- 1State Key Laboratory of Cardiovascular Disease, Division of Prevention and Community Health, National Center for Cardiovascular Disease, National Clinical Research Center of Cardiovascular Disease, Fuwai Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China
- 2School of Population Medicine and Public Health, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Background: The association between reproductive lifespan and risk of hypertension among postmenopausal women is unclear.
Methods: A total of 94,141 postmenopausal women with a mean age of 64.8 years from the China Hypertension Survey were enrolled at baseline from 2012 to 2015. A standardized questionnaire was used to collect relevant information by well-trained interviewers. Blood pressure and physical examination of the participants were performed by trained medical staff. Logistic regression was used to estimate the odds ratios for hypertension by years of reproductive lifespan.
Results: The average years of reproductive lifespan in Chinese women was 34.0 years. Women who were longer in reproductive lifespan were more likely to have older age at recruitment, higher body mass index, larger waist circumference, lower mean systolic blood pressure, and higher mean diastolic blood pressure (p < 0.05). After adjustments, odds ratios (95% confidence interval) for hypertension were 1.035 (0.988–1.085), 1.007 (0.966–1.048), 1.000 (reference), 0.932 (0.899–0.967), and 0.953 (0.909–0.997) for those with reproductive lifespan at ≤ 28, 29–31, 32–34 (reference), 35–37, and ≥ 38 years, respectively, with a significantly inverse association was seen in those with reproductive lifespan at 35–37 and ≥ 38 years. The overall risk of hypertension declined with the increase in reproductive lifespan, and the risk of hypertension was reduced by 1.1% for every 1-year increase in the reproductive lifespan (odds ratio, 0.989; 95% confidence interval, 0985–0.994) per year. The negative association between reproductive lifespan and hypertension was evident among age at recruitment groups, body mass index categories, and education levels, with the strongest association among women aged ≥ 70 years. Positive associations between reproductive lifespan and risk of hypertension were evident among women aged < 60 years, and this association was stronger among current alcohol drinkers.
Conclusion: Based on the large nationally representative sample, Chinese postmenopausal women with a shorter reproductive lifespan have a higher risk of hypertension.
Introduction
Hypertension is one of the most important and preventable risk factors for cardiovascular diseases, which has been recognized as a public health challenge worldwide (1–3). It is estimated that approximately 1.56 billion adults worldwide will be diagnosed with hypertension by 2025 (4). In China, the prevalence of hypertension is increasing from 13.6% in 1991 to 23.2% in 2012 (5, 6). Data from the China National Hypertension Survey Epidemiology Follow-up Study show a strong, linear, and significant association between SBP and DBP and risk for cardiovascular disease (CVD), coronary heart disease (CHD), and stroke, independent of other risk factors (7). Previous studies suggested that premenopausal women typically have lower blood pressure (BP) than men. However, the prevalence of hypertension is higher in postmenopausal women than that in men (8). Therefore, it is important to identify potential risk factors for the prevention of hypertension, particularly among postmenopausal women.
The age of menarche and menopause as the two endpoints of reproductive lifespan may have an implication for trajectory of hypertension later in life. However, the available evidence has remained unclear whether reproductive lifespan is an important risk factor for hypertension due to limited studies. Earlier studies showed inconsistent results on the effect of timing of menarche (9–12) and menopause (13–15) on hypertension risk with very few studies conducted overall. If such a link exists, then the duration of the reproductive lifespan from menarche to menopause might serve as an improved marker of hypertension risk in women. Given that hypertension is an important risk factor for CVD, clarifying the association between reproductive lifespan and the risk of hypertension in postmenopausal women could help identify subgroups of women at risk for hypertension and confirm those who should be targeted for early intervention, which is critical for preventing hypertension.
There is nothing of nationally representative large-sample studies to explore the relationship between reproductive lifespan and hypertension in Chinese women. The present study aimed to investigate the associations between reproductive lifespan and the risk of hypertension among postmenopausal women participating in the Chinese Hypertension Survey (CHS), a large, nationally representative sample study conducted in China.
Materials and methods
Study design and participants
All participants in this study were derived from the CHS, a nationally representative sample survey of the Chinese general population aged ≥ 15 years from all 31 provinces in the mainland conducted from October 2012 to December 2015. More details on CHS can be found in the previous publication (16). A stratified multistage random sampling method was used in the CHS. The first stage of sampling was to select four cities in urban areas and four counties in rural areas by using the probability proportional to size method within each province. Then, a simple random sampling method was used to select two districts or two townships in each city or county, and three communities or villages in each district or township. At the final stage of sampling, a certain number of participants from 14 sex/age groups (men and women aged 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, and ≥ 75 years) were selected from communities using lists compiled by the local government registries of households. A total of 487,353 participants from 262 urban resident cities and rural counties were enrolled, of which 253,531 (52.02%) were women. Of the total sample of 102,710 postmenopausal women, 94,141 participants were included in the analysis after exclusions of 8,569 women with missing or implausible information (Figure 1).
