- 1Student Research Committee, Semnan University of Medical Sciences, Semnan, Iran
- 2Department of Medical Informatics, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
- 3Student Research Committee, Afzalipour Faculty of Medicine Kerman University of Medical Sciences, Kerman, Iran
- 4Student Research Committee, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
- 5Faculty of Medicine, Shahed University, Tehran, Iran
- 6Student Research Committee, Department of Midwifery, Faculty of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 7Student Research Committee, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
- 8Student Research Committee, School of Dentistry, Kermanshah University of Medical Sciences, Kermanshah, Iran
- 9School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
- 10Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
- 11Students Research Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Background: Hypertensive disorders of pregnancy (HDP), including chronic hypertension, preeclampsia and gestational hypertension, is the cause of about 50,000 deaths out of 400,000 perinatal deaths. HDP is an effective risk factor in stroke, type 2 diabetes, and cardiovascular diseases like ischemic heart disease. There is a significant relation between HDP, lifestyle, and knowledge. Unfortunately, many studies showed that pregnant women have lack of knowledge about HDP. Therefore, the importance of educational interventions is, today, more acknowledged than before.
Aim: The goal of this systematic review was to investigate the effect of interventional educations on the knowledge of pregnant women about HDP.
Methods: A systematic review of the related articles was conducted. We included English randomized controlled trials published up to December 2021, including pregnant women as population, HDP as the outcome, and educational interventions as the intervention.
Results: After the process of study selection, six articles containing 819 pregnant women were included in this study. Educational pamphlets, mobile-based application, a mixture of pamphlets, pictographic magnet and videos, and a combination of PowerPoint and data show projectors and conversation were the educational interventions in these studies.
Conclusions: The positive effects of educational interventions on the knowledge of women with HTP were observed in all studies. The higher knowledge leads to HDP-related complications.
Systematic Review Registration: https://archive.org/details/osf-registrations-gcs5r-v1, identifier: doi: 10.17605/OSF.IO/GCS5R.
Introduction
Hypertensive disorders of pregnancy (HDP) is observed in 5–10% of pregnant women worldwide (1). Chronic hypertension, preeclampsia, and gestational hypertension are the three types of HDP. Chronic hypertension, as a hypertension diagnosed before pregnancy or before the 20th week of pregnancy, may convert to preeclampsia. Gestational hypertension, occurred after 20 weeks of pregnancy, can also lead to preeclampsia (2). Preeclampsia is a hypertensive disorder characterized by proteinuria and the onset of hypertension beginning after 20 weeks of pregnancy (3). More than 50,000 deaths of mothers and 400,000 of perinatal deaths happen because of HDP, specially preeclampsia, each year (4, 5). The incidence of stroke and ischemic heart disease in women with preeclampsia is about 2.5 times higher than normal pregnancies (6, 7). The risks of renal disease and type 2 diabetes are also elevated by preeclampsia (8). In addition to preeclampsia, gestational hypertension and chronic hypertension are also long-term risk factors in cardiovascular disease (9). Nowadays, some screening programs are performed all over the world for the identification of women with the signs of preeclampsia. Cooperation of the women is one of the most important factors in the success of these programs. The cooperation is associated with the knowledge and the level of education of pregnant women (10, 11). Many studies found out that pregnant women had poor knowledge about increased cardiovascular risks after HDP (12). Pregnant women often do not participate in the programs for life-style changing because of low amount of knowledge, lack of suitable follow-up, and, also, the higher price of healthier food (13–15). Studies indicated that poor education levels of pregnant women led to dangerous conditions like pre-mature delivery or death of neonates (16). Researchers indicated that women were assessed for their cardiovascular disease less than men or the assessment was generally performed after the diagnosis among them (17). This makes the importance of knowledge of pregnant women about HDP more than before. The patient's knowledge plays an important role in preventing risk factors like cardiovascular disease, monitoring blood pressure, and helping the patient to know about the condition of severity of the disease, symptoms, and the management of them by a good lifestyle, including appropriate diet and lifestyle modifications (18). As noted, due to the importance of increasing the levels of education among pregnant women about HDP, different educational interventions were used in studies. Mobile-based applications, graphics-based educational tools, and pictorial cards are some of the examples (19–21). As far as we know, there are no presently available systematic reviews on the impact of educational interventions on knowledge of pregnant women about HDP. This review can help the medical staff and pregnant women for better choice of educational interventions to better manage HDP.
Methods
This systematic review study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA2020) Statement (22). In accordance with the PICO criteria, the “participants” were exclusive to pregnant women; the types of “intervention” covered were educational interventions; the “comparator” was not determined; and the “outcome” was knowledge about HDP. This review has been registered on The Open Science Framework (OSF) (Registration doi: 10.17605/OSF.IO/GCS5R available at https://archive.org/details/osf-registrations-gcs5r-v1).
