- 1Department of Medicine, Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Department of Health Education, Jinan Health Publicity and Education Center, Jinan, China
- 3Neonatal Intensive Care Unit, Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University, Jinan, China
- 4Department of Women Healthcare, Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University, Jinan, China
- 5Department of Public Health, Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University, Jinan, China
Background: Although congenital heart defect (CHD) was the dominating birth defect, the time trend analysis of CHD was largely unknown. In our study, the time trend analysis of CHD from 2005 to 2020 in Jinan was conducted, aimed to reveal the epidemiological characteristics in a city and provided the data basis for the government to make a policy intervention.
Methods: A multi-institutional and retrospective review of CHD for all births from January 1, 2005 to December 31, 2020 was performed. Proportioner prevalence was used to describe the distribution of CHD. Comparisons of CHD characteristics among different groups were assessed with Chi-squares tests. Cochran-Armitage tests (CAT) were used to track changes in CHD prevalence.
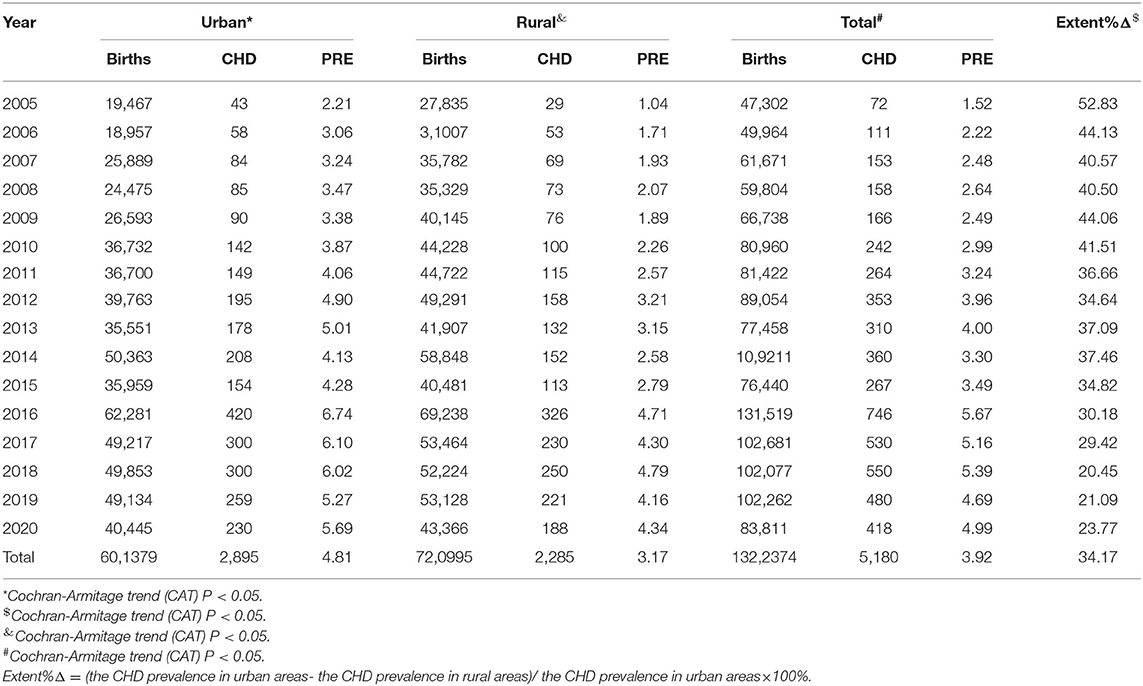
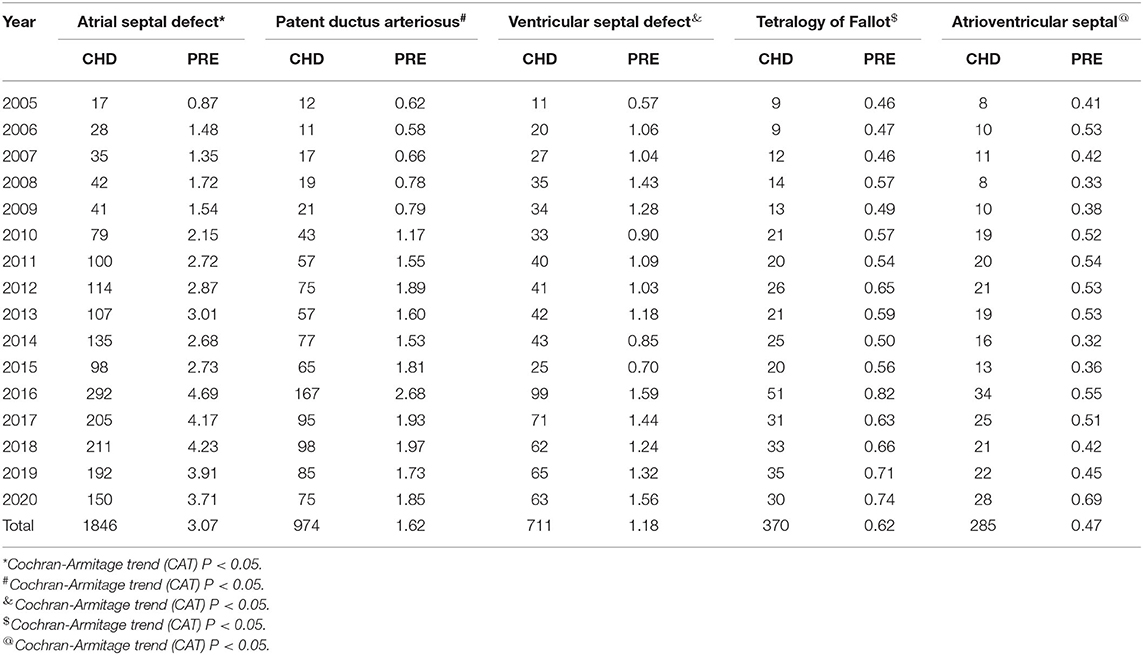
Results: About 322,374 births and 5,180 CHD in Jinan were included from 2005 to 2020, and the total CHD prevalence was 3.92 per 1,000 births. The CHD prevalence showed an upward trend, with a total increase of 227.66% from 2005 to 2020. The CHD prevalence in urban areas was 34.17% higher than that in rural areas, but the gap was narrowing. Atrial septal defect (3.07 per 1,000 births), patent ductus arteriosus (1.62 per 1,000 births), ventricular septal defect (1.18 per 1,000 births), tetralogy of Fallot (0.62 per 1,000 births), and atrioventricular septal defect (0.47 per 1,000 births) were the 5 most common subtypes.
