- 1Department of Neurology, Qingdao Municipal Hospital, Qingdao University, Qingdao, China
- 2Department of Cardiology, Qingdao Municipal Hospital, Qingdao University, Qingdao, China
Background: The effect of extreme sleep duration on the risk of cardiovascular and cerebrovascular diseases (CCDs) remains debatable. The pathology of CCDs is consistent in some respects (e.g., vascular factors), suggesting that there may be an overlapping range of sleep duration associated with a low risk of both diseases We aimed to quantify the dose-response relationship between sleep duration and CCDs.
Study objective: To explore whether there is an optimal sleep duration (SD) in reducing the risk of CCDs.
Methods: PubMed and EMBASE were searched until June 24, 2022 to include cohort studies that investigated the longitudinal relationships of SD with incident CCDs, including stroke and coronary heart disease (CHD). The robusterror meta-regression model (REMR model) was conducted to depict the dose-response relationships based on multivariate-adjusted risk estimates.
Results: A total of 71 cohorts with 3.8 million participants were included for meta-analysis, including 57 for cardiovascular diseases (CVD) and 29 for cerebrovascular disease. A significant U-shaped relationship was revealed of nighttime sleep duration with either cardiovascular or cerebrovascular disease. The nighttime sleep duration associated with a lower risk of CVD was situated within 4.3–10.3 h, with the risk hitting bottom at roughly 7.5 h per night (pnon–linearity < 0.0001). Sleep duration associated with a lower risk of cerebrovascular diseases ranges from 5 to 9.7 h per night, with the inflection at 7.5 h per night (pnon–linearity = 0.05). Similar non-linear relationship exited in daily sleep duration and CCDs. Other subgroup analyses showed non-linear relationships close to the above results.
Conclusion: Rational sleep duration (7.5 h/night) is associated with a reduced risk of cardio-cerebrovascular disease for adults.
Introduction
Ischemic cardiovascular disease contributes significantly to global morbidity and mortality, with approximately 18 million deaths per year, nearly 9 million because of coronary heart disease (CHD) and 6 million as a result of stroke (1, 2). Also, 15 million experience a stroke annually. Concerning the CVD-related deaths in most advanced economies, more than half occur in the middle-aged and one-third in the elderly population (3). Variations in the pathological mechanisms, regional susceptibilities, and stage failures are present in cardiovascular and cerebrovascular diseases (CCDs).
Moreover, the modifiable risk factors that influence the occurrence of CVD encompass stress, depression and anxiety, cholesterol and lipids, unhealthy diet, obesity, physical inactivity, diabetes mellitus, smoking, and hypertension. In this case, lifestyle changes and medications are crucial for the prevention and management of CVD. However, the latter approach could also have negative consequences, such as experiencing a greater degree of side effects, worsening compliance rates, and increasing burden on the organs due to the medications. Such drawbacks underscore the importance of pursuing the former option instead (a healthy lifestyle), which includes enhancing the quality of one’s sleep.
The existing literature has underscored how addressing sleep disorders could serve as a promising goal in preventing CCDs, but the public’s awareness of its importance is yet to be developed, and the evidence is still limited. A key indicator of sleep quality is the duration, where sleep deprivation or oversleeping are linked to the increased risk of CCDs, but since this relationship was found to have a null, J-, or U-shaped curve, it remained controversial. In specific areas, e.g., vascular factors, the pathology of CCDs is reliable, implying the existence of a shared range of sleep deprivation that could decrease people’s risks of both diseases. A limited number of studies examined the overlapping sleep duration for a lower risk of acquiring them. While new papers have been published on this subject in the past 5 years, the findings were inconsistent (4–12). Thus, through meta-analysis, this research seeks to revise the association of sleep duration with CCDs and unveil the sleep duration range valuable to preventing these diseases.
Materials and methods
Literature search strategy and selection criteria
We conducted a literature search on PubMed (Medline) and EMBASE to obtain cohort studies till June 2022, using the following unrestricted search terms: cohort, longitudinal, prospective, retrospective, nested case-control, stroke, cerebral hemorrhage, cerebral infarction, cerebrovascular accident, CVD, cardiovascular disease, CHD, myocardial infarction, CHD, MI, sleep duration, for the search terms see Supplementary File. In addition, we reviewed studies included in the previously published Meta-analysis to identify additional relevant studies. Studies were accepted for inclusion if they also met the following criteria: (1) it is a longitudinal study; (2) the study explored the association between daily or nighttime sleep duration with incident risk of cardiovascular disease and cerebrovascular disease; (3) relative risk (RR) with a 95%confidence interval (CI) was reported for at least two categories of sleep duration. Studies will be excluded if they fail to meet the abovementioned inclusion criteria. We included a larger sample size or longer follow-up if the study population was reported repetitively.
Data extraction
Two researchers (H-YM and T-CC) independently extracted data using a standardized electronic format. The following information was extracted from each study, including the first author, publication year, study name, country, follow-up duration, age, gender, the sample size for analysis, number of incident cases, sleep duration, diagnosis method for cardio-cerebrovascular diseases, adjusted confounders, and the multivariable-adjusted risk estimates. The results by gender were treated as two separate reports.
Assessment of the study quality
A modified Newcastle-Ottawa Quality Assessment Scale (mNOS) (13, 14) was used to assess the quality of qualified studies. The total score of mNOS was regarded here as a proxy to determine the overall risk of bias for every single investigation. The score for each item evaluated the associated risk of bias (Supplementary Table 1) in three domains: selection (generalizability, assessment bias, and potential reverse causality), confounding bias, and outcome (assessment bias and attrition bias).
Statistical analysis
The multivariable–adjusted risk estimates and 95% CI were log-transformed and pooled using random models (DerSimonian-Laird method). Some studies reported odds ratios (OR) but not relative risk (RR) or HRs. Since ORs tend to overestimate the effect size compared with RRs/HRs, especially when the incidence is not low, we used the following algorithm to convert ORs to RRs: (15).
P0 indicates the incidence of endpoint (cardiovascular or cerebrovascular diseases) in the non-exposed group of cohorts. When P0 is not available, the incidence rate of the total sample was used as a proxy (15).
Analyses were performed separately according to outcome (CCDs) and exposure (nighttime and daily sleep duration). We used the inverse variance weighted least squares regression with cluster robust error meta-regression model (REMR model) (16, 17). Heterogeneity was assessed by Q-test and quantified by the I2 metric. Subgroup analyses by gender and outcome group were performed. The robustness of the results was examined by excluding those rated as at a higher risk of bias. The potential publishing bias was estimated Egger regression test. For studies that were not the lowest category in the reference group, we reclassified the lowest category as a reference and recalculated the impact using the Orsini method (18). We took the midpoint of the upper and lower boundaries of each type of sleep duration as the average level. If studies with open boundaries, we multiplied or divided the reported boundary by 1.25. Stata V.15.1 (StataCorp LLC, USA) was used to conduct the dose-response analyses.
