- 1Department of Cardiovascular Surgery, Heart Center Brandenburg, Immanuel Klinikum Bernau, University Hospital Brandenburg Medical School (Theodor Fontane), Bernau bei Berlin, Germany
- 2Faculty of Health Sciences, Brandenburg Medical School Theodor Fontane, Neuruppin, Germany
- 3Center for Health Services Research, Brandenburg Medical School Theodor Fontane, Rüdersdorf bei Berlin, Germany
- 4Hypertension Care UG, Ingolstadt, Germany
- 5AOK Nordost – Die Gesundheitskasse, Strategische Versorgungsanalysen/GeWINO, Berlin, Germany
- 6revFLect GmbH, Hanover, Germany
- 7Brandenburg Medical School Theodor Fontane, Neuruppin, Germany
- 8Hypertension Center Munich, Munich, Germany
- 9Medical Department, Division of Cardiology and Angiology, Charité – Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany
Introduction: Digital health measures promise to further improve the quality of cardiovascular care but have not yet been widely implemented in routine care. The research project Digital preventive measures for arterial hypertension (DiPaH) will systematically identify structural and individual factors in different stakeholders that influence the use of digital preventive measures in patients with arterial hypertension in Germany. Special focus is given to remote and sparsely populated areas, the age-specific impact, as well as influence of digital health literacy.
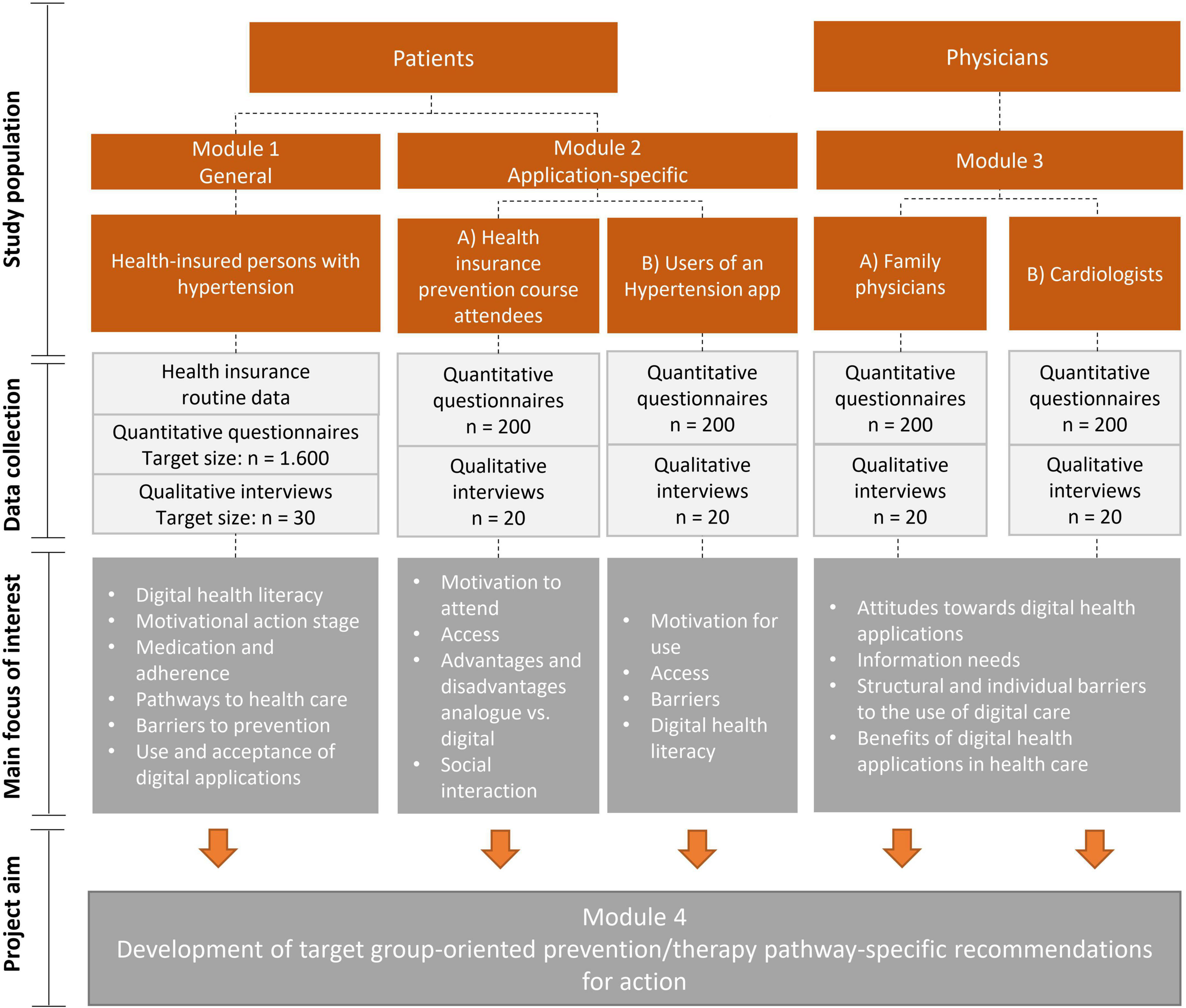
Methods and analysis: The DiPaH project is an exploratory cross-sectional study with a mixed-methods design, in which written surveys and interviews with patients and physicians will be conducted. In addition, secondary data from a health insurance company will be analyzed. In module 1, individuals from the database of the health insurance company with confirmed arterial hypertension will be interviewed (1,600 questionnaires, 30 interviews). Module 2 includes users of digital prevention offers and apps (400 questionnaires, 40 interviews) and in module 3, family physicians and cardiologists will be interviewed (400 questionnaires, 40 interviews). In a final module, the overall results will be analyzed and recommendations for interventions in clinical care will be derived.
