- 1Department of Cardiology, The Second Xiangya Hospital of Central South University, Changsha, China
- 2Department of Cardiology, Wuhan Renmin Hospital of Wuhan University, Wuhan, China
Background: Mahaim-type accessory pathways (MAPs) are rare accessory pathways (APs) with specific properties. They are mostly located in the right side of the heart but rarely exist on the left side.
Objectives: This study aims to analyze the clinical and electrophysiological (EP) characteristics of both-sided MAPs.
Methods: A total of 2,249 patients with AP from our center were enrolled between 1 January 2011 and 27 March 2022. During the EP study (EPS) 17 patients were diagnosed with MAPs (right-sided: n = 13, left-sided: n = 4) according to the properties of Mahaim fibers.
Results: MAPs constitute 0.75% of all APs. Out of 1,553 patients with left-sided APs, four patients (0.26%) were diagnosed with Mahaim fiber-mediated tachycardia. Out of 696 patients with right-sided APs, 13 patients (1.9%) were diagnosed with Mahaim fiber. Most Mahaim fibers were located at the free wall of the tricuspid and mitral annuli. Seven patients of right-sided MAPs were of atriofasicular type, six patients had right-sided MAPs, and all of the patients with left-sided MAPs were of atrioventricular (AV) type. The M potential only was detected in long-length MAPs. Coexistence with other supraventricular tachycardias (SVTs) was also observed both in patients with right-sided and left-sided MAPs. All the patients underwent radiofrequency ablation successfully. Only one patient had tachycardia recurrence during a follow-up.
Conclusion: Although MAPs are commonly located at right sides, left sites are not impossible. The M potential contributes to the improvement of the successful ablation.
Introduction
Mahaim and Benatt first described the Mahaim fiber leading to wide QRS tachycardia (1). Mahaim fibers are uncommon accessory pathways (APs) with specific characteristics. Mahaim-type accessory pathways (MAPs) usually originate from the atrial tissue, cross the atrioventricular (AV) junctions, and finally, insert into the branch of the His bundle (HB) (2). Therefore, MAPs are displayed as anterograde decremental conduction (AV-node-like) and a lack of retrograde conduction. MAPs are commonly located in the right-sided lateral region of the tricuspid annulus (3, 4). However, paraseptal and left-sided MAPs are rarely reported (5–7). Herein, we report on seven patients with right-sided MAPs and four patients with left-sided MAPs. The aim of this study is to describe the electrocardiographic and electrophysiologic characteristics in 17 patients with Mahaim fibers and to compare these findings between the patients with right-sided Mahaim fibers and those with left-sided Mahaim fibers.
Materials and methods
This study enrolled 17 patients with MAPs between 1 January 2011 and 27 March 2022. The various electrophysiological (EP) properties of Mahaim fiber were retrospectively analyzed. Informed and written consent was obtained from study subjects. The study was approved by the Ethics Committee of the Second Xiangya Hospital of Central South University.
EP study
During the study period, programmed electrical stimulation and recordings of the 12-lead surface ECG and intracardiac electrograms were performed by an electrophysiology system (Lead 2000; Sichuan Jinjiang Electronic Science and Technology Co., Ltd). The 3-D electroanatomic mapping and ablation were performed by CARTO system [Biosense Webster Co. or EP study (EPS); HT-Viewer system]. A Decapolar catheter was placed into the coronary sinus through the right internal jugular vein. Three quadripolar catheters were, respectively, positioned at the right ventricular (RV) apex, His bundle (HB), and right atrium. Programmed atrial stimulation and ventricular stimulation were performed to determine the antegrade conduction pattern to the ventricle and the retrograde conduction pattern to the atrium. For patients with right-sided MAP, atrial programmed stimulation induced tachycardia with broad complex LBBB surface ECG morphology. Left-sided MAP in patients induced tachycardia with broad complex RBBB surface ECG morphology (Figure 1). The M potential was recorded during sinus rhythm and tachycardia. The characteristics of Mahaim fibers were defined as follows: (1) baseline normal QRS without pre-excitation or minimal pre-excitation; (2) programmed atrial pacing inducing manifest pre-excitation and a progressive increase in AH and AV interval along with a shortening of HV interval (Figure 2); (3) absence of retrograde conduction over the AP during ventricular stimulation; and; (4) during antegrade pre-excitation, SVT retrograde His bundle activation was detected.