Results
Literature search
The process of literature screen and selection is shown in Figure 1. As for cardiovascular disease (Figure 1A), the search yielded 3,888 articles after deduplication, among which 98 articles were considered potentially eligible after scanning the titles and abstracts. After reviewing the full text, 42 articles were further excluded and one additional article was supplemented. Finally, 57 articles were included, including 33 studies for any cardiovascular disease (CVD), 24 for CHD, and 11 for myocardial infarction (MI). As for cerebrovascular disease (Figure 1B), the search yielded 911 articles after deduplication, among which 54 articles were considered potentially eligible. Finally, 29 articles were included, including 28 studies for stroke, 6 for ischemic stroke and 5 for hemorrhage stroke.
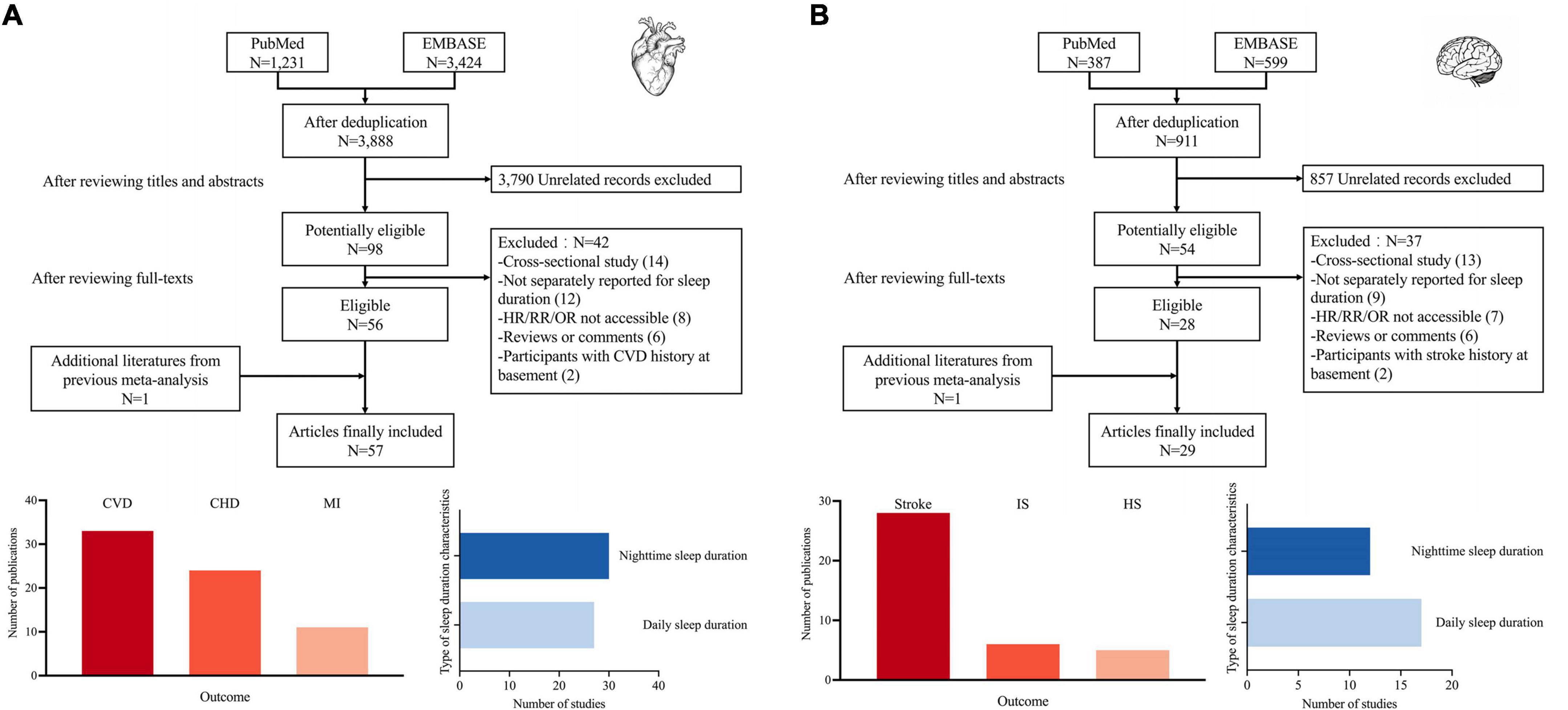
Figure 1. Search flowchart and summary characteristics of included studies, (A) for cardiovascular diseases and (B) for cerebrovascular diseases. CVD, cardiovascular disease; CHD, coronary heart disease; MI, myocardial infarction; IS, ischemic stroke; HS, hemorrhage stroke.
Study characteristics