Discussion: The DiPaH project will contribute to a patient-oriented and demand-based improvement of arterial hypertension prevention services in health care. Challenges and barriers will be analyzed and the respective target groups identified based on their prevention needs and social characteristics to enable a patient-centered implementation of digital prevention of arterial hypertension and cardiovascular services in general, and finally to improve cardiovascular outcomes.
Clinical trial registration: https://drks.de/search/de/trial/DRKS00029761, identifier DRKS00029761.
Introduction
Despite effective guideline-based prevention and treatment options, cardiovascular diseases remain the leading cause of death worldwide (1). Arterial hypertension is one of the most important risk factors for cardiovascular diseases (2), affecting over one billion people worldwide (3). In addition to a genetic predisposition, the development of hypertension is strongly influenced by individual factors such as lifestyle (4), but also by local access to and quality of health care (5). In Germany, the prevalence of such risk factors varies greatly depending on the region. For example, obesity is more prevalent in the rural federal states (6). But it is precisely there that accessibility to medical care is limited due to a low density of doctors (7). As a result, hypertension-related diseases such as ischemic heart disease are most frequent in these states (8). On an individual level, there is also an association between hypertension and lower socioeconomic status and lower educational attainment (9). In summary, there are significant regional differences in Germany, with a higher incidence of arterial hypertension in socioeconomically disadvantaged areas (10).
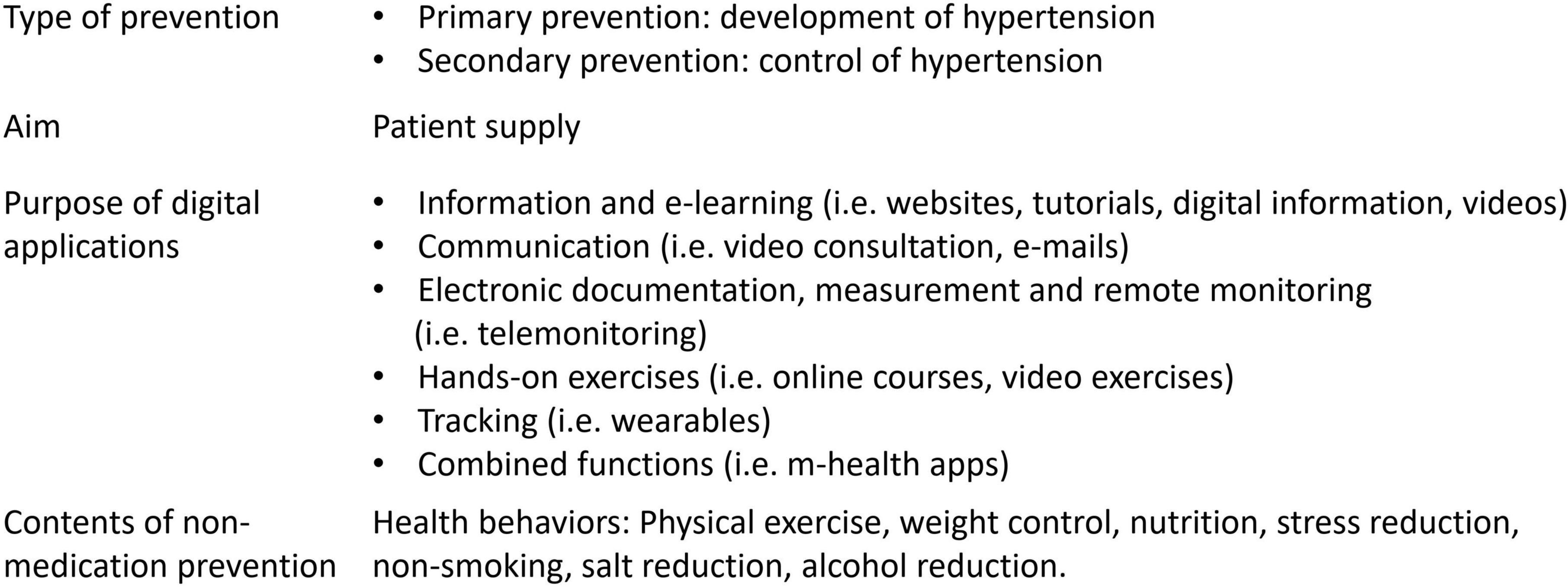
In order to overcome these geographical disparities in health care and to strengthen individual health behavior even in regions with poor access to health care and aging population, digital prevention measures are an innovative and promising approach (11). These are digital applications such as remote monitoring (i.e., telemonitoring), e-learning, or m-health apps. The characteristics of digital preventive measures for arterial hypertension are shown in Figure 1. With telemonitoring, patient data is transmitted to the attending physicians (12). E-learning provides patients with information, e.g., on lifestyle modification through interactive and web-based educational material (12), and m-health apps are stand-alone software on a smartphone or tablet (13). Despite existing technical possibilities, digital health applications have so far only been insufficiently implemented (11), so that there is an increasing risk of a “digital divide” (14), whereby vulnerable groups with low digital health literacy are progressively excluded from innovative health offers. Current data (15) from Germany show low mobile Internet use among older people (only 36% of the population born up to 1945) and among people with lower educational attainment. Importantly, usage is lower in the more rural eastern German states than in the western states. Since people with lower incomes have less access to digital devices (15), one cause could be the lower gross average income in eastern Germany (16). However, people who are more limited in their mobility and have a higher risk of illness could particularly benefit from digital measures. Importantly, data on hypertension-specific digital applications are lacking so far.
