
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Cardiovasc. Med., 19 May 2022
Sec. Cardiovascular Epidemiology and Prevention
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.893811
This article is part of the Research TopicSports CardiologyView all 19 articles
Physical exercise reduces blood pressure (BP) in patients with hypertension in general but more evidence is needed specifically for a high-risk phenotype associated with intensive medication, resistant hypertension (RH). In this systematic review and meta-analysis, we aimed to summarize current evidence of the exercise effects on BP in patients with RH. A systematic search was conducted in PubMed, Web of Science and Cochrane Library (from inception to 3rd November, 2021). A random effects meta-analysis was performed when at least two trials assessed the effect of either acute or regular exercise (vs. a control condition) on the same outcome. Ten studies (N = 380 participants; 51% female; mean age 52 to 67 years) were included in the review, of which four (N = 58) and six (N = 322) assessed the effects of acute and regular exercise, respectively. Evidence overall suggests that a single bout of acute exercise results in a short-term (≤ 24 h) reduction of BP, although no meta-analysis could be performed. As for regular exercise, three randomized controlled trials (N = 144, 50% female) could be meta-analyzed, which showed that exercise training intervention (8–12 weeks, 3 sessions/week) significantly reduces 24-h (−9.9 mmHg, 95% confidence interval −15.4−4.4 for systolic BP; and −5 mmHg, −7.0−3.0 for diastolic BP) and daytime ambulatory BP (−11.7 mmHg, −17.8−5.7; and −7.4 mmHg, −11.9−2.9). In summary, physical exercise appears as an effective option to reduce BP in patients with RH, although more research is needed to confirm these findings as well as to determine the most effective exercise characteristics.
Approximately 12–15% of hypertensive patients have resistant hypertension (RH) (1), traditionally defined as above-goal clinic (“office”) blood pressure (BP) (i.e., systolic BP (SBP)/diastolic BP (DBP) >130/80 mmHg (2) or >140/90 mmHg (3) according to the American College of Cardiology/American Heart Association or European Society of Cardiology/European Society of Hypertension guidelines, respectively) despite the concurrent use of three or more antihypertensive drugs — commonly including a diuretic, a long-acting calcium channel blocker, and a blocker of the renin-angiotensin system — at maximum or maximally tolerated oral doses (1). RH also includes patients whose BP achieves target values on ≥4 antihypertensive medications (i.e., 'controlled' RH) (1). Because the management of this condition based solely on medications has proven only partially successful (1), non-pharmacological strategies should also be considered.
Lifestyle, particularly physical exercise, can play an important role in BP management in individuals with hypertension (4). Meta-analytical evidence shows that exercise training intervention reduces not only office (5) but also ambulatory BP (ABP) in these individuals (6), with the latter measure being a stronger predictor of cardiovascular diseases (CVD) and mortality (7). Notably, there is recent meta-analytical evidence that a single bout of acute exercise (8) and regular exercise training (6) induce significant short (≤ 24 h) and mid-term (up to ~6 months) reductions in ABP, respectively, among patients with hypertension in general. Furthermore, exercise has minimal side effects compared with drugs (9) and is considered as effective as most antihypertensive agents to reduce office BP (10). However, although the benefits of both acute and regular exercise on BP are well-established in patients with hypertension in general (5, 6, 8), scarcer evidence is available in the context of RH specifically.
Available evidence on the effects of exercise intervention in individuals with RH shows promising results, as confirmed by some non-systematic reviews (11–14). Different trials have reported a beneficial effect of acute (15, 16) or regular exercise (17–20) on office BP or ABP in patients with RH. However, to the best of our knowledge there has been no previous attempts to systematically synthesize the evidence available on the effects of acute or regular exercise on BP measures in patients with RH. Under this context, we aimed to summarize current evidence of the effects of acute or regular exercise on ABP measures in patients with RH.