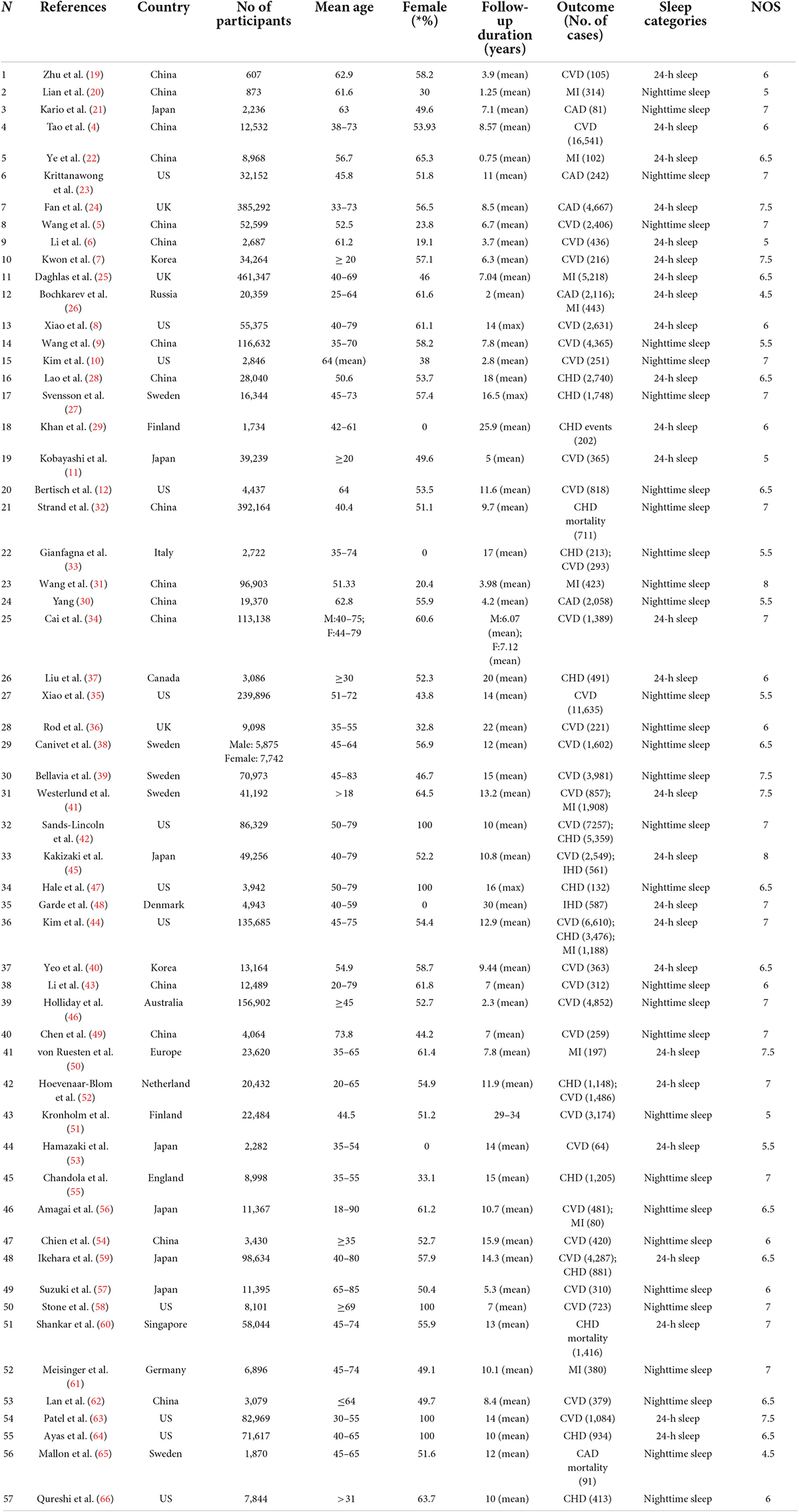
The detailed characteristics of cardiovascular disease studies are summarized in Table 1. All studies are cohort studies with populations from Asian Pacific (15 in China, 7 in Japan, 2 in South Korea, 1 in Singapore, and 1 in Australia), Europe (5 in Sweden, 4 in the UK, 2 in Finland, 1 in Denmark, 1 in Germany, 1 in Italy, 1 in the Netherlands, 1 in Russia and 1 in Europe), and North America (13 in US and 1 in Canada). The mean age ranges from 51 to 77 years old and the mean follow-up duration varied extensively from 0.75 to 34 years. Table 2 shows the detailed characteristics of cerebrovascular disease studies. All studies are cohort studies with populations from Asia (7 in China, 6 in Japan, and 2 in Singapore), Europe (2 in Sweden, 2 in Europe, 1 in Germany, and 1 in the UK), and North America (6 in the US). The mean age is varied from 45.7 to 64.5 years and the mean follow-up is varied from 0.75 to 16 years. The average study quality is moderate (median score = 6.5).
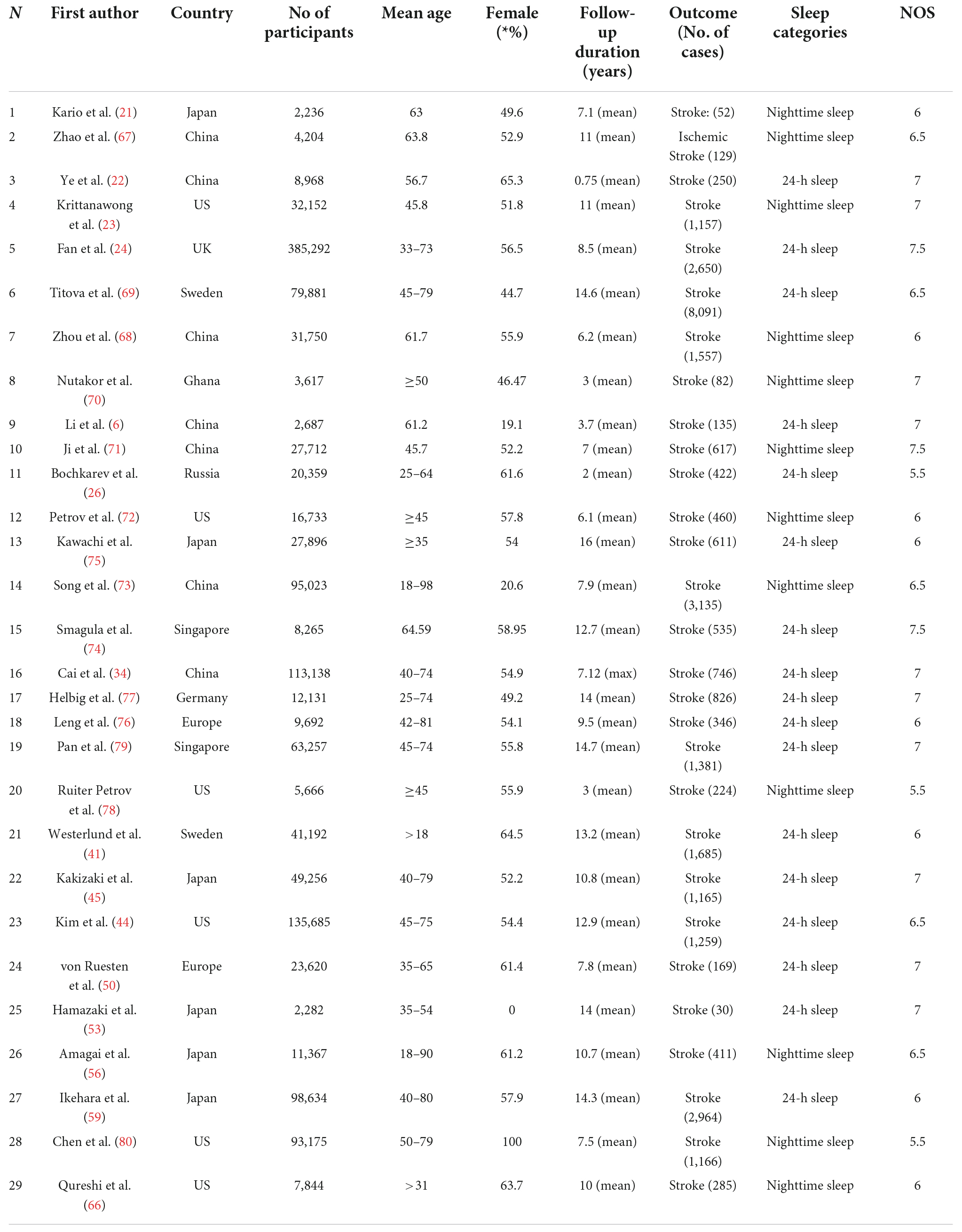
Table 2. Characteristics of 29 studies about cerebrovascular diseases included in the meta-analysis.
