- 1Institute of Geriatrics, The Second Medical Center and National Clinical Research Center for Geriatric Diseases, Chinese PLA General Hospital, Beijing, China
- 2Medical School of Chinese PLA, Chinese PLA General Hospital, Beijing, China
Background: The efficacy and safety of antithrombotic treatment with oral anticoagulants (OACs) in elderly patients with comorbidities of acute coronary syndrome (ACS) and atrial fibrillation (AF) are unclear.
Methods: A cohort of hospitalized elderly patients (≥65 years of age) diagnosed with ACS and AF and treated with oral antithrombotic agents were consecutively recruited. Follow-up was performed for at least 1 year. Major adverse cardiac events (MACEs) were defined as a composite of all-cause death, nonfatal myocardial infarction (MI), nonfatal stroke, and systemic embolism. The safety outcomes of bleeding were defined according to the Bleeding Academic Research Consortium (BARC) criteria.
Results: A cohort of 548 eligible patients (76 ± 6.6 years) was analyzed. Compared to the patients with OAC treatment (n = 184, 33.6%), patients treated without OAC (n = 364, 66.4%) were older, had a lower prevalence of persistent AF and unstable angina (UA), and more often presented with paroxysmal AF, acute myocardial infarction (AMI), stent implantation and dual antiplatelet therapy (DAPT). Compared to the patients without OAC treatment (n = 364, 66.4%), patients treated with OAC (n = 184, 33.6%) had a lower risk of MACEs at both the 1-year (4.3 vs. 15.1%, adjusted HR: 0.34, 95% CI: 0.15–0.80, p = 0.014) and 5-year (17.5 vs. 48.4%, adjusted HR: 0.36, 95% CI: 0.19–0.67, p = 0.001) follow-up. No significant difference was observed for bleeding events of BARC ≥2 between the groups (8.0 vs. 9.0%, adjusted HR: 1.17, 95% CI: 0.58–2.34, p = 0.667). Compared with warfarin-treated patients, the non-vitamin K antagonist oral anticoagulant-treated patients had lower risks of all-cause mortality (2.1 vs. 9.5%, HR: 0.18, 95% CI: 0.03–0.98, p = 0.047) and bleeding events of BARC ≥ 3 (2.1 vs. 4.8%, HR: 0.14, 95% CI: 0.02–1.10, p = 0.062).
Conclusions: Antithrombotic therapy with OACs in elderly patients with ACS and AF was associated with a lower risk of ischemic events without an increase in bleeding events. In real-world practice, the clinical awareness of anticoagulation treatments in elderly patients with ACS and AF needs to be strengthened.
Introduction
The comorbidity of acute coronary syndrome (ACS) and atrial fibrillation (AF), which occurs mostly in elderly patients (1–5), contributes to the increased risk of all-cause death and stroke (1, 2, 6–8). Antithrombosis with dual platelet inhibition or oral anticoagulation (OAC) is most frequently recommended for the prevention of ischemic stroke and mortality in patients with ACS and AF (9). In the recent guideline from the European Society of Cardiology (ESC), long-term administration of OACs, including non-vitamin K antagonist oral anticoagulant (NOAC) or vitamin K antagonist (VKA), is recommended for medically treated or percutaneous coronary intervention (PCI)-treated patients with ACS and AF (9). When considering the use and duration of combined antithrombotic therapy in patients with ACS and AF, the concomitant risks of ischemic events and antithrombotic treatment-related bleeding need to be carefully balanced (10), especially in elderly patients with an increased risk of both bleeding and ischemic events (11, 12). Of note, as only 7% of patients in ACS trials were reported to be elderly (≥75 years) (13), evidence-based recommendations for antithrombotic therapy in elderly patients with ACS and AF have rarely been reported.
Although there is sufficient evidence supporting the use of OACs in elderly patients with AF (14–16), poor adherence to guideline-directed anticoagulation has been reported (17). In addition, physicians are less likely to prescribe OACs in this population due to the risk of bleeding (18–21). OAC treatment in real-world elderly patients with ACS and AF has rarely been reported. Observational studies found that compared to antithrombotic therapy in ACS patients without AF, antithrombotic therapy in patients with ACS and AF was less appropriate and led to more adverse outcomes (22, 23). The situation might be worse in elderly individuals, who are more likely to have multiorgan damage, increased ischemic and bleeding risks, a high incidence of comorbidities and comedication, and decreased adherence to prescriptions (1, 3, 24). Therefore, the present study aimed to investigate the efficacy and safety of antithrombotic therapy with OACs in real-world elderly patients with ACS and AF.
Methods
Patients
Patients aged ≥65 years old with a diagnosis of the comorbidities of coronary artery disease (CAD) and AF were recruited consecutively from the Department of Cardiology, Chinese PLA General Hospital, from 2010 through 2017. Participants were eligible for inclusion if they had both ACS and nonvalvular AF and were treated with oral antithrombotic agents, including antiplatelet agents and/or anticoagulants. ACS, including unstable angina (UA), non-ST elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI), were defined according to the 2018-ESC criteria (10). Nonvalvular AF refers to AF without a mechanical artificial heart valve or with moderate to severe mitral stenosis (usually derived from rheumatism) (9). Nonvalvular AF could be paroxysmal or persistent but not secondary to a reversible disease. Participants were excluded if they had reversible causes of AF, known contraindications to the use of antithrombotic regimens or a life expectancy of no more than 6 months. Patients with any indication for OAC other than AF (e.g., mechanical heart valves, pulmonary embolism, and left ventricular mural thrombus) or who were lost to follow-up were also excluded. This study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Chinese PLA General Hospital, and all patients provided written informed consent. Eligible patients were divided into the “with OAC” group and the “without OAC” group for further analysis.
