- Cardiovascular Division, University of Nebraska Medical Center, Omaha, NE, United States
Coronary angiography has been the gold standard for assessment of coronary artery disease (CAD) and guidance for percutaneous coronary interventions (PCI). Physiology–guided PCI has shown increased safety and efficacy, improved resource utilization, and better clinical outcomes in patients with stable angina and acute coronary syndromes. The three cases presented and discussed in this report illustrate the strengths and weaknesses of the available invasive and non-invasive methods for the physiological assessment of CAD. As technology evolves, invasive non-wire-based (angiography-derived FFR) and non-invasive (FFRCT) modalities for the hemodynamic assessment of CAD appear to provide reliable and user-friendly alternatives to the gold standard invasive wire-based techniques. Interventional cardiologists and cardiovascular healthcare providers should be familiar with the strengths and weaknesses of the available hemodynamic assessment modalities.
Introduction
Coronary angiography has been the gold standard for assessment of coronary artery disease (CAD) and guidance for percutaneous coronary interventions (PCI). However, coronary angiography is limited by its inability to provide information regarding the physiological significance of a given stenosis. The FAME (Fractional Flow Reserve vs. Angiography for Multivessel Evaluation) and FAME 2 trials showed that routine measurement of fractional flow reserve (FFR) in patients with multivessel CAD undergoing PCI significantly reduced the mortality and incidence of myocardial infarction at 2 years compared with standard angiography-guided PCI (1, 2). Furthermore, physiology–guided PCI has shown increased safety and efficacy, improved resource utilization, and better clinical outcomes in patients with stable angina and acute coronary syndromes (3). Currently the most common methods to assess the functional severity of a coronary stenosis are either invasive techniques, including wire-based techniques [i.e., fractional flow reserve (FFR), instantaneous wave-free ratio (iFR, Philips, The Netherlands), diastolic hyperemia-free ratio (DFR, Boston Scientific Inc., Marlborough, Massachusets, USA), resting full-cycle ratio (RFR, Abbott, Chicago, Illinois, USA)], and non-wire-based techniques [angiography-derived FFR (vFFR, Pie Medical Imaging, The Netherlands; QFR from QAngio XA, Medis, The Netherlands; FFRangio, CathWorks, Isarel)] or non-invasive techniques (FFR-computed tomography; FFRCT, HeartFlow, Redwood City, CA, USA).
The three cases presented and discussed in this report illustrate the strengths and weaknesses of the above-mentioned invasive and non-invasive methods for the hemodynamic assessment of CAD. The cutoff value for a hemodynamically significant coronary stenosis is ≤ 0.80 for wire-based FFR, angiography-derived FFR and FFRCT and ≤ 0.89 for iFR.
Case Series
Patient 1: Discrepancy Between Non-invasive and Invasive Hemodynamic Assessment Modalities in Stented and Calcified Coronary Arteries
A 64-year-old female presented with atypical chest pain for 3 months. Her medical history was notable for PCI of the proximal left anterior descending coronary artery (LAD) with two 3.0 × 12 mm drug-eluting stents (DES). She had non-obstructive CAD of the right coronary artery (RCA) and left circumflex (LCX) artery. She had a recent exercise stress echocardiogram which was negative for inducible ischemia. However, given her prior history of atypical chest pain correlating with markedly abnormal coronary angiograms, a decision was made to anatomically assess her coronary arteries with coronary CT coronary angiography (CCTA). CCTA demonstrated patent LAD stents and a focal mixed plaque was noted just distal to the stents resulting in moderate stenosis (50–70%). The proximal LCX demonstrated a mixed plaque resulting in mild stenosis (25–50%), and the mid RCA showed a long, mixed plaque, resulting in moderate stenosis (50–70%). We assessed the hemodynamic significance of the CAD with FFRCT analysis. The FFRCT in the LAD was not interpretable due to prior stents (Figure 1A), whereas the FFRCT of the LCX was 0.90. The RCA stenosis was hemodynamically significant with FFRCT at 0.53 (Figure 1B). Accordingly, we proceeded with invasive coronary angiography, which showed obstructive CAD (>70% stenosis) in the mid LAD, distal to the prior stents (Figure 1C), which was hemodynamically significant by iFR (0.88). The mid RCA showed mild diffuse disease with <50% stenosis and no focal lesions (Figure 1D). Vessel fractional flow reserve (vFFR) of the LAD was significant at 0.73 which correlated well with the invasive iFR values (Figure 1E), whereas vFFR of the RCA was 0.91 (Figure 1F). This case demonstrates the following three points: (i) Excellent correlation between invasive wire-based (iFR) and non-wire-based (vFFR) studies, (ii) Superior performance of invasive functional studies in coronary arteries with stents where FFRCT is uninterpretable, and (iii) Overestimation of the hemodynamic significance of calcified plaques with FFRCT (Figure 1B).
