
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 23 September 2022
Sec. General Cardiovascular Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.893742
This article is part of the Research Topic Case Reports in General Cardiovascular Medicine: 2022 View all 35 articles
 Marcell Krall1
Marcell Krall1 Johannes Gollmer2
Johannes Gollmer2 Marion J. Pollheimer3
Marion J. Pollheimer3 Clemens Reiter4
Clemens Reiter4 Michael Kolland1
Michael Kolland1 Alexander H. Kirsch1
Alexander H. Kirsch1 Andreas Kronbichler5
Andreas Kronbichler5 Kathrin Eller1
Kathrin Eller1 Alexander R. Rosenkranz1
Alexander R. Rosenkranz1 Balazs Odler1*
Balazs Odler1*We report a case of a patient double-seropositive for anti-glomerular basement membrane (anti-GBM) and anti-neutrophil cytoplasmic antibodies (ANCA) who reported retrosternal chest pain during a regular hemodialysis session associated with ST-segment depression in electrocardiogram and an increase of serum high-sensitivity troponin T. Urgent coronary angiography excluded obstructive coronary artery disease, suggesting the diagnosis of ischemia with non-obstructive coronary arteries. This case illustrates an unusual presentation of cardiovascular involvement in a patient with double-positive ANCA/anti-GBM disease, emphasizing the possible relevance of coronary microvascular dysfunction and the need for close cardiovascular follow-up in this patient population.
Anti-neutrophil cytoplasm antibody (ANCA)-associated vasculitides (AAV) and anti-glomerular basement membrane (GBM) disease are rare entities (1, 2). The coincidence of positivity for anti-GBM and ANCA antibodies with clinical features of both diseases represents a life-threatening entity (3). Cardiovascular (CV) events are among the leading causes of death in AAV; thus, a more complex understanding of CV manifestations and their risk factors is required (4). In line, cardiac involvement is an underdiagnosed manifestation in AAV, and involvement of the coronary arteries is only rarely reported (5–9). Our case illustrates that myocardial infarction with non-obstructive coronary arteries (MINOCA) might be an important contributor to cardiac complications seen in patients with AAV and/or anti-GBM disease.
A 61-year-old Caucasian man presented to our university clinic with acute kidney injury. He was diagnosed with scleritis of the right eye approximately 13 years before current admission and had received azathioprine (AZA) for immunosuppression due to suspected myeloperoxidase (MPO)-ANCA positive granulomatosis with polyangiitis (GPA) without evidence of further organ involvements. Besides, he had arterial hypertension treated with angiotensin-converting enzyme inhibitor/hydrochlorothiazide and had been diagnosed with prostate cancer 2 years before current admission (treated by radiotherapy and gonadotropin-releasing hormone analog). The AZA therapy had been discontinued 19 months prior to presentation due to an influenza infection. Thereafter, on admission, a nephritic syndrome was present. Laboratory investigations revealed an increase of MPO-ANCA and anti-glomerular basement membrane (anti-GBM) antibody titers (>100 and 244 U/ml, respectively). Thus, a kidney biopsy was performed, and the diagnosis of double-positive disease was made (Figures 1A,B).
