- 1Department of Neurology, University Medical Center Utrecht Brain Center, University Medical Center Utrecht, Utrecht, Netherlands
- 2Laboratory of Experimental Cardiology, University Medical Center Utrecht, Utrecht, Netherlands
Background: Fundamental aspects of human identity may play a role in the presentation of stroke symptoms and, consequently, stroke recognition. Strokes must be recognized and treated expeditiously, as delays result in poorer outcomes. It is known that sex plays a role in the presentation of symptoms, such that non-traditional symptoms are more commonly observed among women. However, factors such as geographical location and race/ethnicity, and the interactions between these various factors, need to be considered. This will provide an intersectional approach.
Methods: A systematic review and meta-analysis of the literature was conducted to investigate differences in the presentation of stroke symptoms between sexes. Using PubMed and Embase, a search involving the components sex, symptoms and stroke was completed and yielded 26 full-text manuscripts.
Results: Our findings indicate that there is substantial overlap in stroke symptom presentation in men and women. Nonetheless, some differences in the clinical manifestations of stroke were observed. In addition, it was discovered that only three studies were conducted outside of North America and Europe. Furthermore, only two studies reported symptoms based on both sex and racial/ethnic group.
Conclusion: These findings indicate a research gap and call for increased research in order to uncover the possible interactions between sex and race/ethnicity in an intersectional approach. Resultantly, stroke recognition could be improved and greater equity in healthcare can be achieved.
Introduction
Prompt stroke symptom recognition is of critical importance to prevent pre- and in-hospital delays (1). Minimizing these delays is crucial, as the efficacy of ischemic stroke treatment is time-dependent (2). Symptom presentation and, correspondingly, stroke recognition may depend on fundamental aspects of human identity. These aspects should not be considered independently, as they interact and are best described using the term intersectionality. Intersectionality describes the complex interconnectedness of elements such as gender, sex, race and ethnicity, with class, education, nationality and religion (3).
It is known that women are not only older by an average of 5 years when experiencing a stroke, but also suffer from more severe strokes (4). Risk factors and stroke subtypes differ between women and men, with women being more likely to suffer from atrial fibrillation and total anterior circulation syndrome or cardioembolic strokes (4, 5). On the other hand, men are more likely to be diagnosed with atherosclerosis and experience posterior circulation stroke or lacunar stroke (4, 5). Stroke subtypes are linked to symptom presentation, implying potential sex-based symptom differences. A recent systematic review on sex differences in stroke symptoms concluded that women are more likely to present with non-traditional stroke symptoms. Symptoms such as changes in level of consciousness, mental status change and headache are experienced more commonly by women (6).
Racial and ethnic group differences in risk factors and stroke subtypes exist, and potentially lead to additional stroke symptom disparities. Black populations carry a greater burden of stroke risk factors such as hypertension, obesity and diabetes mellitus (7). Diabetes mellitus is also a common risk factor in Hispanic populations (8). On the other hand, prevalence of large artery atherosclerosis is higher in Caucasians (9). Lacunar infarctions and transient ischemic attacks are more common among Blacks compared to Caucasians, whilst Blacks have lower odds of a cardioembolic stroke, which are more prevalent in Hispanic and Caucasian populations (9, 10). In addition to differing distributions of risk factors and stroke subtypes, a study in Northern America indicated in-hospital delays among ethnic minority groups. Blacks experience longer waiting times and additionally, ethnic minorities are less likely to receive thrombolysis as a treatment for acute ischemic stroke (10). Beliefs, attitudes and discrimination are likely to play a role in these delays in addition to a potential role of racial-ethnic symptom differences.
We conducted a systematic review and meta-analysis of the literature investigating differences in the presentation of stroke symptoms between women and men, and analyzed geographic diversity. Secondly, we aimed to identify studies that reported symptoms based on both sex and racial/ethnic group.
Materials and Methods
Search Strategy
Using PubMed and Embase, a search involving the components sex, symptoms and stroke and synonyms was conducted. The search query, last updated on January 18th, 2021, resulted in 21,304 hits in EMBASE and 10,411 in PubMed.
