
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 10 November 2022
Sec. Atherosclerosis and Vascular Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.904685
 Cuijuan Yun1,2†
Cuijuan Yun1,2† Qian Xin2†
Qian Xin2† Sijin Zhang1,2
Sijin Zhang1,2 Shuohua Chen3
Shuohua Chen3 Jianli Wang3
Jianli Wang3 Chi Wang2
Chi Wang2 Miao Wang1
Miao Wang1 Maoxiang Zhao2
Maoxiang Zhao2 Yizhen Sun2
Yizhen Sun2 Ziwei Hou1,2
Ziwei Hou1,2 Shouling Wu3*
Shouling Wu3* Hao Xue2*
Hao Xue2*Objectives: Previous studies have confirmed the relations between inter-arm systolic blood pressure difference (IASBPD) and carotid artery plaque with the risk of cardiovascular diseases (CVD). But it is unclear whether the combined effect of IASBPD and carotid artery plaque further increases the risk of CVD and all-cause mortality.
Materials and methods: We enrolled 4,970 participants (≥40 years old) in the prospective Kailuan study. All participants underwent dual-arm blood pressure and carotid artery ultrasounds. IASBPD was the absolute value of the difference between dual-arm blood pressure. All the participants were divided into four groups according to their IASBPD levels and the presence or absence of carotid artery plaque and Cox proportional hazards models were used to calculate the hazard ratios (HRs) and 95% confidence interval (CI) for incident CVD and all-cause mortality.
Results: During a median follow-up of 7 years, 179 CVD events and 266 deaths occurred. Multivariable Cox Regression showed that participants with IASBPD ≥ 10 mmHg and plaque had a significantly higher incidence of CVD, cerebral infarction (CI), and myocardial infarction (10, 7.27, and 1.36%, respectively). After adjusting for covariates, the IASBPD ≥ 10 mmHg and carotid plaque group significantly increased risks for CVD (HR 2.38; 95% CI, 1.40∼4.05), CI (HR, 2.47; 95% CI, 1.31∼4.67), and all-cause mortality (HR, 2.08; 95% CI, 1.20∼3.59).
Conclusion: Our study indicated that the combination of IASBPD and carotid artery plaque was associated with incident CVD and all-cause mortality.
Cardiovascular disease (CVD) is the leading cause of death in China and has become an important public health problem. Atherosclerosis is the main cause of coronary heart disease, cerebral infarction (CI), and peripheral vascular disease (1), and is also the pathological basis of cardiovascular and cerebrovascular events development. People with multiple vascular atherosclerosis had a significantly increased risk of CVD compared with those with single atherosclerosis. Therefore, in order to improve the accuracy of CVD risk prediction, researchers tried to integrate different vascular markers into traditional risk prediction models.
Carotid artery plaque is a marker of degenerative changes and structural changes in atherosclerosis. The previous study shows that the presence of carotid plaque is associated with the risk of stroke, myocardial infarction (MI), and mortality (2, 3). Meta-analysis shows that carotid plaque is also a better predictor of future cardiovascular events than the intima-media thickness (4). In addition, a multi-ethnic study of atherosclerosis in the United States shows that carotid plaque is associated with future stroke or transient ischemic attack (5). Inter-arm Systolic Blood Pressure Difference (IASBPD) means the systolic blood pressure difference between the two arms. The International Hypertension Guideline recommends checking blood pressure (BP) on both arms when measuring BP and recognizes the association of systolic interarm blood pressure differences with cardiovascular risk (6). Recent studies have found that IASBPD, especially 10 mmHg or more, is associated with subclavian stenosis, peripheral arterial disease, cerebrovascular disease, CVD, and all-cause mortality (7–10).
Previous studies have confirmed the relations between IASBPD and carotid artery plaque with the risk of CVD and all-cause mortality, respectively. However, the contribution of the combination of IASBPD and carotid artery plaque to increase the risk of CVD is not clear. Therefore, in order to address this issue, we prospectively investigate the association of the combination of IASBPD and carotid artery plaque with the risk of CVD and all-cause mortality in the Kailuan study.