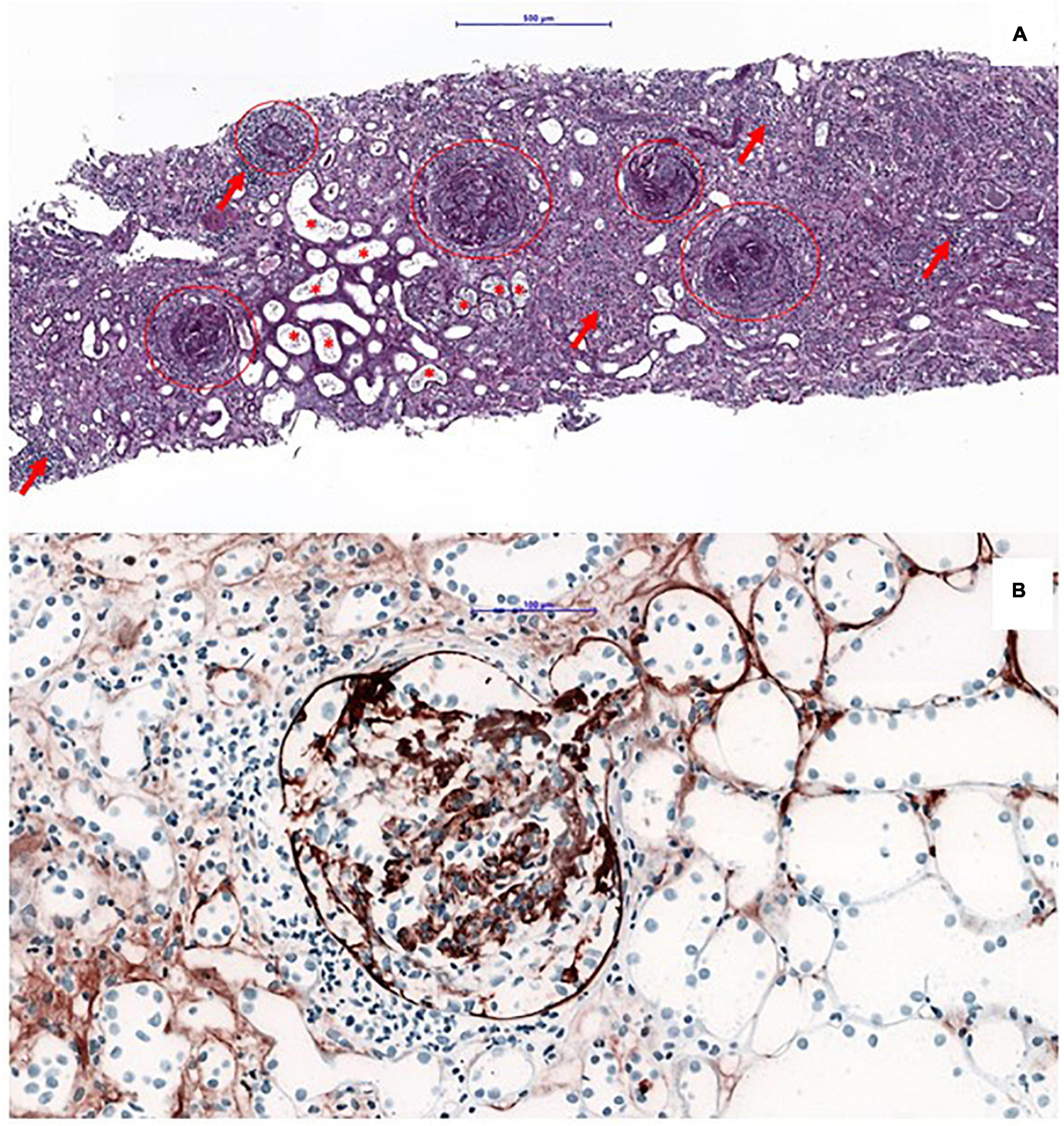
Figure 1. Kidney biopsy: an overview of a PAS-stained kidney biopsy, showing large cellular crescent present in all glomeruli (as highlighted by the circles), in line with a severe presentation of anti-glomerular basement membrane (anti-GBM) disease. Concomitant tubulo-interstitial nephritis (arrows) and signs of severe acute tubular injury with red blood cells within the tubular lumina (asteriks). Bar = 500 μm (A). Immunohistochemical staining with the antibody against IgG, showing a linear staining pattern of the glomerular basement membrane (B).
Plasma exchange (14 sessions), high-dose corticosteroids, and cyclophosphamide (CYC – cumulative dose of 3.3 g) were initiated. However, he progressed to end-stage kidney disease and required hemodialysis (HD). In addition, 2 doses of rituximab (RTX) 500 mg each 2 weeks apart were given followed by 500 mg every 6 months as maintenance immunosuppressive therapy.
After 4 weeks of HD initiation, during a regular HD session, the patient reported retrosternal chest pain. Electrocardiogram (ECG) showed ST depressions in leads II, III, aVF, and V4 to V6 (Figures 2A,B), which changes were absent in a previous ECG 1 month before (Figure 2C). High-sensitive troponin T (hs-Tn) was elevated (the baseline level: 1,514 pg/ml; normal range: <14 pg/ml); thus, the diagnosis of non-ST elevation myocardial ischemia was made (Figure 3). Bed-side echocardiography revealed mildly reduced ejection fraction (40%) with diffuse hypokinesia and pronounced abnormalities in inferior, inferolateral, and anterolateral segments. Urgent coronary angiography (CA) excluded obstructive coronary artery disease (CAD) in major epicardial vessels and did not show signs of ruptured plaque or dissection, suggesting the diagnosis of MINOCA (Figures 3A–E). Cardiac magnetic resonance (CMR) imaging was performed to exclude acute (peri) myocarditis. Cine imaging revealed severe left ventricular and atrial dilatation with global hypokinesia and reduced left ventricular ejection fraction, aortic and mitral insufficiency but preserved right ventricular function. Native myocardial T1-values were globally elevated, myocardial T2-values were within the normal ranges, T2-weighted images showed no signs of edema, and no late enhancement was visualized, therefore not fulfilling diagnostic criteria of an acute myocarditis (10) but consistent with diffuse myocardial fibrosis in dilated cardiomyopathy. Myocarditis was also ruled out by positron emission computed tomography. Notably, ANCA positivity was seen throughout the disease course, while hs-Tn decreased significantly a few weeks after the cardiac event (Figure 4).