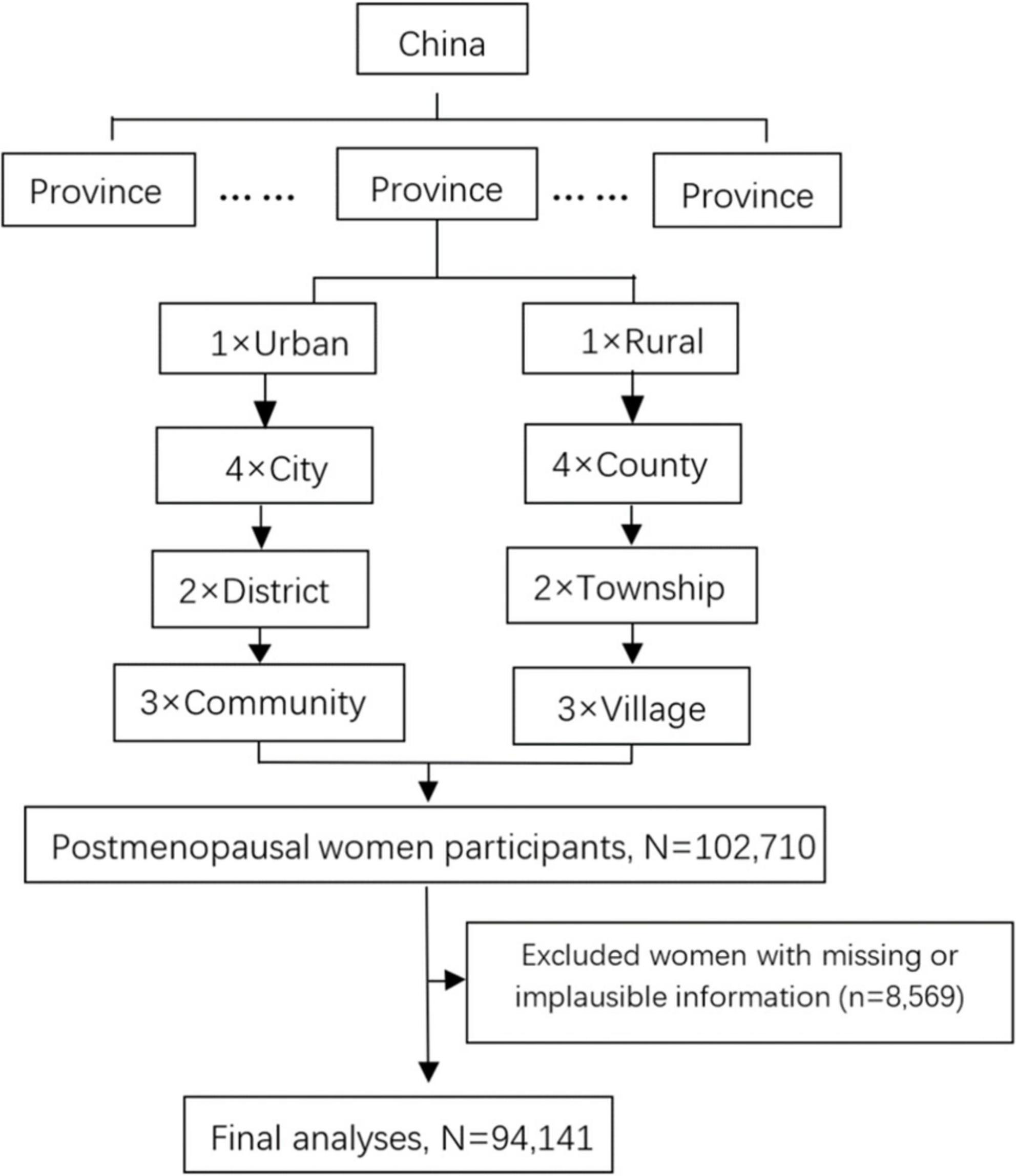
Figure 1. Chart of the subject inclusion and exclusion. PPS, probability proportional to size; SRS, simple random sampling.
Prior to recruitment, written informed consent was obtained from each participant. This study was approved by the Ethics Committee of Fuwai Hospital (Beijing, China).
Measurement and data collection
Blood pressure on the right upper arm was measured three times by trained medical staff after the subjects rested for at least 5 min, with an interval of at least 30 s between each measurement with an observer present, using an OMRON HBP-1300 Professional Portable Blood Pressure Monitor (OMRON, Kyoto, Japan). The average of the three measurements was used for the analysis.
All subjects were interviewed by well-trained interviewers using standardized questionnaires developed by Fuwai Hospital, which covered social-demographic characteristics, lifestyle factors, disease history, and reproductive factors. The physical examinations were conducted by trained physicians and nurses. Height was measured without shoes using a standard right-angle device (accurate to 0.1 cm). Waist circumference was measured using a fixed measuring tape and at the midpoint of the line between the crest of the ilium and the inferior margin of the 12th rib with participants wearing thin clothing (to the nearest 0.1 cm). Body weight without wearing heavy clothing was measured using an OMRON body fat and weight measurement device (V-body HBF-371, OMRON, Japan). Body mass index (BMI) was calculated as weight/height2 (kg/m2).
Definitions
The reproductive lifespan was defined as the interval between age at menarche and menopause. At baseline, each female subject was asked her age at the time of her first period, which was recorded as age at menarche. The menopausal status was defined as menstruation stopped for at least 12 months and no history of hysterectomy or oophorectomy, or current pregnancy or lactation, and the age at which menopause occurred was recorded at baseline. According to the Chinese guidelines for hypertension management, hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg, and/or diastolic blood pressure (DBP) ≥ 90 mmHg, and/or use of antihypertensive medication within 2 weeks.
Educational levels were divided into three groups: elementary or below, junior high school, and high school or above. Criteria for overweight and obesity were considered as BMI ranging from 24.0 to 27.9 kg/m2 and BMI ≥ 28.0 kg/m2, respectively. Current smoking was defined as someone who has smoked at least 20 packets of cigarettes in their lifetime and still smokes. Current alcohol drinking was defined as consuming alcoholic beverages at least once per week in the past month. A family history of hypertension refers to one in which parents, siblings, or children have hypertension.