Outcomes and Follow-Up
The major adverse cardiac events (MACEs) for efficacy evaluation were defined as all-cause death, nonfatal myocardial infarction (MI), nonfatal stroke, and systemic embolism. The definitions for the outcomes were derived from the most recent updated guidelines (10). Safety outcomes of bleeding events were defined according to the Bleeding Academic Research Consortium (BARC) criteria of BARC ≥2 (25). Follow-up was performed via phone call or by a review of the medical records of readmission or repeat outpatient visits. All eligible patients were followed-up for at least 1 year or until the occurrence of MACEs. A well-thought-out follow-up questions by phone call were designed in advance with the certification of the Ethics Committee of Chinese PLA General Hospital. All the follow-ups by phone call were completed by the clinicians with qualifications in cardiology after receiving unified training. To verify the outcomes by phone call, the final judgement of all the endpoints was determined by the experts of the Endpoints Committee, the Clinical Drug Trial Center of Chinese PLA General Hospital.
Statistical Analysis
The CHA2DS2-VASc score was used to assess the risk of ischemic events. The CHA2DS2-VASc score was calculated as congestive heart failure (1 point), hypertension (1 point), age ≥ 75 years (2 points), diabetes (1 point), stroke/transient ischemic attack/thromboembolism (2 points), vascular disease (prior myocardial infarction, peripheral artery disease, or aortic plaque: 1 point), age 65 to 74 years (1 point), and female sex (1 point) (26). A modified HAS-BLED score was used to assess the risk of bleeding. The modified HAS-BLED score was calculated as hypertension (1 point), abnormal renal and liver function (1 point each), stroke (1 point), bleeding (1 point), elderly (age > 65 years: 1 point), drugs or alcohol (1 point each) (27, 28). The labile international normalized ratio (INR) was not available in our study; hence, this factor was not included in the calculation of the modified HAS-BLED score. Continuous and categorical variables were described as the mean ± standard deviation (SD) or median (interquartile range [IQR]) and frequencies (percentages), respectively. Continuous variables were compared using t-tests, while categorical variables were compared using chi-square tests. To