- Department of Anesthesiology, First Affiliated Hospital of Nanchang University, Nanchang, China
Purposes: Pediatric open cardiac surgical patients usually suffer from acute pain after operation. The current work aimed to explore the impact of bilateral PIFB in children suffering from open cardiac surgery.
Methods: This work randomized altogether 110 child patients as bilateral PIFB (PIF) and non-nerve block (SAL) groups. This work adopted post-operative pain at exercise and rest statuses as the primary endpoint, whereas time-to-drain removal/extubation/initial defecation, intraoperative/post-operative fentanyl use, and length of ICU and hospital stay as the secondary endpoints.
Results: MOPS were significantly higher at 24-h post-operatively at coughing and rest statuses in SAL group compared with PIF group. Meanwhile, PIF group exhibited markedly lower intraoperative/post-operative fentanyl use amounts, as well as markedly reduced time-to-extubation/initial flatus, and length of ICU/hospital stay.
Conclusion: Bilateral PIFB in pediatric open cardiac surgical patients provide effective analgesia and lower the length of hospital stay.
Introduction
Pediatric patients receiving open cardiac surgery always experience acute post-operative pain, with median sternotomic incision being the main pain source (1). Insufficient post-operative analgesia may lead to prolonged immobilization, hypertension, hypoxia, pulmonary hypertensive crisis, tachyarrhythmia, the inability to cough due to median sternotomy, increased length of intensive care unit (ICU) stay and length of hospital stay (2). Non-invasive and invasive methods are used in children suffering from open cardiac surgery for post-operative pain management, such as intravenous opioids, thoracic epidural block (TEA), paravertebral block techniques and the transversus thoracis muscle plane (TTMP) block (3, 4). Intravenous opioids for acute pain induce adverse reactions, such as sufficient sedation, respiratory depression, ileus, post-poned tracheal extubation, immunosuppression, nausea/vomiting, drowsiness, and cough suppression (5).
Paravertebral block techniques and TEA provided effective analgesia in pediatric cardiac surgical patients (3). But hypotension resulting from sympathectomy, pneumothorax, block failure, and adverse reactions like epidural hematoma following infection or complete heparinization, and spinal cord injury greatly restrict their application in cases receiving cardiac surgeries (6). TTMP block could be used in pediatric cardiac surgery for post-operative pain (7), but there was a risk of vascular damage and pneumothorax.
The ultrasound-guided Pecto-intercostal Fascial Block (PIFB) was a newly developed technique and has been used in cardiac surgery (8). To the best of our knowledge, there was no randomized controlled trial (RCT) of PIFB block for pediatric cases who underwent open cardiac surgical resection. Therefore, this work focused on assessing the effect of bilateral PIFB on analgesia as well as reducing hospital stay of patients receiving cardiac surgical treatment.
Methods
The Ethics Committee of First Affiliated Hospital of Nanchang University approved our study protocols. This work was registered at the Chinese Clinical Trial Registry (ChiCTR; registration number ChiCTR 2000030609). The parents of child patients were informed of the study protocols, and they provided informed consents for participation.
The present double-blind RCT was carried out on children between the age groups of 2 and 6 years who experienced elective open heart operation via median sternotomy. The exclusion criteria in our trial was as follows: congestive heart failure, allergic to ropivacaine, hepatic or renal failure, psychiatric problems, redo surgery and pre-operative inotropic support. All cases were randomized as PIF and SAL groups to receive bilateral PIFB using 0.2% ropivacaine and saline at the identical volume, respectively.
Surgery and Anesthesia
Pre-medication was given 30 min before anesthesia with oral midazolam (1 mg/kg, 20 mg at most) in each case. Patients' electrocardiography (ECG), pulse oximetry, invasive arterial blood pressure (BP), central venous pressure, central temperature, and end-tidal carbon dioxide were monitored when they entered the operating room. General anesthesia was triggered with midazolam 0.05 mg/kg, fentanyl 6–10 μg/kg, rocuronium 0.6 mg/kg and etomidate 0.3 mg/kg, followed by the implementation of endotracheal intubation. In addition, fentanyl, rocuronium, and propofol were applied for anesthesia maintenance, with BIS being kept at 45–55 in each case. Intravenous fentanyl and acetaminophen were used to perform post-operative analgesia in our study. The same surgeons at our institution were responsible for performing all surgical procedures. Post-operatively, each child patient was set to cardiac surgery ICU according to pre-determined schedule.
