- 1Department of Sport Rehabilitation, School of Kinesiology, Shanghai University of Sport, Shanghai, China
- 2Department of Cardiology, Xinhua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Department of Physiotherapy, MacLehose Medical Rehabilitation Center, Hospital Authority, Hong Kong, China
- 4Department Nursing and Allied Health, Swinburne University of Technology, Melbourne, VIC, Australia
- 5Department of Surgery, Melbourne Medical School, University of Melbourne, Melbourne, VIC, Australia
- 6Department of Physiotherapy, College of Rehabilitation Sciences, Shanghai University of Medicine and Health Sciences, Shanghai, China
- 7Department of Physiotherapy, School of Health and Rehabilitation Sciences, The University of Queensland, Brisbane, QLD, Australia
Background: Sit-To-Stand (STS) tests are reported as feasible alternatives for the assessment of functional fitness but the reliability of these tests in people with coronary artery disease (CAD) has not been reported. This study explored the test-retest reliability, convergent and known-groups validity of the five times, 30-sec and 1-min sit-to-stand test (FTSTS test, 30-s STS test and 1-min STS test respectively) in patients with CAD. The feasibility of applying these tests to distinguish the level of risk for cardiovascular events in CAD patients was also investigated.
Methods: Patients with stable CAD performed a 6MWT and 3 STS tests in random order on the same day. Receiver operating characteristic (ROC) curve analyses were conducted using STS test data to differentiate patients with low or high risk of cardiovascular events based on the risk level determined by distance covered in the 6MWT as > or ≤ 419 m. Thirty patients repeated the 3 STS tests on the following day.
Results: 112 subjects with diagnoses of atherosclerosis or post-percutaneous coronary intervention, or post-acute myocardial infarction (post-AMI) participated in the validity analysis. All 3 STS tests demonstrated moderate and significant correlation with the 6MWT (coefficient values r for the FTSTS, 30-s STS and 1-min STS tests were−0.53, 0.57 and 0.55 respectively). Correlations between left ventricular ejection fraction (LVEF) and all STS tests and between 6MWT and LVEF were only weak (r values ranged from 0.27 to 0.31). Subgroup analysis showed participants in the post-AMI group performed worse in all tests compared to non-myocardial infarction (non-MI) group. The area under the curve (AUC) was 0.80 for FTSTS (sensitivity: 75.0%, specificity: 73.8%, optimal cut-off: >11.7 sec), and the AUC, sensitivity, specificity and optimal cut-off for 30-s STS and 1-min STS test were 0.83, 75.0%, 76.2%, ≤ 12 repetitions and 0.80, 71.4%, 73.8%, ≤ 23 repetitions respectively. The intraclass correlation coefficients (ICC) for repeated measurements of the FTSTS, 30-s STS and 1-min STS tests were 0.96, 0.95 and 0.96 respectively, with the minimal detectable change (MDC95) computed to be 1.1 sec 1.8 repetitions and 3.9 repetitions respectively.
Conclusions: All STS tests demonstrated good test-retest reliability, convergent and known-groups validity. STS tests may discriminate low from high levels of risk for a cardiovascular event in patients with CAD.
Introduction
Coronary artery disease (CAD) is the leading cause of death worldwide and accounts for a significant disease burden in developing countries (1, 2). Cardiac rehabilitation (CR) is supported by evidence as key to CAD management and functional capacity is often a clinical outcome used to reflect the success of a CR programme (3). The 6-min walk test (6MWT) has been used as a prognostic tool to predict the risk of myocardial infarct, heart failure and death in CAD patients (4). The 6MWT demands no expensive or complicated equipment, however it does require a corridor which is at least 30 meters in length, and the full assessment procedure takes at least 20 min. Further, patient performance can be confounded by the motivation and unintentional encouragement provided by the operators (5). In contrast, the sit-to-stand (STS) test requires a chair and minimal space. It was first introduced in 1985 for the evaluation of lower limb muscle strength (6). Recently, an incremental STS test protocol was reported to be highly correlated with peak oxygen consumption during an exercise test in healthy individuals (7). STS tests are now considered feasible alternative tests for the assessment of functional fitness in older adults and in various patient populations (8–10).
Tests or measures in clinical medicine are normally used for three purposes: discriminate between patient characteristics, predict an outcome or inform the prognosis of a condition, and evaluate change over time or change after certain intervention (11). The STS tests have been used to discriminate levels of functional capacity in people with chronic respiratory illness (12, 13) and have also been used to evaluate the effect of pulmonary rehabilitation in people with chronic obstructive pulmonary disease (COPD) (14). The 1-min STS test was shown to be a strong predictor of 2-year mortality in people with COPD (15).
While the reliability and discriminative properties of various STS test protocols, including the five times sit-to-stand (FTSTS) test, 30-sec STS (30-s STS) test and 1-min STS (1-min STS) test, have been reported in different populations (16–18), a gold standard for testing the criterion validity of STS tests in discriminating levels of functional capacity in people with CAD is not yet available. There is therefore a need to establish the construct (convergent and known-groups) validity of STS tests in this population. Further, while STS test performance in patients with heart failure (19) and in patients enrolled in CR (20) have been reported, comparison of the reliability of various STS test protocols in patients with CAD has not been reported.
The focus of this current study is to examine the discriminative properties of the FTSTS, 30-s STS and 1-min STS tests. The primary objective of this current study is to examine the test-retest reliability, convergent and known-groups validity of the 3 STS tests. Convergent validity was examined through investigation of the correlation between STS test scores and the distance covered by the 6MWT, a valid test for measurement of functional capacity. Known-groups validity was examined through the evaluation of statistical and clinically important differences in STS tests of known groups, that is, participants with post-AMI and those without myocardial infarction (non-MI).