The review protocol is registered in PROSPERO (International Prospective Register of Systematic Reviews) (https://www.crd.york.ac.uk/PROSPERO/; Unique identifier: CRD42021287788). Two researchers (GSL, PLV) independently conducted a systematic search — first by title and abstract, and then by full-text — in PubMed, Cochrane Library and Web of Science from inception to 3rd November 2021 using the following search strategy: (“exercise” OR “physical activity” OR “training”) AND (“blood pressure” OR “BP” OR “SBP” OR “DBP”) AND (“resistant hypertension” OR “resistant hypertensive”). This search was supplemented by a manual review of reference lists from relevant publications. We did not search abstracts, posters, and workshop presentations.
Eligibility criteria were defined in accordance with the Population, Intervention, Comparison, Outcome and Study Design (PICOS) approach (21). We included studies that met each of the following inclusion criteria:
- Population: Adults diagnosed with RH.
- Intervention: Physical exercise, including both a single acute exercise bout and/or regular exercise training (i.e., for several weeks/months). No restrictions were made regarding the frequency, duration, or length of the exercise interventions.
- Comparison: The comparator was a control condition where participants performed no physical exercise.
- Outcomes: Office or ABP.
- Study design: There were no exclusion criteria regarding the study design.
When two studies included part of the same patients' cohort, only data from the study with more participants were included in the meta-analysis.
Two reviewers (GSL, PLV) independently identified for each study the number and characteristics of participants, exercise intervention details, endpoints, and results. Data were extracted as mean (standard deviation) when available. When data were provided as intervention effects or using other measures of dispersion (e.g., standard error, 95% confidence interval), the required information was estimated following published guidelines (22). A specific software (WebPlotDigitizer 4.2, San Francisco, CA) was used to extract data provided as a figure in one study (18).
Two authors (GSL, PLV) independently assessed the methodological quality of the different studies using the Tool for the Assessment of Study Quality and Reporting in Exercise (TEXTES) for chronic exercise interventions (23). For studies assessing the short-term effects of a single bout of acute exercise, we used a modified version of the TEXTES scale as proposed elsewhere (24).
We performed meta-analyses when a minimum of two studies assessed the effects of either acute or regular exercise on a given outcome. A random-effects (DerSimonian and Laird) meta-analysis was performed to assess the mean difference between exercise and control groups using baseline and post-intervention data. Because none of the included studies provided information on the correlation between baseline and post-intervention BP, we used a Pearson's correlation coefficient (r) value of 0.8, in consistence with previous research (25, 26). Publication bias and heterogeneity across studies was assessed with the Begg's test and the I2 statistic, respectively. Sensitivity analyses were performed by removing one study at a time. Analyses were conducted using Comprehensive Meta-analysis 2.0 (Biostat; Englewood, NJ) with α = 0.05.
Ten studies (N = 380 participants, 51% female, age range 52 to 67 years) were included in the review, of which four (15, 16, 27, 28) (N = 58, 50% female) assessed the short-term (≤ 24 h) effects of acute physical exercise and six (17, 18, 20, 29–31) (N = 322, 51% female) assessed the mid-term (up to 6 months) effects of exercise training intervention (Table 1, Flowchart available as Supplementary Figure 1). Participants of two studies (19, 32) were enrolled in a larger RCT (18). Therefore, we only considered the study with more participants (18).
One study was excluded because the same patients had also participated in previous published research (33). In addition, another study was excluded because analyses were solely focused on the BP effects of exercise training cessation (34).
Studies assessing the short-term effects of a single acute exercise bout applied sessions of ~10–45 min of strength exercise [moderate intensity, corresponding to 3–5 on the adapted Borg' 0–10 scale of rating of perceived exertion (RPE)] (16), aerobic [50-75% of maximum heart rate (HRmax) (15), 50–60% of HRmax (16), walking at a speed of 3 km/h (27), incremental cycling test (28)], or combined exercise (aerobic exercise at 50–60% of HRmax and strength exercise at moderate intensity, corresponding to 3–5 on the adapted Borg's 0–10 RPE scale) (16).