Due to the importance of digital health interventions, the ESC e-Cardiology Working Group has published a position paper in 2019 addressing the challenges of digital health adoption in cardiovascular medicine (11). In addition to technical issues, there are also patient- and physician-related barriers [e.g., lack of information about available and qualified m-health apps (17), lack of digital skills (15)] as well as reimbursement and legal considerations to the introduction of digital health in cardiovascular medicine that need to be carefully analyzed and addressed prior to their successful deployment.
To overcome such barriers, the healthcare research project digital preventive measures for arterial hypertension (DiPaH) will therefore systematically identify individual, structural and application-related factors that influence the use of digital preventive measures in patients with arterial hypertension in Germany. Due to the regional differences already described, a particular focus of the study is on remote and sparsely populated areas, the age-specific effects as well as the influence of digital health literacy.
The study identifies not only general barriers to the use of digital prevention services, but also barriers specific to patient groups (e.g., with regard to motivation and health literacy). In order to take into account the complexity of prevention in statutory health insurance, the DiPaH study relates the experiences of patients and users of digital applications to the perspective of physicians. In this way, potentials, but also barriers that only emerge in the overall context of the health care system, can be identified and corresponding concrete recommendations for implementation can be derived.
This study protocol presents the study design for each subgroup and describes the study population, the methodological approach (including data collection and data analysis), the relevant outcomes and the quality criteria of the study, and discusses the expected benefits and limitations. The aim is to give an overview of the different sub-studies (modules), to describe contexts and to present the methodological approach.
Methods and analysis
Design and setting of the study
The mixed-methods study will be conducted in multiple phases. Quantitative and qualitative methods will be performed in a parallel or in a sequential order (18). Standardized surveys are used to obtain a representative and comprehensive understanding of the different stakeholder groups and to make the answers comparable. The qualitative methods are suitable to contextualize and interpret the data appropriately (18). The methodological openness of qualitative methods also allows aspects to be included that arise from everyday conditions and are accordingly not yet theoretically accessible at the beginning of the study, for example organizational barriers in everyday practice (19). Methodological triangulation allows the results of quantitative and qualitative interviews to be validated against each other (20).
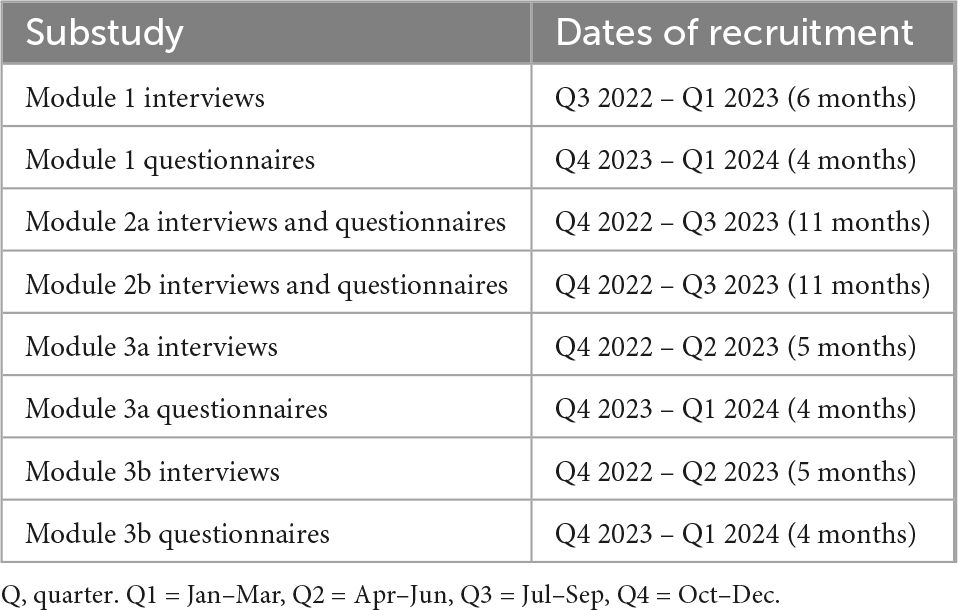
Figure 2 shows a summary of the study design, methods and the main focus of interest in each module. Since the focus is on the user perspective, we will include patients with arterial hypertension, users of digital health services and physicians. The timeline of recruitment is presented in Table 1.