Statistical analysis
Baseline characteristics of participants were presented as mean and standard deviation (SD) for normally distributed data or as a proportion for categorical data. Categorical variables were analyzed using the chi-square test, and continuous variables were analyzed by one-way analysis of variance (ANOVA). Logistic regression was used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for hypertension associated with reproductive lifespan (classified as ≤ 28, 29–31, 32–34, 35–37, and ≥ 38 years) with 32–34 years as the reference group. This study further investigated these associations by making additional adjustments for age at recruitment (continuous), ethnicity (Han or other ethnicities), region (urban or rural), education level (elementary or below, junior high school, high school or above), BMI (continuous), waist circumference (continuous), current smoking (yes or no), current alcohol drinking (yes or no), previously pregnant (yes or no), contraceptive use (yes or no), breastfeeding experience (continuous), stroke (yes or no), myocardial infarction (yes or no), and family history of hypertension (yes or no). We also examined the risk of hypertension in subgroups of women previously defined by age at recruitment, education level, and BMI. The threshold of statistical significance was set as p < 0.05. We used R 3.6.2 software to conduct our analyses.
Results
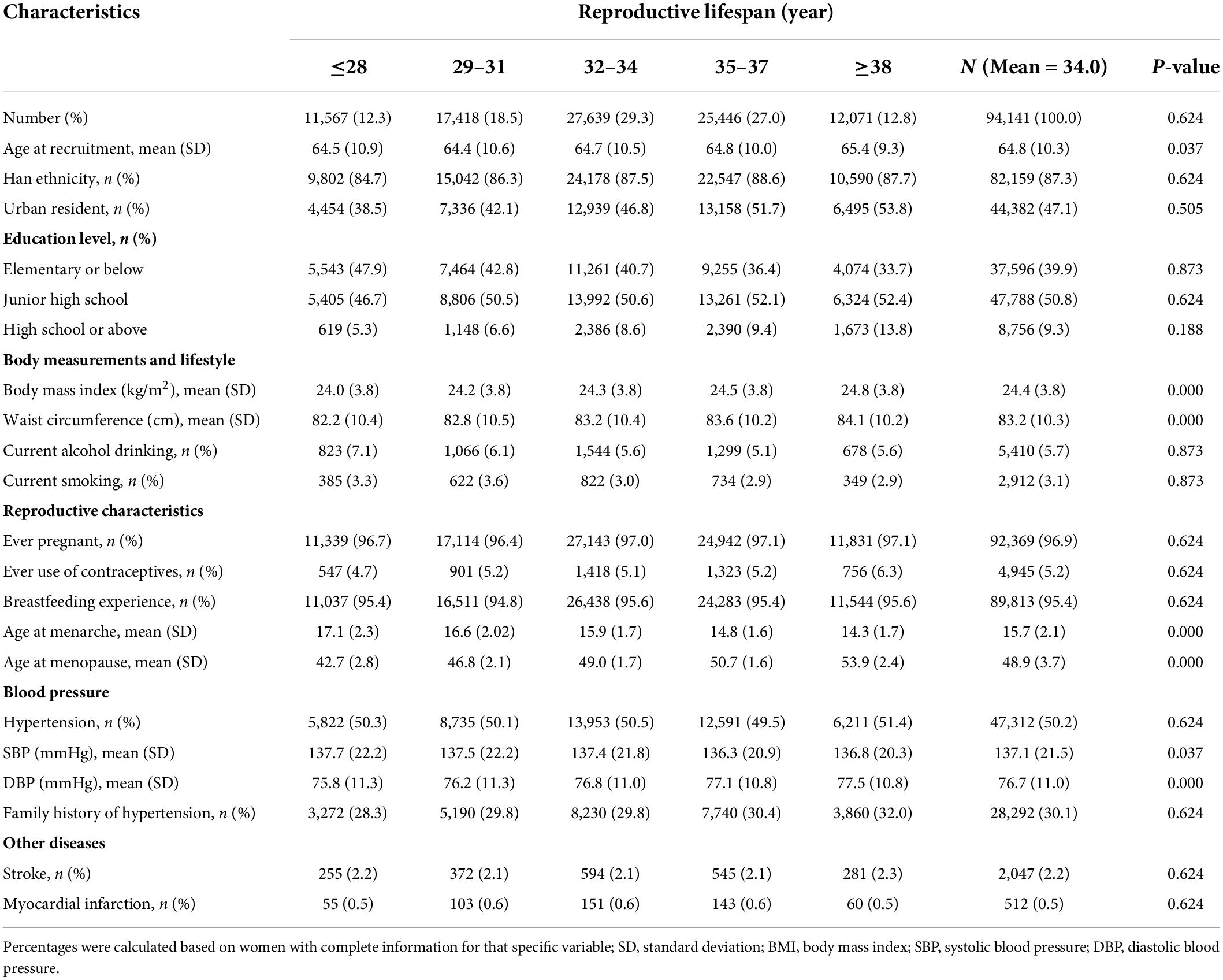
The characteristics of the study participants are listed in Table 1. The mean (SD) age of study participants at recruitment was 64.8 (10.3) years, and the mean age at menarche, age at menopause, and reproductive lifespan were 15.7 (2.1), 48.9 (3.7), and 34.0 (3.3) years, respectively. The mean (SD) BMI, SBP, and DBP were 24.4 (3.8) kg/m2, 137.1 (21.5) mmHg, and 76.7 (11.0) mmHg, respectively. The proportions of women with reproductive lifespan at ≤ 28, 29–31, 32–34, 35–37, and ≥ 38 years were 12.3, 18.5, 29.3, 27.0, and 12.8%, respectively. A minority of women had an education level at high school or above (9.3%) and were current smokers (3.1%), current alcohol drinkers (5.7%), ever pregnant (3.1%), and users of contraceptives (5.2%). Women who were longer in reproductive lifespan were more likely to have older age at recruitment, higher BMI, larger waist circumference, and lower mean SBP and higher mean DBP (p < 0.05). Most women had been pregnant (96.9%) and had breastfed (95.4%).