Conclusion: The prevalence of CHD in Jinan was gradually on the rise, which needs to be highly focused on by the health management department. Older pregnant women and women in rural areas should be concerned, and targeted measures need to be introduced.
Introduction
Congenital heart disease (CHD) was defined as clinically significant structural heart and/or great vessels disease present at birth (1). It was estimated that the global average prevalence of CHD was 9.4 per 1,000 live births in 2010–2017 (2). CHD accounts for 28% of all birth defects, which was the most common birth defect (3). In China, 90–150 thousand new births with CHD were diagnosed every year, and infant mortality due to CHD reached 3.91 per 1,000 births in 2018 (4). Although child mortality caused by CHD has declined, the burden of disease caused by CHD was still serious in developing countries (5). CHD was also an important cause of disability in children (6). Infants with CHD frequently required early surgical treatment after birth to improve outcomes (7, 8), which always caused serious economic burden. The annual healthcare costs associated with CHD were estimated to be $5.6 billion, accounting for 15.1% of total pediatric hospitalization costs (9). In China, the total economic burden of CHD exceeded 12.6 billion RMB every year (10). In view of the heavy disease burden and serious health damage caused by CHD, the comprehensive prevention and control of CHD had become a public health issue. Therefore, the reliable epidemiological characteristics of CHD were important in order to have a better insight into its etiology and a finding of high-risk population.
Many studies in China have reported the prevalence of CHD. However, the period for identifying CHD in most studies was from 28 gestation weeks to 7 days after births. In fact, as with the large-scale use of ultrasound in obstetrics, more and more CHDs were diagnosed before 28 gestation weeks. So, that monitoring period cannot reflect the real level of CHD.
Jinan is the most representative city in eastern China for its geographic character, economic figure, and composition of population. In 2005, Jinan established a birth defect monitoring network, covering all medical institutions in the city. In 2011, all maternal and newborn information, including information on CHD, was reported through the web-based reporting system, and accurate and reliable data were available.
In this study, we extended the monitoring period of CHD, from 12 gestation weeks to 7 days after birth. We also performed a trend analysis and a difference test on the characteristics and subtypes of CHD, and the causes of these results were also analyzed. We believe that our study would provide suggestions for the government to formulate scientific policies and serve as a model for some developing cities to prevent CHD.
Methods
Study Population
A multi-institutional and retrospective review of CHD for all births from January 1, 2005 to December 31, 2020 was performed. The study population involved all the pregnant women and fetus/neonates in hospitals of Jinan. The period of identifying CHD was from 12 gestation weeks to 7 days after births, during which CHD diagnosed for the first time was required to report. CHD was coded according to the International Classification of Diseases (10th edition) (11).
Data Collection
Data collection was based on the three-level network of the Maternal and Child Healthcare Institutions (MCH), including hospitals, county-level MCH, and city-level MCH (12). The doctors in hospitals reported the information of pregnant women and fetus/neonates to county-level MCH. The submitted data were verified by the staff in county-level MCH and reported to the city-level MCH every month. Ultimately, 52 hospitals, including 1,322,374 births and 5,180 CHD, were included in the study.
Variables such as the diagnosis gestation week of CHD, the gender of CHD, the maternal age of CHD, the subtype of CHD, and the other demographic characteristics were collected and analyzed.
Data Quality Management
In order to keep high-quality data, a series of standard operating procedures, including data collection, data abstraction, data evaluation, were developed. To ensure accuracy and completeness of CHD, quality control was routinely performed, and 10% normal findings and all abnormal findings were reviewed by cardiologists.
In the process of quality control, the related variables of CHD, such as the gestation week, the CHD subtype, the maternal age, and so on, were the key check contents.