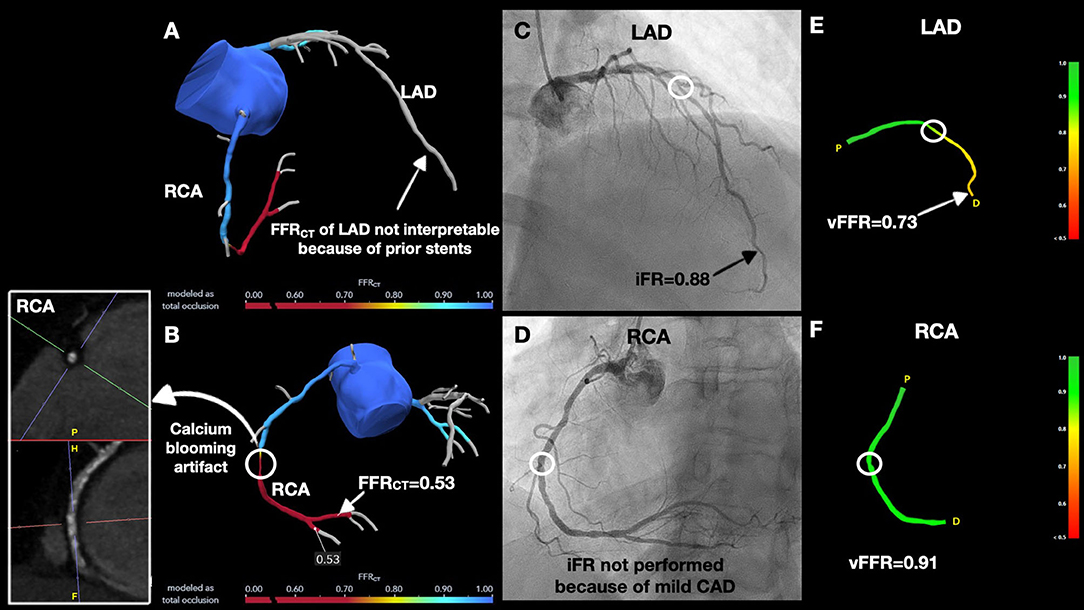
Figure 1. Discrepancies between non-invasive and invasive hemodynamic assessment modalities in stented and calcified coronary arteries. (A) FFRCT of left anterior descending (LAD) could not to be interpreted because of prior stents. (B) CCTA showed calcium blooming artifact in right coronary artery (RCA) lesion and FFRCT was significant at 0.53. (C) Coronary angiogram demonstrated an anatomically obstructive > 70% stenosis in the mid LAD (white circle) with instantaneous wave-free ratio (iFR) of 0.88 and, (D) Non-obstructive coronary artery disease (CAD) in the RCA. (E) Vessel fractional flow reserve (vFFR) was hemodynamically significant in distal LAD (black arrow). (F) vFFR of the RCA was hemodynamically insignificant.