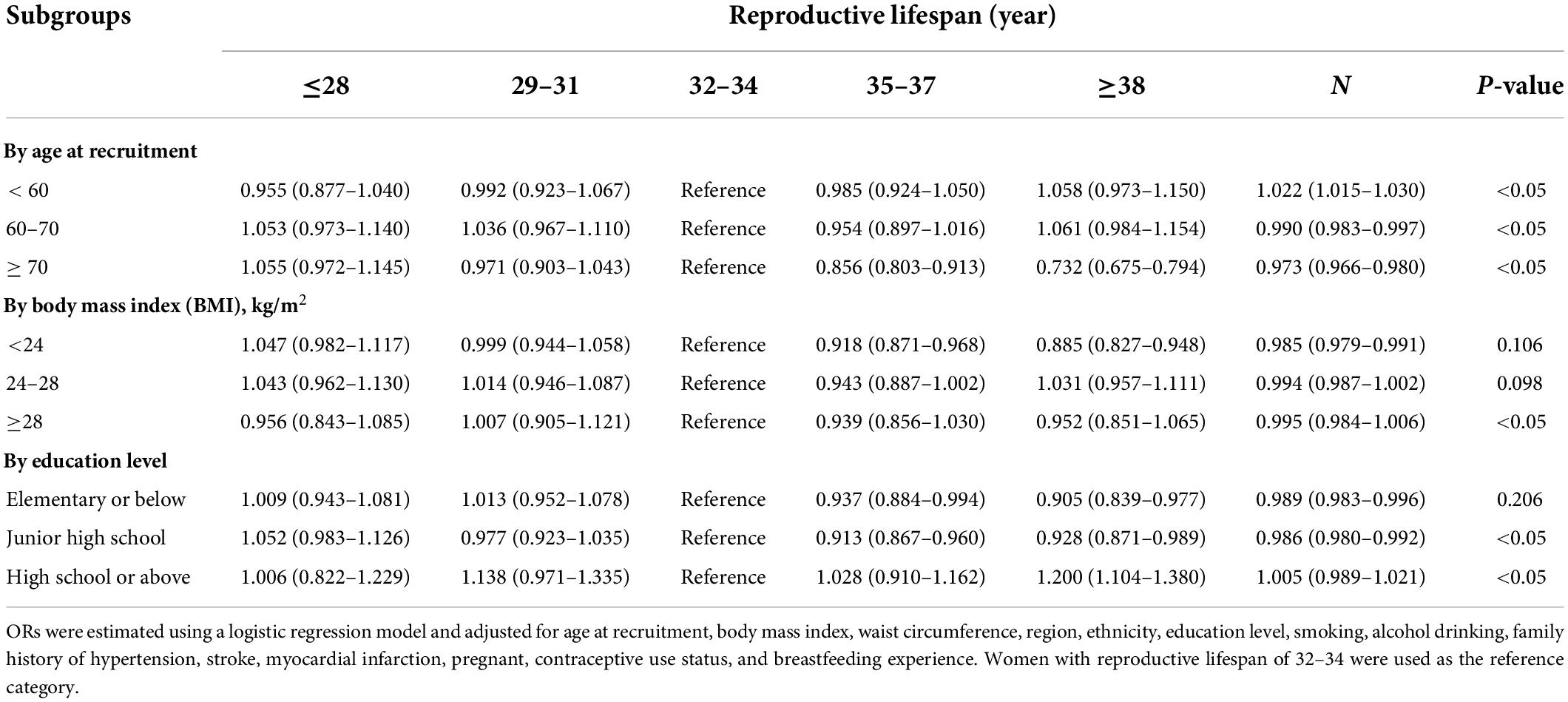
Figure 2 shows the adjusted ORs for hypertension by reproductive lifespan (≤28, 29–31, 32–34, 35–37, and ≥ 38 years). After adjustment for age at recruitment, ethnicity, region, education level, BMI, waist circumference, current smoking, current alcohol drinking, family history of hypertension, stroke, myocardial infarction, and reproductive factors, the ORs (95%CIs) were 1.035 (0.988–1.085), 1.007 (0.966–1.048), 1.000 (reference), 0.932 (0.899–0.967) and 0.953 (0.909–0.997) for those with reproductive lifespan at ≤ 28, 29–31, 32–34 (reference), 35–37, and ≥ 38 years, respectively. The significantly inverse association was seen in those with reproductive lifespan at 35–37 and ≥ 38 years. The overall risk of hypertension declined with the increase of reproductive lifespan. After adjustments, ORs (95%CI) of hypertension in subgroups of women defined by age at recruitment, BMI, and education level are shown in Table 2. Subgroup analyses were also performed based on age at recruitment, region, education level, smoking status, alcohol consumption status, BMI, menopausal status, use of contraceptives, and family history of hypertension (Figure 3). Reproductive lifespan was inversely associated with hypertension, with an adjusted OR of 0.989 (95%CI: 0985–0.994) per year. The risk of hypertension was reduced by 1.1% for every 1-year increase in reproductive lifespan. Negative associations between reproductive lifespan and risk of hypertension were evident among urban and rural women; women aged ≥ 70 and 60–70 years; women with BMI < 24kgm2; women with education level in junior high school and elementary or below groups; no current alcohol drinker, no current smoker, ever use of contraceptives, and no family history of hypertension. This association was strongest in women aged ≥ 70. Positive associations between reproductive lifespan and risk of hypertension were evident among women aged < 60 years and strongest among current alcohol drinkers.