The study will be conducted in Germany with a regional focus on the metropolitan area of Berlin and the rural, sparsely populated federal states of Brandenburg and Mecklenburg-Western Pomerania.
Selection of subjects
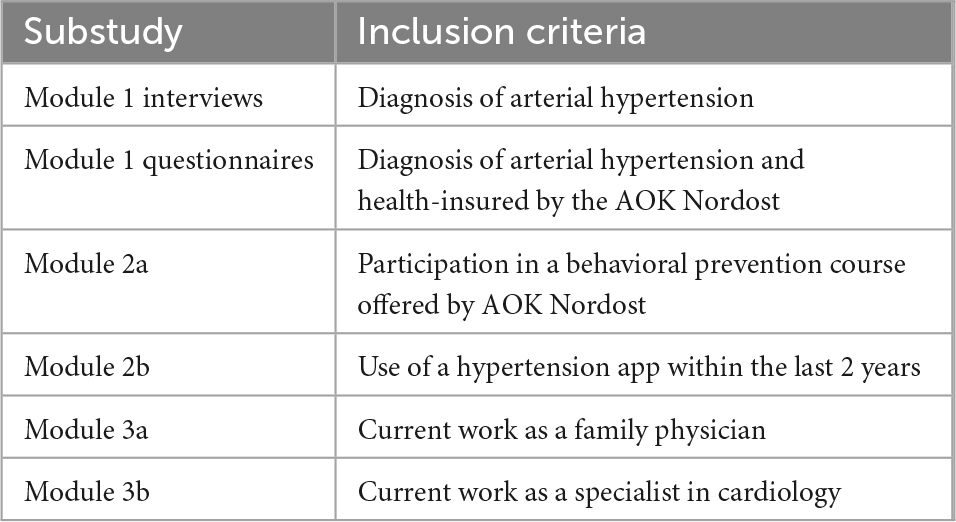
The sub-study specific inclusion criteria are summarized in Table 2. Exclusion criteria are age under 18, lack of consent and considerable limitations to speak and understand German fluently.
In module 1, insured persons of the statutory health insurance company AOK Nordost with arterial hypertension will be surveyed on preferences and barriers to the use of (digital) prevention measures (n = 1,600 questionnaires). Questionnaire data will be linked to routine data to analyze further health-related factors. Prior to the AOK Nordost survey, a preparatory qualitative interview study will be conducted with hypertension patients recruited through clinics and practices (n = 30).
In module 2a, users of (digital) prevention services offered by AOK Nordost will be surveyed on their motivation to participate in the interventions, the advantages and disadvantages of digital vs. analog measures, and possible barriers to the services (n = 200 questionnaires, n = 20 interviews).
In module 2b, users of the hypertension-specific app “Hypertonie.App” (21) will be interviewed about their motivation for using the app, about possible restraining factors when using a hypertension app and how they became aware of the app (n = 200 questionnaires, n = 20 interviews). The app includes features for documenting blood pressure, personalized health information, breathing exercises, and reminder functions.
In module 3, family physicians (3a) and cardiologists (3b) will be surveyed on their attitudes toward digital health applications, structural and individual barriers, and information needs in medical practice (n = 400 questionnaires, n = 40 interviews).
Sample size calculation
A sample number of n = 200 is required per subgroup. The sample number is calculated according to an a priori power analysis (G*Power) for the χ2 test for dichotomous variables with the following assumptions: moderate effect (w = 0.2), α = 0.05, power (1-β) = 0.80, Df = 1 (required sample size n = 197).
In Module 1, eight subgroups will be identified by age, gender, and rural vs. urban residence (per subgroup n = 200, total n = 1,600).
