- 1Department of Cardiology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 2Office of Infection Management, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 3Department of Cardiology, Xinjiang Yili Friendship Hospital, Yili Kazak Autonomous Prefecture, Xinjiang, China
Background: Recently, the Age–Bleeding–Organ Dysfunction (ABO) algorithm was recommended by the Asian Pacific Society of Cardiology Consensus as a binary approach to evaluate bleeding risk. This analysis made comparison of the predictive performances between the PRECISE-DAPT and ABO bleeding score in identifying the risk of 12-months major bleeding in Chinese elderly patients over 65 years old patients who underwent percutaneous coronary intervention (PCI) during dual-antiplatelet therapy period.
Methods: A total of 2,037 elderly coronary artery disease (CAD) patients (≥65 years) receiving dual antiplatelet therapy (DAPT) after PCI were enrolled in the study. The predictive accuracy of the two bleeding risk scores (PRECISE-DAPT and ABO) was compared for identifying the risk of bleeding during the dual-antiplatelet therapy in patients who underwent PCI. Major clinically relevant bleeding events were defined according to the Bleeding Academic Research Consortium (BARC) criteria.
Results: The PRECISE-DAPT score in the no bleeding, BARC = 1 bleeding, BARC ≥ 2 bleeding patients was 23.55 ± 10.46, 23.23 ± 10.03, and 33.54 ± 14.33 (p < 0.001), respectively. Meanwhile, the ABO score in the three groups was 0.72 ± 0.80, 0.69 ± 0.81, and 1.49 ± 0.99 (p < 0.001), respectively. The C-statistic of the PRECISE-DAPT model for prediction of BARC ≥ 2 bleeding in overall patients was 0.717 (95% CI, 0.656–0.777) and 0.720 (95% CI, 0.656–0.784) in acute coronary syndrome (ACS) patients. Similar discriminatory capacity was demonstrated in the ABO risk score [overall, patients, AUC: 0.712 (95% CI, 0.650–0.774); ACS patients, AUC: 0.703 (95% CI, 0.634–0.772)]. No differences were observed when the ABO model was in comparison with the PRECISE-DAPT model, regardless in overall patients (z = −0.199, p = 0.842) or ACS patients (z = −0.605, p = 0.545). The calibration for BARC ≥ 2 bleeding of the PRECISE-DAPT and ABO score were acceptable, regardless in overall patients [goodness-of-fit (GOF) Chi-square = 0.432 and 0.001, respectively; p-value = 0.806 and 0.999, respectively] or ACS patients (GOF Chi-square = 0.008 and 0.580, respectively; p-value = 0.996 and 0.748, respectively).
Conclusion: No matter of clinical presentation in Asian 65-years older patients with DAPT, the PRECISE-DAPT, and ABO scores had the similar discriminative ability for 12-months BARC ≥ 2 bleeding. Considering the simplicity and reliability, the PRECISE-DAPT score might be more clinically applicable in the overall population and ACS patients in bleeding prediction.
Introduction
Cardiovascular diseases (CVDs), consisting of acute (ACS) or chronic coronary syndromes (CCS) and a diverse range of other CVDs, pose the leading cause of worldwide mortality and significantly contribute to reduce quality of life (1, 2). While the combination of anti-thrombotic medications such as aspirin and P2Y12 inhibitors, and the use of invasive risk stratification such as percutaneous coronary intervention (PCI) at early stage has improved the outcomes of ACS and CCS patients, the postoperative bleeding risk, especially during the dual-antiplatelet therapy period, remains a significant adverse complication (3). The bleeding complication is a common serious complication after PCI and during the duration of dual antiplatelet therapy (DAPT), notably in elderly patients, because the elderly frequently displays high possibility of more vessel’s lesions and life-threatening bleeding and other complex comorbidities (4, 5). Furthermore, it is also combined with incremental morbidity and mortality (6).
Up to now, various bleeding risk models have been confirmed to predict bleeding events at early and late stage, such as the CRUSADE (7, 8) and ACUITY (9, 10), PRECISE-DAPT, and ARC–HBR (11, 12) bleeding risk scores. Due to the unique and distinct characteristics of ACS/CCS patients in the Asia-Pacific region, including differences in clinical characteristics, the invasiveness and complexity of the procedure and low number of observed patients from the Asia-Pacific region in pivotal research on bleeding, the above mentioned bleeding risk scores, therefore, may not be directly applicable to these populations (13). The Age–Bleeding–Organ Dysfunction (ABO) was recently proposed as a binary approach to assist clinicians to evaluate bleeding risk of Asian Pacific Society and guide treatment by The Asian Pacific Society of Cardiology (14).
In order to guide clinical practice and, if possible, improve our awareness about bleeding complications, our study tried to evaluate and compare the performances of the PRECISE-DAPT, and ABO scores for predicting 12 months serious bleeding in coronary artery disease (CAD) patients receiving DAPT after PCI therapy.
Materials and Methods
Study Population
This was a multi-centered, retrospective study conducted among the patients who were diagnosed as coronary heart disease and received DAPT after PCI from the first affiliated hospital with Nanjing Medical University, the first affiliated Hospital of Soochow University, and the affiliated hospital of Yangzhou University from September 2016 to July 2018. All patients who met the inclusion criteria were retrospectively selected from the electronic medical records database at above centers. Inclusion criteria were as follows: (1) age equal to or older than 65 years, (2) all the patients received 1-year DAPT therapy, except for some of them changed to single antiplatelet therapy (SAPT) treatment due to bleeding complications. Patients were excluded for the following reasons: (1) patients that had contraindications to DAPT therapy such as active bleeding, peptic ulcer or were allergic to one or more antiplatelet drugs; (2) patients with hematological disorders; (3) patients with anticoagulation indications receiving oral anticoagulation therapy within 1 year after PCI according to the current principles of treatment; (4) the patients were complicated with serious diseases such as malignant tumor with less than 1 year life expectancy; and (5) incomplete follow-up data due to loss of contact. Furthermore, patients with a history of PCI intervention or coronary artery bypass surgery within 1 year before enrollment were also excluded in order to rule out possible increased bleeding risks associated with prolonged DAPT. Finally, there were 2,037 patients constituted the study population.
The details of clinical characteristics, antithrombotic therapy, angiography parameters, biochemical, blood routine test, and electrocardiography were collected retrospectively from the hospital medical electronic database at the time of index PCI (15). The study protocol was conducted in accordance with the Declaration of Helsinki and was approved by the institutional ethics committee of each participating center (No. 2020-SR-472). The informed consent of the participants was waived in the study and approved by our ethical committee.