Randomization and Blinding
The random number table method was utilized to randomize all cases as PIF and SAL groups for 0.2% ropivacaine and saline treatment, separately. The allocation of different groups was maintained within a sealed envelope. Ropivacaine and saline, which looked the same, were prepared by a nurse at the post-anesthesia care unit. Thereafter, the as-prepared solution was injected in the pecto-intercostal fascial plane by an experienced anesthesiologist who was blind to group allocation in a 20-min period. Post-operative data were collected via a third reviewer blind to grouping. Surgeons, cases, anesthesiologist, nurses, ICU staff, or additional reviewers were blind to medication assignment in the present double-blind RCT.
Ultrasound-Guided PIFB
By adopting the high-frequency linear ultrasound probe (Mindray, Shenzhen, China), this work carried out PIFB in the supine position. In brief, a probe was inserted at 2 cm lateral from and parallel to the sternum. Thereafter, the external intercostal muscle, pectoralis major muscle, lungs, pleura, and costal cartilage were found. Later, after the localization of pecto-intercostal fascial plane between costal cartilage or external intercostal muscle and pectoralis major muscle, by adopting the in-plane approach, this work inserted a 22-G needle (diameter, 70 mm; Tuoren, Henan, China) beneath pectoralis major while on the top of external intercostal muscle. In the meantime, the correct placement of the needle tip was determined by injecting 1 ml saline. At last, this work injected 0.2% ropivacaine (1.5 mg/kg) into the plane at two positions, over the second and fourth ribs. The identical approach was applied for contralateral PIFB process.
Study Parameters
Post-operative pain was set as the primary endpoint in this work, which was measured at 3/6/9/12/24/48-h post-extubation at exercise (coughing) and rest statuses, as determined through Modified Objective Pain Score (MOPS) (9). Meanwhile, time-to-drain removal/extubation/first defecation, intraoperative/post-operative fentanyl use, length of ICU/hospital stay, together with potential PIFB complications were deemed as the secondary endpoints.
Statistical Analysis
Sample size in this work was determined according to one preliminary research (n = 12/each) comparing pain scores post-operatively. Therefore, for achieving the type-I, type-II error and power of α = 0.05, β = 0.1 and 90%, separately, we needed 92 cases, with a dropout rate of 20%. At last, this work required 110 child patients altogether.
SAS software (version 9.1.3, North Carolina, USA) was adopted for statistical analysis. Continuous data between both groups were compared by Mann-Whitney U-test and student t-test. At the same time, Fisher's exact or Chi-square test was applied in comparing qualitative data. This work also compared MOPS post-extubation between two groups by repeated-measures (two-way) ANOVA. P < 0.05 indicated statistical significance.