Following the assumption that STS tests are feasible alternative measurement tool for functional capacity, the secondary objective of the study was to explore the feasibility of using STS test protocols to discriminate the level of risk of cardiovascular events in people with CAD. Categorization of risk of cardiovascular events was adopted from a previous report, that patients who covered ≤ 419 m during a 6MWT were classified at high risk of cardiovascular events (4).
Materials and methods
Study design and participants
A cross-sectional study (Chinese Clinical Trial Registry Number: 2000037435) was conducted from July 2020 to February 2021. Approval to conduct the study was granted by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine (Approval Number: XHEC-C-2020-078-1). Participants were considered eligible for enrolment if they were older than 18 years with CAD with a diagnosis of atherosclerosis (as confirmed by angiography), post percutaneous coronary intervention, or at least 6 months post-acute myocardial infarction (post-AMI). The exclusion criteria included: a) raised cardiac troponin I level, b) acute infectious disease, respiratory disease, uncontrolled metabolic disease or hypertension; c) with neuromusculoskeletal, cognitive disorders, visual or auditory dysfunction that would affect performance of STS tests; d) heart failure at Class III or IV of the New York Heart Association (NYHA) classification; e) having previously participated in a CR program.
Procedures
Patients attending follow up at the Xinhua Hospital were screened for eligibility for this study. Eligible patients were invited to participate, with the nature of the study explained and written informed consent obtained from each patient prior to commencement of the study. The socio-demographic characteristics of each participant were then recorded.
Participants were asked to complete a 6MWT, FTSTS, 30-s STS and 1-min STS tests at random order on the same day. All tests were performed once only without any trial runs. This was deemed appropriate as test-retest reliability of FTSTS test was shown to be reliable with a single evaluation session (17). The order of testing was written in a card placed in a sealed envelope and the participants were asked to draw an envelope with the concealed order enclosed. A rest period of 30 min was set between the 6MWT and any of the STS tests, and all participants were given a 5-min rest period between each STS test protocol (21). Blood pressure (BP), heart rate (HR) and level of fatigue (using a CR-10 Borg scale) were recorded before and immediately after each test. Any adverse events were documented. All tests were conducted by the same physiotherapist.
All participants were also invited to draw from another sealed envelope which determined whether they were invited to return on the follow day to repeat the 3 STS tests.
Sit-to-stand test protocols
A chair without arms, with rubber tips on the legs, a hard seat of fixed height 46 cm was positioned against a wall. All 3 STS test protocols required the participant to commence in a seated position with the feet resting flat and ankle joints in the neutral position. All participants were given the instruction to perform the sit-to-stand task as quickly as possible with their arms crossed over the chest and hands on the shoulders (8). A standard STS movement was viewed as the legs being fully straightened when the stand phase concluded and the hip landing firmly on the chair when seated. A test would be terminated if the participant required assistance or was unable to complete the movement. No encouragement was provided during any STS test protocol.
The time for the participant to complete the STS movement five times was recorded for the FTSTS test (12). For 30-s and 1-min STS tests, subjects were required to perform as many STS movements as possible within 30 sec (22) or 1 min, respectively. The number of STS movements completed within the time required was recorded, as appropriate.
6MWT
The 6MWT was conducted following the American Thoracic Society guidelines for the 6MWT (23). All participants completed the 6MWT on a 30-meter flat corridor.
Statistical analysis
Data analyses were performed using the IBM SPSS Statistics 25.0 for Windows (IBM Corp., Armonk, NY) and the MedCalc 18.2.1 (Ostend, Belgium). Continuous variables were reported as mean and standard deviation (SD), and categorical data were shown as a number and percentage. The Kolmogorov-Smirnov test was used to check the normality of data distribution. Test-retest reliability, defined as consistency of the STS test scores recorded in the two separate days, was determined by the intraclass correlation coefficient (ICC) calculated by a two-way mixed model with absolute agreement method (24). The ICC was considered as poor, fair, good and excellent with values of <0.5, 0.5 to 0.75, 0.75 to 0.9, >0.9 respectively (25). Bland-Altman plots were constructed to display the distribution difference of repeated measurements and calculate the limits of agreement (LoA) via mean difference ± 1.96 SD of difference (26). Standard error of measurement (SEM) and a minimal detectable change with 95% confidence intervals (MDC95) were calculated with the formulae SD and SEM × 1.96 respectively, to estimate the measurement variability (27). Pearson's or Spearman's correlation coefficients were used to measure the magnitude of correlation between STS tests, 6MWT and LVEF, depending on the data distribution. The correlation was considered “negligible to weak,” “moderate,” and “well-accepted” with values <0.3, 0.3 to 0.6, and >0.6 respectively (28, 29). One way to support the convergent validity of the STS tests was a satisfactory correlation value between the STS scores and outcomes recorded with another tool valid for measurement of functional capacity, thus it was hypothesized that the correlation value (r) generated between STS tests and recorded 6MWD should be at least 0.5. Independent Samples t test or Mann-Whitney test was used to explore the known-groups validity through analysis of the differences in all tests between groups of patients with non-MI and post-AMI. Based on previous reported values of minimal clinically important differences (MCID) in STS tests in subjects with COPD, the between-group mean difference (MD) in STS tests was hypothesized to be ≥1.3s for the FTSTS test (12), ≥2 repetitions for 30-s STS test (14) and ≥3 repetitions for the 1-min STS test (30). Chi-square test was used to compare distributions of gender, coronary artery lesions, cardiovascular risk factors and type of medications between subgroups.
Lastly, if STS tests are deemed feasible alternatives to 6MWT in assessment of functional capacity in people with CAD, we wish to explore whether STS tests were able to discriminate participants with high and low risk of cardiovascular events, thus, receiver operating characteristic (ROC) curve analyses (31) were performed. The area under the curve (AUC) of the ROC curve would indicate the discriminative ability of the STS tests to differentiate the risk of cardiovascular events. The selection of the optimal cut-off scores for the STS tests was based on principle of minimizing the misclassification with minimum absolute difference between sensitivity and specificity (32). Based on a previous report by Beatty and colleagues, the “cut-off” value adopted in this study to differentiate participants with low or high risk of cardiovascular events was 419 m from the 6MWT (4). The AUC of all STS tests were compared. All statistical tests were two-tailed with the level of significance set at 0.05.