Search Strategy
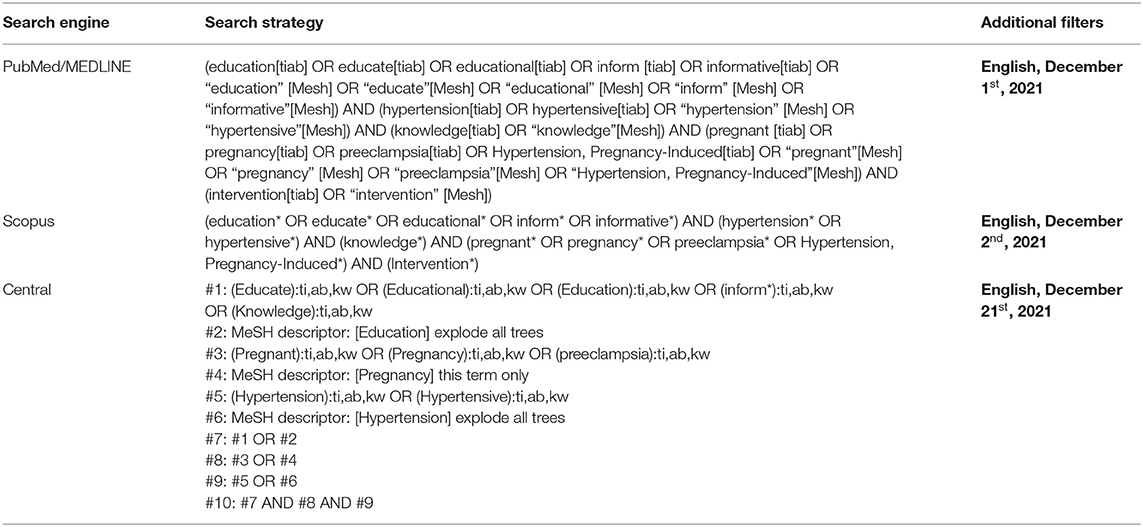
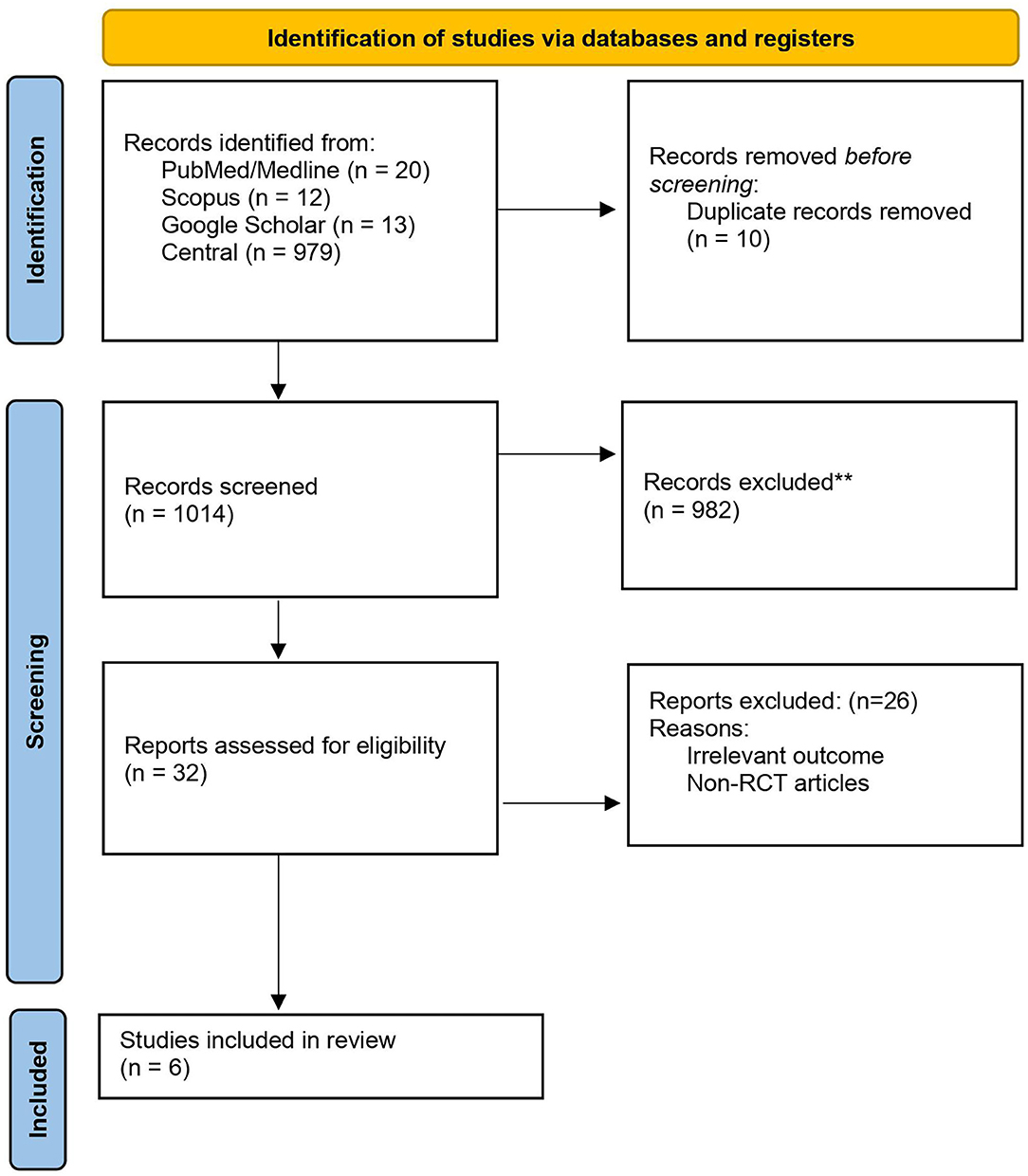
We identified original RCTs through searching for English language articles published up to December 2021 in PubMed/MEDLINE, Scopus, Google Scholar, and Cochrane Central Register of Controlled Trials (CENTRAL) databases. Additionally, the duplicate records were removed using EndNote (v.7, Thomson Reuters, Toronto, Canada). Two reviewers (MD and KGh) developed the search strategy as followed: (“hypertension*” OR “hypertensive” OR “hypertensive disorders”) AND (“education*” OR “inform*” OR “knowledge”) AND (“pregnancy” OR “pregnant”). Table 1 shows the search strategies for PubMed/Medline, Scopus, and central databases. We also screened the references of relevant studies to identify eligible studies. The PRISMA flow diagram is available in Figure 1.
Inclusion Criteria
All primary research studies that found the following PICOS criteria were included for review if:
(A) Population: pregnant women (P);
(B) Interventions: educational intervention (I);
(C) The control group: standard care or forfeiture of any intervention; if there was no control group (C);
(D) Type of the primary outcome: hypertensive disorders of pregnancy (O);
(E) Type of study design: English language RCTs (S).
Data Screening and Extraction