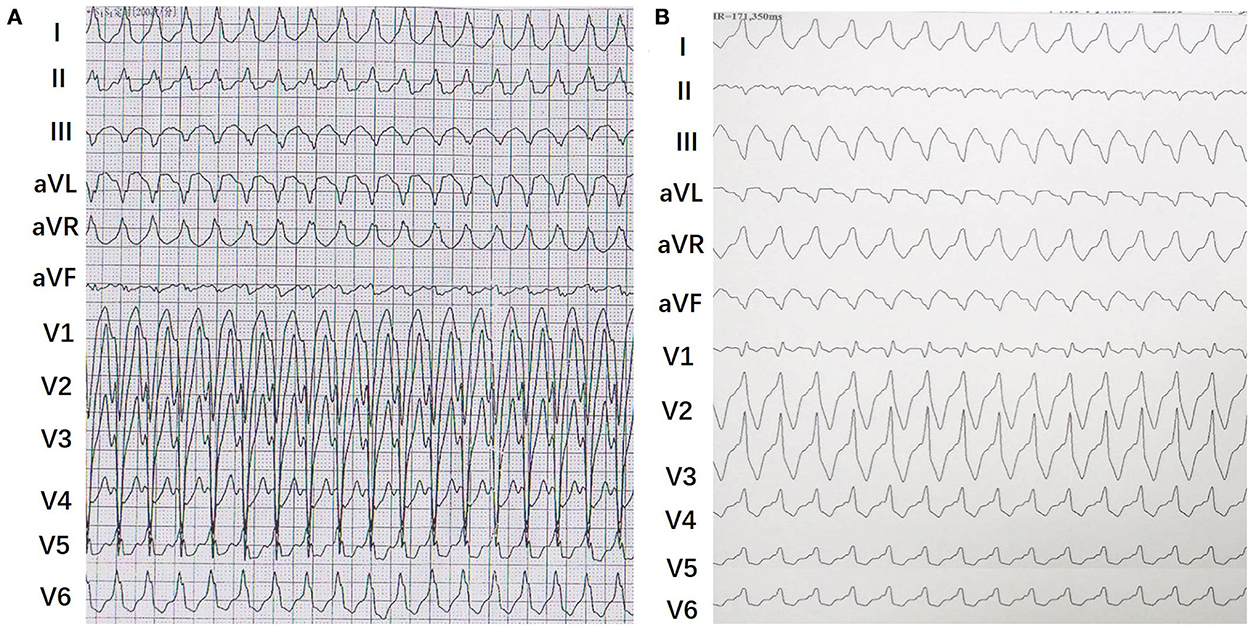
Figure 1. Representative 12-leads surface electrocardiograms of tachycardia in patients with right-sided and left-sided Mahain-type accessory pathways (MAPs). (A) It showed a typical wide QRS complex tachycardia with a left bundle branch block (LBBB) pattern. (B) It showed a typical wide QRS complex tachycardia with a right bundle branch block (RBBB) pattern.

Figure 2. Representative intracardiac electrocardiogram from a patient with right-sided MAP and a patient with left-sided MAP. (A) Atrial programmed atrial stimulation (S1S1) induced a pre-excitation of QRS complex with LBBB pattern. It presents antegrade long conduction with lengthening of the A-H interval and A-V interval, a contemporary shortening of the H-V interval. (B) Atrial programmed stimulation (S1S1) induced tachycardiac with a broad QRS complex. The tachycardia has an RBBB pattern, long AV interval, and short VA interval. The earliest atrial activation was detected at the His-bundle electrodes during the tachycardia.
VAbl-QRS was defined as the interval between the beginning of ventricular ECG and the beginning of the QRS complex. The type of MAPs VAbl-QRS was determined by the VAbl-RVApex interval and was treated as the interval between the beginning of ventricular ECG at the successful ablation point and the ventricular ECG recorded from the RV apex. Vabl-RVapx intervals contribute to the guidance of MAPs ablation.
RF ablation
After MAP was confirmed by the EP properties, a catheter (8 Fr, 3.5-mm-tip electrode, DD or JJ curve, 1-6-2 mm spacing, 115 insertion length, Thermocool SmartTouch SF® Biosense Webster Co.; or EPS, HT-Viewer system) was used for mapping and ablation. The MAPs were ablated with a target contact force of 10–15 g, a target ablation index (AI) of 500–600 watts/grams/second, and an impedance drop of 5–10 Ω. The tricuspid annulus and mitral annulus were mapped during sinus rhythm. For the left-sided MAPs, the transseptal approach was performed. The M potential was detected between atrial and ventricular intracardiac potential during sinus rhythm (Figure 3). The AM interval (between the beginning of the atrial electrogram and the M potential) and MV interval (between the M potential and the beginning of the ventricular electrogram) were recorded. The M potential was recorded at the atrial insertion site of the Mahaim fibers. It was considered a good predictor of a suitable ablation site (8). Successful ablation includes no ventricular pre-excitation, no AP conduction, and no inducible tachycardia observed during repeated programmed stimulation.
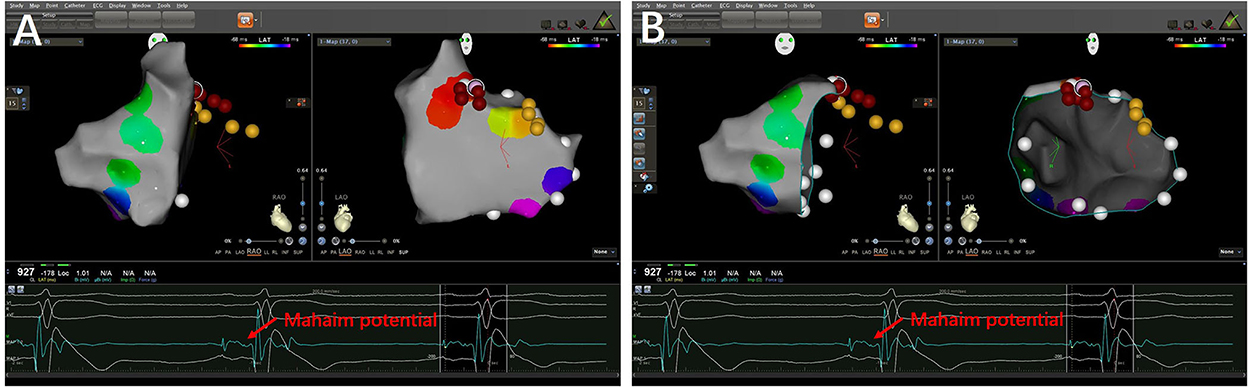
Figure 3. 3-D mapping images of successful ablation sites in a patient with right-sided MAP. (A) The targets of Mahaim fiber located at the right anterior wall of tricuspid annulus (12:00 p.m.). (B) The target in ablated catheter presented Mahaim potentials.