Outcomes
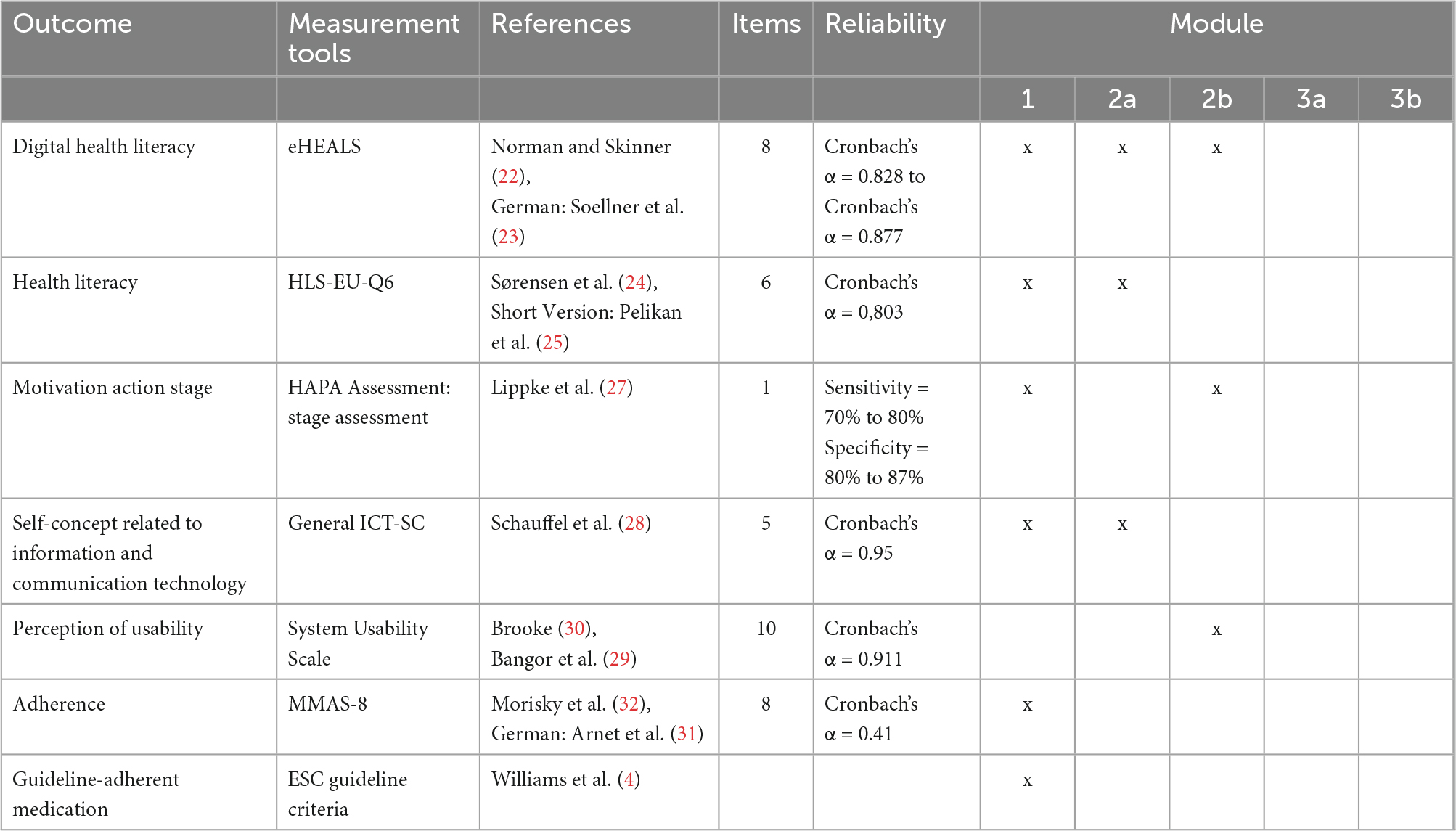
The DiPaH study will collect data through questionnaires and interviews on a one-time basis. The relevant outcomes are digital health literacy [eHEALS (22, 23)], health literacy [HLS-EU-Q6 (24, 25)], motivation action stage [HAPA Assessment (26, 27)], self-concept related to information and communication technology (28), perception of usability [System Usability Scale (29, 30)], guideline-adherent medication (4), adherence [MMAS-8D (31, 32)]. The outcomes and measurement tools are presented in Table 3. In addition, the following outcomes will be explored in all modules: attitudes toward digital prevention, use of digital prevention, motivation to use digital prevention, barriers to digital prevention, perceived advantages and disadvantages of digital prevention, information needs, and – just for patients – pathways to health care. For these outcomes, module-specific items will be developed and piloted by the research team. In addition, these themes will be explored in greater detail in the qualitative interviews.
Input variables in all modules will be sociodemographic characteristics of patients (age, gender, rural vs. urban residence, federal state, education, income) and physicians (age, gender, rural vs. urban location of medical practice, federal state, experience). In Modules 1 and 2b, health-related characteristics will be collected in more detail (current medication, disease status, comorbidities). In Module 2a, the interactivity of the course is additionally assessed as an input variable.
Statistical analyses
First, the data from the standardized questionnaires will be presented descriptively (absolute and relative frequency, median and standard deviation). In further steps, correlation analyses will be performed. The correlation between two binary variables is analyzed with the χ2-test. For continuous outcome variables and binary influence factors, t-tests will be performed and means and 95% confidence intervals will be reported. Regression analyses will be performed to analyze possible associations between patient characteristics (such as sociodemographic variables) and outcomes of interest (e.g., digital health literacy).
Qualitative analyses
For the qualitative part of the study, problem-centered interviews will be conducted. In this type of exploratory interview, the theoretical concepts are changeable in the research process. Thus, the method enables to integrate the subjective perspectives, experiences and contextual conditions of the participants. In addition to the interview guide, short questionnaires will be applied to collect sociodemographic and health-related characteristics.
The interviews will be recorded and transcribed. The qualitative data from the interviews and from the free text answers in the questionnaire will be analyzed with the qualitative content analysis according to Kuckartz (33). This allows a rule-driven reduction and systematization of the data. The aim is to develop a comprehensive category system. For validation of the category system, a member check will be performed (34).