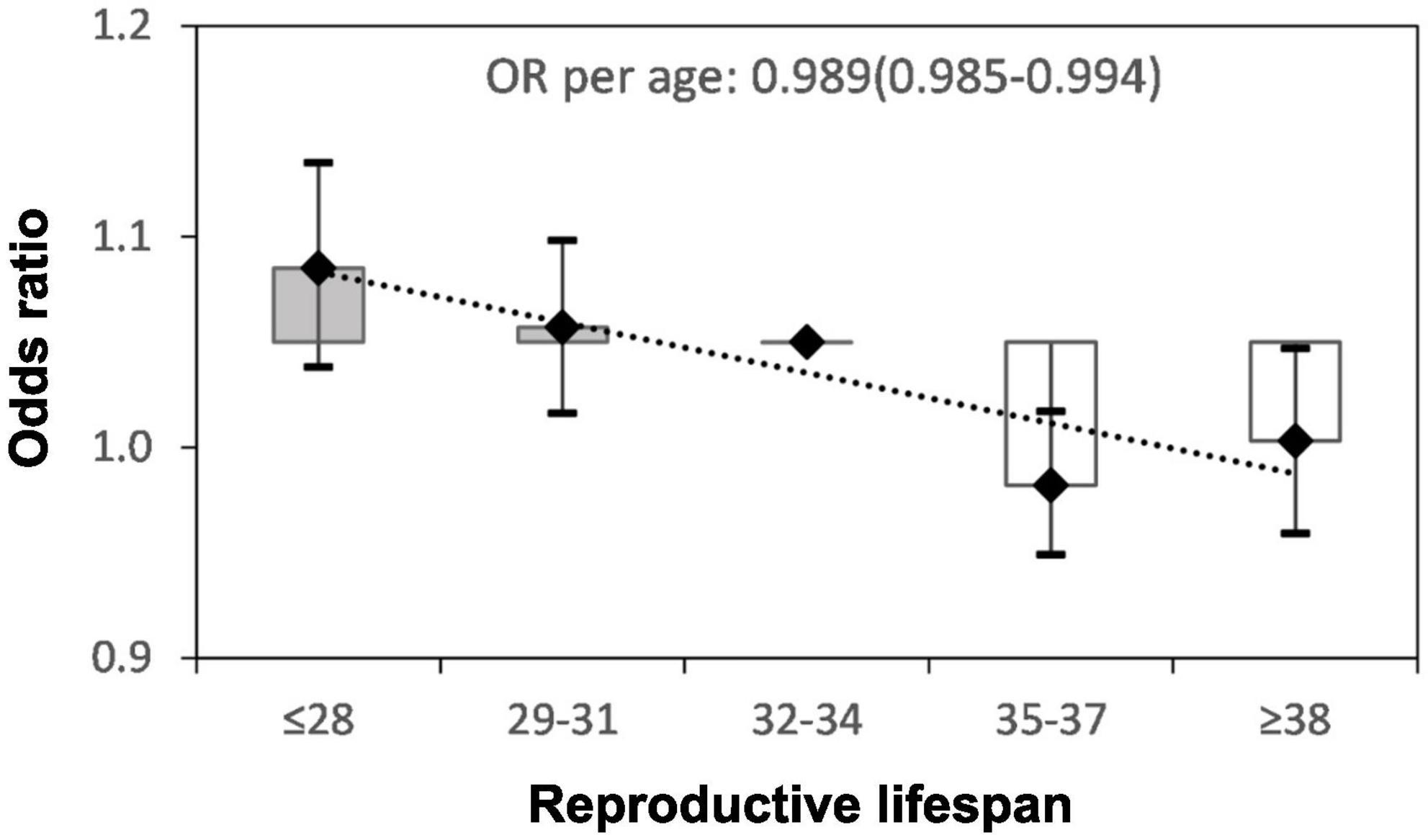
Figure 2. Adjusted odds ratio (OR) and 95% confidence interval (CI) for hypertension by the years of reproductive lifespan. Adjusted for age at recruitment, body mass index, waist circumference, region, ethnicity, education level, smoking, alcohol drinking, family history of hypertension, stroke, myocardial infarction, pregnant, contraceptive use status, and breastfeeding experience.
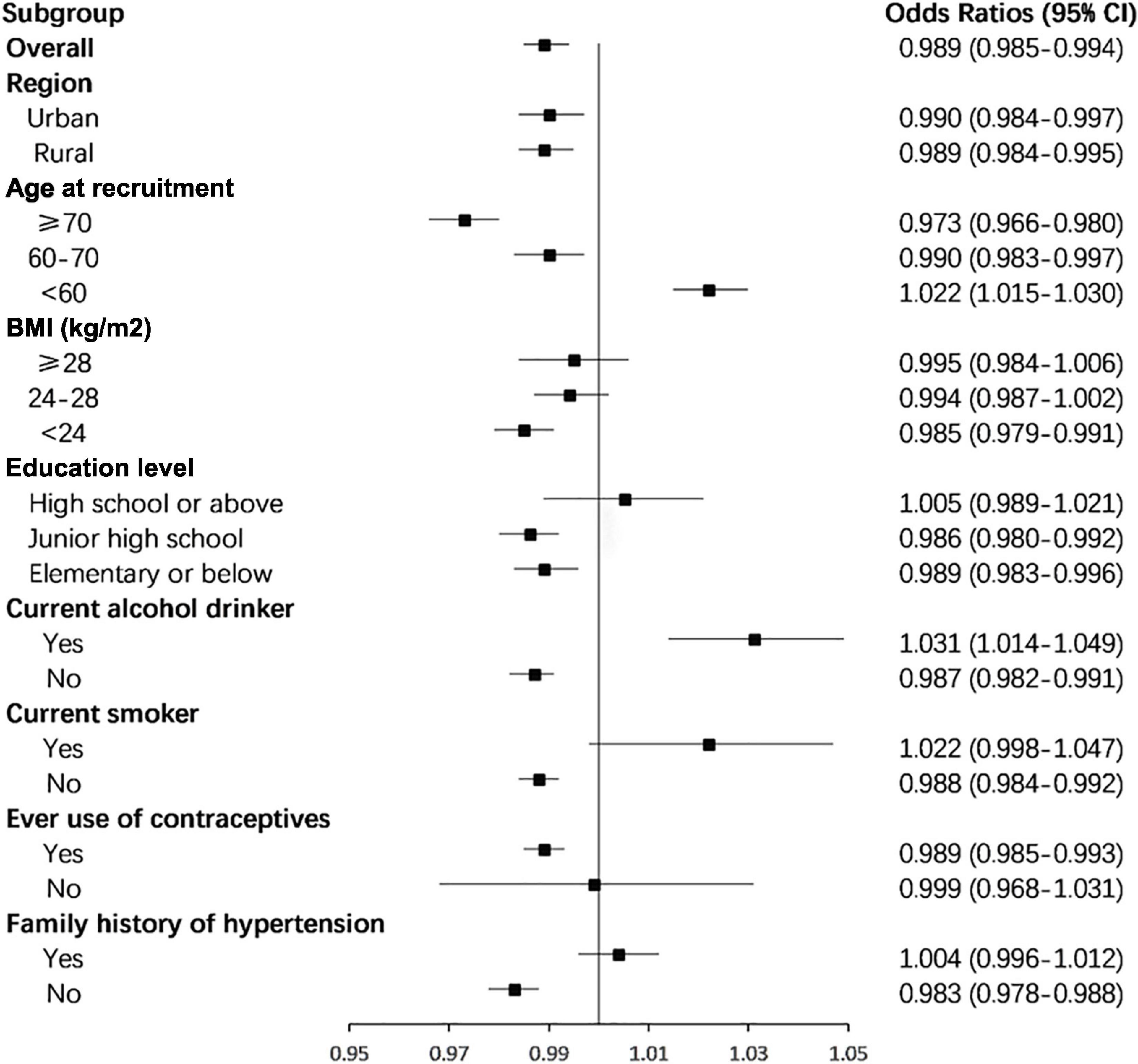
Figure 3. Subgroup analyses of the associations between total reproductive years and risk of hypertension according to possible influencing factors. Analyses were adjusted for age at recruitment, body mass index, waist circumference, region, ethnicity, education level, smoking, alcohol drinking, family history of hypertension, stroke, myocardial infarction, pregnant, contraceptive use status, and breastfeeding experience.
Discussion
Based on a nationally representative sample, we found that women with a reproductive lifespan of 35–37 and ≥ 38 years had decreased risk of hypertension. The longer the reproductive lifespan, the lower the risk of hypertension. The risk of hypertension was reduced by 1.1% for every 1-year increase in the reproductive lifespan. This association also appeared to be similar among subgroups. To our knowledge, this was the first comprehensive study to investigate the associations between reproductive lifespan and risk of hypertension in Chinese postmenopausal women. It is helpful to identify markers that are critical for preventing hypertension in women.
The interval between menarche and menopause defines a woman’s natural reproductive span. However, previous studies indicated both contradictory results about the effect of age at menarche and age at menopause on hypertension risk, and rare studies examined both factors during the reproductive lifespan. We found only one study conducted by Feng et al. that simultaneously examined the effects of age at menarche, reproductive lifespan, and menopause on the metabolic risk factors for cardiovascular diseases. The study found that every year’s increase in reproductive lifespan was associated with only a marginal increase in SBP and DBP and did not reach statistical significance (9). However, this study only selected a certain southern city in China as the population source, which cannot well represent the whole population of China. In addition, the study adjusted for only a small number of confounding factors, perhaps leading to a statistical bias.