Patient 2: Discrepancy Between Non-invasive and Invasive Hemodynamic Assessment Modalities in Severely Calcified Coronary Arteries
A 76-year-old male with no prior cardiac history presented with dyspnea on exertion. Exercise stress echocardiogram was suboptimal. CCTA showed a severely calcified plaque in the mid LAD which could not be accurately quantified because of the calcium blooming artifact (Figure 2A). The total coronary artery calcium score was elevated at 1,212. A focal mixed plaque was noted in the mid RCA resulting in moderate stenosis (50–70%). FFRCT analysis of the LAD was 0.66, reflecting a hemodynamically significant stenosis (Figure 2B). FFRCT of the LCX was 0.88 and FFRCT was uninterpretable in the RCA because of motion artifact (Figure 2C). The patient underwent invasive coronary angiography which showed anatomically non-obstructive <50% stenosis of the mid LAD with iFR at 1.0 and vFFR at 0.85 (Figures 2D,F), and non-obstructive <50% stenosis in mid RCA with vFFR 0.95 (Figures 2E,G). This case illustrates that calcium blooming or motion artifacts on CCTA can potentially preclude the accurate assessment of the severity of coronary stenoses, resulting in erroneous or uninterpretable FFRCT measurements. Instead, hemodynamic assessment of severely calcified lesions can be accurately performed by vFFR, which can serve as the least invasive alternative to the iFR gold standard.
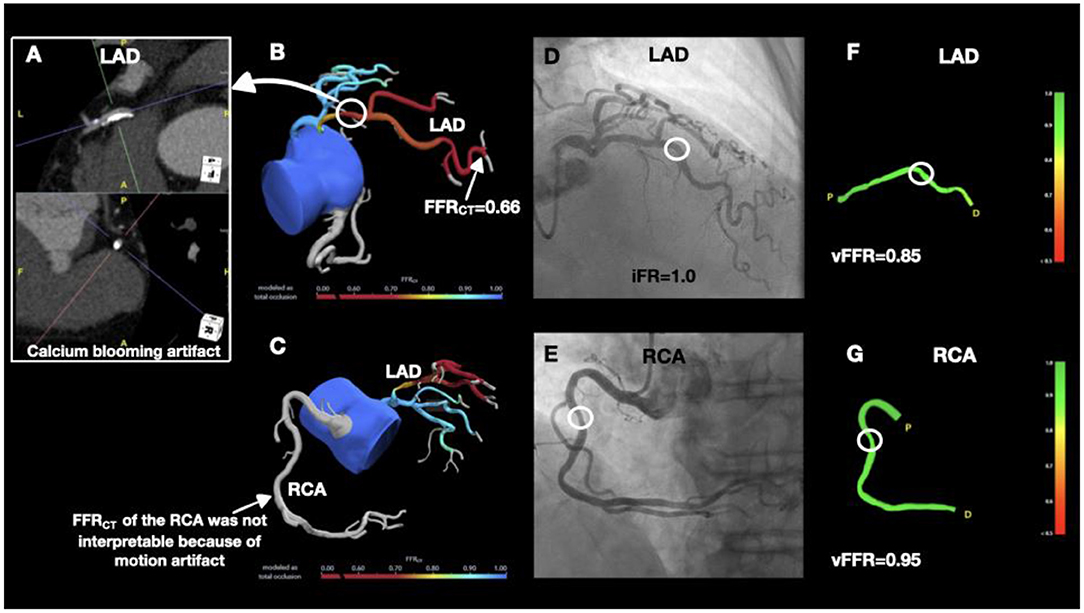
Figure 2. Discrepancy between non-invasive and invasive hemodynamic assessment modalities in severely calcified coronary arteries. (A) CCTA showing severely calcified plaque in the mid LAD. (B) FFRCT of the LAD was hemodynamically significant. (C) FFRCT could not be interpreted in the RCA because of motion artifact. (D) Coronary angiogram demonstrated <50% stenosis in the mid LAD (white circle) and iFR of 1.0. (E) Coronary angiography showed <50% stenosis in the mid RCA (white circle). Both, vFFR of the LAD (F) and vFFR of the RCA (G) were not hemodynamically significant.
