- 1Department of Epidemiology and Health Statistics, Hangzhou Medical College School of Public Health, Hangzhou, China
- 2Department of Non-communicable Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 3Centre for Chronic Conditions and Injuries, Public Health Foundation of India, New Delhi, India
- 4National Institute of Nutrition, Hyderabad, India
There are more and more proofs about the impact of neighborhood alcohol environment on alcohol-associated events. The relationship between the neighborhood availability and accessibility of alcohol outlet with individual level of alcohol consumption along with 11 cardiovascular risk factors was explored for the first time in India using data from the 3rd follow-up of the Andhra Pradesh children and parents study (APCAPS) (n = 6156, for liquor intake and 5,641 for heart and blood vessel risk elements). In fully adjusted models, volunteers in the lowest tertile performed worse than volunteers in the highest tertile of distance to the closest alcohol outlet were more probably to exhibit less alcohol consumption (−14.40 g/day, 95% CI: −26.21, −2.59). A unit per km2 rise in alcohol outlet density in 400 m buffering area was related to a rise in waist circumference (1.45 mm, 95% CI: 0.13, 2.77), SBP (0.29 mmHg, 95% CI: 0.09, 0.49), and DBP (0.19 mmHg, 95% CI: 0.03, 0.35). A unit per 100 m rise in distance to the closest alcohol outlet was related to a rise in waist circumference (−2.39 mm, 95% CI: −4.18, −0.59), SBP (−0.41 mmHg, 95% CI: −0.68, −0.15), and DBP (−0.29 mmHg, 95% CI: −0.51, −0.07). Neighborhood availability of alcohol outlets within immediate locality of participants’ households had a closer relationship with cardiovascular risk factors than that within the whole village. Public health policies designed to limit neighborhood availability and accessibility of alcohol outlets ought to be advocated in southern India.
Introduction
Cardiovascular disease (CVD) causes huge disease burden and deaths worldwide (1). In India, it contributed 28.1% of the total deaths and 14.1% of the total disability-adjusted life-years in 2016 (2). Alcohol use is a key modifiable risk factor for acute and chronic diseases globally, causing 2.8 million deaths in 2016 (3). Heavy drinking is associated with an increased risk of initial presentation of several symptomatic manifestations of CVD, such as coronary death, heart failure, cardiac arrest, transient ischemic attack, ischemic stroke, intracerebral hemorrhage, and peripheral arterial disease (4). In India, alcohol attributable deaths would lead to a loss of 258 million life years between 2011 and 2,050, causing significant negative health impact and economic burden (5).
Data from multiple countries indicate a close connection between the neighborhood alcohol environment, especially the availability and accessibility of alcohol (on and/or off-premises), and the individual alcohol consumption (6). However, most of the existing studies have been conducted in high-income countries and have focused on the association between alcohol environment and drinking behaviors and beliefs among adolescents or young adults (7–9). Very few studies have been carried out in low- and middle-income countries. Ibitoye et al. found that high density of alcohol-selling outlets and outdoor advertisements increased alcohol use among adolescents in Tanzania (10). Study from rural South Africa found that density of alcohol outlets was associated with problematic drinking among young men (11).
Further, there is increasing evidence about the impact of neighborhood alcohol environment on alcohol-related events including experienced violence, injuries, and drunk-driving fatalities (12–14). Higher alcohol outlet density was also shown to be associated with non-injury health outcomes such as liver problems, mental health, sexually transmitted infections, and total deaths (15–17). By now, to the best of our knowledge, no study has addressed the association between the availability and accessibility of alcohol with individual level of alcohol consumption and cardiovascular risk factors in general population in low- and middle-income countries.
In order to inform policies for the control of local alcohol use and disease burden of CVD in low- and middle- income countries, further evidence on the effect of alcohol environment on individual alcohol use as well as cardiovascular risk is urgently needed. Therefore, we carried out data analysis from a peri-household cohort study in southern India here to investigate whether access to and availability of alcohol outlets in the local neighborhood is related with alcohol consumption and cardiovascular risk factors.
Materials and Methods
Study Participants
The Andhra Pradesh children and parents study (APCAPS) study has been explained previously (18, 19). In short, it’s an inter-generation cohort in south India, which started with the follow-up of the participants of the Hyderabad Nutrition Trial (HNT) conducted from 1987 to 1990. It was conducted in 29 villages close to Hyderabad in Ranga Reddy district, Andhra Pradesh. The data used in this cross-sectional analysis are from the 3rd follow-up where the index participants of HNT and their family members were enrolled. Between 2010 and 2012, data on sociodemographic features, lifestyle-related factors, anthropometric measurements, and heart and blood vessel biomarkers of study participants was collected (20–22). Of the 6,659 participants from 3rd follow-up, current analysis is based on data from 6,156 participants after removing 503 participants with missing information on household address, sociodemographic features, or drinking quantity. For analysis of association between alcohol environment and cardiovascular risk factors, data from n = 5,641 participants was considered after removing participants with diagnosed heart disease and/or missing data on lifestyle risk factors.
