou Y, Bao Q, et al. The effectiveness of Baduanjin exercise for hypertension: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med Ther. (2020) 2:304. doi: 10.1186/s12906-020-03098-w
12. Guan Y, Hao Y, Guan Y, Wang H. Effects of Baduanjin exercise on essential hypertension: a meta-analysis of randomized controlled trials. Medicine (Baltimore). (2020) 99:e21577. doi: 10.1097/MD.0000000000021577
13. Moher D, Liberati A, Tetzlaff J, Altman D. G., PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
14. Pescatello LS, Kulikowich JM. The aftereffects of dynamic exercise on ambulatory blood pressure. Med Sci Sports Exerc. (2001) 33:1855–61. doi: 10.1097/00005768-200111000-00009
15. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. Cochrane Bias Methods Group, & Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed). (2011) 343:d5928. doi: 10.1136/bmj.d5928
16. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
17. Johnson BT. Huedo-Medina TB. Meta-Analytic Statistical Inferences for Continuous Measure Outcomes as a Function Of Effect Size Metric and Other Assumptions. (2019). Available online at: www.ncbi.nlm.nih.gov/books/NBK140575/ (accessed on August 20, 2019).
18. Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester: John Wiley & Sons (2019).
19. Johnson BT, Low RE, MacDonald HV. Panning for the gold in health research: incorporating studies' methodological quality in meta-analysis. Psychol Health. (2015) 30:135–52. doi: 10.1080/08870446.2014.953533
20. Harbord RM, Higgins J. Meta-regression in Stata. Stata J. (2008) 8:493–519. doi: 10.1177/1536867X0800800403
21. Yang H, Zhao Y, Li J. Effects of Baduanjin exercise on autonomic responses in hypertensive patients. Chin Med J National Coal Indus. (2014) 7:1143–46. doi: 10.11723/mtgyyx.1007-9564.201407038
22. Lin Q, Yan X. Promoting effect of fitness Baduanjin on rehabilitation of elderly patients with hypertension. Chin J Gerontolo. (2017) 37:3024–26. doi: 10.3969/j.issn.1005-9202.2017.12.075
23. Chen Z. Mechanistic study of the effect of baduanjin exercise intervention in essential hypertension based on the L-Arg / NOS / NO pathway[D]. (Ph.D. dissertation). Fujian University of Traditional Chinese Medicine (2019).
24. Chunmei X, Yang Y, Zhuang Y. Effect of health qigong ba duan jin on blood pressure of individuals with essential hypertension. J Am Geriatrics Soc. (2016) 64:211–13. doi: 10.1111/jgs.13913
25. Pan HS, Feng YC. Clinical observation of Baduanjin exercise on the rehabilitation treatment of grade 1 hypertension in the elderly. J Nanjing Univer Phy Edu. (2010) 01:4–6. doi: 10.15877/j.cnki.nsin.2010.01.006
26. Chen W, Lu Q, Lian Y. Influence of the effect of seating Baduanjin exercise combined with health education on the antihypertensive effect of elderly hypertensive patients in the communityShanghai. Med Pharmaceutical J. (2020) 41:47–50.
27. Lin F, He Q. Observation of Baduanjin exercise on grade 1 hypertension in the elderly. Chin Geriatr Health Care Med. (2014) 03:25–6. doi: 10.3969/j.issn.1672-4860.2014.03.009
28. Jiang Y, Fu G, Wang Q, Bao X, Liu X. Effects of Baduanjin on elderly patients with hypertension and anxiety. Qilu Nurs Magazine. (2019) 1:104–06.
29. Bao L. A brief history of Ba Duan Jin (Eight Infantile Finger Loops and Whorls, A Kind of Qigong. J Trad Chin Med Liter. (2001) 2001:37–9. doi: 10.3969/j.issn.1006-4737.2001.02.023
30. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ (Clinical Research ed). (2009) 338:1665. doi: 10.1136/bmj.b1665
31. Wu Y, Johnson BT, Chen S, Chen Y, Livingston J, Pescatello LS. Tai Ji Quan as antihypertensive lifestyle therapy: A systematic review and meta-analysis. J Sport Health Sci. (2021) 10:211–21/ doi: 10.1016/j.jshs.2020.03.007
32. Moker EA, Bateman LA. Kraus WE, Pescatello LS. The relationship between the blood pressure responses to exercise following training and detraining periods. PLoS ONE. (2014) 9:e105755. doi: 10.1371/journal.pone.0105755
33. Lee YM. The effects of tai chi on waist circumference and blood pressure in the elderly. J Phys Ther Sci. (2017) 29:172–5. doi: 10.1589/jpts.29.172
34. Wu Y, Johnson BT, Acabchuk RL, Chen S, Lewis HK, Livingston J, et al. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc. (2019) 94:432–46. doi: 10.1016/j.mayocp.2018.09.023
35. Cramer H. The efficacy and safety of yoga in managing hypertension. Exp Clin Endocrinol Diabetes. (2016) 124:65–70. doi: 10.1055/s-0035-1565062
36. Tyagi A, Cohen M. Yoga and hypertension: a systematic review. Altern Ther Health Med. (2014) 20:32–59.
37. Shi Y. Study on the prevention of pulmonary function and complications in Tuberculosis patients. Chin J Prevent Med. (2019) 20:799–802.
38. Gu K, Hu G. Study on the effects of Tai Chi and fitness Qigong Baduanjin on blood lipids in elderly and elderly in the community. National J Prevent Med. (2019) 20:799–802.
39. Du W, Su S, Zhao Y. Came to the clinical observation to improve the balance function and gait of the elderly. Hebei Trad Chin Med. (2018) 40:987–90.
40. Li W, Wu Z, Jing C, Pan H. Effect of Baduanjin on blood sugar and blood pressure in patients with prediabetes mellitus with mild hypertension. New Trad Chin Med. (2019) 51:291–4. doi: 10.13457/j.cnki.jncm.2019.07.086
41. Pont L, Alhawassi T. Challenges in the management of hypertension in older populations. Adv Exp Med Biol. (2017) 956:167–80. doi: 10.1007/5584_2016_149
42. Safar ME, Lacolley P. Disturbance of macro- and microcirculation: relations with pulse pressure and cardiac organ damage. Am J Physiol Heart Circ Physiol. (2007) 293:H1–7. doi: 10.1152/ajpheart.00063.2007
43. Touyz RM. Reactive oxygen species, vascular oxidative stress, and redox signaling in hypertension: what is the clinical significance?. Hypertension. (2004) 44:248–52. doi: 10.1161/01.HYP.0000138070.47616.9d
Keywords: Baduanjin, hypertension, BP, SBP, DBP, exercise
Citation: Ma Z, Lei H, Tian K, Liu Z, Chen Y, Yang H and Zhu X (2022) Baduanjin exercise in the treatment of hypertension: A systematic review and meta-analysis. Front. Cardiovasc. Med. 9:936018. doi: 10.3389/fcvm.2022.936018
Received: 10 May 2022; Accepted: 25 July 2022;
Published: 15 August 2022.
Edited by:
Chayakrit Krittanawong, New York University, United StatesReviewed by:
Susanna Rampichini, Università degli studi di Milano, ItalyCopyright © 2022 Ma, Lei, Tian, Liu, Chen, Yang and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangyu Zhu, MTE2NDkxOTkyQHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.