identify the independent predictive ability of OAC treatment on the efficacy and safety of adverse clinical outcomes, Cox multivariate models were used with the adjustment of the covariances, including the significantly different baseline clinical characteristics between the groups with or without OAC. Kaplan–Meier estimates of MACEs and bleeding events were used to construct time-to-event curves. All analyses were performed using SPSS (version 26.0), R software (version 3.6.0), and GraphPad Prism (version 8.0.1) software. All tests were two-tailed, and P values < 0.05 were considered statistically significant.
Results
Patient Characteristics
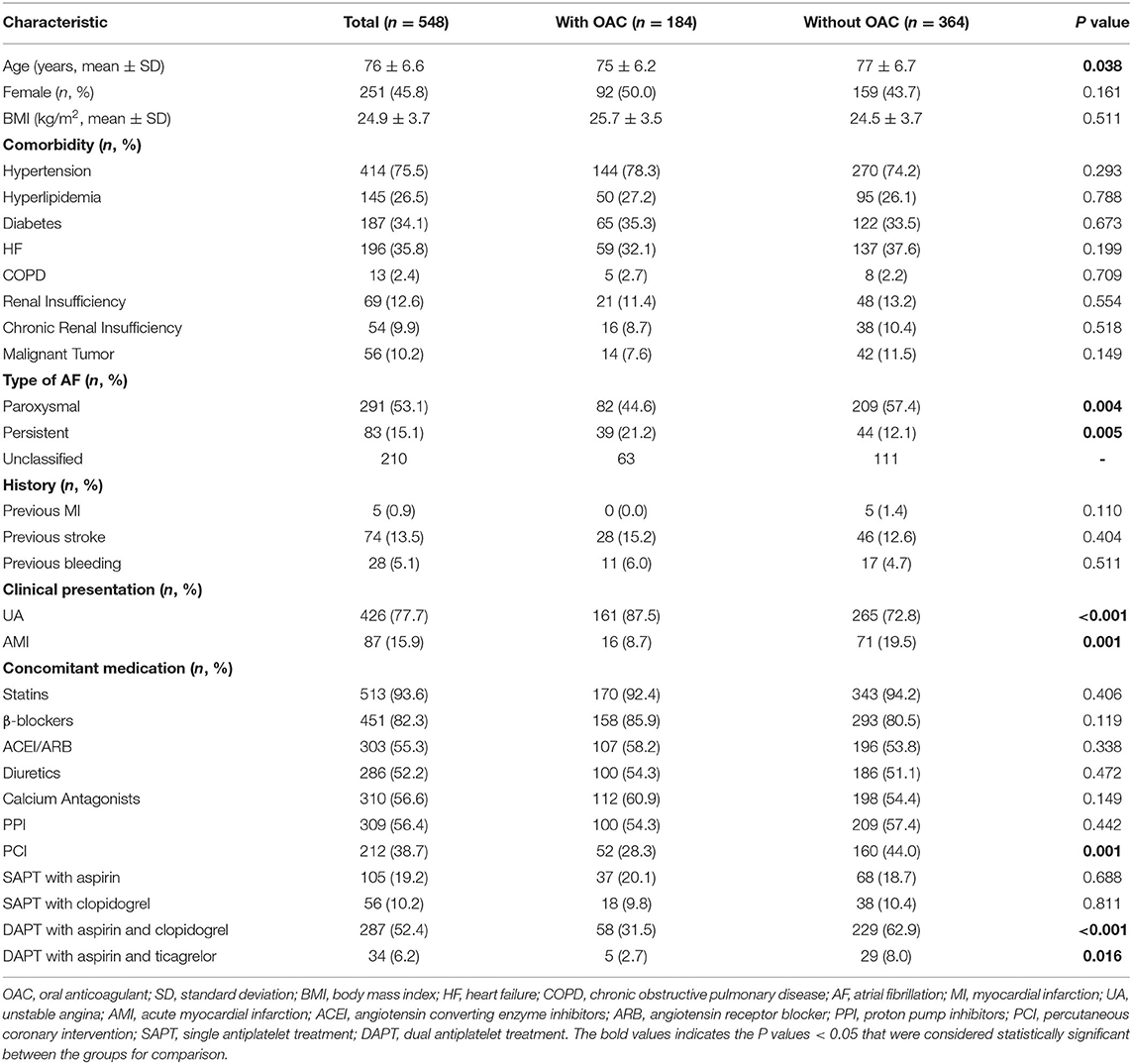
Among the 2,437 continuously enrolled patients diagnosed with CAD and AF, the overall follow-up response rate of the cohort was 93.2%. A total of 548 eligible patients with ACS and AF were ultimately included in the analysis (Figure 1). The baseline characteristics of the patients according to the different treatment regimens with or without OAC are shown in Table 1. Overall, the patients had a mean age of 76 years (76 ± 6.6), and 251 (45.8%) were women. Among the included patients, 184 (33.6%) were treated with OACs, and 364 (66.4%) were not treated with OACs (Figure 2). All the included patients were followed up for 1 year, and a total of 290 patients were followed up for 5 years (with 83 patients treated with OAC and 207 without OAC). Compared to patients without OACs, patients treated with OACs were younger, had a higher prevalence of persistent AF and UA, and less often presented with paroxysmal AF, acute myocardial infarction (AMI), stent implantation and dual antiplatelet therapy (DAPT) (Table 1). With the increase in the CHA2DS2-VASc score, the percentage of patients treated with OACs did not increase accordingly (Figure 3A). With an increasing HAS-BLED score, the percentage of patients treated with OACs decreased accordingly (Figure 3B).
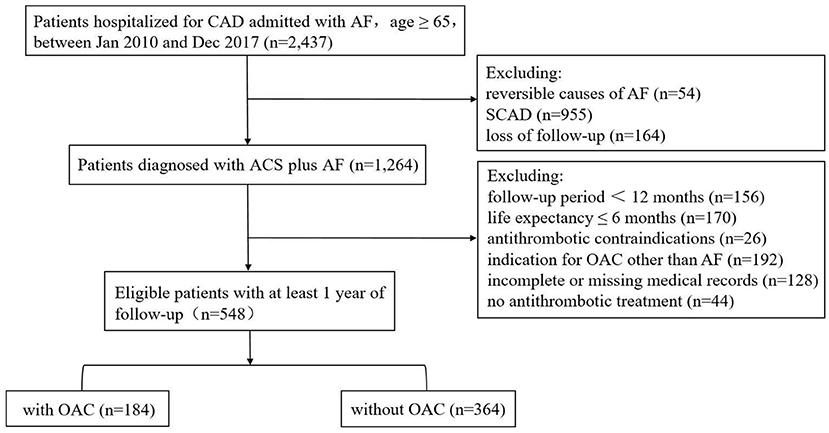
Figure 1. Flow chart over selection of the cohort. CAD, coronary artery disease; AF, atrial fibrillation; SCAD, stable coronary artery disease; OAC, oral anticoagulant.
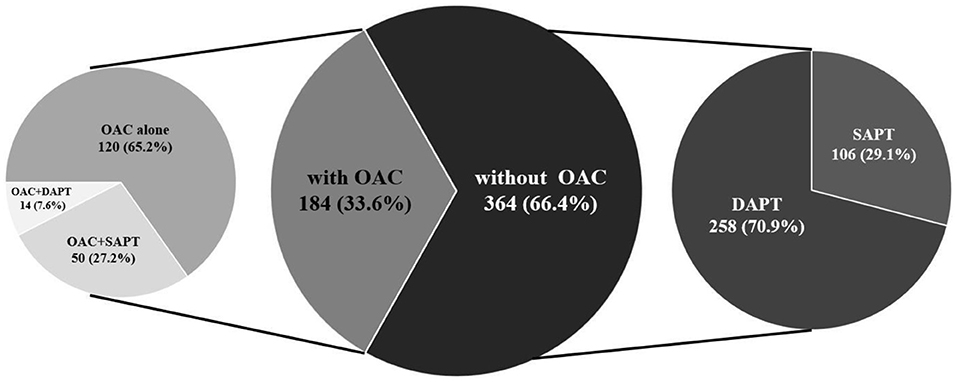
Figure 2. Prevalence of antithrombotic strategies. OAC, oral anticoagulant; DAPT, dual antiplatelet treatment; SAPT, single antiplatelet treatment.