Statistical analysis
SPSS software (version 23.0; SPSS, Inc., Chicago, IL) was used for statistical analyses. The medians and minimum-maximum were presented for the non-normally distributed variables. The Mann-Whitney U-test was performed to compare the differences in non-normally distributed variables between the right-sided group and the left-sided group. Categorical variables were analyzed by the chi-square test. A p-value < 0.05 was considered statistically significant.
Results
The records of 2,249 patients with AP who underwent EPS were evaluated. Among these patients, 1,553 (69.1%) were diagnosed with left-sided APs and 696 patients (30.9%) were diagnosed with right-sided APs. In our center, MAPs constituted 0.75% of all APs. Out of 1,553 patients with left-sided APs, four patients (0.26%) were diagnosed with Mahaim fiber-mediated pathway. Out of 696 patients with right-sided APs, 13 patients (1.9%) were diagnosed with MAPs. According to the abovementioned results, it was observed that these APs were more often right-sided rather than left-sided.
Clinical characteristic analysis
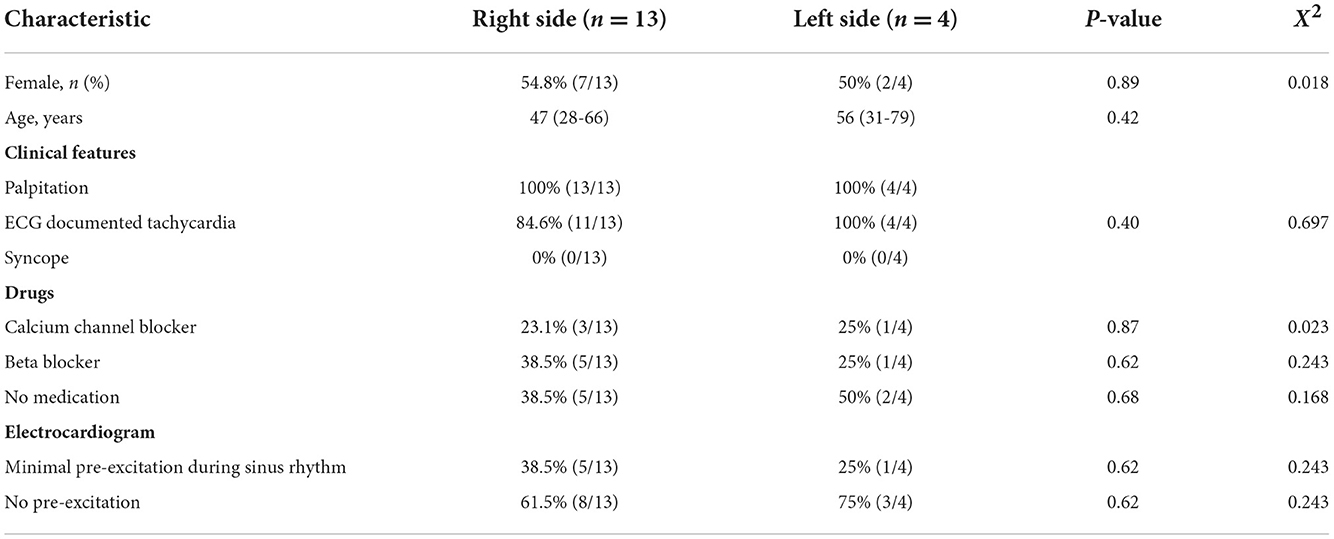
The baseline characteristics of the 17 patients are summarized in Table 1. Approximately 54.8% were female in the right-sided group, while 50% were male in the left-sided group. The mean age was 47 (28–66) years in the right-sided group, while it was 56 (31–79) years in the left-sided group. All of the patients had palpitations, and none of them had syncope. Antiarrhythmic drugs were prescribed before RF ablation therapy for three patients in the right-sided group and two patients in the left-sided group. A resting 12-lead ECG revealed a minimal pre-excitation during sinus rhythm in five patients of the right-sided group and in one patient of the left-sided group.
Electrophysiological study
Tables 2, 3 show the EPS characteristics of the patients studied. Atrial pacing protocol showed manifest pre-excitation with decremental AV conduction in all patients. With incremental atrial pacing, AH was prolonged, HV was shortened, and tachycardia was induced (Figure 2).
