Cardiovascular Risk According to Body Mass Index in Women of Reproductive Age With Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis
- 1The Second Clinical Medical College of Zhejiang Chinese Medical University, Hangzhou, China
- 2The First Clinical Medical College of Zhejiang Chinese Medical University, Hangzhou, China
- 3Department of Clinical Evaluation Center, The First Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, China
by Zhuang, C., Luo, X., Wang, W., Sun, R., Qi, M., and Yu, J. (2022). Front. Cardiovasc. Med. 9:822079. doi: 10.3389/fcvm.2022.822079
Introduction
Recently, we read a systematic review and meta-analysis written by Zhuang et al. (1), which is of great clinical significance and value. It was found that high-baseline blood pressure and dyslipidemia were common in women of reproductive age with PCOS: mainly, the increase of SBP and DBP, TG, nonHDL-C, and LDL-C and the decrease of HDL-C. However, these changes seem to have nothing to do with BMI.
Discussion
There were four retrieved databases mentioned in the abstract (the Cochrane Library, EMBASE, MEDLINE, and PubMed), but only three (the Cochrane Library, EMBASE, and MEDLINE) were demonstrated in the Search Strategy. The search strategy formats of PubMed and MEDLINE are different, but they are the same in this review, so the authors should clarify which one this strategy refers to. Meanwhile, the expression of medical subject headings in Pubmed-Medline (Table 1) sometimes used “mh” and sometimes used “Mesh.” It is recommended to use the same expression in one database. In addition, the search terms for different databases in the Study Design were not consistent. Adopting a proven and reliable search strategy is very necessary to obtain all the relative studies.
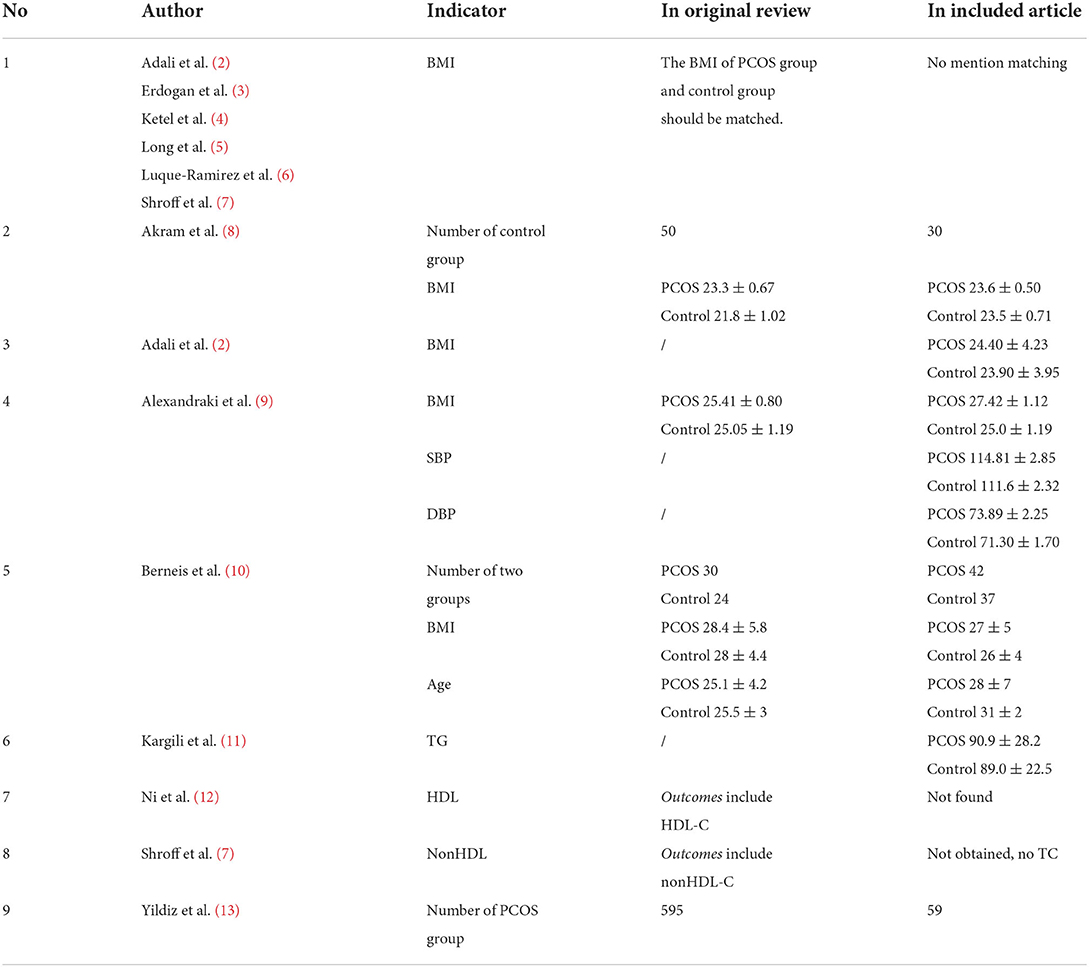
For the Study Selection and Criteria section, the inclusion and exclusion criteria were relatively clear. As mentioned in this article, the BMI of the PCOS group and control group should be matched, and their age should be roughly in one range. However, only parts of the included articles were explicitly BMI-matched; more details are shown in Table 1. Additionally, it is better to clarify the exact meaning of “roughly in one range.” Finally, there was a contradictive expression about language. The exclusion criteria mentioned articles published in languages other than English, but the authors declared they operated “without any language restriction” during retrieval in the Search Strategy section.