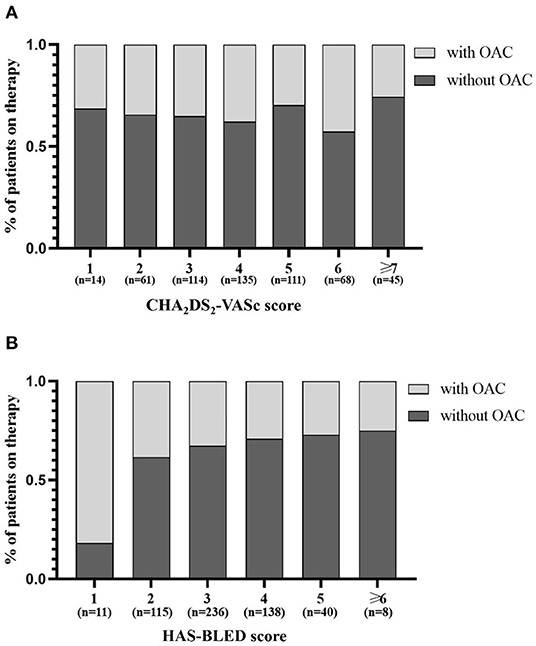
Figure 3. Distribution of antithrombotic strategies by CHA2DS2-VASc score (A) and HAS-BLED score (B). OAC, oral anticoagulant.
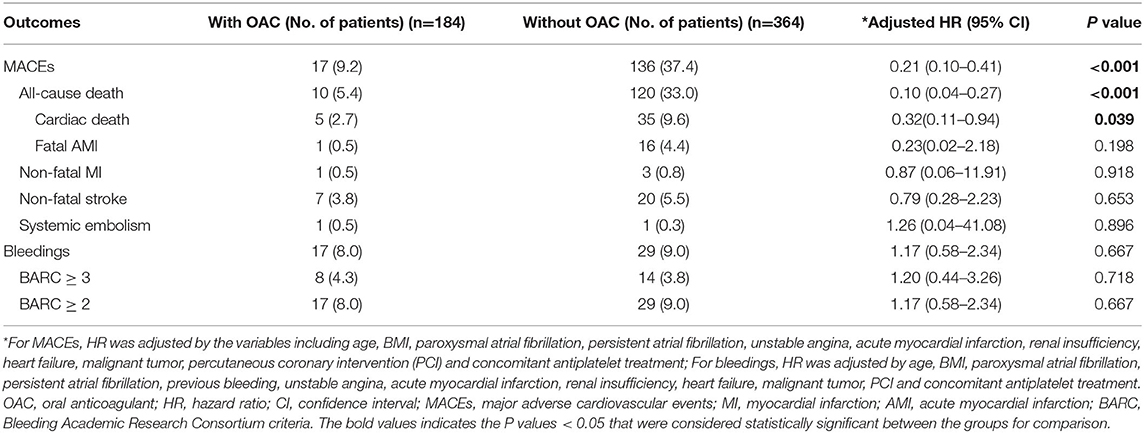
Efficacy and Safety of OAC Treatment in Elderly Patients With ACS and AF
The median follow-up was 6.2 years (IQR: 4.2 to 8.5 years). During the follow-up, MACEs occurred in 153 (27.9%) patients, including all-cause death in 130, nonfatal MI in 4, nonfatal stroke in 27, and systemic embolism in 2 patients. After multivariable adjustment, the incidence of MACEs was significantly lower in patients treated with OACs than in those without OACs (9.2 vs. 37.4%, HR: 0.21, 95% CI: 0.10–0.41, p < 0.001) (Table 2). The efficacy of OACs could be found in patients followed-up for 1 year (4.3 vs. 15.1%, HR: 0.34, 95% CI: 0.15–0.80, p = 0.014) and 5 years (17.5 vs. 48.4%, HR: 0.36, 95% CI: 0.19–0.67, p = 0.001) (Figure 4). In terms of safety outcomes, bleeding events of BARC ≥ 2 occurred in 46 (8.4%) patients, including bleeding events of BARC ≥ 3 in 22 (4.0%) patients (Table 2). However, no significant difference in bleeding events was found between the patients with and without OAC (8.0 vs. 9.0%, HR: 1.17, 95% CI: 0.58–2.34, p = 0.667). Kaplan-Meier curves showed a significant decrease in MACEs (Figure 5) but not bleeding (Figure 6) among patients treated with OACs compared with patients without OACs at both the 1-year and 5-year follow-up.
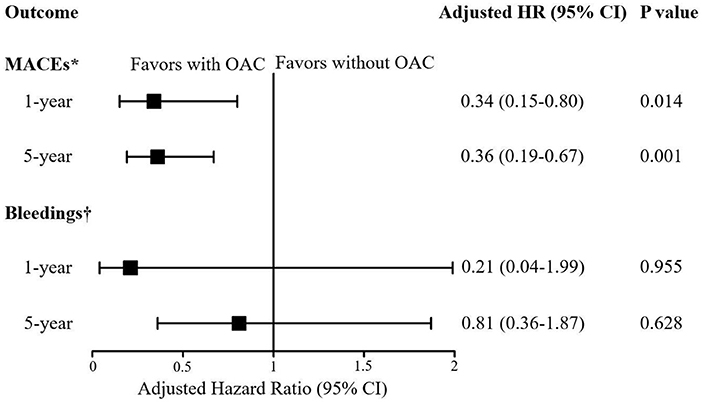
Figure 4. Forest plot for the risk of MACEs and bleedings in patients with or without OAC according to the length of follow-ups. *For MACEs, HR was adjusted by the variables including age, BMI, paroxysmal atrial fibrillation, persistent atrial fibrillation, unstable angina, acute myocardial infarction, renal insufficiency, heart failure, malignant tumor, percutaneous coronary intervention (PCI) and concomitant antiplatelet treatment;†For bleedings, HR was adjusted by age, BMI, paroxysmal atrial fibrillation, persistent atrial fibrillation, previous bleeding, unstable angina, acute myocardial infarction, renal insufficiency, heart failure, malignant tumor, PCI and concomitant antiplatelet treatment. HR, hazard ratio; CI, confidence interval; MACEs, Major Adverse Cardiovascular Events; Bleeding was defined as BARC ≥ 2; OAC, oral anticoagulant.