The study was a community-based prospective cohort (11–13). As detailed elsewhere, from June 2006 to September 2007 (visit 1) and June 2008 to September 2009 (visit 2), the employer of Tangshan Kailuan Company sponsored two times of health examinations for all 101,510 employees (81,110 men and 20,400 women, aged: 18–98 years) (14). A total of 5,816 participants were selected as an observational cohort using a random stratified sampling method and the response rate was 99%. A total of 5,440 individuals met the inclusion criteria (≥40 years old; no history of stroke, transient ischemic attack, or MI; no serious physical disability) and participated in the 2010–2011 health examination (visit 3). Finally, 4,970 adults were included in the analysis after excluding the following subjects: (a) the absence of information about brachial BP or sonography examination (n = 312); (b) a history of atrial fibrillation (n = 11); (c) a history of peripheral vascular disease (n = 82); (d) a history of MI and stroke (n = 41); (e) extreme value (n = 24). Data for 4,970 employees (2,960 men and 2,010 women) aged 18–96 years (55.00 ± 11.72) were used for the present analysis (a flowchart of participant inclusion appears in Figure 1). The study (ChiCTR-TNC-11001489) was performed according to the guidelines of the 1964 Declaration of Helsinki, and was approved by the Ethics Committee of the Kailuan Medical Group, Kailuan Company. Written informed consent had been given by all participants.
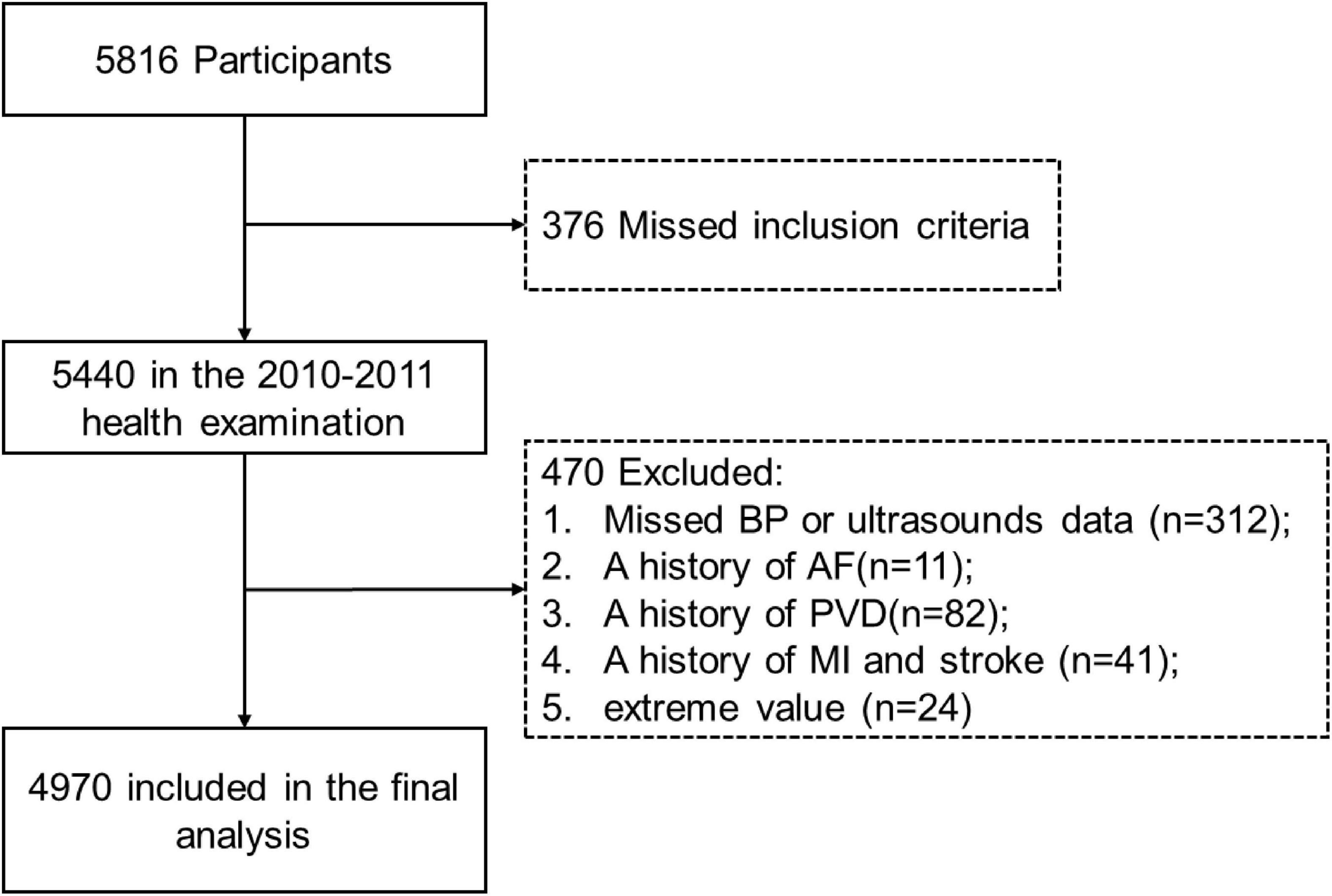
Figure 1. Selection of study population. BP, blood pressure; AF, atrial fibrillation; PVD, peripheral vascular disease; MI, myocardial infarction.