Results
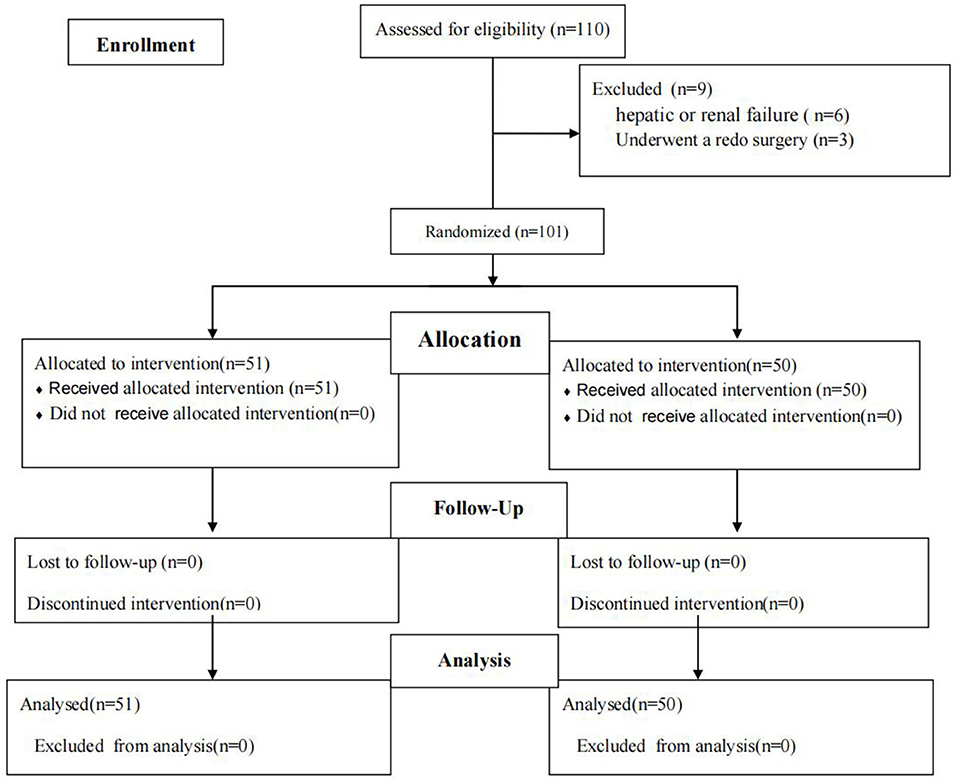
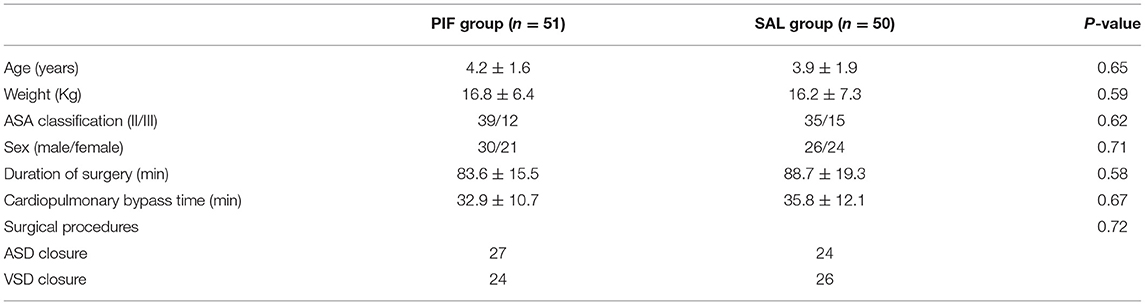
One hundred and 10 children were randomized (55 in per group). This work eliminated four and five cases from PIF and SAL groups, separately due to redo surgery (n = 3) as well as hepatic or renal failure (n = 6). Finally, 101 children were left in our study for subsequent analyses, with 51 in the PIFB and 50 in the SALI groups (Figure 1). Baseline features of patients during surgery were comparable between two groups (Table 1). No complications of PIFB were occurred in our patients.
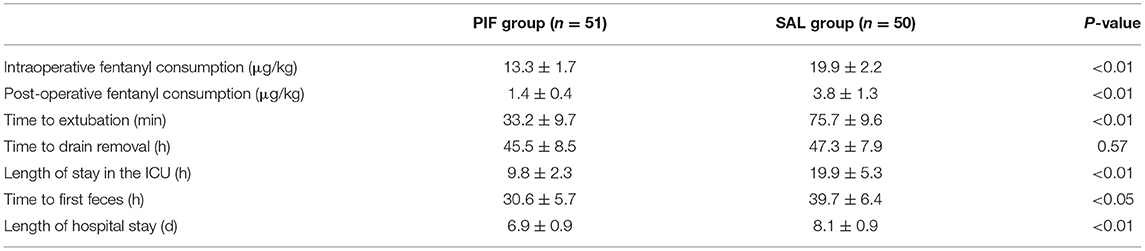
Modified objective pain score markedly increased at 3/6/9/12/24-h post-extubation at exercise (coughing) and rest statuses, and difference at 48-h post-extubation were not significant between two groups (Figure 2). The PIF group reported significantly less intraoperative/post-operative fentanyl use (Table 2), along with markedly reduced time-to-extubation/first flatus, and length of ICU/hospital stay (Table 2). Difference in time-to-drain removal was not significant between two groups (Table 2).