Two reviewers (ShK and AJA) assessed and screened titles and abstracts to recognize related studies using a form developed by the research team. Full texts of studies were retrieved for “Yes” and “Maybe” assessment for eligibility study. We resolved discrepancies and disagreement by consensus. Data extraction was completed by two independent assessors (MS and HGh). Discrepancies were resolved by consensus and discussion between two reviewers.
Quality Assessment of Included Studies
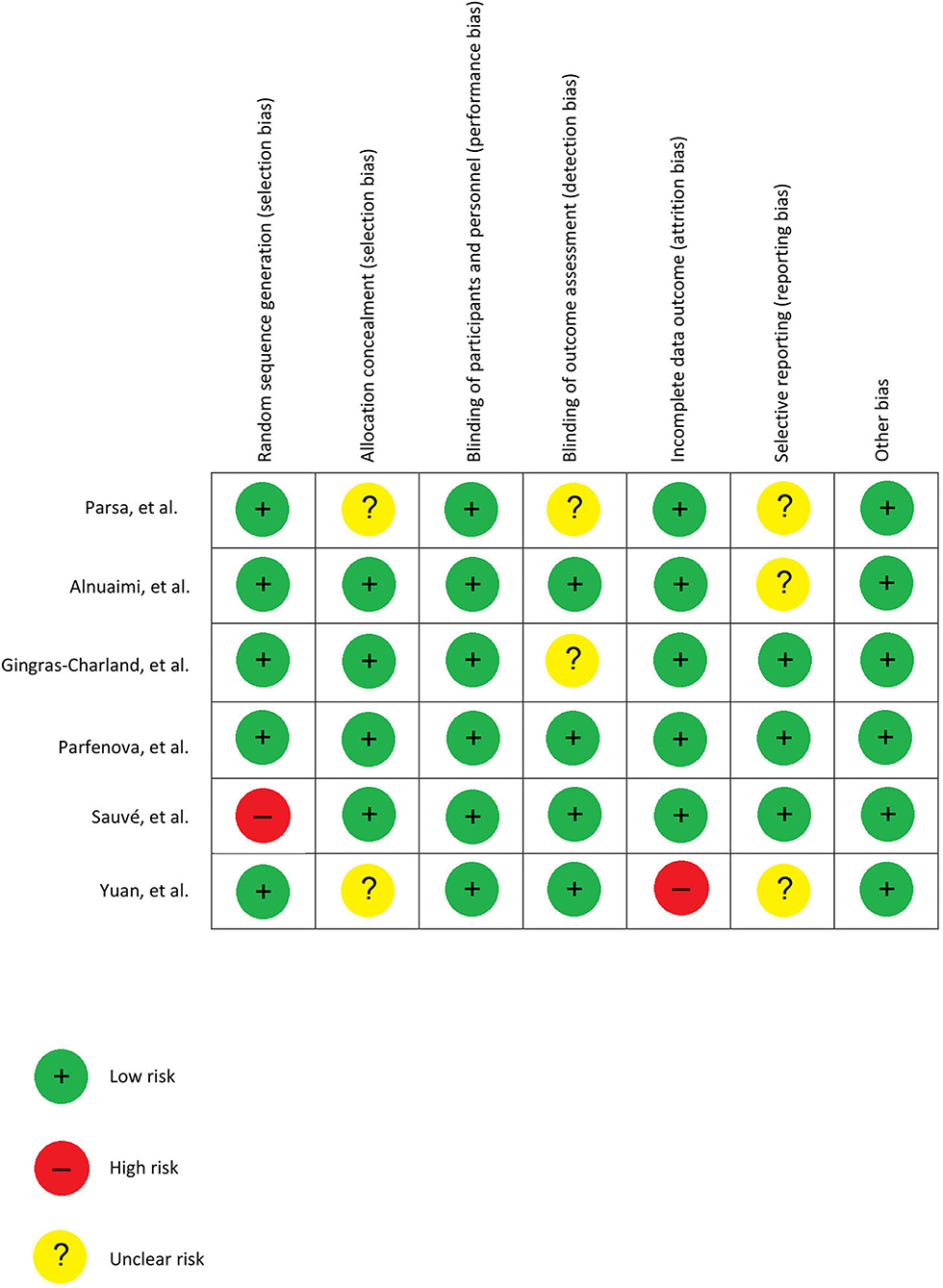
For each study, two assessors (YS and KGh) independently assessed all included studies according to the Cochrane risk of bias tool (23). The Cochrane risk of bias tool is a standard and common tool that includes all the essential questions to determine and judge the methodological quality and the risk of bias focusing on 6 domains, including sequence generation, allocation concealment, blinding, in-complete data, and selective reporting, and other bias and disagreement were resolved by consensus and discussion via two assessors (Figure 2).
Results
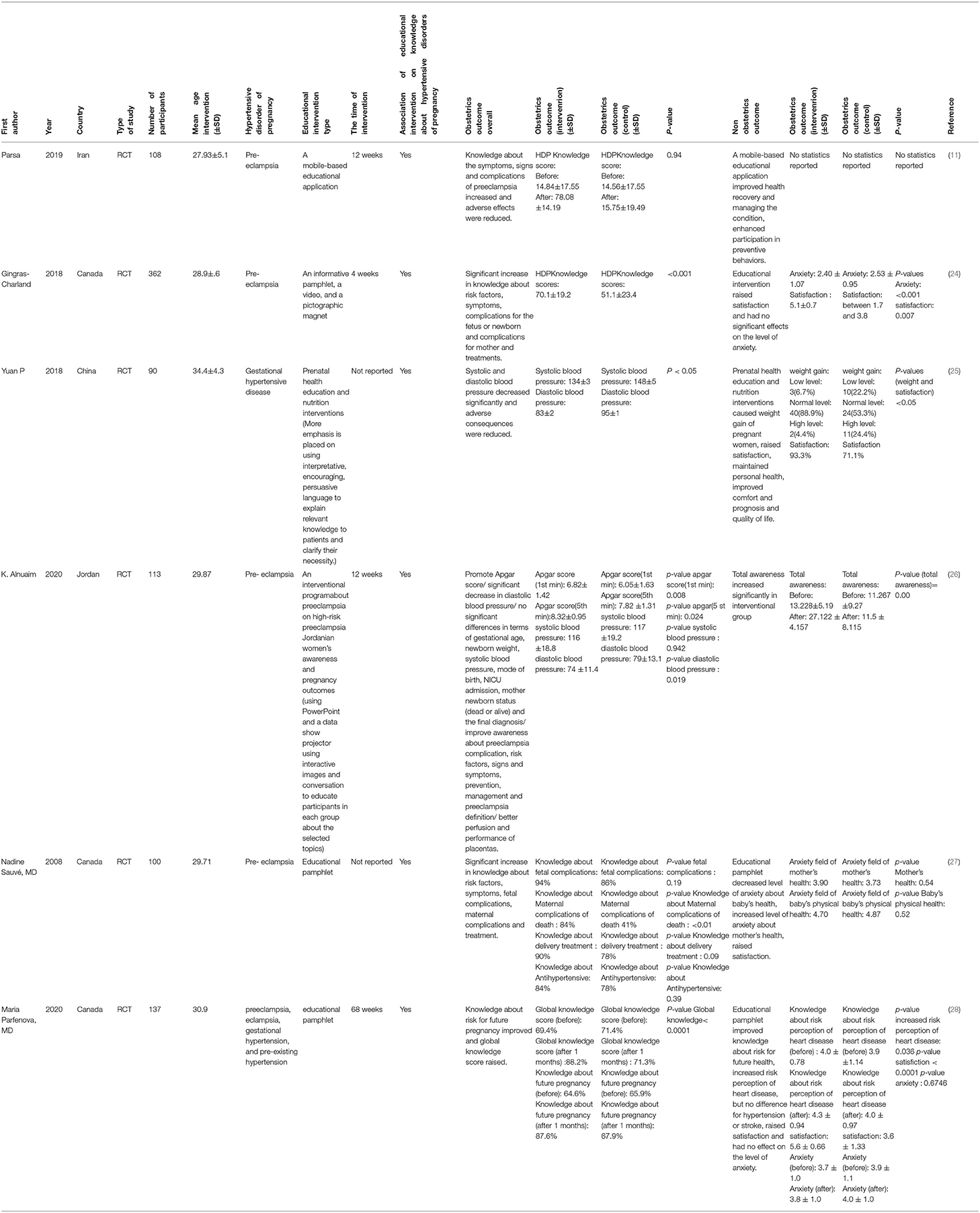
Through the process of selection, six articles were included in this study; the summary of the findings of included studies is summarized in Table 2. All of the included studies were randomized clinical trials. Three of the studies were performed in Canada. The other studies were conducted in Iran, Jordan, and China. These studies investigated the effect of educational interventions on some obstetrics and non-obstetrics outcomes, such as knowledge, Apgar score, systolic blood pressure (SBP), diastolic blood pressure (DBP), satisfaction, awareness, weight gain, and anxiety about hypertensive disorders of pregnancy (including pre-eclampsia