Variable Definition
At the time of enrollment into the study, the patients’ clinical data were recorded, and the PRECISE-DAPT (16) and ABO (14) scores were calculated. The PRECISE-DAPT score was composed of five variables, such as age, hemoglobin, white blood cell count, creatinine clearance, and previous spontaneous bleeding. The ABO score was constituted by three category variables, including age (Frail elderly >75 years, advanced age >85 years, and life expectancy <1 year), bleeding (spontaneous intracranial hemorrhage, recurrent gastrointestinal bleeding, and hemoglobin <9 g/dl), organ dysfunction (liver cirrhosis, end-stage renal failure requiring dialysis, and bone marrow failure, e.g., severe thrombocytopenia, platelet count <50,000/μl, and stroke in the last 6 months) (14). Because the ABO score is a qualitative variable of binary classification, in order to facilitate comparison with the PRECISE-DAPT scores, we define each risk factor as 1 point, and then add each point for comparison. The total bleeding risk scores of PRECISE-DAPT were assessed using an online calculator by entering all variables for each patient.1 The predictive accuracy of the two bleeding risk scores was compared to identifying the bleeding risk during the dual-antiplatelet therapy in ACS/CCS patients undergoing PCI.
Endpoint Definition
The enrolled patients were followed up by a clinical visit supported by the phone interviewer (at least 1 year) after admission for the PCI in order to obtain the endpoint information. According to the Bleeding Academic Research Consortium (BARC) criteria, the clinically relevant bleeding events were defined as type 2 to 5 to compare the predictive accuracy of these scores (17). In addition, the patients with BARC 3 and 5 type bleeding events were further analyzed due to its serious clinical consequence. Details of the BARC criteria have been reported elsewhere (18). The information of bleeding sites, the levels of admission hemoglobin and nadir hemoglobin, and transfusion of red blood cells were recorded in our study, and clinically relevant bleeding events were defined as BARC 2 to BARC 5 bleeding (excluding BARC 4), no bleeding was defined as BARC 0 and minor and unactionable bleeding that does not need patients to seek unscheduled professional treatment was defined as BARC 1.
Statistical Analysis