As for regular exercise, training programs lasted 2 to 24 weeks and included 3 weekly sessions of ~30-60 min duration. Interventions included aerobic [at an intensity of 70-85% of heart rate reserve (29), 50-70% of peak oxygen uptake (17), or slightly above the aerobic threshold (20)] or combined training (i.e., calisthenics and walking against water resistance in a 30–32°C–heated pool at an intensity corresponding to 11–13 on the Borg's 0–20 RPE scale) (18). Three studies reported adherence to the intervention, which averaged 89–100% (17, 18, 29). No major adverse events were noted (e.g., no excessive hypertensive/hypotensive response) in any of the studies (17, 18, 20).
Both the studies assessing the effects of acute (Supplementary Table 1) and regular exercise (Supplementary Table 2) were of overall good quality (median total score = 6.5 and 11, respectively; quality score = 3 and 3.5; reporting score = 6.5 and 7.5).
Three of the four included studies that assessed the short-term effects of a single bout of acute exercise found a beneficial effect on at least one BP measure. Two RCT found significant benefits on ABP measures after acute exercise (15, 16). One study lacking a control group found benefits of acute exercise on central and peripheral DBP — but not on SBP (27). Finally, one study failed to report a significant reduction in SPB following cardiopulmonary exercise testing in patients with RH who had not undergone renal sympathetic denervation (28).
As for regular exercise, all six studies (17, 18, 20, 29–31) found significant reductions in office BP or ABP measures after exercise training intervention. Five studies showed significant benefits to 24-hour or daytime ABP measures (17, 18, 20, 29, 32), and one found significant benefits to nighttime ABP measures (29). Four studies (17, 18, 29, 30) reported a significant reduction in office BP measures. Three RCT could be meta-analyzed (N = 144; 50% female; mean participants' age ranging from 52 to 67 years; weighted average office BP and ABP of 148/83 mmHg and 134/77 mmHg, respectively) (17, 18, 20). Pooled analyses indicated that exercise training tended to decrease office SBP (p=0.059) while significantly reducing office DBP as well as all the different ABP measures (24-h, daytime, and nighttime SBP/DBP, respectively) with no sign of publication bias (all Begg's test p > 0.15) (Table 2). The results of 24-h and daytime ABP remained significant in sensitivity analyses. Due to the differences in study designs (i.e., no control group) (30, 31), inclusion of nutritional interventions together with exercise training (29, 30), and the fact that some participants were also enrolled in a larger RCT (19, 32), we could not meta-analyze more studies.
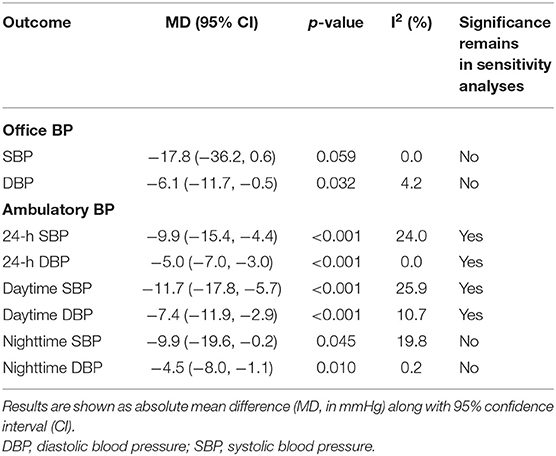
Table 2. Pooled analysis of the effect of exercise training intervention on blood pressure (BP) measures in patients with resistant hypertension.