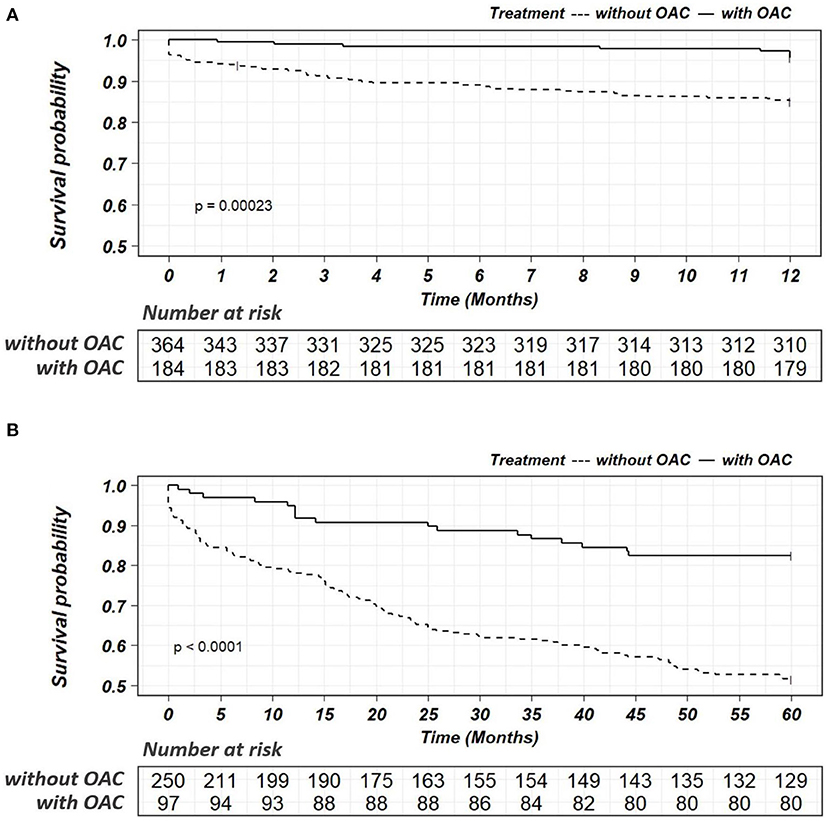
Figure 5. Kaplan-Meier survival curves for the endpoints of MACEs within a follow-up of 1 year (A) or 5 years (B) in patients with or without OAC. OAC, oral anticoagulant.
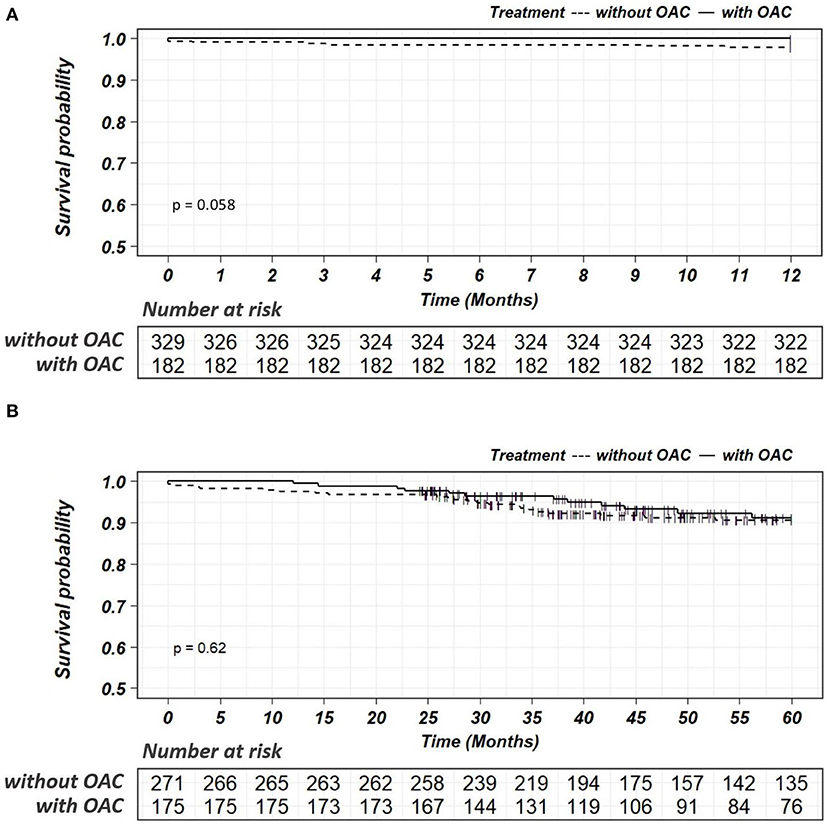
Figure 6. Kaplan-Meier survival curves for the endpoints of bleedings within a follow-up of 1 year (A) or 5 years (B) in patients with or without OAC. OAC, oral anticoagulant.