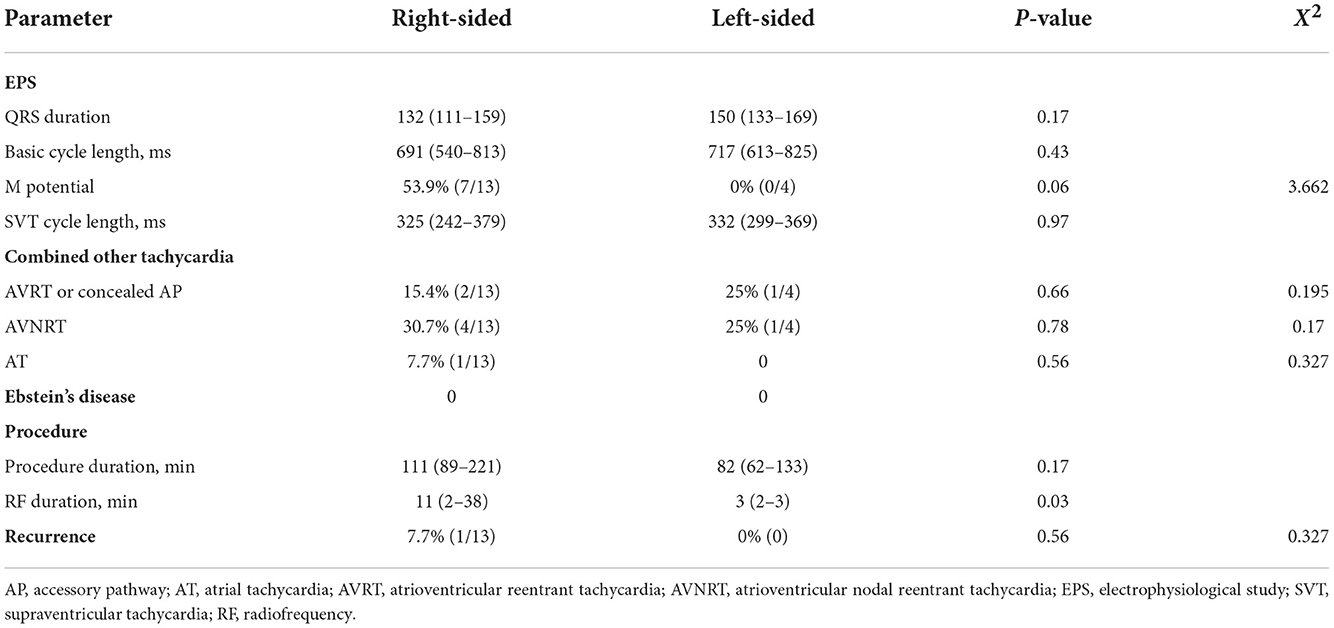
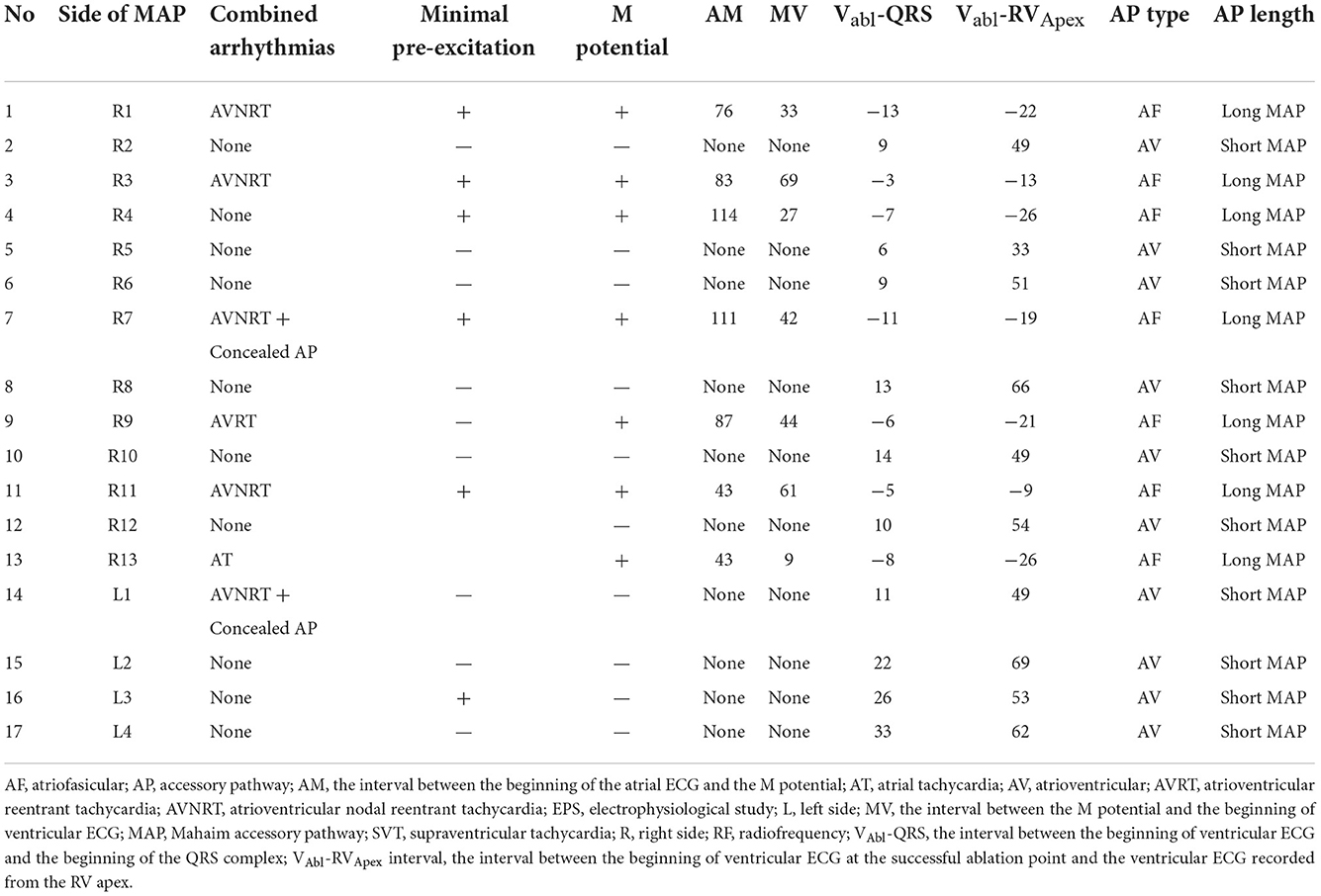
Table 2. Electrophysiological data from 17 patients with Mahaim-type accessory pathways who underwent electrophysiological study.