Patient 3: Agreement Between Non-invasive and Invasive Hemodynamic Assessment Modalities
A 65-year-old male with a history of PCI in the left posterior descending artery (LPDA) presented with dyspnea on exertion. CCTA showed a left dominant system with a long, calcified plaque, resulting in moderate stenosis (50–70%) of the proximal LAD and mild stenosis (25–50%) of the mid LAD. A focal mixed plaque was noted in the distal LCX resulting in mild stenosis (25–50%), whereas the LPDA stent was patent. A mixed plaque was noted in a non-dominant, proximal RCA resulting in moderate stenosis (50–70%). FFRCT of the LAD and RCA were hemodynamically significant at 0.50 and 0.59, respectively (Figures 3A,B). FFRCT of LCX could not be interpreted because of the prior stent. Invasive coronary angiography showed 70% stenoses of the proximal and mid LAD (Figure 3C), patent LPDA stent with no evidence of obstructive disease in the LCX and a small, non-dominant RCA with proximal 70% stenosis. iFR of the LAD was 0.83 distally and during the iFR pullback jumped to 0.95 in the proximal LAD (Figure 3C). iFR pullback showed excellent correlation with FFRCT values. vFFR of the LAD was 0.67, which correlated with the iFR and FFRCT values (Figure 3D). This case illustrates how both non-invasive (FFRCT) and invasive non-wire-based techniques (vFFR) techniques correlate accurately with invasive wire-based techniques (iFR) in appropriately selected patients without severely calcified or stented coronary arteries.
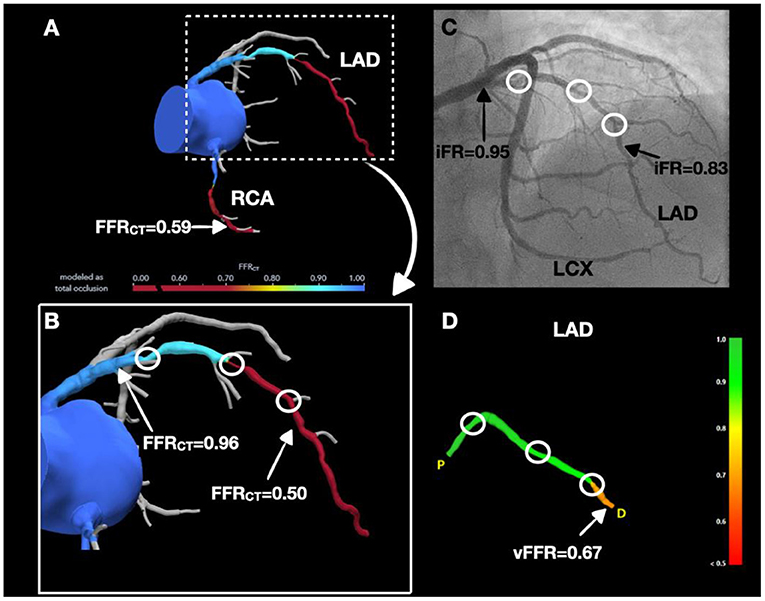
Figure 3. Agreement between non-invasive and invasive hemodynamic assessment modalities. (A,B) Significant LAD and RCA stenoses by FFRCT. (C) Coronary angiogram demonstrated 70% stenoses in the proximal and mid LAD (white circles) and iFR values of 0.95 in proximal LAD and 0.83 in the distal LAD (black arrows). (D) LAD stenosis was significant by vFFR (white arrow).
Discussion
Increasing evidence strongly suggests that presence of ischemia should help guide treatment rather than just anatomic assessment (4). Coronary angiography is limited by its ability to assess the hemodynamic significance of a given stenosis. The use of FFR to guide revascularization in patients with angina and angiographically intermediate stenoses is a Class I recommendation according to the 2021 guidelines endorsed by the major cardiovascular societies worldwide (5, 6). Despite the clinical benefits and Class I recommendation for using invasive physiology to guide coronary revascularization, its utilization in cardiac catheterization laboratories has been low due to high costs, procedural complications, contrast use and adenosine-related contraindications (Table 1) (7). Alternatively, phase-specific indices, like iFR, are equally favorable with reduced procedural times and avoidance of the adenosine-related discomfort and adverse events (8, 9). However, both hyperemic indices (FFR) and resting indices (e.g., iFR) may result in complications related to their invasive nature (e.g., coronary dissection and perforation). Non-invasive (FFRCT) and invasive wire-free techniques (angiographic FFR) have demonstrated comparable predictive values to FFR and iFR in determining functionally obstructive CAD with no wire-related risks, and reduced cost, contrast, and radiation exposure (10–12).