Statistical Analysis
Demographic and clinical characteristics of CHD were expressed as proportion or prevalence. Cochran-Armitage tests (CATs) were used to track changes of the prevalence of CHD in rural and urban areas, the proportion of CHD before and after 28 gestation weeks, and the prevalence of CHD subtypes. The prevalence of CHD according to different maternal characteristics was assessed with Chi-squares tests. Cochran-Armitage tests (CATs) were used to track changes of the CHD prevalence. R version 3.5.1 (the Comprehensive R Archive Network) was used for the data analysis, with a significance level at p < 0.05.
Results
The Prevalence of CHD in Jinan From 2005 to 2020
We counted 1,322,374 births and 5,180 CHD from 2005 to 2020, and the prevalence was 3.92 per 1,000 births. Time trend analysis showed that the prevalence of total CHD was increased, from 1.52 per 1,000 births in 2005 to 4.99 per 1,000 births in 2020, with a total increase of 227.66% and an annual increase of 14.23%.
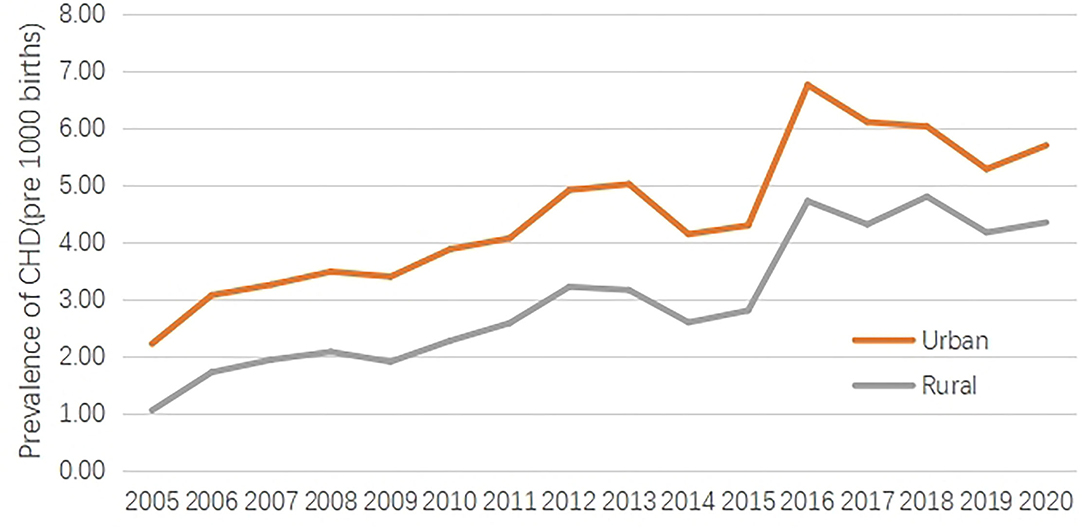
Overall, during the study period, an “S” shape curve can be found in the time trend of CHD prevalence. The first stage was from 2005 to 2010, during which the CHD prevalence was about 2.46 per 1,000 births. The second stage was from 2011 to 2015, during which the CHD prevalence was about 3.58 per 1,000 births. The third stage was from 2016 to 2020, during which the CHD prevalence was about 5.21 per 1,000 births (Table 1, Figure 1).
The Prevalence of CHD Between Urban Areas and Rural Areas in Jinan From 2005 to 2020
From 2005 to 2020, the CHD prevalence was 4.81 per 1,000 births in urban areas and 3.17 per 1,000 births in rural areas. Time trend analysis showed an upward trend of the CHD prevalence in urban and rural areas, and respectively increased by 157.45% and 316.03% in 2020 compared with 2005. Obviously, the increasing range in rural areas was larger than that in urban areas.
The gap of CHD prevalence between urban and rural areas was analyzed. Overall, the CHD prevalence in urban areas was 34.17% higher than that in rural areas, but the gap, gradually, was narrowed, from 52.83% in 2005 to 23.77% in 2020 (Table 1, Figure 1).
The Proportion of CHD Before 28 Gestation Weeks and After 28 Gestation Weeks in Jinan From 2005 to 2020
Between 2005 and 2020, the proportion of CHD was 31.20% before 28 gestation weeks and 68.80% after 28 gestation weeks. Time trend analysis showed an upward trend of the CHD proportion before 28 gestation weeks and increased by 192.82% in 2020 compared with 2005. On the contrary, a downward trend of the CHD proportion was found after 28 gestation weeks, which decreased by 31.11% in 2020 compared with 2005.
Overall, the gap of the CHD proportion between before 28 gestation weeks and after 28 gestation weeks gradually narrowed, from 520% in 2005 to 45.88% in 2020 (Table 2, Figure 2).
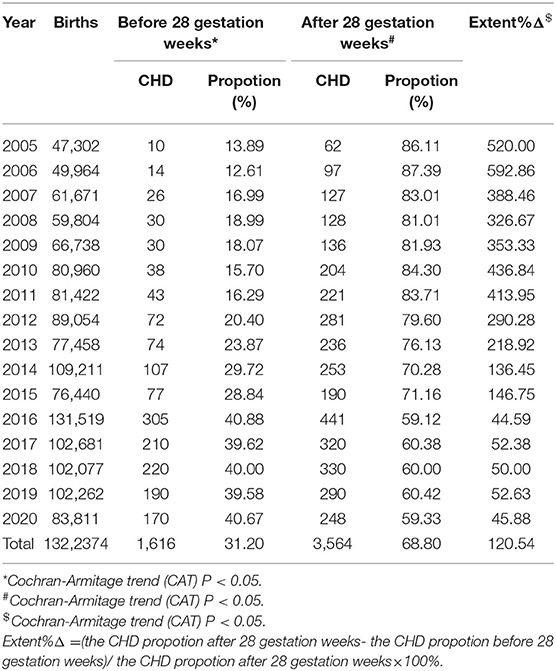
Table 2. The propotion of CHD before 28 gestation weeks and after 28 gestation weeks from 2005 to 2020.