The medical and family history of all participants was obtained with a questionnaire including information about demographic data and occupational status, behavior (sleep, smoking, drinking alcohol, exercise, and diet habits), past medical history, and family history. Questionnaires were administered face-to-face by investigators. Height, weight, and waist circumference were measured and body mass index was calculated as kg/m2. The biochemical tests included total cholesterol, triglyceride, fasting blood glucose, high-density lipoprotein, and low-density lipoprotein.
We simultaneously measured the BP in four extremities, in the supine position after at least 5 min bed rest using an arteriosclerosis detection device (Model BP203RPE III, Omron, China), for each participant detected twice and averaged for the final results. IASBPD was defined as the absolute value of the right arm minus the left arm systolic BP.
Carotid artery ultrasonography used a diagnostic ultrasonic instrument (HD-15, PHILIPS, China), with a high-frequency probe and frequency of 5–12 mHz. The carotid artery and bifurcation, the origin of the internal carotid artery, and the external carotid artery were routinely scanned, and the intima and media thickness were measured to observe the existence of plaque, and the location and size of plaque were recorded.
Carotid artery plaque was defined as invading the arterial lumen by at least 0.5 mm or 50% of the surrounding intima–media thickness value or showing a thickness > 1.5 mm from the media-adventitia interface to the intima–lumen interface (15). The ultrasound images were jointly judged by two ultrasound doctors with more than 5 years of working experience according to the above criteria and were randomly rechecked by different ultrasound doctors to judge intima-media thickness and plaque again (retest reliability was 97%).
Cardiovascular disease events, including MI and CI, were ascertained by investigating the annual discharge form from local hospitals and death certificates of state vital statistics offices and by contacting participants annually for a history of CVD events, in the Kailuan study. MI was diagnosed based on the patient’s clinical symptoms, electrocardiograph changes, and dynamic myocardial enzyme changes in line with the World Health Organization’s Multinational Monitoring of Trends and Determinants in Cardiovascular Disease Criteria (16). For patients with CI, the diagnosis depends on the signs and symptoms and photocopied neuroimages (computed tomography or magnetic resonance imaging) and other diagnostic reports, in line with the World Health Organization criteria (17). According to the American Diabetes Association (18), the diagnostic criteria for Diabetes were defined as fasting blood glucose ≥ 7.0 mmol/L, random blood glucose ≥ 11.1 mmol/L, or taking hypoglycemic drugs. Hypertension was diagnosed as follows: systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg or the use of an antihypertensive medication following the JNC7 Guideline (19). All-cause death data were obtained from the Kailuan Social Security Information system every year.
Statistical analyses were performed using SAS version 9.4 (SAS Institute). According to IASBPD and carotid plaque, the participants’ objects were divided into four groups: IASBPD < 10 mmHg without carotid plaque; IASBPD ≥ 10 mmHg without carotid plaque; IASBPD < 10 mmHg with carotid plaque; and IASBPD ≥ 10 mmHg with carotid plaque. Continuous variables were described as means ± standard deviations and were compared by analysis of variance (ANOVA). Categorical variables were exhibited as frequencies and percentages and were compared using the chi-square test. Multivariate Cox proportional hazards regression was used to estimate the risks of cardiovascular events. The incidence of events was estimated using the Kaplan-Meier method. A P-value of less than 0.05 was considered statistically significant.