Sample size estimation
With two observations per subject, to achieve 80% power to detect an estimated ICC of 0.8 under the alternative hypothesis, and with the ICC estimated as 0.5 under the null hypothesis, with a significance level of 0.05, the minimum sample size for the STS test-retest reliability was computed as 22. For the known-groups validity testing, the sample size estimation was based on a hypothesized effect size index of 0.6 in testing the mean STS test difference between groups of non-MI and post-AMI patients, using a two-tailed independent t-test with a level of significance of 0.05 and statistical power of 0.8. A minimum of 90 patients was required. In the ROC curve analyses of STS tests for differentiating patients with low or high risk of cardiovascular events, a minimum sample of 82 patients was required to achieve 80% power to detect a difference of 0.15 between the AUC of the ROC curve analysis under the null hypothesis of 0.70 and an AUC under the alternative hypothesis of 0.85 using a two-sided z-test at a significance level of 0.05. All the sample size estimations were performed using the PASS 15.0.5 (NCSS, Kaysville, Utah, USA).
Results
Subjects characteristics
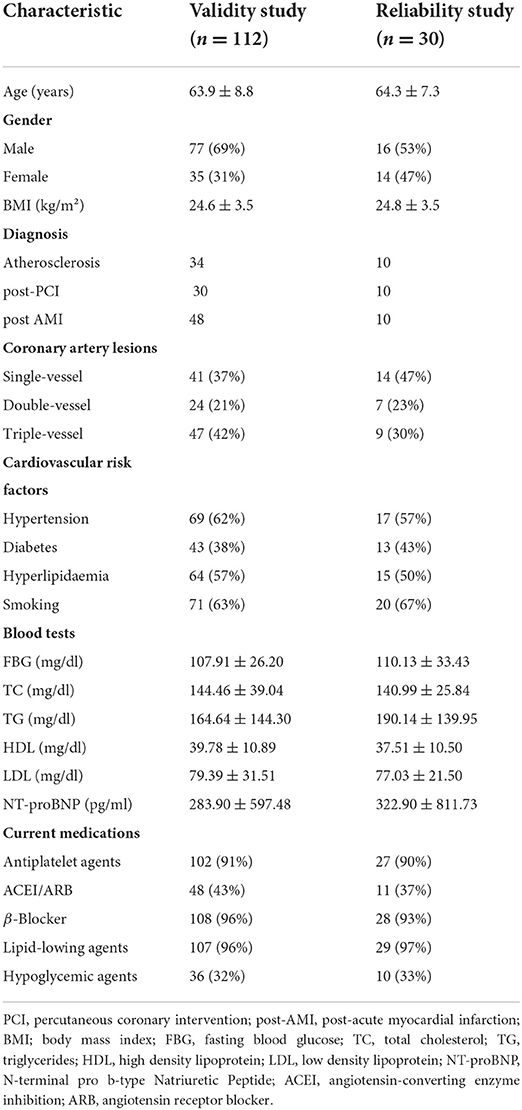
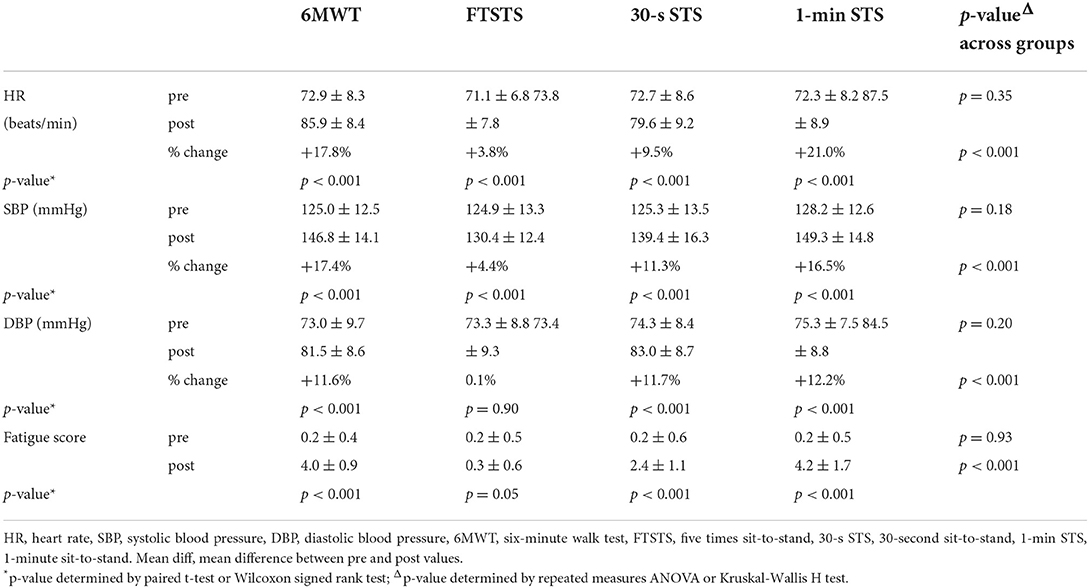
A total of 112 patients (mean age 63.9 ± 8.8 years, male 69%) were included in the study and the mean age of the 30 patients participated in the reliability tests was 64.3 ± 7.3 years, (males 53%). The number of post-AMI and non-MI participants was 48 and 64 respectively. Demographic characteristics of all patients are summarized in Table 1. Table 2 displays the HR, BP and level of fatigue at pre and immediately post STS tests and 6MWT. There was no adverse event during all tests. In the post-AMI group, 1 patient required a permanent pacemaker, 2 patients received coronary arterial bypass grafting operations.