For right-sided and left-sided MAPs, the median paced duration of the QRS interval was 132 ms (111–159) and 150 ms (133–169), respectively (P = 0.17). The median of basic cycle length was 691 ms in the right-sided and 717 ms in the left-sided groups, respectively (P = 0.43). Only seven patients with right-sided MAPs presented with “Mahaim potential,” but no patients with left-sided MAPs were observed to have M potentials. After ablation, all of the M potentials were eliminated. The median SVT cycle length was 325 ms in the right-sided and 332 ms in the left-sided groups, respectively (P = 0.97).
Among 11 patients with right-sided MAPs, there were two patients found with atrioventricular reentrant tachycardia (AVRT) or concealed AP, four patients accompanied with atrioventricular nodal reentrant tachycardia (AVNRT), and one patient accompanied with AT. In four patients with left-sided MAPs, only one patient was induced with AVRT or concealed AP and one patient was accompanied with AVNRT. None of the patients had Ebstein's disease. Radiofrequency ablation was delivered in temperature-controlled mode at a target temperature of 55–60°C and a power output of 30–35 W in all the cases. All of the patients underwent successful ablation, and the median procedure duration time was 111 min in the right side and 82 min in the left side groups, respectively (P = 0.17). The median RF ablation duration time was 11 min in the right side and 3 min in the left side groups, respectively (P = 0.03). Only one patient with right-sided MAPs had recurrence during the 1-year follow-up.
According to our study, MAPs were located on the tricuspid annuli (right-sided, n = 13) and mitral annuli (left-sided, n = 4). In the right-sided group, one patient had anteroseptal MAP, two patients with anterolateral MAP, six patients with lateral MAPs, two patients with posterolateral MAP, and two patients with posteroseptal MAP. In the left-sided group, there were three patients with anterolateral MAPs and one patient with posterolateral MAP (Figure 4).
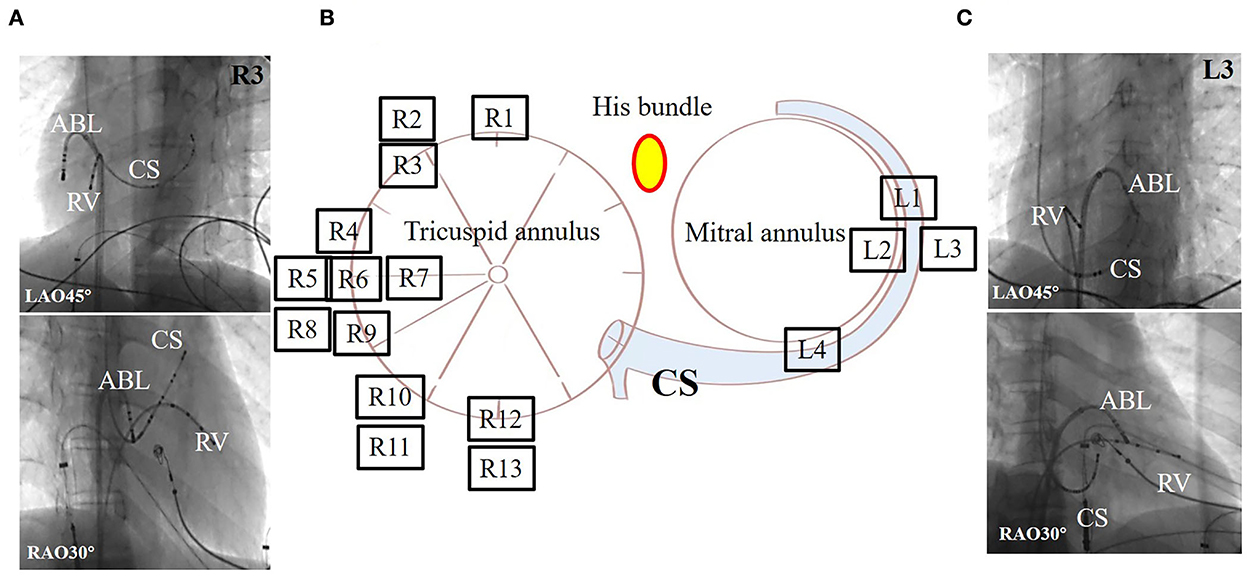
Figure 4. Representative fluoroscopic images of successful ablation sites in two patients with Mahaim-type accessory pathway of 17 patients. (A) The fluoroscopic images in a patient with right-sided MAP. (B) Solid circles show radiofrequency ablation targets around the tricuspid and mitral annuli. There were 13 patients showing MAPs around the tricuspid annulus, but for most patients they were located at the free wall. In total, four patients had them around the mitral annulus, but in most of the patients, it was located at the free wall. The dot was represented as his bundle. (C) The fluoroscopic images in a patient with left-sided MAP. ABL, ablation catheter; CS, coronary sinus; L, patient with left-sided Mahaim; LAO, left anterior oblique; R, patient with right-sided Mahaim; RAO, right anterior oblique; RV, right ventricular.