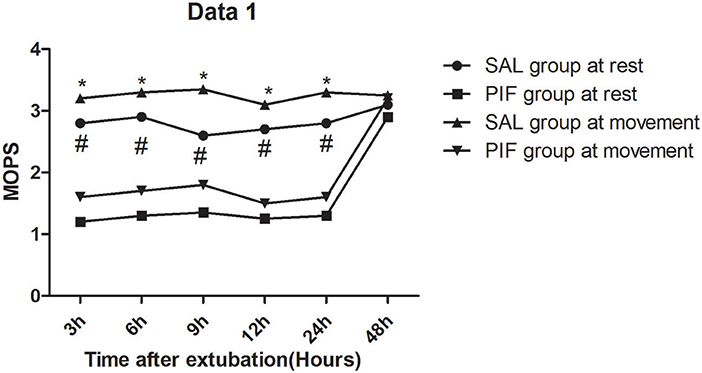
Figure 2. Pain intensity at rest after extubation which was measured by Modified Objective Pain Score (MOPS). #P < 0.05 considered statistically significant. Pain intensity at movement after extubation which was measured by Modified Objective Pain Score (MOPS). *P < 0.05 considered statistically significant.
Discussion
This RCT illustrated the applying bilateral PIFB under ultrasonic guidance in pediatric patients undergoing open cardiac surgery offered efficient analgesia till 24-h post-extubation, while reducing fentanyl use perioperatively. Meanwhile, this technique decreased time-to-extubation/first flatus, along with length of hospital/ICU stay.
High-dose fentanyl is usually adopted in the infusion regimen or as bolus dosing for the anesthesia of cardiac surgery in child patients, which can attain stable hemodynamics and efficient post-operative analgesia (10). Nonetheless, high-dose opioids may induce side reactions such as pruritus, respiratory depression, ileus, post-poned recovery, extended ventilation (11), along with longer ICU/hospital stays (12). According to our results, bilateral PIFB under ultrasonic guidance substantially decreased perioperative fentanyl use with no side reactions. After surgery, PIF group had markedly reduced mean time-to-extubation relative to SAL group, while the reduced fentanyl use perioperatively might be its major cause. The shorter ICU stay length might be possibly associated with the efficient analgesic effect induced by bilateral PIFB under ultrasonic guidance, significantly reduced fentanyl used and shorter time-to-extubation post-operatively. Consequently, decreasing fentanyl use might lay the foundation to promote recovery after open cardiac surgery.
The PIFB offered efficient analgesia for thymectomy via median sternotomy (13, 14) and cardiac surgery (8). Moreover, several articles have described PIFB in sternal fracture pain (15), rib cage pain in ICU patients (16), breast surgery (17), and the subcutaneous-implantable cardioverter defibrillator system implantation (18). As far as we know, the present double-blind RCT first identified the effect of bilateral PIFB on providing efficient pain relief perioperatively for child patients receiving cardiac surgical treatment without adverse events. Bilateral transversus thoracic muscle plane (TTMP) block under ultrasonic guidance can also be adopted for cardiac surgical treatment in child patients for post-sternotomy pain (7). The advantages of PIFB over TTMP block in those suffering from open cardiac surgery were as follows (4, 19). First, both internal mammary vein and artery penetrated TTMP, which was associated with the risk of vascular laceration when blocking. Second, transversus thoracic muscle is usually very thin, especially in children. Therefore, the transversus thoracic muscle, which is also very close to the pleura, can hardly be visualized by ultrasonography (20). That's why there's a risk of pneumothorax in TTMP block. Third, in patients with previous chest surgery, the scar tissue would influence the spread of local anesthetic (21).