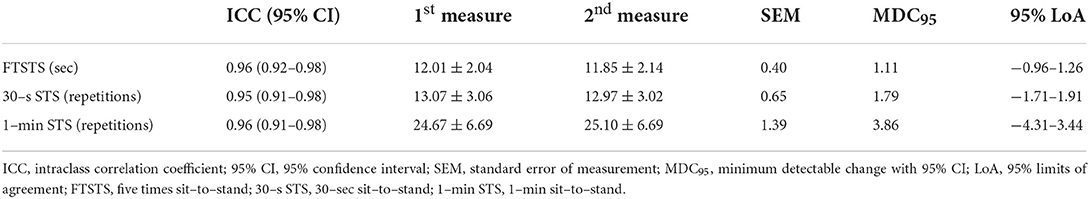
Relative and absolute reliability
The relative reliability for FTSTS, 30-s STS, 1-min STS tests were excellent with ICC values all above 0.95 between the two testing days in all STS tests. The minimum detectable change values with 95% confidence interval (MDC95) were 1.11 s, 1.79 repetitions and 3.86 repetitions, respectively (Table 3).
Convergent validity
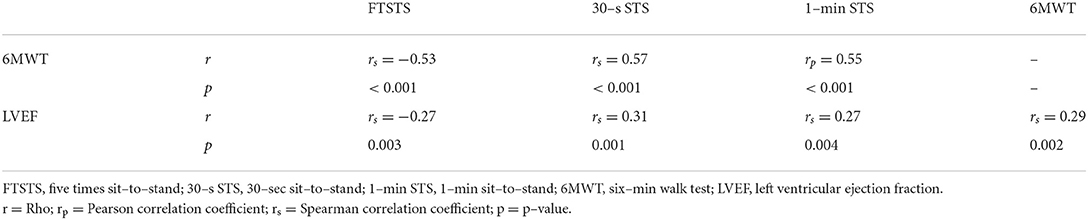
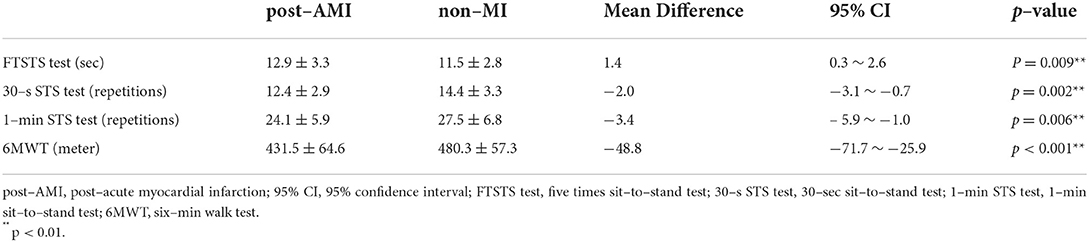
Correlation between performance of 6MWT and the 3 STS tests were moderate (FTSTS test, r = −0.53, p < 0.001; 30-s STS test, r = 0.57, p < 0.001; 1-min STS test, r = 0.55, p < 0.001). Correlations between recorded LVEF and STS performance or with 6MWT were both weak (Table 4, Figure 1).
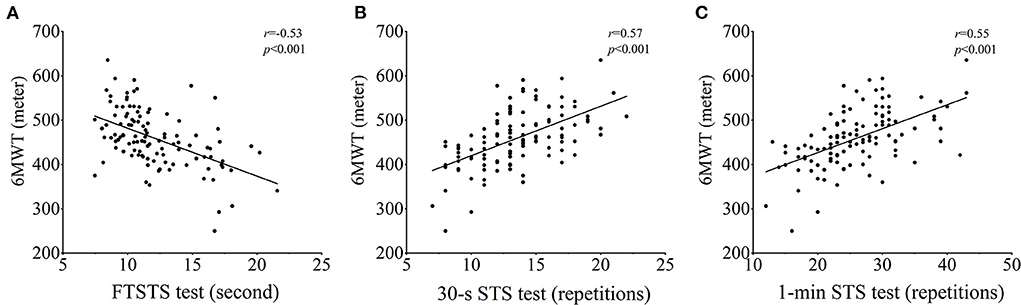
Figure 1. Correlations between 6MWT and the 3 STS tests. FTSTS test: five times sit-to-stand test, 30-s STS test: 30-sec sit-to-stand test, 1-min STS test: 1-min sit-to-stand test, 6MWT: six-min walk test.
Known-groups validity
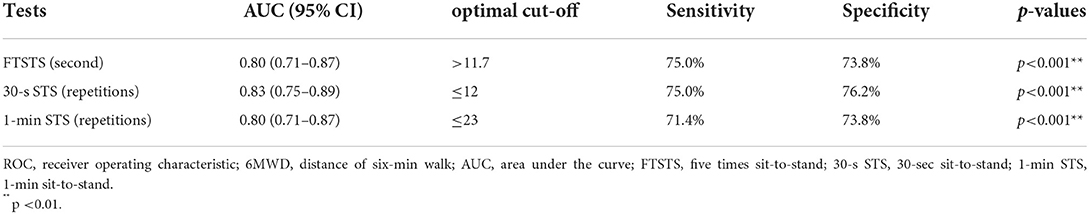
Table 5 displays results of known-groups validity analyses between patients in the post-AMI and non-MI groups. Patients with post-AMI required significantly longer time in completion of the FTSTS test, means difference (MD) and 95%CI being 1.4 s, 0.3 to 2.6, (p = 0.009), less repetitions in both the 30-s STS, MD−2.0, 95% CI: −3.1 to −0.7, (p = 0.002) and 1-min STS test MD−3.4, 95%CI: −5.9 to −1.0 (p = 0.006); the distance covered in the 6MWT (431.5 ± 64.6 vs. 480.3 ± 57.3, MD −48.8, 95% CI: −71.7 to −25.9, p < 0.001) was also less in this group (Table 5, Figure 2). These mean differences were similar or larger than the pre-specified differences with reference to the MCID values of the STS tests of patients with COPD.