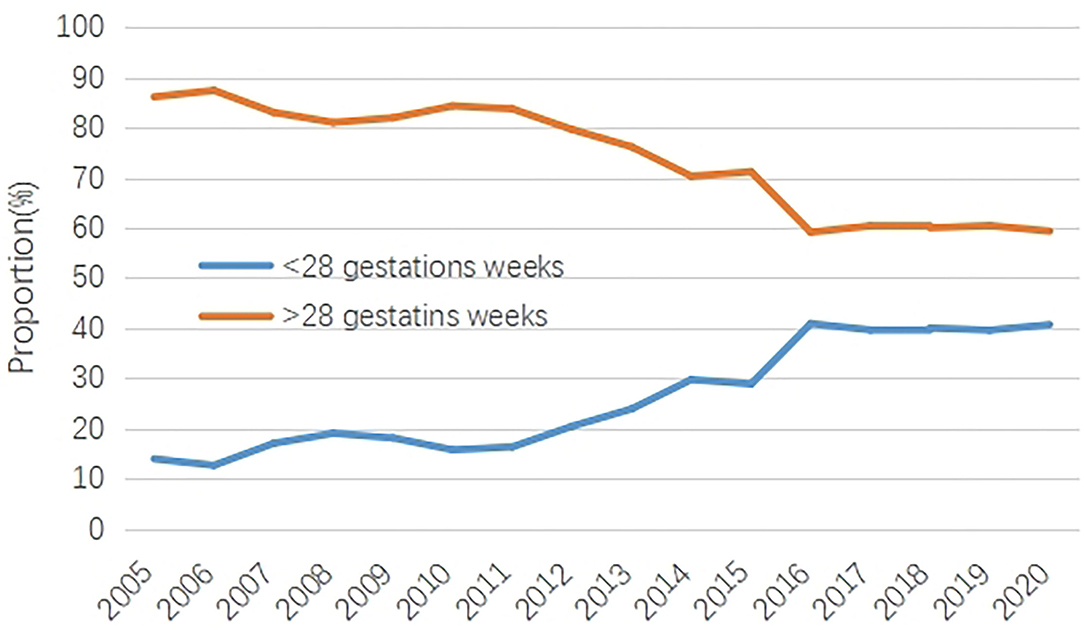
Figure 2. The proportion of CHD before 28 gestation weeks and after 28 gestation weeks from 2005 to 2020.
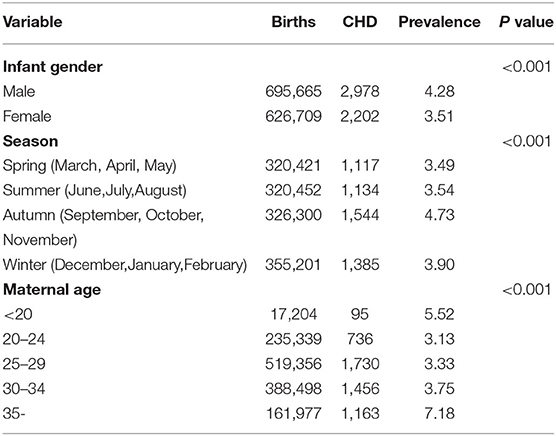
The Difference of CHD Prevalence in Jinan According to Different Maternal Characteristics
Firstly, the CHD prevalence of male births was 17.92% higher than that of female births, and this difference was statistically significant (p < 0.05). Secondly, the CHD prevalence of maternal delivery season was highest in autumn (4.73 per 1,000 births) and least in spring (3.49 per 1,000 births), and the difference was statistically significant (p < 0.05). Besides, significant differences were also found in different maternal age groups. The highest CHD prevalence was found in over 35 years old (7.18 per 1,000 births), followed by under 20 years old (5.52 per 1,000 births) (Table 3, Figure 3).
The Prevalence of the 5 Most Common CHD Subtypes in Jinan From 2005 to 2020
Overall, atrial septal defect (ASD), patent ductus arteriosus (PDA), ventricular septal defect (VSD), tetralogy of Fallot (TOF), and atrioventricular septal (AVSD) were the 5 most common subtypes. The prevalence of these CHD subtypes was 3.07 per 1,000 births, 1.62 per 1,000 births, 1.18 per 1,000 births, 0.62 per 1,000 births, and 0.47 per 1,000 births, respectively.
Time trend analysis showed that the total CHD prevalence in different subtypes increased over time. Compared with 2005, the 5 most common CHD subtypes, respectively, increased by 251.51, 162.74, 109.23, 33.08, and 15.32%. Obviously, the increasing range of ASD was largest among the 5 most common CHD subtypes. Besides, we also found that ASD, PDA, VSD, and TOF had the highest prevalence in 2016 from 2005 to 2020 (Table 4).