Sleep duration and risk of cardiovascular disease
Overall, 57 articles with 3.2 million participants about CVD were included in our meta-analysis (4–12, 19–66). A U-shaped relationship was found between CVD and the nighttime sleep duration category (Pnon–linearity < 0.0001; Figure 2A). Specifically, we found the nighttime sleep duration associated with lower risk was roughly situated between 4.3 and 10.3 h/night (Figure 2A) with the lowest risk corresponding to roughly 7.5 h/night. As for daily sleep duration, findings were similar to what was described above: the optimal sleep duration was roughly 7.5 h per day. (pnon–linearity < 0.0001; Figure 2B).
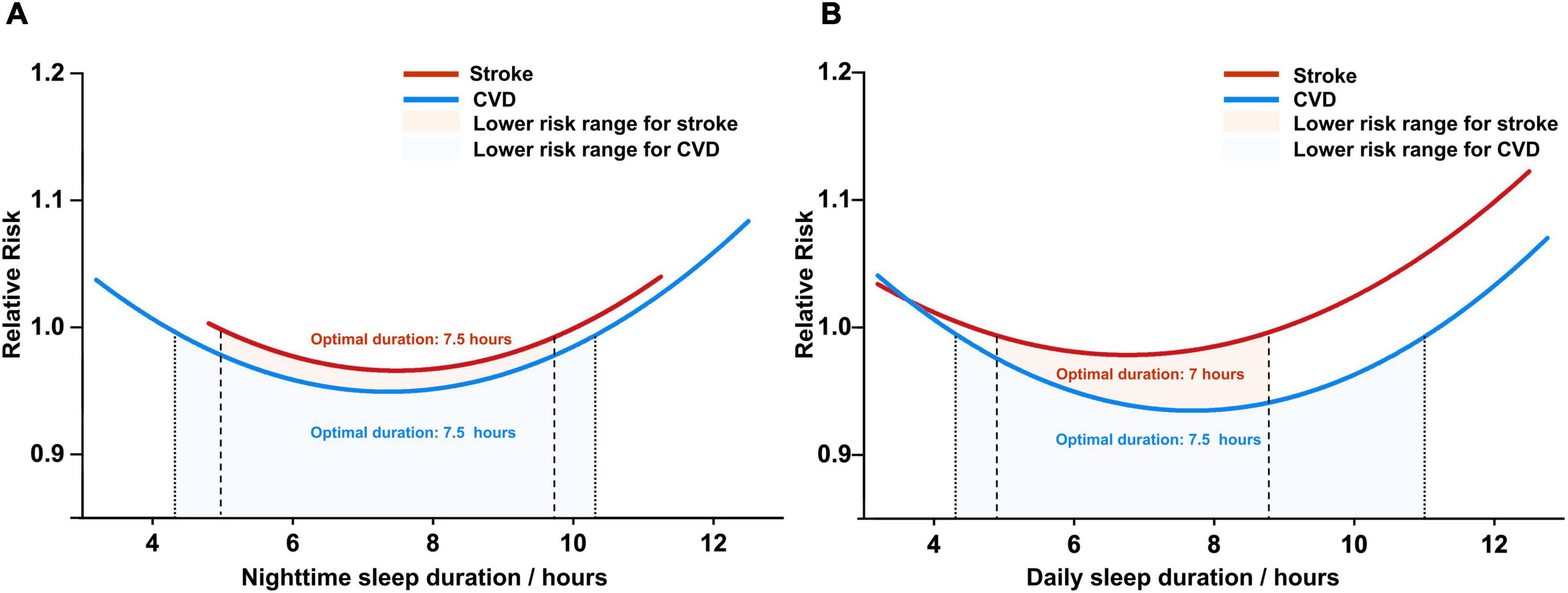
Figure 2. The dose-response analysis of cardio-cerebrovascular disease and sleep duration, (A) for nighttime sleep duration and (B) for daily sleep duration. CVD, cardiovascular disease.
In total, 24 articles were included in our study of CHD and sleep duration, and 11 articles were included in MI. A U-shaped relationship was found between CHD and nighttime sleep duration (pnon–linearity = 0.0001; Supplementary Figure 2), with a lower risk of CHD at 4.5–10.8 h which the optimal duration at approximately 7 h/night. The non-linear relationship between nighttime duration and MI showed non-significant significance (p = 0.2268), probably due to the limited number of included studies. Similarly, the dose-response analyses revealed significant non-linear associations between sleep duration and risks of CHD (p < 0.0001 for the daily duration) or MI (p = 0.0001 for the daily duration). Specifically, as for the daily sleep duration, the optimal duration was found to be roughly 7.5 h for the lowest risk of CHD and 7 h for lower risk of MI (Supplementary Figure 2). The risk of CHD or MI would be significantly elevated when the daily sleep duration was over 11 h or less than 4 h (4.6–11 for CHD and 4–10.6 for MI). Subgroup analysis showed that the results were consistent with the above results after stratification by region (pnon–linearity < 0.0001 for Asian Pacific, Europe and North America), follow-up duration (pnon–linearity < 0.0001 for < 10 and ≥ 10 years), and gender (pnon–linearity < 0.0001 for male and female) (Supplementary Figures 4–6).
Sleep duration and risk of cerebrovascular disease
A total of twenty-nine studies related to cerebrovascular disease with 1.4 million participants were included in our study (6, 21–24, 26, 34, 41, 44, 45, 50, 53, 56, 59, 66–80). The dose-response analyses revealed significant U-shaped association between sleep duration and risk of cerebrovascular disease (pnon–linearity = 0.05 for nighttime and pnon–linearity < 0.0001 for the daily duration). Specifically, as for the nighttime sleep duration, the optimal duration was found to be roughly 7.5 h for the lowest risk of cerebrovascular disease (Figure 2A). The risk of cerebrovascular disease will be significantly elevated when the nighttime sleep duration is over 9.7 h or less than 5 h. Similarly, as for daily sleep duration, our study noted that the optimal sleep duration of cerebrovascular disease was roughly 7 h/day. Subgroup analysis showed that the results were consistent with the above results after stratification by region (pnon–linearity < 0.0001 for Asian Pacific, pnon–linearity = 0.0052 for Europe, and pnon–linearity = 0.0002 for North America), follow-up duration (pnon–linearity = 0.0077 for < 10 years and pnon–linearity < 0.0001 for ≥ 10 years) (Supplementary Figures 4, 5).
Sensitivity analysis and publication bias
Sensitivity analysis excluded low-quality studies in turn did not alter the combined RR. Egger regression tests for evidence of publication bias were discussed extensively, (p = 0.010 for short sleep duration and total cardiovascular disease; p = 0.040 for short sleep duration and stroke) and we found that potential publication bias existed, but there was no change in the pooled results after correction.