Pediatric open cardiac surgical patients usually suffered from extended and serious post-operative pain, in particular in median sternotomic incision (22). Poorly controlled post-operative pain in pediatric open cardiac surgical patients could lead to destructive outcomes like tachyarrhythmia, pulmonary hypertensive crisis, hypertension, extended immobilization, longer ICU/hospital stay length, and hypoxia (2). Our study demonstrated that the ultrasound-guided PIFB provided effective analgesia for 24 h after extubation to children. PIFB shows a decreased risk and invasive degree compared with TTMP block, paravertebral nerve block and thoracic epidural analgesia due to concern of epidural or spinal hemorrhage and hematoma, pneumothorax, vascular laceration and hypotension. And PIFB could reduce the sympathetic excitement and opioid consumption perioperatively, so it could reduce time to first flatus in our study. Therefore, PIFB represented the new, efficient and safe technology for local analgesia in child cases who received open cardiac surgical treatment.
Finally, bilateral PIFB in pediatric open cardiac surgical patients could reduce perioperative consumption of fentanyl, decreased the time-to-extubation/first flatus as well as ICU stay length. The above findings lay the foundation for decreasing hospital stay length.
This study was limited by the uncertain optimal volume and concentration and the short duration impairing the ability to assess long-term post-operative chronic pain.
And, Continuous PIFB block may provide persistent post-operative analgesia for the median sternotomy, but the technology was not utilized in the present work. In further study, we should gradually solve these three problems for pediatric cardiac surgery patients.
In conclusion, our study demonstrated that ultrasound-guided bilateral PIFB in pediatric open cardiac surgical patients shortens hospital stay length through offering the efficient post-operative analgesia, which has substantially reduced the use of fentanyl perioperatively, decreased the time-to-extubation/first flatus as well as ICU stay length.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of First Affiliated Hospital of Nanchang University and it was registered in the Chinese Clinical Trial Registry (ChiCTR) (registration number ChiCTR 2000030609). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
YZ, JM, and SC: study design/planning and data analysis. YZ and JM: study conduct. YZ and SC: writing the manuscript. All authors revised the manuscript.
Funding
The project was funded by Department of Science and Technology of Jiangxi Province [20203BBGL73195] and [20212BAG70034].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lahtinen P, Kokki H, Hynynen M. Pain after cardiac surgery: a prospective cohort study of 1-year incidence and intensity. Anesthesiology. (2006) 105:794–800. doi: 10.1097/00000542-200610000-00026
2. Huang AP, Sakata RK. Pain after sternotomy—review. Braz J Anesthesiol. (2016) 66:395–401. doi: 10.1016/j.bjane.2014.09.013
3. Rodriguez-Aldrete D, Candiotti KA, Janakiraman R. Trends and new evidence in the management of acute and chronic post-thoracotomy pain—an overview of the literature from 2005 to 2015. J Cardiothorac Vasc Anesth. (2016) 30:762–72. doi: 10.1053/j.jvca.2015.07.029
4. Simón DG, Perez MF. Safer alternatives to transversus thoracis muscle plane block. Reg Anesth Pain Med. (2019). doi: 10.1155/2019/1716365
5. Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. (2014) 112:991–1004. doi: 10.1093/bja/aeu137
6. Landoni G, Isella F, Greco M. Benefits and risks of epidural analgesia in cardiac surgery. Br J Anaesth. (2015) 115:25–32 doi: 10.1093/bja/aev201
7. Zhang Y, Chen S, Gong H, Zhan B. Efficacy of bilateral transversus thoracis muscle plane block in pediatric patients undergoing open cardiac surgery. J Cardiothorac Vasc Anesth. (2020). doi: 10.1053/j.jvca.2020.02.005