Global Positioning System-Dependent Surveys of Alcohol Environment
In 2016, geographic coordinates (latitude and longitude) of all the alcohol outlets in study villages were captured by Global Positioning System (GPS). Both availability and accessibility were examined to measure neighborhood alcohol environment. Availability of alcohol outlets was measured near the participants’ households and in the entire village by determining density of outlets in two buffering regions of participants’ households, 400 and 1,600 m, respectively. The degree of accessibility of an alcohol outlet was measured as the distance from a household to the closest outlet. The R software 3.5.1 was adopted to obtain the geography exposures.
Alcohol Intake and Cardiovascular Risk Factors
Data on alcohol intake were collected through questionnaire by well-experienced researchers in the 3rd follow-up. Fasting glucose, insulin, body mass index (BMI), waist circumference, waist-hip-ratio (WHR), blood pressure, serum triglycerides, total cholesterol, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) were analyzed as cardiovascular risk factors herein. Fasting blood specimens were collected and prepared for physiological measurements and biochemical assays in the 3rd follow-up (19). Glucose level was estimated via the glucose oxidase/peroxidase-4-aminophenazone-phenol procedure. Insulin level was estimated using an electrochemiluminescence immunoassay. Concentrations of triglycerides and cholesterols (HDL, total) were measured using enzymatic calorimetric method (23, 24). LDL-C level was calculated by standard Friedewald–Fredrickson equation (25). The anthropometry evaluations included weight (identified to the nearest 0.1 kg by digitalized SECA scale), height (nearest 1 mm by portable plastic stadiometer), as well as waist circumference and hip circumference (nearest 1 mm by portable plastic stadiometer). The BMI was calculated by dividing weight in kilograms by the square of height in meters. The WHR was calculated by dividing waist circumference by hip circumference. The blood pressure was measured at the right arm in the seated posture via an oscillometry equipment (Omron M5-I). Three results were recorded and the average value was considered for these measurements.
Covariates
The data on sociodemographic and lifestyle variables such as age, gender, educational level (illiterate, primary school, middle school, and above), occupation (unskilled, skilled, and others), Standard of Living Index (SLI) (low, middle, and high), smoking (never, former, and current), drinking (gram/day), and physical activity (extremely inactive, sedentary, moderately active, and vigorously active) were collected using standardized questionnaires by practiced researchers. The SLI was adopted to measure the family socioeconomic conditions (20). The data on diet intake (in the last year) and physical activities (in the last week) were gathered by semi-quantitation questionnaires (19).
Statistical Analysis
Considering the possible clustering of neighborhood alcohol environment, three-level mixed-effects linear regression was employed to evaluate the relationship between the densities and distances of alcohol outlets (exposures) with individual level of alcohol consumption (outcome 1) and cardiovascular risk factors (outcome 2). In the analysis of alcohol consumption, age (continuous, year), and gender [categorical, (male and female)] were adjusted in model 1; education level [categorical, (illiterate, primary school, and middle school and above)], occupation [categorical, (unskilled, skilled, and others)], and SLI [categorical, (low, middle, and high)] were further adjusted in model 2. In the analysis of cardiovascular risk factors, we adjusted for same variables in model 1 and 2; we further included tobacco use [categorical, (never, former, and current)], physical activity [categorical, (extremely inactive, sedentary, moderately active, and vigorously active)], and daily energy intake (continuous, kcal/day) in model 3. To account for the effect of disease diagnosis on behaviors, we performed a sensitivity analysis by excluding participants with diagnosed high blood pressure and/or diabetic disease to account for the effect of disease diagnosis on behaviors.
Stata software 15.1 was used for statistical analyses. PASS software 15.0 was used for power analysis in linear regression. Take SBP for example, a sample size of 5,641 achieves 99% power to detect a change in slope from 0.00 under the null hypothesis to 0.31 under the alternative hypothesis when the standard deviation of the alcohol outlet density (units/km2) within 400 m buffering area is 2.96, the standard deviation of SBP (mmHg) is 15.89, and the two-sided significance level is 0.05.
Results
Baseline Characteristics
Our data set for the analysis of the association between alcohol environment and cardiovascular risk factors included 5,641 individuals (3,244 men and 2,397 women) residing in 29 villages with median age of 29.1 years. Table 1 presents the sociodemographic characteristics of participants, densities and distances of alcohol outlets, and measures of alcohol intake and cardiovascular risk factors. The median intake of alcohol was 29.1 gram (interquartile range: 68.6 gram) per day and the densities of alcohol outlets (on and/or off-premise) within 400 m were higher than that within 1,600 m.