This is the first systematic review and meta-analysis of the exercise effects on BP in patients with RH. Our findings overall suggest that a single bout of acute exercise might reduce BP in the short-term (i.e., within ~24 h) in these patients, although no meta-analysis could be performed. Moreover, “chronic” exercise training interventions (e.g., three sessions/week for up to 6 months) seem to induce significant reductions in office and ABP measures. These results might therefore support the role of exercise as an effective co-adjuvant treatment in patients with RH. This finding is of clinical relevance, particularly when considering that these individuals are at high risk of cardiovascular complications (1). In fact, subjects with elevated resting and/or exercise BP show a worse cardiorespiratory fitness — a strong predictor of CVD and associated mortality — than those with normal BP levels (35), and BP reductions considerably lower than those reported here (e.g., −1.0−2.0 mmHg) have been associated with a reduced risk of cardiovascular complications in people with hypertension in general (36, 37).
In line with our findings, a recent meta-analysis showed that a single bout of acute aerobic exercise induces short-term reductions on ABP measures in patients with hypertension (8). To the best of our knowledge, only four studies to date have analyzed the short-term effects of acute exercise on BP in patients with RH (15, 16, 27, 28), although results seem overall promising. Two randomized cross-over studies found a beneficial effect on ABP after different types of acute exercise in patients with RH (15, 16), and Ribeiro et al. found a significant reduction of central and peripheral DBP — but not SBP — after walking for only 10 min using a non-RCT design in a group of patients with RH (27). It must be noted, nonetheless, that Ukena et al. found no significant effects on SPB after cardiopulmonary exercise testing in patients with RH who had not undergone renal sympathetic denervation (28). Unfortunately, due to the differences in study designs and the paucity of available studies, we could not meta-analyze the effects of acute exercise on BP. Further research is thus needed to confirm whether the benefits of acute exercise previously corroborated in hypertensive patients in general also apply to patients with RH specifically.
The reductions of BP observed in the present study in individuals with RH after exercise training intervention are overall in line with those reported by us in a recent meta-analysis, in which we observed that exercise interventions with a duration of eight to 24 weeks decrease 24-h (average reduction of −5.4 and −3.0 mmHg for SBP and DBP, respectively), daytime (−4.5 and −3.2 mmHg), and nighttime ABP (−4.7 and −3.1 mmHg), respectively, in patients with hypertension in general (N = 910) (6). However, greater reductions of ABP seem to occur in patients with RH. These differences might be due to the so-called Wilder's principle (38) — that is, exercise induces larger effects in those patients with higher BP at baseline, such as those with the most severe hypertension phenotypes, notably RH. Other factors can also be involved in these differences, notably the lower number of studies included in the present meta-analysis, which could have partly confounded our results, along with the fact that in one study exercise was performed in a heated pool, which can magnify the hypotensive effects of exercise per se (18).
Some limitations must be acknowledged, notably the limited number of studies meta-analyzed, which precluded us from performing sub-analyses attending to variables such as the characteristics of the interventions (in terms of exercise modality or total duration of the exercise training programs) or of the participants (notably, in terms of age, sex or medication status). More research is needed in order to identify the most effective exercise characteristics (modality, intensity, duration) for reducing office BP/ABP in patients with RH, as well as to confirm whether exercise training per se might allow reducing the number and/or dosage of drugs needed to manage BP in patients with this condition. The latter question is important because a reduction in medication is associated with lower mortality in individuals with RH (39). Finally, the long-term (i.e., more than 6 months) effects of exercise training intervention also remain to be determined.
In conclusion, our results suggest that exercise training interventions (8–12 weeks, 3 sessions per week, ideally combining aerobic activities at light-moderate intensities such as walking or cycling) as well as muscle strengthening sessions (such as light-moderate intensity weight lifting or calisthenics) decrease both “office” and ABP measures, with even a single bout of acute exercise potentially reducing BP within the following ~24 h. Although further high-quality research (e.g., using a RCT design) is needed to confirm these findings as well as to corroborate the beneficial effects of a single bout of acute exercise on BP, physical exercise appears as an overall effective option to induce meaningful BP reductions in patients with RH.