Study Selection
A title-abstract screen followed by a full-text screen was performed. The screening procedure was completed by two independent reviewers (F.H. and S.E.). Debatable cases were discussed with L.E. to achieve consensus. Included articles focused on ischemic strokes or transient ischemic attacks, articles solely about hemorrhagic strokes or not about strokes were excluded. Included articles stated the quantitative results for symptom presentation differences between men and women. Only articles in Dutch or English were considered. Case studies, meta-analyses and systematic and literature reviews were excluded. Studies involving animals, patients under the age of 18 or only men/women were excluded from the review. The full-text screen excluded abstract-only congress papers and cases in which the full-text article was unavailable even after contacting the authors. A total of 282 articles were screened in the full-text screen, eventually yielding a total of 25 remaining papers. Snowballing allowed for the identification of an additional article, resulting in a total of 26 eligible studies in this systematic review and meta-analysis (Supplementary Material 1).
Results
A total of 493,289 participants were involved in these studies, 50.1% of whom were women. The results of the meta-analysis indicate that there are sex differences in the presentation of stroke symptoms. Despite substantial overlap in stroke symptom presentation in women and men, some differences in the clinical manifestations of stroke were observed. Men have higher odds of presenting with the traditional symptoms of postural instability (OR 0.72; 95% CI, 0.59–0.88) and dysarthria (OR 1.03; 95% CI, 0.94–1.12). Women have higher odds of experiencing the traditional symptom aphasia (OR 1.18; 95% CI, 1.09–1.28). Non-traditional symptoms were found to be more common in women, who were shown to have increased odds of headache (OR 1.22; 95% CI, 1.04–1.43), mental status change (OR 1.24; 95% CI, 1.02–1.52), seizure/convulsions (OR 1.27; 95% CI 1.01–1.60), dysphagia (OR 1.33; 95% CI, 1.06–1.68), incontinence (OR 1.45; 95% CI, 1.32–1.59) and altered consciousness (OR 1.49; 95% CI, 1.32–1.68) (Supplementary Material 2).
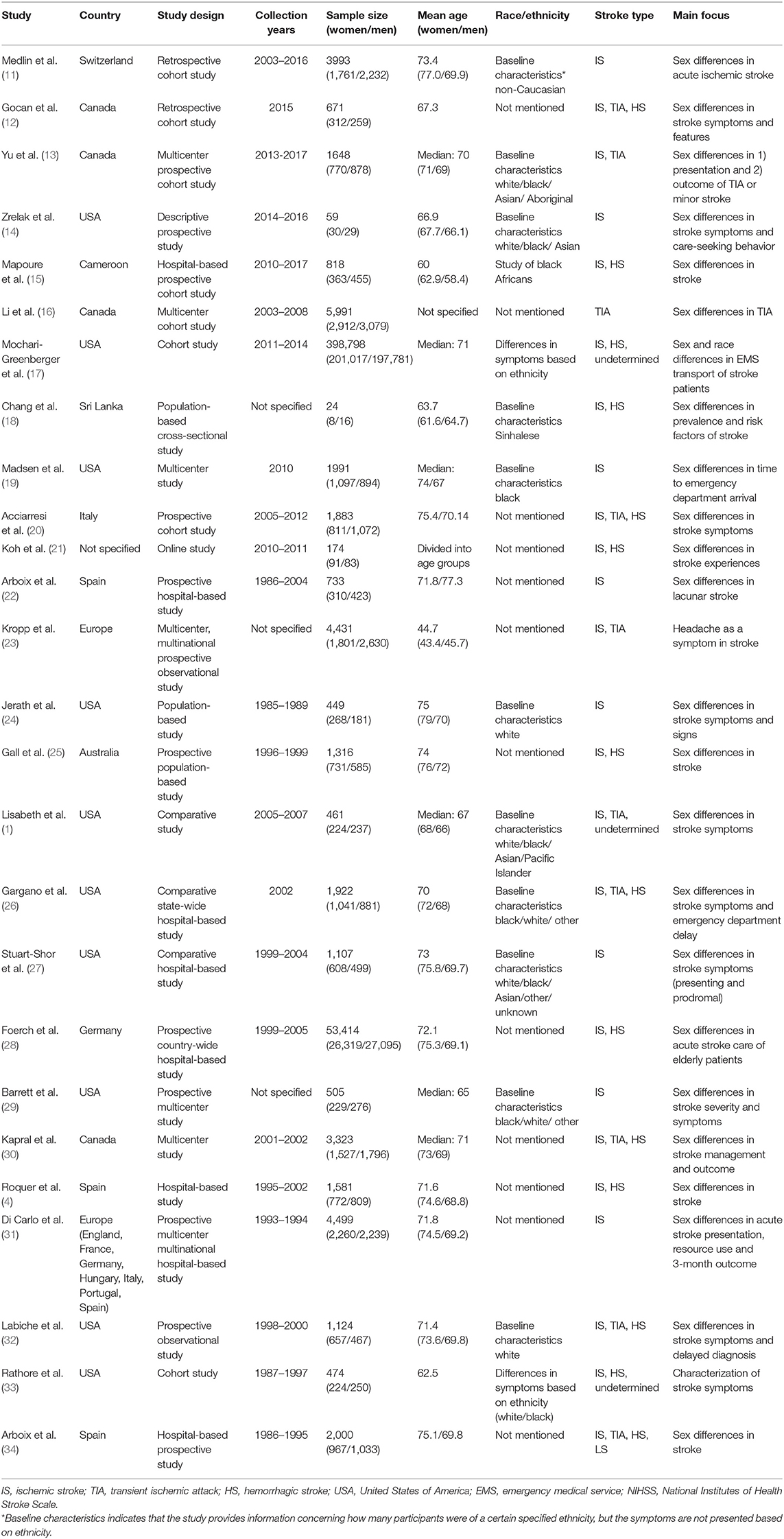