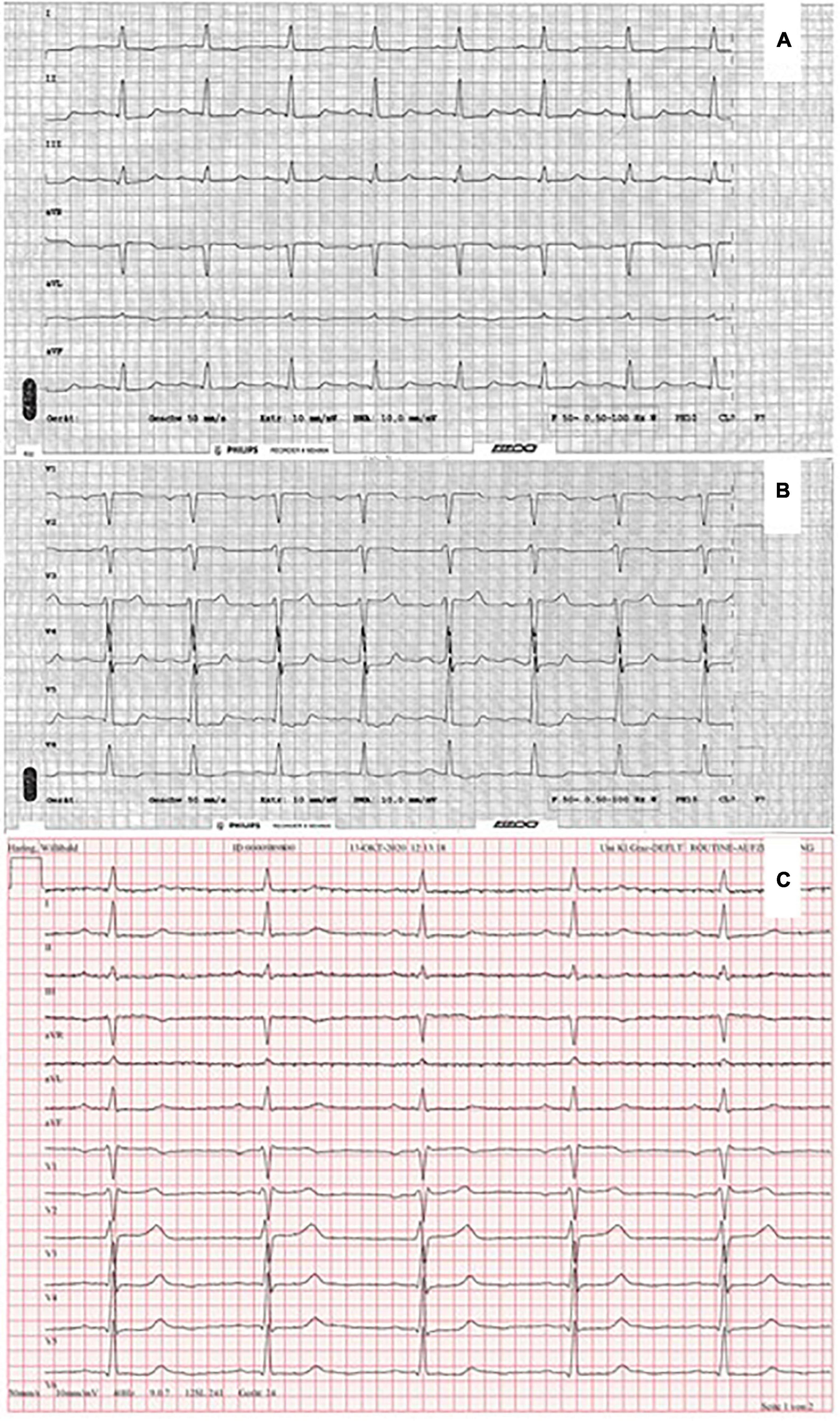
Figure 2. Electrocardiogram showing ST-segment depression in II, III, aVF (A), and V4–V6 (B). Electrocardiogram (with a paper speed of 50 mm/s) 1 month before MINOCA (C).