Although several studies have explored the association between the risk of hypertension and age at menarche in women in China, these studies were limited to one province/city/area, included a smaller number of participants, and the conclusions of those studies were inconsistent (11, 17, 18). Therefore, using data from a representative sample of 234,867 Chinese women, our findings confirmed the association between age at menarche and the risk of hypertension, and showed that each 1-year delay in menarche was associated with a 6.2% increase in the prevalence of hypertension. The relationships between age at menarche and hypertension were also inconsistent in other countries. The result from 12,336 participants in the Korean National Health and Nutrition Examination Survey manifested no significant association between age at menarche and hypertension (19). However, a Brazilian study of 33,715 participants found that age at menarche was inversely associated with increased blood pressure (10).
There was limited and contradictory literature on the effect of age at menopause on the risk of hypertension among postmenopausal women. One study among middle-aged and older Chinese women showed that for each 1-year delay in menopause, the prevalence of hypertension decreased by 2% (20). Another study from China reported that the association between post-menopause and blood pressure disappeared after adjusting for BMI (9).
The mechanisms by which age at menarche or menopause is associated with hypertension are complex and are yet to be fully elucidated. The reproductive years can be regarded as the simplest measurement of cumulative exposure to sex hormones. A systematic review on the association between reproductive lifespan characteristics and risk of Type 2 diabetes and hypertension suggests a protective effect for a longer reproductive lifespan, while estrogen exposure may have an independent effect. In addition, various genes that regulate the renin-angiotensin system and adrenergic system, estradiol, testosterone, estrogen/androgen ratio, and environmental factors such as age, BMI, insulin, oxidative stress, and cholesterol affect the risk of hypertension among postmenopausal women (21). In particular, the decrease of estrogen level reduces the vascular relaxation effect of estrogen and improves the vasoconstriction effect of endothelin (22), leading to an increased risk of hypertension during the menopausal transition (23). Therefore, future longitudinal studies are needed to examine the relationship between reproductive markers and the risk of hypertension as well as the risk attributable to the administration of exogenous hormones, such as contraceptives and menopause hormone therapy (MHT).