Additional analyses of the geographical location of included studies allowed us to observe that only three of the 26 studies in this systematic review were conducted outside of North America or Europe (Figure 1). Out of the 26 studies, 14 reported the racial/ethnic distribution of the population whilst only two studies reported symptom presentation differences based on ethnicity (Table 1) (10, 33). These two studies included all stroke types and the results indicated that the frequency of stroke symptoms varies by sex as well as race/ethnicity. When evaluating differences between 226 Blacks and 248 Caucasians, Rathore et al. (33) found that Blacks are more likely to experience paresis of the face, arm or leg (78.2 vs. 85.4%; p = 0.044). Results also indicate that Caucasians are more likely to experience gait disturbance (13.3 vs. 8.0%; p = 0.061) and vertigo (3.2 vs. 0.9%; p = 0.077) (33). In line with this, Mochari-Greenberger et al. (17) (n = 398,798) found that, compared to Caucasians, weakness/paresis is more likely to be experienced by Blacks (OR 1.16; 95% CI, 1.14–1.19), as well as Asian (OR 1.23; 95% CI, 1.17–1.29) and Hispanic (OR 1.09; 95% CI, 1.06–1.12) populations. Mochari-Greenberger et al. (17) also more intricately examined the interaction between sex and racial/ethnic group and found that there were significant differences for the symptoms aphasia and altered consciousness. Namely, when compared to Caucasian men, aphasia is more common among Black men (OR 1.07; 95% CI, 1.04–1.10) and less common among Hispanic men (OR 0.95; 95% CI, 0.92–0.99). In women, Hispanics (OR 0.90; 95% CI, 0.87–0.94) and Asians (OR 0.91; 95% CI, 0.85–0.96) are less likely to experience this symptom compared to Caucasians. As for altered levels of consciousness, compared to Caucasian men, this symptom is more common among Black (OR 1.17; 95% CI, 1.13–1.20), Hispanic (OR 1.11; 95% CI, 1.06–1.16), and Asian (OR 1.07; 95% CI, 1.00–1.13) male populations. In women, however, presentation with this symptom does not differ significantly between Caucasians, Blacks, Hispanics, and Asians (17). It is important to note that both studies were conducted in the United States of America. Thus, more geographically diverse research is of interest. A meta-analysis looking at the intersection between sex and ethnicity in stroke symptom presentation was not feasible with only two studies.