Discussion
Based on our understanding, this paper is the most extensive and largest study of the correlation between sleep duration and cardiovascular events (Supplementary Table 4). The optimal sleep duration (hours/night) was found to be linked to the lowest risk of cardiovascular disease. Additionally, its reminder feature evaluates oversleeping or sleep deprivation that could increase one’s risk. It is worth noting that estimating the relative risk only represents the study population (not in the analysis). Thus, it may significantly impact an individual.
As observed above, sleep duration was also linked to the increased risk of diseases beyond CCDs. From the standpoint of one’s overall health, it is vital to conduct further research on the protective nature of an optimal sleep duration range (4.7–8.9 h/day) in addressing CCDs against other diseases. Upon searching the keywords “dose-response,” “meta-analysis,” and “sleep duration” on the PubMed database, seven papers were found to delve into a dose-response connection with other diseases, such as metabolic syndrome, cognitive disorder, colorectal cancer, breast cancer, osteoporosis, all cancer types, and AD. For comparative purposes, 5–9.7 h/night was identified to still shield a person from all diseases, which was aligned with our research (Supplementary Figure 1).
Compared with the previously circulated meta-analyses (81–83), the advantages of this study are fourfold. First, a total of 27 new included studies have been added to achieve a significantly expanded sample size. Second, instead of summarizing risk estimates based only on extreme classifications (lowest and highest) and their comparisons, which could cause significant differences in the findings, dose-response meta-analysis should be the primary choice when performing a systematic review. Third, the two sleep categories were the daily and nighttime sleep durations. We analyzed the dose-response relationship between them and CCDs independently. Fourth, as detailed in Supplementary Table 1, more robust and enhanced NOS evaluation criteria were adopted.
In light of the sleep duration and adverse outcomes, a few mechanisms could influence their direct relationship. Several studies have demonstrated that a chronic stressor like short sleep duration could impact the biological activities of adipokines (adiponectin, ghrelin, and leptin) and the hormonal regulators of appetite. Consequently, it increases the risk of obesity, which has been proven to be one of the risk factors for CCDs. Bain et al.’s research exhibited the link of short sleep duration to impaired NO-mediated endothelium-dependent vasodilation (84), which increases CCD-related risks. Moreover, a robust predictor of CCDs is the inflammatory marker CRP, which, along with other pro-inflammatory markers (IL-17, –6, –1, and TNF-α), have been observed to rise after being sleep-deprived (85, 86). Regarding insomnia with short sleep duration, patients experience a significant weakening of their parasympathetic nerve activation and an increase in their sympathetic nerve imbalance (87). Lastly, habitually short sleep duration results in circadian rhythm disruption, affecting physiological functions like the diurnal blood pressure variation (88), which increases the risk of hypertension. These risk factors are collectively relevant to CCDs.
Furthermore, the following factors may be associated with the link mechanism of long-term sleep with the increased risk of CCDs. Pulse wave velocity (PWV) and cerebral small vascular disease have a close relationship (89). Nevertheless, long sleep duration serves as a fundamental determinant of the incidence of stroke resulting from the PWV increase among those with a higher risk of CCDs (90). The increased risk of cardiometabolic dysfunction is associated with both long and short sleep durations (91). Over time, having a long sleep duration leads to lower levels of physical activity, causing poor health and physical weakness (92).
There are four primary limitations to our paper. First, the correlation deduced from analyzing observational cohort studies does not imply causation. To address this, future research must utilize Mendelian randomization techniques to evaluate the role of sleep duration management in CCD prevention. Second, compared with the gold standard of polysomnography that accurately measures sleep duration, the self-reported data across all the studies may not qualify as an objective measurement. However, due to its high costs, the former method may be unfeasible in large-scale prospective cohort studies. Meanwhile, an existing paper validated the moderate correlation between the sleep duration that was self-reported and measured by a wrist monitor (r = 0.47). Third, participants in most studies may have modified their sleep patterns after one follow-up, which assessed their respective sleep duration. As a result, the continuous effect of sleep duration on the long-term risk of CCD may not be fully captured by a single exposure measurement. Fourth, given the small sample size, we were unable to quantify the link of nap duration to CCDs through the dose-response analysis. Ultimately, recent literature has exhibited that sleep duration and sleep onset timing are related to CCDs (93), providing a new focus for our follow-up research.
In summary, our study provides varying degrees of evidence, indicating that the adults sleeping 5–9.7 h per night can reduce the risk of both CCDs, with the lowest risk with 7.5 h per night of sleep duration. Future research needs to confirm the relationship with cardio-cerebrovascular diseases and examine the role of sleep management in improving the risk of CCDs.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
Y-MH: collection and analysis of the data, drafting and revision of the manuscript, and prepared all the figures. WXi: collection and analysis of the data and revision of the manuscript. Y-JG and J-HH: revision of the manuscript. WXu, C-CT, and LT: conceptualization and design of the study and revision of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (grants 81901121 and 82001136) and the Qilu Health Care Outstanding Young Talent Program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.907990/full#supplementary-material
References
1. Drieu A, Levard D, Vivien D, Rubio M. Anti-inflammatory treatments for stroke: from bench to bedside. Ther Adv Neurol Disord. (2018) 11:1756286418789854.
2. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
3. Gupta A, Taqueti VR, van de Hoef TP, Bajaj NS, Bravo PE, Murthy VL, et al. Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation. (2017) 136:2325–36. doi: 10.1161/CIRCULATIONAHA.117.029992
4. Tao F, Cao Z, Jiang Y, Fan N, Xu F, Yang H, et al. Associations of sleep duration and quality with incident cardiovascular disease, cancer, and mortality: a prospective cohort study of 407,500 UK biobank participants. Sleep Med. (2021) 81:401–9. doi: 10.1016/j.sleep.2021.03.015
5. Wang YH, Wang J, Chen SH, Li JQ, Lu QD, Vitiello MV, et al. Association of longitudinal patterns of habitual sleep duration with risk of cardiovascular events and all-cause mortality. JAMA Netw Open. (2020) 3:e205246. doi: 10.1001/jamanetworkopen.2020.5246
6. Li J, Zheng D, Loffler KA, Wang X, McEvoy RD, Woodman RJ, et al. Sleep duration and risk of cardiovascular events: The SAVE study. Int J Stroke. (2020) 15:858–65.
7. Kwon S, Lee H, Lee JT, Shin MJ, Choi S, Oh H. Sleep duration and mortality in Korean adults: a population-based prospective cohort study. BMC Public Health. (2020) 20:1623. doi: 10.1186/s12889-020-09720-3
8. Xiao Q, Blot WJ, Matthews CE. Weekday and weekend sleep duration and mortality among middle-to-older aged White and Black adults in a low-income southern US cohort. Sleep Health. (2019) 5:521–7. doi: 10.1016/j.sleh.2019.04.008
9. Wang C, Bangdiwala SI, Rangarajan S, Lear SA, AlHabib KF, Mohan V, et al. Association of estimated sleep duration and naps with mortality and cardiovascular events: a study of 116 632 people from 21 countries. Eur Heart J. (2019) 40:1620–9. doi: 10.1093/eurheartj/ehy695
10. Kim JH, Hayek SS, Ko YA, Liu C, Samman Tahhan A, Ali S, et al. sleep duration and mortality in patients with coronary artery disease. Am J Cardiol. (2019) 123:874–81.