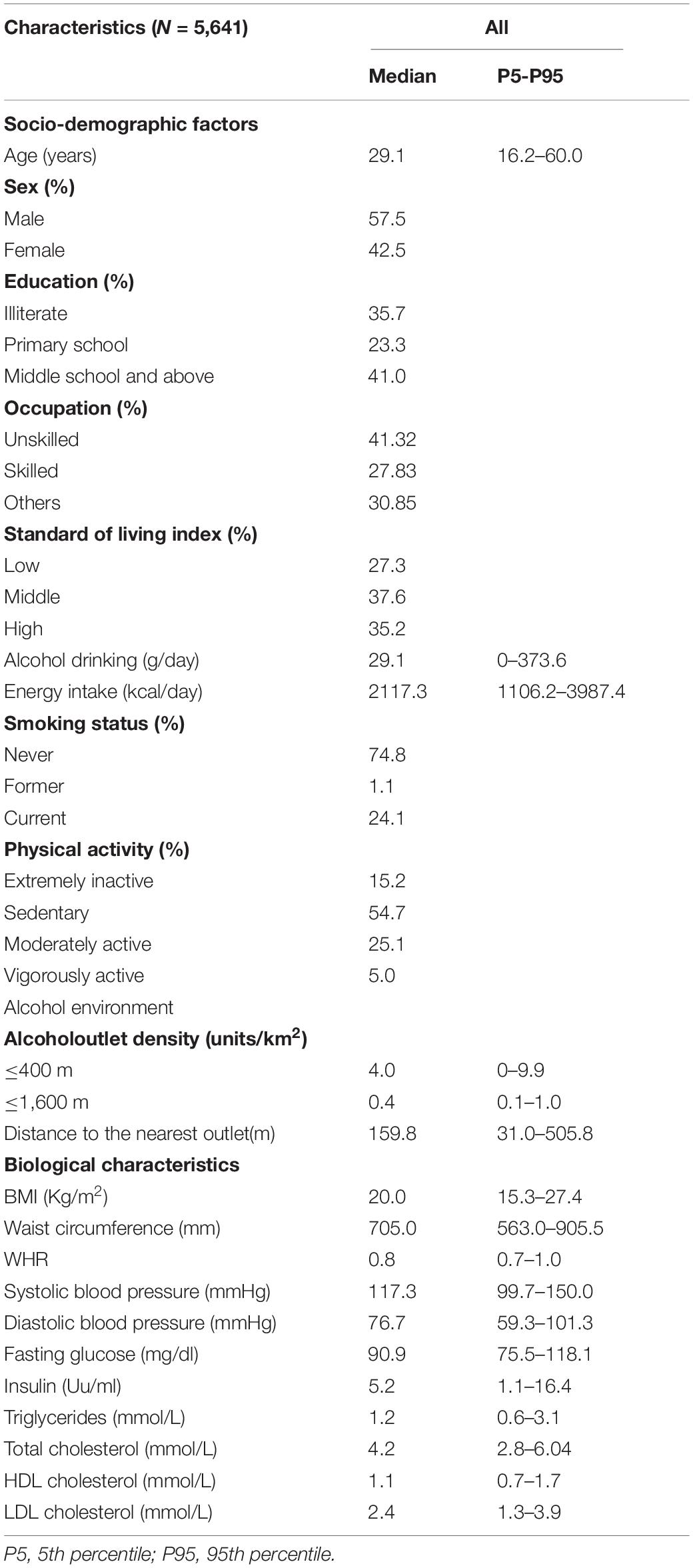
Table 1. Socio-demographic, food environment, and biological characteristics of APCAPS participants.
Alcohol Outlet and Alcohol Consumption
Table 2 presents associations between availability and accessibility of alcohol outlets and individual level of alcohol consumption. In model 1, compared with participants at the lowest tertile, those at the highest tertile of distance to the nearest alcohol outlet were more likely to have lower level of alcohol consumption [−14.07 g/day, 95% CI: −26.02, −2.12]. The association stayed robust in fully adjusted model 2 (−14.40 g/day, 95% CI: −26.21, −2.59). There was no association between density of alcohol outlet within 400 m buffering area or 1,600 m buffering area with daily alcohol intake.