Discussion
This study evaluated clinical and EP characteristics in patients with right-sided and left-sided MAPs. The main findings were as follows: (1) the incidence of MAPs was very low in APs. MAPs mainly existed in the lateral aspect of the tricuspid annulus, but could also exist in the mitral annulus. (2) The success rate of catheter ablation was very high. (3) Not all of the right-sided MAPs have M potential, but we did not detect the M potential in the left-sided MAP. The M potential provided a suitable target for the ablation of MAPs and improved the successful ablation.
Mahaim-type accessory pathways are rare APs with unique properties. They were usually found in the right side of the heart. MAPs in the left side are very rare, and only a few cases have been reported. In our center, MAPs constitute 0.75% of all APs. Out of 1,553 patients with left-sided APs, four patients (0.26%) were diagnosed with Mahaim fiber-mediated pathway. MAPs in right-sided patients are more common than in left-sided. Consistent with a previous study (9), MAPs were commonly located at the lateral tricuspid annulus site (10–12). However, the incidence in our study is much lower than others (9). This may be due to regional differences between different countries. Ozcan et al. indicated that it was possibly ascribed to the fact that their center is a referral hospital for atypical AP ablation. Incidence may vary from region to region or race to race. Therefore, it is a more representative response to the prevalence of MAPs.
Yanni et al. demonstrated that the “primary ring” formed the AV node and the AV conduction axis which only contributed to the tricuspid annulus. MAPs originated from inferior extensions of the AV node. Therefore, right-sided MAPs are more commonly found than left-sided MAPs. MAPs are AV ring tissues, which are the remnants of the primary ring and have the similar properties to AV node and Kent bundle (13). Therefore, MAPs display AV node-like conduction properties and a slight pre-excitation. Recently, more cases with left-sided MAPs were reported (9). It was hypothesized that left-sided MAPs were attributed to a defect in embryological migration accompanied by AV isolation defect.
The length of the MAPs was determined by Vabl-QRS intervals. If the earliest ventricular potentials in the ablated MAPs were later at QRS complexes (a negative Vabl-QRS interval), it was considered long-length MAPs and defined as atriofasicular MAPs (Table 3). It was a long accessory from atrial insertion to ventricular insertion. If the earliest ventricular potentials in the ablated MAPs were preceded the surface QRS complexes (a positive Vabl-QRS interval), it was considered short-length MAPs and defined as AV MAPs (Figure 5). In those cases, all of the left-sided MAPs and parts of the right-sided MAPs were short-length MAPs and AV MAPs. Long-length MAPs were only existed in the right side. It indicated that long-length MAPs were just only appeared in the right-sided. However, the left-sided MAPs just only presented as short-length MAPs. Short-length MAPs also existed in the right side. In our cases, the M potential was not detected in all patients. We found that parts of patients with right-sided MAPs and all of the patients with left-sided MAPs were not observed M potential. M potential were only detected in long-length MAPs or atriofasicular MAPs. The M potential is helpful for the improvement of successful ablation. The earliest ventricular potential as well as Vabl-RVapx intervals contribute to the guidance of MAPs ablation in patients without M potentials.