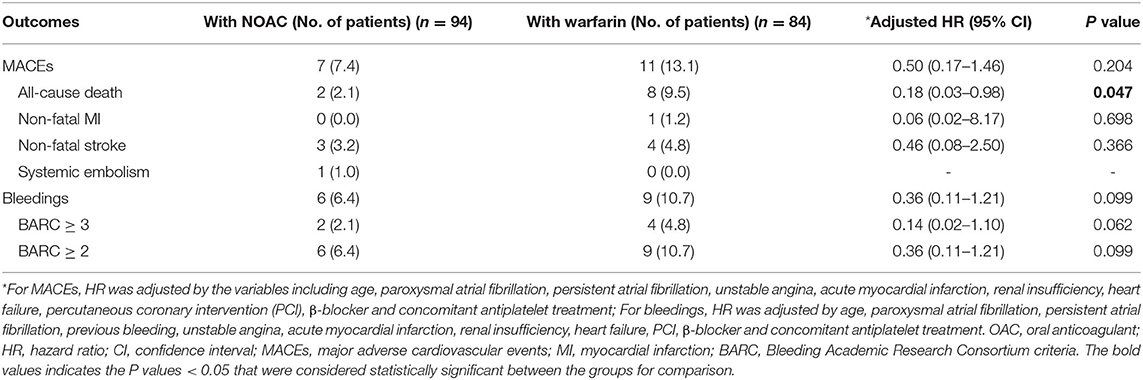
Efficacy and Safety of NOACs vs. Warfarin Treatment in Elderly Patients With ACS and AF
We also performed a subgroup analysis of the efficacy and safety of NOAC treatment vs. warfarin treatment. A total of 94 (51.1%) patients were treated with NOACs, and 84 (45.6%) patients were treated with warfarin, excluding 6 (3.3%) patients who switched from warfarin to rivaroxaban during follow-up. The baseline characteristics according to the different treatment regimens (NOAC or warfarin) are shown in Supplementary Table. Multivariable Cox regression analysis showed that NOAC and warfarin were comparable in terms of efficacy (MACEs: 7.4 vs. 13.1%, HR: 0.50, 95% CI: 0.17–1.46, p = 0.204) and safety (bleeding: 6.4vs. 10.7%, HR: 0.36, 95% CI: 0.11–1.21, p = 0.099), respectively (Table 3). NOAC treatment yielded a marginally much reduction in all-cause mortality compared with warfarin treatment in elderly patients with ACS and AF (2.1 vs. 9.5%, adjusted HR: 0.18, 95% CI: 0.03–0.98, p = 0.047) (Table 3).
Discussion
In the present study, the major findings obtained from real-world elderly patients with comorbidities of ACS and AF are the following: (1) The selection of oral antithrombotic strategies is mainly affected by the risk of bleeding. (2) The application of OACs can reduce the risk of major ischemic events without increasing bleeding. This suggests that in real-world clinical practice, OACs could be safely applied in elderly patients with ACS and AF. To our knowledge, this is the first real-world study to investigate the efficacy and safety of OACs in elderly patients with both ACS and AF.
Therapy with OAC was recommended in patients with both ACS and AF after PCI or medical treatment, whichever initial plan was chosen (9). However, patients with both ACS and AF were less likely to receive appropriate antithrombotic therapy (23) and more likely to suffer from adverse outcomes (9, 22). Our study showed that only 33.6% of elderly patients with both ACS and AF were treated with OACs. The proportion was comparable to that recently reported (44.7%) in elderly Chinese patients with AF alone (21) and that reported (36.5%) in Chinese AF patients with a CHA2DS2-VASc score ≥2 (29). The reason for the underutilization of OACs in the present study could be attributed to the factors age, type of AF, AMI, PCI, and the concomitant use of DAPT. As we know, physicians in real-world clinical practice are reluctant to discontinue antiplatelet treatment, especially among PCI-treated ACS patients with AF, therefore discouraging physicians from prescribing OACs (30). In addition, elderly patients who presented with both ACS and AF were more likely to be prescribed DAPT rather than OAC by physicians (21, 31). The rate of the present elderly patients with ACS and AF underwent PCI was relatively low (38.7%), mostly attributing to the mild coronary stenosis (<50%), patients' unwillingness, contraindications for PCI, advanced age (>85), or recommending to cardiac surgery. Despite the lower percentage, there was absolutely an increased trend for PCI in the present elderly patients with ACS and AF with the increasing years (data not shown). However, even with the fewer patients underwent PCI, the OACs remained under-prescription. Moreover, the present study found that the ratio of OAC treatment showed a significant decrease with increasing HAS-BLED score but did not increase with increasing CHA2DS2-VASc score. This result indicated that the antithrombotic strategies in real-world elderly patients with both ACS and AF were affected mostly by the risk of bleeding instead of ischemic events. However, the application of OACs in the present elderly patients with ACS and AF conferred a 4 times lower risk of death, without an increase in bleeding. Similar efficacy of OACs was found in elderly individuals with AF (21, 30, 32). Therefore, greater efforts to improve the prescription of OACs in the elderly are necessary, especially among older subjects with ACS and AF. It was recommended by consensus that a short course of dual therapy with OAC and an antiplatelet agent (preferably P2Y12) should be considered as a preferred antithrombotic strategy in the therapeutic process of patients with both ACS and AF (9, 33), and OAC should be applied in the long term of the patients' antithrombotic procedure (9). In our study, we found that even after a long-term follow-up of 5 years, OACs could still safely reduce mortality in elderly patients with both ACS and AF.
The comparative efficacy and safety of NOAC and warfarin treatment among patients with AF has been the focus of clinical trials. The Asian subgroup analysis (34) of four major randomized control trials showed that NOACs were comparable to warfarin in the reduction in ischemic stroke and myocardial infarction. However, all-cause mortality and major bleeding were significantly lower in patients treated with NOACs. Consistent with the results, although the sample size was small, our study in elderly patients with ACS and AF validated the advantage of NOAC over warfarin for the reduction in all-cause mortality and major bleeding. This result indicated that NOACs could be safely applied in elderly patients with ACS and AF, especially in those who are at higher risk of bleeding when treated via comedication with antiplatelet agents.