and gestational hypertensive disease) among 910 pregnant women. The most frequent disorder was pre-eclampsia. Various educational intervention tools were used for assessment of efficacy of education in the included studies: educational pamphlets (27, 28), mobile-based educational application (11), a combination of pamphlets, pictographic magnet, and videos (24), prenatal health education and nutrition interventions (29), and a mixture of PowerPoint, as well as data, show projectors and conversation (26) were used for the purpose of education (Table 2). All studies reported a positive impact of educational interventions on the hypertensive disorders of pregnancy. Not only the educational interventions improved the obstetrics outcomes, but also the non-obstetric parameters were affected by them. Overall, the significant higher knowledge score (24, 26), greater levels of decreased DBP (26, 28), reduced SBP (28), the higher Apgar score (26) and satisfaction (26, 28), and more awareness about HDP complications (26) were observed in the included studies (The p-value of the mentioned outcomes was reported <0.05 in the articles).
Discussion
The present study reviewed research on the effect of educational intervention on pregnant women's knowledge about HDP (including chronic hypertension, preeclampsia, and gestational hypertension). All included studies showed that providing training related to HDP is effective in increasing pregnant women's knowledge about the disease. Accordingly, providing educational interventions through various methods, including mobile applications (11), pamphlets (24, 27, 28), face-to-face training approaches (25, 26), and a combination of different training methods, increases the knowledge of pregnant women in this regard.
The low mean score of pre-eclampsia knowledge before the educational intervention indicates a very poor perception of possible risks of elevated hypertension by pregnant mothers (11). So, increasing relevant knowledge results in early awareness about the signs and symptoms leading to timely referral to physicians which, in turn, followed by suitable care and treatment, which totally provide healthier outcomes for both mothers and babies (30). Evenly, this kind of intervention was considered as the fundamental element for the recovery of maternal hypertension, which prepares the healthy conditions for pregnant women (25).
A graphitic educational tool increased the knowledge of pre-eclampsia 8 and 22% compared with standard pamphlets and peers with no education, respectively (21). However, the impact of a mobile-based educational application on the knowledge of the subjects was considerably higher (11). This increased growth in the level of knowledge that is related to the type of educational intervention. Widespread use of smartphones, along with the ease of access to a variety of information through different applications, improves the process of training. Also, this approach is effective in maintaining the individuals' health, controlling the related condition, and preventing risky behaviors (31).