AL, GS-L, and PV: study concept and design, methodology, supervision, interpretation of data, and drafting of the manuscript. PV: statistical analysis. All authors critically revised the manuscript for important intellectual content and approved the final version of the manuscript.
Research by LR and GS-L is funded by FEDER/Ministerio de Ciencia e Innovación – Agencia Estatal de Investigación, Spain (PID2020-114862RB-I00/AEI/10.13039/501100011033). PV is supported by a Sara Borrell post-doctoral contract by Instituto de Salud Carlos III (CD21/00138). Research by AL is funded by the Spanish Ministry of Science and Innovation (Instituto de Salud Carlos III, Fondo de Investigaciones Sanitarias and Fondos FEDER, grant number PI18/00139).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.893811/full#supplementary-material
1. Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. American Heart Association Professional/Public Education and Publications Committee of the Council on Hypertension; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Genomic and Precision Medicine; Council on Peripheral Vascular Disease; Council on Quality of Care and Outcomes Research; and Stroke Council. Resistant hypertension: Detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. (2018) 72:e53–90. doi: 10.1161/HYP.0000000000000084
2. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. (2018) 71:1269–324. doi: 10.1161/HYP.0000000000000066
3. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, et al. ESC Scientific Document Group. ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
4. Valenzuela PL, Carrera-Bastos P, Gálvez BG Ruiz-Hurtado G, Ordovas JM, Ruilope LM, Lucia A. Lifestyle interventions for the prevention and treatment of hypertension. Nat Rev Cardiol. (2021) 18:251–75. doi: 10.1038/s41569-020-00437-9
5. Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. (2019) 51:1314–23. doi: 10.1249/MSS.0000000000001943
6. Saco-Ledo G, Valenzuela PL, Ruiz-Hurtado G, Ruilope LM, Lucia A. Exercise reduces ambulatory blood pressure in patients with hypertension: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. (2020) 9:e018487. doi: 10.1161/JAHA.120.018487
7. Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N., McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. (2005) 46:156–61. doi: 10.1161/01.HYP.0000170138.56903.7a
8. Saco-Ledo G, Valenzuela PL, Ramírez-Jiménez M, Morales JS, Castillo-García A, Blumenthal JA, et al. Acute aerobic exercise induces short-term reductions in ambulatory blood pressure in patients with hypertension: a systematic review and meta-analysis. Hypertension. (2021) 78:1844–58. doi: 10.1161/HYPERTENSIONAHA.121.18099
9. Fiuza-Luces C, Garatachea N, Berger NA, Lucia A. Exercise is the real polypill. Physiology (Bethesda). (2013) 28:330–58. doi: 10.1152/physiol.00019.2013
10. Naci H, Salcher-Konrad M, Dias S, Blum MR, Sahoo SA, Nunan D, et al. How does exercise treatment compare with antihypertensive medications? A network meta-analysis of 391 randomised controlled trials assessing exercise and medication effects on systolic blood pressure. Br J Sports Med. (2019) 53:859–69. doi: 10.1136/bjsports-2018-099921
11. Ozemek C, Tiwari S, Sabbahi A, Carbone S, Lavie CJ. Impact of therapeutic lifestyle changes in resistant hypertension. Prog Cardiovasc Dis. (2020) 63:4–9. doi: 10.1016/j.pcad.2019.11.012
12. Sabbahi A, Severin R, Laddu D, Sharman JE, Arena R, Ozemek C. Nonpharmacological management of resistant hypertension. Curr Cardiol Rep. (2021) 23:166. doi: 10.1007/s11886-021-01601-4