The baseline characteristics of the study population are shown in Table 1. In this study, 4,790 participants (mean age 55.00 ± 11.72 years, 2,960 males) were concluded. The proportion of smoking, drinking alcohol, hypertension, and Hyperlipidemia and the average value of blood pressure and fasting blood glucose were higher in the group of IASBPD ≥ 10mmHg with plaque, compared with other groups.
During the follow-up period of 4 years, 179 cases of CVD events (including 127 cases of CI and 42 cases of MI) and 266 deaths occurred. Compared with other groups, participants with IASBPD ≥ 10 mmHg with plaque had a significantly higher incidence of CVD, CI, and MI (10, 7.27, and 1.36%, respectively). The cumulative incidence of all-cause mortality significantly increased in the IASBPD < 10 mmHg in the carotid plaque group; however, the two groups with a plaque were higher than the groups without plaque for all-cause mortality (Table 2).
The IASBPD < 10 mmHg without carotid plaque group was defined as a control group. We conducted the univariate regression analysis of the relevant risk factors, refer to Appendix 1 for details. Multivariable Cox Regression evaluated the association of the combined effect of IASBPD and carotid artery plaque with CVD events and all-cause mortality (Table 3). After adjusting for confounding factors (including age, gender, body mass index, smoking, drinking alcohol, hypertension, diabetes, taking hypotensive drugs, total cholesterol, and high-density lipoprotein), we did not find an increased risk in the group of IASBPD ≥ 10 mmHg without carotid plaque compared with IASBPD < 10 mmHg without carotid plaque group. The IASBPD < 10 mmHg and carotid plaque group showed the risk of all-cause mortality was 1.73 times higher (95% CI, 1.20∼2.48). The IASBPD ≥ 10 mmHg and carotid plaque group significantly increased risks for CVD (HR 2.38; 95% CI, 1.40∼4.05), CI (HR, 2.47; 95% CI, 1.31∼4.67), and all-cause mortality (HR, 2.08; 95% CI, 1.20∼3.59), but the risk for MI was no significant difference.
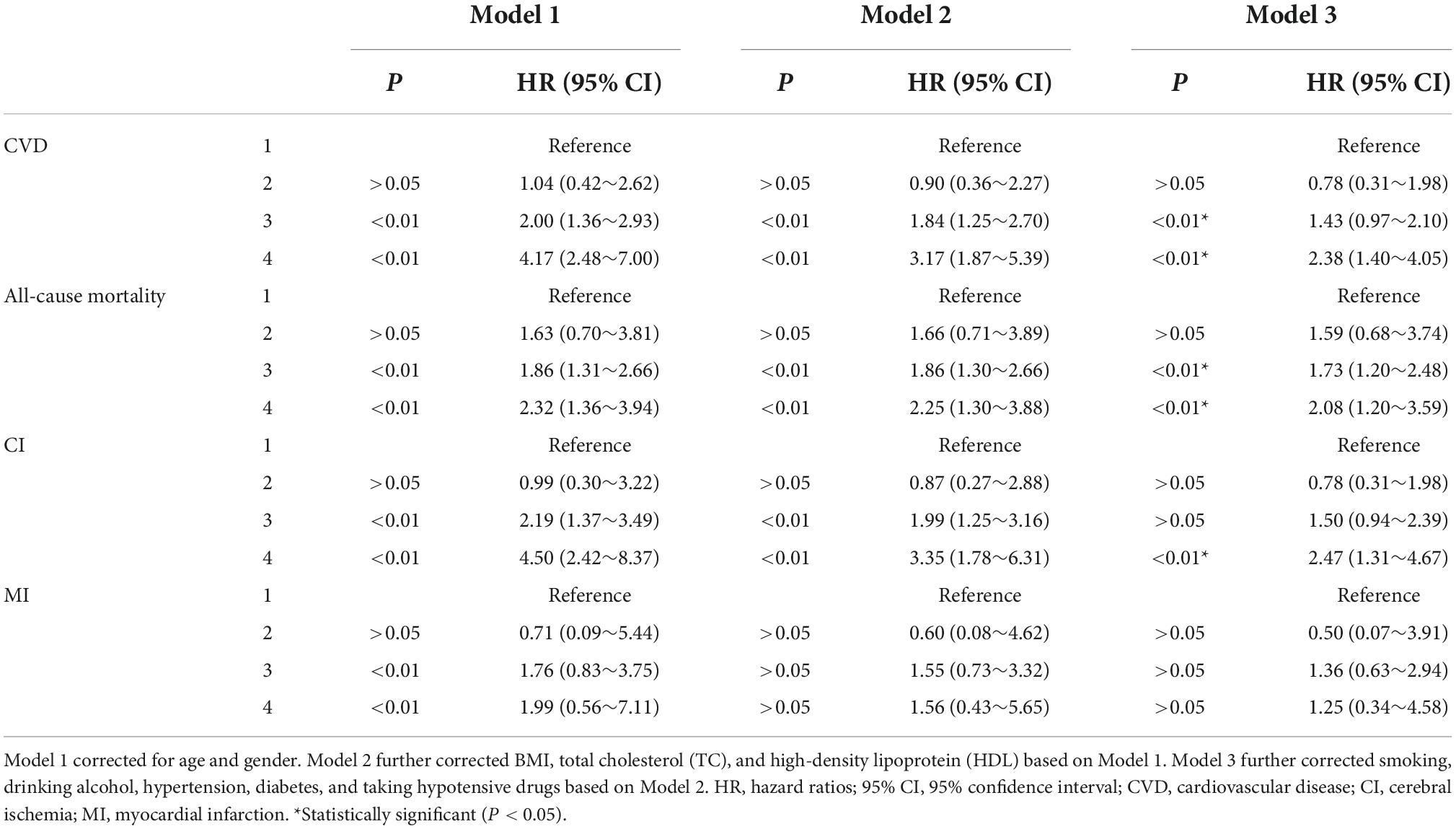
Table 3. Multivariable Cox regression analysis for cardiovascular disease events and all-cause mortality.
The present study confirmed that carotid artery plaque was an independent risk factor for all-cause mortality in the general population. The combination of IASBPD and carotid artery plaque improved the prognostic value.