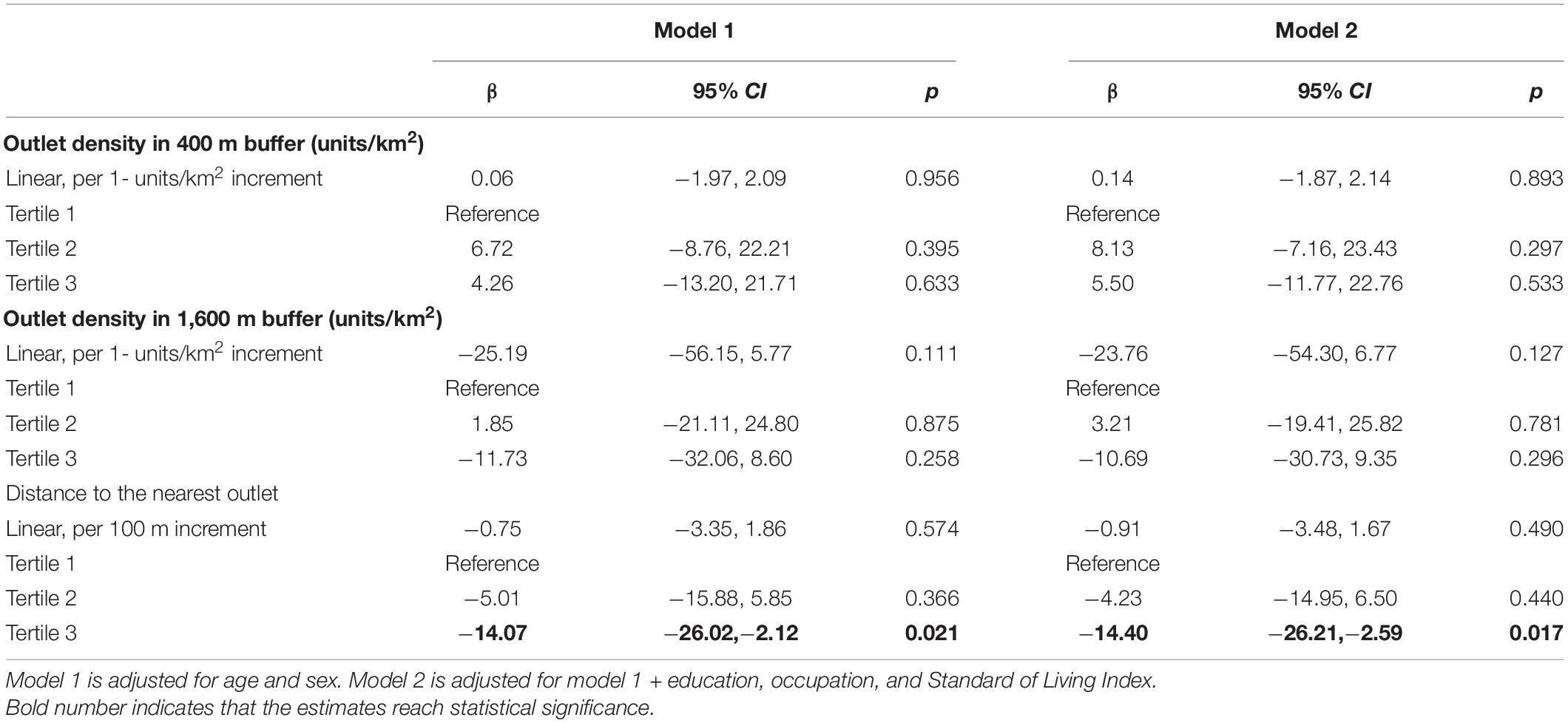
Table 2. Association between alcohol availability and accessibility with individual level of alcohol intake in APCAPS participants (n = 6,156).
Alcohol Outlet and Cardiovascular Risk Factors
The association between availability and accessibility of alcohol outlets and cardiovascular risk factors is presented in Table 3. In fully adjusted models, a unit per km2 increase in alcohol outlets’ density within 400 m buffering area was associated with an increase in waist circumference (1.45 mm, 95% CI: 0.13, 2.77), systolic blood pressure (SBP) (0.29 mmHg, 95% CI: 0.09, 0.49), and diastolic blood pressure (DBP) (0.19 mmHg, 95% CI: 0.03, 0.35). There was no association between densities of alcohol outlets within 1,600 m buffering area with cardiovascular risk factors.