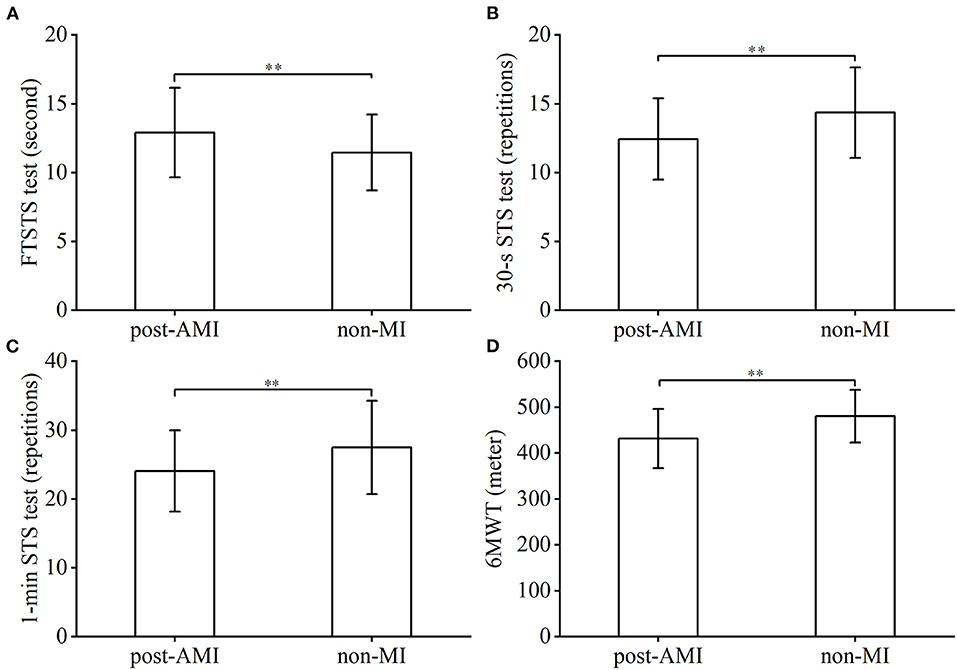
Figure 2. Intergroup comparison of STS tests and 6MWT performance. FTSTS test: five times sit-to-stand test, 30-s STS test: 30-sec sit-to-stand test, 1-min STS test: 1-min sit-to-stand test, 6MWT: six-min walk test, post-AMI: post-acute myocardial infarction. ** p < 0.01.
ROC curve analysis
A total of 84 patients achieved more than 419 m in their 6MWT and were thus classified as low- risk cardiovascular event group (4), 28 patients who covered ≤ 419 m were in the high-risk group. ROC curve analysis illustrated that the AUC of FTSTS, 30-s STS,and 1-min STS tests were 0.80 (sensitivity: 75.0%, specificity: 73.8%, optimal cut-off: 11.7 s), 0.83 (sensitivity: 75.0%, specificity: 76.2%, optimal cut-off: 12 repetitions), and 0.80 (sensitivity: 71.4%, specificity: 73.8%, optimal cut-off: 23 repetitions) respectively (Table 6). There were no statistically significant differences in the AUC of the ROC curve analyses among the three STS tests.
Discussion
The use of FTSTS test has been shown to be an instrument of high reliability in healthy adults (33) as well as in people with spinal cord injury (34), hip arthroplasty (17) and in people with chronic obstructive pulmonary disease (12). The 1-min STS test and 30-s STS test were also shown to be reliable measures in people with pulmonary hypertension (22), total knee arthroplasty (35), with COPD (13) and cystic fibrosis (36). This current study is the first that compared all three STS tests in the same population of people with CAD. Findings of our study demonstrated excellent test-retest reliability for all 3 STS tests in this subject-cohort. Further, we found that compared to FTSTS and 30-s STS tests, the 1-min STS test induced the greatest changes in heart rate and SBP, and associated with the highest post-test fatigue score (Table 2). Amongst the 3 STS tests, changes induced by the 1-min STS test were closest to the physiological changes induced by the 6MWT. This suggests that the 1-min STS test is superior than 30-s STS and FTSTS tests if considered as an assessment tool for functional capacity in people with CAD. Our findings were in accord with a previous report which recommended the 1-min STS test to be a superior STS protocol for evaluation of functional capacity in subjects with COPD (8). Further, oxygen consumption was shown to be highest during a 1-min STS test compared to FTSTS in a cohort of patients with COPD (30). Although we have not measured oxygen consumption during the STS tests in our participants with CAD, we postulate that the pattern of oxygen uptake during STS tests would be similar in our subject cohort compared to those with COPD; further analysis is necessary to confirm this assumption.
As anticipated, findings of the current study illustrated moderate correlation between the 3 STS tests and the 6MWT, the correlation coefficient data of our study are similar to those previously reported in community-dwelling older adults (10) and in a cohort of patients with COPD (37). The correlation between LVEF and 6MWT and between LVEF and any STS tests was however only weak. This is not surprising. A lack of correlation between distanced covered in a 6MWT and ejection fraction was also reported in patients with heart failure (38). Exercise capacity was shown to be inversely associated with diastolic dysfunction but not associated with variation of left ventricular systolic function in people with LVEF within normal range (39). The LVEF of our patient cohort was all above 56%, it is therefore not surprising that there existed only a weak correlation between LVEF and exercise capacity (reflected by 6MWT or STS tests). While cardiac dysfunction partly contributes to poor exercise capacity, skeletal muscle fatigability plays an important mechanism in exercise tolerance (40); further, in patients with a normal ejection fraction, exercise capacity is associated with left ventricular dimensions (41), however, assessment of skeletal muscle fatigability and appraisal of left ventricular dimension was outside of the scope of this study.