An educational program on pre-eclampsia increased the awareness of high-risk women significantly, which is reflected in improving certain pregnancy outcomes like Apgar scores and mean diastolic blood pressure. Intriguingly, self-monitoring, which is represented in adherence to the provided information and recommendations, was also increased upon improving awareness on pre-eclampsia. For instance, informed mothers control their mean diastolic blood pressure with more caution compared with those without educational intervention (26). In order to guarantee adherence and commitment of patients to a self-monitoring process, an educational program preferably includes physicians, obstetricians, and other health care providers (26).
Studies have shown that raising awareness is strongly associated with early detection of pregnancy risks, which, in turn, can prevent dangerous complications (21, 30). In a study from Ethiopia, Wassihun et al. (31) found that mothers who participated in antenatal care were 1.26 times more likely to be aware of the symptoms of labor risk than those who were not. It was also found that the participants who gave birth in specialized health centers were 3.57 times more aware of the danger signs of childbirth than those who had labor at home, which is mainly due to the information given by the medical staff. Another study in Australia also supported that increasing the coverage of prenatal care and the education level of women elevates mothers' knowledge about the symptoms of childbirth risks. In another study, it was observed that the level of awareness was significantly associated with age, the level of education, employment status, and monthly household income of pregnant women (28). Therefore, the importance of raising awareness in pregnant women has been indicated previously, and the need for interventions to increase awareness is, today, felt more than ever.
Parsa et al. used a mobile application to educate pregnant women on pre-eclampsia. The results of this study emphasized the positive and significant effect of educational interventions on pregnant women's awareness about the symptoms of preeclampsia. This would reduce the risk of further serious complications of preeclampsia. Other studies also showed increased awareness of pregnant women undergoing educational intervention in the field of preeclampsia and gestational hypertensive disease (24–26, 29).
While education increases the ability of women to recognize pre-eclampsia and prevent related complications, being more informed is not associated with anxiety exacerbation (24). Pregnant women were very satisfied with receiving a pamphlet containing information on lethal potential of pre-eclampsia because their knowledge was increased without worsening the anxiety during the critical period of pregnancy (27). An HDP pamphlet developed patients' knowledge about future risks of health and pregnancy in a population of women with recent HDP diagnosis with the anxiety level remained unchanged. This knowledge that lasted at least for 1 month also elevated the perception of long-term heart disease. The authors concluded that lifestyle behavior is changed toward decreasing cardiovascular risk in this way (28).
It has been previously shown that maternal knowledge and awareness strongly affect the health of the child, which can be partly attributed to differences in prenatal care and reduction of adverse delivery outcomes (32). It is better to initiate educational programs as early as possible in pregnant women, and it should maintain for at least 3 months after partum (26). Different studies have investigated the effects of educational programs on pregnant women with different characteristics. Pregnant women of 20 to 32 weeks were recruited for receiving an educational tool in one study (24). Another study included postpartum women between 4 weeks and 18 months for educational intervention (28). A sample of 100 pregnant women who were hospitalized for suspected or proven pre-eclampsia was studied in the other study (27). In some studies, the duration of intervention was a 1-month period (11), whereas a 2-h educational session on pre-eclampsia was given to high-risk pregnant women in another study (26). With the implementation of educational programs, the health status of mothers and their babies are improved due to appropriate actions. This shows the importance of educational programs to reduce the risks and complications around pregnancy (26). However, some hurdles are identified that hamper effective use of health information during pregnancy, such as mistrust between patients and health care providers, and lack of suitable communication between them due to bad attitude of the latter (33).
One important strength of the present study is that it is the first systematic review on the effect of educational intervention on knowledge of pregnant women's knowledge about HDP. However, since the studies were conducted in three Asian countries and Canada, it is not possible to generalize the results to other populations and ethnicities.
Conclusion
Altogether, the included studies showed that educational intervention strategies have a positive and significant impact on increasing the awareness of pregnant women about hypertensive disorders of pregnancy, which may help to reduce the severe complications caused by the disease. Future RCTs may compare the impact of various types of educational interventions on pregnant women.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
KG and MD performed the search. AA and SK performed first screening. MS and HG performed second screening. KG and YS evaluated risk of bias. NN and MK drafted the manuscript. AK and SH revised the manuscript. ND designed, critically revised, and supervised the course of drafting the article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The protocol of this systematic review is available at https://archive.org/details/osf-registrations-gcs5r-v1.