Carotid plaque is considered a surrogate marker of subclinical atherosclerosis and is associated with the risk of stroke, MI, and mortality (2, 3, 20). In the present results, we found that carotid artery plaque significantly increased the risk of all-cause mortality by 1.73 times in the general Chinese population. This finding is consistent with the results reported in a prospective cohort study based on a community of 2,956 Chinese adults, which found that persons with carotid plaque had a higher risk for mortality (21). Besides, the Atherosclerosis Risk in Communities and the Cardiovascular Health Study have demonstrated that carotid plaque was associated with a 35% increased risk of sudden cardiac death (22). Atherosclerotic plaques not only increased the risk for all-cause mortality but also increased the risk for cardiac and cerebrovascular events. The Suita Study conducted in the general Japanese population indicated that the progression of incident carotid plaque increased the risk of incident CVD and stroke by 1.95 and 2.01 times, respectively (23). Another research found that compared with people without plaque, the total risk of stroke was 1.58 and the risk of cardiovascular disease was 1.71 (3). However, the presence of carotid plaque alone in our study was marginally significant in predicting cardiovascular risk, suggesting carotid plaque alone may be limited in predicting CVD in the Chinese general population, and the reason for this result may be related to a smaller sample size of this group with carotid plaque alone and our study included more males.
International hypertension guidelines recommend checking BP on both arms for the first time, choosing the arm with higher BP to measure subsequently for the detection and management of hypertension (6, 19). As the guidelines mentioned, IASBPD is a simple, accessible risk marker for cardiovascular events in patients with hypertension (6). On the other hand, IASBPD was concerned about patients with diabetes, chronic kidney disease, coronary heart disease, peripheral vascular disease, or other populations relevant to primary care (7–9, 24). Studies further demonstrated that the increase of IASBPD was still associated with the additional risk of CVD after adjustment for the Framingham risk scores, Atherosclerotic Cardiovascular Disease, or cardiovascular risk score scores (9, 25, 26). Therefore, IASBPD may be more efficacy for the prediction of CVD events and mortality than the existing cardiovascular risk scores. Consistent with guidelines for hypertension and recent studies (25, 27), a 10 mmHg difference in IASBPD was regarded as an upper limit of normal in our study. However, IASBPD ≥ 10 mmHg alone did not have a significant impact on CVD or all-cause mortality, it may be related to our small sample size. There were only 244 people in this group of IASBPD ≥ 10 mmHg without carotid plaque.