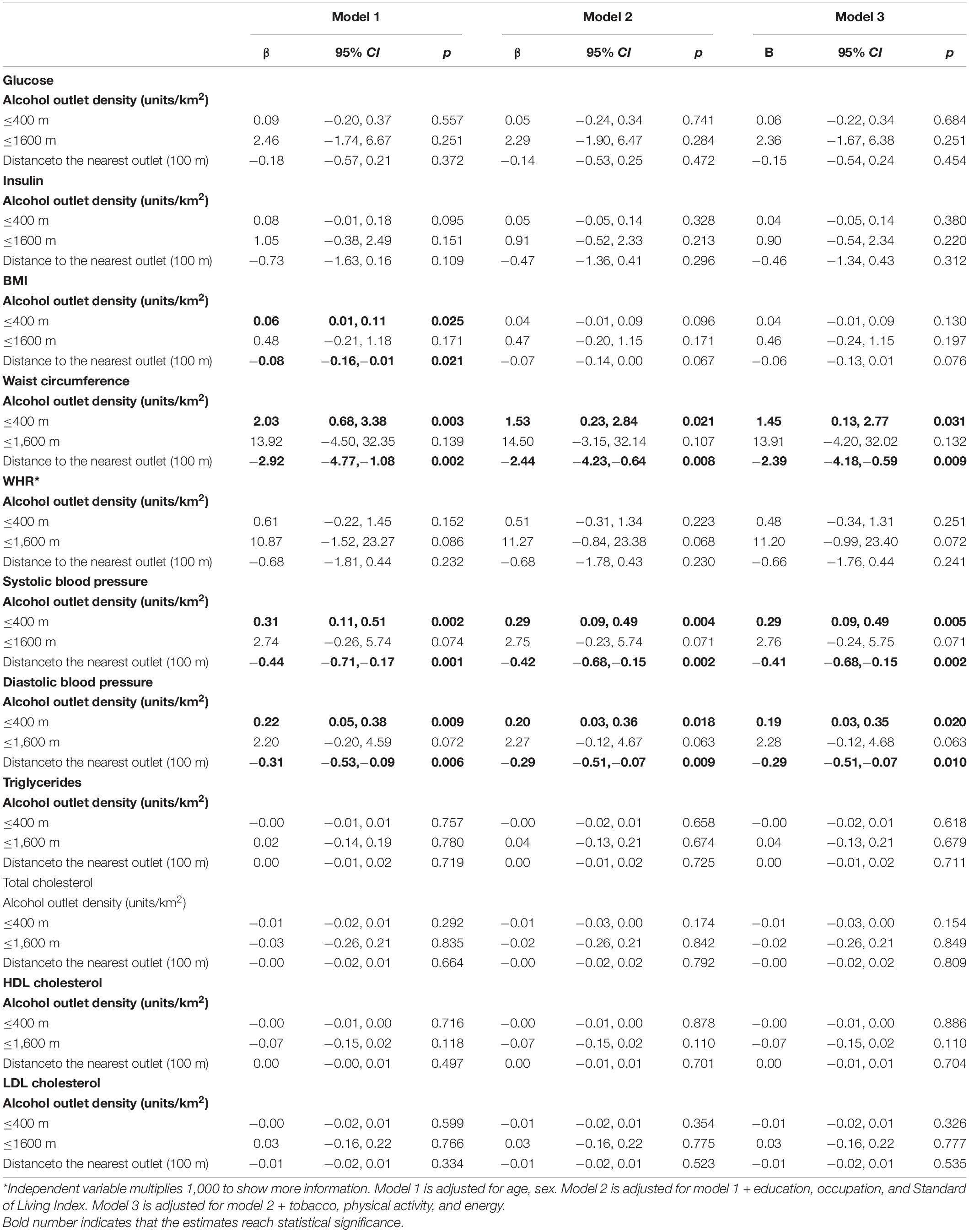
Table 3. Association between alcohol availability and accessibility with cardiovascular risk factors in APCAPS participants (n = 5,641).
In fully adjusted models, a unit per 100 m increase in distance to the closest alcohol outlet was associated with a decrease in waist circumference (−2.39 mm, 95% CI: −4.18, −0.59), SBP (−0.41 mmHg, 95% CI: −0.68, −0.15), and DBP (−0.29 mmHg, 95% CI: −0.51, −0.07). Association between density and distance of alcohol outlet with other cardiovascular risk factors was weak and inconsistent across different models.
Sensitivity Analysis
Supplementary Table 1 presents associations between availability and accessibility of alcohol outlets and cardiovascular risk factors after excluding participants with high blood pressure and diabetic disease (n = 5,294). The results were largely unchanged except the association between alcohol outlets density within 400 m buffering area and waist circumference. The significant association disappeared in fully adjusted model (1.15 mm, 95% CI: −0.12, 2.43).
Discussion
We examined associations between neighborhood alcohol environment with individual level alcohol intake and cardiovascular risk factors in data from the 3rd wave of follow-up of APCAPS. Greater distance to the nearest alcohol outlet was associated with a lower daily alcohol intake, waist circumference and blood pressure. Higher density of alcohol outlets within 400 m buffering area was associated with higher waist circumference and blood pressure. There was no link found between alcohol outlets within 1,600 m buffering zone and daily alcohol intake and cardiovascular risk factors. To the best of our knowledge, this is the first study to examine both availability and accessibility of alcohol outlets in the local neighborhood in relation to both alcohol intake and multiple cardiovascular risk factors in India.