13. Dassanayake S, Sole G, Wilkins G, Skinner M. Exercise: a therapeutic modality to treat blood pressure in resistant hypertension. Phys Ther Rev. (2020) 25:149–58. doi: 10.1080/10833196.2020.1733781
14. Lopes S, Mesquita-Bastos J, Alves AJ, Ribeiro F. Exercise as a tool for hypertension and resistant hypertension management: current insights. Integr Blood Press Control. (2018) 11:65–71. doi: 10.2147/IBPC.S136028
15. Santos LP, Moraes RS, Vieira PJC, Ash GI, Waclawovsky G, Pescatello LS, et al. Effects of aerobic exercise intensity on ambulatory blood pressure and vascular responses in resistant hypertension: a crossover trial. J Hypertens. (2016) 34:1317–24. doi: 10.1097/HJH.0000000000000961
16. Pires NF, Coelho-Júnior HJ, Gambassi BB, de Faria APC, Ritter AMV, de Andrade Barboza C, et al. Combined aerobic and resistance exercises evokes longer reductions on ambulatory blood pressure in resistant hypertension: a randomized crossover trial. Cardiovasc Ther. (2020) 2020:8157858. doi: 10.1155/2020/8157858
17. Lopes S, Mesquita-Bastos J, Garcia C, Bertoquini S, Ribau V, Teixeira M, et al. Effect of exercise training on ambulatory blood pressure among patients with resistant hypertension: a randomized clinical trial. JAMA Cardiol. (2021) 6:1317–23. doi: 10.1001/jamacardio.2021.2735
18. Cruz LG, de B, Bocchi EA, Grassi G, Guimaraes GV. Neurohumoral and endothelial responses to heated water-based exercise in resistant hypertensive patients. Circ J. (2017) 81:339–45. doi: 10.1253/circj.CJ-16-0870
19. Guimaraes GV, de Barros Cruz LG, Fernandes-Silva MM, Dorea EL, Bocchi EA. Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistant hypertensive patients: a randomized controlled trial (HEx trial). Int J Cardiol. (2014) 172:434–41. doi: 10.1016/j.ijcard.2014.01.100
20. Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH. Aerobic exercise reduces blood pressure in resistant hypertension. Hypertension. (2012) 60:653–8. doi: 10.1161/HYPERTENSIONAHA.112.197780
21. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
22. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0 (updated July 2019). Cochrane, 2019. Available online at: www.training.cochrane.org/handbook (accessed November 20, 2021).
23. Smart NA, Waldron M, Ismail H, Giallauria F, Vigorito C, Cornelissen V, et al. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int J Evid Based Healthc. (2015) 13:9–18. doi: 10.1097/XEB.0000000000000020
24. Farah BQ, Germano-Soares AH, Rodrigues SLC, Santos CX, Barbosa SS, Vianna LC, et al. Acute and chronic effects of isometric handgrip exercise on cardiovascular variables in hypertensive patients: a systematic review. Sports (Basel). (2017) 5:55. doi: 10.3390/sports5030055
25. Fujiwara T, Hoshide S, Kanegae H, Nishizawa M, Kario K. Reliability of morning, before-dinner, and at-bedtime home blood pressure measurements in patients with hypertension. J Clin Hypertens (Greenwich). (2018) 20:315–23. doi: 10.1111/jch.13165
26. Ash GI, Walker TJ, Olson KM, Stratton JH, Gómez AL, Kraemer WJ, et al. Reproducibility of ambulatory blood pressure changes from the initial values on two different days. Clinics (São Paulo). (2013) 68:1509–15. doi: 10.6061/clinics/2013(12)06
27. Ribeiro F, Almeida N, Ferreira R, Oliveira N, Oliveira J, Alves AJ, et al. Central and peripheral blood pressure response to a single bout of an exercise session in patients with resistant hypertension. Hypertens Res. (2019) 42:114–6. doi: 10.1038/s41440-018-0100-y