Our study found that carotid artery plaque and IASBPD synergistically increased the risks of CVD and all-cause mortality, especially the risk of cerebral ischemic stroke by 2.47 times. According to a recent cohort study of 117,407 people, IASBPD was associated with arterial stiffness, reflecting arteriosclerosis, but not with the presence of coronary artery calcium, reflecting atherosclerosis (28). Arteriosclerosis involves the structural changes of the arterial wall (the damage or degradation of the elastic fibers, or an increase in aggregating glycosaminoglycans or collagen fibers, or both), which affect the hemodynamic stress of the vascular wall leading to the increase of arterial stiffness finally (29). Atherosclerosis is a chronic process involving many factors, which starts from endothelial dysfunction, develops to intima thickening, and finally forms atherosclerotic plaque, characterized by lipid deposition in the inner walls of blood vessels and involving the inflammatory response (1). Therefore, arteriosclerosis and atherosclerosis are two pathological processes of vascular damage, which synergistically increase the risk of cardiovascular events. The combination of plaque and IASBPD may improve the identification of people at high risk for CVD. Based on the present, individuals with IASBPD ≥ 10 mmHg should be screened routinely for the presence of carotid artery plaque. In addition, some studies demonstrated that Lipid-lowering therapy helps stabilize, regress or even eliminate plaques (30, 31). Therefore, to reduce the burden of CVD and mortality, we suggest earlier early lipid-lowering therapy for the patients with IASBPD ≥ 10 mmHg and plaque together.
The strength of this study was the prospective large cohort for a long follow-up study. The combination of IASBPD and carotid plaque may become a simple, accessible, and non-invasive marker for screening individuals at high-cardiovascular risk, to guide patients to take intervention lifestyle or drug treatment as soon as possible. Besides, ascertainments of CVD and mortality were recorded based on the Municipal Social Insurance Institution and Hospital Discharge Register, which was updated annually during the follow-up period. As a result, we seldom lose the sample size to follow up.
However, some limitations still need to be considered. First, we only focused on whether the carotid artery plaque exists. Other features of the plaque including area, properties, and thickness were not measured, which may also be associated with CVD and mortality. The effect of carotid plaque characteristics on cardiovascular disease and mortality remains to be further studied. Second, we only measured IASBPD and plaque at baseline, but it represents the impact of vascular damage status on long-term prognosis. Third, our study included more men. Because, the study was based on the Kailuan study, from which the subjects were mostly male coal miner workers.
In conclusion, the combination of IASBPD and carotid artery plaque was associated with incident CVD and all-cause mortality. Therefore, early screening and intervention for IASBPD and carotid plaque may be a strategy to prevent CVD in the general population.
The data analyzed in this study is subject to the following licenses/restrictions: The datasets generated and/or analyzed during the current study are not publicly available, as per internal protocol, but are available from the corresponding author on reasonable request. Requests to access these datasets should be directed to HX.
The studies involving human participants were reviewed and approved by Ethics Committee of the Kailuan Medical Group, Kailuan Company. The patients/participants provided their written informed consent to participate in this study.
HX and SW designed the research. SW and CY conducted the research. CY and QX wrote the manuscript. SC and JW analyzed the data. SZ, CW, MW, MZ, YS, and ZH edited the manuscript. All authors read and approved the final manuscript.
This study was supported by the National Natural Science Foundation of China (No. 82070433).
We thank all the survey teams of the Kailuan Study Group for their contribution and the study participants who contributed their information.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
IASBPD, inter-arm systolic blood pressure difference; CVD, cardiovascular diseases; CI, cerebral infarction; MI, myocardial infarction; HRs, hazard ratios; CI, confidence interval; BP, blood pressure.