11. Kobayashi D, Kuriyama N, Osugi Y, Arioka H, Takahashi O. Longitudinal relationships between cardiovascular events, risk factors, and time-dependent sleep duration. Cardiol J. (2018) 25:229–35. doi: 10.5603/CJ.a2017.0088
12. Bertisch SM, Pollock BD, Mittleman MA, Buysse DJ, Bazzano LA, Gottlieb DJ, et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: sleep heart health study. Sleep. (2018) 41:zsy047. doi: 10.1093/sleep/zsy047
13. Xu W, Tan CC, Zou JJ, Cao XP, Tan L. Sleep problems and risk of all-cause cognitive decline or dementia: an updated systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. (2020) 91:236–44.
14. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: University of Oxford (2000).
15. Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ. (2014) 348:f7450. doi: 10.1136/bmj.f7450
16. Hedges LV, Tipton E, Johnson MC. Robust variance estimation in meta-regression with dependent effect size estimates. Res Synth Methods. (2010) 1:39–65.
17. Xu C, Doi SAR. The robust error meta-regression method for dose-response meta-analysis. Int J Evid Based Healthc. (2018) 16:138–44.
18. Orsini N. From floated to conventional confidence intervals for the relative risks based on published dose-response data. Comput Methods Programs Biomed. (2010) 98:90–3. doi: 10.1016/j.cmpb.2009.11.005
19. Zhu CY, Hu HL, Tang GM, Sun JC, Zheng HX, Zhai CL, et al. Sleep quality, sleep duration, and the risk of adverse clinical outcomes in patients with myocardial infarction with non-obstructive coronary arteries. Front Cardiovasc Med. (2022) 9:834169. doi: 10.3389/fcvm.2022.834169
20. Lian X, Gu J, Wang S, Yan J, Chen X, Wang M, et al. Effects of sleep habits on acute myocardial infarction risk and severity of coronary artery disease in Chinese population. BMC Cardiovasc Disord. (2021) 21:481. doi: 10.1186/s12872-021-02251-8
21. Kario K, Hoshide S, Nagai M, Okawara Y, Kanegae H. Sleep and cardiovascular outcomes in relation to nocturnal hypertension: the J-HOP nocturnal blood pressure study. Hypertens Res. (2021) 44:1589–96. doi: 10.1038/s41440-021-00709-y
22. Ye Y, Zhang L, Wang A, Wang Y, Wang S, Ning G, et al. Association of sleep duration with stroke, myocardial infarction, and tumors in a Chinese population with metabolic syndrome: a retrospective study. Lipids Health Dis. (2020) 19:155. doi: 10.1186/s12944-020-01328-1
23. Krittanawong C, Kumar A, Wang Z, Jneid H, Baber U, Mehran R, et al. sleep duration and cardiovascular health in a representative community population (from NHANES, 2005 to 2016). Am J Cardiol. (2020) 127:149–55. doi: 10.1016/j.amjcard.2020.04.012
24. Fan M, Sun D, Zhou T, Heianza Y, Lv J, Li L, et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK biobank participants. Eur Heart J. (2020) 41:1182–9. doi: 10.1093/eurheartj/ehz849
25. Daghlas I, Dashti HS, Lane J, Aragam KG, Rutter MK, Saxena R, et al. Sleep Duration and Myocardial Infarction. J Am Coll Cardiol. (2019) 74:1304–14.
26. Bochkarev M, Korostovtseva L, Medvedeva E, Rotar O, Sviryaev Y, Zhernakova Y, et al. Sleep duration and cardiovascular risk: results of the large-scale epidemiology study ESSE-RF. Arterial Hypertens. (2019) 23:248–55.
27. Svensson AK, Svensson T, Kitlinski M, Almgren P, Engström G, Nilsson PM, et al. Incident diabetes mellitus may explain the association between sleep duration and incident coronary heart disease. Diabetologia. (2018) 61:331–41.
28. Lao XQ, Liu X, Deng HB, Chan TC, Ho KF, Wang F, et al. Sleep quality, sleep duration, and the risk of coronary heart disease: a prospective cohort study with 60,586 adults. J Clin Sleep Med. (2018) 14:109–17. doi: 10.5664/jcsm.6894
29. Khan H, Kella D, Kunutsor SK, Savonen K, Laukkanen JA. Sleep duration and risk of fatal coronary heart disease, sudden cardiac death, cancer death, and all-cause mortality. Am J Med. (2018) 131:1499–505.e2. doi: 10.1016/j.amjmed.2018.07.010
30. Yang L, Yang H, He M, Pan A, Li X, Min X, et al. Longer sleep duration and midday napping are associated with a higher risk of CHD incidence in middle-aged and older chinese: the dongfeng-tongji cohort study. Sleep. (2016) 39:645–52. doi: 10.5665/sleep.5544
31. Wang X, Liu X, Song Q, Wu S. Sleep duration and risk of myocardial infarction and all-cause death in a Chinese population: the Kailuan study. Sleep Med. (2016) 19:13–6. doi: 10.1016/j.sleep.2015.09.027
32. Strand LB, Tsai MK, Gunnell D, Janszky I, Wen CP, Chang S-S. Self-reported sleep duration and coronary heart disease mortality: a large cohort study of 400,000 Taiwanese adults. Int J Cardiol. (2016) 207:246–51. doi: 10.1016/j.ijcard.2016.01.044
33. Gianfagna F, Veronesi G, Bertù L, Cesana G, Grassi G, Stranges S, et al. Influence of sleep disturbances on age at onset and long-term incidence of major cardiovascular events: the MONICA-Brianza and PAMELA cohort studies. Sleep Med. (2016) 21:126–32. doi: 10.1016/j.sleep.2016.01.007
34. Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. (2015) 38:529–36. doi: 10.5665/sleep.4564
35. Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol. (2014) 180:997–1006. doi: 10.1093/aje/kwu222
36. Rod NH, Kumari M, Lange T, Kivimäki M, Shipley M, Ferrie J. The joint effect of sleep duration and disturbed sleep on cause-specific mortality: results from the Whitehall II cohort study. PLoS One. (2014) 9:e91965. doi: 10.1371/journal.pone.0091965
37. Liu J, Yuen J, Kang S. Sleep duration, C-reactive protein and risk of incident coronary heart disease–results from the Framingham Offspring Study. Nutr Metab Cardiovasc Dis. (2014) 24:600–5. doi: 10.1016/j.numecd.2013.12.012
38. Canivet C, Nilsson PM, Lindeberg SI, Karasek R, Östergren P-O. Insomnia increases risk for cardiovascular events in women and in men with low socioeconomic status: a longitudinal, register-based study. J Psychos Res. (2014) 76:292–9. doi: 10.1016/j.jpsychores.2014.02.001
39. Bellavia A, Åkerstedt T, Bottai M, Wolk A, Orsini N. Sleep duration and survival percentiles across categories of physical activity. Am J Epidemiol. (2014) 179:484–91. doi: 10.1093/aje/kwt280
40. Yeo Y, Ma SH, Park SK, Chang S-H, Shin H-R, Kang D, et al. A prospective cohort study on the relationship of sleep duration with all-cause and disease-specific mortality in the Korean Multi-center Cancer Cohort study. J Prevent Med Public Health. (2013) 46:271–81. doi: 10.3961/jpmph.2013.46.5.271
41. Westerlund A, Bellocco R, Sundström J, Adami HO, Åkerstedt T, Trolle Lagerros Y. Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur J Epidemiol. (2013) 28:463–73. doi: 10.1007/s10654-013-9802-2
42. Sands-Lincoln M, Loucks EB, Lu B, Carskadon MA, Sharkey K, Stefanick ML, et al. Sleep duration, insomnia, and coronary heart disease among postmenopausal women in the Women’s Health Initiative. J Womens Health. (2013) 22:477–86. doi: 10.1089/jwh.2012.3918
43. Li Y, Sato Y, Yamaguchi N. Potential biochemical pathways for the relationship between sleep duration and mortality. Sleep Med. (2013) 14:98–104.