Interestingly, we also found that the reproductive lifespan at 35–37 years was most associated with hypertension compared to > 38 years. In addition, when stratified by the age of recruitment, compared with 60–70 years and ≥ 70 years, positive associations between reproductive lifespan and risk of hypertension were evident among women aged < 60 years. Age is an important risk factor due to reproductive stages being part of the aging process. Considering both the timing of menarche and menopause during the reproductive lifespan, the study found that the effect of menopausal status disappeared after adjusting for age implying that much of the hypertension risk in menopausal transition was possibly related to biological aging (14). This explains the rational behavior of the phenomenon to some extent. In our study, to assess the effects of the reproductive lifespan on hypertension independent of the normal aging process, we removed the effect of age at recruitment before the analyses. This may result in underestimated effect sizes. Even in this case, we still get a significant effect that reflects a possible real association between reproductive lifespan and hypertension. We also discovered that the positive association between reproductive lifespan and hypertension was stronger among current alcohol drinkers in subgroup analyses. The alcohol-hypertension relationship has been well documented (24, 25). The study found that chronic exposure to alcohol alters the production of this same set of hormones (i.e., estrogen and testosterone), and hence, alcohol’s effects on the cardiovascular system could involve an indirect mechanism in which alcohol alters hormone levels and, in turn, the hormones affect the BP (26).
Limitations and strengths
The important strength of our study is to explore the relationship between reproductive lifespan and hypertension in Chinese women for the first time in a nationally representative sample. In addition, standardized approaches and stringent quality control measures were also taken to ensure data quality and reliability. We adjusted for potential risk factors for hypertension and performed a detailed subgroup analysis to improve the reliability of the findings. Several limitations need to be considered. First, our participants were Chinese women, which minimized the confounding effects of ethnic background but might minish the generalization of our findings to other ethnic groups. Second, the reproductive lifespan was calculated based on age at menarche and menopause, which were self-reported and not based on medical documentation, raising the possibility of misclassification due to recall bias. However, previous studies have reported that the recall of age at menarche (27, 28) and menopause is relatively accurate (29, 30). Lastly, although we have fully adjusted for potential confounders, the possibility of residual confounding from other known or unknown risk factors cannot be completely ruled out. Finally, the cross-sectional design could not prove a causal relationship.
Conclusion
Based on a representatively national sample of 94,141 Chinese postmenopausal women, we found that the longer the reproductive lifespan, the lower the risk of hypertension. The risk of hypertension is reduced by 1.1% for every 1-year increase in reproductive lifespan.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Fuwai Hospital (Beijing, China). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZH: conceptualization and writing – original draft preparation. LC: methodology, formal analysis, and software. XW: investigation and writing – original draft preparation partly. ZC, LZ, and CZ: data curation, formal analysis, and software; HZ, XC, YT, JC, YH, RG, YT, and LS: investigation. ZW: conceptualization, funding acquisition, and writing – review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the CAMS Innovation Fund for Medical Sciences (grant number: 2017-I2M-1-004); the China National Science & Technology Pillar Program (grant number: 2011BAI11B01); the surveillance of cardiovascular and its risk factors among Chinese Residents; and the National Key R&D Program of China during the Thirteen Five-Year Plan Period (grant number: No. 2018YFC1315303).
Acknowledgments
This study was accomplished through the fine work of the staff at the national level. We thank all of the colleagues involved in the survey and we also gratefully acknowledge Suning Li for maintaining the data. The authors are grateful to OMRON Corporation, Kyoto, Japan, for supporting the Blood Pressure Monitor (HBP-1300) and body fat and weight measurement device (V-body HBF-371); Henan Huanan Medical Science and Technology Co., Ltd., China, for Digital ECG device (GY-5000); and Microlife, Taipei, Taiwan, for Automated ABI device (Watch BP Office device). OMRON, Henan Huanan Medical Science and Technology, and Microlife provided medical devices but were not involved in the study design, collection, analysis, interpretation of data, and the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.898608/full#supplementary-material
Abbreviations
BP, blood pressure; CHS, Chinese Hypertension Survey; CVD, Cardiovascular disease; SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index; SD, standard deviation; OR, odds ratio; CI, confidence interval; MHT, menopause hormone therapy.
References
1. Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. (2008) 371:1513–8. doi: 10.1016/S0140-6736(08)60655-8
2. Hussen FM, Adem HA, Roba HS, Mengistie B, Assefa N. Self-care practice and associated factors among hypertensive patients in public health facilities in Harar Town, Eastern Ethiopia: a cross-sectional study. SAGE Open Med. (2020) 8:2050312120974145. doi: 10.1177/2050312120974145
3. Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 386:2287–323.
4. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. (2005) 365:217–23. doi: 10.1016/S0140-6736(05)17741-1
5. National Blood Pressure Sampling Survey Collaboration Group. Prevalence, awareness, treatment and control of hypertension in china: results of the 1991 sample survey. J Hyperten. (1995) S1:16–20.
6. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of Hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. (2018) 137:2344–56.
7. Gu D, Kelly TN, Wu X, Chen J, Duan X, Huang JF, et al. Blood pressure and risk of cardiovascular disease in Chinese men and women. Am J Hypertens. (2008) 21:265–72.