Previous studies have indicated that density of alcohol outlets is significantly associated with increased alcohol consumption in developed countries (26–28). Few studies have been reported from the low- and middle-income countries. A study carried out in rural South Africa found that alcohol outlet density was not associated with prevalence of heavy drinking (11), which was in accordance with our results. We found no association between density of alcohol outlets within 400 m buffering area or 1,600 m buffering area with daily alcohol intake. Azar et al. found significant association between density of alcohol outlets and clubs with risky drinking only existed among residents in urban communities but not in rural areas of Australia (29). On the other hand, a systematic review found that density measures are far more frequently examined than distance measures in studies on alcohol environment and alcohol consumption (30). No significant association was found between the physical distance from an individual’s home to their nearest alcohol outlet with frequency and quantity of alcohol consumption in both urban and mixed communities of developed countries (31–33). However, a study carried out in Tanzania found that close distance to alcohol outlets may facilitate and increase adolescent alcohol use (10). In the current study, greater distance to the nearest alcohol outlet was associated with a decrease in daily alcohol consumption. The relationship between neighborhood alcohol outlet density and distance with alcohol consumption is complex and may vary due to differences in neighborhood design, travel patterns, local alcohol control policies, and enforcement, as well as drinking norms (34).
In a previous study carried out in south India, Li et al. found that higher density of unhealthy food vendors was associated with increased prevalence of obesity-related outcomes and blood pressure (35). Immoderate consumption of alcohol, like unhealthy food, is associated with serious health problems (36). To our knowledge, no study has been reported to assess the association between densities or physical distance of alcohol outlets with individual levels of cardiovascular risk factors, such as adiposity measures, glucose-insulin, blood pressure, and lipid profile. We found that not only density of alcohol outlets but also distance to the nearest alcohol outlet were associated with waist circumference and blood pressure. Annual gain in waist circumference was associated with increased consumption of alcoholic beverages in the PREDIMED trial (37). A systematic review and meta-analysis found that a reduction in alcohol intake was associated with increased blood pressure reduction in people who drank more than two drinks per day (38). Higher density and lower physical distance may increase the frequency of cues related to drinking and make alcohol more accessible, thus increasing the risk of obesity and high blood pressure through immoderate alcohol consumption.
Some limitations of this study must be acknowledged. One thing is that the coordinates of alcohol outlets were derived in 2016, which was 4 years after the third wave of follow-up in APCAPS. The temporal association between alcohol environment with higher levels of waist circumference and blood pressure cannot be ascertained in the present study. Awareness of having CVDs may change the behavior of alcohol access and alcohol drinking in participants and generate bias (39). Thus, we conducted sensitivity analysis in dataset after excluding participants with diagnosed hypertension and diabetes. The results were largely unchanged. Other limitations should also be mentioned. We only assessed the physical availability and accessibility of alcohol outlets. The available data did not allow us to look into other alcohol environment factors such as travel patterns, local alcohol control policies, or drinking norms, which could also influence alcohol consumption as well as cardiovascular risk factors. Moreover, the resulting data on alcohol use was self-reported through semi-quantitative questionnaires, which may have resulted in under-reporting by respondents (40).
Conclusion
Despite limitations, our study is the first to examine the association between neighborhood availability and accessibility of alcohol outlets with alcohol consumption as well as cardiovascular risk factors in south India. Shorter distance to the nearest alcohol outlet was associated with increased alcohol consumption. Higher waist circumference and blood pressure were associated with a shorter distance to the nearest alcohol outlet as well as a higher density of alcohol outlets. Neighborhood availability of alcohol outlets within immediate locality of participants’ households had a closer relationship with cardiovascular risk factors than that within the whole village. Public health policies designed to limit neighborhood availability and accessibility of alcohol outlets should be encouraged in south India.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
YL and PM: study conception and study design. AA, BK, and SK: data analysis. YL, PM, and AA: manuscript drafting. All authors have approved the submitted version and agreed to publication.
Funding
This study was supported by a Wellcome Trust Strategic Award Grant No Z/084674.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge our dedicated field teams led by Santhi Bhogadi and the study participants who made this study possible. We also acknowledge the contribution of Srivalli Addanki and Naveen Chittaluri to data processing and management and the reviewers for their constructive comments.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.844086/full#supplementary-material
References
1. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/S0140-6736(17)32152-9
2. India State-Level Disease Burden Initiative CVD Collaborators. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health. (2018) 6:e1339–51. doi: 10.1016/S2214-109X(18)30407-8
3. GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2018) 392:1015–35.
4. Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ. (2017) 356:j909. doi: 10.1136/bmj.j909
5. Jyani G, Prinja S, Ambekar A, Bahuguna P, Kumar R. Health impact and economic burden of alcohol consumption in India. Int J Drug Policy. (2019) 69:34–42. doi: 10.1016/j.drugpo.2019.04.005
6. Popova S, Giesbrecht N, Bekmuradov D, Patra J. Hours and days of sale and density of alcohol outlets: impacts on alcohol consumption and damage: a systematic review. Alcohol Alcohol. (2009) 44:500–16.