Data capture and storage
In modules 1 and 2a, the insured persons receive the questionnaire from their health insurer AOK Nordost with a stamped return envelope. By giving written consent, participants in module 1 agree to the linking of questionnaire data with the billing data of the health insurance funds. The pseudonymization of the data will be carried out by a trust center on the basis of a coding list. The trust center is separated from the evaluating unit in terms of space, technology, and staff. In modules 2 and 3 online participation will also be possible. For this, participants will receive a link to the questionnaire on the online platform “unipark” (35).
To receive the incentive (money or gift card), participants need to consent that their contact details will be used for this purpose. Written consent is also required for the audio recording of the interviews. The interviews will be coded with a pseudonym before the analysis. Contact information and consent will be kept separate from research data.
Research data will not contain personal data that would allow the identification of individuals. The data will be stored securely on the server of the Brandenburg Medical School or on local computers.
Data quality
To ensure high data quality, several data validation checks will be performed: checking for correct data type, numeric value ranges, data format, missing data, and consistency of the chronology in the dates. The completeness of the data is checked per case. The quality of the interview data will be controlled by a member check (36).
Discussion
Global health systems today confront fundamental challenges in providing optimal care due to aging populations, shortages of health workers, financing, accessibility and affordability of cardiovascular disease medicines and services. Digital health technologies have the potential to overcome these challenges (37). Consequently, the establishment of e-health to improve widespread cardiovascular care is a central goal of the ESC. In terms of arterial hypertension, a digital hypertension program and m-health tools have already been shown to lead to significant improvement in blood pressure control rates and lifestyle change compared to standard care (38, 39). However, before successful and widespread implementation, there is still a great need for research on hindering and supportive elements in special patient populations (11). To our knowledge, DiPaH is the largest health services research study on the topic of digital cardiovascular prevention measures and will fill this important knowledge gap. Different patient cohorts will be characterized according to their prevention needs and possible barriers to the use of digital prevention measures. At the same time, physicians will be involved as a main contact for their patients in order to identify structural and individual obstacles as well as information needs in medical practice. Based on this, practical recommendations will eventually be developed at the levels of patients, physicians, service providers, and health insurers to increase the implementation, accessibility, use of, as well as the adherence to digital prevention measures. These will enable hypertensive patients to take a more active role in their own care and will have the potential to significantly improve current clinical care pathways (11). We are also convinced that these findings will help to implement digital health-based care models for cardiovascular disease in general, beyond the application field of arterial hypertension.
Strengths and limitations
The strengths of DiPaH include an integrative approach of a mixed-methods study protocol that comprehensively considers the perspectives of patients, physicians and participants of analog and digital prevention measures. Special attention is paid to rural and sparsely populated areas, age-specific effects and the influence of digital health literacy. This allows concrete recommendations to be derived for wider adoption and sustainable use of digital prevention interventions in cardiovascular medicine. A limitation of the study is that it is only conducted in Germany. But by using internationally validated questionnaires, relevant findings can also be obtained for other countries.
Even though we are only survey the users of a single hypertension app, the aim is not to evaluate this one app. Rather, in DiPaH we want to characterize the app users and find out why they use a digital hypertension app. Accordingly, a gain in knowledge is expected for other apps. In particular, it is assumed that barriers, motivations, attitudes, and pathways to health care are not app-specific.
However, the AOK Nordost is the largest statutory health insurance fund in north-eastern Germany with about 1.7 million insured and covers about 18% of the population in north-eastern Germany (approx. 7.82 million inhabitants, 2021 (40)). As there is no standardized electronic patient record in Germany so far, we will not use primary data from hospitals and health care facilities. Surveying participants via a health insurer has the advantage that there are no gatekeepers, e.g., physicians enrolling patients in the study and thereby selecting them (intentionally or unintentionally), and that the billing data is complete. The limitation of billing data (e.g., shows only picking up medications, not actually taking them) is compensated for by the use of questionnaires. The secondary data from the health insurance funds are available 9 months later. This time period was taken into account in the study design.
Conclusion
The roadmap for digital health adoption in cardiology is challenging but imperative to address future challenges in cardiovascular medicine. DiPaH will make an important contribution by identifying the specific barriers to the adoption of digital health technologies for arterial hypertension and providing recommendations for overcoming them.
Ethics statement
The study complies with good clinical practice in accordance with the Declaration of Helsinki and the laws and regulations applicable in Germany. The local Ethics Committee of the Brandenburg Medical School approved the study (Record number E-02-20220620). Due to the sequential approach of the mixed-methods design, the questionnaires in modules 1 and 3 will be modified based on the qualitative analysis. Therefore, an amendment will be requested from the Ethics Committee before the survey starts. If necessary, the relevant information in the German Clinical Trials Register will be updated.
Author contributions
DB, SS, ML, MH, FM, SM, E-LB, EW, GF, OJ, and MM contributed to the study conception and design. SS, DB, and ML contributed to the obtaining funding. DB, SS, SM, FM, EW, JA, E-LB, KR, and OJ contributed to the collection of data. DB, SM, FM, EW, and E-LB contributed to the analysis of data. SS, DB, ML, MH, JA, and MM contributed to the supervision. DB and SS drafted and revised the manuscript. All authors read and approved the final manuscript.