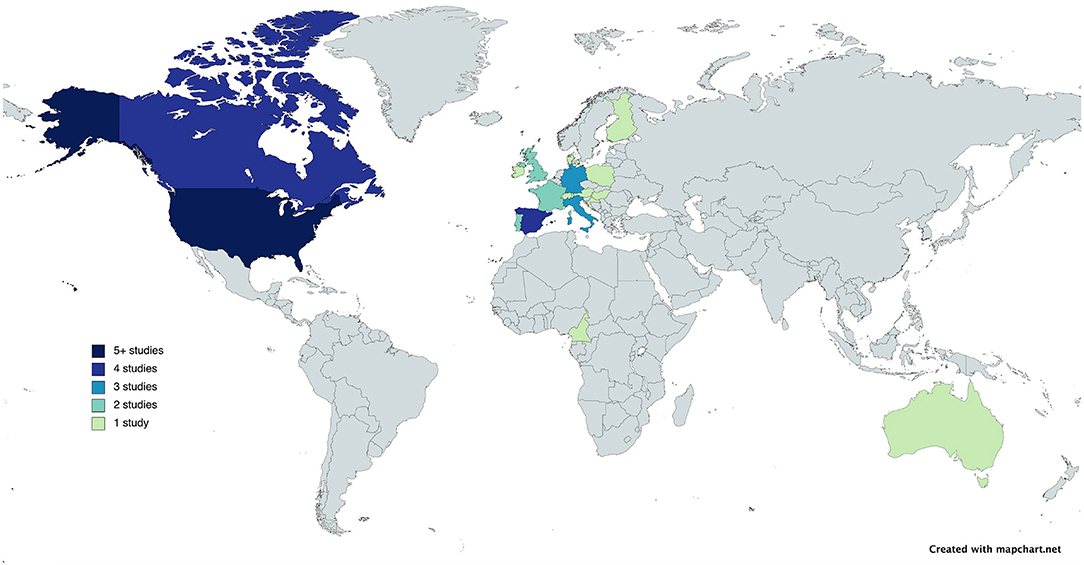
Figure 1. World map depicting the number of studies (color) on stroke symptoms in women and men were conducted.
Discussion
The majority of studies on sex differences in stroke presentation were conducted in North America and Europe. The meta-analysis indicates that there are some differences in the clinical manifestations of stroke between men and women. Namely, traditional symptoms such as postural instability and dysarthria are observed more frequently in men, whilst women are more likely to experience non-traditional symptoms such as headache, mental status change, seizure/convulsions, incontinence and altered consciousness. This is in line with previous findings (6). Furthermore, the results of this mini-review indicate that only two previous studies have reported stroke symptom presentation differences based on sex and race/ethnicity. Their results suggest that the frequency of certain stroke symptoms vary by sex as well as race/ethnicity. Only one study investigated the interaction between sex and racial/ethnic group, and found that there were significant differences for the symptoms aphasia and altered consciousness.
It is incongruous that the majority of research concerning stroke symptoms has been conducted in North America and western Europe, when across the globe, age-standardized stroke incidence is reported to be highest in northern Asia, followed by eastern Europe (35). Other sources indicate that the highest stroke burden is observed in sub-Saharan Africa (36). Increased longevity as well as changes in lifestyle and socio-demographic factors contribute to a trend of increasing stroke burden in low- and middle-income country settings (37, 38). In addition to geographical factors, race can also be linked to stroke incidence. Blacks have double the risk of stroke compared to Caucasians, and worse outcomes as well as higher mortality rates are observed among Black populations (39). The question of a conceivable role of race/ethnicity in symptom presentation is raised by these epidemiological patterns in combination with knowledge of the distribution of stroke risk factors and subtypes among races. Since research concerning stroke symptoms is largely based in western countries with mainly Caucasian populations, Caucasians are overrepresented in this field of research, whilst insights into racial-ethnic differences in symptom presentation could prove to be relevant in stroke recognition and, accordingly, outcome improvement.
The systematic review and meta-analysis is not without limitations. Firstly, the quality of the data on stroke symptoms is dependent on the methods used in individual studies. Prospective data capture, for example, may be considered more reliable than retrospective data capture. Additionally, distinct data collection methods used in the included studies, such as medical record review and interviews, subsequently lead to different types of bias such as misclassification bias and recall bias, respectively. Secondly, multiple stroke symptoms can be present in one patient. It is not clear how often patients with stroke show isolated non-traditional symptoms—in other words, non-traditional symptoms that are not seen in combination with traditional symptoms. Furthermore, symptom frequency may be underreported due to a lack of recognition, especially for non-traditional symptoms, which could result in publication bias. Lastly, the data does not indicate the extent to which a symptom was experienced: whether it was mild or severe. Nor which symptom is most burdensome in terms of post-stroke disability. This is all relevant data within the scheme of stroke recovery.