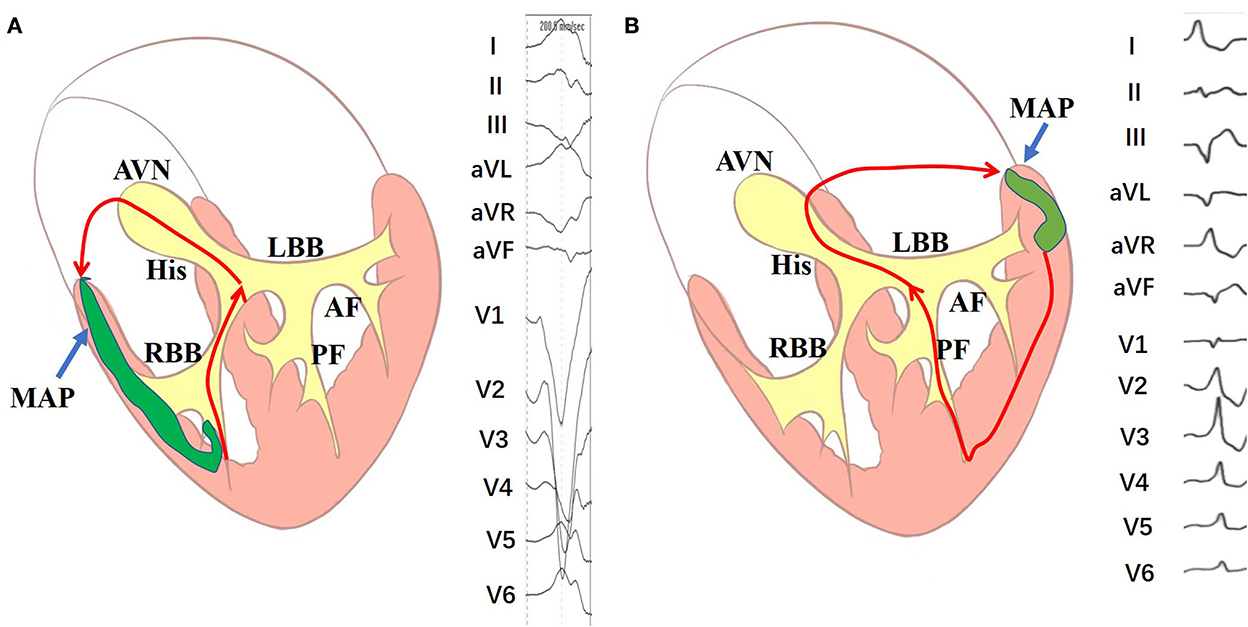
Figure 5. Schematic diagram of the mechanism of the long-length and short-length Mahaim-mediated tachycardias. (A) The mechanism of right-sided long-length Mahaim-mediated tachycardias. (B) The mechanism of left-sided short-length Mahaim-mediated tachycardias. AF, anterior fascicle; AVN, atrioventricular node; LBB, left bundle branch; MAP, Mahaim accessory pathway; PF, posterior fascicle; RBB, right bundle branch.
Both the right-sided and left-sided MAPs have similar clinical and EP characteristics. In the present study, we found that the AM and the MV intervals were longer in the right-sided MAPs than that in the left-sided MAPs. Ozcan et al. demonstrated that they were associated with decremented conduction rather than the length of the MAPs. Previous studies have reported that the coexistence of AVNRT in patients with right-sided MAPs was from 9 to 40% (9, 14–16). However, in our center experience, we found that the incidence of AVNRT was 42.8% and the incidence of AVRT was 28.3%. Ozcan et al. found that no AVNRT coexisted in patients with left-sided MAPs (9). However, in our study, we found that one patient was with AVNRT and one patient was with AVRT. It indicated that the coexistence was not specific to the right-sided MAPs but also existed in the left-sided MAPs.
Limitations
The present study included only 17 patients with MAPs, which is a very small number for an observational, retrospective, and single-center study. More patients with MAPs in other EP centers could be involved in future studies.
Conclusion
The reported incidence of MAPs is very low. MAPs are generally located in the right side and occasionally the left. The M potential only is detected in long-length MAPs. The coexistence of other arrhythmias is also a common phenomenon. The radiofrequency ablation of MAPs has high success rates.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Second Xiangya Hospital of Central South University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MC, ZWa, and SZ participated in the study design and drafted the manuscript. HY, ZL, XL, ZWu, SW, and LH contributes to data collection. MC and ZWu were responsible for writing the manuscript. HY, ZL, XL, and QL contributes to the manuscript revision. All authors contributed to the article and approved the submitted version.
Funding
Financial support was obtained from the National Natural Science Foundation of China (Grant No. 81800302) and the Provincial Natural Science Foundation of Hunan (Grant No. 2019JJ50871).
Acknowledgments
We would like to thank Aitian Gao and the Chinese HT-View System for their support during the study of these cases.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mahaim I, Benatt A. Nouvelles re 'cherches sur les connections supe 'rieures de la branche du faisceau de His-Tawara avec cloison interventriculaire. Cardiologia. (1937) 1:61–76. doi: 10.1159/000164567
2. Gallagher JJ, Smith WM, Kasell JH, Benson DWJ, Sterba R, Grant AO. Role of Mahaim fibers in cardiac arrhythmias in man. Circulation. (1981) 64:176–89. doi: 10.1161/01.CIR.64.1.176
3. Gillette PC, Garson A Jr, Cooley DA, McNamara DG. Prolonged and decremental antegrade conduction properties in right anterior accessory connections: wide QRS antidromic tachycardia of left bundle branch block pattern without Wolff-Parkinson-White configuration in sinus rhythm. Am Heart J. (1982) 103:66–74. doi: 10.1016/0002-8703(82)90531-2
4. Chen M, Li X, Wu Z, Liu Z, Hu L, Liu Q, et al. Right-sided Mahaim-mediated tachycardia combined with atypical atrioventricular nodal reentrant tachycardia and left free wall accessory pathway: a case report. Ann Noninvasive Electrocardiol. (2022) 2022:e12964. doi: 10.1111/anec.12964
5. Francia P, Pittalis MC, Ali H, Cappato R. Electrophysiological study and catheter ablation of a Mahaim fibre located at the mitral annulus–aorta junction. J Interv Card Electrophysiol. (2008) 23:153–7. doi: 10.1007/s10840-008-9279-1
6. Tada H, Nogami A, Naito S, Oshima S, Tanigughi K, Kutsumi Y. Left posteroseptal Mahaim fiber associated with marked longitudinal dissociation. Pacing Clin Electrophysiol. (1999) 22:1696–9. doi: 10.1111/j.1540-8159.1999.tb00393.x
7. Faizel O, Peter JS, Andre Ng G. Looks like VT but isn't—successful ablation of a left free wall accessory pathway with Mahaim-like properties. Indian Pacing Electrophysiol J. (2009) 9:112–8.