The 6MWT has been suggested to be a prognostic tool for cardiovascular events in patients with stable CAD (4). Beatty and colleagues reported that patients in the lowest quartile of 6MWD of 87-419 m had 4 times the risk of cardiovascular events compared to those in the highest 6MWD quartile of 544-837 m. Based on Beatty and colleagues' work, we used 6MWD of 419 m to demarcate high or low-risk cardiovascular event groups. With ROC curve analysis of our data, we showed that the 3 STS tests demonstrated good discriminative ability to differentiate patients between high and low risk cardiovascular events. Results of this analysis suggest that for patients with CAD, those who required more than 11.7 sec to complete a FTSTS test, or those who completed <12 repetitions of STS sequence in 30 sec or <23 STS-repetitions in 1 min were subjected to higher risk of cardiovascular events.
The MDC95 data generated from this study illustrated the measurement errors on repeated measurements of the STS tests. The MDC95 value for FTSTS test was previously reported in patients with COPD to be 3.1s (12). Our study showed that the MDC95 value for FTSTS test in people with CAD was 1.1s. This suggests that the measurement error of FTSTS test was less in our cohort of participants with CAD compared to people with COPD. Similarly, MDC95 value for the 30-s STS test reported in subjects with COPD (42) was also higher than that generated in this study. The MDC95 of 1-min STS test reported by Crook and colleagues (30) was however smaller than our results (2.2 repetitions compared to 3.86 repetitions in our CAD cohort). Direct comparison between our study and previous reports however may not be appropriate. As the MDC95 in other reports were generated from tests conducted in patients with COPD, whose exercise capacity was limited by impairment of the ventilatory system, and our data were obtained from patients with CAD, whose functional capacity is often restricted by cardiac performance.
Smoking, hyperlipaemia, hyperglycaemia, and hypertension are known risks factors of cardiovascular disease (43). Table 1 shows that the rate of smoking is high amongst our participants. Unfortunately, China is the largest consumer of tobacco in the world (WHO-Tobacco in China) (44) and smoking prevalence is about 26.6% (45); there are more than 300 million smokers in China, this suggests that greater effort is required to foster public health strategies of smoking cessation.
In summary, this study showed that all 3 STS tests have excellent test-retest reliability. The MDC95 values reported in this study provide a useful guide for the versatile use of STS protocols. The relationship of the STS tests with 6MWT demonstrated that these tests have good convergent validity in assessment of functional capacity in patients with CAD. Known-groups validity of these STS test was illustrated through distinct performance level by non-MI and post-AMI groups. STS tests are easy to perform and can be used as an assessment as well as an exercise training tool. Lastly this study inferred that STS test can also be considered as a discriminative tool to predict high or low risk of cardiovascular events in patients with CAD.
Limitations of the study
This study demonstrated a satisfactory correlation between 6MWD and the STS tests and proposed that STS tests can be considered as a useful tool to assess function capacity. While we have demonstrated similar haemodynamic responses between 6MWT and the STS test, we did not have appropriate equipment to measure oxygen consumption during the STS tests. Information on oxygen uptake during the STS test would provide a more detailed picture of physiological demands of STS tests.
High and low risk cardiovascular events was categorized using 6MWD of 419 m as the demarcation level. While the predictive validity of this assumption was proven (4), inclusion of cumulative biometric risk factors may provide a stronger profile of risks of cardiovascular events. Validity of an index which combines the 6MWD and biometric risk factors requires further investigation.
The focus of this study was to establish discriminative properties of the three STS tests; establishment of the evaluative and prognostic properties of these tests in people with CAD was outside the scope of this study. Further research in examining the evaluative and prognostic value of STS tests is warranted.
Conclusion
This is the first study that compared FTSTS test, 30-s STS test, and 1-min STS test in patients with CAD. This study showed that all 3 STS tests had good test-retest reliability, convergent and known-groups validity in assessing functional capacity in CAD patients. All 3 STS tests demonstrated good discriminative property in distinguishing patients with high and low risk of cardiovascular events and as such may inform the individualized clinical management, targeted exercise programmes and rehabilitation in this patient population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine (Approval Number: XHEC-C-2020-078-1). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Study conceptualization: ZW, JY, SM, JL, JH, and AJ. Data curation: ZW, JY, SM, JL, YY, and TZ. Statistical analysis: RT and DE-A. Manuscript preparation and writing the first draft: ZW, JY, and SM. Writing the section of the manuscript: JL, YY, TZ, DE-A, RT, JH, and AJ. All authors contributed to manuscript revision and have read and approved the final version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 31870936).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CAD, coronary artery disease; CR, cardiac rehabilitation; 6MWT, 6-min walk test; STS, sit-to-stand; FTSTS test, five times sit-to-stand test; 30-s STS test, 30-sec sit-to-stand test; 1-min STS test, 1-min sit-to-stand test; LVEF, left ventricular ejection fraction; post-PCI, post percutaneous coronary intervention; non-MI, non-myocardial infarction; post-AMI, post-acute myocardial infarction; BP, blood pressure; HR, heart rate; SD, standard deviation; ICC, intraclass correlation coefficient; LoA, limits of agreement; SEM, standard error of measurement; MDC95, minimal detectable change with 95% confidence interval; ANOVA, one-way analysis of variance; ROC, receiver operating characteristic; AUC, area under the curve; COPD, chronic obstructive pulmonary disease; 6MWD, the distance of 6MWT; MCID, minimal clinically important difference; MD, mean difference.
References
1. World Health Organisation. The Top 10 Causes of Death. (2021). Available online at: https://www.who.int/news- room/fact-sheets/detail/the-top-10-causes-of-death (accessed May 22, 2022).