Discussion
The total CHD prevalence in Jinan was 3.92 per 1,000 births from 2005 to 2020 and 5.61 per 1,000 births from 2016 to 2020, which were roughly equivalent to the CHD prevalence in China (13) over the same period but were higher than that in Changzhou (14), and lower than that in Zhejiang (15), in Asia, and in the world (2). We speculated that there may be several reasons for this difference. Firstly, it might be due to the different monitored periods. The monitored period, in our study, was from 12 gestation weeks to 7 days after births, but that in Asia or in the world was from birth to 6 years old, and that in Changzhou was from 28 gestation weeks to 7 days after births. Secondly, various screening approaches also played an important role. In our study, B-ultrasound was the main screening method for CHD in Jinan. However, in the study in Zhejiang, in addition to B-ultrasound examination, the pulse oximetry was used for CHD screening after birth.
In our study, 5 epidemiological characteristics of congenital heart disease in Jinan were found.
Firstly, the total CHD prevalence increased significantly over time in Jinan; the upward trend was also found in other studies in China (16, 17). We found an “S” shape in the time trend of the CHD prevalence, and 2011 and 2016 were two obvious growth inflection points. In particular, the prevalence of atrial septal defect (ASD) and ventricular septal defect (VSD) reached their highest levels in 2016 in nearly 15 years. The phenomenon was explained by the following two reasons. On the one hand, it might be attributed to the established information systems. Jinan Maternal and Child Health Information System was an information system based on case collection. Since 2011, every examination of pregnant women throughout pregnancy, especially ultrasound examination, can be found in the information system. However, previous information collections were aggregated data, and information omissions or misdiagnosis of CHD existed. On the other hand, the comprehensive two-child policy implemented in 2016 had a significant impact on the increase in the prevalence of CHD (18, 19). After the implementation of the policy, women over 35 years old in Jinan increased by 45% (20), which undoubtedly increased the prevalence of CHD.
Secondly, we found that the proportion of CHD before 28 gestation weeks increased gradually. This phenomenon was also found in other studies on the CHD diagnosis gestational weeks (21). Large-scale B-ultrasound examination was an important reason for this phenomenon. After 2016, free prenatal ultrasound was included in public health projects in Jinan. Every pregnant woman can obtain a free prenatal ultrasound examination at about 24 gestation weeks, and more and more CHD can be found in the perinatal period, resulting in increasing prevalence.
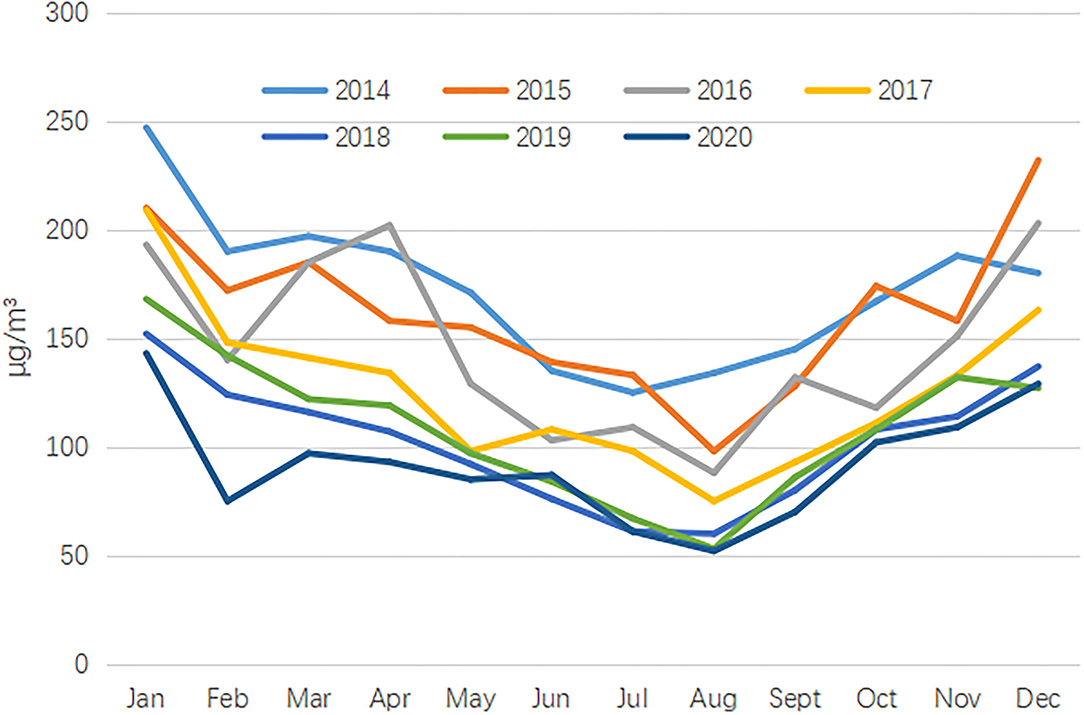
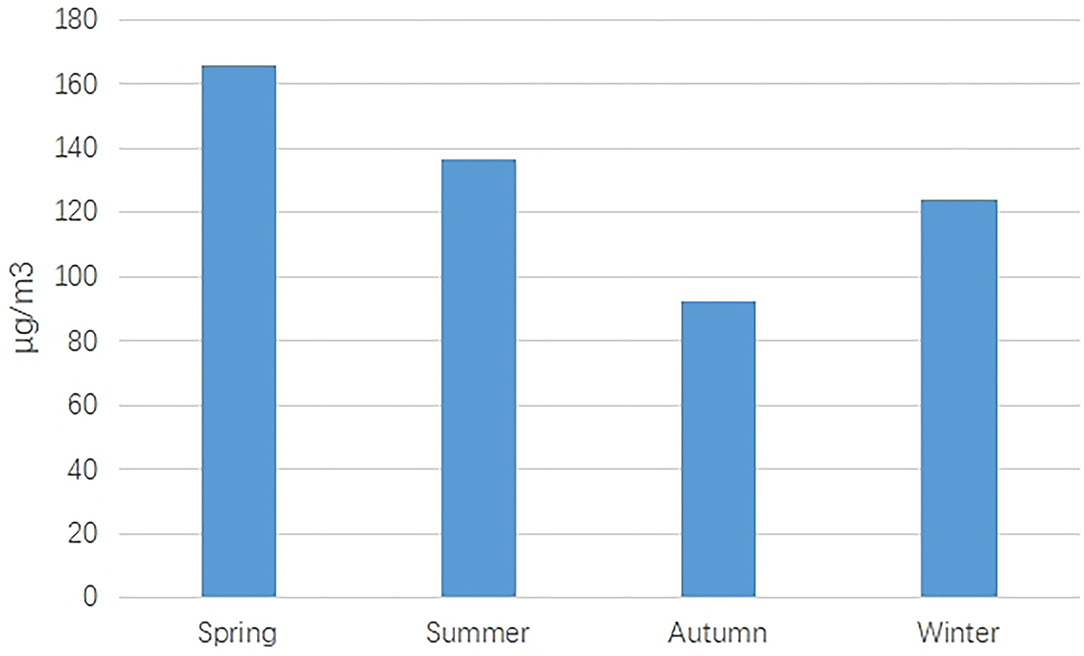
Thirdly, significant differences across gender, maternal delivery season, and maternal age were found. (i) The CHD prevalence in male births was higher than that in female births, which was consistent with some previous studies (22, 23). This difference may be explained by the higher susceptibility of Y chromosome than X chromosome (24). (ii) The CHD prevalence in autumn was highest. As we all know, the critical period of fetal heart and embryo development was 3–8 gestation weeks. In our study, the CHD prevalence in autumn was highest, which