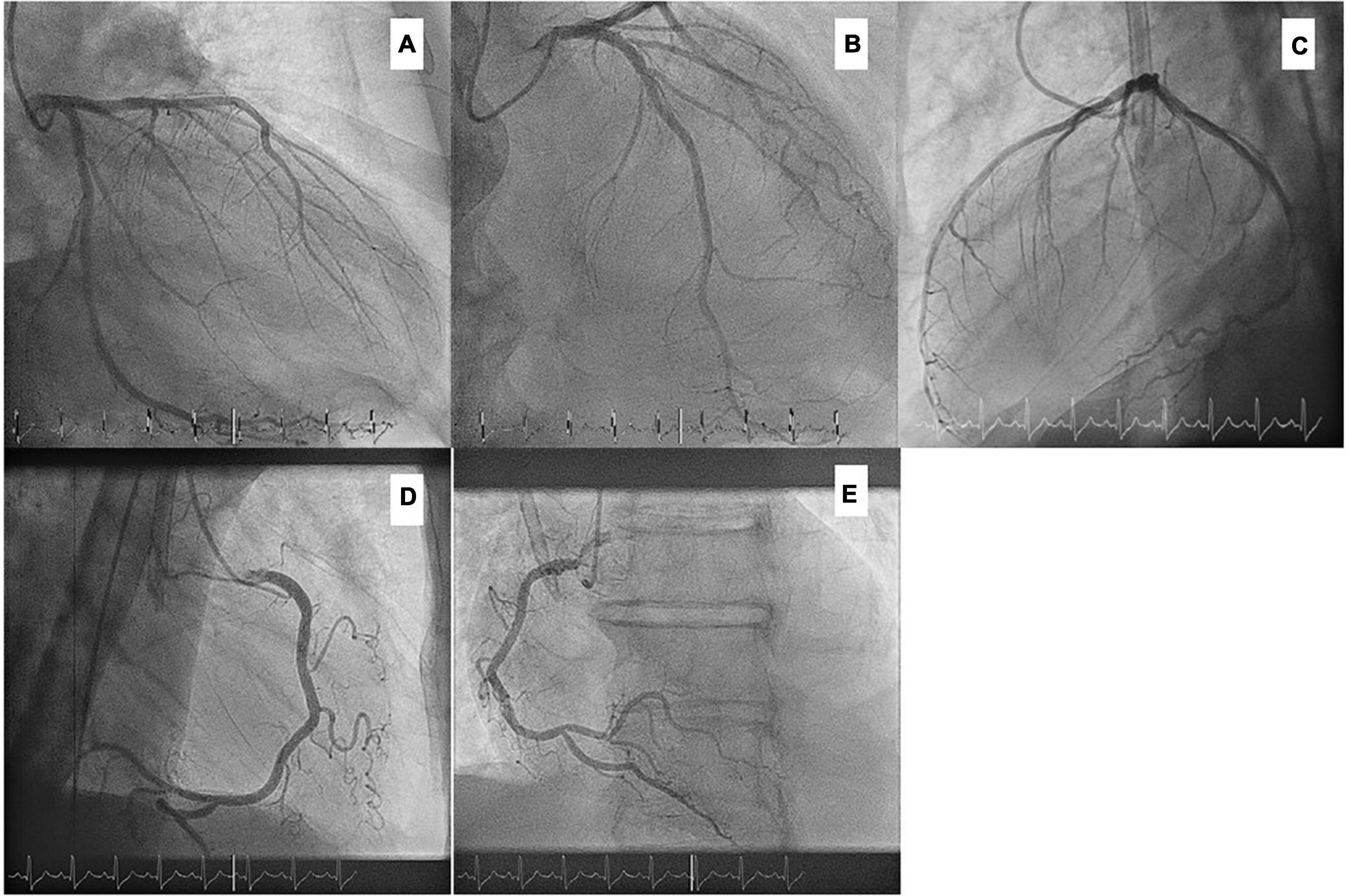
Figure 3. Coronary angiography without significant obstructive coronary artery disease. (A) cranial, 40° (B) RAO, 20°; caudal, 30° (C) LAO, 90° (D) RAO, 90° (E) LAO, 30°.