44. Kim Y, Wilkens LR, Schembre SM, Henderson BE, Kolonel LN, Goodman MT. Insufficient and excessive amounts of sleep increase the risk of premature death from cardiovascular and other diseases: the Multiethnic Cohort Study. Prev Med. (2013) 57:377–85. doi: 10.1016/j.ypmed.2013.06.017
45. Kakizaki M, Kuriyama S, Nakaya N, Sone T, Nagai M, Sugawara Y, et al. Long sleep duration and cause-specific mortality according to physical function and self-rated health: the Ohsaki Cohort Study. J Sleep Res. (2013) 22:209–16. doi: 10.1111/j.1365-2869.2012.01053.x
46. Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PLoS One. (2013) 8:e82305. doi: 10.1371/journal.pone.0082305
47. Hale L, Parente V, Dowd JB, Sands M, Berger JS, Song Y, et al. Fibrinogen may mediate the association between long sleep duration and coronary heart disease. J Sleep Res. (2013) 22:305–14. doi: 10.1111/jsr.12020
48. Garde AH, Hansen ÅM, Holtermann A, Gyntelberg F, Suadicani P. Sleep duration and ischemic heart disease and all-cause mortality: prospective cohort study on effects of tranquilizers/hypnotics and perceived stress. Scand J Work Environ Health. (2013) 39:550–8. doi: 10.5271/sjweh.3372
49. Chen H-C, Su T-P, Chou P. A nine-year follow-up study of sleep patterns and mortality in community-dwelling older adults in Taiwan. Sleep. (2013) 36:1187–98. doi: 10.5665/sleep.2884
50. von Ruesten A, Weikert C, Fietze I, Boeing H. Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. PLoS One. (2012) 7:e30972. doi: 10.1371/journal.pone.0030972
51. Kronholm E, Laatikainen T, Peltonen M, Sippola R, Partonen T. Self-reported sleep duration, all-cause mortality, cardiovascular mortality and morbidity in Finland. Sleep Med. (2011) 12:215–21.
52. Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. (2011) 34:1487–92. doi: 10.5665/sleep.1382
53. Hamazaki Y, Morikawa Y, Nakamura K, Sakurai M, Miura K, Ishizaki M, et al. The effects of sleep duration on the incidence of cardiovascular events among middle-aged male workers in Japan. Scand J Work Environ Health. (2011) 37:411–7. doi: 10.5271/sjweh.3168
54. Chien KL, Chen PC, Hsu HC, Su TC, Sung FC, Chen MF, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. (2010) 33:177–84. doi: 10.1093/sleep/33.2.177
55. Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep. (2010) 33:739–44. doi: 10.1093/sleep/33.6.739
56. Amagai Y, Ishikawa S, Gotoh T, Kayaba K, Nakamura Y, Kajii E. Sleep duration and incidence of cardiovascular events in a Japanese population: the Jichi Medical School cohort study. J Epidemiol. (2010) 20:106–10. doi: 10.2188/jea.je20090053
57. Suzuki E, Yorifuji T, Ueshima K, Takao S, Sugiyama M, Ohta T, et al. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med. (2009) 49:135–41. doi: 10.1016/j.ypmed.2009.06.016
58. Stone KL, Ewing SK, Ancoli-Israel S, Ensrud KE, Redline S, Bauer DC, et al. Self-reported sleep and nap habits and risk of mortality in a large cohort of older women. J Am Geriatr Soc. (2009) 57:604–11. doi: 10.1111/j.1532-5415.2008.02171.x
59. Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. (2009) 32:295–301. doi: 10.1093/sleep/32.3.295
60. Shankar A, Koh WP, Yuan JM, Lee HP, Yu MC. Sleep duration and coronary heart disease mortality among Chinese adults in Singapore: a population-based cohort study. Am J Epidemiol. (2008) 168:1367–73. doi: 10.1093/aje/kwn281
61. Meisinger C, Heier M, Löwel H, Schneider A, Döring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. (2007) 30:1121–7. doi: 10.1093/sleep/30.9.1121
62. Lan T-Y, Lan T-H, Wen C-P, Lin Y-H, Chuang Y-L. Nighttime sleep. Chinese afternoon nap, and mortality in the elderly. Sleep. (2007) 30:1105–10. doi: 10.1093/sleep/30.9.1105
63. Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. (2004) 27:440–4.
64. Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. (2003) 163:205–9.
65. Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. (2002) 251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x
66. Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. (1997) 48:904–11. doi: 10.1212/wnl.48.4.904
67. Zhao B, Wu Y, Jin X, Yang L, Yang J, Ma X, et al. Objectively measured sleep characteristics and incidence of ischemic stroke: the sleep heart health study. Nat Sci Sleep. (2021) 13:1485–94.
68. Zhou L, Yu K, Yang L, Wang H, Xiao Y, Qiu G, et al. Sleep duration, midday napping, and sleep quality and incident stroke: the dongfeng-tongji cohort. Neurology. (2020) 94:e345–56. doi: 10.1212/WNL.0000000000008739
69. Titova OE, Michaëlsson K, Larsson SC. Sleep duration and stroke: prospective cohort study and mendelian randomization analysis. Stroke. (2020) 51:3279–85.