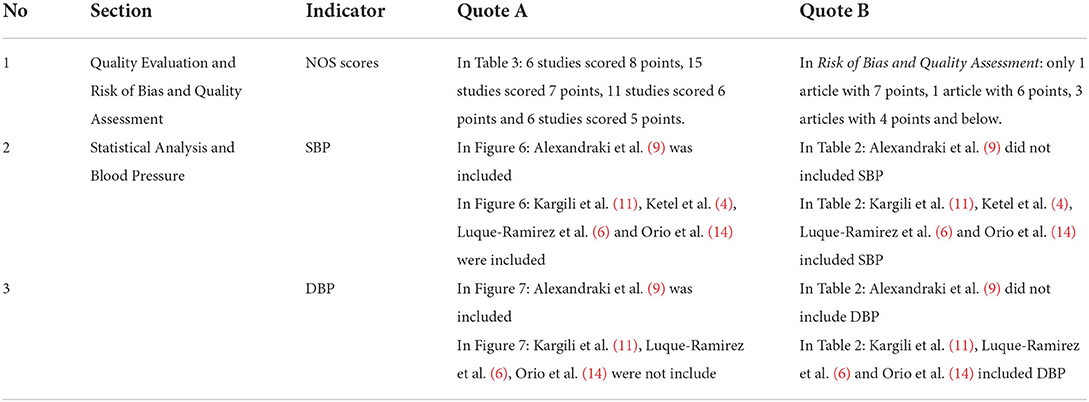
For the Data Extraction section, since nonHDL was not involved in any included articles, the authors pointed out that the nonHDL value is TC minus HDL. A detailed formula of its mean and deviation or relative references would make the results more reliable. For the Quality Evaluation section, the NOS scores were inconsistent with the description in Risk of Bias and Quality Assessment. Table 2 demonstrates the inconsistent descriptions. For the Analysis Characteristics section, the incorrectly extracted information is shown in Table 1. For the Result section, some inconsistent descriptions are listed in Table 2. Moreover, SBP and WHR lacked sensitivity analysis in the Result section.
The Discussion section was relatively detailed and clear. However, according to the inclusion and exclusion criteria, there were some inappropriate articles included and some incomplete data. Furthermore, it is noted that during the discussion of lipid profiles, the change of HDL in different subgroups seems to be ignored.
This meta-analysis links PCOS, obesity, and cardiovascular risk factors, which have great clinical guiding value. However, due to some inappropriate information, an updated meta-analysis is needed to better draw conclusions and clarify the impact of BMI on cardiovascular risk factors in patients with PCOS with reliable methods. Additionally, more rigorous and standardized clinical research reports are an important premise for reasonable systematic reviews with meaningful conclusions.