28. Ukena C, Mahfoud F, Kindermann I, Barth C, Lenski M, Kindermann M, et al. Cardiorespiratory response to exercise after renal sympathetic denervation in patients with resistant hypertension. J Am Coll Cardiol. (2011) 58:1176–82. doi: 10.1016/j.jacc.2011.05.036
29. Blumenthal JA, Hinderliter AL, Smith PJ, Mabe S, Watkins LL, Craighead L, et al. Effects of lifestyle modification on patients with resistant hypertension: results of the TRIUMPH randomized clinical trial. Circulation. (2021) 144:1212–26. doi: 10.1161/CIRCULATIONAHA.121.055329
30. Kruk PJ, Nowicki M. Effect of the physical activity program on the treatment of resistant hypertension in primary care. Prim Health Care Res Dev. (2018) 19:575–83. doi: 10.1017/S1463423618000154
31. Carvalho CJ, Bouzas Marins JC, de Lade CG, de Rezende Castilho P, Teixeira Reis HH, dos Santos Amorim PR, et al. Aerobic and resistance exercise in patients with resistant hypertension. Rev Bras Med Esporte. (2019) 25:107–11. doi: 10.1590/1517-869220192502175333
32. Guimarães Gv, Cruz LGB, Tavares AC, Dorea EL, Fernandes-Silva MM, Bocchi EA. Effects of short-term heated water-based exercise training on systemic blood pressure in patients with resistant hypertension: a pilot study. Blood Press Monit. (2013) 18:342–5. doi: 10.1097/MBP.0000000000000000
33. Kruk PJ, Nowicki M. Effects of regular physical activity on pain, anxiety, and depression in patients with treatment-resistant arterial hypertension. Fam Med Prim Care Rev. (2016) 18:268–73. doi: 10.5114/fmpcr/63060
34. Guimaraes GV, Fernandes-Silva MM, Drager LF, de Barros Cruz LG, Castro RE, Ciolac EG, et al. Hypotensive effect of heated water-based exercise persists after 12-week cessation of training in patients with resistant hypertension. Can J Cardiol. (2018) 34:1641–7. doi: 10.1016/j.cjca.2018.09.013
35. Biffi A, Gallo G, Fernando F, Sirico F, Signorello MG, De Martino L, et al. Relationship between cardiorespiratory fitness, baseline blood pressure and hypertensive response to exercise in the ferrari corporate population. High Blood Press Cardiovasc Prev. (2022) 29:81–8. doi: 10.1007/s40292-021-00491-5
36. Hardy ST, Loehr LR, Butler KR, Chakladar S, Chang PP, Folsom AR, et al. Reducing the blood pressure-related burden of cardiovascular disease: impact of achievable improvements in blood pressure prevention and control. J Am Heart Assoc. (2015) 4:e002276. doi: 10.1161/JAHA.115.002276
37. Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. (1995) 155:701–9. doi: 10.1001/archinte.1995.00430070053006
38. Mora-Rodriguez R, Ortega JF, Morales-Palomo F, Ramirez M, Moreno-Cabañas A, Alvarez-Jimenez L. Endurance exercise training reduces blood pressure according to the wilder's principle. Int J Sports Med. (2021) 43:336–43. doi: 10.1055/a-1548-6985
Keywords: office blood pressure, ambulatory blood pressure, nighttime, daytime, hypertensives
Citation: Saco-Ledo G, Valenzuela PL, Ruilope LM and Lucia A (2022) Physical Exercise in Resistant Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Cardiovasc. Med. 9:893811. doi: 10.3389/fcvm.2022.893811
Received: 10 March 2022; Accepted: 22 April 2022;
Published: 19 May 2022.
Edited by:
Fabrizio Ricci, University of Studies G. d'Annunzio Chieti and Pescara, ItalyReviewed by:
Stefano Palermi, University of Naples Federico II, ItalyCopyright © 2022 Saco-Ledo, Valenzuela, Ruilope and Lucia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gonzalo Saco-Ledo, Z29uemFsby5zYWNvQHVuaXZlcnNpZGFkZXVyb3BlYS5lcw==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.