Limitations
This study has several limitations, which should be mentioned. First, due to the relatively small sample size of the whole cohort, it is difficult to compare the outcomes among subgroups with various combinations of antiplatelet and anticoagulation strategies. However, we compared the efficacy and safety between NOAC (n = 94) and warfarin (n = 84) in elderly patients with ACS and AF. The advantage of NOAC over warfarin could be observed in the form of the lower risk of all-cause mortality and major bleeding (BARC ≥ 3), with marginal significance. These results are in agreement with previous studies, indicating the benefit of NOAC compared with warfarin extending to older adults with AF (35–37). Second, the consecutively recruited patients were followed-up for various lengths of time, ranging from 1 to 9 years. However, the efficacy and safety outcomes were compared in patients with the same length of follow-up, including 1-year and 5-year intervals. During both follow-up intervals, treatment with OAC was consistently associated with a lower risk of MACEs and bleeding. Finally, the present observational study was retrospectively designed and based on a single center cohort. The findings should be further validated in multicenter prospectively recruited patients.
Conclusion
Antithrombotic therapy with OACs in elderly patients with ACS and AF could decrease the risk of ischemic events without increasing bleeding. In real-world practice, it is necessary to strengthen the awareness of anticoagulant treatment in elderly patients with ACS and AF.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Chinese PLA General Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
TY: study concept and design and critical revision of the manuscript for important intellectual content. YWu, HL, LQ, YWa, SZ, YZ, and ZW: acquisition of data. YWu, HL, LQ, and TY: analysis and interpretation of data. YWu, HL, and TY: drafting of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 81870262 and 82170352) and Special Project on Logistics Health Care (No. 22BJZ31).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.923684/full#supplementary-material
References
1. Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. (2005) 149:67–73. doi: 10.1016/j.ahj.2004.06.003
2. Taggar JS, Lip GY. Anticoagulation for elderly patients with atrial fibrillation: not to be neglected. Europace. (2008) 10:1–2. doi: 10.1093/europace/eum223
3. Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. (2009) 373:1849–60. doi: 10.1016/S0140-6736(09)60503-1
4. Stegemann S, Ecker F, Maio M, Kraahs P, Wohlfart R, Breitkreutz J, et al. Geriatric drug therapy: neglecting the inevitable majority. Ageing Res Rev. (2010) 9:384–98. doi: 10.1016/j.arr.2010.04.005
5. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J. (2013) 34:3028–34. doi: 10.1093/eurheartj/eht356
6. Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. (2009) 30:1038–45. doi: 10.1093/eurheartj/ehn579
7. De Luca L, Casella G, Rubboli A, Gonzini L, Lucci D, Boccanelli A, et al. Recent trends in management and outcome of patients with acute coronary syndromes and atrial fibrillation. Int J Cardiol. (2017) 248:369–75. doi: 10.1016/j.ijcard.2017.08.019
8. Gallet R, Teiger E. Oral anticoagulants in elderly patients with coronary artery disease and atrial fibrillation. Ann Cardiol Angeiol (Paris). (2018) 67:404–10. doi: 10.1016/j.ancard.2018.09.013
9. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. (2021) 42:373–498. doi: 10.1093/eurheartj/ehab648
10. Lip GYH, Collet JP, Haude M, Byrne R, Chung EH, Fauchier L, et al. 2018 Joint European consensus document on the management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous cardiovascular interventions: a joint consensus document of the European Heart Rhythm Association (EHRA), European Society of Cardiology Working Group on Thrombosis, European Association of Percutaneous Cardiovascular Interventions (EAPCI), and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), Latin America Heart Rhythm Society (LAHRS), and Cardiac Arrhythmia Society of Southern Africa (CASSA). Europace. (2019) 21:192–3. doi: 10.1093/europace/euy174
11. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. (2016) 37:2893–962. doi: 10.5603/KP.2016.0172
12. January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. (2019) 140:e125–51. doi: 10.1161/CIR.0000000000000719
13. Aronow WS. Approach to symptomatic coronary disease in the elderly: TIME to change? Lancet. (2001) 358:945–6. doi: 10.1016/S0140-6736(01)06111-6
14. Rash A, Downes T, Portner R, Yeo WW, Morgan N, Channer KS. A randomised controlled trial of warfarin versus aspirin for stroke prevention in octogenarians with atrial fibrillation (WASPO). Age Ageing. (2007) 36:151–6. doi: 10.1093/ageing/afl129
15. Sardar P, Chatterjee S, Chaudhari S, Lip GY. New oral anticoagulants in elderly adults: evidence from a meta-analysis of randomized trials. J Am Geriatr Soc. (2014) 62:857–64. doi: 10.1111/jgs.12799
16. Siu CW, Tse HF. Net clinical benefit of warfarin therapy in elderly Chinese patients with atrial fibrillation. Circ Arrhythm Electrophysiol. (2014) 7:300–6. doi: 10.1161/CIRCEP.113.000858