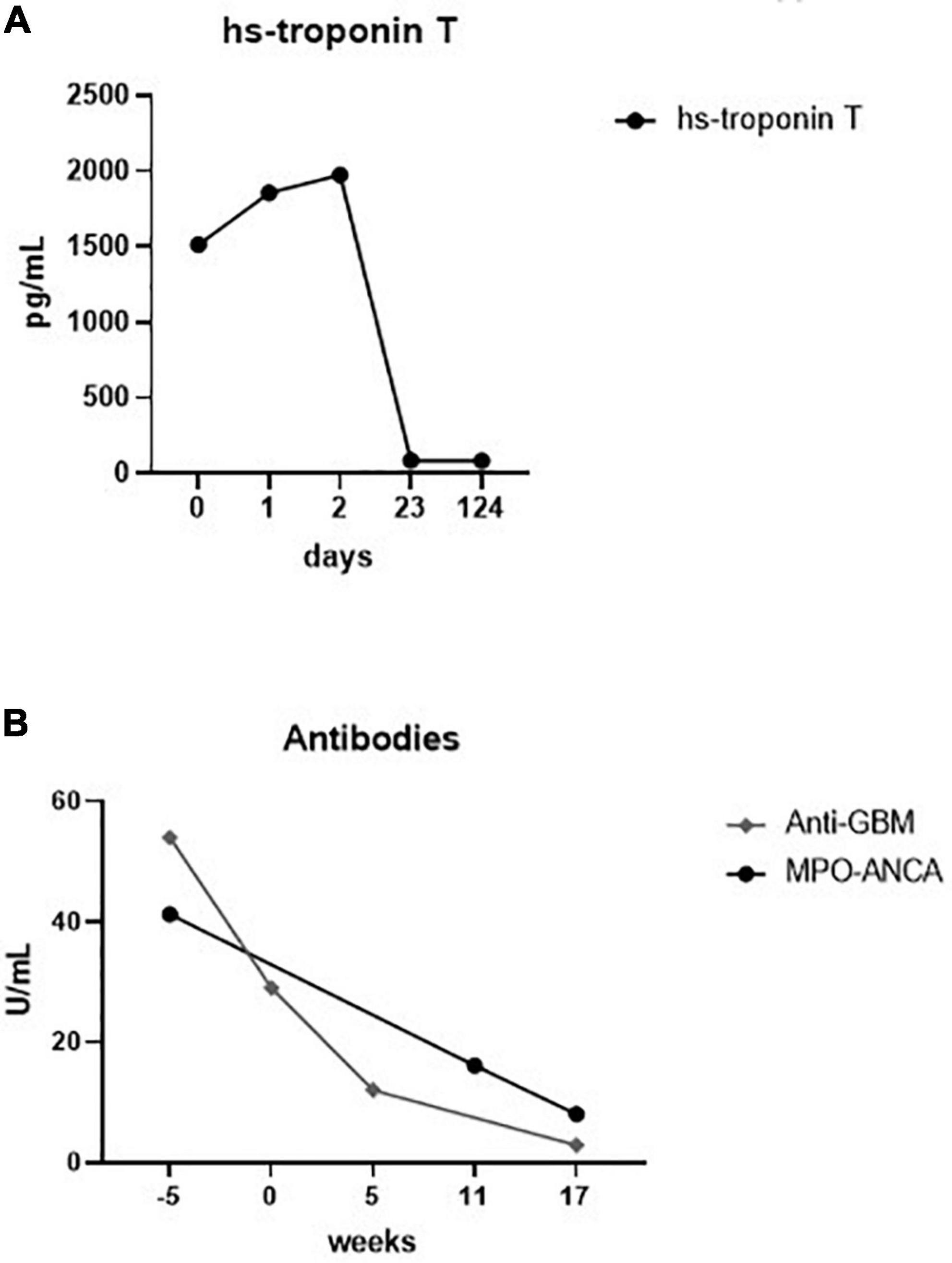
Figure 4. Laboratory charts of the time-dependent development of high-sensitive (hs) troponin T (A) and myeloperoxidase anti-neutrophil cytoplasm (MPO-ANCA) and anti-glomerular basement membrane (anti-GBM) antibodies (B). Zero on both scales indicates the time point of chest pain.
Double-positive disease is a life-threatening disorder characterized by small vessel vasculitis affecting the kidneys and the lungs with a coincidence of anti-GBM disease and AAV (11). Cardiac involvement is a known disease manifestation in AAV, predominantly in those with MPO-ANCA positivity, and associated with increased mortality (12). On the contrary, CV complications are rarely reported in patients with anti-GBM disease. Only one case of anti-GBM disease with cardiac involvement was reported in our literature review (13).