References
1. Payne BA, Hanson C, Sharma S, Magee LA, von Dadelszen P. Epidemiology of the hypertensive disorders of pregnancy. In: Magee LA, von Dadelszen P, Stones W, editors. The International Federation of Gynaecology and Obstetrics Textbook of Pregnancy Hypertension. London: Global Lib Wom Med (2016). p. 63–74.
2. Lowe SA, Bowyer L, Lust K, McMahon LP, Morton M, North RA, et al. SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust N Z J Obstet Gynaecol. (2015) 55:e1–29. doi: 10.1111/ajo.12399
3. Nirupama R, Divyashree S, Janhavi P, Muthukumar S, Ravindra P. Preeclampsia: Pathophysiology and management. J Gynecol Obst Human Reprod. (2021) 50:101975. doi: 10.1016/j.jogoh.2020.101975
4. Duley L, editor The global impact of pre-eclampsia and eclampsia. Seminars in Perinatology. (2009): Elsevier. doi: 10.1053/j.semperi.2009.02.010
5. Ghulmiyyah L, Sibai B, editors. Maternal mortality from preeclampsia/eclampsia. Seminars in Perinatology. (2012): Elsevier. doi: 10.1053/j.semperi.2011.09.011
6. McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. (2008) 156:918–30. doi: 10.1016/j.ahj.2008.06.042
7. Roth H, Henry A, Roberts L, Hanley L, Homer CS. Exploring education preferences of Australian women regarding long-term health after hypertensive disorders of pregnancy: a qualitative perspective. BMC Women's Health. (2021) 21:1–9. doi: 10.1186/s12905-021-01524-w
8. Giorgione V, Ridder A, Kalafat E, Khalil A, Thilaganathan B. Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis. BJOG: Int J Obst Gynaecol. (2021) 128:495–503. doi: 10.1111/1471-0528.16545
9. Riise HKR, Sulo G, Tell GS, Igland J, Nygård O, Iversen AC, et al. Association between gestational hypertension and risk of cardiovascular disease among 617 589 Norwegian women. J Am Heart Assoc. (2018) 7:e008337. doi: 10.1161/JAHA.117.008337
10. Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. Screening for preeclampsia: US preventive services task force recommendation statement. Jama. (2017) 317:1661–7. doi: 10.1001/jama.2017.3439
11. Parsa S, Khajouei R, Baneshi MR, Aali BS. Improving the knowledge of pregnant women using a pre-eclampsia app: a controlled before and after study. Int J Med Inform. (2019) 125:86–90. doi: 10.1016/j.ijmedinf.2019.03.001
12. Roth H, LeMarquand G, Henry A, Homer C. Assessing knowledge gaps of women and healthcare providers concerning cardiovascular risk after hypertensive disorders of pregnancy—A scoping review. Front Cardiovasc Med. (2019) 6:178. doi: 10.3389/fcvm.2019.00178
13. Brown M, Bell R, Collins C, Waring G, Robson S, Waugh J, et al. Women's perception of future risk following pregnancies complicated by preeclampsia. Hyperten Preg. (2013) 32:60–73. doi: 10.3109/10641955.2012.704108
14. Hoedjes M, Berks D, Vogel I, Franx A, Duvekot JJ, Oenema A, et al. Motivators and barriers to a healthy postpartum lifestyle in women at increased cardiovascular and metabolic risk: a focus-group study. Hyperten Preg. (2012) 31:147–55. doi: 10.3109/10641955.2010.544803
15. Seely EW, Rich-Edwards J, Lui J, Nicklas JM, Saxena A, Tsigas E, et al. Risk of future cardiovascular disease in women with prior preeclampsia: a focus group study. BMC Pregy Childbirth. (2013) 13:1–7. doi: 10.1186/1471-2393-13-240
16. Ogunyemi D, Benae J-L, Ukatu C. Is eclampsia preventable? A case control review of consecutive cases from an urban underserved region. Southern Med J. (2004) 97:440–6. doi: 10.1097/00007611-200405000-00005
17. Hyun KK, Redfern J, Patel A, Peiris D, Brieger D, Sullivan D, et al. Gender inequalities in cardiovascular risk factor assessment and management in primary healthcare. Heart. (2017) 103:492–8. doi: 10.1136/heartjnl-2016-310216
18. Sakthi S, Thomas S, Sivakumar K, Karhikeyan J, Saravana Kumar N. Assessment of antihypertensive prescribing pattern and patient counseling in an urban population. Der Pharmacia Lettre. (2010) 2:156–63. doi: 10.1136/adc.45.239.13
19. Lupton D, Pedersen S. An Australian survey of women's use of pregnancy and parenting apps. Women Birth. (2016) 29:368–75. doi: 10.1016/j.wombi.2016.01.008
20. Willcox JC, van der Pligt P, Ball K, Wilkinson SA, Lappas M, McCarthy EA, et al. Views of women and health professionals on mHealth lifestyle interventions in pregnancy: a qualitative investigation. JMIR mHealth uHealth. (2015) 3:e4869. doi: 10.2196/mhealth.4869
21. You WB, Wolf MS, Bailey SC, Grobman WA. Improving patient understanding of preeclampsia: a randomized controlled trial. Am J Obst Gynecol. (2012) 206:431. doi: 10.1016/j.ajog.2012.03.006
22. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
23. Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane (2021).