2. Roser M, Ritchie H. Burden of disease. Institute for health metrics evaluation. (2018). Available online at: : https://ourworldindata.org/burden-of-disease (accessed May 22, 2022).
3. Prabhu NV, Maiya AG, Prabhu NS. Impact of cardiac rehabilitation on functional capacity and physical activity after coronary revascularization: a scientific review. Cardiol Res Pract. (2020) 2020:1–9. doi: 10.1155/2020/1236968
4. Beatty AL, Schiller NB, Whooley MA. Six-Minute walk test as a prognostic tool in stable coronary heart disease. Arch Int Med. (2012) 172:2198. doi: 10.1001/archinternmed.2012.2198
5. Singh SJ, Puhan MA, Andrianopoulos V, Hernandes NA, Mitchell KE, Hill CJ, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Res J. (2014) 44:1447–78. doi: 10.1183/09031936.00150414
6. Csuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strength. Am J Med. (1985) 78:77–81. doi: 10.1016/0002-9343(85)90465-6
7. Nagasawa Y, Nakamura K, Yokokawa Y, Ohira M. Validity and reproducibility of an incremental sit-to-stand exercise test in healthy middle-aged individuals. J Physical Therapy Sci. (2019) 31:414–7. doi: 10.1589/jpts.31.414
8. Morita AA, Bisca GW, Machado FVC, Hernandes NA, Pitta F, Probst VS, et al. Best protocol for the sit-to-stand test in subjects with COPD. Respir Care. (2018) 63:1040–9. doi: 10.4187/respcare.05100
9. Silva PF, Quintino LF, Franco J, Faria CD. Measurement properties and feasibility of clinical tests to assess sit-to-stand/stand-to-sit tasks in subjects with neurological disease: a systematic review. Brazilian J Phys Therapy. (2014) 18:99–110. doi: 10.1590/S1413-35552012005000155
10. Yee XS, Ng YS, Allen JC, Latib A, Tay EL, Abu Bakar HM, et al. Performance on sit-to-stand tests in relation to measures of functional fitness and sarcopenia diagnosis in community-dwelling older adults. Eur Rev Aging Phys Activity. (2021) 18:1. doi: 10.1186/s11556-020-00255-5
11. Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chronic Dis. (1985) 38:27–36. doi: 10.1016/0021-9681(85)90005-0
12. Jones SE, Kon SSC, Canavan JL, Patel MS, Clark AL, Nolan CM, et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax. (2013) 68:1015–20. doi: 10.1136/thoraxjnl-2013-203576
13. Reychler G, Boucard E, Peran L, Pichon R, Le Ber-Moy C, Ouksel H, et al. One minute sit-to-stand test is an alternative to 6MWT to measure functional exercise performance in COPD patients. Clin Respir J. (2018) 12:1247–56. doi: 10.1111/crj.12658
14. Zanini A, Crisafulli E, D'Andria M, Gregorini C, Cherubino F, Zampogna E, et al. Minimum clinically important difference in 30-s sit-to-stand test after pulmonary rehabilitation in subjects with COPD. Respir Care. (2019) 64:1261–9. doi: 10.4187/respcare.06694
15. Puhan MA, Siebeling L, Zoller M, Muggensturm P, Riet GT. Simple functional performance tests and mortality in COPD. Eur Resp J. (2013) 42:956–63. doi: 10.1183/09031936.00131612
16. Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Quarter Ex Sport. (1999) 70:113–9. doi: 10.1080/02701367.1999.10608028
17. Özden F, Coşkun G, Bakirhan S. The test-retest reliability and concurrent validity of the five times sit to stand test and step test in older adults with total hip arthroplasty. Experimental Gerontol. (2020) 142:111143. doi: 10.1016/j.exger.2020.111143
18. Reychler G, Pincin L, Audag N, Poncin W, Caty G. One-minute sit-to-stand test as an alternative tool to assess the quadriceps muscle strength in children. Res Med Res. (2020) 78:100777. doi: 10.1016/j.resmer.2020.100777
19. Yang C, Xu G, Lan Y. The measurement of 5-minutes-sit-to-stand test performance in patients with chronic heart failure. Chin J Rehabili Med. (2015) 30:661–6. doi: 10.3969/j.issn.1001-1242.2015.07.006
20. Puthoff ML, Saskowski D. Reliability and responsiveness of gait speed, five times sit to stand, and hand grip strength for patients in cardiac rehabilitation. Cardiopulm Phys Ther J. (2013) 24:31–7. doi: 10.1097/01823246-201324010-00005
21. Gurses HN, Zeren M, Denizoglu Kulli H, Durgut E. The relationship of sit-to-stand tests with 6-minute walk test in healthy young adults. Medicine. (2018) 97:e9489. doi: 10.1097/MD.0000000000009489
22. Kahraman BO, Ozsoy I, Akdeniz B, Ozpelit E, Sevinc C, Acar S, et al. Test-retest reliability and validity of the timed up and go test and 30-second sit to stand test in patients with pulmonary hypertension. Int J Cardiol. (2020) 304:159–63. doi: 10.1016/j.ijcard.2020.01.028
23. Statement ATS. American Journal of Respiratory and Critical Care. Medicine. (2002) 166:111–17. doi: 10.1164/ajrccm.166.1.at1102
24. Qin S, Nelson L, McLeod L, Eremenco S, Coons SJ. Assessing test-retest reliability of patient-reported outcome measures using intraclass correlation coefficients: recommendations for selecting and documenting the analytical formula. Quality Life Res. (2019) 28:1029–33. doi: 10.1007/s11136-018-2076-0
25. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. (2016) 15:155–63. doi: 10.1016/j.jcm.2016.02.012