The patients were classified in three risk categories for bleeding (no bleeding, BARC < 2 type bleeding and BARC ≥ 2 type bleeding and their characteristics were reported by descriptive statistics. Quantitative variables are reported as standard deviation (mean ± SD) or interquartile range, and qualitative variables are expressed as absolute numeric values and percentages. The χ2 test or Fisher Exact test was appropriately compared between quantitative and qualitative variables, and separate analysis was conducted among the patients’ diagnosed as CCS and ACS. A statistically significant difference indication was considered as a two-sided p-value < 0.05. Receiver operating characteristics (ROC) curves were used to evaluate the discriminative capacities of the two scores, and C-statistics greater than 0.7 was considered as an acceptable discriminatory capacity (19). The calibration of the models was evaluated using the Hosmer–Lemeshow goodness-of-fit (GOF) statistical test (20). A significant p-value less than 0.05 indicated a poor calibration. The C-statistics for the two risk models were compared to each other using the DeLong test (21). All data were processed by SPSS (version 26.0) statistical software and R language software (version 3.6.0).
Results
Baseline Characteristics
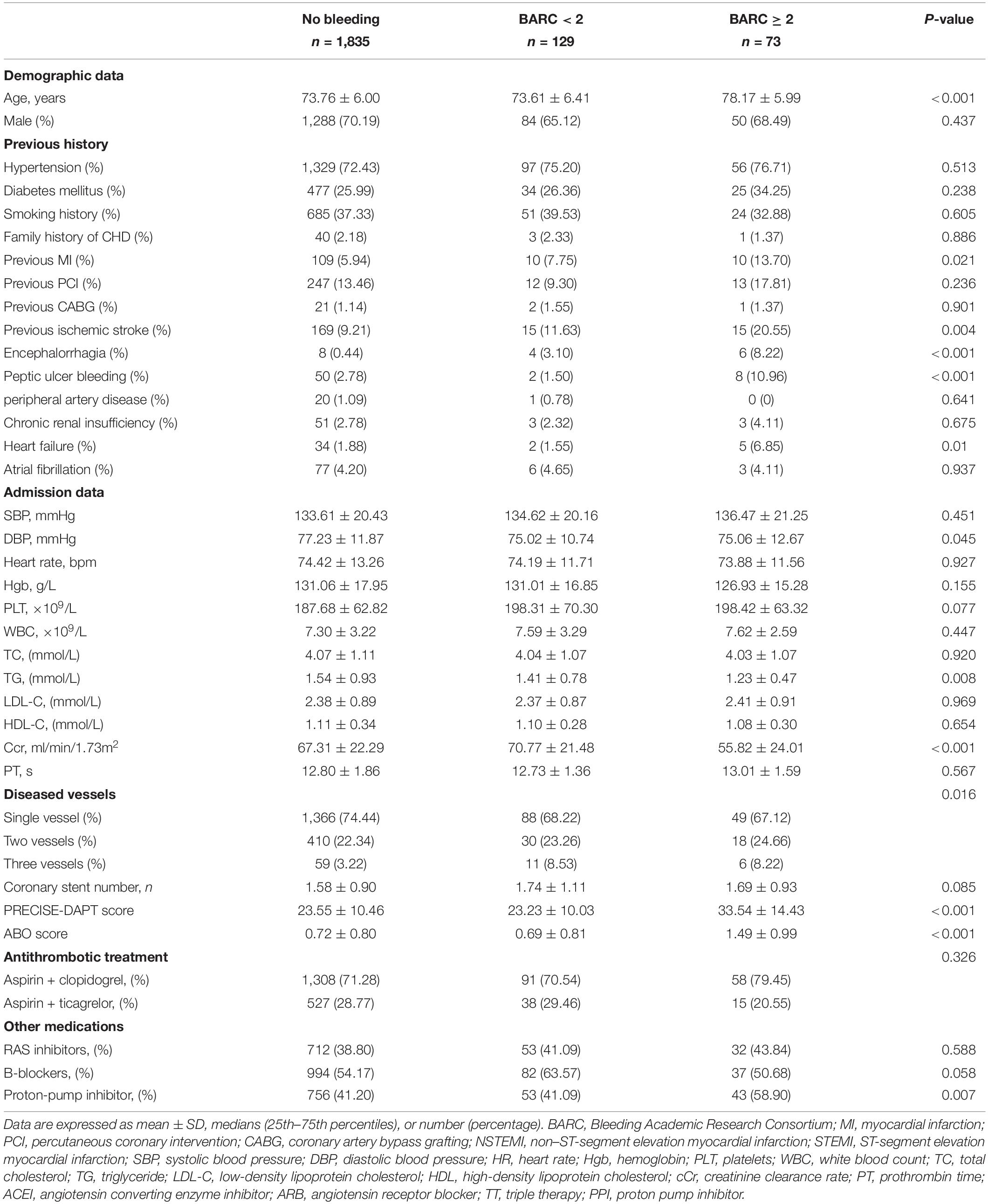
Table 1 shows the baseline characteristics of the study. The overall population age was 73.76 ± 6.00 years old, and women was 29.81%. Patients presented by ACS in 84.63% of cases, CCS in 15.37% of cases. Bleeding complications occurred in 202 patients, corresponding to an overall bleeding rate of almost 10%, BARC ≥ 2 bleeding complications occurred in 73 patients, among which, 22 cases of gastrointestinal hemorrhage, 8 cases of cerebral hemorrhage, 9 cases of urinary tract hemorrhage, 25 cases of skin and mucous membrane hemorrhage, and 9 cases of pulmonary hemorrhage. In addition, one type 5 and 10 BARC type 3 patients were recorded in our enrolled patients. Figure 1 shows details of the clinically relevant bleeding types. According to the above BARC bleeding criteria, the patients were stratified in three risk categories for bleeding: no bleeding group (n = 1,835), BARC < type 2 group (n = 129) and BARC ≥ type 2 group (n = 73). Among the three groups, age, history of myocardial infarction, cerebral infarction, cerebral hemorrhage, peptic ulcer bleeding and heart failure, the level of triglyceride, diastolic blood pressure, and creatinine, the number of diseased vessels, the score of PRECISE-DAPT score and ABO, the usage of PPI were statistically different (p < 0.05).
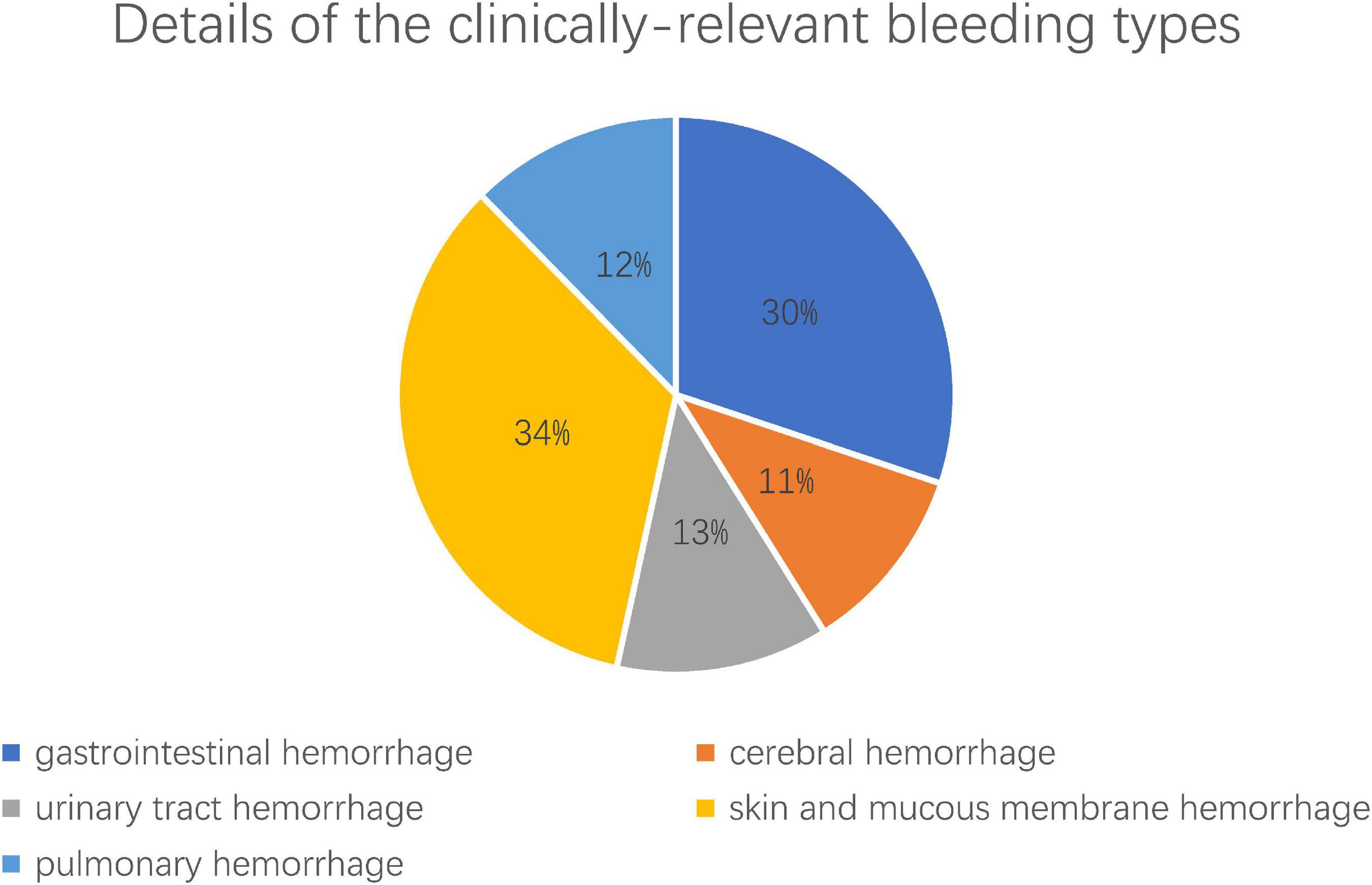
Figure 1. The details of the clinically relevant bleeding types after PCI. Clinically relevant bleeding complications (BARC = type 2–5, excluding BARC 4) including 22 (30%) cases of gastrointestinal hemorrhage, 8 (11%) cases of cerebral hemorrhage, 9 (13%) cases of urinary tract hemorrhage, 25 (34%) cases of skin and mucous membrane hemorrhage, and 9 (12%) cases of pulmonary hemorrhage.