7. Chen MJ, Grube JW, Gruenewald PJ. Community alcohol outlet density and underage drinking. Addiction. (2010) 105:270–8. doi: 10.1111/j.1360-0443.2009.02772.x
8. Paschall MJ, Lipperman-Kreda S, Grube JW. Effects of the local alcohol environment on adolescents’ drinking behaviors and beliefs. Addiction. (2014) 109:407–16. doi: 10.1111/add.12397
9. Morrison CN, Byrnes HF, Miller BA, Wiehe SE, Ponicki WR, Wiebe DJ. Exposure to alcohol outlets, alcohol access, and alcohol consumption among adolescents. Drug Alcohol Depend. (2019) 205:107622. doi: 10.1016/j.drugalcdep.2019.107622
10. Ibitoye M, Kaaya S, Parker R, Likindikoki S, Ngongi L, Sommer M. The influence of alcohol outlet density and advertising on youth drinking in urban Tanzania. Health Place. (2019) 58:102141. doi: 10.1016/j.healthplace.2019.05.019
11. Leslie HH, Ahern J, Pettifor AE, Twine R, Kahn K, Gomez-Olive FX, et al. Collective efficacy, alcohol outlet density, and young men’s alcohol use in rural South Africa. Health Place. (2015) 34:190–8. doi: 10.1016/j.healthplace.2015.05.014
12. Treno AJ, Johnson FW, Remer LG, Gruenewald PJ. The impact of outlet densities on alcohol-related crashes: a spatial panel approach. Accid Anal Prev. (2007) 39:894–901. doi: 10.1016/j.aap.2006.12.011
13. Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. (2009) 373:2234–46. doi: 10.1016/S0140-6736(09)60744-3
14. Nesoff ED, Milam AJ, Pollack KM, Curriero FC, Bowie JV, Knowlton AR, et al. Neighbourhood alcohol environment and injury risk: a spatial analysis of pedestrian injury in Baltimore City. Inj Prev. (2019) 25:350–6. doi: 10.1136/injuryprev-2018-042736
15. Theall KP, Scribner R, Cohen D, Bluthenthal RN, Schonlau M, Lynch S, et al. The neighborhood alcohol environment and alcohol-related morbidity. Alcohol. (2009) 44:491–9. doi: 10.1093/alcalc/agp042
16. Richardson EA, Hill SE, Mitchell R, Pearce J, Shortt NK. Is local alcohol outlet density related to alcohol-related morbidity and mortality in Scottish cities? Health Place. (2015) 33:172–80. doi: 10.1016/j.healthplace.2015.02.014
17. Theall KP, Wallace M, Felker-Kantor E, Madkour AS, Brashear M, Ferguson T, et al. Neighborhood alcohol environment: differential effects on hazardous drinking and mental health by sex in persons living with HIV (PLWH). AIDS Behav. (2019) 23:3237–46. doi: 10.1007/s10461-019-02632-3
18. Kinra S, Rameshwar Sarma KV, Ghafoorunissa, Mendu VV, Ravikumar R, Mohan V, et al. Effect of integration of supplemental nutrition with public health programmes in pregnancy and early childhood on cardiovascular risk in rural Indian adolescents: long term follow-up of Hyderabad nutrition trial. BMJ. (2008) 337:a605. doi: 10.1136/bmj.a605
19. Kinra S, Radha Krishna KV, Kuper H, Rameshwar Sarma KV, Prabhakaran P, Gupta V, et al. Cohort profile: Andhra Pradesh Children and Parents Study (APCAPS). Int J Epidemiol. (2014) 43:1417–24. doi: 10.1093/ije/dyt128
20. Ebrahim S, Kinra S, Bowen L, Andersen E, Ben-Shlomo Y, Lyngdoh T, et al. The effect of rural-to-urban migration on obesity and diabetes in India: a cross-sectional study. PLoS Med. (2010) 7:e1000268. doi: 10.1371/journal.pmed.1000268
21. Kinra S, Johnson M, Kulkarni B, Rameshwar Sarma KV, Ben-Shlomo Y, Smith GD. Socio-economic position and cardiovascular risk in rural Indian adolescents: evidence from the Andhra Pradesh children and parents study (APCAPS). Public Health. (2014) 128:852–9. doi: 10.1016/j.puhe.2014.06.005
22. Matsuzaki M, Sullivan R, Ekelund U, Krishna KVR, Kulkarni B, Collier T, et al. Development and evaluation of the Andhra pradesh children and parent study physical activity questionnaire (APCAPS-PAQ): a cross-sectional study. BMC Public Health. (2016) 16:48. doi: 10.1186/s12889-016-2706-9
23. Roeschlau P, Bernt E, Gruber W. Enzymatic determination of total cholesterol in serum. Z Klin Chem Klin Biochem. (1974) 12:226.