indicated that early maternal exposure was in winter. In Jinan, air pollution was relatively serious in winter, especially PM10 (Figures 4, 5). Some studies have pointed out that PM2.5 or PM10 was an important risk factor in birth defects (25, 26). (iii) Like other studies, we also found high CHD prevalence in elderly pregnant women (27–29). As more and more women delay their childbearing age, the government should attach great importance to the above issue. It is estimated that the maternal age has delayed from 26.12 years old in 2005 to 31.26 years old in 2020.
Fourthly, the total CHD prevalence in urban areas was higher than that in rural areas, which was also reported in many other pieces of literature (30, 31). Perhaps, the stronger overall health awareness, the wider use of prenatal diagnosis techniques, more accessibility, and reporting practices in urban areas can be used to explain the phenomenon (32). Interestingly, the gap of the CHD prevalence between urban areas and rural areas was getting smaller and smaller. Several reasons can be used to explain this phenomenon. (i) After 2011, with the advancement of public health projects, the use of prenatal diagnostic techniques became more widespread in rural areas, allowing a large number of congenital heart diseases to be detected prenatally. (ii) An important reason for the phenomenon was changes in environmental exposures. In recent years, the environmental protection measures implemented in urban areas of Jinan have become more and more strict, and the environmental quality has become better and better. On the contrary, the environmental quality in rural areas has not been greatly improved. Especially during the Spring Festival, due to the use of firecrackers, the environmental quality in rural areas was very poor (33). National Environmental Monitoring Center reports that more than 60% cities in rural areas have excessive air pollution during the Spring Festival holiday (34), and the data in our study also showed the poor air quality in January, each year during the Spring Festival from 2014 to 2018.
Fifthly, in Jinan, the reported CHD was dominated by mild lesions (84.31%), such as VSD, ASD, and PDA. The finding also was confirmed in other studies (35). The following reasons can explain this phenomenon. Firstly, comprehensive use of echocardiography and improved echocardiographic techniques were likely to account substantially for the increased prevalence of mild lesions. With the improvement of health awareness, more and more pregnant women were checked fetal health by B-ultrasound. In 2020, the proportion of fetal cardiac ultrasound examination reached 92.13%. So, many previous mild lesions were reported in the prenatal period. The second reason should be attributed to air pollution. The terrain in Jinan belonged to a basin bottom structure, which made the air pollutants, especially PM10, unable to be dissipated in time. Some epidemiologic studies have suggested the possible association of maternal exposure to PM10 during the first trimester of gestation with VSD, ASD, and PDA (25, 36).
Limitation
Firstly, the prevalence of CHD in our study was based on hospitals; births with CHD given out of hospital would be missed. Therefore, the actual prevalence of CHD might be underestimated. Secondly, as a cross-sectional study, some risk factors of CHD, such as the natural environment or other maternal complications, were not considered because of limited data.