24. Gingras-Charland M-E, Côté A-M, Girard P, Grenier A, Pasquier J-C, Sauvé N. Pre-eclampsia educational tool impact on knowledge, anxiety, and satisfaction in pregnant women: a randomized trial. J Obst Gynaecol Canada. (2019) 41:960–70. doi: 10.1016/j.jogc.2018.10.003
25. Yuan P, Yang Y, Ruizhi L, editors. Application of Prenatal Health Education and Nutrition Intervention in Patients with Pregnancy-induced Hypertension. Proceedings of the 8th International Conference on Education, Management, Information and Management Society (EMIM 2018). (2018): Atlantis Press.
26. Alnuaimi K, Abuidhail J, Abuzaid H. The effects of an educational programme about preeclampsia on women's awareness: a randomised control trial. Int Nurs Rev. (2020) 67:501–11. doi: 10.1111/inr.12626
27. Sauvé N, Powrie RO, Larson L, Phipps MG, Weitzen S, Fitzpatrick D, et al. The impact of an educational pamphlet on knowledge and anxiety in women with preeclampsia. Obst Med. (2008) 1:11–7. doi: 10.1258/om.2008.070001
28. Parfenova M, Côté A-M, Cumyn A, Pesant M-H, Champagne M, Roy-Lacroix M-È, et al. Impact of an educational pamphlet on knowledge about health risks after hypertensive disorders of pregnancy: a randomized trial. J Obst Gynaecol Canada. (2021) 43:182–90. doi: 10.1016/j.jogc.2020.07.008
29. Pan Y, Yu Y, Liu R, editors. Application of Prenatal Health Education and Nutrition Intervention in Patients with Pregnancy-induced Hypertension. 8th International Conference on Education, Management, Information and Management Society (EMIM 2018). (2018): Atlantis Press. doi: 10.2991/emim-18.2018.4
30. Wallis AB, Tsigas EZ, Saftlas AF. Sibai BMJTJoM-F, Medicine N. Prenatal education is an opportunity for improved outcomes in hypertensive disorders of pregnancy: results from an Internet-based survey. J Matern Fetal Neonatal Med. (2013) 26:1565–7. doi: 10.3109/14767058.2013.797403
31. Whitehead L, Seaton PJ. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res. (2016) 18:e4883. doi: 10.2196/jmir.4883
32. Maxwell S, Brameld K, Bower C, Dickinson JE, Goldblatt J, Hadlow N, et al. Socio-demographic disparities in the uptake of prenatal screening and diagnosis in Western Australia. Au N Z J Obstet Gynaecol. (2011) 51:9–16. doi: 10.1111/j.1479-828X.2010.01250.x
Keywords: hypertensive disorders of pregnancy, preeclampsia, education, hypertension, pregnancy
Citation: Gholami K, Norouzkhani N, Kargar M, Ghasemirad H, Ashtiani AJ, Kiani S, Sajedi Far M, Dianati M, Salimi Y, Khalaji A, Honari S and Deravi N (2022) Impact of Educational Interventions on Knowledge About Hypertensive Disorders of Pregnancy Among Pregnant Women: A Systematic Review. Front. Cardiovasc. Med. 9:886679. doi: 10.3389/fcvm.2022.886679
Received: 28 February 2022; Accepted: 19 May 2022;
Published: 20 June 2022.
Edited by:
Avash Das, University of Texas Southwestern Medical Center, United StatesReviewed by:
Stefania Triunfo, University of Milan, ItalyPolina Popova, Almazov National Medical Research Centre, Russia
Copyright © 2022 Gholami, Norouzkhani, Kargar, Ghasemirad, Ashtiani, Kiani, Sajedi Far, Dianati, Salimi, Khalaji, Honari and Deravi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Niloofar Deravi, bmlsb29mYXJkZXJhdmlAc2JtdS5hYy5pcg==
†These authors have contributed equally to this work
 Kosar Gholami1†
Kosar Gholami1† Narges Norouzkhani
Narges Norouzkhani Hamidreza Ghasemirad
Hamidreza Ghasemirad Niloofar Deravi
Niloofar Deravi