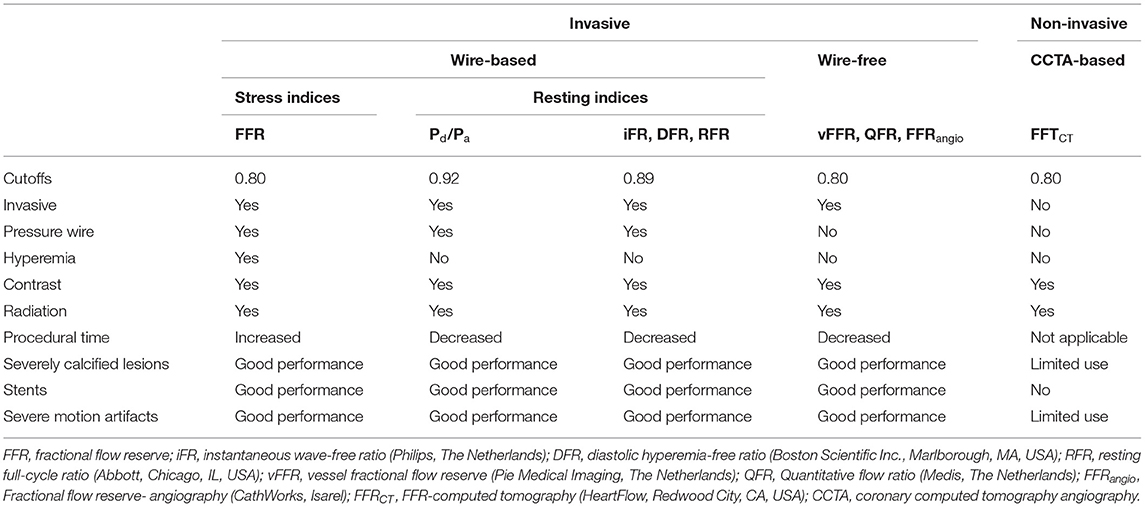
Table 1. Comparison between invasive and non-invasive methods of hemodynamic assessment of coronary stenoses.
FFRCT is based on the application of computational fluid dynamic analysis to a CCTA dataset under maximum computationally simulated hyperemia. FFRCT is cost-effective and has lesser complication rates, thus decreasing the need for invasive coronary angiography (Table 1) (13, 14). FFRCT has been noted to correlate very well with the reference standard invasive indices (i.e. FFR, iFR) (15). The biggest advantage of FFRCT is that on top of the hemodynamic assessment of a given stenosis, it provides useful information on plaque morphology, and identification of high-risk plaques, which are the precursors of a significant portion of acute coronary syndromes (12). However, FFRCT requires high quality CCTA images which are difficult in patients with large body habitus and suboptimal heart rates. Furthermore, FFRCT might provide suboptimal results in cases with motion artifact or noise, severe coronary calcifications and prior stents.
Angiography-derived FFR software uses coronary angiography to calculate the pressure drop across the anatomical stenoses (Table 1). Multiple clinical trials including, the FAST I, FAVOR, and FAST-FFR study have validated the accuracy, reliability, and reproducibility of different angiography-derived FFR softwares, i.e., vFFR, QFR and FFRangio, respectively (16–19). Angiography-derived FFR has consistently shown similar accuracy to the pressure wire–based FFR in large prospective trials and cohort studies (20). Angiography-derived FFR is an easier and potentially faster method for physiology-guided assessment of coronary vessels compared to wire-based techniques (17, 21). However, angiographic FFR requires high-quality angiography in specific orthogonal views without any vessel overlap. This high-quality imaging would be difficult in severely tortuous and very small caliber vessels, obese patients, and patients with chronic kidney disease where contrast use is limited (20).
Newer non-wire based modalities are being increasingly studied. For example, myocardial blush grade reserve has been noted to closely correlate with FFR (22). As technology evolves, invasive wire-free (angiographic FFR) and non-invasive (FFRCT) modalities for the hemodynamic assessment of the CAD, appear to provide reliable and user-friendly alternatives to the gold standard invasive wire-based techniques. Interventional cardiologists and cardiovascular healthcare providers should be familiar with the strengths and weaknesses of the available hemodynamic assessment modalities.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained fromthe participants for the publication of this case report.