17. Guo Y, Kotalczyk A, Imberti JF, Wang Y, Lip GYH. Poor adherence to guideline-directed anticoagulation in elderly Chinese patients with atrial fibrillation. A report from the Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. Eur Heart J Qual Care Clin Outcomes. (2021). qcab054. doi: 10.1093/ehjqcco/qcab054
18. Singh P, Arrevad PS, Peterson GM, Bereznicki LR. Evaluation of antithrombotic usage for atrial fibrillation in aged care facilities. J Clin Pharm Ther. (2011) 36:166–71. doi: 10.1111/j.1365-2710.2010.01167.x
19. Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. (2015) 131:157–64. doi: 10.1161/CIRCULATIONAHA.114.012061
20. Ajam T, Cumpian TL, Tilkens BL, Jahangir IA, Frost J, Ceretto C, et al. Non-vitamin K antagonist oral anticoagulants for stroke prevention in atrial fibrillation: safety issues in the elderly. Expert Rev Clin Pharmacol. (2020) 13:1309–27. doi: 10.1080/17512433.2020.1842191
21. Guo Y, Kotalczyk A, Imberti JF, Wang Y, Lip GYH. Quality indicators in the management of elderly Chinese patients with atrial fibrillation: a report from the optimal thromboprophylaxis in elderly chinese patients with atrial fibrillation (ChiOTEAF) registry. Eur Heart J Qual Care Clin Outcomes. (2021). qcab057. doi: 10.1093/ehjqcco/qcab057
22. Erez A, Goldenberg I, Sabbag A, Nof E, Zahger D, Atar S, et al. Temporal trends and outcomes associated with atrial fibrillation observed during acute coronary syndrome: Real-world data from the Acute Coronary Syndrome Israeli Survey (ACSIS), 2000-2013. Clin Cardiol. (2017) 40:275–80. doi: 10.1002/clc.22654
23. Guimarães PO, Zakroysky P, Goyal A, Lopes RD, Kaltenbach LA, Wang TY. Usefulness of antithrombotic therapy in patients with atrial fibrillation and acute myocardial infarction. Am J Cardiol. (2019) 123:12–8. doi: 10.1016/j.amjcard.2018.09.031
24. Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. (2007) 115:2689–96. doi: 10.1161/CIRCULATIONAHA.106.653048
25. Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. (2011) 123:2736–47. doi: 10.1161/CIRCULATIONAHA.110.009449
26. Shuvy M, Zwas DR, Keren A, Gotsman I. Value of the CHA(2) DS(2) -VASc score for predicting outcome in patients with heart failure. ESC Heart Fail. (2020) 7:2553–60. doi: 10.1002/ehf2.12831
27. Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J Am Coll Cardiol. (2011) 57:173–80. doi: 10.1016/j.jacc.2010.09.024
28. Sindet-Pedersen C, Lamberts M, Staerk L, Nissen Bonde A, Berger JS, Pallisgaard JL, et al. Combining oral anticoagulants with platelet inhibitors in patients with atrial fibrillation and coronary disease. J Am Coll Cardiol. (2018) 72:1790–800. doi: 10.1016/j.jacc.2018.07.054
29. Chang SS, Dong JZ, Ma CS, Du X, Wu JH, Tang RB, et al. Current status and time trends of oral anticoagulation use among chinese patients with nonvalvular atrial fibrillation: the Chinese atrial fibrillation registry study. Stroke. (2016) 47:1803–10. doi: 10.1161/STROKEAHA.116.012988
30. Winijkul A, Kaewkumdee P, Yindeengam A, Krittayaphong R. Characteristics and antithrombotic treatment patterns of patients with concomitant coronary artery disease and atrial fibrillation from Thailand's COOL-AF registry. BMC Cardiovasc Disord. (2021) 21:117. doi: 10.1186/s12872-021-01928-4
31. Wei L, Su E, Liu W, Xing W, Liu X, Zhang Y, et al. Antithrombotic therapy in coronary artery disease patients with atrial fibrillation. BMC Cardiovasc Disord. (2020) 20:323. doi: 10.1186/s12872-020-01609-8
32. Gabet A, Chatignoux E, Grave C, Vallée A, Tuppin P, Béjot Y, et al. Stroke incidence and death in atrial fibrillation patients newly treated with direct oral anticoagulants. Clin Epidemiol. (2021) 13:131–40. doi: 10.2147/CLEP.S290707
33. Mumoli N, Amellone C, Antonelli G, Augello G, Cloro C, D'Alleva A, et al. Clinical discussions in antithrombotic therapy management in patients with atrial fibrillation: a delphi consensus panel. CJC Open. (2020) 2:641–51. doi: 10.1016/j.cjco.2020.07.016
34. Wang KL, Lip GY, Lin SJ, Chiang CE. Non-Vitamin K antagonist oral anticoagulants for stroke prevention in asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. (2015) 46:2555–61. doi: 10.1161/STROKEAHA.115.009947
35. Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. (2014) 383:955–62. doi: 10.1016/S0140-6736(13)62343-0
36. Amin A, Garcia Reeves AB, Li X, Dhamane A, Luo X, Di Fusco M, et al. Effectiveness and safety of oral anticoagulants in older adults with non-valvular atrial fibrillation and heart failure. PLoS ONE. (2019) 14:e0213614. doi: 10.1371/journal.pone.0213614
Keywords: acute coronary syndrome, atrial fibrillation, oral anticoagulant, elderly, antithrombotic treatment
Citation: Wu Y, Liu H, Qin L, Wang Y, Zhang S, Wang Z, Zou Y and Yin T (2022) Efficacy and Safety of Antithrombotic Therapy With Oral Anticoagulants in Real-World Elderly Patients With Acute Coronary Syndrome and Atrial Fibrillation. Front. Cardiovasc. Med. 9:923684. doi: 10.3389/fcvm.2022.923684
Received: 19 April 2022; Accepted: 31 May 2022;
Published: 29 June 2022.
Edited by:
Jinfeng Xu, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Alberto Monello, Ospedaliera di Piacenza, ItalyPeng Yin, Chinese Center for Disease Control and Prevention, China
Copyright © 2022 Wu, Liu, Qin, Wang, Zhang, Wang, Zou and Yin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tong Yin, eWludG9uZzMwMUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Yangxun Wu
Yangxun Wu Haiping Liu1,2†
Haiping Liu1,2† Tong Yin
Tong Yin