Racial-ethnic and sex/gender stratification of stroke symptom presentation is necessary to deepen our understanding of symptom presentation, subsequently improving recognition. Improved recognition is directly associated with improved stroke outcomes (1). Recognition does not only entail recognition by the general public, but also by front line health workers and hospital staff. Although focus should remain upon the recognition of traditional symptoms, additional educational intervention programs or public health campaigns concerning racial-ethnic and sex/gender disparities in stroke symptoms may be necessary. However, the big picture is more complex. Stroke recognition is tied to social and environmental determinants. Here, there is room for intersectional research, investigating ethnicity and gender-based social constructions, as well as prejudice and discrimination, and how this affects stroke recognition. Limited recognition of the importance of intersectional research can be attributed to the reliance upon reductionist frameworks. Ultimately, research in this area and tackling underlying risk factors can aid the journey toward health equity in underrepresented populations. Lastly, improvements in the reporting of non-traditional symptoms are necessary to gain a more complete understanding of the sex and gender differences in this area, as well as potential racial-ethnic dissimilarities, and interactions between the two.
Author Contributions
FH and SE: acquisition of data. FH: analysis of data and writing the first draft. HR and LE: conception and design. All authors contributed to the article and approved the submitted version.
Funding
LE is WP leader sex differences in the Heart-Brain Connection Consortium, which was supported by the Netherlands CardioVascular Research Initiative: the Dutch Heart Foundation (CVON 2018-28 & 2012-06 Heart Brain Connection), Dutch Federation of University Medical Centers, the Netherlands Organization for Health Research and Development, and the Royal Netherlands Academy of Sciences. LE is recipient of 2020 Prize for Best Integration of Sex and Gender Considerations in a Cardiovascular Research Project, made available by Libin International Trainee Symposium: Research is Better with Sex and Gender!
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.874239/full#supplementary-material
References
1. Lisabeth LD, Brown DL, Hughes R, Majersik JJ, Morgenstern LB. Acute stroke symptoms. Stroke. (2009) 40:2031–6. doi: 10.1161/STROKEAHA.109.546812
2. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. (2014) 384:1929–35. doi: 10.1016/S0140-6736(14)60584-5
3. Allana S, Ski CF, Thompson DR, Clark AM. Intersectionality and heart failure: what clinicians and researchers should know and do. Curr Opin Support Palliative Care. (2021) 15:141–6. doi: 10.1097/SPC.0000000000000547
4. Roquer J, Campello AR, Gomis M. Sex differences in first-ever acute stroke. Stroke. (2003) 34:1581–5. doi: 10.1161/01.STR.0000078562.82918.F6
5. Reid JM, Dai D, Gubitz GJ, Kapral MK, Christian C, Phillips SJ. Gender differences in stroke examined in a 10-year cohort of patients admitted to a Canadian teaching hospital. Stroke. (2008) 39:1090–5. doi: 10.1161/STROKEAHA.107.495143
6. Ali M, van Os HJA, van der Weerd N, Schoones JW, Heymans MW, Kruyt ND, et al. Sex differences in presentation of stroke: a systematic review and meta-analysis. Stroke. (2022) 53:345–54. doi: 10.1161/STROKEAHA.120.034040
7. Boehme AK, Esenwa C, Elkind MSV. Stroke risk factors, genetics, and prevention. Circ Res. (2017) 120:472–95. doi: 10.1161/CIRCRESAHA.116.308398