8. Liu V, Mariano ER, Prabhakar C. Pecto-intercostal fascial block for acute post-sternotomy pain: a case report. A A Pract. (2018) 10:319–22. doi: 10.1213/XAA.0000000000000697
9. Kaushal B, Chauhan S, Magoon R, Krishna NS, Saini K, Bhoi D, et al. Efficacy of bilateral erector spinae plane block in management of acute post-operative surgical pain after pediatric cardiac surgeries through a midline sternotomy. J Cardiothorac Vasc Anesth. (2019). doi: 10.1053/j.jvca.2019.08.009
10. Kwanten LE, O'Brien B, Anwar S. Opioid-based anesthesia and analgesia for adult cardiac surgery: history and narrative review of the literature. J Cardiothorac Vasc Anesth. (2019) 33:808–16 doi: 10.1053/j.jvca.2018.05.053
11. Lena P, Balarac N, Lena D. Fast-track anesthesia with remifentanil and spinal analgesia for cardiac surgery: the effect on pain control and quality of recovery. J Cardiothorac Vasc Anesth. (2008) 22:536–42. doi: 10.1053/j.jvca.2008.04.012
12. Mazzeffi M, Khelemsky Y. Post-sternotomy pain: a clinical review. J Cardiothorac Vasc Anesth. (2011) 25:1163–78. doi: 10.1053/j.jvca.2011.08.001
13. Song W, Wang W, Zhan L. Perioperative analgesia during thymectomy via sternotomy: ultrasound-guided bilateral parasternal block. Anaesthesist. (2019) 68:848–51. doi: 10.1007/s00101-019-00700-w
14. Jones J, Murin PJ, Tsui JH. Opioid free post-operatively using Pecto-intercostal fascial block (PIFB) with multimodal analgesia (MMA) in a patient with myasthenia gravis underwent thymectomy via sternotomy. J Clin Anesth. (2020) 59:32–3. doi: 10.1016/j.jclinane.2019.06.009
15. Raza I, Narayanan M, Venkataraju A, Ciocarlan A. Bilateral subpectoral interfascial plane catheters for analgesia for sternal fractures: a case report. Reg Anesth Pain Med. (2016) 41:607–9. doi: 10.1097/AAP.0000000000000388
16. López-Matamala B, Fajardo M, Estébanez-Montiel B, Blancas R, Alfaro P, Chana M, et al. New thoracis interfascial plane block as anesthesia for difficult weaning due to ribcage pain in critically ill patients. Med Intensiva. (2014) 38:463–5. doi: 10.1016/j.medin.2013.10.005
17. Hong B, Yoon SH, Youn AM, Kim BJ, Song S, Yoon Y. Thoracis interfascial nerve block for breast surgery in a pregnant woman: a case report. Korean J Anesthesiol. (2017) 70:209–12. doi: 10.4097/kjae.2017.70.2.209
18. Droghetti A, Fusco P, Marini M, Harizai F, Scimia P. Ultrasound-guided serratus anterior plane block and parasternal block in cooperative sedation for S-ICD implantation. Pacing Clin Electrophysiol. (2019) 42:1076–8. doi: 10.1111/pace.13727
19. Fujii S. Transversus thoracis muscle plane block and alternative techniques. Reg Anesth Pain Med. (2019). doi: 10.1136/rapm-2019-100755
20. Ohgoshi Y, Ino K, Matsukawa M. Ultrasound guided parasternal intercostal nerve block. J Anesth. (2016) 30:916. doi: 10.1007/s00540-016-2202-5
21. Fujii S, Vissa D, Ganapathy S, Johnson M, Zhou J. Transversus thoracis muscle plane blockon a cadaver with history of coronary artery bypassgrafting. Reg Anesth Pain Med. (2017) 42:535–7. doi: 10.1097/AAP.0000000000000607
Keywords: Pecto-intercostal Fascial Block, pediatric patients, the length of hospital stay, open cardiac surgery, pain
Citation: Zhang Y, Min J and Chen S (2022) Perioperative Pain Management With Bilateral Pecto-intercostal Fascial Block in Pediatric Patients Undergoing Open Cardiac Surgery. Front. Cardiovasc. Med. 9:825945. doi: 10.3389/fcvm.2022.825945
Received: 01 February 2022; Accepted: 30 May 2022;
Published: 22 June 2022.
Edited by:
Oswin Grollmuss, Université Paris-Sud, FranceReviewed by:
Enrico M. Camporesi, USF Health, United StatesDonald Penning, Henry Ford Hospital, United States
Copyright © 2022 Zhang, Min and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shibiao Chen, Y2hlbmxhb3NoaTExMTFAMTYzLmNvbQ==
 Yang Zhang
Yang Zhang Jia Min
Jia Min