In comparison with no bleeding group, patients of BARC ≥ type 2 group had a lower creatinine clearance rate (55.82 ± 24.01 vs. 67.31 ± 22.29 ml/min/1.73 m2, p < 0.001), lower level of triglyceride (1.22 ± 0.47 vs. 1.54 ± 0.93 mmol/L, p = 0.006), more advanced age (78.17 ± 5.99 vs. 73.76 ± 6.00, p < 0.001), higher ABO score (1.49 ± 0.99 vs. 0.72 ± 0.80, p < 0.001), and PRECISE-DAPT score (33.54 ± 14.33 vs. 23.55 ± 10.46, p < 0.001). More patients with BARC ≥ 2 type bleeding events had a history of myocardial infarction (13.70 vs. 5.94%, p = 0.007), cerebral infarction (20.55 vs. 9.21%, p = 0.001), cerebral hemorrhage (8.22 vs. 0.44%, p < 0.001), peptic ulcer (10.96 vs. 2.78%, p < 0.001), heart failure (6.85 vs. 1.88%, p = 0.003) and PPI usage after PCI (58.90 vs. 41.20%, p = 0.002) than the patients without bleeding events. In addition, patients of BARC ≥ type 2 group have a higher ABO score (1.49 ± 0.99 vs. 0.69 ± 0.81, p < 0.001) and PRECISE-DAPT score (33.54 ± 14.33 vs. 23.23 ± 10.03, p < 0.001) than the patients in BARC < type 2 group.
The Performance of Bleeding Prediction in the PRECISE-DAPT and Age–Bleeding–Organ Dysfunction Risk Score
In the study, we calculated the PRECISE-DAPT and ABO scores of 2,037 patients who underwent PCI. The PRECISE-DAPT score in the no bleeding, BARC < type 2 bleeding, BARC ≥ type 2 patients were 23.55 ± 10.46, 23.23 ± 10.03, and 33.54 ± 14.33 (p < 0.001), respectively. Meanwhile, the ABO score in the three groups was 0.72 ± 0.80, 0.69 ± 0.81, and 1.49 ± 0.99 (p < 0.001), respectively. The C-statistic of the PRECISE-DAPT model for prediction of BARC ≥ 2 bleeding in overall patients was 0.717 (95% CI, 0.656–0.777) and in ACS patients was 0.720 (95% CI, 0.656–0.784). The cutoff value of the PRECISE-DAPT model for prediction of BARC ≥ 2 bleeding in overall patients was 25 while in ACS patients was 32. In the overall population and ACS patients, respectively, the ABO risk score (C-statistics: 0.712 and 0.703, respectively; 95% CI: 0.650–0.774 and 0.634–0.772, respectively) was demonstrated similar discriminatory capacity. The cutoff value of the ABO model for prediction of BARC ≥ 2 bleeding was 1 both in overall and ACS patients (Table 2).
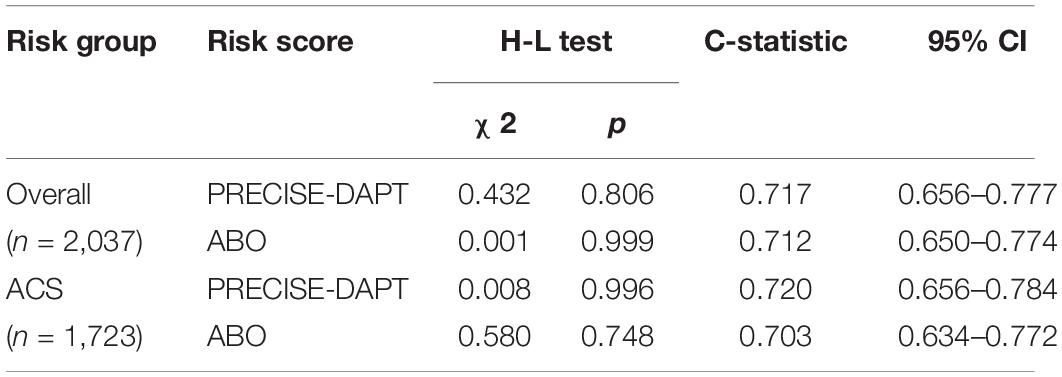
Table 2. Discrimination for the two risk scores of 12-months after PCI BARC ≥ 2 bleeding events in overall and STEMI patients.
Comparison of the Bleeding Prediction Ability in the PRECISE-DAPT and Age–Bleeding–Organ Dysfunction Risk Score
In order to compare the discriminative power of the two risk scores for predicting BARC ≥ 2 bleeding, the DeLong test was used to evaluate C-statistics each other. Table 3 showed that there were no statistical differences between the PRECISE-DAPT model and the ABO model in prediction of the BARC ≥ 2 bleeding events after PCI, regardless in overall patients (z = −0.199, p = 0.842) or ACS patients (z = −0.605, p = 0.545) (Figures 2 3). In addition, similar discriminative performance of the two risk score was observed in patients with BARC 3 and 5 bleeding events (Figure 4). The calibration abilities of the two risk scores were assessed by the Hosmer–Lemeshow GOF test. The calibration for BARC ≥ 2 bleeding of the PRECISE-DAPT and ABO score were acceptable, regardless in overall patients (GOF Chi-square = 0.432 and 0.001, respectively; p-value = 0.806 and 0.999, respectively) or ACS patients (GOF Chi-square = 0.008 and 0.580, respectively; p-value = 0.996 and 0.748, respectively) (Figures 2, 3).
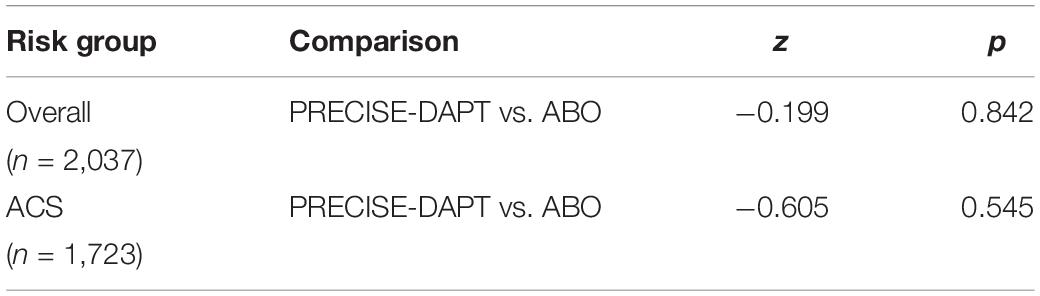
Table 3. Comparisons of the discriminative power of the two risk scores for predicting BARC ≥ 2 bleeding.