8. Morgenstern LB, Steffen-Batey L, Smith MA, Moyé LA. Barriers to acute stroke therapy and stroke prevention in Mexican Americans. Stroke. (2001) 32:1360–4. doi: 10.1161/01.STR.32.6.1360
9. Gutierrez J, Koch S, Dong C, Casanova T, Modir R, Katsnelson M, et al. Racial and ethnic disparities in stroke subtypes: a multiethnic sample of patients with stroke. Neurol Sci. (2014) 35:577–82. doi: 10.1007/s10072-013-1561-z
10. Cruz-Flores S, Rabinstein A, Biller J, Elkind MSV, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: the American experience. Stroke. (2011) 42:2091–116. doi: 10.1161/STR.0b013e3182213e24
11. Medlin F, Amiguet M, Eskandari A, Michel P. Sex differences in acute ischaemic stroke patients: clinical presentation, causes and outcomes. Eur J Neurol. (2020) 27:1680–8. doi: 10.1111/ene.14299
12. Gocan S, Fitzpatrick T, Wang CQ, Taljaard M, Cheng W, Bourgoin A, et al. Diagnosis of transient ischemic attack. Stroke. (2020) 51:3371–4. doi: 10.1161/STROKEAHA.120.031510
13. Yu AYX, Penn AM, Lesperance ML, Croteau NS, Balshaw RF, Votova K, et al. Sex differences in presentation and outcome after an acute transient or minor neurologic event. JAMA Neurol. (2019) 76:962. doi: 10.1001/jamaneurol.2019.1305
14. Zrelak PA. Sex-based differences in symptom perception and care-seeking behavior in acute stroke. Permanente J. (2018) 22:18–042. doi: 10.7812/TPP/18-042
15. Mapoure YN, Eyambe NL, Dzudie AT, Ayeah CM, Ba H, Hentchoya R, et al. Gender-related differences and short-term outcome of stroke: results from a hospital-based registry in Sub-Saharan Africa. Neuroepidemiology. (2017) 49:179–88. doi: 10.1159/000484319
16. Li OL, Silver FL, Lichtman J, Fang J, Stamplecoski M, Wengle RS, et al. Sex differences in the presentation, care, and outcomes of transient ischemic attack. Stroke. (2016) 47:255–7. doi: 10.1161/STROKEAHA.115.010485
17. Mochari-Greenberger H, Xian Y, Hellkamp AS, Schulte PJ, Bhatt DL, Fonarow GC, et al. Racial/ethnic and sex differences in emergency medical services transport among hospitalized US stroke patients: analysis of the national get with the guidelines–stroke registry. J Am Heart Assoc. (2015) 4:e002099. doi: 10.1161/JAHA.115.002099
18. Chang T, Gajasinghe S, Arambepola C. Prevalence of stroke and its risk factors in urban Sri Lanka. Stroke. (2015) 46:2965–8. doi: 10.1161/STROKEAHA.115.010203
19. Madsen TE, Sucharew H, Katz B, Alwell KA, Moomaw CJ, Kissela BM, et al. Gender and time to arrival among ischemic stroke patients in the Greater Cincinnati/Northern Kentucky stroke study. J Stroke Cerebrovasc Dis. (2016) 25:504–10. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.026
20. Acciarresi M, de Luca P, Caso V, Agnelli G, D'Amore C, Alberti A, et al. Acute stroke symptoms: do differences exist between sexes? J Stroke Cerebrovasc Dis. (2014) 23:2928–33. doi: 10.1016/j.jstrokecerebrovasdis.2014.07.044
21. Koh S, Gordon AS, Wienberg C, Sood SO, Morley S, Burke DM. Stroke experiences in weblogs: a feasibility study of sex differences. J Med Internet Res. (2014) 16:e84. doi: 10.2196/jmir.2838
22. Arboix A, Blanco-Rojas L, Oliveres M, García-Eroles L, Comes E, Massons J. Clinical characteristics of acute lacunar stroke in women: emphasis on gender differences. Acta Neurologica Belgica. (2014) 114:107–112. doi: 10.1007/s13760-013-0257-8
23. Kropp P, Holzhausen M, Kolodny E, Becker U, Dichgans M, Diez-Tejedor E, et al. Headache as a symptom at stroke onset in 4,431 young ischaemic stroke patients. Results from the “stroke in young fabry patients (SIFAP1) study.” J Neural Trans. (2013) 120:1433–40. doi: 10.1007/s00702-013-1014-0
24. Jerath NU, Reddy C, Freeman WD, Jerath AU, Brown RD. Gender differences in presenting signs and symptoms of acute ischemic stroke: a population-based study. Gender Med. (2011) 8:312–9. doi: 10.1016/j.genm.2011.08.001