70. Nutakor JA, Dai B, Gavu AK, Antwi OA. Relationship between chronic diseases and sleep duration among older adults in Ghana. Qual Life Res. (2020) 29:2101–10.
71. Ji A, Lou H, Lou P, Xu C, Zhang P, Qiao C, et al. Interactive effect of sleep duration and sleep quality on risk of stroke: an 8-year follow-up study in China. Sci Rep. (2020) 10:8690. doi: 10.1038/s41598-020-65611-y
72. Petrov ME, Howard G, Grandner MA, Kleindorfer D, Molano JR, Howard VJ. Sleep duration and risk of incident stroke by age, sex, and race: The REGARDS study. Neurology. (2018) 91:e1702–9. doi: 10.1212/WNL.0000000000006424
73. Song Q, Liu X, Zhou W, Wang L, Zheng X, Wang X, et al. Long sleep duration and risk of ischemic stroke and hemorrhagic stroke: the kailuan prospective study. Sci Rep. (2016) 6:33664. doi: 10.1038/srep33664
74. Smagula SF, Koh WP, Wang R, Yuan JM. Chronic disease and lifestyle factors associated with change in sleep duration among older adults in the Singapore Chinese Health Study. J Sleep Res. (2016) 25:57–61. doi: 10.1111/jsr.12342
75. Kawachi T, Wada K, Nakamura K, Tsuji M, Tamura T, Konishi K, et al. Sleep duration and the risk of mortality from stroke in japan: the takayama cohort study. J Epidemiol. (2016) 26:123–30. doi: 10.2188/jea.JE20140272
76. Leng Y, Cappuccio FP, Wainwright NW, Surtees PG, Luben R, Brayne C, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. (2015) 84:1072–9.
77. Helbig AK, Stöckl D, Heier M, Ladwig KH, Meisinger C. Symptoms of insomnia and sleep duration and their association with incident strokes: findings from the population-based MONICA/KORA augsburg cohort study. PLoS One. (2015) 10:e0134480. doi: 10.1371/journal.pone.0134480
78. Ruiter Petrov ME, Letter AJ, Howard VJ, Kleindorfer D. Self-reported sleep duration in relation to incident stroke symptoms: nuances by body mass and race from the REGARDS study. J Stroke Cerebrovasc Dis. (2014) 23:e123–32. doi: 10.1016/j.jstrokecerebrovasdis.2013.09.009
79. Pan A, De Silva DA, Yuan JM, Koh WP. Sleep duration and risk of stroke mortality among Chinese adults: Singapore Chinese health study. Stroke. (2014) 45:1620–5.
80. Chen JC, Brunner RL, Ren H, Wassertheil-Smoller S, Larson JC, Levine DW, et al. Sleep duration and risk of ischemic stroke in postmenopausal women. Stroke. (2008) 39:3185–92.
81. Wang H, Sun J, Sun M, Liu N, Wang M. Relationship of sleep duration with the risk of stroke incidence and stroke mortality: an updated systematic review and dose-response meta-analysis of prospective cohort studies. Sleep Med. (2022) 90:267–78. doi: 10.1016/j.sleep.2021.11.001
82. Yin J, Jin X, Shan Z, Li S, Huang H, Li P, et al. Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc. (2017) 6:e005947. doi: 10.1161/JAHA.117.005947
83. Li W, Wang D, Cao S, Yin X, Gong Y, Gan Y, et al. Sleep duration and risk of stroke events and stroke mortality: A systematic review and meta-analysis of prospective cohort studies. Int J Cardiol. (2016) 223:870–6.
84. Bain AR, Weil BR, Diehl KJ, Greiner JJ, Stauffer BL, DeSouza CA. Insufficient sleep is associated with impaired nitric oxide-mediated endothelium-dependent vasodilation. Atherosclerosis. (2017) 265:41–6.
85. Grandner MA, Sands-Lincoln MR, Pak VM, Garland SN. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. (2013) 5:93–107.
86. Grandner MA, Jackson N, Gerstner JR, Knutson KL. Dietary nutrients associated with short and long sleep duration. data from a nationally representative sample. Appetite. (2013) 64:71–80. doi: 10.1016/j.appet.2013.01.004
87. Jarrin DC, Ivers H, Lamy M, Chen IY, Harvey AG, Morin CM. Cardiovascular autonomic dysfunction in insomnia patients with objective short sleep duration. J Sleep Res. (2018) 27:e12663. doi: 10.1111/jsr.12663
88. Gangwisch JE. A review of evidence for the link between sleep duration and hypertension. Am J Hypertens. (2014) 27:1235–42.
89. Miwa K, Tanaka M, Okazaki S, Yagita Y, Sakaguchi M, Mochizuki H, et al. Multiple or mixed cerebral microbleeds and dementia in patients with vascular risk factors. Neurology. (2014) 83:646–53.
90. Niijima S, Nagai M, Hoshide S, Takahashi M, Shimpo M, Kario K. Long sleep duration: a nonconventional indicator of arterial stiffness in Japanese at high risk of cardiovascular disease: the J-HOP study. J Am Soc Hypertens. (2016) 10:429–37. doi: 10.1016/j.jash.2016.02.010
91. Tobaldini E, Fiorelli EM, Solbiati M, Costantino G, Nobili L, Montano N. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat Rev Cardiol. (2019) 16:213–24.
92. Nakakubo S, Makizako H, Doi T, Tsutsumimoto K, Hotta R, Lee S, et al. Long and short sleep duration and physical frailty in community-dwelling older adults. J Nutr Health Aging. (2018) 22:1066–71.
Keywords: sleep duration, cardiovascular disease, cerebrovascular disease, meta-analysis, dose-response
Citation: Huang Y-M, Xia W, Ge Y-J, Hou J-H, Tan L, Xu W and Tan C-C (2022) Sleep duration and risk of cardio-cerebrovascular disease: A dose-response meta-analysis of cohort studies comprising 3.8 million participants. Front. Cardiovasc. Med. 9:907990. doi: 10.3389/fcvm.2022.907990
Received: 30 March 2022; Accepted: 09 September 2022;
Published: 27 September 2022.
Edited by:
Benjamin D. Pollock, Mayo Clinic Florida, United StatesReviewed by:
Karl-Heinz Ladwig, Technical University of Munich, GermanyHao Sun, The First Affiliated Hospital of China Medical University, China
Copyright © 2022 Huang, Xia, Ge, Hou, Tan, Xu and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lan Tan, ZHIudGFubGFuQDE2My5jb20=; Wei Xu, ZHJfeHV3ZWlAcWR1LmVkdS5jbg==; Chen-Chen Tan, dGFuY2hlbmNoZW4xMjg1QDE2My5jb20=
 Yi-Ming Huang
Yi-Ming Huang Wei Xia2
Wei Xia2 Lan Tan
Lan Tan Chen-Chen Tan
Chen-Chen Tan