1. Meng Q, Pu L, Luo X, Wang B, Li F, Liu B. Regulatory roles of related long non-coding RNAS in the process of atherosclerosis. Front Physiol. (2020) 11:564604. doi: 10.3389/fphys.2020.564604
2. Mehta A, Rigdon J, Tattersall MC, German CA, Barringer TA III, Joshi PH, et al. Association of carotid artery plaque with cardiovascular events and incident coronary artery calcium in individuals with absent coronary calcification: the mesa. Circ Cardiovasc Imaging. (2021) 14:e011701. doi: 10.1161/circimaging.120.011701
3. Shimoda S, Kitamura A, Imano H, Cui R, Muraki I, Yamagishi K, et al. Associations of carotid intima-media thickness and plaque heterogeneity with the risks of stroke subtypes and coronary artery disease in the Japanese general population: the circulatory risk in communities study. J Am Heart Assoc. (2020) 9:e017020. doi: 10.1161/JAHA.120.017020
4. Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. (2012) 220:128–33. doi: 10.1016/j.atherosclerosis.2011.06.044
5. Gepner AD, Young R, Delaney JA, Tattersall MC, Blaha MJ, Post WS, et al. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Imaging. (2015) 8:e002262. doi: 10.1161/CIRCIMAGING.114.002262
6. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 Esc/Esh Guidelines for the management of arterial hypertension. Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
7. Yu Y, Liu L, Lo K, Tang S, Feng Y. Prevalence and associated factors of inter-arm blood pressure difference in Chinese community hypertensive population. Postgrad Med. (2021) 133:188–94. doi: 10.1080/00325481.2020.1826184
8. Heshmat-Ghahdarijani K, Ghasempour Dabaghi G, Rabiee Rad M, Bahri Najafi M. The Relation between inter arm blood pressure difference and presence of cardiovascular disease: a review of current findings. Curr Probl Cardiol. (2021) 47:101087. doi: 10.1016/j.cpcardiol.2021.101087
9. Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ. (2012) 344:e1327. doi: 10.1136/bmj.e1327
10. Zhou M, Gao Z, Chen F, Xu H, Dong X, Ma L. The inter-arm systolic blood pressure difference and risk of cardiovascular mortality: a meta-analysis of cohort studies. Clin Exp Hypertens. (2016) 38:317–24. doi: 10.3109/10641963.2015.1116542
11. Li W, Jin C, Vaidya A, Wu Y, Rexrode K, Zheng X, et al. Blood pressure trajectories and the risk of intracerebral hemorrhage and cerebral infarction: a prospective study. Hypertension. (2017) 70:508–14. doi: 10.1161/HYPERTENSIONAHA.117.09479
12. Zhang Q, Zhou Y, Gao X, Wang C, Zhang S, Wang A, et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic Stroke. Stroke. (2013) 44:2451–6. doi: 10.1161/STROKEAHA.113.678839
13. Wu S, Huang Z, Yang X, Zhou Y, Wang A, Chen L, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial City. Circ Cardiovasc Qual Outcomes. (2012) 5:487–93. doi: 10.1161/CIRCOUTCOMES.111.963694
14. Wu S, Li Y, Jin C, Yang P, Li D, Li H, et al. Intra-individual variability of high-sensitivity c-reactive protein in Chinese general population. Int J Cardiol. (2012) 157:75–9. doi: 10.1016/j.ijcard.2010.12.019
15. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the advisory board of the 3rd and 4th watching the risk symposium, 13th and 15th European stroke conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis. (2007) 23:75–80. doi: 10.1159/000097034
16. Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the world health organization Monica project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. (1994) 90:583–612. doi: 10.1161/01.cir.90.1.583
17. WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke–1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the who task force on stroke and other cerebrovascular disorders. Stroke. (1989) 20:1407–31. doi: 10.1161/01.str.20.10.1407
18. Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. (2003) 26:3160–7. doi: 10.2337/diacare.26.11.3160
19. Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 Acc/Aha/Aapa/Abc/Acpm/Ags/Apha/Ash/Aspc/Nma/Pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American college of cardiology/American Heart association task force on clinical practice guidelines. Hypertension. (2018) 71:1269–324. doi: 10.1161/hyp.0000000000000066