25. Gall SL, Donnan G, Dewey HM, Macdonell R, Sturm J, Gilligan A, et al. Sex differences in presentation, severity, and management of stroke in a population-based study. Neurology. (2010) 74:975–81. doi: 10.1212/WNL.0b013e3181d5a48f
26. Gargano JW, Wehner S, Reeves MJ. Do presenting symptoms explain sex differences in emergency department delays among patients with acute stroke? Stroke. (2009) 40:1114–20. doi: 10.1161/STROKEAHA.108.543116
27. Stuart-Shor EM, Wellenius GA, DelloIacono DM, Mittleman MA. Gender differences in presenting and prodromal stroke symptoms. Stroke. (2009) 40:1121–6. doi: 10.1161/STROKEAHA.108.543371
28. Foerch C, Misselwitz B, Humpich M, Steinmetz H, Neumann-Haefelin T, Sitzer M. Sex disparity in the access of elderly patients to acute stroke care. Stroke. (2007) 38:2123–6. doi: 10.1161/STROKEAHA.106.478495
29. Barrett KM, Brott TG, Brown RD, Frankel MR, Worrall BB, Silliman SL, et al. Sex differences in stroke severity, symptoms, and deficits after first-ever ischemic stroke. J Stroke Cerebrovasc Dis. (2007) 16:34–9. doi: 10.1016/j.jstrokecerebrovasdis.2006.11.002
30. Kapral MK, Fang J, Hill MD, Silver F, Richards J, Jaigobin C, et al. Sex differences in stroke care and outcomes. Stroke. (2005) 36:809–14. doi: 10.1161/01.STR.0000157662.09551.e5
31. di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Basile AM, Wolfe CDA, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe. Stroke. (2003) 34:1114–9. doi: 10.1161/01.STR.0000068410.07397.D7
32. Labiche LA, Chan W, Saldin KR, Morgenstern LB. Sex and acute stroke presentation. Ann Emerg Med. (2002) 40:453–60. doi: 10.1067/mem.2002.128682
33. Rathore SS, Hinn AR, Cooper LS, Tyroler HA, Rosamond WD. Characterization of incident stroke signs and symptoms. Stroke. (2002) 33:2718–21. doi: 10.1161/01.STR.0000035286.87503.31
34. Arboix A, Oliveres M, García-Eroles L, Maragall C, Massons J, Targa C. Acute cerebrovascular disease in women. Eur Neurol. (2001) 45:199–205. doi: 10.1159/000052130
35. Johnson CO, Nguyen M, Roth GA, Nichols E, Alam T, Abate D, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:439–58. doi: 10.1016/S1474-4422(19)30034-1
36. Sarfo FS, Ovbiagele B, Gebregziabher M, Wahab K, Akinyemi R, Akpalu A, et al. Stroke among young west Africans. Stroke. (2018) 49:1116–22. doi: 10.1161/STROKEAHA.118.020783
37. Owolabi M, Olowoyo P, Popoola F, Lackland D, Jenkins C, Arulogun O, et al. The epidemiology of stroke in Africa: a systematic review of existing methods and new approaches. J Clin Hypertens. (2018) 20:47–55. doi: 10.1111/jch.13152
38. Owolabi M, Akarolo-Anthony S, Akinyemi R, Arnett D, Gebregziabher M, Jenkins C, et al. The burden of stroke in Africa: a glance at the present and a glimpse into the future: review article. Cardiovasc J Africa. (2015) 26:S27–38. doi: 10.5830/CVJA-2015-038
Keywords: stroke, sex, intersectionality, ethnic diversity, symptoms
Citation: Hosman FL, Engels S, den Ruijter HM and Exalto LG (2022) Call to Action for Enhanced Equity: Racial/Ethnic Diversity and Sex Differences in Stroke Symptoms. Front. Cardiovasc. Med. 9:874239. doi: 10.3389/fcvm.2022.874239
Received: 11 February 2022; Accepted: 04 April 2022;
Published: 03 May 2022.
Edited by:
Hendrik Tevaearai Stahel, Bern University Hospital, SwitzerlandReviewed by:
Cheryl Bushnell, Wake Forest School of Medicine, United StatesCopyright © 2022 Hosman, Engels, den Ruijter and Exalto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lieza G. Exalto, bC5nLmV4YWx0by0yQHVtY3V0cmVjaHQubmw=
 Floortje L. Hosman
Floortje L. Hosman Sabine Engels
Sabine Engels Hester M. den Ruijter
Hester M. den Ruijter Lieza G. Exalto
Lieza G. Exalto