26. Giavarina D. Understanding bland altman analysis. Biochemia medica. (2015) 25:141–51. doi: 10.11613/BM.2015.015
27. Furlan L, Sterr A. The applicability of standard error of measurement and minimal detectable change to motor learning research—a behavioral study. Front Human Neurosci. (2018) 12:95 doi: 10.3389/fnhum.2018.00095
28. Andresen EM. Criteria for assessing the tools of disability outcomes research. Arch Physical Med Rehabili. (2000) 81(12 Suppl. 2):S15–20. doi: 10.1053/apmr.2000.20619
29. Post MW. What to do with “Moderate” reliability and validity coefficients? Arch Physical Med Rehabili. (2016) 97:1051–2. doi: 10.1016/j.apmr.2016.04.001
30. Crook S, Büsching G, Schultz K, Lehbert N, Jelusic D, Keusch S, et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Euro Resp J. (2017) 49:1601871. doi: 10.1183/13993003.01871-2016
31. Streiner DL, Cairney J. What's under the ROC? an introduction to receiver operating characteristics curves. Can J Psychiatry. (2007) 52:121–8. doi: 10.1177/070674370705200210
32. Unal I. Defining an optimal cut-point value in roc analysis: an alternative approach. Comput Math Methods Med. (2017) 2017:1–14. doi: 10.1155/2017/3762651
33. Northgraves MJ, Hayes SC, Marshall P, Madden LA, Vince RV. The test-retest reliability of four functional mobility tests in apparently healthy adults. Isokinet Exerc Sci. (2016) 24:171–9. doi: 10.3233/IES-160614
34. Khuna L, Thaweewannakij T, Wattanapan P, Amatachaya P, Amatachaya S. Five times sit-to-stand test for ambulatory individuals with spinal cord injury: a psychometric study on the effects of arm placements. Spinal Cord. (2020) 58:356–64. doi: 10.1038/s41393-019-0372-3
35. Unver B, Kalkan S, Yuksel E, Kahraman T, Karatosun V. Reliability of the 50-foot walk test and 30-sec chair stand test in total knee arthroplasty. Acta Ortopedica Brasileira. (2015) 23:184–7. doi: 10.1590/1413-78522015230401018
36. Radtke T, Puhan MA, Hebestreit H, Kriemler S. The 1-min sit-to-stand test A simple functional capacity test in cystic fibrosis? J Cystic Fibrosis. (2016) 15:223–6. doi: 10.1016/j.jcf.2015.08.006
37. Zhang Q, Li Y, Li X, Yin Y, Li R, Qiao X, et al. A comparative study of the five-repetition sit-to-stand test and the 30-second sit-to-stand test to assess exercise tolerance in COPD patients. Int J Chron Obstruct Pulmon Dis. (2018) 13:2833–9. doi: 10.2147/COPD.S173509
38. Muoneme AS, Isiguzo GC, Iroezindu MO, Okeahialam BN. Relationship between Six-Minute Walk Test and Left Ventricular Systolic Function in Nigerian Patients with Heart Failure. West Afr J Med. (2015) 34:133–8.
39. Grewal J, McCully RB, Kane GC, Lam C, Pellikka PA. Left ventricular function and exercise capacity. JAMA. (2009) 301:286–94. doi: 10.1001/jama.2008.1022
40. Keller-Ross ML, Larson M, Johnson BD. Skeletal muscle fatigability in heart failure. Front Physiol. (2019) 10:129. doi: 10.3389/fphys.2019.00129
41. Meyer M, McEntee RK, Nyotowidjojo I, Chu G, Lewinter MM. Relationship of exercise capacity and left ventricular dimensions in patients with a normal ejection fraction. An Exploratory Study Plos ONE. (2015) 10:e0119432. doi: 10.1371/journal.pone.0119432
42. Hansen H, Beyer N, Frlich A, Godtfredsen N, Bieler T. Intra- and inter-rater reproducibility of the 6-minute walk test and the 30-second sit-to-stand test in patients with severe and very severe COPD. Int J Chron Obstruct Pulmon Dis. (2018) 13:3447–57. doi: 10.2147/COPD.S174248
43. Fioranelli M, Bottaccioli AG, Bottaccioli F, Bianchi M, Rovesti M, Roccia MG. Stress and Inflammation in Coronary Artery Disease: A Review Psychoneuroendocrineimmunology-Based. Front Immunol. (2018) 9:031 doi: 10.3389/fimmu.2018.02031
44. World Health Organisation. Tobacco in China. Available online at: https://www.who.int/China/health-topics/tobacco (accessed May 20, 2022).
Keywords: coronary artery disease, sit-to-stand, reliability, validity, discriminative ability, 6-minute walk test
Citation: Wang Z, Yan J, Meng S, Li J, Yu Y, Zhang T, Tsang RCC, El-Ansary D, Han J and Jones AYM (2022) Reliability and validity of sit-to-stand test protocols in patients with coronary artery disease. Front. Cardiovasc. Med. 9:841453. doi: 10.3389/fcvm.2022.841453
Received: 22 December 2021; Accepted: 04 August 2022;
Published: 25 August 2022.
Edited by:
Paolo Calabrò, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Milo Alan Puhan, University of Zurich, SwitzerlandIlaria Cavallari, Policlinico Universitario Campus Bio-Medico, Italy
Copyright © 2022 Wang, Yan, Meng, Li, Yu, Zhang, Tsang, El-Ansary, Han and Jones. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Han, amlhLmhhbkBjYW5iZXJyYS5lZHUuYXU=; Alice Y. M. Jones, YS5qb25lczE1QHVxLmVkdS5hdQ==
†These authors have contributed equally to this work and share first authorship
 Zheng Wang
Zheng Wang Jianhua Yan
Jianhua Yan Shu Meng2†
Shu Meng2† Jiajia Li
Jiajia Li Raymond C. C. Tsang
Raymond C. C. Tsang Jia Han
Jia Han Alice Y. M. Jones
Alice Y. M. Jones