Author contributions
SL: design study, drafting the article, and making critical revisions. YK and KW: data collection, analysis, and drafting of the article. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhuang C, Luo X, Wang W, Sun R, Qi M, Yu J. Cardiovascular risk according to body mass index in women of reproductive age with polycystic ovary syndrome: a systematic review and meta-analysis. Front Cardiovasc Med. (2022) 9:822079. doi: 10.3389/fcvm.2022.822079
2. Adali E, Yildizhan R, Kurdoglu M, Bugdayci G, Kolusari A, Sahin HG. Increased plasma thrombin-activatable fibrinolysis inhibitor levels in young obese women with polycystic ovary syndrome. Fertil Steril. (2010) 94:666–72. doi: 10.1016/j.fertnstert.2009.03.037
3. Erdogan M, Karadeniz M, Alper GE, Tamsel S, Uluer H, Caglayan O, et al. Thrombin-activatable fibrinolysis inhibitor and cardiovascular risk factors in polycystic ovary syndrome. Exp Clin Endocrinol Diab. (2008) 116:143–7. doi: 10.1055/s-2007-992118
4. Ketel IJ, Stehouwer CD, Henry RM, Serné EH, Hompes P, Homburg R, et al. Greater arterial stiffness in polycystic ovary syndrome (PCOS) is an obesity but not a PCOS-associated phenomenon. J Clin Endocrinol Metab. (2010) 95:4566–75. doi: 10.1210/jc.2010-0868
5. Long J, Li L, Wang F, Yang G, Cheng W, Wei J, et al. Screening for a simple and effective indicator of insulin resistance in Chinese women of reproductive age, with the insulin clamp technique as a reference. Metab Syndr Relat Disord. (2019) 17:423–9. doi: 10.1089/met.2019.0019
6. Luque-Ramírez M, Mendieta-Azcona C, Alvarez-Blasco F, Escobar-Morreale HF. Androgen excess is associated with the increased carotid intima-media thickness observed in young women with polycystic ovary syndrome. Hum Reproduct. (2007) 22:3197–203. doi: 10.1093/humrep/dem324
7. Shroff R, Kerchner A, Maifeld M, Van Beek EJ, Jagasia D, Dokras A. Young obese women with polycystic ovary syndrome have evidence of early coronary atherosclerosis. J Clin Endocrinol Metab. (2007) 92:4609–14. doi: 10.1210/jc.2007-1343
8. Akram T, Hasan S, Imran M, Karim A, Arslan M. Association of polycystic ovary syndrome with cardiovascular risk factors. Gynecol Endocrinol. (2010) 26:47–53. doi: 10.3109/09513590903159565
9. Alexandraki K, Protogerou AD, Papaioannou TG, Piperi C, Mastorakos G, Lekakis J, et al. Early microvascular and macrovascular dysfunction is not accompanied by structural arterial injury in polycystic ovary syndrome. Hormones. (2006) 5:126–36. doi: 10.14310/horm.2002.11176
10. Berneis K, Rizzo M, Hersberger M, Rini GB, Di Fede G, Pepe I, et al. Atherogenic forms of dyslipidaemia in women with polycystic ovary syndrome. Int J Clin Pract. (2009) 63:56–62. doi: 10.1111/j.1742-1241.2008.01897.x
11. Kargili A, Karakurt F, Kasapoglu B, Derbent A, Koca C, Selcoki Y. Association of polycystic ovary syndrome and a non-dipping blood pressure pattern in young women. Clinics. (2010) 65:475–9. doi: 10.1590/S1807-59322010000500004
12. Ni RM, Mo Y, Chen X, Zhong J, Liu W, Yang D. Low prevalence of the metabolic syndrome but high occurrence of various metabolic disorders in Chinese women with polycystic ovary syndrome. Eur J Endocrinol. (2009) 161:411–8. doi: 10.1530/EJE-09-0298
13. Yildiz BO, Haznedaroglu IC, Kirazli S, Bayraktar M. Global fibrinolytic capacity is decreased in polycystic ovary syndrome, suggesting a prothrombotic state. J Clin Endocrinol Metab. (2002) 87:3871–5. doi: 10.1210/jcem.87.8.8716
Keywords: polycystic ovary syndrome, cardiovascular risk, reproductive age, body mass index, meta-analysis
Citation: Ke Y, Wu K and Liu S (2022) Commentary: Cardiovascular risk according to body mass index in women of reproductive age with polycystic ovary syndrome: A systematic review and meta-analysis. Front. Cardiovasc. Med. 9:920144. doi: 10.3389/fcvm.2022.920144
Received: 14 April 2022; Accepted: 19 July 2022;
Published: 10 August 2022.
Edited by:
Dexter Canoy, University of Oxford, United KingdomReviewed by:
Helena Teede, Monash University, AustraliaCopyright © 2022 Ke, Wu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shan Liu, Z3JheXN0YXI5MkAxNjMuY29t
 Yani Ke
Yani Ke Kaihan Wu
Kaihan Wu Shan Liu
Shan Liu