24. Siedel J, Schiefer S, Rosseneu M, Bergeaud R, De Keersgieter W, Pautz B, et al. Immunoturbidimetric method for routine determinations of apolipoproteins A-I, A-II, and B in normo- and hyperlipemic sera compared with immunonephelometry. Clin Chem. (1988) 34:1821–5. doi: 10.1093/clinchem/34.9.1816
25. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. (1972) 18:499–502. doi: 10.1093/clinchem/18.6.499
26. Brenner AB, Borrell LN, Barrientos-Gutierrez T, Diez Roux AV. Longitudinal associations of neighborhood socioeconomic characteristics and alcohol availability on drinking: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Soc Sci Med. (2015) 145:17–25. doi: 10.1016/j.socscimed.2015.09.030
27. Foster S, Hooper P, Knuiman M, Lester L, Trapp G. Associations between proposed local government liquor store size classifications and alcohol consumption in young adults. Health Place. (2018) 52:170–3. doi: 10.1016/j.healthplace.2018.06.001
28. Slutske WS, Deutsch AR, Piasecki TM. Neighborhood alcohol outlet density and genetic influences on alcohol use: evidence for gene-environment interaction. Psychol Med. (2019) 49:474–82. doi: 10.1017/S0033291718001095
29. Azar D, White V, Coomber K, Faulkner A, Livingston M, Chikritzhs T, et al. The association between alcohol outlet density and alcohol use among urban and regional Australian adolescents. Addiction. (2016) 111:65–72. doi: 10.1111/add.13143
30. Shih RA, Mullins L, Ewing BA, Miyashiro L, Tucker JS, Pedersen ER, et al. Associations between neighborhood alcohol availability and young adolescent alcohol use. Psychol Addict Behav. (2015) 29:950–9. doi: 10.1037/adb0000081
31. Abbey A, Scott RO, Smith MJ. Physical, subjective, and social availability: their relationship to alcohol consumption in rural and urban areas. Addiction. (1993) 88:489–99. doi: 10.1111/j.1360-0443.1993.tb02055.x
32. Scribner RA, Cohen DA, Fisher W. Evidence of a structural effect for alcohol outlet density: a multilevel analysis. Alcohol Clin Exp Res. (2000) 24:188–95. doi: 10.1111/j.1530-0277.2000.tb04590.x
33. Young R, Macdonald L, Ellaway A. Associations between proximity and density of local alcohol outlets and alcohol use among Scottish adolescents. Health Place. (2013) 19:124–30. doi: 10.1016/j.healthplace.2012.10.004
34. Schonlau M, Scribner R, Farley TA, Theall K, Bluthenthal RN, Scott M, et al. Alcohol outlet density and alcohol consumption in Los Angeles county and southern Louisiana. Geospat Health. (2008) 3:91–101. doi: 10.4081/gh.2008.235
35. Li Y, Mallinson PAC, Bhan N, Turner C, Bhogadi S, Sharma C, et al. Neighborhood physical food environment and cardiovascular risk factors in India: cross-sectional evidence from APCAPS. Environ Int. (2019) 132:105108. doi: 10.1016/j.envint.2019.105108
36. Cohen D, Rabinovich L. Addressing the proximal causes of obesity: the relevance of alcohol control policies. Prev Chronic Dis. (2012) 9:E94. doi: 10.5888/pcd9.110274
37. Konieczna J, Romaguera D, Pereira V, Fiol M, Razquin C, Estruch R, et al. Longitudinal association of changes in diet with changes in body weight and waist circumference in subjects at high cardiovascular risk: the PREDIMED trial. Int J Behav Nutr Phys Act. (2019) 16:139. doi: 10.1186/s12966-019-0893-3
38. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. (2017) 2:e108–20. doi: 10.1016/S2468-2667(17)30003-8
39. Eames S, Hoffmann TC, Phillips NF. Evaluating stroke patients’ awareness of risk factors and readiness to change stroke risk-related behaviors in a randomized controlled trial. Top Stroke Rehabil. (2014) 21(Suppl. 1):S52–62. doi: 10.1310/tsr21S1-S52
Keywords: alcohol environment, availability, accessibility, alcohol intake, cardiovascular risk, APCAPS
Citation: Li Y, Mallinson PAC, Aggarwal A, Kulkarni B and Kinra S (2022) Association of Neighborhood Alcohol Environment With Alcohol Intake and Cardiovascular Risk Factors in India: Cross-Sectional Evidence From APCAPS. Front. Cardiovasc. Med. 9:844086. doi: 10.3389/fcvm.2022.844086
Received: 27 December 2021; Accepted: 05 April 2022;
Published: 29 April 2022.
Edited by:
Stefania Triunfo, University of Milan, ItalyReviewed by:
Tim Welborn, Sir Charles Gairdner Hospital, AustraliaMustafa Agah Tekindal, İzmir Kâtip Çelebi University, Turkey
Copyright © 2022 Li, Mallinson, Aggarwal, Kulkarni and Kinra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingjun Li, MjAxNjAzNDAzNkBobWMuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Yingjun Li
Yingjun Li Poppy Alice Carson Mallinson2†
Poppy Alice Carson Mallinson2† Bharati Kulkarni
Bharati Kulkarni Sanjay Kinra
Sanjay Kinra