Author Contributions
GG involved with the management of the patients and leading the write up of the manuscript. SS made significant contributions to writing the manuscript and proofreading. CH involved with processing of coronary CT and FFT CT images. YSC involved directly in treating the patient, mentored, and made suggestions in the preparation of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
YSC has speaker honoraria, advisory board fees and a research grant from Boston Scientific Inc. and a research grant and advisory board fees from Medtronic Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CAD, Coronary artery disease; CT, Computed tomography; CCTA, Computed tomography coronary angiography; DES, Drug-eluting stent; DFR, Diastolic hyperemia-free ratio; FFR, Fractional flow reserve; iFR, Instantaneous wave-free ratio; LAD, Left anterior descending artery; LCX, Left circumflex artery; LPDA, Left posterior descending artery; PCI, Percutaneous coronary interventions; RCA, Right coronary artery; RFR, resting full-cycle ratio; QFR, Quantitative flow ratio; vFFR, Vessel fractional flow reserve.
References
1. Tonino PAL, De Bruyne B, Pijls NHJ, Siebert U, Ikeno F, van ‘t Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. (2009) 360:213–24. doi: 10.1056/NEJMoa0807611
2. Xaplanteris P, Fournier S, Pijls NHJ, Fearon WF, Barbato E, Tonino PAL, et al. Five-year outcomes with pci guided by fractional flow reserve. N Engl J Med. (2018) 379:250–9. doi: 10.1056/NEJMoa1803538
3. Chowdhury M, Osborn EA. Physiological assessment of coronary lesions in 2020. Curr Treat Options Cardiovasc Med. (2020) 22:2. doi: 10.1007/s11936-020-0803-7
4. Puymirat E, Cayla G, Simon T, Steg PG, Montalescot G, Durand-Zaleski I, et al. Multivessel pci guided by ffr or angiography for myocardial infarction. N Engl J Med. (2021) 385:297–308. doi: 10.1056/NEJMoa2104650
5. Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, et al. 2021 Acc/Aha/Scai guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. (2022) 145:e18–114. doi: 10.1161/CIR.0000000000001060
6. Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 Esc/Eacts guidelines on myocardial revascularization. Eur Heart J. (2019) 40:87–165. doi: 10.1093/eurheartj/ehy855
7. Götberg M, Cook CM, Sen S, Nijjer S, Escaned J, Davies JE. The evolving future of instantaneous wave-free ratio and fractional flow reserve. J Am Coll Cardiol. (2017) 70:1379–402. doi: 10.1016/j.jacc.2017.07.770
8. Davies JE, Sen S, Dehbi H-M, Al-Lamee R, Petraco R, Nijjer SS, et al. Use of the instantaneous wave-free ratio or fractional flow reserve in pci. N Engl J Med. (2017) 376:1824–34. doi: 10.1056/NEJMoa1700445
9. Götberg M, Christiansen EH, Gudmundsdottir IJ, Sandhall L, Danielewicz M, Jakobsen L, et al. Instantaneous wave-free ratio versus fractional flow reserve to guide pci. N Engl J Med. (2017) 376:1813–23. doi: 10.1056/NEJMoa1616540
10. Mathew RC, Gottbrecht M, Salerno M. Computed tomography fractional flow reserve to guide coronary angiography and intervention. Intervent Cardiol Clin. (2018) 7:345–54. doi: 10.1016/j.iccl.2018.03.008
11. Ball C, Pontone G, Rabbat M. Fractional flow reserve derived from coronary computed tomography angiography datasets: the next frontier in noninvasive assessment of coronary artery disease. Biomed Res Int. (2018) 2018:2680430. doi: 10.1155/2018/2680430
12. Giusca S, Schütz M, Kronbach F, Wolf D, Nunninger P, Korosoglou G. Coronary computer tomography angiography in 2021-acquisition protocols, tips and tricks and heading beyond the possible. Diagnostics. (2021) 11:1072. doi: 10.3390/diagnostics11061072