Funding
This project was supported by a grant of the Federal Joint Committee (Gemeinsamer Bundesausschuss, G-BA) in Germany from May 2022 to April 2025 (Innovation fund grant number 01VSF21042). The funder of the study had no influence in the study design.
Acknowledgments
We gratefully acknowledge Dr. Sebastian Liersch (at that time AOK Nordost) for his contributions to the study concept.
Conflict of interest
E-LB was employed by revFLect GmbH. GF and ML are the CEOs of revFLect GmbH. OJ is CEO of Hypertension Care UG, which offers the Hypertonie.App. OJ and MM are the founder of the Hypertonie.App. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
G-BA, Federal Joint Committee (Gemeinsamer Bundesausschuss); ESC, European Society of Cardiology; DiPaH, digital preventive measures for arterial hypertension.
References
1. Roth G, Mensah G, Johnson C, Addolorato G, Ammirati E, Baddour L, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
2. Forouzanfar M, Liu P, Roth G, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. (2017) 317:165–82. doi: 10.1001/jama.2016.19043
3. Parati G, Torlasco C, Omboni S, Pellegrini D. Smartphone applications for hypertension management: a potential game-changer that needs more control. Curr Hypertens Rep. (2017) 19:48. doi: 10.1007/s11906-017-0743-0
4. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
5. Egan B, Li J, Sutherland S, Rakotz M, Wozniak G. Hypertension control in the United States 2009 to 2018: factors underlying falling control rates during 2015 to 2018 across age-and race-ethnicity groups. Hypertension. (2021) 78:578–87. doi: 10.1161/HYPERTENSIONAHA.120.16418
6. Steffen A, Holstiege J, Akmatov M, Bätzing J. Trends in Prevalence of Obesity in the Outpatient Health Service Sector in Germany, 2009 to 2018. Berlin: Central Research Institute of Ambulatory Health Care in Germany (2021).
7. Kassenärztlichen Vereinigung Brandenburg [KVBB], Association of Statutory Health Insurance Physicians Brandenburg. Demand Planning in 2020 for the Area of the Association of Statutory Health Insurance Physicians Brandenburg. Potsdam: Association of Statutory Health Insurance Physicians Brandenburg (2020).
8. Holstiege J, Akmatov M, Steffen A, Bätzing J. Ischemic Heart Disease in German Ambulatory Care—Temporal Trends and Regional Variations. Berlin: Versorgungsatlas-Bericht (2020).
9. Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. (2015) 33:221–9. doi: 10.1097/HJH.0000000000000428
10. Holstiege J, Akmatov M, Steffen A, Bätzing J. [Trends in Prevalence of Hypertension in the Outpatient Health Service Sector in Germany]. Berlin: Versorgungsatlas-Bericht (2020).
11. Frederix I, Caiani E, Dendale P, Anker S, Bax J, Böhm A, et al. ESC e-Cardiology Working Group Position Paper: overcoming challenges in digital health implementation in cardiovascular medicine. Eur J Prev Cardiol. (2019) 26:1166–77. doi: 10.1177/2047487319832394
12. Frederix I, Vandenberk T, Janssen L, Geurden A, Vandervoort P, Dendale P. eEduHeart I: a multicenter, randomized, controlled trial investigating the effectiveness of a cardiac web-based elearning platform – rationale and study design. Cardiology. (2017) 136:157–63. doi: 10.1159/000448393
13. Neubeck L, Cartledge S, Dawkes S, Gallagher R. Is there an app for that? Mobile phones and secondary prevention of cardiovascular disease. Curr Opin Cardiol. (2017) 32:567–71. doi: 10.1097/HCO.0000000000000428
14. Cornejo Müller A, Wachtler B, Lampert T. [Digital divide-social inequalities in the utilisation of digital healthcare]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2020) 63:185–91. doi: 10.1007/s00103-019-03081-y
15. Initiative D21.D21-Digital-Index 2021/2022. Jährliches Lagebild zur digitalen Gesellschaft [Annual report on the digital society]. Berlin: Vertiefungsthema (2022).
16. Federal Statistical Office.Average Gross Wages per Employee in East and West Germany from 1996 to 2020. Wiesbaden: Federal Statistical Office (2022).
17. Wangler J, Jansky M. Gesundheits-Apps in der hausarztbasierten Versorgung–Empirische Befunde zur Perspektive von Allgemeinmedizinern und Patienten. mHealth-Anwendungen für chronisch Kranke. Berlin: Springer (2020). doi: 10.1007/978-3-658-29133-4_10
18. Creswell J, Klassen A, Plano Clark V, Smith K. Best Practices for Mixed Methods Research in the Health Sciences. Bethesda, MD: National Institutes of Health (2011). doi: 10.1037/e566732013-001
19. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. (2008) 337:a1655. doi: 10.1136/bmj.a1655
20. O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ. (2010) 341:c4587. doi: 10.1136/bmj.c4587
22. Norman C, Skinner H. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:e27. doi: 10.2196/jmir.8.4.e27
23. Soellner R, Huber S, Reder M. The concept of eHealth literacy and its measurement: German translation of the eHEALS. J Media Psychol. (2014) 26:29. doi: 10.1027/1864-1105/a000104
24. Sørensen K, Van den Broucke S, Pelikan J, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health. (2013) 13:948. doi: 10.1186/1471-2458-13-948
25. Pelikan J, Röthlin F, Ganahl K. Measuring comprehensive health literacy in general populations: validation of instrument, indices and scales of the HLS-EU study. Proceedings of the 6th Annual Health Literacy Research Conference. Bethesda, MD (2014).
26. Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. (2008) 57:1–29. doi: 10.1111/j.1464-0597.2007.00325.x
27. Lippke S, Ziegelmann J, Schwarzer R, Velicer W. Validity of stage assessment in the adoption and maintenance of physical activity and fruit and vegetable consumption. Health Psychol. (2009) 28:183. doi: 10.1037/a0012983
28. Schauffel N, Schmidt I, Peiffer H, Ellwart T. Self-concept related to information and communication technology: Scale development and validation. Comput Hum Behav Rep. (2021) 4:100149. doi: 10.1016/j.chbr.2021.100149
29. Bangor A, Kortum P, Miller J. An empirical evaluation of the system usability scale. Int J Hum–Comput Interact. (2008) 24:574–94. doi: 10.1080/10447310802205776
31. Arnet I, Metaxas C, Walter P, Morisky D, Hersberger K. The 8-item Morisky Medication Adherence Scale translated in German and validated against objective and subjective polypharmacy adherence measures in cardiovascular patients. J Eval Clin Pract. (2015) 21:271–7. doi: 10.1111/jep.12303
32. Morisky D, Ang A, Krousel-Wood M, Ward H. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. (2008) 10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x
34. Onwuegbuzie A, Leech N. Validity and qualitative research: An oxymoron? Qual Q. (2007) 41:233–49. doi: 10.1007/s11135-006-9000-3
35. Tivian XI GmbH.Online Survey Software: Surveys Made Easy With Unipark. Cologne: Tivian XI GmbH (2021).
36. Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. (2008) 337:a1035. doi: 10.1136/bmj.a1035
37. Tromp J, Jindal D, Redfern J, Bhatt A, Séverin T, Banerjee A, et al. World heart federation roadmap for digital health in cardiology. Global Heart. (2022) 17:61. doi: 10.5334/gh.1141
38. Milani R, Lavie C, Bober R, Milani A, Ventura H. Improving hypertension control and patient engagement using digital tools. Am J Med. (2017) 130:14–20. doi: 10.1016/j.amjmed.2016.07.029
39. Albini F, Xiaoqiu L, Torlasco C, Soranna D, Faini A, Ciminaghi R, et al. An ICT and mobile health integrated approach to optimize patients’ education on hypertension and its management by physicians: the Patients Optimal Strategy of Treatment(POST) pilot study. Annu Int Conf IEEE Eng Med Biol Soc. (2016) 2016:517–20. doi: 10.1109/EMBC.2016.7590753
Keywords: hypertension, digital prevention measures, mixed-methods design, digital health literacy, rural regions
Citation: Bruch D, Muehlensiepen F, May S, Wengemuth E, Johannsen O, Reber KC, Blankenstein E-L, Fleige G, Middeke M, Albes J, Heinze M, Lehnen M and Spethmann S (2023) Digital preventive measures for arterial hypertension (DiPaH) – a mixed-methods study protocol for health services research. Front. Cardiovasc. Med. 9:1089968. doi: 10.3389/fcvm.2022.1089968
Received: 04 November 2022; Accepted: 22 December 2022;
Published: 10 January 2023.
Edited by:
Guido Iaccarino, University of Naples Federico II, ItalyReviewed by:
Susana Pedras, Centro Hospitalar Universitário do Porto, PortugalVincenzo De Luca, Università degli Studi di Napoli Federico II, Italy
Copyright © 2023 Bruch, Muehlensiepen, May, Wengemuth, Johannsen, Reber, Blankenstein, Fleige, Middeke, Albes, Heinze, Lehnen and Spethmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dunja Bruch, ZHVuamEuYnJ1Y2hAbWhiLWZvbnRhbmUuZGU=
†ORCID: Dunja Bruch, orcid.org/0000-0002-9511-8487; Felix Muehlensiepen, orcid.org/0000-0001-8571-7286; Susann May, orcid.org/0000-0003-3847-4861; Eileen Wengemuth, orcid.org/0000-0001-8213-2426; Martin Middeke, orcid.org/0000-0003-2228-7359; Johannes Albes, orcid.org/0000-0003-4722-3896; Martin Heinze, orcid.org/0000-0003-3645-1033; Sebastian Spethmann, orcid.org/0000-0003-0987-8007
 Dunja Bruch
Dunja Bruch Felix Muehlensiepen2,3†
Felix Muehlensiepen2,3† Susann May
Susann May Eileen Wengemuth
Eileen Wengemuth Gerrit Fleige
Gerrit Fleige Sebastian Spethmann
Sebastian Spethmann