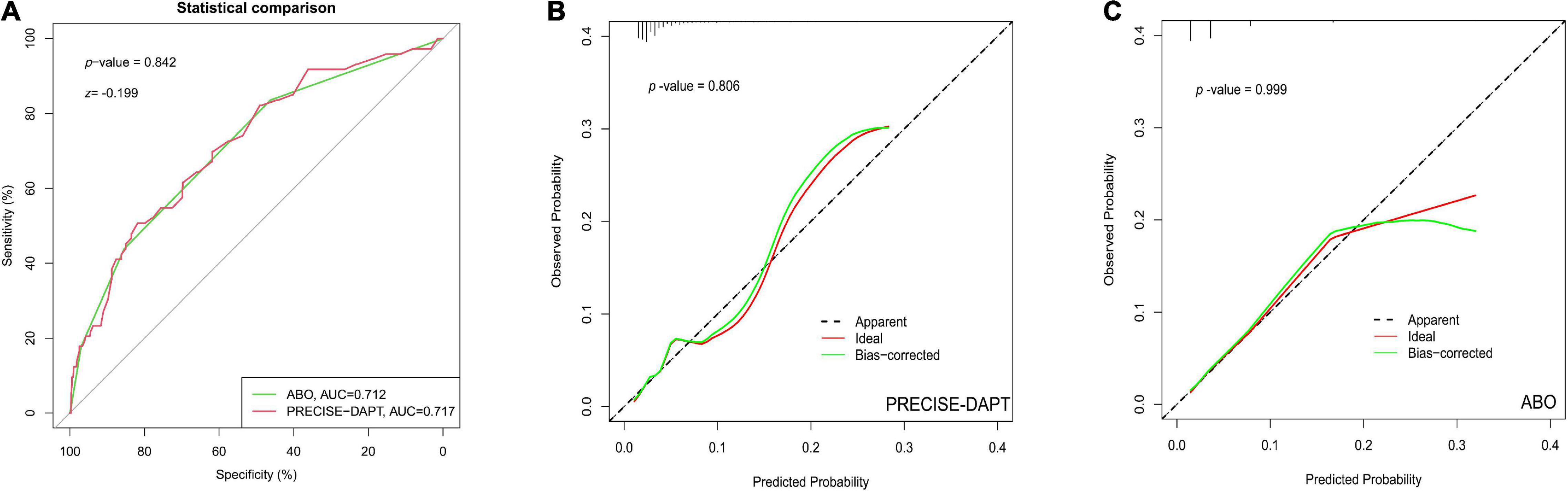
Figure 2. The performance of receiver operating characteristic (ROC) curve and calibration plot for PRECISE-DAPT and ABO risk score systems in overall patients with 1-year DAPT after PCI. (A) ROC curve for the prediction of BARC ≥ 2 type bleeding events by PRECISE-DAPT and ABO risk score systems in overall patients with 1-year DAPT after PCI [AUC: 0.717 and 0.712, respectively; (95% CI, 0.656–0.777)and (95% CI, 0.650–0.774), respectively; p < 0.001]. The C-statistics for the two risk models were compared to each other by the DeLong test (z = –0.199, p = 0.842). (B) The calibration plot for PRECISE-DAPT risk score in overall patients (GOF Chi-square = 0.432, p-value = 0.806). (C) The calibration plot for ABO risk score in overall patients (GOF Chi-square = 0.001 p-value = 0.999).
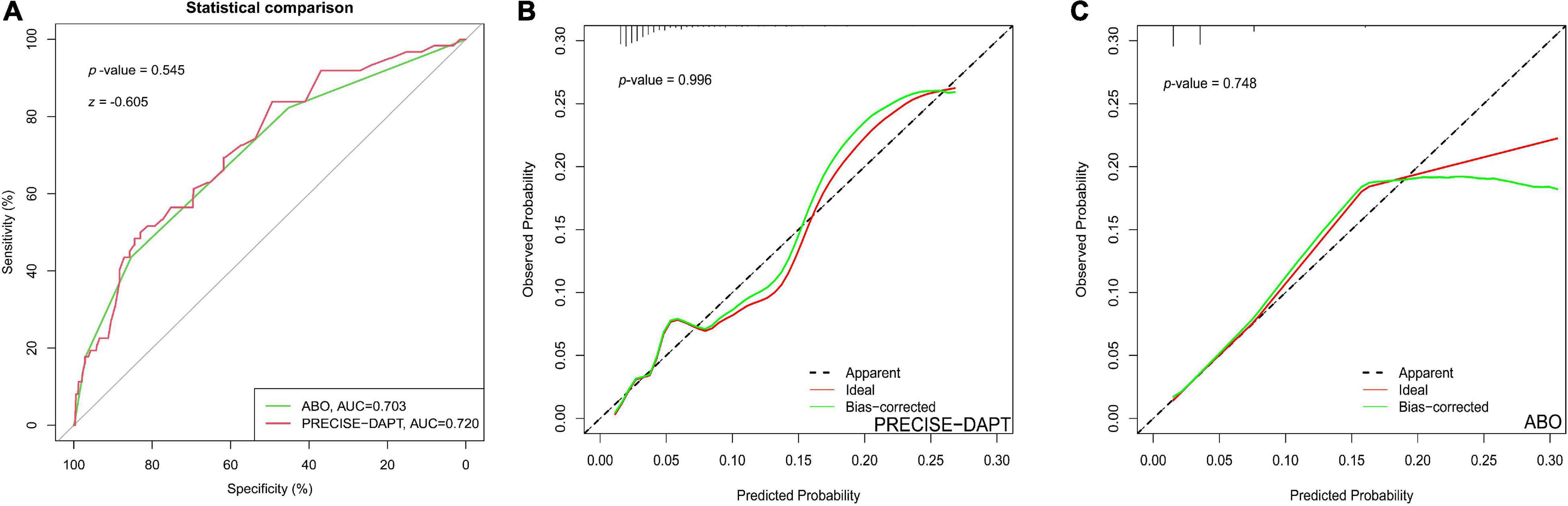
Figure 3. The performance of ROC curve and calibration plot for PRECISE-DAPT and ABO risk score systems in ACS patients with 1-year DAPT after PCI. (A) ROC curve for the prediction of BARC ≥ 2 type bleeding events by PRECISE-DAPT and ABO risk score systems in ACS patients with 1-year DAPT after PCI [AUC: 0.720 and 0.703, respectively; (95% CI, 0.656–0.784) and (95% CI, 0.634–0.772), respectively; p < 0.001]. The C-statistics for the two risk models were compared to each other by the DeLong test (z = –0.605, p = 0.545). (B) The calibration plot for the PRECISE-DAPT risk score in ACS patients (GOF Chi-square = 0.008, p-value = 0.996). (C) The calibration plot for the ABO risk score in ACS patients (GOF Chi-square = 0.580 p-value = 0.748).