Myocardial infarction with non-obstructive coronary arteries represents a major health problem and is often misdiagnosed, leading to possible undertreatment (14). Patients with small-vessel vasculitis have a high CV event rate, even exceeding high-risk populations, such as those with chronic kidney disease (4). Recently, there has been an increasing interest to identify patients at risk since they have a higher risk of developing major cardiovascular events and being hospitalized due to heart failure or repeated CA (15–17). Adequate diagnosis is challenging; however, if clinical surrogate markers of myocardial ischemia without evidence of obstructive CAD are present, the diagnosis of MINOCA can be considered (18). Dilated cardiomyopathy as a possible cause of chest pain in our patient cannot be excluded entirely. However, he had typical angina pectoris with dynamic ischemic ECG changes and a high-serum level of hs-Tn (again, later falling despite chronic HD), while invasive angiography did not reveal coronary stenosis (≥50%). In accordance, the absence of myocarditis and tear on angiography also underlines the clinical diagnosis of MINOCA. Importantly, the use of CYC is a considerable risk factor in cardiotoxicity; however, its triggering minimum dose is not known. Registry data reveal an association between high-dose CYC (>36 g) and ischemic heart disease in patients with GPA (19).
A study by Pugnet et al. analyzed patients with GPA who underwent CMR (20). In patients, who had simultaneous CA with normal coronary findings, subendocardial late gadolinium enhancement (LGE) with perfusion defects, suggesting ischemic lesions possibly due to small vessel vasculitis, was seen. In our case, CMR showed no late enhancement, suggesting the absence of inflammation.
Mechanisms contributing to the development of MINOCA seem to be heterogeneous but characterized mainly by coronary vasospasm and microvascular dysfunction (14, 21). In our patient, invasive functional CA and pharmacological reactivity testing was not performed; thus, the contributing mechanism behind his symptoms remains unclear. Nevertheless, strong evidence on the association between coronary vascular dysfunction and small vessel disease exists (22). In patients with AAV, ANCA-activated neutrophils induce endothelial injury, which might lead to coronary vascular dysfunction and promote the induction of epicardial vessel spasm in predisposed coronary segments. In addition, the endothelial impairment resulting in altered vascular tone enhances smooth muscle contractility and might be responsible for myocardial ischemia via decreased coronary flow and perfusion pressure. Moreover, similar to patients with systemic lupus erythematosus, systemic inflammation in AAV patients might also contribute to coronary vasomotor abnormalities (23). A recent European multicenter study has found that patients with double-positive disease have a relapse rate comparable to patients with AAV alone, suggesting the importance of long-term follow-up and maintenance immunosuppressive therapy in this patient population (11). In our patient, a preexisting extrarenal vasculitis with continuous ANCA positivity might be a possible endogenous contributor responsible for his myocardial ischemia besides the predominant clinical phenotype of anti-GBM disease.
As coronary microvascular dysfunction might have a significant impact on the patients’ quality of life as well as a clinical outcome, sufficient therapeutic strategies are of particular interest (24, 25). Since – to our knowledge – no studies are published dealing with this entity in patients with AAV and/or double-positive ANCA/anti-GBM disease, it is unclear which medical treatment might be the most sufficient. Recent major guidelines issued by the leading cardiology societies have provided a guidance on various pharmacological treatment options of MINOCA related to the underlying mechanism (14, 26). Accordingly, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers might depict a useful option to reduce systemic inflammation and endothelial dysfunction (27). Calcium antagonists might be used in patients with evidence of either epicardial or microvascular spasm who underwent acetylcholine testing (14). As patients with AAV face increased CV risk even in the early phase of the disease, adequate lifestyle changes and rigorous CV risk management are of particular importance (28, 29).
There are some clear limitations to this presented case that merit notification. Invasive testing of coronary artery spasm and microvascular dysfunction, which might have provided direct evidence on some of the possible mechanisms of MINOCA, have not been performed in this case; therefore, MINOCA remains a “working diagnosis.” Also, certain underlying conditions, such as coronary thrombosis with a quick spontaneous lysis of the thrombus or uncontrolled blood pressure, cannot be fully excluded. Finally, our patient was on dialysis, and, thus, the contribution of prominent accumulation of uremic toxins over time as a specific trigger of microvascular dysfunction might also be occurred.