20. Rundek T, Arif H, Boden-Albala B, Elkind MS, Paik MC, Sacco RL. Carotid plaque, a subclinical precursor of vascular events: the Northern Manhattan study. Neurology. (2008) 70:1200–7. doi: 10.1212/01.wnl.0000303969.63165.34
21. Yang CW, Guo YC, Li CI, Liu CS, Lin CH, Liu CH, et al. Subclinical atherosclerosis markers of carotid intima-media thickness, carotid plaques, carotid stenosis, and mortality in community-dwelling adults. Int J Environ Res Public Health. (2020) 17:4745. doi: 10.3390/ijerph17134745
22. Suzuki T, Wang W, Wilsdon A, Butler KR, Adabag S, Griswold ME, et al. Carotid intima-media thickness and the risk of sudden cardiac death: the Aric study and the Chs. J Am Heart Assoc. (2020) 9:e016981. doi: 10.1161/JAHA.120.016981
23. Kokubo Y, Watanabe M, Higashiyama A, Nakao YM, Nakamura F, Miyamoto Y. Impact of Intima-media thickness progression in the common carotid arteries on the risk of incident cardiovascular disease in the Suita study. J Am Heart Assoc. (2018) 7:e007720. doi: 10.1161/JAHA.117.007720
24. Aboyans V, Kamineni A, Allison MA, McDermott MM, Crouse JR, Ni H, et al. The epidemiology of subclavian stenosis and its association with markers of subclinical atherosclerosis: the multi-ethnic study of atherosclerosis (Mesa). Atherosclerosis. (2010) 211:266–70. doi: 10.1016/j.atherosclerosis.2010.01.013
25. Ena J, Pérez-Martín S, Argente CR, Lozano T. Association between an elevated inter-arm systolic blood pressure difference, the ankle-brachial index, and mortality in patients with diabetes mellitus. Clin Investig Arterioscler. (2020) 32:94–100. doi: 10.1016/j.arteri.2019.11.003
26. Weinberg I, Gona P, O’Donnell CJ, Jaff MR, Murabito JM. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham heart study. Am J Med. (2014) 127:209–15. doi: 10.1016/j.amjmed.2013.10.027
27. Clark CE, Taylor RS, Butcher I, Stewart MC, Price J, Fowkes FG, et al. Inter-arm blood pressure difference and mortality: a cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract. (2016) 66:e297–308. doi: 10.3399/bjgp16X684949
28. Lee SJ, Kim H, Oh BK, Choi HI, Lee JY, Lee SH, et al. Association of inter-arm systolic blood pressure differences with arteriosclerosis and atherosclerosis: a cohort study of 117,407 people. Atherosclerosis. (2022) 342:19–24. doi: 10.1016/j.atherosclerosis.2021.12.003
29. Boutouyrie P, Chowienczyk P, Humphrey JD, Mitchell GF. Arterial stiffness and cardiovascular risk in hypertension. Circ Res. (2021) 128:864–86. doi: 10.1161/CIRCRESAHA.121.318061
30. Alidadi M, Montecucco F, Jamialahmadi T, Al-Rasadi K, Johnston TP, Sahebkar A, et al. Beneficial effect of statin therapy on arterial stiffness. Biomed Res Int. (2021) 2021:1–19. doi: 10.1155/2021/5548310
31. Almeida SO, Budoff M. Effect of statins on atherosclerotic plaque. Trends Cardiovasc Med. (2019) 29:451–5. doi: 10.1016/j.tcm.2019.01.001
Keywords: inter-arm systolic blood pressure difference, carotid artery plaque, cardiovascular disease, all-cause mortality, combined effect
Citation: Yun C, Xin Q, Zhang S, Chen S, Wang J, Wang C, Wang M, Zhao M, Sun Y, Hou Z, Wu S and Xue H (2022) Combined effect of inter-arm systolic blood pressure difference and carotid artery plaque on cardiovascular diseases and mortality: A prospective cohort study. Front. Cardiovasc. Med. 9:904685. doi: 10.3389/fcvm.2022.904685
Received: 25 March 2022; Accepted: 20 October 2022;
Published: 10 November 2022.
Edited by:
Hiroshi Iwata, Juntendo University, JapanReviewed by:
Osama Rifaie, Ain Shams University, EgyptCopyright © 2022 Yun, Xin, Zhang, Chen, Wang, Wang, Wang, Zhao, Sun, Hou, Wu and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Xue, eHVlaGFveGgzMDFAMTYzLmNvbQ==; orcid.org/0000-0001-5915-4811; Shouling Wu, ZHJ3dXNsQDE2My5jb20=; orcid.org/0000-0002-2921-7583
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.