8. McClelland JH, Wang X, Beckman KJ, Hazlitt HA, Prior MI, Nakagawa H et al. Radiofrequency catheter ablation of right atriofascicular (Mahaim) accessory pathways guided by accessory pathway activation potentials. Circulation. (1994) 89:2655–66. doi: 10.1161/01.CIR.89.6.2655
9. Ozcan EE, Turan OE, Akdemir B, Inevi UD, Yilancioglu RY, Baskurt AA, et al. Comparison of electrophysiological characteristics of right- and left-sided Mahaim-type accessory pathways. J Cardiovasc Electrophysiol. (2021) 32:360–9. doi: 10.1111/jce.14852
10. Gormel S, Yasar S, Yildirim E, Asil S, Baris VO, Gokoglan Y, et al. Comprehensive assessment of Mahaim accessory pathways' anatomic distribution. J Int Med Res. (2022) 50:3000605211069751. doi: 10.1177/03000605211069751
11. Bohora S, Dora SK, Namboodiri N, Valaparambil A, Tharakan J. Electrophysiology study and radiofrequency catheter ablation of atriofascicular tracts with decremental properties (Mahaim fibre) at the tricuspid annulus. Europace. (2008) 10:1428–33. doi: 10.1093/europace/eun283
12. Sternick EB, Fagundes ML, Cruz FE, Timmermans C, Sosa EA, Rodriguez LM, et al. Short atrioventricular Mahaim fibers: observations on their clinical, electrocardiographic, and electrophysiologic profile. J Cardiovasc Electrophysiol. (2005) 16:127–34. doi: 10.1046/j.1540-8167.2004.40508.x
13. Sternick EB, Gerken LM, Vrandecic M. Appraisal of Mahaim automatic tachycardia. J Cardiovasc Electrophisiol. (2002) 13:244–9. doi: 10.1046/j.1540-8167.2002.00244.x
14. Grogin HR, Lee RJ, Kwasman M, Epstein LM, Schamp DJ, Lesh MD, et al. Radiofrequency catheter ablation of atriofascicular and nodoventricular Mahaim tracts. Circulation. (1994) 90:272–810. doi: 10.1161/01.CIR.90.1.272
15. Heald SC, Davies DW, Ward DE, Garratt CJ, Rowland E. Radiofrequency catheter ablation of Mahaim tachycardia by targeting Mahaim potentials at the tricuspid annulus. Br Heart J. (1995) 73:250–7. doi: 10.1136/hrt.73.3.250
16. Kottkamp H, Hindricks G, Shenasa H, Chen X, Wichter T, Borggrefe M, et al. Variants of preexcitation specialized atriofascicular pathways, nodofascicular pathways, and fasciculoventricular pathways: electrophysiologic findings and target sites for radiofrequency catheter ablation. J Cardiovasc Electrophysiol. (1996) 7:916–30. doi: 10.1111/j.1540-8167.1996.tb00466.x
Keywords: Mahaim, accessory pathway, decremental, tachycardiac, right-sided, left-sided
Citation: Chen M, Wang Z, Wang S, Liu Z, Li X, Yang H, Hu L, Wu Z, Li Q and Zhou S (2022) Electrophysiological characteristics of right- and left-sided Mahaim accessory pathways: A single-center experience in China. Front. Cardiovasc. Med. 9:1052465. doi: 10.3389/fcvm.2022.1052465
Received: 24 September 2022; Accepted: 08 November 2022;
Published: 07 December 2022.
Edited by:
Bart Mulder, University Medical Center Groningen, NetherlandsReviewed by:
Nikolaos Fragakis, Aristotle University Medical School, GreeceEnes Gul, Istanbul University, Turkey
Copyright © 2022 Chen, Wang, Wang, Liu, Li, Yang, Hu, Wu, Li and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhihong Wu, d3V6aGlob25nOTE1QGNzdS5lZHUuY24=
 Mingxian Chen
Mingxian Chen Zhuo Wang
Zhuo Wang Songyun Wang
Songyun Wang Zhenjiang Liu
Zhenjiang Liu Xuping Li
Xuping Li Hui Yang
Hui Yang Lin Hu
Lin Hu Zhihong Wu
Zhihong Wu Qiming Li
Qiming Li Shenghua Zhou
Shenghua Zhou