In summary, we report a case of a patient double-seropositive for anti-GBM and ANCA antibodies with extrarenal vasculitis who presented with MINOCA. Now, studies improving our understanding of underlying mechanisms associated with excessive CV mortality in AAV patients are essential. Coronary microvascular dysfunction or vasospastic angina due to endothelial injury and/or systemic inflammation might be a significant contributor of MINOCA in patients with AAV and/or double-positive disease, who can be at higher risk to develop this condition. Given the increased risk of adverse CV outcomes associated with AAV, this entity might be an important and reversible cause, which needs a multidisciplinary care approach and further exploration in addition to traditional CV risk factors.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Medical University of Graz. The patients/participants provided their written informed consent to participate in this case study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
MaK and BO wrote the first draft of the manuscript. JG described the coronary angiography and ECG. CR evaluated and interpreted the cardiac MRI findings. MP performed the histological work-up. MaK, AKi, AKr, KE, and AR contributed to the data acquisition and drafting of the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. McAdoo SP, Pusey CD. Anti-glomerular basement membrane disease. Clin J Am Soc Nephrol. (2017) 12:1162–72. doi: 10.2215/CJN.01380217
2. Kitching AR, Anders H-J, Basu N, Brouwer E, Gordon J, Jayne DR, et al. ANCA-associated vasculitis. Nat Rev Dis Primers. (2020) 6:71. doi: 10.1038/s41572-020-0204-y
3. Philip R, Dumont A, Martin Silva N, de Boysson H, Aouba A, Deshayes S. ANCA and anti-glomerular basement membrane double-positive patients: a systematic review of the literature. Autoimmun Rev. (2021) 20:102885. doi: 10.1016/j.autrev.2021.102885
4. Kronbichler A, Leierer J, Gauckler P, Shin JI. Comorbidities in ANCA-associated vasculitis. Rheumatology. (2020) 59:iii79–83. doi: 10.1093/rheumatology/kez617
5. Florian A, Slavich M, Blockmans D, Dymarkowski S, Bogaert J. Cardiac involvement in granulomatosis with polyangiitis (Wegener Granulomatosis). Circulation. (2011) 124:e342–4. doi: 10.1161/CIRCULATIONAHA.111.030809
6. Mathur K, Saini A, Bah T, Katikaneni P. Case report: acute ST elevation myocardial infarction in fulminant systemic p-ANCA vasculitis: a rare catastrophic complication. BMJ Case Rep. (2016) 2016:bcr2016215628. doi: 10.1136/bcr-2016-215628
7. Yoshida M, Nakaya I, Sakuma T, Soma J. Cardiac small vessel vasculitis in a case of microscopic polyangiitis. Intern Med. (2014) 53:2655–6. doi: 10.2169/internalmedicine.53.2556
8. Kim YK, Chekka P, Mysore M, Childress J, Alfaraidhy M, Thomas A, et al. Isolated antineutrophil cytoplasmic antibody-associated coronary vasculitis and valvulitis. JACC Case Rep. (2021) 3:309. doi: 10.1016/j.jaccas.2020.12.007
9. Cuminetti G, Regazzoni V, Vizzardi E, Bonadei I, de Jong MMJ, Lorusso R, et al. Cardiac ANCA-associated vasculitis mimicking an acute coronary syndrome. Int J Cardiol. (2016) 214:200–1. doi: 10.1016/j.ijcard.2016.03.117
10. Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation. J Am Coll Cardiol. (2018) 72:3158–76. doi: 10.1016/j.jacc.2018.09.072
11. McAdoo SP, Tanna A, Hrušková Z, Holm L, Weiner M, Arulkumaran N, et al. Patients double-seropositive for ANCA and anti-GBM antibodies have varied renal survival, frequency of relapse, and outcomes compared to single-seropositive patients. Kidney Int. (2017) 92:693. doi: 10.1016/j.kint.2017.03.014
12. Wallace ZS, Fu X, Harkness T, Stone JH, Zhang Y, Choi H. All-cause and cause-specific mortality in ANCA-associated vasculitis: overall and according to ANCA type. Rheumatology. (2020) 59:2308–15. doi: 10.1093/rheumatology/kez589
13. Solak Y, Selcuk NY, Polat I, Atalay H, Turkmen K. Dilated cardiomyopathy in a patient with antibody-negative Goodpasture’s syndrome and pulmonary relapse. Saudi J Kidney Dis Transpl. (2010) 21:332.
14. Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas AHEM, et al. An EAPCI expert consensus document on ischaemia with non-obstructive coronary arteries in collaboration with European society of cardiology working group on coronary pathophysiology & microcirculation endorsed by coronary vasomotor disorders international study group. Eur Heart J. (2020) 41:3504. doi: 10.1093/eurheartj/ehaa503
15. Radico F, Zimarino M, Fulgenzi F, Ricci F, Di Nicola M, Jespersen L, et al. Determinants of long-term clinical outcomes in patients with angina but without obstructive coronary artery disease: a systematic review and meta-analysis. Eur Heart J. (2018) 39:2135–46. doi: 10.1093/eurheartj/ehy185
16. Shimokawa H, Suda A, Takahashi J, Berry C, Camici PG, Crea F, et al. Clinical characteristics and prognosis of patients with microvascular angina: an international and prospective cohort study by the Coronary Vasomotor Disorders International Study (COVADIS) Group. Eur Heart J. (2021) 42:4592–600. doi: 10.1093/eurheartj/ehab282
17. Jespersen L, Abildstrom SZ, Hvelplund A, Madsen JK, Galatius S, Pedersen F, et al. Burden of hospital admission and repeat angiography in angina pectoris patients with and without coronary artery disease: a registry-based cohort study. PLoS One. (2014) 9:e93170. doi: 10.1371/journal.pone.0093170
18. Beltrame JF, Tavella R, Jones D, Zeitz C. Management of ischaemia with non-obstructive coronary arteries (INOCA). BMJ. (2021) 375:e060602. doi: 10.1136/bmj-2021-060602
19. Faurschou M, Mellemkjaer L, Sorensen IJ, Svalgaard Thomsen B, Dreyer L, Baslund B. Increased morbidity from ischemic heart disease in patients with Wegener’s granulomatosis. Arthritis Rheum. (2009) 60:1187–92. doi: 10.1002/art.24386
20. Pugnet G, Gouya H, Puéchal X, Terrier B, Kahan A, Legmann P, et al. Cardiac involvement in granulomatosis with polyangiitis: a magnetic resonance imaging study of 31 consecutive patients. Rheumatology. (2017) 56:947–56. doi: 10.1093/rheumatology/kew490
21. Del Buono MG, Montone RA, Camilli M, Carbone S, Narula J, Lavie CJ, et al. Coronary microvascular dysfunction across the spectrum of cardiovascular diseases. J Am Coll Cardiol. (2021) 78:1352–71. doi: 10.1016/j.jacc.2021.07.042
22. Ford TJ, Rocchiccioli P, Good R, McEntegart M, Eteiba H, Watkins S, et al. Systemic microvascular dysfunction in microvascular and vasospastic angina. Eur Heart J. (2018) 39:4086. doi: 10.1093/eurheartj/ehy529
23. Weber BN, Stevens E, Barrett L, Bay C, Sinnette C, Brown JM, et al. Coronary Microvascular Dysfunction in Systemic Lupus Erythematosus. J Am Heart Assoc. (2021) 10:e018555. doi: 10.1161/JAHA.120.018555
24. Sucato V, Novo G, Saladino A, Rubino M, Caronna N, Luparelli M, et al. Ischemia in patients with no obstructive coronary artery disease: classification, diagnosis and treatment of coronary microvascular dysfunction. Coron Artery Dis. (2020) 31:472–6. doi: 10.1097/MCA.0000000000000855
25. Bajaj NS, Singh A, Zhou W, Gupta A, Fujikura K, Byrne C, et al. Coronary microvascular dysfunction, left ventricular remodeling, and clinical outcomes in patients with chronic kidney impairment. Circulation. (2020) 141:21–33. doi: 10.1161/CIRCULATIONAHA.119.043916
26. Tamis-Holland JE, Jneid H, Reynolds HR, Agewall S, Brilakis ES, Brown TM, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American heart association. Circulation. (2019) 139:e891–908. doi: 10.1161/CIR.0000000000000670
27. Ruilope LM, Redón J, Schmieder R. Cardiovascular risk reduction by reversing endothelial dysfunction:ARBs, ACE inhibitors, or both? Expectations from the ONTARGET trial programme. Vasc Health Risk Manag. (2007) 3:1–9.
28. Massicotte-Azarniouch D, Petrcich W, Walsh M, Canney M, Hundemer GL, Milman N, et al. Association of anti-neutrophil cytoplasmic antibody-associated vasculitis and cardiovascular events: a population-based cohort study. Clin Kidney J. (2022) 15:681. doi: 10.1093/ckj/sfab229
Keywords: MINOCA, ANCA, anti-GBM, double-positive, coronary, therapy
Citation: Krall M, Gollmer J, Pollheimer MJ, Reiter C, Kolland M, Kirsch AH, Kronbichler A, Eller K, Rosenkranz AR and Odler B (2022) Myocardial infarction with non-obstructive coronary arteries in a patient double-seropositive for anti-glomerular basement membrane and anti-neutrophil cytoplasmic antibodies: A case report. Front. Cardiovasc. Med. 9:893742. doi: 10.3389/fcvm.2022.893742
Received: 28 March 2022; Accepted: 02 August 2022;
Published: 23 September 2022.
Edited by:
Junjie Xiao, Shanghai University, ChinaReviewed by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyCopyright © 2022 Krall, Gollmer, Pollheimer, Reiter, Kolland, Kirsch, Kronbichler, Eller, Rosenkranz and Odler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Balazs Odler, YmFsYXpzLm9kbGVyQG1lZHVuaWdyYXouYXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.