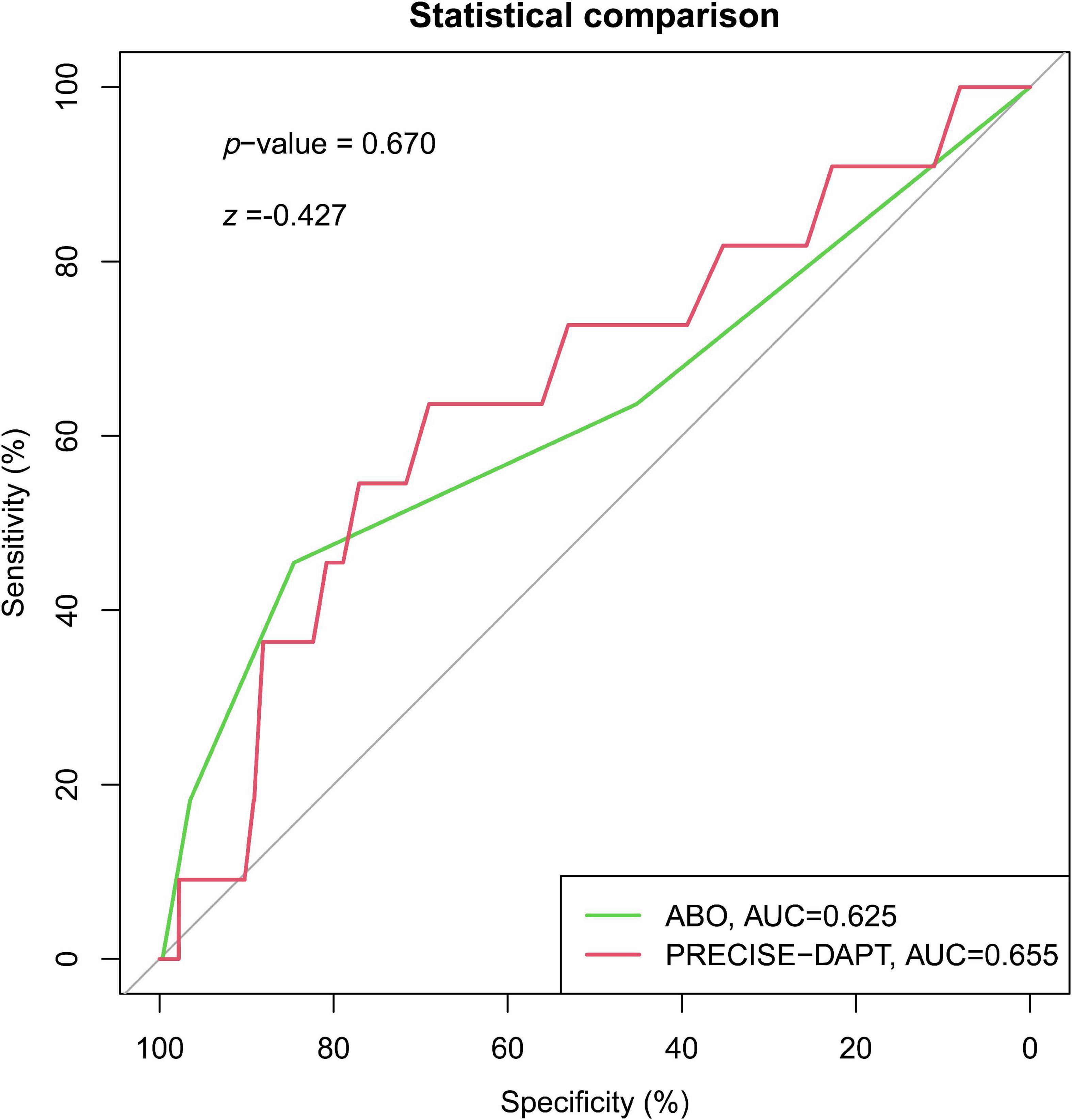
Figure 4. Receiver operating characteristic curve for the prediction of BARC = 3 or 5 type bleeding events by PRECISE-DAPT and ABO risk score systems in overall patients with 1-year DAPT after PCI [AUC: 0.655 and 0.625, respectively; (95% CI, 0.486–0.823) and (95% CI, 0.428–0.823), respectively; p = 0.076 and p = 0.152, respectively). The C-statistics for the two risk models were compared to each other by the DeLong test (z = –0.427, p = 0.670).
Discussion
Our study investigated the predictive performance between the PRECISE-DAPT and the ABO bleeding risk score, for 12-months clinically relevant bleeding complications post-PCI in Asian 65 year-older patients with DAPT. The main findings reported in this study can be summarized as follows: (1) No matter of clinical presentation, the PRECISE-DAPT, and ABO scores had adequate discriminative abilities (C-statistics: 0.70–0.75) for predicting 12-months BARC ≥ 2 bleeding after PCI. (2) Compared with the PRECISE-DAPT score, the ABO score showed a similar discriminative capacity for BARC ≥ 2 bleeding both in the overall and ACS patients.
Considering the higher mortality rate associated with bleeding manifestations, especially DAPT-related bleeding after PCI, bleeding prediction models play a more significant role in risk stratification and the choice of treatment. Approximately 11 years ago, the CRUSADE and ACUITY scores were designed to assess bleeding in ACS patients after PCI (8, 22). However, the bleeding predictive performance of the two risk scores should be updated, as the interventional procedure such as the access route of coronary angiography and anti-thrombotic medications have changed over time. Considering the changes, the PRECISE-DAPT score system was proposed in 2017 (6), which focused on the assessment of bleeding risk within 12 months after PCI. The short-term DAPT treatment was recommended for patients with score >25, which can outweigh the risks of extended treatment duration (23, 24), and we previously found that the PRECISE-DAPT score can predict BARC ≥ 2 bleeding events with a cutoff value of 32 in elderly patients over 75 (15). Consistently, this study found that the PRECISE-DAPT score remained efficient to predict 12-months BARC ≥ 2 bleeding in Asian elderly patients (≥65 years) receiving DAPT therapy. Even more, in the elderly ACS sub-group, the predictive performance of the PRECISE-DAPT score for clinically relevant bleeding was still efficient. Taken together, our results may indicate that PRECISE-DAPT is a feasible and reliable algorithm to evaluate the bleeding risk in Asian patients (aged ≥65 years) with DAPT within 12-month post-PCI. Furthermore, compared with patients on standard DAPT after drug-eluting stent implantation, the PRECISE-DAPT showed consistently prediction of bleeding risk, either in patients on ticagrelor monotherapy after 1-month DAPT or on aspirin monotherapy after 12-month DAPT (25). Even more, the 4-item PRECISE-DAPT score showed the similar discriminative ability to the 5-item iteration when white-blood-cell count was not available.