8. Lima R, Wofford M, Reckelhoff JF. Hypertension in postmenopausal women. Curr Hypertens Rep. (2012) 14:254–60. doi: 10.1007/s11906-012-0260-0
9. Feng Y, Hong X, Wilker E, Li Z, Zhang W, Jin D, et al. Effects of age at menarche, reproductive years, and menopause on metabolic risk factors for cardiovascular diseases. Atherosclerosis. (2008) 196:590–7. doi: 10.1016/j.atherosclerosis.2007.06.016
10. Werneck AO, Oyeyemi AL, Cyrino ES, Ronque ERV, Szwarcwald CL, Coelho ESMJ, et al. Association between age at menarche and blood pressure in adulthood: is obesity an important mediator? Hypertens Res. (2018) 41:856–64. doi: 10.1038/s41440-018-0079-4
11. Zhang L, Li Y, Zhou W, Wang C, Dong X, Mao Z, et al. Mediation effect of BMI on the relationship between age at menarche and hypertension: the Henan rural cohort study. J Hum Hypertens. (2020) 34:448–56. doi: 10.1038/s41371-019-0247-2
12. Bubach S, De Mola CL, Hardy R, Dreyfus J, Santos AC, Horta BL. Early menarche and blood pressure in adulthood: systematic review and meta-analysis. J Public Health. (2018) 40:476–84. doi: 10.1093/pubmed/fdx118
13. de Kat AC, Dam V, Onland-Moret NC, Eijkemans MJ, Broekmans FJ, van der Schouw YT. Erratum to: unraveling the associations of age and menopause with cardiovascular risk factors in a large population-based study. BMC Med. (2017) 15:74. doi: 10.1186/s12916-017-0841-5
14. Casiglia E, d’Este D, Ginocchio G, Colangeli G, Onesto C, Tramontin P. Lack of influence of menopause on blood pressure and cardiovascular risk profile: a 16-year longitudinal study concerning a cohort of 568 women. J Hypertens. (1996) 14:729–36. doi: 10.1097/00004872-199606000-00008
15. Dreyfus J, Jacobs DR Jr., Mueller N, Schreiner PJ, Moran A, Carnethon MR, et al. Age at menarche and cardiometabolic risk in adulthood: the coronary artery risk development in young adults study. J Pediatr. (2015) 167:344–52.e1. doi: 10.1016/j.jpeds.2015.04.032
16. Wang Z, Zhang L, Chen Z, Wang X, Shao L, Guo M, et al. Survey on prevalence of hypertension in China: background, aim, method and design. Int J Cardiol. (2014) 174:721–3.
17. Shen L, Wang L, Hu Y, Liu T, Guo J, Shen Y, et al. Associations of the ages at menarche and menopause with blood pressure and hypertension among middle-aged and older Chinese women: a cross-sectional analysis of the baseline data of the China Health and Retirement Longitudinal Study. Hypertens Res. (2019) 42:730–8. doi: 10.1038/s41440-019-0235-5
18. Liu G, Yang Y, Huang W, Zhang N, Zhang F, Li G, et al. Association of age at menarche with obesity and hypertension among southwestern Chinese women: a new finding. Menopause. (2018) 25:546–53. doi: 10.1097/GME.0000000000001027
19. Won JC, Hong JW, Noh JH, Kim DJ. Association between age at menarche and risk factors for cardiovascular diseases in Korean women: the 2010 to 2013 Korea national health and nutrition examination survey. Medicine. (2016) 95:e3580. doi: 10.1097/MD.0000000000003580
20. Song L, Shen L, Li H, Liu B, Zheng X, Zhang L, et al. Age at natural menopause and hypertension among middle-aged and older Chinese women. J Hypertens. (2018) 36:594–600. doi: 10.1097/HJH.0000000000001585
21. Coylewright M, Reckelhoff JF, Ouyang P. Menopause and hypertension: an age-old debate. Hypertension. (2008) 51:952–9. doi: 10.1161/HYPERTENSIONAHA.107.105742
22. Reckelhoff JF, Fortepiani LA. Novel mechanisms responsible for postmenopausal hypertension. Hypertension. (2004) 43:918–23. doi: 10.1161/01.HYP.0000124670.03674.15
23. Maas AH, Franke HR. Women’s health in menopause with a focus on hypertension. Neth Heart J. (2009) 17:68–72. doi: 10.1007/BF03086220
24. Liu F, Liu Y, Sun X, Yin Z, Li H, Deng K, et al. Race- and sex-specific association between alcohol consumption and hypertension in 22 cohort studies: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. (2020) 30:1249–59. doi: 10.1016/j.numecd.2020.03.018
25. Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OSM, et al. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J Am Heart Assoc. (2018) 7:e008202. doi: 10.1161/JAHA.117.008202
26. Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens. (2012) 14:792–8. doi: 10.1111/jch.12008
27. Must A, Phillips S, Naumova E, Blum M, Harris S, Dawson-Hughes B, et al. Recall of early menstrual history and menarcheal body size: after 30 years, how well do women remember? Am J Epidemiol. (2002) 155:672–9. doi: 10.1093/aje/155.7.672
28. Casey V, Dwyer J, Coleman K, Krall E, Gardner J, Valadian I. Accuracy of recall by middle-aged participants in a longitudinal study of their body size and indices of maturation earlier in life. Ann Hum Biol. (1991) 18:155–66. doi: 10.1080/03014469100001492
29. Colditz GA, Stampfer MJ, Willett WC, Stason WB, Rosner B, Hennekens CH, et al. Reproducibility and validity of self-reported menopausal status in a prospective cohort study. Am J Epidemiol. (1987) 126:319–25. doi: 10.1093/aje/126.2.319
Keywords: CHS, Chinese Hypertension Survey, postmenopausal women, reproductive lifespan, hypertension, risk, blood pressure
Citation: Hu Z, Chen L, Wang X, Zhang L, Chen Z, Zheng C, Cao X, Song Y, Zhou H, Tian Y, Cai J, Huang Y, Gu R, Tian Y, Shao L and Wang Z (2022) Reproductive lifespan in association with risk of hypertension among Chinese postmenopausal women: Results from a large representative nationwide population. Front. Cardiovasc. Med. 9:898608. doi: 10.3389/fcvm.2022.898608
Received: 17 March 2022; Accepted: 11 July 2022;
Published: 08 August 2022.
Edited by:
Stefania Triunfo, University of Milan, ItalyReviewed by:
Palash Chandra Banik, Bangladesh University of Health Sciences, BangladeshLingkan Barua, Bangladesh University of Health Sciences, Bangladesh
Copyright © 2022 Hu, Chen, Wang, Zhang, Chen, Zheng, Cao, Song, Zhou, Tian, Cai, Huang, Gu, Tian, Shao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zengwu Wang, wangzengwu@foxmail.com
†These authors have contributed equally to this work
 Zhen Hu
Zhen Hu