Conclusion
The CHD prevalence was increased in Jinan from 2005 to 2020. The CHD prevalence in urban areas and before 28 gestation weeks was increased faster. Mild lesions, such as VSD, ASD, and PDA, were the dominating subtypes. Elderly pregnant women and women in rural areas should be focused.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LZ, BL, and HL participated in data collection. ZL conceived the idea, participated in data analysis, and drafted the manuscript. CW and SY participated in the design and implementation of the study. All authors read and approved the final manuscript.
Funding
This investigation was supported by the Shandong province medical and health science development project (2018WS488) and the Jinan medical and health science development project (2018-1-29).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank all the participants for their contribution and also acknowledge the help and support from Prof. Weimin Fang for this study.
References
1. Mitchell SC, Korones SCSB, Berendes HWW. Congenital Heart Disease in 56,109 Births Incidence and Natural History. Circulation. (1971) 43:323–32. doi: 10.1161/01.CIR.43.3.323
2. Liu Y, Chen S, Zühlke L, Black GC, Choy MK, Li N, et al. Global birth prevalence of congenital heart defects 1970-2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. (2019) 48:1–9. doi: 10.1093/ije/dyz009
3. Linde D, Koningsc E, Slagerc M, Witsenburg M, Helbing WA, Takkenberg JJM, et al. Birth Prevalence of Congenital Heart Disease Worldwide. J Am Coll Cardiol. (2011) 58:2241–7. doi: 10.1016/j.jacc.2011.08.025
4. Manchen G, Fengwen Z, Xiangbin P. Interpretation of the section of congenital heart diseases in Annual Report on Cardiovascular Health and Diseases in China (2019). Chin J Clin Thorac Cardiovasc Surg. (2021) 28:384–7. doi: 10.1097/CD9.0000000000000040
5. Collaborators GCHD. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health. (2020) 4:185–200. doi: 10.1016/S2352-4642(19)30402-X
6. Teun V, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder B. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. (2011) 8:50–60. doi: 10.1038/nrcardio.2010.166
7. Bakker MK, Bergman J, Krikov S, Amar E, Botto LD. Prenatal diagnosis and prevalence of critical congenital heart defects: an international retrospective cohort study. BMJ Open. (2019) 9:e028139. doi: 10.1136/bmjopen-2018-028139
8. Colaco SM, Karande T, Bobhate PR, Jiyani R, Kulkarni S. Neonates with critical congenital heart defects: Impact of fetal diagnosis on immediate and short-term outcomes. Ann Pediatr Cardiol. (2017) 10:126. doi: 10.4103/apc.APC_125_16
9. Simeone RM, Oster ME, Cassell CH, Armour BS, Gray DT, Honein MA. Pediatric inpatient hospital resource use for congenital heart defects. Birth Defects Res A Clin Mol Teratol. (2014) 100:934–43. doi: 10.1002/bdra.23262
10. Huaijin Q, Zhu J. Birth Defect Prevention Report 2012. Beijing: People's Sanitary Publishing Press (2013).
11. WHO Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. Acta Chirurgica Iugoslavica. (2010) 56:65–9. doi: 10.2298/ACI0903065V.
12. Dai L, Zhu J, Liang J, Wang YP, Wang H, Mao M. Birth defects surveillance in China. World J Pediatr. (2011) 7:302–10. doi: 10.1007/s12519-011-0326-0
13. Zhao L, Chen L, Yang T, Wang T, Qin J. Birth prevalence of congenital heart disease in China, 1980–2019: a systematic review and meta-analysis of 617 studies. Eur J Epidemiol. (2020) 35:1–12. doi: 10.1007/s10654-020-00653-0
14. Zhou Y, Mao X, Zhou H, Qin Z, Yu B. Epidemiology of birth defects based on a birth defect surveillance system in Southern Jiangsu, China, 2014–2018. J Matern Fetal Neonatal Med. (2020) 7:1–7. doi: 10.3389/fpubh.2020.00378
15. Zhang X, Sun Y, Zhu J, Zhu Y, Qiu L. Epidemiology, prenatal diagnosis, and neonatal outcomes of congenital heart defects in eastern China: a hospital-based multicenter study. BMC Pediatr. (2020) 20:1–8. doi: 10.1186/s12887-020-02313-4
16. Sun PF, Ding GC, Zhang MY, He SN, Gao Y, Wang JH. Prevalence of Congenital Heart Disease among Infants from 2012 to 2014 in Langfang, China. Chin Med J. (2017) 130:1069–73. doi: 10.4103/0366-6999.204923
17. Qu Y, Liu X, Zhuang J, Chen G, Mai J, Guo X, et al. Incidence of Congenital Heart Disease: The 9-Year Experience of the Guangdong Registry of Congenital Heart Disease, China. PLoS ONE. (2016) 11:e0159257. doi: 10.1371/journal.pone.0159257
18. Hesketh T, Zhou X, Wang Y. The End of the One-Child Policy: Lasting Implications for China. JAMA. (2015) 314:2349–50. doi: 10.1001/jama.2015.16279
19. Zeng Y, Hesketh T. The effects of China's universal two-child policy. Lancet. (2016) 388:1930–8. doi: 10.1016/S0140-6736(16)31405-2
20. Yu D, Zhang L, Yang S, Chen Q, Li Z. Trends, causes and solutions of maternal mortality in <city>Jinan </city>, China: the epidemiology of the MMR in 1991-2020. BMC Public Health. (2021) 21:1792. doi: 10.1186/s12889-021-11816-3
21. Xie D, Fang J, Liu Z, Wang H, Yang T, Sun Z, et al. Epidemiology and major subtypes of congenital heart defects in Hunan Province, China. Medicine. (2018) 97:1–11. doi: 10.1097/MD.0000000000011770
22. Li JJ, Liu Y, Xie SY, Zhao GD, Dai T, Chen H, et al. Newborn screening for congenital heart disease using echocardiography and follow-up at high altitude in China. Int J Cardiol. (2019) 274:106–112. doi: 10.1016/j.ijcard.2018.08.102
23. Li S, Hong SX, Wang TM. A population-based surveillance system on birth defects and its application. Chin J Epidemiol. (2001) 22:172–5.