However, it was worth noting that, when compared with Western patients, the Asian patients had some special characteristics, such as lower systolic blood pressure (SBP) and heart rate, the amount of the prevalence of anemia and the rate of iatrogenic vessel access injury was relatively small (26–28). Therefore, the Age–Bleeding–Organ Dysfunction (“ABO”) algorithm was recently recommended by the Asian Pacific Society of Cardiology Consensus to evaluate bleeding risk in Asian stable CCS patients. In order to test the applicability of the new proposed recommendation in Asian elderly patients, we then analyzed the performance of the ABO algorithm in the prediction for the 1-year bleeding outcome in our study. Surprisingly, a similar discriminative performance of clinically relevant (BARC ≥ 2 type) or (BARC 3 or 5 type) bleeding during 12 months was observed in the ABO score when compared with the PRECISE-DAPT scores, irrespective in the overall population or ACS patients. Therefore, our results may indicate that the ABO score could be a candidate algorithm for Asian patients with clinically relevant bleeding prediction within 12-months DAPT post-PCI.
Limitations
Several limitations in our study should be considered. Firstly, compared with other studies, this retrospective study had a relatively small sample size and a lower incidence of bleeding complications. Secondly, several drawbacks of the ABO algorithm should be mentioned before its clinical use. The ABO score lacks specific quantitative points and is relatively rough because of its binary approach, to facilitate calculating the bleeding risk of ABO score, and our study defines each risk factor as 1 point in the model. In fact, the weight of each risk factor is quite different (for example, both Frail elderly >75 years, advanced age >85 years, and life expectancy <1 year was 1 point when calculating the bleeding risk). Therefore, more samples are needed to calculate the weight of each risk factor in bleeding. Also, the ACS presentation per se has been confirmed to enhance major and actionable bleeding risks within 1 year after PCI (12, 29). The ABO score was originally designed to evaluate the bleeding risk in CCS patients and did not include the acute presentation, which may underestimate the risk of bleeding in ACS patients. Thirdly, the ABO algorithm, including those variables such as end-stage renal failure requiring dialysis or bone marrow failure (severe thrombocytopenia, platelet count <50,000/μl). Considering the high bleeding risk (HBR) after PCI in those kinds of patients, most of them will not receive PCI treatment or the intensity of antiplatelet therapy is usually relatively low in those patients. Therefore, there may be certain of selection bias when using the ABO algorithm to predict the bleeding after PCI in the real world. Consequently, considering the simplicity and reliability for calculation, the PRECISE-DAPT score might be more suitable than ABO score for clinical use in Asian patients at present. In addition, the recently developed ARC–HBR (the Academic Research Consortium for HBR) consortium was used to identify HBR patients after PCI, which has been validated the ability in large real-world cohorts of patients undergoing PCI for ACS and CCS (11, 29). Therefore, more consortiums, including ARC–HBR, PRECISE-DAPT, or ABO should be applied to identify the high bleeding patients after PCI in the future.
Conclusion
No matter of clinical presentation, the PRECISE-DAPT, and ABO scores had possibly the similar discriminative ability for 12-months BARC ≥ 2 bleeding in Asian 65-year older patients with DAPT. Considering simplicity, reliability, and discriminative ability, the PRECISE-DAPT score might be more suitable in the overall population and ACS patients for the clinically relevant bleeding prediction of 12-months post-PCI. However, the ABO score also proves that along with the risk category, transition from low to high in 1 year, the probability of bleeding would increase subsequently.
This study would help clinicians make a distinction between different risk stratifications and provide assistance in the assessment and management of bleeding and ischemic risks in Asian ACS/CCS patients.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The study protocol was conducted in accordance with Declaration of Helsinki and was approved by the Institutional Ethics Committee of each participating center (No. 2020-SR-472). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
LD: conceptualization, methodology, software, investigation, formal analysis, and writing—original draft. CLu: data curation and writing—original draft. CW, CF, DX, and LG: visualization, investigation, data curation, and follow-up. MK: review and editing. QY and ZY: resources and supervision. LX, CLe, and WJ: visualization and writing—review and editing. WJ: conceptualization, funding acquisition, resources, supervision, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC 82170269 and 81570328), the Jiangsu Province’s Key Provincial Talents Program (ZDRCB2016005), the Foundation of Clinical Medical Research Center of Yili Autonomous Prefecture (YL2020ms09), and the Jiangsu Students’ Platform for Innovation and Entrepreneurship Training Program (2020103112008Y).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. (2019) 74:2529–32.
2. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes the task force for the diagnosis and management of chronic coronary syndromes of the European society of cardiology (ESC). Eur Heart J. (2020) 41:407–77.
3. Rao SV, O’Grady K, Pieper KS, Granger CB, Newby LK, Mahaffey KW, et al. A comparison of the clinical impact of bleeding measured by two different classifications among patients with acute coronary syndromes. J Am Coll Cardiol. (2006) 47:809–16. doi: 10.1016/j.jacc.2005.09.060
4. Choi SY, Kim MH, Cho YR, Sung Park J, Min Lee K, Park TH, et al. Performance of PRECISE-DAPT score for predicting bleeding complication during dual antiplatelet therapy. Circ Cardiovasc Interv. (2018) 11:e006837.
5. Sandhu K, Nadar SK. Percutaneous coronary intervention in the elderly. Int J Cardiol. (2015) 199:342–55.
6. Costa F, van Klaveren D, James S, Heg D, Räber L, Feres F, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. (2017) 389:1025–34. doi: 10.1016/S0140-6736(17)30397-5
7. Xi SZ, Zhou S, Wang X, Liu J, Qin L, Liu J, et al. The performance of CRUSADE and ACUITY bleeding risk scores in ticagrelor-treated ACS patients who underwent PCI. Thromb Haemost. (2017) 117:2186–93. doi: 10.1160/TH17-04-0237
8. Subherwal S, Bach RG, Chen AY, Gage BF, Rao SV, Newby LK, et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) bleeding score. Circulation. (2009) 119:1873–82.