13. Douglas PS, Pontone G, Hlatky MA, Patel MR, Norgaard BL, Byrne RA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of Ffr(Ct): outcome and resource impacts study. Eur Heart J. (2015) 36:3359–67. doi: 10.1093/eurheartj/ehv444
14. De Maria GL, Garcia-Garcia HM, Scarsini R, Hideo-Kajita A, Gonzalo López N, Leone AM, et al. Novel indices of coronary physiology. Circul Cardiovasc Interv. (2020) 13:e008487. doi: 10.1161/CIRCINTERVENTIONS.119.008487
15. Baumann S, Hirt M, Schoepf UJ, Rutsch M, Tesche C, Renker M, et al. Correlation of machine learning computed tomography-based fractional flow reserve with instantaneous wave free ratio to detect hemodynamically significant coronary stenosis. Clin Res Cardiol. (2020) 109:735–45. doi: 10.1007/s00392-019-01562-3
16. Pellicano M, Lavi I, De Bruyne B, Vaknin-Assa H, Assali A, Valtzer O, et al. Validation study of image-based fractional flow reserve during coronary angiography. Circul Cardiovasc Interv. (2017) 10:e005259. doi: 10.1161/CIRCINTERVENTIONS.116.005259
17. Fearon William F, Achenbach S, Engstrom T, Assali A, Shlofmitz R, Jeremias A, et al. Accuracy of fractional flow reserve derived from coronary angiography. Circulation. (2019) 139:477–84. doi: 10.1161/CIRCULATIONAHA.118.037350
18. Kaneshka M, Laurens JCVZ, Matthew MB, Frank JHG, Jurgen MRL, Marcel CMR, et al. Validation of a three-dimensional quantitative coronary angiography-based software to calculate fractional flow reserve: the fast study. EuroIntervention. (2020) 16:591–9. doi: 10.4244/EIJ-D-19-00466
19. Tu S, Westra J, Yang J, von Birgelen C, Ferrara A, Pellicano M, et al. Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the international multicenter favor pilot study. JACC Cardiovasc Interv. (2016) 9:2024–35. doi: 10.1016/j.jcin.2016.07.013
20. Morris PD, Curzen N, Gunn JP. Angiography-derived fractional flow reserve: more or less physiology? J Am Heart Assoc. (2020) 9:e015586. doi: 10.1161/JAHA.119.015586
21. Witberg G, De Bruyne B, Fearon WF, Achenbach S, Engstrom T, Matsuo H, et al. Diagnostic performance of angiogram-derived fractional flow reserve: a pooled analysis of 5 prospective cohort studies. JACC Cardiovasc Interv. (2020) 13:488–97. doi: 10.1016/j.jcin.2019.10.045
22. Hoffman NP, Stefan H, Markus E, Hartmut D, Hugo AK, Grigorios K. Quantitative myocardial blush grade reserve during pharmacologic hyperaemia: a way to perform a real wireless fractional flow reserve measurement in patients with coronary artery disease and intermediate coronary lesions. EuroIntervention. (2017) 12:e2219–27. doi: 10.4244/EIJ-D-16-00460
Keywords: fractional flow reserve, vFFR, CT FFR, CCTA, coronary physiology, coronary artery disease, coronary CT angiography
Citation: Gajanan G, Samant S, Hovseth C and Chatzizisis YS (2022) Case Report: Invasive and Non-invasive Hemodynamic Assessment of Coronary Artery Disease: Strengths and Weaknesses. Front. Cardiovasc. Med. 9:885249. doi: 10.3389/fcvm.2022.885249
Received: 27 February 2022; Accepted: 25 March 2022;
Published: 25 April 2022.
Edited by:
Grigorios Korosoglou, GRN Klinik Weinheim, GermanyReviewed by:
Andreas Giannopoulos, University Hospital Zürich, SwitzerlandStefan Baumann, UMM Mannheim, Germany
Copyright © 2022 Gajanan, Samant, Hovseth and Chatzizisis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yiannis S. Chatzizisis, eWNoYXR6aXppc2lzQGljbG91ZC5jb20=
 Ganesh Gajanan
Ganesh Gajanan Saurabhi Samant
Saurabhi Samant Chad Hovseth
Chad Hovseth Yiannis S. Chatzizisis
Yiannis S. Chatzizisis