24. Sokal R, Tata LJ, Fleming KM. Sex prevalence of major congenital anomalies in the United Kingdom: a national population-based study and international comparison meta-analysis. Birth Defects Res A Clin Mol Teratol. (2014) 100:79–91. doi: 10.1002/bdra.23218
25. Zhang B, Liang S, Zhao J, Qian Z, Bassig BA, Yang R, et al. Maternal exposure to air pollutant PM2.5 and PM10 during pregnancy and risk of congenital heart defects. J Expo Sci Environ Epidemiol. (2016) 26:422–7. doi: 10.1038/jes.2016.1
26. Vrijheid M, Martinez D, Manzanares S, Dadvand P, Schembari A, Nieuwenhuijsen RM. Ambient Air Pollution and Risk of Congenital Anomalies: a Systematic Review and Meta-analysis. Environ Health Perspect. (2011) 119:598–606. doi: 10.1289/ehp.1002946
27. Miller A, Riehle-Colarusso T, Siffel C, Frías JL, Correa A. Maternal age and prevalence of isolated congenital heart defects in an urban area of the United States. Am J Med Genet A. (2011) 155A:2137–45. doi: 10.1002/ajmg.a.34130
28. Luo YL, Cheng YL, Gao XH, Tan SQ, Li JM, Wang W, et al. Maternal age, parity and isolated birth defects: a population-based case-control study in Shenzhen, China. PLoS ONE. (2017) 8:1–11. doi: 10.1371/journal.pone.0081369
29. Baird PA, Sadovnick AD, Yee IM. Maternal Age and birth defects: a population study. Lancet. (1991) 337:527–530. doi: 10.1016/0140-6736(91)91306-F
30. Pei L, Kang Y, Zhao Y, Yan H. Prevalence and risk factors of congenital heart defects among live births: a population-based cross-sectional survey in Shaanxi province, Northwestern China. BMC Pediatr. (2017) 17:18. doi: 10.1186/s12887-017-0784-1
31. Zhang X, Su L, Wu S, Hao X, Guo S, Kota S, et al. Prevalence of birth defects and risk-factor analysis from a population-based survey in Inner Mongolia, China. BMC Pediatr. (2012) 12:125. doi: 10.1186/1471-2431-12-125
32. Tang S, Meng Q, Chen L, Bekedam H, Whitehead M. Tackling the challenges to health equity in China. Lancet. (2008) 372:1493–501. doi: 10.1016/S0140-6736(08)61364-1
33. Xiao-Hui MA, Sun ZB, Ding HY, Zi-Ming LI. Effect of fireworks and meteorological conditions on air quality during Spring Festival in Beijing. J Meteorol Environ. (2015) 31:50–5.
34. Pan BF, Li-Na LI. The influence of burning fireworks on the air quality in major cities during the spring festival in chin. Environ Eng. (2016) 34:34–7. doi: 10.13205/j.hjgc.201601016
35. Morris JK, Springett AL, Greenlees R, Loane M, Addor MC, Arriola L, et al. Trends in congenital anomalies in Europe from 1980 to 2012. PLoS ONE. (2018) 13:1–18. doi: 10.1371/journal.pone.0194986
Keywords: epidemiology, congenital heart disease, prevalence, time trend analysis, causes analysis
Citation: Zhang L, Liu B, Li H, Wang C, Yang S and Li Z (2022) Epidemiology of Congenital Heart Disease in Jinan, China From 2005 to 2020: A Time Trend Analysis. Front. Cardiovasc. Med. 9:815137. doi: 10.3389/fcvm.2022.815137
Received: 15 November 2021; Accepted: 21 March 2022;
Published: 27 April 2022.
Edited by:
Massimo Caputo, University of Bristol, United KingdomReviewed by:
Pietro Scicchitano, ASLBari - Azienda Sanitaria Localedella Provincia di Bari (ASL BA), ItalyVladimir Uspenskiy, Almazov National Medical Research Centre, Russia
Copyright © 2022 Zhang, Liu, Li, Wang, Yang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongliang Li, bGl6aG9uZ2xpYW5nOTAzQDE2My5jb20=
†These authors have contributed equally to this work
 Lihua Zhang
Lihua Zhang Bei Liu2†
Bei Liu2† Zhongliang Li
Zhongliang Li