9. Liu R, Lyu SZ, Zhao GQ, Zheng W, Wang X, Zhao XD, et al. Comparison of the performance of the CRUSADE, ACUITY-HORIZONS, and ACTION bleeding scores in ACS patients undergoing PCI: insights from a cohort of 4939 patients in China. J Geriatr Cardiol. (2017) 14:93–9. doi: 10.11909/j.issn.1671-5411.2017.02.011
10. Castini D, Centola M, Ferrante G, Cazzaniga S, Persampieri S, Lucreziotti S, et al. Comparison of CRUSADE and ACUITY-HORIZONS bleeding risk scores in patients with acute coronary syndromes. Heart Lung Circ. (2019) 28:567–74.
11. Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the academic research consortium for high bleeding risk. Eur Heart J. (2019) 40:2632–53. doi: 10.1093/eurheartj/ehz372
12. Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. (2021) 42:1289–367.
13. Chi GC, Kanter MH, Li BH, Qian L, Reading SR, Harrison TN, et al. Trends in acute myocardial infarction by race and ethnicity. J Am Heart Assoc. (2020) 9:e013542.
14. Tan JWC, Chew DP, Brieger D, Eikelboom J, Montalescot G, Ako J, et al. 2020 asian pacific society of cardiology consensus recommendations on antithrombotic management for high-risk chronic coronary syndrome. Eur Cardiol. (2021) 16:e26. doi: 10.15420/ecr.2020.45
15. Qian Y, Xu B, Qian X, Cao L, Cheng Y, Liu X, et al. Incidence and risk factors for antiplatelet therapy-related bleeding complications among elderly patients after coronary stenting: a multicenter retrospective observation. Front Pharmacol. (2021) 12:661619. doi: 10.3389/fphar.2021.661619
16. Watanabe H, Domei T, Morimoto T, Natsuaki M, Shiomi H, Toyota T, et al. Effect of 1-month dual antiplatelet therapy followed by clopidogrel vs 12-month dual antiplatelet therapy on cardiovascular and bleeding events in patients receiving PCI The STOPDAPT-2 randomized clinical trial. JAMA. (2019) 321:2414–27.
17. Le May M, Wells G, So D, Chong AY, Dick A, Froeschl M, et al. Safety and efficacy of femoral access vs radial access in ST-segment elevation myocardial infarction: the SAFARI-STEMI randomized clinical trial. JAMA Cardiol. (2020) 5:126–34. doi: 10.1001/jamacardio.2019.4852
18. Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium. Circulation. (2011) 123:2736–47. doi: 10.1161/CIRCULATIONAHA.110.009449
19. Núñez E, Steyerberg EW, Núñez J. [Regression modeling strategies]. Rev Esp Cardiol. (2011) 64:501–7.
20. Lemeshow S, Hosmer DW Jr. A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. (1982) 115:92–106.
21. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. (1988) 44:837–45.
22. Mehran R, Pocock SJ, Nikolsky E, Clayton T, Dangas GD, Kirtane AJ, et al. A risk score to predict bleeding in patients with acute coronary syndromes. J Am Coll Cardiol. (2010) 55:2556–66.
23. Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. (2016) 68:1082–115.
24. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention. (2019) 14:1435–534.
25. Gragnano F, Heg D, Franzone A, McFadden EP, Leonardi S, Piccolo R, et al. PRECISE-DAPT score for bleeding risk prediction in patients on dual or single antiplatelet regimens: insights from the GLOBAL LEADERS and GLASSY. Eur Heart J Cardiovasc Pharmacother. (2022) 8:28–38.
26. Liu J, Hong Y, D’Agostino RB Sr., Wu Z, Wang W, Sun J, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese multi-provincial cohort study. JAMA. (2004) 291:2591–9. doi: 10.1001/jama.291.21.2591
27. Kang HJ, Clare RM, Gao R, Held C, Himmelmann A, James SK, et al. Ticagrelor versus clopidogrel in Asian patients with acute coronary syndrome: a retrospective analysis from the platelet inhibition and patient outcomes (PLATO) trial. Am Heart J. (2015) 169:899–905.e1. doi: 10.1016/j.ahj.2015.03.015
28. Jones DA, Gallagher S, Rathod KS, Redwood S, de Belder MA, Mathur A, et al. Mortality in South Asians and Caucasians after percutaneous coronary intervention in the United Kingdom: an observational cohort study of 279,256 patients from the BCIS (British Cardiovascular Intervention Society) National Database. JACC Cardiovasc Interv. (2014) 7:362–71. doi: 10.1016/j.jcin.2013.11.013
Keywords: bleeding risk scores, percutaneous coronary intervention, dual-antiplatelet therapy, PRECISE-DAPT, ABO score
Citation: Dong L, Lu C, Wensen C, Fuzhong C, Khalid M, Xiaoyu D, Guangjuan L, Yanxia Q, Yufeng Z, Xinjian L, Leilei C and Junhong W (2022) Performance of PRECISE-DAPT and Age–Bleeding–Organ Dysfunction Score for Predicting Bleeding Complication During Dual Antiplatelet Therapy in Chinese Elderly Patients. Front. Cardiovasc. Med. 9:910805. doi: 10.3389/fcvm.2022.910805
Received: 01 April 2022; Accepted: 31 May 2022;
Published: 08 July 2022.
Edited by:
Ying Xian, Duke University, United StatesReviewed by:
Felice Gragnano, University of Campania Luigi Vanvitelli, ItalyAndreas Mitsis, University of Cyprus, Cyprus
Copyright © 2022 Dong, Lu, Wensen, Fuzhong, Khalid, Xiaoyu, Guangjuan, Yanxia, Yufeng, Xinjian, Leilei and Junhong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chen Leilei, Y2hlbmxlaTE5NzYyMDAyQDE2My5jb20=; Wang Junhong, d2FuZ2p1bmhvbmdAanNwaC5vcmcuY24=
†These authors have contributed equally to this work
 Liang Dong
Liang Dong Cao Lu
Cao Lu Chen Wensen
Chen Wensen Chen Fuzhong1
Chen Fuzhong1 Qian Yanxia
Qian Yanxia Liu Xinjian
Liu Xinjian